Abstract
An effective approach for determining the clinical classification of heart failure (HF) patients is to estimate cardiac hemodynamics during exercise. This approach is further strengthened when measurements including cardiac power are used to describe cardiac hemodynamics. We hypothesize cardiac power quantifies the hemodynamic and pressure generating capability of the heart; relating with exercise tolerance better than traditional measurements in HF.
Keywords: cardiac power, stroke work, circulatory power, prognosis, peak exercise, HFpEF, HFrEF
INTRODUCTION: DOES CARDIAC FUNCTION MATTER MOST IN HEART FAILURE?
Chronic heart failure (HF) is a clinical syndrome that is a leading cause of hospitalizations and mortality in developed countries (11, 30). Heart failure is a syndrome which burdens patients but also poses significant challenges to healthcare systems and providers (11, 23). Heart failure is no longer considered primarily an impairment in systolic function, but it is now recognized that nearly half of HF cases are patients with preserved ejection fraction (HFpEF) (4, 28, 30). Most importantly, however, the evidence currently indicates HFpEF share a mortality risk similar to HF patients with reduced ejection fraction (HFrEF) (4, 28).
The New York Heart Association (NYHA) functional classification system is useful for assessing syndrome severity and prognosis in HF (11). Classification of HF using NYHA criteria is based on symptoms (e.g. dyspnea, fatigue, or peripheral edema) and perception of exercise tolerance. However, despite the value of the NYHA class system for the clinical evaluation of HF, little evidence suggests that NYHA functional class correlates with the magnitude of objective signs of cardiovascular impairment in these patients (31, 34). The lack of close association between NYHA functional class and cardiovascular impairment in HF is noteworthy because observations from cardiopulmonary exercise testing suggest direct measurements of cardiac and or pulmonary system function provide information which strongly relate with prognosis in patients (9, 13, 18, 28, 34). Therefore, complimentary to the NYHA functional class system is the Weber-Janicki classification system, which suggests evaluation of functional impairment (e.g. exercise tolerance) based on traditional cardiopulmonary responses (e.g. oxygen uptake and cardiac index) during exercise testing is critical in the clinical evaluation of HF (36). As such, the numerous but variable evidence supporting the current models for the clinical classification of HF has led our group to question which system, index, or indices are optimal for evaluating syndrome severity and prognosis in HF.
Heart failure syndrome is a pathophysiological state that evolves because of impaired cardiac function concurrent with comorbidities, which frequently include hypertension and coronary artery diseases (11, 28, 30). Closely associated with mortality in HF and commonly recognized as consequences of this cardiovascular syndrome include pulmonary system and cardiac dysfunction irrespective of preserved or reduced ejection fraction percentage (EF%) classification (9, 11, 13, 18, 28, 39). Cardiac dysfunction in HF is often described using values of cardiac output (Q), stroke volume (SV), or resting EF% which are abnormally low and may be useful for estimating syndrome severity and prognosis in HFrEF and HFpEF (8, 11, 18, 28). Although, despite the common use of resting EF% to describe HF severity in the clinical setting, this index is a poor indicator of exercise tolerance and cardiac reserve (i.e. change from rest to peak exercise) in these individuals (32). In contrast, although Q and SV measures at rest may not fully encapsulate the magnitude of cardiac dysfunction in HF, exercise cardiac function assessment is known to elicit hemodynamic responses which provide critical information pertaining to the magnitude of absolute and reserve cardiac impairment in these patients (1, 5, 11, 28). Further, it has been demonstrated that exercise cardiac hemodynamic responses may be the strongest indicators of prognosis in HF (18, 37).
In addition to the more recognized impairments related to cardiac dysfunction or low ventilatory efficiency (i.e. high ratio of minute ventilation to the production of carbon dioxide [VE/VCO2 slope]), HF patients have also been observed to demonstrate low forced expiratory volume in one second, attenuated capacity for gas transfer within lungs, and low oxygen consumption (VO2) (24, 25, 27, 33, 39). Moreover, when assessed during exercise, pulmonary system function worsens in HF, which is consistent with the increased hemodynamic stress imposed on the lungs due to the hemodynamic backup of fluid as a result of the blunted Q and SV responses to exercise in these individuals (8, 24, 25, 27, 39). Nevertheless, despite the supporting evidence highlighting the value of pulmonary or ventilatory markers in describing syndrome severity or predicting prognosis in HF, independent use of these indices in comparison to cardiac hemodynamics for the clinical classification of patients remains open to question (18, 37). Therefore, although there is ample evidence which demonstrates the importance of the information gathered from symptoms and signs of HF which comprise the criteria for NYHA functional and Weber-Janicki classification systems, the question “What surrogate index or indices of cardiac and or pulmonary function best estimate syndrome severity and prognosis in HF?” remains a challenge. Although the factors which may influence an answer to the above question are broad, to ensure brevity and conciseness, we aimed to focus our answer to this question with evidence that favors metrics closely related to the blood flow and pressure generating capability of the heart, particularly during exercise, in determining a robust index or set of indices for the clinical classification of HF irrespective of categorization based on EF%. Cardiac pumping capacity and cardiac pumping reserve in healthy individuals and in HF may be described using non-traditional measures such as cardiac power (CP) and stroke work (SW) (18, 22). In contrast to Q and SV, both CP (Q × mean arterial pressure [MAP]) and SW (SV × MAP) directly account for the contribution of cardiac blood flow to the maintenance of arterial pressure which are both necessary for the maintenance of perfusion pressure and oxygen delivery to metabolically active tissue. Exercise measures of CP and SW in HF are suggested to be particularly useful in describing cardiac responsiveness to hemodynamic stress such as that caused by exercise (i.e. cardiac reserve) (18, 22). Moreover, observations from exercise studies suggest that CP and SW may be the strongest indicators of prognosis in HF compared to traditional measures of Q and SV, as well as in comparison to ventilatory markers (18, 22). Indirect non-invasive measurements of CP and SW, which include circulatory power (CircP = VO2 × MAP) and pulse work (PW = VO2/heart rate × MAP), respectively, may also estimate cardiac pumping capacity while also being valuable indices for predicting prognosis in HF (7, 38).
