Summary
Background
Maternal depression in the postpartum period confers substantial morbidity and mortality, but the definition of postpartum depression remains controversial. We investigated the heterogeneity of symptoms with the aim of identifying clinical subtypes of postpartum depression.
Methods
Data were aggregated from the international perinatal psychiatry consortium Postpartum Depression: Action Towards Causes and Treatment, which represents 19 institutions in seven countries. 17 912 unique subject records with phenotypic data were submitted. We applied latent class analyses in a two-tiered approach to assess the validity of empirically defined subtypes of postpartum depression. Tier one assessed heterogeneity in women with complete data on the Edinburgh postnatal depression scale (EPDS) and tier two in those with postpartum depression case status.
Findings
6556 individuals were assessed in tier one and 4245 in tier two. A final model with three latent classes was optimum for both tiers. The most striking characteristics associated with postpartum depression were severity, timing of onset, comorbid anxiety, and suicidal ideation. Women in class 1 had the least severe symptoms (mean EPDS score 10·5), followed by those in class 2 (mean EPDS score 14·8) and those in class 3 (mean EPDS score 20·1). The most severe symptoms of postpartum depression were significantly associated with poor mood (mean EPDS score 20·1), increased anxiety, onset of symptoms during pregnancy, obstetric complications, and suicidal ideation. In class 2, most women (62%) reported symptom onset within 4 weeks postpartum and had more pregnancy complications than in other two classes (69% vs 67% in class 1 and 29% in class 3).
Interpretation
PPD seems to have several distinct phenotypes. Further assessment of PPD heterogeneity to identify more precise phenotypes will be important for future biological and genetic investigations.
Funding
Sources of funding are listed at the end of the article.
Introduction
Postpartum depression affects 10–15% of women and confers substantial morbidity and mortality to mothers and children,1,2 being associated with increased risk of suicide, decreased maternal sensitivity and attachment to infants, infanticide, and poor child development.3–5 The strongest predictors of postpartum depression are history of depression or anxiety during pregnancy or post partum,6 a personal or family history of mood disorders, including bipolar disorder,7 previous perinatal loss, experiencing stressful life events, and lack of social support.6,8 Moderate predictors include parity, unplanned pregnancy, obstetric factors, and maternal personality characteristics.9,10
Postpartum depression has been understudied and, consequently, there are significant controversies about the disorder, including whether it is a distinct disorder or part of major depressive disorder, whether childbirth acts as a specific trigger for the onset of depression, and whether the diagnostic criteria for postpartum depression should be specific to the postpartum period or extended to include symptom onset during pregnancy? One view is that postpartum depression is partly or wholly distinctive from major depressive disorder, and that its risk is confined to the immediate postpartum period. Women with postpartum depression are suggested to be biologically different from those with major depressive disorder and, therefore, more sensitive to the dramatic fluctuations in gonadal hormones during the perinatal period.11 An alternative perspective is that postpartum depression is essentially an episode of major depressive disorder that manifests in a specific temporal period. The debate about timing of onset has multiple important implications. As a field, perinatal psychiatry is attempting to disentangle the biological, genetic, psychological, and social contributions that determine prognosis and long-term outcomes for postpartum depression, and to identify risk factors and phenotypic characteristics that might distinguish postpartum depression from major depressive disorder occurring at other times of a woman’s life.12
The diagnostic definition of postpartum depression also remains a topic of debate, with varying temporal definitions having been proposed.13 The Diagnostic and Statistical Manual of Mental Disorders (DSM), fifth edition, has expanded the definition to include onset of symptoms during pregnancy and for up to 4 weeks postpartum.14 In contrast, the International Statistical Classification of Diseases, tenth revision, defines postpartum depression as onset within 6 weeks postpartum, and WHO and the Centers for Disease Control and Prevention extend the risk period to 12 months postpartum.15–17 Thus, timing of symptom onset is a crucial line of inquiry.
Clinical screening for depressive symptoms might occur only once in the postpartum period. A positive screen will be diagnosed as postpartum depression but will not delineate when symptoms began and the length of time for which they have been present. This lack of specificity could lead to diagnostic confusion and inadequate or ineffective treatment, as the factors that distinguish treatment response or prognosis, or whether they will differ as a function of when the depressive episode began, are not yet clearly understood. Identification of whether the episode began before and continued into the pregnancy, during pregnancy, or in the postpartum period is, therefore, very important.
Postpartum depression might differ from major depressive disorder outside the perinatal period in terms of clinical presentation and heritability of the trigger,7 but postpartum depression in itself might also be heterogeneous. Characterisation of heterogeneity would have important diagnostic, therapeutic, and prognostic implications.12 A well defined classification of phenomena in postpartum depression based on symptom profiles and timing of onset will inform future research and advance understanding of the causes of this disorder.
We did an empirical investigation of heterogeneity in postpartum depression to identify possible clinical subtypes within a large, well characterised, aggregated dataset. A common method used to assess the validity of phenomenological subtypes is latent class analysis (LCA), which has been widely applied in psychiatry and other medical disciplines.18,19 LCA is a categorical analogue to factor analysis and is particularly appropriate for data on the presence or absence of symptoms.19 The central premise of LCA, which is an inherently iterative process, is that a heterogeneous group can be reduced to several homogeneous subgroups through assessment and minimisation of associations in responses across multiple indicator variables. The technique clusters similar response profiles to create distinct classes.20,21 We applied LCA to explore whether postpartum depression can be categorised into empirically defined subtypes.
Methods
Data sources
All data were aggregated from an international perinatal psychiatry consortium called Postpartum Depression: Action Towards Causes and Treatment (PACT), which was initiated in 2010 with the aim of gathering information about the causes of postpartum depression. 19 international investigators from seven countries who are active members of PACT contributed anonymised clinical data for analysis, including detailed descriptions of the study designs and methods, recruitment, and clinical variables assessed, organised according to the PACT codebook (appendix).
Participants
17 912 unique records were submitted to PACT. These included women with depression in the postpartum period and controls recruited from multiple settings, including psychiatric clinics, obstetric clinics, primary care, and community advertisements. Each site obtained consent from participants and approval from its institutional review board for data sharing. We restricted our analyses to one livebirth of a singleton per women and excluded multiple births. For women who had multiple assessment ratings across the perinatal period, the highest rating scale score was used.
