Abstract
Background:
Tibial platfond fractures are usually associated with massive swelling of the foot and ankle, as well as with open wounds. This swelling may cause significant decrease of the blood flow, so the state of the soft tissue is determinant for the surgical indication and the type of implant. This retrospective study compares the union times in cases of tibial plafond fractures managed with a hybrid external fixation as a definitive procedure versus those managed with a two stage strategy with final plate fixation.
Materials and Methods:
A retrospective study in a polytrauma referral hospital was performed between 2005 and 2011. Patients with a tibial plafond fracture, managed with a hybrid external fixation as a definitive procedure or managed with a two stage strategy with the final plate fixation were included in the study. Postoperative radiographs were evaluated by two senior surgeons. Fracture healing was defined as callus bridging of one cortex, seen on both lateral and anteroposterior X-ray. The clinical outcome was evaluated by means of 11 points Numerical Rating Scale for pain and The American Orthopedic Foot and Ankle Society ankle score, assessed at the last followup visit. Thirteen patients had been managed with a hybrid external fixation and 18 with a two-stage strategy with the final plate fixation. There were 14 males and 17 females with a mean age of 48 years (range 19–82 years). The mean followup was 24 months (range 24–70 months).
Results:
The mean time from surgery to weight bearing was 7 ± 6.36 days for the hybrid fixation group and 57.43 ± 15.46 days for the plate fixation group (P < 0.0001); and the mean time from fracture to radiological union was 133.82 ± 37.83) and 152.8 ± 72.33 days respectively (P = 0.560).
Conclusion:
Besides the differences between groups regarding the baseline characteristics of patients, the results of this study suggest that in cases of tibial plafond fractures, the management with a hybrid external fixation as a definitive procedure might involve a faster union than a two-stage management with final plate fixation.
Keywords: Fracture healing, hybrid external fixation, polyaxial locking plates, tibial plafond fractures
MeSh terms: Tibial fracture, fracture fixation, orthopedic fixation devices
INTRODUCTION
Tibial plafond fractures are comminuted fractures of the distal tibia, which involve a traumatic axial load mechanism that leads to destruction of the joint surface. These fractures are usually associated with massive swelling of the foot and ankle, as well as with open wounds. The swelling may cause a significant decrease in the blood flow and the state of the soft tissues is detrimental for the therapeutic indication and the type of implant.1 The surgeon's preference and experience also plays an important role in the choice of treatment.2
Treatment options are open reduction and internal “rigid” fixation, closed reduction and internal “biological” fixation with minimal periosteal stripping and preservation of soft tissues and external fixation with preservation of the soft tissues, with or without minimal osteosynthesis and the possibility of immediate weight bearing.
There is broad consensus that status of the soft tissue is the first priority because it is the basis for fracture healing and good long-term outcomes. Surgical intervention can be managed as a one- or multi-stage procedure, with internal or external fracture fixation.3 The surgical approaches necessary for plating might cause a great insult to the soft tissue, which might involve the development of surgical wound infections and skin necrosis that could compromise and delay the union process and compromise the functional outcome. The importance of the hybrid fixation lies in the fact that the soft tissue is minimally affected, the joint movement is preserved, the weight bearing can be allowed early thus promoting fracture union.
This retrospective study compares the union times in cases of tibial plafond fractures managed with a hybrid external fixation as a definitive procedure versus those managed with a two-stage strategy with final plate fixation. This study also compares the long term clinical and radiological results of patients who had a tibial plafond fracture that were definitely treated with a hybrid external fixator or with a two stage strategy with final plate fixation.
MATERIALS AND METHODS
This study was performed in a polytrauma referral hospital between 2005 and 2011. 31 patients with a tibial plafond fracture managed with a hybrid external fixation as a definitive procedure or managed with a two-stage strategy with final plate fixation were included in the study. The following retrospective data were gathered from the electronic medical files: Date of birth, gender, date of tibial plafond fracture, type of tibial plafond fracture according to the AO/OTA classification, mechanism of injury, associated lesions, date of surgery, type of surgery and adverse events related to treatment.