Therefore, because of an emerging body of evidence supporting the use of non-traditional measures of cardiac pumping capacity for assessing syndrome severity and prognosis related to cardiac dysfunction in HF, we hypothesized that both direct and indirect metrics specific to estimating cardiac pumping capacity, specifically during exercise, can be used to strengthen the clinical classification of HFrEF and HFpEF. We present this hypothesis schematically in Figure 1 which suggests that the strength of index for the evaluation of HF increases moving top to bottom, in addition to exercise evaluation demonstrating higher value compared to rest.
Figure 1.
Schematic figure which illustrates our hypothesis that metrics specific to describing the pumping capability of the heart, specifically during exercise, can provide robust estimates for the clinical classification of both HFrEF and HFpEF.
TECHNIQUES USED FOR MEASURING CARDIAC FUNCTION IN HEART FAILURE
The optimal technique for estimating Q and SV is the direct Fick method (15, 17), however, this technique requires arterial catheterization with arterial and mixed venous blood samples which make it not only invasive but impractical for routine clinical and research use. Other techniques which require right heart catheterization (e.g. thermodilution or continuous Q) can be used for not only measuring Q and SV but also cardiac pressures (15). However, similar to direct Fick, these right heart catheterization techniques are highly invasive and require the availability of a catheterization laboratory and cardiology team.
In contrast, echocardiography (ECHO) is a non-invasive technique which can be used to describe both cardiac structure and function, and therefore has become widely used in clinical and research settings for assessing cardiac health in HF. Validation studies have presented evidence which suggest that ECHO agrees with the “gold standard” (i.e. direct Fick) for estimating Q and SV at rest and during exercise in HF (16, 19). However, use of ECHO for the precise and accurate measurement of Q and SV at rest and particularly during exercise poses its own set of challenges, namely that it is a highly user dependent technique requiring highly skilled trained sonographers to acquire images, and equally skilled cardiologists to interpret the images accurately for clinical purposes (20).
Accordingly, there remains considerable interest in other non-invasive techniques such as inert gas breathing (e.g. acetylene, nitrous oxide, or carbon dioxide gases) for the measurement of cardiac hemodynamics at rest and during exercise in HF. Observations from comparison studies which have tested cardiac hemodynamic measurements using inert gas breathing in comparison to invasive (i.e. direct Fick and thermodilution) or non-invasive (i.e. ECHO or oxygen pulse [O2pulse]) techniques are promising and suggest that inert gas breathing is an adequate technique for the assessment of cardiac hemodynamics in patient populations (2, 15, 17). Our group recently demonstrated that the acetylene rebreathing technique can provide similar estimates of SV when compared with ECHO or standard gas-exchange (i.e. O2pulse) techniques at rest or at peak exercise in healthy individuals and in HFpEF (unpublished data from our lab). Others have also demonstrated that inert gas breathing or standard gas-exchange closely agrees with direct Fick at rest and during exercise in healthy individuals and in HFrEF (2, 15, 33).
IS CLINICAL CLASSIFICATION OF HEART FAILURE AT REST OUTDATED?
Despite the numerous techniques available for estimating cardiac hemodynamics, each with limitations, we sought to illustrate in this review that indices descriptive of cardiac function during exercise are optimal for the clinical classification of HF; whereas, traditional measures of cardiac function at rest may be better served for identifying the potential presence of cardiac abnormalities in HF. For example, previous observations suggest that both invasive (radionuclide, cardiac index) and non-invasive (ECHO, EF%) estimates of resting left ventricular (LV) function do not directly relate with the degree of exercise intolerance (i.e. VO2peak) in HFrEF (14). Others have demonstrated that resting Q and SV measured using non-invasive CO2 rebreathe also do not correlate with exercise tolerance in HFrEF (12). In contrast, it has been observed that despite weak relationships between resting measures of cardiac function and exercise tolerance in HFrEF, exercise measures of cardiac index correlate closely with VO2max and exercise duration in these patients (32). More importantly, it was also demonstrated that HF patients with a higher VO2max (>10.0 mL/kg/min) had a lower mortality rate (14 vs. 77%) at one-year follow-up versus HF patients with a low VO2max (<10.0 mL/kg/min), suggesting that evaluation of cardiac function during exercise is superior at predicting mortality outcomes when compared to evaluation at rest (32). In further support of exercise testing as a method for the clinical evaluation of HF, results of six-minute walk testing have been shown to directly correlate with VO2peak as well as predict short-term prognosis (i.e. <one-year) in these patients (6). Thus, although invasive or non-invasive techniques can be used reliably to identify the presence of impaired cardiac function at rest in HF, it remains unclear whether functional and prognostic implications of cardiac dysfunction associated with HF can be adequately described by measurement of cardiac function at rest in these patients.
WHAT IS THE VALUE OF PEAK OXYGEN UPTAKE VERSUS PEAK CARDIAC FUNCTION?
The contribution of exercise tolerance testing using VO2 or its estimate, six-minute walk test, for estimating functional capacity or prognosis cannot be ignored in HF. Heart failure patients with a low VO2peak (e.g. <10 – 14 mL/kg/min) are suggested to be at higher risk for mortality compared to patients with a higher VO2peak (e.g. >10 – 14 mL/kg/min) (11, 32). Also a consideration, assessment of VO2peak or six-minute walk test requires the use of no advanced technology and are readily available tests in most clinical and research settings. In contrast, reliable and accurate measurement of cardiac hemodynamics via catheterization laboratories or imaging modalities can be variable and highly dependent on factors related to equipment or physician availability, technician experience, or cost of technology.