Definition of postpartum depression
After a review of the literature, we restricted our focus to women with a clinical diagnosis of major depression, defined as a non-psychotic episode of major depressive disorder that occurred within 12 weeks postpartum, with no history of schizophrenia, bipolar disorder, or psychotic symptoms. Depressive symptoms were assessed with the Edinburgh Postnatal Depression Scale (EPDS) or the Hamilton Depression Rating Scale 17 item (HAM-D-17),22 dependent on the type of scale used by the individual site submitting data. Both scales have been validated for use in the perinatal period.23 A range of cutoff scores for the EPDS and the HAM-D-17 based on how best to capture the range of depression severity was decided a priori by the PACT phenotype committee.
The EPDS is a 10-item questionnaire aimed at investigating self-reported depressive and anxiety symptoms in the previous week.24 It is the most widely used validated screening tool for depressive symptoms in pregnant and postpartum women.24 The reported split-half reliability of the EPDS is 0·88 and the standardized Cronbach›s α coefficient is 0·87.24 Each item is scored on a four-point Likert scale ranging from 0 to 3. Thus the total scores on this ten-item scale ranged from 0 to 30, with worsening symptom severity being represented by increasing score. A score of 12 or higher indicates major depressive disorder and a score of 10–12 indicates probable cases of minor depression that require additional clinical monitoring.25 We included women with EPDS scores of 10 or higher to capture a range of severity of postpartum depression (minor to severe).12 The HAM-D-17 was developed more than 50 years ago, and is one of the most commonly used depression rating instruments, and is routinely used in clinical trials.22 We included women with HAM-D-17 scores of 8 or more to include non-euthymic women in the sample and capture a range of symptom severity.26 For women who completed symptom assessments at multiple points in the postpartum period, we used data for the most severe episode.
Psychiatric comorbidity was assessed by some sites in a subset of participants, with the structured clinical interview for DSM, fourth edition (SCID),27 or the schedules for clinical assessment in neuropsychiatry (SCAN).28 Where these data were available, we included them.
Statistical analysis
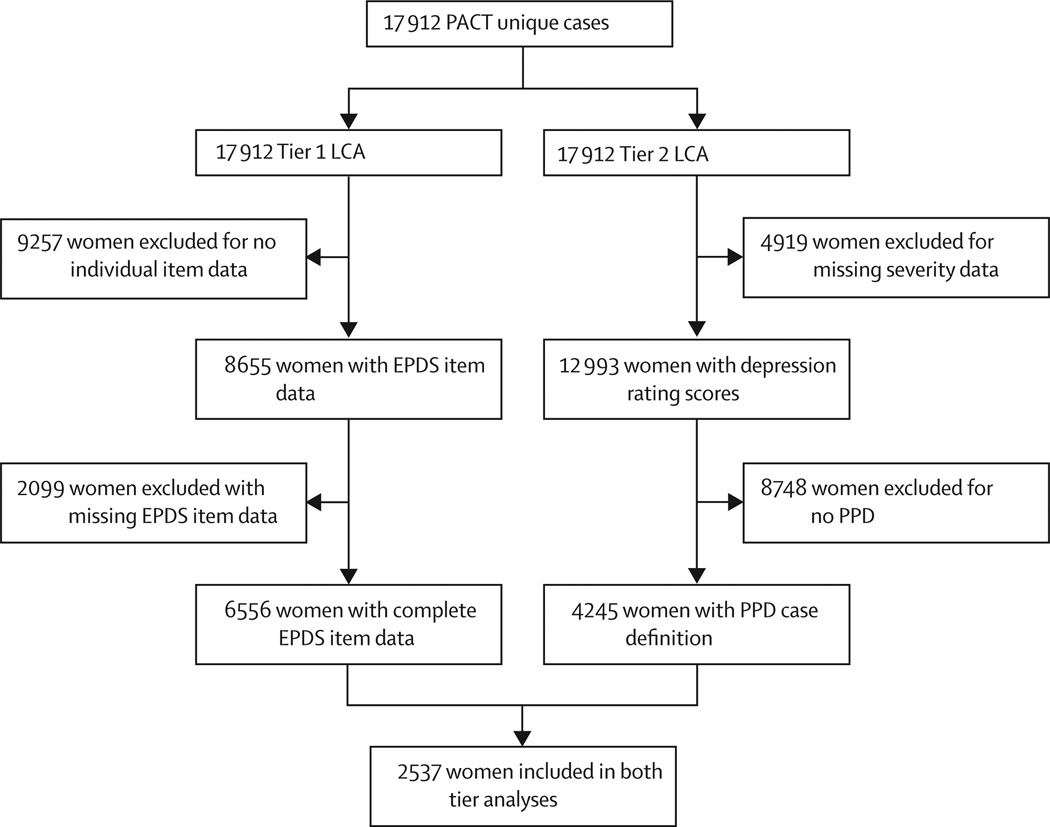
Data were cleaned and aggregated with SAS (version 9.2). Univariate statistics and distributions were assessed for variables. The data were compiled to examine what variables could be used in LCA. In view of the expected wide range of frequencies and types of available data, we employed a two-tiered approach to rigorously examine phenotypic patterns of postpartum depression (figure 1). We decided on this approach because the EPDS is commonly used to measure postpartum depression but how effectively it captures the heterogeneity of this disorder is unknown. Further information on the LCA and definitions of the categorical variables are presented in the appendix.
Figure 1. Two-tiered approach to latent class analysis to identify phenotypic heterogeneity in postpartum depression.
PACT=Postpartum Depression: Action Towards Causes and Treatment Consortium data. LCA=latent class analysis. EPDS=Edinburgh postnatal depression scale. PPD=postpartum depression.
To keep ascertainment bias to a minimum, in the tier one analyses, we assessed heterogeneity of postpartum depression in women with complete EPDS item data. Consequently, women with postpartum depression and controls who had reported depressive symptoms during pregnancy or postpartum might have been included. Tier two included only women with postpartum depression established by structured clinical diagnostic interview (SCID or SCAN), total EPDS score of 10 or higher, HAM-D-17 score of 8 or higher, or psychiatric clinical interview. If women had data from more than one type of assessment, those from EPDS were given preference if available, followed by HAM-D-17, then psychiatric clinical interview. LCA was used to identify distinct classes from the profiles of ordinal, categorical, and continuous indicator variables.20,29 Mixture models were applied for inclusion of all variables. The two tiers of analysis used step-up LCA procedures, starting with the null hypothesis of a single LCA class solution.20 Analyses were done with Mplus statistical software (version 7.2; appendix).