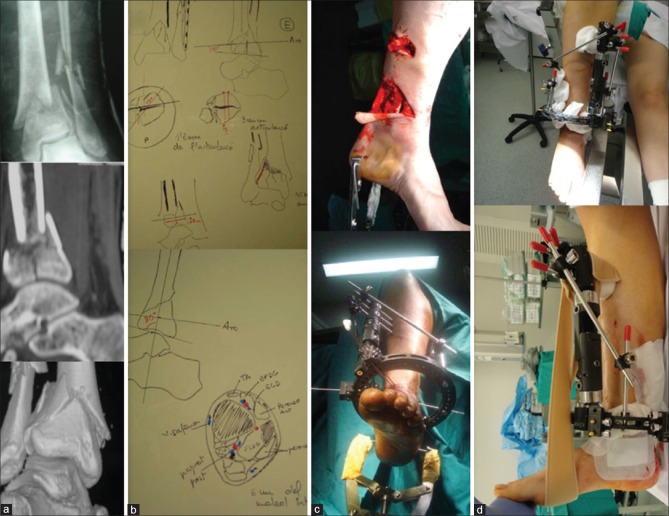
Simple X-ray in the anteroposterior and lateral views were performed in all the cases, as well as preoperative computed tomography (CT)-scan with three-dimensional reconstructions. Fracture type was classified according to the AO/OTA classification [Figure 1a]. Open fractures were classified according to the Gustilo and Anderson classification.4
Figure 1.
(a) Simple X-ray, computed tomography (CT)-scan sagittal reconstruction and CT-scan three-dimensional reconstruction showing tibial plafond fracture AO/OTA 43-C2. (b) Drawing of the preoperative planning for the proper reduction and pin placement. (c) Intraoperative transcalcaneal traction useful to achieve proper reduction. (d) Immediate postoperative fixation, in which a sling is placed to hold the foot in order to avoid the equinus position of the foot thus saving metatarsal pinning
The type of surgery and the timing of the management were decided by the consultant in charge of every case. These decisions were mainly based on the status of the soft tissue, which is the most important factor for the surgical timing and the type of surgery. Surgery was performed when the skin showed wrinkles and there were no blisters. Careful preoperative planning was performed in all cases [Figure 1b].
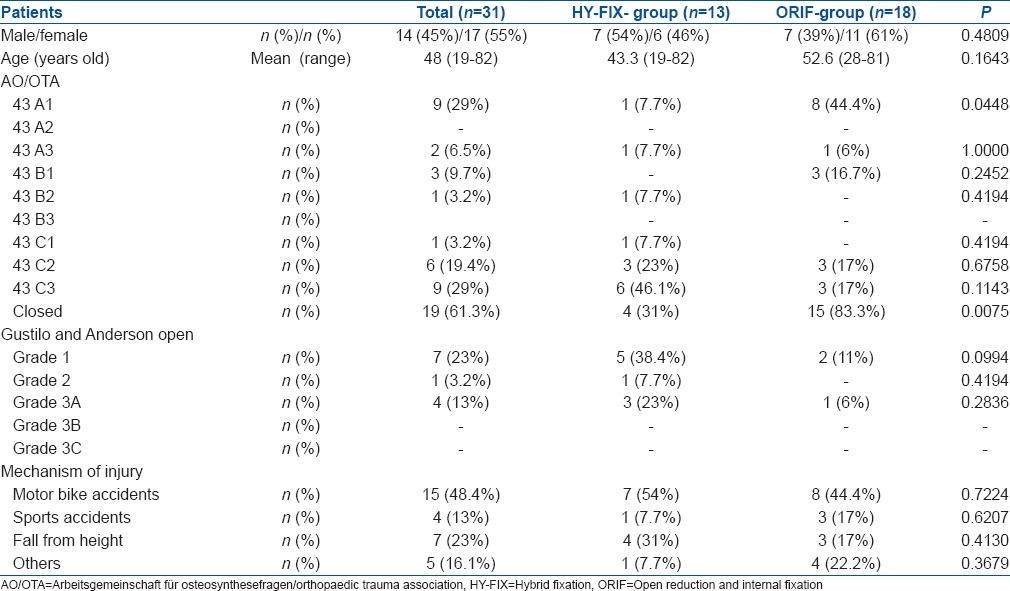
13 patients had been managed with a hybrid external fixation and 18 patients had been managed with a two-stage strategy with final plate fixation. There were 14 males and 17 females with a mean age of 48 years (range 19–82 years). The mean followup was 24 months (range 24–70 months). The right tibia was involved in 17 patients and the left in 14 patients. The associated lesions were fracture middle third forearm (n = 1), fracture distal radius (n = 2) in the Open Reduction and Internal Fixation Group (ORIF-group) and elbow fracture dislocation (olecranon fracture) (n = 1), distal radius fracture (n = 1) and proximal humeral fracture (n = 1) in the Hybrid Fixation Group (HY-FIX-group), [Table 1].