Despite the encouraging observations from studies of VO2peak in HF in addition to potential limitations influential in preventing cardiac hemodynamic assessment during exercise, several noteworthy observations suggest that symptoms, signs, and prognosis in HF directly relate with cardiac pump dysfunction and, hence, exercise cardiac hemodynamic evaluation may be essential for the clinical classification of these patients (7, 18, 32, 37). Support for cardiac hemodynamic measures such as CP suggests that assessment of this index during exercise predicts survival to the greatest extent compared to traditional measures of cardiovascular function in HFrEF (18, 37). Further, consistent amongst studies of CP are observations which demonstrate higher survival amongst HF patients is associated with individuals who have the highest levels of peak CP at baseline (18, 37). Also, although VO2peak may relate with survival in HF, it is suggested that VO2peak contributes no additional value for assessing survival risk independent of measures directly related to cardiac pumping capacity measured during exercise in HF patients (18, 37). We argue, therefore, that although a valuable component in describing Weber-Janicki functional class in HF, VO2 provides information that may not be consistently relied upon to be unique and directly specific in estimating cardiac pumping capacity; perhaps, because VO2 is a metric that is highly influenced by non-cardiac factors (e.g. motivation, muscle deconditioning, peripheral oxygen extraction, and/or abnormal pressor reflexes) in this population (18, 29, 36, 37). We and others before us recommend that independent measures of VO2 should not be used as direct surrogates for the blood flow and pressure generating capability of the heart during exercise in HF (18, 37).
THE CARDIAC PUMPING CAPACITY MODEL IN HEART FAILURE
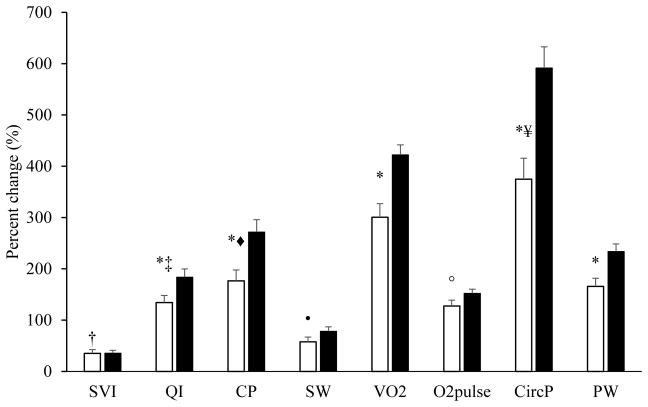
Consistent with observations which describe the clinical value of assessing cardiac hemodynamics during exercise, particularly cardiac pumping capacity in HFrEF (7, 18, 37), we have recently observed in HFpEF no contradictory evidence which is presented in Tables 1 and 2 as well as in Figure 2 (unpublished data from our lab). Heart failure patients with preserved EF% (n = 18; EF% = 62.2 ± 1.3%) although demonstrating similarities in peak stroke volume index (SVI) in comparison to healthy individuals (n = 26; age, height, weight, and body surface area not significantly different between groups; body mass index significantly higher in HFpEF), clearly demonstrated a deficit in cardiac pumping capacity, which is evident when comparing both direct and indirect peak and reserve (absolute or relative change rest to peak exercise) indices between groups. As such, in an attempt to better understand the value of cardiac pumping capacity in HFpEF, we aimed to study relationships between cardiac pumping capacity and exercise tolerance in this population. We also sought to understand whether VO2peak alone or in parallel with other factors (i.e. blood pressure) can be used as a surrogate estimate for cardiac pumping capacity during exercise in HFpEF.
Table 1.
Exercise duration, intensity, symptoms, VO2, and cardiac hemodynamics
| Baseline | Peak exercise | |
|---|---|---|
| Exercise intensity and symptoms | ||
| Exercise duration, seconds | ||
| CTL | - | 845 ± 48 |
| HFpEF | - | 470 ± 49* |
| Work performed, watts | ||
| CTL | - | 94 ± 5 |
| HFpEF | - | 52 ± 5* |
| RPE, Borg 6–20 | ||
| CTL | 6.0 ± 0.0 | 16.1 ± 0.4† |
| HFpEF | 6.0 ± 0.0 | 15.9 ± 0.4† |
| Ventilation | ||
| VO2, ml · kg−1 · min−1 | ||
| CTL | 3.6 ± 0.1 | 18.6 ± 0.6† |
| HFpEF | 3.3 ± 0.2 | 12.7 ± 0.8*† |
| Direct cardiac hemodynamics | ||
| SVI, mL · m−2 | ||
| CTL | 47 ± 2 | 63 ± 3† |
| HFpEF | 46 ± 3 | 61 ± 4† |
| QI, L · min−1 · m−2 | ||
| CTL | 3.3 ± 0.1 | 8.9 ± 0.4† |
| HFpEF | 3.1 ± 0.2 | 7.0 ± 0.4*† |
| CP, L · min−1 · m−2 mm Hg | ||
| CTL | 311 ± 16 | 1088 ± 53† |
| HFpEF | 270 ± 15 | 731 ± 56*† |
| SW, L · m−2 mm Hg | ||
| CTL | 4.4 ± 0.2 | 7.6 ± 0.4† |
| HFpEF | 4.1 ± 0.3 | 6.2 ± 0.4*† |
| Surrogate cardiac hemodynamics | ||
| O2pulse index, mL · beat−1 · m−2 | ||
| CTL | 2.2 ± 0.1 | 5.4 ± 0.2† |
| HFpEF | 2.2 ± 0.1 | 4.8 ± 0.2*† |
| CircP, ml · kg−1 · min−1 mm Hg | ||
| CTL | 347 ± 13 | 2274 ± 114† |
| HFpEF | 290 ± 16* | 1326 ± 110*† |
| PW, mL · beat−1 · m−2 mm Hg | ||
| CTL | 203 ± 7 | 662 ± 30† |
| HFpEF | 191 ± 10 | 495 ± 29*† |
Data presented as means ± SEM. CTL = healthy controls; HFpEF = heart failure with preserved ejection fraction; RPE = rate of perceived exertion; VO2 = oxygen uptake; SVI = stroke volume index; QI = cardiac index; CP = cardiac power; SW = stroke work. O2pulse index = oxygen pulse indexed to BSA; CircP = circulatory power; PW = O2pulse work.
HFpEF vs. CTL, p < 0.05.
Baseline vs. peak exercise, p < 0.05.
Table 2.