In tier one of the LCA analysis, EPDS data were pooled without any transformations for missing data to reduce the risk of measurement error across sites. We did not impute data because they varied substantially. The ten EPDS questionnaire items (table 1) were used as the indicator variables and subjected to LCA. The entropy value, and the Vuong-Lo-Mendell-Rubin likelihood ratio value, which indicates an improvement in fit from the previous solution in conjunction with the stability and clinical meaningfulness of the latent class solutions across programme iterations, was used to assess the optimum number of classes for the model solution. The EPDS total, EPDS anxiety subscale (items three to five), pregnancy and obstetric complications, and psychiatric history of major depression or anxiety were used in the validation analyses for LCA tier one. The PACT phenotype committee selected the validation variables on the basis of clinical relevance.
Table 1.
Class membership and EPDS symptom Endorsement Probabilities across latent classes, including cases and controls
| Class 1 (n=3484) |
Class 2 (n=2342) |
Class 3 (n=730) |
|
|---|---|---|---|
| EPDS1 Laugh and see the funny side of things | |||
| As much as I could | 0·92 | 0·28 | 0·56 |
| Not quite as much | 0·07 | 0·52 | 0·16 |
| Definitely not so much now | 0 | 0·19 | 0·18 |
| Not at all | 0·01 | 0·01 | 0·11 |
| EPDS2- Look forward with enjoyment | |||
| As much as I ever did | 0·92 | 0·32 | 0·54 |
| Rather less than I used to | 0·08 | 0·49 | 0·15 |
| Definitely less than I used to | 0 | 0·16 | 0·17 |
| Hardly at all | 0 | 0·03 | 0·14 |
| EPDS3- Blamed myself unnecessarily | |||
| No, never | 0·56 | 0·09 | 0·33 |
| Not very often | 0·27 | 0·20 | 0·18 |
| Yes, some of the time | 0·16 | 0·56 | 0·30 |
| Yes, most of the time | 0·01 | 0·14 | 0·19 |
| EPDS4- Anxious or worried for no good reason | |||
| No, not at all | 0·37 | 0·09 | 0·09 |
| Hardly ever | 0·26 | 0·32 | 0·15 |
| Yes, sometimes | 0·18 | 0·43 | 0·29 |
| Yes, very often | 0·20 | 0·16 | 0·47 |
| EPDS5-Scared or panicky for no very good reason | |||
| No, not at all | 0·79 | 0·25 | 0·05 |
| No, not much | 0·16 | 0·35 | 0·11 |
| Yes sometimes | 0·04 | 0·34 | 0·24 |
| Yes quite a lot | 0·01 | 0·06 | 0·61 |
| EPDS6- Things have been getting on top of me | |||
| No, coping as well as ever | 0·52 | 0·07 | 0·03 |
| No, coped quite well most of the time | 0·37 | 0·35 | 0·09 |
| Yes, I haven’t been coping as well as usual | 0·11 | 0·53 | 0·42 |
| Yes, Most of the time I haven’t been able to cope | 0 | 0·05 | 0·47 |
| EPDS7- Been so unhappy had difficulty sleeping | |||
| No, not at all | 0·94 | 0·26 | 0·01 |
| Not very often | 0·06 | 0·38 | 0·03 |
| Yes, sometimes | 0 | 0·32 | 0·20 |
| Yes, Most of the time | 0 | 0·04 | 0·77 |
| EPDS8- Felt sad or miserable | |||
| No, not at all | 0·82 | 0·04 | 0·01 |
| Not very often | 0·17 | 0·46 | 0·01 |
| Yes, quite often | 0·01 | 0·46 | 0·26 |
| Yes, most of the time | 0 | 0·05 | 0·73 |
| EPDS9- been so unhappy that I have been crying | |||
| No, never | 0·86 | 0·12 | 0·01 |
| Only occasionally | 0·14 | 0·53 | 0·02 |
| Yes, quite often | 0 | 0·30 | 0·25 |
| Yes, most of the time | 0 | 0·04 | 0·72 |
| EPDS10- thought of harming myself has occurred to me | |||
| Never | 0·99 | 0·80 | 0·19 |
| Hardly ever | 0·01 | 0·11 | 0·07 |
| Sometimes | 0 | 0·06 | 0·12 |
| Yes, quite often | 0 | 0·04 | 0·63 |
EPDS=Edinburgh postnatal depression scale.
The tier two LCA analyses used additional clinical data on severity and included sites with EPDS total scores of 10 or more that were not included in tier one. We tested the hypothesis that indicator variables would capture distinguishing clinical features of postpartum depression that were common to multiple sites. These indicator variables included severity of depression, EPDS total score, EPDS anxiety subscale score, complications of pregnancy, obstetric complications, suicidal ideation, and psychiatric history of anxiety and depression. We used Mplus method and missing data were not imputed. The model parameters were individually estimated from the available data before using the full information maximum likelihood. The assumption of conditional independence was assessed by examination of bivariate residuals of the indicator variables. The assumption of conditional independence is central to LCA, yet models can be modified to allow for partial conditional independence among indicator variables. Therefore, we adjusted our model for correlation between continuous variables. Examination of entropy, the Vuong-Lo-Mendell-Rubin likelihood ratio, Bayesian information criterion, Akaike’s information criterion, and bivariate residuals, along with the clinical meaningfulness of the classes, were used in selection of the final model solution.