Table 1.
Clinical details of the patients
In the ORIF-group, temporary stabilization was performed at the first moment in 22.22% (4/18) patients. In 5.6% (1/18) of these patients, a transcalcaneal traction with Braun's frame was used, and in 16.7% (3/18) of the patients, a monolateral external fixator was used. In the rest of the patients of the ORIF-group, the first stage of the management consisted of an immobilization of the leg and ankle with a posterior slab. In 100% (13/13) of the patients of the HY-FIX-group, hybrid external fixation was performed within the first 48 h after fracture.
The surgery was performed under epidural anesthesia and femoral nerve block. In patients with closed fractures and in patients with open fractures Grade I and II, 2 g of cefazolin was administrated half an hour before surgery and 2 g every 8 h during 24 h. In patients with open fractures Grade III, 1 g of cefazolin every 8 h and 240 milligrams of gentamicin per day was administrated for 3 days starting since the patient was admitted in the hospital. In open fractures, an exhaustive lavage was done in all cases at time of admission. In those patients with open fractures in which surgery had to be delayed for more than 3 days, antibiotics were administrated during the first 3 days. Low-molecular heparin prophylaxis was given from the day of admission until 20 days after discharge.5
All patients were operated by two senior surgeons (LSV and JDC).
HY-FIX-group
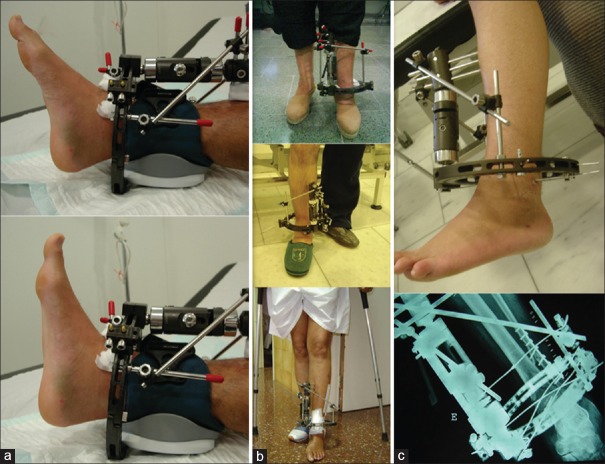
All patients of the HY-FIX-group were operated without tourniquet. In 53.84% (7/13) of patients of the HY-FIX-group, an intraoperative transcalcaneal traction was placed in order to achieve proper alignment and reduction [Figure 1c]. The hybrid external fixators used were Orthofix® (Texas, USA). The postoperative immediate equinus attitude of the foot was managed by means of a sling that was holded to the external fixator [Figure 1d]. In none of the patients of the HY-FIX-group pinning in the first metatarsal was performed, in order to allow a free range of motion (ROM) of the ankle [Figure 2a] and early weight bearing [Figure 2b]. Intraarticular reduction was achieved by means of the transcalcaneal traction, ligamentotaxis and Olivewire. In none of the patients with the HY-FIX-group minimal internal fixation of the tibia was performed. In 92.3% (12/13) of the cases of the HY-FIX-group a fibular plate was used [Figure 2c]. In one of the patients of the HY-FIX-group lateral translation of the distal fracture fragment was observed [Figure 3a] so it had to be surgically corrected by means of a second surgery that consisted of pulling medially with Olivewire [Figure 3b and c]. In the HY-FIX-group, no bone grafting was used.
Figure 2.
(a) Clinical photograph showing ankle range of motion 10 days after hybrid externalfixation. (b) Clinical photograph showing that early weight bearing is allowed in order to promote union (c) Clinical and radiological aspect of a tibial plafond fracture AO/OTA 43-C1 30 days after fixation
Figure 3.