Ventilation and cardiac reserve
| Reserve (Δ) | P-value | |
|---|---|---|
| Ventilation | ||
| VO2, mL · kg−1 · min−1 | 0.000 | |
| CTL | 15.0 ± 0.6 | |
| HFpEF | 9.4 ± 0.7 | |
| Cardiac hemodynamics | ||
| SVI, mL · m−2 | 0.739 | |
| CTL | 15.4 ± 2.4 | |
| HFpEF | 14.1 ± 3.3 | |
| QI, L · min−1 · m−2 | 0.003 | |
| CTL | 5.7 ± 0.4 | |
| HFpEF | 4.0 ± 0.4 | |
| CP, L · min−1 · m−2 mm Hg | 0.024 | |
| CTL | 702 ± 78 | |
| HFpEF | 461 ± 53 | |
| SW, L · m−2 mm Hg | 0.424 | |
| CTL | 2.8 ± 0.6 | |
| HFpEF | 2.2 ± 0.4 | |
| Surrogate cardiac hemodynamics | ||
| O2pulse index, mL · beat−1 · m−2 | 0.194 | |
| CTL | 3.2 ± 0.2 | |
| HFpEF | 2.6 ± 0.2 | |
| CircP, ml · kg−1 · min−1 mm Hg | 0.002 | |
| CTL | 1759 ± 165 | |
| HFpEF | 1036 ± 107 | |
| PW, mL · beat−1 · m−2 mm Hg | 0.081 | |
| CTL | 414 ± 48 | |
| HFpEF | 304 ± 28 | |
Data presented as means ± SEM. Reserve calculated as absolute difference, peak exercise - rest. CTL = healthy controls; HFpEF = heart failure with preserved ejection fraction; VO2 = oxygen uptake; SVI = stroke volume index; QI = cardiac index; CP = cardiac power; SW = stroke work. O2pulse index = oxygen pulse indexed to BSA; CircP = circulatory power; PW = O2pulse work.
Figure 2.
Data presented as means ± SEM. Functional reserve expressed as a percentage (%) change in SVI (stroke volume index), QI (cardiac index), CP (cardiac power), SW (stroke work), or VO2 (oxygen uptake) compared with rest. Filled bars represent healthy controls. *Between groups, HFpEF versus healthy controls (p<0.05). †Different versus QI, CP, VO2, O2pulse, CircP, PW for HFpEF, p < 0.05. ‡Different versus SVI, SW, VO2, CircP for HFpEF, p < 0.05. ◆Different versus SVI, SW, VO2, O2pulse, CircP for HFpEF, p < 0.05. ●Different versus QI, CP, VO2, O2pulse, CircP, PW for HFpEF, p < 0.05. ○Different versus SVI, CP, SW, VO2, CircP for HFpEF, p < 0.05. ¥Different versus SVI, QI, CP, SW, O2pulse, PW for HFpEF, p < 0.05. For healthy controls, all indices differed from one another, p < 0.05.
Exercise Tolerance in Heart Failure
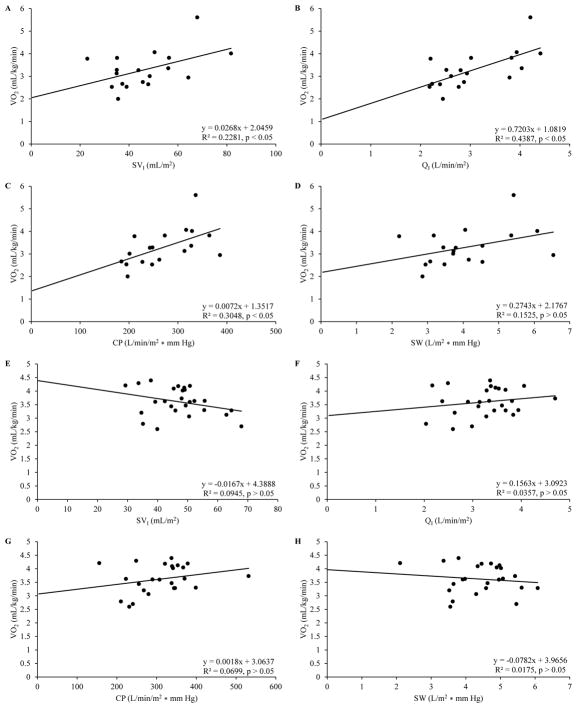
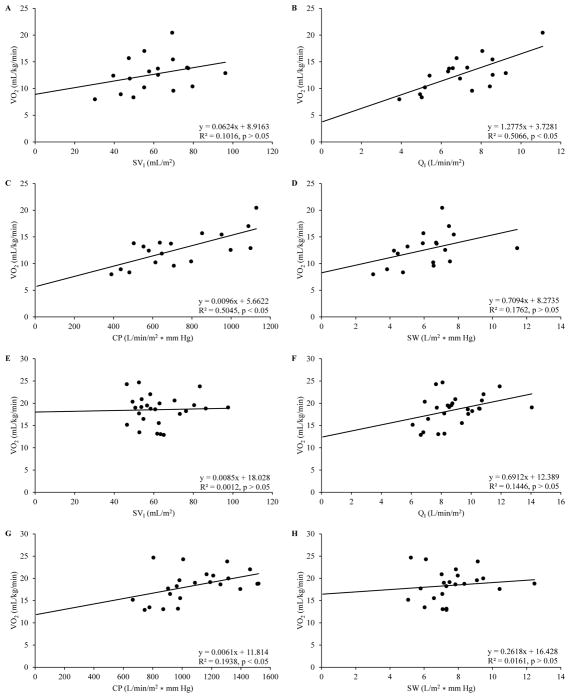
Our group has previously demonstrated that healthy non-highly trained individuals share curvilinear relationships between VO2 and Q during exercise which was observed to be largely attributable to concurrent non-linear adjustments in heart rate versus VO2 or SV relationships during exercise (3). In contrast, observations from a study including a sample of moderate severity HFrEF suggest that VO2peak weakly relates to both peak Q and cardiac index in these patients (6). Although, others have also observed in HFrEF that exercise measures of cardiac index correlate closely with both VO2 and exercise duration (32). As such, it was not unexpected that linear regressions presented in Figures 3 and 4 between VO2 and SVI, QI, CP, or SW at rest and at peak exercise were variable amongst HFpEF and healthy individuals. Although, in support of the present hypothesis and in contrast to healthy individuals, we demonstrate in Table 3 and Figures 3 and 4 that peak exercise measures of cardiac hemodynamics consistently related with exercise tolerance (i.e. VO2peak, exercise duration, and exercise peak power output) to a greater extent compared to resting measures.