Results
17 912 unique records representing individual cases were identified in 13 prospective, four retrospective, and two mixed (prospective and retrospective) studies. 6556 women were included in the tier one analysis, 4245 in tier two, and 2537 women were analysed in both tiers (figure 1). A three-class solution yielded the best fit for both LCA tiers. The Vuong-Lo-Mendell-Rubin likelihood ratio supported this model solution (value 6189) over solutions with one, two, or four classes. The final model had a strong positive entropy value of 0·925; in LCA, entropy values lower than 0·8 reflect poor class separation, whereas those approaching 1·0 indicate clear delineation of classes.30
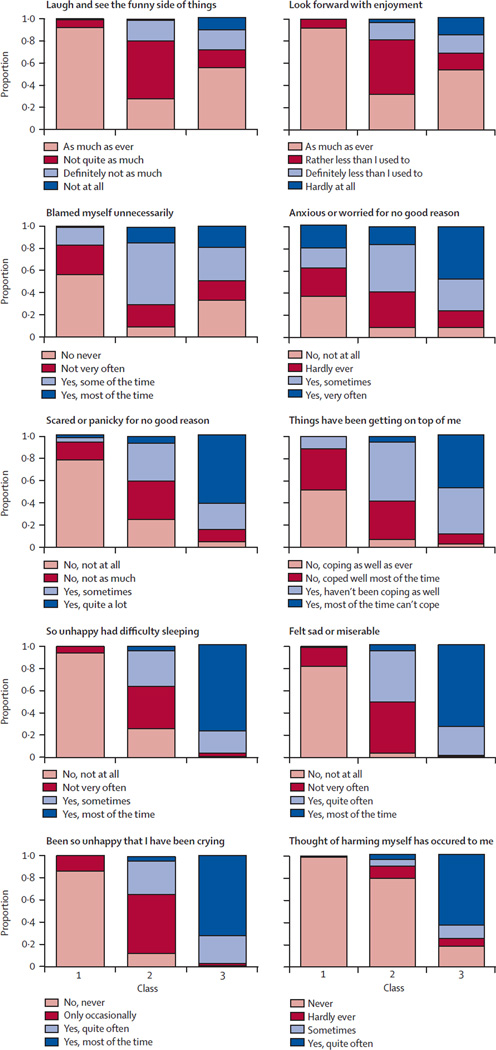
Of the tier one LCA sample, 3484 (53%) women were assigned to class 1, 2342 (36%) to class 2, and 730 (11%) to class 3. Table 1 and figure 2 illustrate the response probabilities of the EPDS item ratings across latent classes. Class 1 members did not rate themselves as depressed or anxious, with 92% reporting that they were able to laugh and see the funny side of things as much as they always could (mean EPDS score 3·3). Individuals assigned to classes 2 and 3 rated themselves as feeling symptomatic in terms of sadness, blaming themselves unnecessarily, and having difficulty sleeping. Members of class 3 had notably more severe symptoms than those in class 2 for feeling panicky, sad, and crying often, and particularly for thoughts of harming oneself often (table 1, figure 2). Women in class 2 were notably differentiated from those in class 3 for blaming themselves unnecessarily (56% vs 30%).
Figure 2. Response probabilities for ten Edinburgh postnatal depression scale questions, by latent class.
The questions “Blamed myself unnecessarily”, “Anxious or worried for no good reason”, and “Scared or panicky for no good reason” included scores from the Edinburgh postnatal depression scale anxiety subscale.
Age varied substantially across the latent classes. Most women across all the classes were married or cohabiting during the postpartum depression rating period, and most were white (table 2). Women assessed in prospective studies were generally younger than those in retrospective studies at time of interview. The prospective and retrospective studies were compared with the EPDS total mean scores and those for the anxiety subscale. Total mean EPDS scores were similar in the two types of study (8·4 vs 8·3, p=0·29), but those for the EPDS anxiety subscale differed (3·3 vs 3·7, p<0·001).
Table 2.
Demographic characteristics of women across latent classes
| Class 1 (n=3484) |
Class 2 (n=2342) |
Class 3 (n=730) |
χ2 and p values | |
|---|---|---|---|---|
| Race (%) | ||||
| White | 79·5 | 72·0 | 78·7 | 33·4; p<0·0001 |
| African American | 14·7 | 21·0 | 14·3 | |
| Other | 5·8 | 7·0 | 6·9 | |
| Education (%) | ||||
| High school or less | 38·5 | 56·5 | 33·9 | 214·9; p<0·0001 |
| College | 37·8 | 28·6 | 39·9 | |
| Professional or graduate | 23·7 | 14·9 | 26·2 | |
| Marital status (%) | ||||
| Married/cohabiting | 88·1 | 74·6 | 76·7 | 181·2; p<0·0001 |
| Single | 11·8 | 25·4 | 23·3 | |
| Low income proxy* (%) | ||||
| No | 90·3 | 80·8 | 60·0 | 63·9; p0<·0001 |
| Yes | 9·7 | 19·2 | 40·0 | |
| Study design | ||||
| Prospective | 73·4 | 68·6 | 89·0 | 117·2; p<0·0001 |
| Retrospective | 26·6 | 31·4 | 11·0 | |
Government or State assistance.
Phenotypic measures of complications during pregnancy (ie, gestational diabetes, pre-eclampsia) and delivery (obstetric), history of mood or anxiety disorders, and timing of onset of symptoms differed between latent classes in the tier one analysis (table 3). Onset of postpartum depression during pregnancy was notably more frequent among women in class 3 than in the other classes. The frequency of obstetric complications was also significantly higher in women in class 3 than in those in classes 2 or 1. In contrast, more women in classes 1 and 2 reported complications of pregnancy than those in class 3. The EPDS mean total and anxiety subscale scores increased in severity from latent class 1 to 3 (clinically non-relevant in class 1, to moderately depressed in class 2, and to severely depressed in class 3).
Table 3.
Phenotypic characteristics across latent classes
| Class 1 (n=3484) | Class 2 (n=2342) | Class 3 (n= 730) | χ2 and p values | |
|---|---|---|---|---|
| EPDS total | 3·27 (2·2) | 12·33 (3·5) | 20·32 (2·4) | .. |
| EPDS anxiety subscale | 2·08 (1·6) | 4·63 (1·6) | 5·88 (1·6) | .. |
| PPD onset* | ||||
| Pregnancy | 218/2016 (11%) | 233/680 (34%) | 222/331 (67%) | |
| Postpartum | 1798/2016 (89%) | 447/680 (66%) | 109/331 (33%) | 532·6; p<0·0001 |
| Obstetric complications† | ||||
| No | 1925/2501 (77%) | 702/952 (74%) | 293/514 (57%) | |
| Yes | 576/2501 (23%) | 250/952 (26%) | 221/514 (43%) | 80·9; p<0·0001 |
| Pregnancy complications‡ | ||||
| No | 853/2240 (38%) | 293/743 (39%) | 333/463 (72%) | |
| Yes | 1387/2240 (62%) | 450/743 (61%) | 130/463 (28%) | 184·7; p<0·0001 |
| Mood disorder history§ | ||||
| No | 89/169 (53%) | 155/359 (43%) | 75/454 (17%) | |
| Yes | 80/169 (47%) | 204/359 (57%) | 379/454 (83%) | 106·5; p<0·0001 |
| Anxiety disorder history¶ | ||||
| No | 139/164 (85%) | 159/292 (54%) | 169/435 (39%) | |
| Yes | 25/164 (15%) | 133/292 (46%) | 266/435 (61%) | 109·3; p<0·0001 |
Data are number (%) or mean (SD). EPDS=Edinburgh postnatal depression scale. DSM-IV=Diagnostic and Statistical Manual of Mental Disorders, fourth edition.
Categories were first trimester, second trimester, third trimester, postpartum 0–4 weeks, postpartum 4–8 weeks, postpartum >8 weeks, and not assessed.