(a) Postoperative X-ray of ankle joint with leg bones showing lateral translation of the distal fragment (b) The lateral translation was corrected by means of a Olive-wire in same patient (c) X-ray anteroposterior view of ankle joint and clinical photograph (d) showing fracture union and fixator has been removed; patient weight bearing (at 5 months followup)
ORIF-group
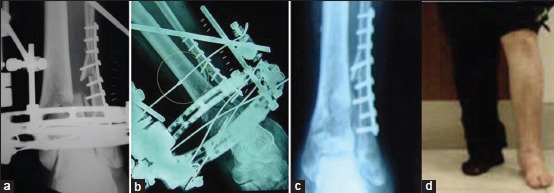
In the ORIF-group, the timing of definitive plate fixation was established by means of daily evaluation of the skin. All patients in the ORIF-group were operated under tourniquet. Intraarticular reduction was achieved by means of direct manipulation of the fragments and provisional fixation with K-wire. The polyaxial locking plates (A.L.P.S, Biomet, London, United Kingdom) used were: 14 medial plates [Figure 4a and b], 4 anterolateral plates [Figure 4c] and 12 fibular plates [Figure 4d]. In 27.77% (5/18) of patients of the ORIF-group, minimal internal fixation of the tibia was performed by means of screws. In 66.7% (12/18) of the cases of the ORIF-group a fibular plate was used. In the ORIF-group bone grafting was used in 1 case.
Figure 4.
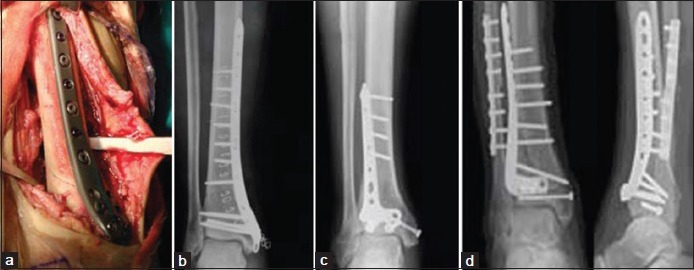
(a) Peroperative photograph showing anteromedial approach to the distal tibia used to perform open reduction and internal fixation with a medial plate (b) Postoperative X-ray leg bones with ankle joint showing the reduction achieved. (c and d) X-rays of leg bones with ankle showing A.L.P.S. Anterolateral plates, without fibular plate (c) and with fibular plate (d)
The postoperative radiographs were evaluated by both the senior surgeons (LSV and JDC). Fracture healing was defined as callus bridging of one cortex, seen on both lateral and anteroposterior (AP) X-rays.6 In 22.2% (4/18) of the cases of the ORIF-group, fracture healing had to be assessed by means of a CT-scan, because the plate obstructed the visualization of the callus on the X-ray.
The clinical outcome was evaluated by means of the 11 points Numerical Rating Scale (NRS7) for pain and The American Orthopedic Foot and Ankle Society (AOFAS) ankle score, assessed at the last followup visit. The Checketts-Otterburns classification was used to describe pin infections.8
Statistical analysis
In this study, no formal sample size was calculated. The sample was confirmed by all of the patients of the study period who fulfilled the inclusion criteria. Statistical analysis was carried out according to the complete sample analysis.
Continuous variables are presented as mean and standard deviation (SD), mean and range or median and interquartil range (IQR). Categorical variables are presented as percentages and frequencies. The relationship between variables was analyzed with contingency tables for the categorical ones, and the inference was studied with the χ2 test or Fisher's exact test depending on what corresponded. The inference in continuous variables was calculated with the Mann-Whitney test, and their results are presented with their corresponding SD. The level of significance was set at 5% (α = 0.05). Data were analyzed by use of the SPSS 19 (SPSS Inc., Chicago, IL, USA).
RESULTS
In the HY-FIX-group, the mean time elapsed from external fixation to removal of the device was 146.87 ± 53.51 days. In one of the patients, the external fixator had to be removed 3 weeks after fixation because of intolerance of the pins, so the rest of the treatment was managed with a cast.