Figure 3.
Data presented as ordinary least squares regression via univariate modeling with coefficient of determination (R2) at rest for heart failure patients with preserved ejection fraction (HFpEF) or healthy controls. Dependent variable in all plots was oxygen uptake (VO2). A–D plots are HFpEF. A) stroke volume index (SVI); B) cardiac index (QI); C) cardiac power (CP); D) stroke work (SW). E–H plots are healthy controls. E) SVI; F) QI; G) CP; H) SW.
Figure 4.
Data presented as ordinary least squares regression via univariate modeling with coefficient of determination (R2) at peak exercise for heart failure patients with preserved ejection fraction (HFpEF) or healthy controls. Dependent variable in all plots was oxygen uptake (VO2). A–D plots are HFpEF. A) stroke volume index (SVI); B) cardiac index (QI); C) cardiac power (CP); D) stroke work (SW). E–H plots are healthy controls. E) SVI; F) QI; G) CP; H) SW.
Table 3.
Predictors of exercise tolerance
| Exercise tolerance
|
||
|---|---|---|
| CTL | HFpEF | |
|
|
||
| Cardiac hemodynamics | ||
| SVI, mL · m−2 | 0.10 | 0.10 |
| QI, L · min−1 · m−2 | 0.26* | 0.37* |
| CP, L · min−1 · m−2 mm Hg | 0.26* | 0.28* |
| SW, L · m−2 mm Hg | 0.13 | 0.12 |
| O2pulse index, mL · beat−1 · m−2 | 0.46* | 0.28* |
| CircP, ml · kg−1 · min−1 mm Hg | 0.39* | 0.33* |
| PW, mL · beat−1 · m−2 mm Hg | 0.45* | 0.22* |
| Cardiac hemodynamic reserve | Delta (Δ) | |
| SVI, mL · m−2 | 0.01 | 0.02 |
| QI, L · min−1 · m−2 | 0.23* | 0.38* |
| CP, L · min−1 · m−2 mm Hg | 0.17* | 0.29* |
| SW, L · m−2 mm Hg | 0.10 | 0.00 |
| O2pulse index, mL · beat−1 · m−2 | 0.41* | 0.18 |
| CircP, ml · kg−1 · min−1 mm Hg | 0.22* | 0.37* |
| PW, mL · beat−1 · m−2 mm Hg | 0.21* | 0.19* |
| Cardiac hemodynamic reserve | Percent (%) | |
| SVI, mL · m−2 | 0.00 | 0.02 |
| QI, L · min−1 · m−2 | 0.12 | 0.22* |
| CP, L · min−1 · m−2 mm Hg | 0.27* | 0.24* |
| SW, L · m−2 mm Hg | 0.09 | 0.00 |
| O2pulse index, mL · beat−1 · m−2 | 0.13 | 0.03 |
| CircP, ml · kg−1 · min−1 mm Hg | 0.62* | 0.39* |
| PW, mL · beat−1 · m−2 mm Hg | 0.35* | 0.07 |
| Ventilation | ||
| VO2peak, ml · kg−1 · min−1 | 0.48* | 0.54* |
| VO2reserve, ml · kg−1 · min−1 (Δ) | 0.56* | 0.60* |
| VO2reserve, ml · kg−1 · min−1 (%) | 0.60* | 0.45* |
Data are presented as the coefficient of determination (R2) estimated from univariate linear regression. Exercise tolerance is represented as total exercise duration (commensurate with workload at peak exercise). CTL = healthy controls; HFpEF = heart failure with preserved ejection fraction patients. Cardiac pumping capacity indices were estimated at peak exercise. Cardiac pumping reserve was calculated as absolute change (Δ) or percentage change (%) in cardiac pumping capacity at peak exercise compared to rest. SVI = stroke volume index; QI = cardiac index; CP = cardiac power; SW = stroke work; O2pulse index = oxygen pulse indexed to BSA; CircP = circulatory power; PW = O2pulse work; VO2peak = peak exercise oxygen uptake; VO2reserve was calculated as Δ or % in VO2 at peak exercise compared to rest;
p < 0.05.
Our observations presented in Table 3 may suggest that VO2 and VO2 reserve were the strongest predictors of exercise tolerance in comparison to cardiac hemodynamics in HFpEF and in healthy individuals. Although, it may be necessary to reexamine the interpretation of these observations when considering the model of blood flow and pressure generation described by CP and CircP (7, 18, 37). Therefore, after accounting for arterial pressure generated with VO2 (i.e. CircP), VO2 does not predict exercise tolerance to a greater extent compared to cardiac function indices such as CP in HFpEF. Moreover, upon examining differences in coefficient of determinations between HFpEF and healthy individuals in Table 3, it is apparent that healthy individuals rely more on the capacity for VO2 in determining exercise tolerance in comparison to HFpEF. Whereas, consistent with dysfunctional cardiac pumping capacity in HF, exercise tolerance in HFpEF appears to depend on the rise in cardiac pumping capacity to a greater extent compared to healthy individuals.
Cardiac Hemodynamic Reserve and Exercise Intolerance in Heart Failure
Differences in cardiac hemodynamic reserve between HFpEF and healthy individuals could have been attributable to mechanisms uncovered in recent studies by our group in HFrEF and HFpEF (1, 26). For example, observations from Olson et al. suggest that in an attempt to accommodate excessive metabolic demands of inefficient ventilation during exercise in HFrEF, when paralleled with limited cardiac reserve, muscles of the respiratory system detrimentally attain necessary blood flow intended for metabolically active skeletal muscle (26). This deprives metabolically active skeletal muscle of oxygen and nutrients essential for meeting the demands of exercise (26). Moreover, the findings from Abudiab et al. indicate that low exercise tolerance in HFpEF may be primarily related to impairment in the ability to increase cardiac hemodynamics (i.e. low cardiac reserve) and secondarily to attenuations in VO2, which are observations consistent with the present hypothesis as well as the abnormal blood flow distribution model described by Olson et al. in HFrEF (1, 26). Hence, it could be suggested that the detrimental effects of attenuated cardiac reserve in HF is further exacerbated by metabolic activity of respiratory muscles which require augmented perfusion during exercise and therefore contributory to excessive and inefficient metabolic activity of the heart. This influence of respiratory muscles on blood flow distribution during exercise could lead to a critical reduction in skeletal muscle perfusion. Thus, a decreased power generating capability of skeletal muscle may contribute to premature fatigue and low exercise tolerance in HF patients.