Included endorsement of any of the five items for fetal stress, postpartum haemorrhage, premature rupture of membranes, delivery type, or low birthweight.
Included endorsement of any of the five items for gestational hypertension, maternal obesity, pre-eclampsia, gestation diabetes, and high-risk pregnancy status.
Included endorsement at any time of any of the following DSM-IV lifetime diagnoses: postpartum depression, major depressive disorder, depression disorder not otherwise specified, and dysthymia.
Included endorsement at any time of any one or more of the following DSM-IV lifetime diagnoses: generalised anxiety disorder, panic, agoraphobia, post-traumatic stress disorder, social phobia, specific phobia, anxiety not otherwise specified, and obsessive compulsive.
The restriction of analyses to women with postpartum depression and expanded indicator variables in the tier two analysis captured more data for clinical variables than the tier one analysis. A three-class solution again yielded the best fit, as the iterations stepped up from the single class LCA model, with an entropy statistic of 0·83 and the lowest Bayesian information criterion statistic among iterations. Average latent class probabilities for the most likely latent class membership in the three-class solution were 0·89, 1·0, and 0·92. The Vuong-Lo-Mendell-Rubin likelihood ratio supported the three-class solution (value 1333) over solutions of one, two, or four classes.
The tier two LCA comprised 4245 women who met our case definition of postpartum depression (table 4) and, therefore, the clinical profile differs from that in tier one. Cross-tabulation of sites by class membership revealed that all sites except one contributed to all three class assignments and, therefore, results are not biased by individual sites. Demographic characteristics were similar to those in the tier one analysis (appendix). On the basis of EPDS cutoff scores, class 1 was characterised by fewer cases of severe postpartum depression than classes 2 and 3, in which postpartum depression was classified as major. The timing of onset of depressive symptoms varied between the classes (table 4). Suicidal thoughts were very common in women in class 3 compared with those in classes 1 and 2. All latent classes had high proportions of patients with psychiatric comorbidity (history of depression, anxiety, or mood disorders).
Table 4.
Frequency of phenotypes across latent classes
| Class 1 (n=759) |
Class 2 (n=2099) |
Class 3 (n=1387) |
|
|---|---|---|---|
| EPDS total | 10·5 | 14·8 | 20·1 |
| EPDS anxiety subscale | 4·4 | 5·4 | 5·8 |
| Depression severity | |||
| Minor | 1·00 | 0 | 0 |
| Major | 0 | 1·00 | 1·00 |
| Gravidity | 0·32 | 0·24 | 0·28 |
| Primiparous | |||
| Multiparous | 0·68 | 0·76 | 0·72 |
| PPD onset | |||
| 1st trimester | 0·04 | 0·03 | 0·13 |
| 2nd trimester | 0·17 | 0·11 | 0·27 |
| 3rd trimester | 0·06 | 0·03 | 0·15 |
| 0–4 weeks PPD | 0·54 | 0·62 | 0·17 |
| 5–8 weeks PPD | 0·13 | 0·09 | 0·07 |
| >8 weeks PPD | 0·02 | 0·06 | 0·21 |
| Obstetric complications* | |||
| No | 0·74 | 0·73 | 0·58 |
| Yes | 0·26 | 0·27 | 0·43 |
| Pregnancy complications† | |||
| No | 0·33 | 0·31 | 0·71 |
| Yes | 0·67 | 0·69 | 0·29 |
| History of anxiety or mood disorders‡ | |||
| None | 0·14 | 0·27 | 0·04 |
| Anxiety only | 0·04 | 0·03 | 0·06 |
| Mood only | 0·27 | 0·34 | 0·30 |
| Anxiety and mood | 0·55 | 0·36 | 0·60 |
| Suicidal thoughts | |||
| Never | 0·87 | 0·80 | 0·10 |
| Hardly ever | 0·09 | 0·14 | 0·08 |
| Sometimes | 0·02 | 0·06 | 0·16 |
| Yes, quite often | 0·01 | 0 | 0·67 |
| Mood in pregnancy | |||
| Depressed | 0·15 | 0·14 | 0·47 |
| Well | 0·37 | 0·21 | 0·36 |
| Unknown | 0·48 | 0·64 | 0·18 |
EPDS=Edinburgh postnatal depression scale. PPD=postpartum depression. DSM-IV=Diagnostic and Statistical Manual of Mental Disorders, fourth edition.
Included endorsement of any one of the five items for fetal stress, postpartum haemorrhage, PROM, delivery type, and low birthweight.
Included endorsement of any of the five items for gestational hypertension, maternal obesity, pre-eclampsia, gestation diabetes, and high-risk pregnancy status.
Mood diagnoses included endorsement at any time of any one or more of the following DSM-IV lifetime diagnoses: PPD, major depressive disorder, depression disorder not otherwise specified, and dysthymia; anxiety disorders included endorsement at any time of any one or more of the following DSM-IV lifetime diagnoses: generalised anxiety disorder, panic, agoraphobia, posttraumatic stress disorder, social phobia, specific phobia, anxiety not otherwise specified, and obsessive compulsive disorder.
Discussion
Despite the wealth of research on risk factors for postpartum depression, understanding of heterogeneity and related underlying mechanisms has not substantially progressed. The overarching goal of PACT was to create an international perinatal psychiatry consortium that would allow for novel investigations with large sample sizes. In this collaborative project, we chose to use extant data to examine the heterogeneity of postpartum depression and broadly define subgroups of depression in the postpartum period, taking into account varying times of symptom onset, to enable phenomena in multiple diagnostic domains to be assessed together.
With use of the common data elements, we identified three latent classes of postpartum depression in the tier one analysis of 6556 women. The diversity and number of the cases assessed, which were identified from a broad range of settings and across 19 international sites, provide important evidence of quality control and keep ascertainment bias to a minimum. Our results support heterogeneity in postpartum depression, and have important implications for prognosis, tailoring of treatment to individual women’s needs, and future genetics studies. We identified several features that differentiated groups, including timing of onset of symptoms (during pregnancy vs postpartum), severity of symptoms, perinatal complications, and history of mood disorders, which might be important to future work. Because LCA is an iterative process, we used a two-tiered approach to assess the phenotypic heterogeneity of postpartum depression. In the tier one and tier two LCA analyses, the most striking characteristic was the distinction between classes by severity of symptoms, timing of symptom onset, degree of comorbid anxiety, and suicidal ideation.