Early weight bearing was allowed in 84.6% (11/13) of the cases in the HY-FIX-group and in none of the cases in the ORIF-group. The mean time elapsed from surgery to weight bearing in both groups is shown in Table 2.
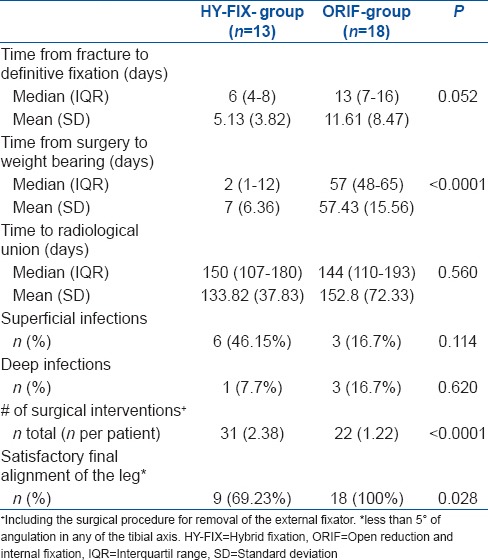
Table 2.
Comparative results between groups
Radiographic followup
92.3% (12/13) of cases in the HY-FIX-group united without the need of any extra surgical revision. In the ORIF-group, there were no alignment defects or limb length differences in the telemetry x-rays. In the HY-FIX-group, the final alignment was satisfactory (<5° of angulation in any axis of the tibia) in 9 cases. One case united in a 10° varus position of the distal fibula, reason why an osteotomy of the distal fibula had to be performed 5 months after the fracture. In 1 case, an osteotomy of the fibula had to be performed to correct valgus malunion of the fibula. In 2 cases, the final union was achieved with a tibial antecurvatum of 9° and 10° respectively [Figure 5a] and in 1 case the final union showed a valgus deformity of the ankle of 11°.
Figure 5.
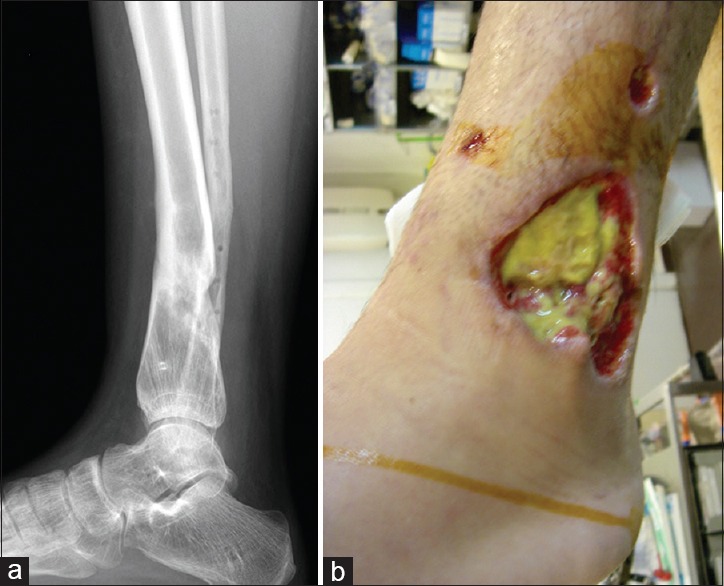
(a) Last followup X-ray of leg bones with ankle joint lateral view of a case of the hybrid fixation group (HY-FIX-group) in which union was achieved with 10° of antecurvatum. (b) Clinical photograph showing a deep infection of a case of the HY-FIX-group that conditioned removal of the external fixator
Clinical followup evaluations
At the last followup visit, the mean NRS for pain was 3.1 ± 2.53 in the HY-FIX-group and 2.64 ± 1.87 in the ORIF-group (P = 0.836) and all the patients of both groups were able to walk without the need of crutches. The mean value of the AOFAS scale at the final followup was 84.4 (±22.47) in the ORIF-group and 77.33 ± 32.33 in the HY-FIX-group (P = 0.646).
The ROM of the ankle was: Mean plantar flexion 35 ± 4.3° in the ORIF-group and 33 ± 2.8° in the HY-FIX group (P = 1.000); mean dorsiflexion 10 ± 3.3° in the ORIF-group and 11 ± 2.9° in the HY-FIX group (P = 1.000).