However, it is also evident that by simply increasing cardiac hemodynamic reserve this does not independently improve exercise tolerance in HF. For example, when HF patients receive inotropic therapy (e.g. dobutamine or cardiac resynchronization therapy), observations suggest that there is neither a consistent beneficial response to therapy nor a uniform improvement in exercise tolerance amongst these individuals (10, 21). Although, in the case of responders and non-responders, exercise tolerance still appears to be related to the relative magnitude of cardiac impairment estimated during exercise which is consistent with observations from studies that did not include interventions to increase inotropy (7, 10, 18, 37).
Therefore, considered together, previous observations and the present discussion provide compelling and thought provoking reasons why exercise exposes associations between exercise intolerance and impaired cardiac pumping capacity in HFpEF. Heart failure patients with preserved EF% demonstrated significantly lower peak cardiac hemodynamics (i.e. QI, CP, SW, O2pulse index, CircP, and PW) in comparison to healthy individuals (Table 1). Heart failure patients with preserved EF% also demonstrated significantly lower cardiac reserve (i.e. cardiac index, CP, and CircP) compared to healthy individuals (Table 2). Thus, low peak and reserve cardiac function appear to translate into lower exercise tolerance in HFpEF compared to healthy individuals.
Non-cardiac Factors Exacerbate the Effects of Low Cardiac Pumping Capacity in Heart Failure
There is ample data to support the description of mechanisms which may explain reasons for symptoms that are common in HF. For example, a promising theory is the “muscle hypothesis” posed by Piepoli et al. which suggests that exercise intolerance and abnormal cardiovascular function in HF are related to the influence of peripheral neural factors on the exacerbation of tonic sympathoexcitation in these patients (29). In support of this theory, we recently demonstrated that contraction and or metabolically activated neural feedback from skeletal muscle nerve fibers contributes to ventilatory inefficiency and augmentation of peripheral arterial pressure during exercise in HFrEF (27); which, perhaps could be mechanistically related to the imbalanced blood flow distribution model posed by Olson et al. during exercise in HFrEF (26). In contrast, we have also demonstrated that neither metabolite- nor mechanical-sensitive neural feedback from skeletal muscle afferents directly influences cardiac hemodynamics during exercise in HFrEF (35). Thus, it could be expected that in the absence of increased inotropy during exercise which would normally contribute to the maintenance of arterial pressure, a critical response of the cardiovascular system may be to increase peripheral vascular resistance to mobilize blood flow in an attempt to maintain arterial pressure and to accommodate coronary, respiratory, and skeletal muscle circulation. With a limited capacity to increase myocardial contractile reserve, perhaps related to an impaired Frank—Starling mechanism that could be associated with ischemic/necrotic cardiac tissue and non-responsive cardiac β-adrenergic receptors, HF patients may be relatively ‘preload’ insensitive and instead rely heavily on decreased afterload for adjustments in cardiac hemodynamics. Hence, blunted myocardial contractile reserve when mirrored with increases in the metabolic demands of cardiac, respiratory, and skeletal muscle during exercise, results in poor organ perfusion, metabolic inefficiency, and an overall systemic energy deficit. These deficits are accompanied by abnormalities which may be described by skeletal muscle ischemia, truncated oxygen and nutrient delivery, and attenuation in skeletal muscle power generating capability, all of which likely contribute to exercise intolerance in HF.
SUMMARY AND FUTURE DIRECTIONS
Estimation of cardiac hemodynamics at rest, while effective for potentially identifying or confirming the presence of abnormal cardiac function in HF, do not appear to be strong indicators of functional capacity (i.e. exercise tolerance) or prognosis. Therefore, resting cardiac function should not be used independently for the clinical classification of HF. Alternatively, assessment of VO2 during exercise testing has the potential to estimate both functional capacity as well as prognosis in HF. However, recent findings suggest that although useful as an adjunct clinical and research tool, VO2 alone does not demonstrate clinical value similar to that of cardiac hemodynamics and also should not be considered a direct surrogate for estimating cardiac pumping capacity in HF. Therefore, traditional measurements of cardiac hemodynamics, which include Q, QI, SV, or SVI during exercise testing should be considered strong indicators of functional capacity and prognosis in HF. Moreover, when available, the assessment of cardiac hemodynamics should be described using the cardiac pumping capacity model which accounts for not only the hemodynamic generating capabilities of the heart, but equally important, the pressure generating potential as well. Measurement of CP and to a lesser extent CircP during exercise should be considered robust metrics for describing relationships between cardiac function, functional capacity, and the clinical classification of HF.
In conclusion, although we suggest our response to the question “What surrogate index or indices of cardiac and or pulmonary function best estimates syndrome severity and prognosis in HF?” is well supported while also addressing several of the notable inconsistencies in the literature to date on this topic, we acknowledge that there are still numerous gaps in the understanding of the clinical and bench knowledge of HF. The controversy and challenges to the present remarks may stem from the lack of systematic consensus amongst scientists as to the mechanistic pathways posed to explain many of the yet undefined and complex relationships between the physiology, biology, and biochemistry intrinsic to the pathophysiology of HF. Although, observations to date suggest that assessment of cardiac pumping capacity during exercise provides valuable insight concerning the magnitude of cardiac impairment in addition to closely relating with signs, symptoms, and prognosis which are critical for the clinical classification of HF patients.
SUMMARY.
Cardiac power and cardiac output estimated during exercise closely relate with exercise tolerance, making them valuable for clinical classification of heart failure patients.