The timing of onset of postpartum depression is an area of intense investigation. This feature was the sole change in the diagnostic criteria between the fourth and fifth editions of DSM. Thus, we wished to find out whether it was associated with a particular subgroup of women. In the tier one LCA analysis, we found that around 67% of those in class 3, the most severely depressed group, reported onset of symptoms during pregnancy. This group might, therefore, be more likely to have more chronic or remitting and relapsing presentations of symptoms, obstetric complications, and suicidal ideation in the postpartum period. Class 3 was further differentiated from class 2 by history of mood and anxiety disorders, which suggests that the onset of psychiatric symptoms could have predated pregnancy and might implicate worse prognosis, including the risk of bipolarity.34 Identification of timing of onset of symptoms, therefore, becomes a crucial part of assessment and has important implications for understanding the cause and prognosis of perinatal psychiatric illness. In the tier two LCA analysis, which enabled more detailed examination of the differences between classes, 62% of women in class 2 reported onset of symptoms in the first 4 weeks postpartum, whereas in class 3, in which symptoms were more severe, most women reported onset during pregnancy. We speculate that the timing of symptom onset might be a useful indicator for use in future biological and genetic analyses of postpartum depression.
In the tier one analysis, women assigned to class 2 reported depressive and anxiety symptoms on the individual EPDS items, but these were less severe than those in class 3 and did not include suicidal ideation. Class 3 was also characterized by the presence of severe anxiety symptoms and feeling overwhelmed. These findings are consistent with women in class 3 reporting severe mood symptoms present most of the time and reporting suicidal ideation quite often. Suicidal ideation is the primary cause of psychiatric hospital admissions in the postpartum period31,32 and suicide is the leading cause of maternal death.33 The identification of a distinct class characterised by suicidal thoughts, therefore, is noteworthy. Additionally, whether class 3 constitutes women at higher risk of worse prognosis of bipolarity than class 2 needs to be assessed further, since our data are based only on women with a diagnosis of unipolar depression. For example, Munk-Olsen and colleagues33 reported that 14% of women who sought psychiatric evaluation within 1 month of giving birth developed lifetime bipolar disorder, and that inpatient admissions were associated with increased diagnostic rates of bipolar disorder than outpatient contacts.34 Wisner and colleagues12 also found a high prevalence of bipolar disorder (22%) in structured psychiatric interviews of women with positive EPDS screening scores in the first 4–6 weeks postpartum. Our findings, therefore, suggest that the underlying biological or genetic vulnerabilities in women who manifest this most severe form of postpartum depression, and the degree to which these might represent bipolarity that would require a different approach to treatment, warrant further exploration.
Consistent with the findings in our tier one analysis, where class 3 was the most severely depressed, the tier two analysis showed increased rates of history of anxiety and mood disorders in this class. These findings support those of previous studies in which history of depression has been one of the greatest risk factors for postpartum depression.2,6 Additionally, class 3 was further distinguished by the type of perinatal complication: 43% reported obstetric complications, whereas in classes 1 and 2 complications of pregnancy, such as high-risk pregnancy, gestational diabetes, gestational hypertension, maternal obesity, and pre-eclampsia, were more likely. Obstetric complications, therefore, might serve as a potential trigger for, or contributing factor to, increased anxiety, depression, and suicidal ideology in women who develop postpartum depression. Future studies should investigate whether factors, such as treatment history, treatment efficacy before pregnancy, and the interval between remission of the previous depressive episode and pregnancy are relevant in women with a history of major depressive disorder before pregnancy.
We obtained data from prospective and retrospective studies in this study. The two study types had similar total mean EPDS scores. This finding largely confirms earlier work by Cox and colleagues,35 who reported that women can accurately recall previous episodes of postpartum depression, including duration and severity of symptoms.
This study has several limitations that should be taken into account for interpretation of the results. First, the hypotheses were tested on extant data across 19 sites. Although careful and strict attention was given to the aggregation and creation of the PACT data pool, study protocols had inherent differences, including selection criteria and recruitment settings. Such differences can contribute to ascertainment bias. Additionally, missing data differed by site. Our results should, therefore, be interpreted as providing an important hypothesis-generating foundation for future work. Second, the phenotypic committee rigorously identified clinically relevant variables to test the heterogeneity of postpartum depression, but this list was limited to commonality of data submitted and protocol attributes across sites. Other phenotypic features that we were unable to assess might, therefore, also be important to postpartum depression. For example, most of the data are from white women, which might limit the generalisability of the findings to more ethnically diverse populations. Moreover, we had little data about history of stressful life events, such as abuse or trauma. Lastly, we acknowledge the potential disadvantages of LCA include overestimation of classes because of local dependence, and when class membership numbers are small the LCA might be unable to distinguish low prevalence from zero. Our study also has some notable strengths, including the large sample size, diverse characteristics for sites and countries, inclusion of women from a wide range of socioeconomic statuses, and detailed phenotyping and classification of the symptoms by standardized assessment measures.
Our results indicate that postpartum depression is heterogeneous and that differentiation of subgroups is likely to be crucial when considering the underlying causes, treatment options, and prognosis of perinatal depression (panel). The two-tiered LCA approach yielded consistent subclasses of postpartum depression. The most relevant features differentiating classes were timing of onset of symptoms (during pregnancy vs postpartum), severity of symptoms, perinatal complications, and history of a mood disorder. Our findings expand understanding of postpartum depression, but further clarification of the clinical subgroups will be necessary to facilitate the search for biomarker signatures for postpartum depression and major depressive disorder in general. We will apply our findings from PACT to future biological and genetic studies of depression in women across the perinatal period.
Supplementary Material
Panel: Research in context.
Systematic review
Our data were aggregated from the international perinatal psychiatry consortium Postpartum Depression: Action Towards Causes and Treatment (PACT), whose members represent 19 institutions in seven countries. The study was an empirical investigation of the heterogeneity of postpartum depression to identify possible clinical subtypes within a large well characterised dataset. Because diagnostic criteria notably affect the implementation and interpretation of screening, diagnosis, treatment, and research of perinatal mood disorders, it has become important to ensure the empirical validity of phenomenological subtypes of postpartum depression.
Interpretation
We assessed aggregated extant data from 17 912 unique subject records with phenotypic information. We found that postpartum depression is heterogeneous and identified three distinct classes of symptoms. Our findings have important implications for prognosis and tailoring of treatment to individual women with postpartum depression. The features that differentiated groups were timing of onset of symptoms (during pregnancy vs postpartum), severity of symptoms, perinatal complications, and history of a mood disorder. Clinicians should be aware of the heterogeneity of women with postpartum depression. A thorough assessment of history will be necessary to guide clinical and treatment decisions. Our data suggest that the timing of symptom onset is of particular importance, and that mothers whose symptoms begin during pregnancy might be at risk of more severe postpartum depression than those whose symptoms begin after birth. Medical complications during pregnancy and at birth might also be distinguishing features for severity of postpartum depression.