Complications
Infections were divided into superficial infections (superficial to the fascia), Pin-site infections and surgical incision infection) and deep infections (deep to the fascia, like osteomyelitis). One case in the HY-FIX-group developed a deep infection 3 months after fracture, which had to be treated by means of removing the external fixator, surgical debridement and antibiotics [Figure 5b]. Totally, 3 cases in the HY-FIX-group had a late infection of pin tracts and were managed with antibiotics. Skin necrosis was observed in 3 cases of the ORIF-group and in 1 case the fibular plate had to be removed.
DISCUSSION
The main finding of our study shows that in cases of tibial plafond fractures, the management with a hybrid external fixation as a definitive procedure might involve a faster union than a two stage management with final plate fixation. Even though the differences between the two groups were not statistically significant vis-a-vis the elapsed time from fixation to radiological union; and the fact that there were important differences between groups regarding the type of fractures, we believe that the early weight bearing of patients of the HY-FIX-group and the lesser aggression to the soft tissues involved with this treatment method, could suppose a determinant factor in the biomechanics of the union process.
Previous studies have reported satisfactory union rates when using the external fixation strategy as a definitive method of treatment in cases of tibial plafond fractures.9 Hybrid external fixation systems in cases of tibial plafond fractures allow early mobilization and weight bearing. The use of circular frames is considered to allow better indirect reduction, progressive correction of deformities and offer improved results.10,11 The dynamization effect of the fracture that is obtained with the hybrid fixation is considered to promote healing and union. Systems too rigid and surgical approaches too aggressive might predispose to the development of nonunion.
Open reduction and internal fixation with plating remains the gold standard for the treatment of tibial plafond fractures.12 There has been an increasing trend toward the use of contoured polyaxial locking plates because the good match between the plate and the distal part of the tibia reduces the prominence and soft tissue trauma.13 It has been shown that they maximize periarticular fragment fixation, provide a better pullout strength and angular stability around small distal fragments.14 Despite the theoretical advantages of this type of fixation, scarce information regarding the clinical results of treatment has been published. On the other side, it has been certainly proved that minimally invasive techniques reduce wound complications thus favoring the healing process.15
It has been shown that closed fractures heal significantly faster than open fractures; and that fractures managed with minimally invasive techniques also heal faster than fractures managed with open conventional approaches.13 In our study, open fractures were more prevalent in the group that was managed with a minimally invasive technique (HY-FIX-group). Even though time to radiological union was shorter in the HY-FIX-group when compared to the ORIF-group, these results make us ratify the idea that minimally invasive techniques that are less aggressive with the soft tissues preserve the bone healing potential.
Previous studies have reported a low rate of reoperations when managing tibial plafond fractures with a Hybrid external fixation as a definitive method of treatment.16 It has been observed a lesser loss of alignment with hybrid external fixators that with monolateral fixators.17 Randomized prospective studies that compared ORIF and external fixation concluded that external fixation was associated with significantly fewer complications when treating high-energy tibial plafond injuries.18,19
Lower rates of infections have been reported when hybrid thin wire external fixation methods were used for the management of articular fractures.20 It has been also reported that the soft tissue affection of ORIF methods could predispose to high rate of infections as the skin vascularity might be compromised by the surgical approach.21 As far as our knowledge, there is scarce comparative data regarding the rate of infections in cases of tibial plafond fractures managed with an Hybrid external fixation or with a two-stage management with final plate fixation. Although the differences in our study are not statistically significant, the proportion of deep infections was lower in the HY-FIX-group when compared to the ORIF-group. We believe that less aggressive surgical approach performed in cases of the HY-FIX-group had an influence on these results.
Previous studies have reported that osteosynthesis of the fibula is crucial in order to guarantee a proper reduction and alignment of the ankle joint in cases of tibial plafond fractures.22 All fibular fractures (92.3%) in the HY-FIX-group of our study were managed with internal fixation associated to the hybrid external fixation of the tibia. In all these cases, internal fixation of the fibula was performed first followed by the external fixation of the tibia, because initial fixation of the distal fibula restores the length of the limb and facilitates indirect closed reduction and percutaneous pinning of the tibial plafond fracture.