Acknowledgments
None
Footnotes
Conflicts of interest: None
Disclosure of funding: HL-108962-05
References
- 1.Abudiab MM, Redfield MM, Melenovsky V, et al. Cardiac output response to exercise in relation to metabolic demand in heart failure with preserved ejection fraction. Eur J Heart Fail. 2013;15(7):776–85. doi: 10.1093/eurjhf/hft026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agostoni P, Cattadori G, Apostolo A, et al. Noninvasive measurement of cardiac output during exercise by inert gas rebreathing technique: a new tool for heart failure evaluation. J Am Coll Cardiol. 2005;46(9):1779–81. doi: 10.1016/j.jacc.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 3.Beck KC, Randolph LN, Bailey KR, Wood CM, Snyder EM, Johnson BD. Relationship between cardiac output and oxygen consumption during upright cycle exercise in healthy humans. Journal of Applied Physiology. 2006;101(5):1474–80. doi: 10.1152/japplphysiol.00224.2006. [DOI] [PubMed] [Google Scholar]
- 4.Bhatia RS, Tu JV, Lee DS, et al. Outcome of heart failure with preserved ejection fraction in a population-based study. The New England journal of medicine. 2006;355(3):260–9. doi: 10.1056/NEJMoa051530. [DOI] [PubMed] [Google Scholar]
- 5.Borlaug BA, Olson TP, Lam CS, et al. Global cardiovascular reserve dysfunction in heart failure with preserved ejection fraction. J Am Coll Cardiol. 2010;56(11):845–54. doi: 10.1016/j.jacc.2010.03.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cahalin LP, Mathier MA, Semigran MJ, Dec GW, DiSalvo TG. The six-minute walk test predicts peak oxygen uptake and survival in patients with advanced heart failure. Chest. 1996;110(2):325–32. doi: 10.1378/chest.110.2.325. [DOI] [PubMed] [Google Scholar]
- 7.Cohen-Solal A, Tabet JY, Logeart D, Bourgoin P, Tokmakova M, Dahan M. A non-invasively determined surrogate of cardiac power (‘circulatory power’) at peak exercise is a powerful prognostic factor in chronic heart failure. Eur Heart J. 2002;23(10):806–14. doi: 10.1053/euhj.2001.2966. [DOI] [PubMed] [Google Scholar]
- 8.Cohn JN, Johnson GR, Shabetai R, et al. Ejection fraction, peak exercise oxygen consumption, cardiothoracic ratio, ventricular arrhythmias, and plasma norepinephrine as determinants of prognosis in heart failure. The V-HeFT VA Cooperative Studies Group. Circulation. 1993;87(6 Suppl):VI5–16. [PubMed] [Google Scholar]
- 9.Corra U, Mezzani A, Bosimini E, Scapellato F, Imparato A, Giannuzzi P. Ventilatory response to exercise improves risk stratification in patients with chronic heart failure and intermediate functional capacity. Am Heart J. 2002;143(3):418–26. doi: 10.1067/mhj.2002.120772. [DOI] [PubMed] [Google Scholar]
- 10.Diaz-Infante E, Mont L, Leal J, et al. Predictors of lack of response to resynchronization therapy. Am J Cardiol. 2005;95(12):1436–40. doi: 10.1016/j.amjcard.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 11.Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM) Eur J Heart Fail. 2008;10(10):933–89. doi: 10.1016/j.ejheart.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 12.Franciosa JA, Park M, Barry Levine T. Lack of correlation between exercise capacity and indexes of resting left ventricular performance in heart failure. The American journal of cardiology. 1981;47(1):33–9. doi: 10.1016/0002-9149(81)90286-1. [DOI] [PubMed] [Google Scholar]
- 13.Francis DP, Shamim W, Davies LC, et al. Cardiopulmonary exercise testing for prognosis in chronic heart failure: continuous and independent prognostic value from VE/VCO2slope and peak VO2. Eur Heart J. 2000;21(2):154–61. doi: 10.1053/euhj.1999.1863. [DOI] [PubMed] [Google Scholar]
- 14.Francis GS, Goldsmith SR, Cohn JN. Relationship of exercise capacity to resting left ventricular performance and basal plasma norepinephrine levels in patients with congestive heart failure. Am Heart J. 1982;104(4 Pt 1):725–31. doi: 10.1016/0002-8703(82)90003-5. [DOI] [PubMed] [Google Scholar]
- 15.Hoeper MM, Maier R, Tongers J, et al. Determination of cardiac output by the Fick method, thermodilution, and acetylene rebreathing in pulmonary hypertension. Am J Respir Crit Care Med. 1999;160(2):535–41. doi: 10.1164/ajrccm.160.2.9811062. [DOI] [PubMed] [Google Scholar]
- 16.Holland DJ, Prasad SB, Marwick TH. Contribution of exercise echocardiography to the diagnosis of heart failure with preserved ejection fraction (HFpEF) Heart. 2010;96(13):1024–8. doi: 10.1136/hrt.2009.183947. [DOI] [PubMed] [Google Scholar]
- 17.Johnson BD, Beck KC, Proctor DN, Miller J, Dietz NM, Joyner MJ. Cardiac output during exercise by the open circuit acetylene washin method: comparison with direct Fick. J Appl Physiol (1985) 2000;88(5):1650–8. doi: 10.1152/jappl.2000.88.5.1650. [DOI] [PubMed] [Google Scholar]
- 18.Lang CC, Karlin P, Haythe J, Lim TK, Mancini DM. Peak cardiac power output, measured noninvasively, is a powerful predictor of outcome in chronic heart failure. Circulation. Heart failure. 2009;2(1):33–8. doi: 10.1161/CIRCHEARTFAILURE.108.798611. [DOI] [PubMed] [Google Scholar]
- 19.Loeppky JA, Hoekenga DE, Greene ER, Luft UC. Comparison of noninvasive pulsed Doppler and Fick measurements of stroke volume in cardiac patients. Am Heart J. 1984;107(2):339–46. doi: 10.1016/0002-8703(84)90384-3. [DOI] [PubMed] [Google Scholar]