Acknowledgments
The National Institute of Mental Health support SM-B (K23 MH085165-01A1), TM-O, DRR, PFS, and SM-B (1R01MH104468-01), ERB (K23MH080290), and a young investigator award from the Brain & Behavior Research Foundation), KMS (5K23MH086689, JP (K23 MH074799-01A2), VB (FP7-Health-2007 Project no 222963), MWO (MH50524 NIMH), KLW (5R01MH60335, NIMH, 5R01MH071825 NIMH, 5R01MH075921 NIMH, and 5-2R01MH057102), SJR and HT (ZonMW 10.000.1003, NIMH K23 MH097794, and NIH UL1 TR000161), and PJS (ZIA MH002865-09 BEB). KMD is supported by the Worcester Foundation for Biomedical Research. CNE is supported by Pfizer Pharmaceuticals and a young investigator award from the National Alliance for Research on Schizophrenia and Depression. GA and ED are supported by the French Ministry of Health (PHRC 98/001) and Mustela Foundation. BWP is supported by the Geestkracht program of the Netherlands Organisation for Health Research and Development (10-000-1002) and VU University Medical Centre, GGZ Geest, Arkin, Leiden University Medical Centre, GGZ Rivierduinen, University Medical Centre in Groningen, Lentis, GGZ Fries land, GGZ Drenthe, IQ Healthcare, Netherlands Institute for Health Services Research, and Netherlands Institute of Mental Health and Addiction. CG is supported by South Carolina Clinical and Translational Research Institute (UL1 TR000062) & Building Interdisciplinary Research Careers in Women’s Health (K12 HD055885). ZNS is supported by the National Institutes for Health (P50 MH-77928 and P50 MH 68036). IJ is supported by the National Centre for Mental Health Wales.
The PACT Consortium
Karen Putnam (The University of North Carolina at Chapel Hill, Department of Psychiatry, USA); Emma Robertson-Blackmore (University of Florida at Jacksonville, Department of Psychiatry, USA); Katherine Sharkey (Alpert Medical School of Brown University/Rhode Island Hospital, Department of Psychiatry, USA); Jennifer Payne (The Johns Hopkins University, Department of Psychiatry, USA); Veerle Bergink (Erasmus MC, Department of Psychiatry/Psychology, Rotterdam, The Netherlands); Trine Munk-Olsen (Aarhus University, Department of Economics and Business [NCRR]-National Centre for Integrated Register-based Research, Denmark); Kristina Deligiannidis (University of Massachusetts Medical School, Department of Psychiatry, USA); Margaret Altemus (Weill Cornell Medical College, Department of Psychiatry USA); Jeffrey Newport (University of Miami, Department of Psychiatry, USA); Gisele Apter (Erasme Hospital, Paris Diderot University, France); Emmanuel Devouche (Erasme Hospital, Paris Descartes University, France); Alexander Vikorin, Patrik Magnusson, and Paul Lichtenstein (Karolinska Institute, Department of Medical Epidemiology and Biostatistics, Sweden); Brenda Penninx (VU University Medical Center, Department of Psychiatry, The Netherlands); Anne Buist and Justin Bilszta (University of Melbourne, Women’s Mental Health, Australia); Michael O’Hara, Scott Stuart, and Rebecca Brock (The University of Iowa, Department of Psychology, USA); Sabine Roza and Henning Tiemeier (Erasmus MC, Department of Psychiatry/Psychology, Rotterdam, The Netherlands); Constance Guille (Medical University of South Carolina, Department of Psychiatry, USA); C Neill Epperson and Deborah Kim (University of Pennsylvania, Department of Psychiatry, USA); Peter Schmidt and Pedro Martinez (National Institutes of Mental Health); Katherine L Wisner (Northwestern University Feinberg School of Medicine, Asher Center for the Study and Treatment of Depressive Disorders, USA); Zachary Stowe (University of Arkansas for Medical Sciences, Department of Psychiatry, USA), Ian Jones (Cardiff University School of Medicine, Institute of Psychological Medicine and Clinical Neuroscience, UK); David Rubinow (The University of North Carolina at Chapel Hill, Department of Psychiatry, USA); Patrick Sullivan (The University of North Carolina at Chapel Hill, Department of Genetics, USA); and Samantha Meltzer-Brody (The University of North Carolina at Chapel Hill, Department of Psychiatry, USA).
Footnotes
Contributors
The individual studies contributing to the PACT analyses were led by ER-B, KMS, JLP, VB, KMD, MA, GA, AV, PKM, PL, BWP, MWO, SJR, CG, CNE, PJS, KLW, ZNS, IJ, DRR, PFS, and SM-B. The core statistical analysis group was led by KTP, TM-O, PFS, and SM-B. The management group, which comprised the study leaders and the core statistical group and was responsible for the management of the project and the overall content of the manuscript was led by KTP and SM-B. The PACT phenotype committee comprised ER-B, KMS, JLP, VB, KMD, MA, DJN, GA, and SM-B. The executive and coordinating committee comprised PJS, KLW, ZNS, IJ, DRR, PFS, and SM-B. The remaining authors contributed to the recruitment or data processing of the latent class analysis. KTP and SM-B took responsibility for the primary drafting of the manuscript, which was shaped by the phenotype and executive committees. All authors saw, had the opportunity to comment on, and approved the final draft.
Declaration of interest
We declare no competing interests.
References
- 1.Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005;106:1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- 2.Gaynes BN, Gavin N, Meltzer-Brody S, et al. Perinatal depression: prevalence, screening accuracy, and screening outcomes. Evid Rep Technol Assess (Summ) 2005;119:1–8. doi: 10.1037/e439372005-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005;8:77–87. doi: 10.1007/s00737-005-0080-1. [DOI] [PubMed] [Google Scholar]
- 4.Paulson JF, Dauber S, Leiferman JA. Individual and combined effects of postpartum depression in mothers and fathers on parenting behavior. Pediatrics. 2006;118:659–668. doi: 10.1542/peds.2005-2948. [DOI] [PubMed] [Google Scholar]
- 5.Marmorstein NR, Malone SM, Iacono WG. Psychiatric disorders among offspring of depressed mothers: associations with paternal psychopathology. Am J Psychiatry. 2004;161:1588–1594. doi: 10.1176/appi.ajp.161.9.1588. [DOI] [PubMed] [Google Scholar]
- 6.O’Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annu Rev Clin Psychol. 2013;9:379–407. doi: 10.1146/annurev-clinpsy-050212-185612. [DOI] [PubMed] [Google Scholar]
- 7.Jones I, Craddock N. Searching for the puerperal trigger: molecular genetic studies of bipolar affective puerperal psychosis. Psychopharmacol Bull. 2007;40:115–128. [PubMed] [Google Scholar]
- 8.Robertson-Blackmore E, Putnam FW, Rubinow DR, et al. Antecedent trauma exposure and risk of depression in the perinatal period. J Clin Psychiatry. 2013;74:e942–e948. doi: 10.4088/JCP.13m08364. [DOI] [PubMed] [Google Scholar]
- 9.Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. 2004;26:289–295. doi: 10.1016/j.genhosppsych.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 10.Mercier RJ, Garrett J, Thorp J, Siega-Riz AM. Pregnancy intention and postpartum depression: secondary data analysis from a prospective cohort. BJOG. 2013;120:1116–1122. doi: 10.1111/1471-0528.12255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bloch M, Rubinow DR, Schmidt PJ, Lotsikas A, Chrousos GP, Cizza G. Cortisol response to ovine corticotropin-releasing hormone in a model of pregnancy and parturition in euthymic women with and without a history of postpartum depression. J Clin Endocrinol Metab. 2005;90:695–699. doi: 10.1210/jc.2004-1388. [DOI] [PubMed] [Google Scholar]
- 12.Wisner KL, Sit DK, McShea MC, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry. 2013;70:490–498. doi: 10.1001/jamapsychiatry.2013.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wisner KL, Moses-Kolko EL, Sit DK. Postpartum depression: a disorder in search of a definition. Arch Womens Ment Health. 2010;13:37–40. doi: 10.1007/s00737-009-0119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Arlington, VA: American Psychiatric Press; 2013. [Google Scholar]
- 15.WHO. International Statistical Classification of Diseases and Related Health Problems. 10th. Geneva: World Health Organization; 1992. [Google Scholar]
- 16.WHO. mhGAP intervention guide for mental, neurological and substance use disorders in non-specialized health settings. Geneva: World Health Organization; 2010. [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Prevalence of self-reported postpartum depressive symptoms—17 states, 2004–2005. MMWR Morb Mortal Wkly Rep. 2008;11:361–366. [PubMed] [Google Scholar]
- 18.Tsai J, Harpaz-Rotem I, Pilver CE, et al. Latent class analysis of personality disorders in adults with posttraumatic stress disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2014;75:276–284. doi: 10.4088/JCP.13m08466. [DOI] [PubMed] [Google Scholar]
- 19.Sullivan PF, Kessler RC, Kendler KS. Latent class analysis of lifetime depressive symptoms in the national comorbidity survey. Am J Psychiatry. 1998;155:1398–1406. doi: 10.1176/ajp.155.10.1398. [DOI] [PubMed] [Google Scholar]
- 20.Hagenaars JA, McCutcheon AL, editors. Applied latent class analysis. Cambridge: Cambridge University Press; 2002. [Google Scholar]
- 21.Garrett ES, Zeger SL. Latent class model diagnosis. Biometrics. 2000;56:1055–1067. doi: 10.1111/j.0006-341x.2000.01055.x. [DOI] [PubMed] [Google Scholar]
- 22.Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6:278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- 23.Ji S, Long Q, Newport DJ, et al. Validity of depression rating scales during pregnancy and the postpartum period: impact of trimester and parity. J Psychiatr Res. 2011;45:213–219. doi: 10.1016/j.jpsychires.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 25.Meltzer-Brody S, Boschloo L, Jones I, Sullivan PF, Penninx BW. The EPDS-Lifetime: assessment of lifetime prevalence and risk factors for perinatal depression in a large cohort of depressed women. Arch Womens Ment Health. 2013;16:465–473. doi: 10.1007/s00737-013-0372-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leucht S, Fennema H, Engel R, Kaspers-Janssen M, Lepping P, Szegedi A. What does the HAMD mean? J Affect Disord. 2013;148:243–248. doi: 10.1016/j.jad.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 27.First MB, Gibbon M, Spitzer RL, Williams JBW, editors. Structured clinical interview for DSM-IV axis 1 disorders: clinical version (SCID-CV) Washington, DC: American Psychiatric Press; 1995. [Google Scholar]
- 28.Wing JK, Babor T, Brugha T, et al. SCAN. Schedules for clinical assessment in neuropsychiatry. Arch Gen Psychiatry. 1990;47:589–593. doi: 10.1001/archpsyc.1990.01810180089012. [DOI] [PubMed] [Google Scholar]
- 29.Muthen B, Asparouhov T. Bayesian structural equation modeling: a more flexible representation of substantive theory. Psychol Methods. 2012;17:313–335. doi: 10.1037/a0026802. [DOI] [PubMed] [Google Scholar]
- 30.Celeux G, Soromenho G. An entropy criterion for assessing the number of clusters in a mixture model. J Classification. 1996;13:195–212. [Google Scholar]
- 31.Byrne EM, Carrillo-Roa T, Penninx BW, et al. Applying polygenic risk scores to postpartum depression. Arch Womens Ment Health. 2014;17:519–528. doi: 10.1007/s00737-014-0428-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meltzer-Brody S, Brandon AR, Pearson B, et al. Evaluating the clinical effectiveness of a specialized perinatal psychiatry inpatient unit. Arch Womens Ment Health. 2014;17:107–113. doi: 10.1007/s00737-013-0390-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meltzer-Brody S, Stuebe A. The long-term psychiatric and medical prognosis of perinatal mental illness. Best Pract Res Clin Obstet Gynaecol. 2014;28:49–60. doi: 10.1016/j.bpobgyn.2013.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Munk-Olsen T, Laursen TM, Meltzer-Brody S, Mortensen PB, Jones I. Psychiatric disorders with postpartum onset: possible early manifestations of bipolar affective disorders. Arch Gen Psychiatry. 2012;69:428–434. doi: 10.1001/archgenpsychiatry.2011.157. [DOI] [PubMed] [Google Scholar]
- 35.Cox JLRA, Thomas PF, Wrate RW. How accurately do mothers recall postnatal depression? Further data from a 3 year follow-up study. J Psychosomatic Obstet Gynecol. 1984;3:185–189. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.