- 20.Marwick TH, Nemec JJ, Pashkow FJ, Stewart WJ, Salcedo EE. Accuracy and limitations of exercise echocardiography in a routine clinical setting. J Am Coll Cardiol. 1992;19(1):74–81. doi: 10.1016/0735-1097(92)90054-q. [DOI] [PubMed] [Google Scholar]
- 21.Maskin CS, Forman R, Sonnenblick EH, Frishman WH, LeJemtel TH. Failure of dobutamine to increase exercise capacity despite hemodynamic improvement in severe chronic heart failure. Am J Cardiol. 1983;51(1):177–82. doi: 10.1016/s0002-9149(83)80032-0. [DOI] [PubMed] [Google Scholar]
- 22.Metra M, Faggiano P, D’Aloia A, et al. Use of cardiopulmonary exercise testing with hemodynamic monitoring in the prognostic assessment of ambulatory patients with chronic heart failure. J Am Coll Cardiol. 1999;33(4):943–50. doi: 10.1016/s0735-1097(98)00672-x. [DOI] [PubMed] [Google Scholar]
- 23.O’Connell JB, Bristow MR. Economic impact of heart failure in the United States: time for a different approach. The Journal of heart and lung transplantation : the official publication of the International Society for Heart Transplantation. 1994;13(4):S107–12. [PubMed] [Google Scholar]
- 24.Olson, Miller AD, Hulsebus ML, Flood KS, Johnson BD, Borlaug BA. Lung Diffusion and Alveolar-Capillary Recruitment during Exercise in Heart Failure with Preserved Ejection Fraction. Journal of cardiac failure. 2008;14(6):S25. [Google Scholar]
- 25.Olson LJ, Snyder EM, Beck KC, Johnson BD. Reduced rate of alveolar-capillary recruitment and fall of pulmonary diffusing capacity during exercise in patients with heart failure. J Card Fail. 2006;12(4):299–306. doi: 10.1016/j.cardfail.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 26.Olson TP, Joyner MJ, Dietz NM, Eisenach JH, Curry TB, Johnson BD. Effects of respiratory muscle work on blood flow distribution during exercise in heart failure. J Physiol. 2010;588(Pt 13):2487–501. doi: 10.1113/jphysiol.2009.186056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Olson TP, Joyner MJ, Eisenach JH, Curry TB, Johnson BD. Influence of locomotor muscle afferent inhibition on the ventilatory response to exercise in heart failure. Experimental physiology. 2014;99(2):414–26. doi: 10.1113/expphysiol.2013.075937. [DOI] [PubMed] [Google Scholar]
- 28.Paulus WJ, Tschöpe C, Sanderson JE, et al. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. European heart journal. 2007;28(20):2539–50. doi: 10.1093/eurheartj/ehm037. [DOI] [PubMed] [Google Scholar]
- 29.Piepoli MF, Ponikowski P, Clarka AL, Banasiak W, Capucci A, Coats AJ. A neural link to explain the “muscle hypothesis” of exercise intolerance in chronic heart failure. Am Heart J. 1999;137(6):1050–6. doi: 10.1016/s0002-8703(99)70361-3. [DOI] [PubMed] [Google Scholar]
- 30.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart Disease and Stroke Statistics—2012 Update A Report From the American Heart Association. Circulation. 2012;125(1):e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stevenson LW, Perloff JK. The limited reliability of physical signs for estimating hemodynamics in chronic heart failure. JAMA : the journal of the American Medical Association. 1989;261(6):884–8. [PubMed] [Google Scholar]
- 32.Szlachcic J, Massie BM, Kramer BL, Topic N, Tubau J. Correlates and prognostic implication of exercise capacity in chronic congestive heart failure. Am J Cardiol. 1985;55(8):1037–42. doi: 10.1016/0002-9149(85)90742-8. [DOI] [PubMed] [Google Scholar]
- 33.Taylor BJ, Olson TP, Chul Ho K, Maccarter D, Johnson BD. Use of noninvasive gas exchange to track pulmonary vascular responses to exercise in heart failure. Clinical medicine insights. Circulatory, respiratory and pulmonary medicine. 2013;7:53–60. doi: 10.4137/CCRPM.S12178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van den Broek SA, van Veldhuisen DJ, de Graeff PA, Landsman ML, Hillege H, Lie KI. Comparison between New York Heart Association classification and peak oxygen consumption in the assessment of functional status and prognosis in patients with mild to moderate chronic congestive heart failure secondary to either ischemic or idiopathic dilated cardiomyopathy. The American journal of cardiology. 1992;70(3):359–63. doi: 10.1016/0002-9149(92)90619-a. [DOI] [PubMed] [Google Scholar]
- 35.VanIterson EH, Snyder EM, Joyner MJ, Johnson BD, Olson TP. Effect of Locomotor Muscle Afferent Feedback Inhibition on Cardiac Power During Submaximal Exercise in Heart Failure. Circulation. 2014;130(Suppl 2):A16770-A. [Google Scholar]
- 36.Weber KT, Janicki JS. Cardiopulmonary exercise testing for evaluation of chronic cardiac failure. Am J Cardiol. 1985;55(2):22A–31A. doi: 10.1016/0002-9149(85)90792-1. [DOI] [PubMed] [Google Scholar]
- 37.Williams, Jackson M, Cooke GA, et al. How do different indicators of cardiac pump function impact upon the long-term prognosis of patients with chronic heart failure? American heart journal. 2005;150(5):983.e1–e6. doi: 10.1016/j.ahj.2005.08.018. [DOI] [PubMed] [Google Scholar]
- 38.Williams SG, Tzeng BH, Barker D, Tan LB. Comparison and relation of indirect and direct dynamic indexes of cardiac pumping capacity in chronic heart failure. Am J Cardiol. 2005;96(8):1149–50. doi: 10.1016/j.amjcard.2005.06.051. [DOI] [PubMed] [Google Scholar]
- 39.Woods PR, Olson TP, Frantz RP, Johnson BD. Causes of breathing inefficiency during exercise in heart failure. J Card Fail. 2010;16(10):835–42. doi: 10.1016/j.cardfail.2010.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]