Management of tibial plafond fractures is technically demanding and it should be only relegated to specific trauma units with experience in the treatment of this kind of complex injuries. Open anatomical reduction and plate fixation is technically a highly demanding procedure; but closed anatomic reduction, pinning fixation and stabilization with a circle frame, is a procedure that should be only relegated to surgeons familiarized with this kind of specific procedures.
The main limitations of this study are: Its retrospective design, the heterogeinicity of the pathology and the treatments strategies, the fact that the population was not stratified in sub-groups, and the fact that the patients of the HY-FIX-group were mainly operated by one surgeon and the cases of the ORIF-group were mainly operated by another surgeon.
Besides the differences between groups regarding the baseline characteristics of patients, the results of this study suggest that in cases of tibial platfond fractures, the management with an hybrid external fixation as a definitive procedure might involve a faster union than a two stage management with final plate fixation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Tang X, Liu L, Tu CQ, Li J, Li Q, Pei FX. Comparison of early and delayed open reduction and internal fixation for treating closed tibial pilon fractures. Foot Ankle Int. 2014;35:657–64. doi: 10.1177/1071100714534214. [DOI] [PubMed] [Google Scholar]
- 2.Rommens PM, Claes P, Broos PL. Therapeutic strategy in pilon fractures type C2 and C3: Soft tissue damage changes treatment protocol. Acta Chir Belg. 1996;96:85–92. [PubMed] [Google Scholar]
- 3.Huebner EJ, Iblher N, Kubosch DC, Suedkamp NP, Strohm PC. Distal tibial fractures and pilon fractures. Acta Chir Orthop Traumatol Cech. 2014;81:167–76. [PubMed] [Google Scholar]
- 4.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: Retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453–8. [PubMed] [Google Scholar]
- 5.Testroote M, Stigter WA, Janssen L, Janzing HM. Low molecular weight heparin for prevention of venous thromboembolism in patients with lower-leg immobilization. Cochrane Database Syst Rev. 2014;4:CD006681. doi: 10.1002/14651858.CD006681.pub3. [DOI] [PubMed] [Google Scholar]
- 6.Bhandari M, Guyatt GH, Swiontkowski MF, Tornetta P, 3rd, Sprague S, Schemitsch EH. A lack of consensus in the assessment of fracture healing among orthopaedic surgeons. J Orthop Trauma. 2002;16(8):562–6. doi: 10.1097/00005131-200209000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Grimmer-Somers K, Vipond N, Kumar S, Hall G. A review and critique of assessment instruments for patients with persistent pain. J Pain Res. 2009;2:21–47. doi: 10.2147/jpr.s4949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Checketts RG, Otterburn M, Mac Eachern AG. Pin track infection; Definition, incidence and prevention. Int J Orthop Trauma. 1993;3:16–8. [Google Scholar]
- 9.Ristiniemi J. External fixation of tibial pilon fractures and fracture healing. Acta Orthop Suppl. 2007;78:3, 5–34. [PubMed] [Google Scholar]
- 10.Bacon S, Smith WR, Morgan SJ, Hasenboehler E, Philips G, Williams A, et al. A retrospective analysis of comminuted intra-articular fractures of the tibial plafond: Open reduction and internal fixation versus external Ilizarov fixation. Injury. 2008;39:196–202. doi: 10.1016/j.injury.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 11.Giotakis N, Panchani SK, Narayan B, Larkin JJ, Al Maskari S, Nayagam S. Segmental fractures of the tibia treated by circular external fixation. J Bone Joint Surg Br. 2010;92:687–92. doi: 10.1302/0301-620X.92B5.22514. [DOI] [PubMed] [Google Scholar]
- 12.Calori GM, Tagliabue L, Mazza E, de Bellis U, Pierannunzii L, Marelli BM, et al. Tibial pilon fractures: Which method of treatment? Injury. 2010;41:1183–90. doi: 10.1016/j.injury.2010.08.041. [DOI] [PubMed] [Google Scholar]
- 13.Gao H, Zhang CQ, Luo CF, Zhou ZB, Zeng BF. Fractures of the distal tibia treated with polyaxial locking plating. Clin Orthop Relat Res. 2009;467:831–7. doi: 10.1007/s11999-008-0459-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kääb MJ, Frenk A, Schmeling A, Schaser K, Schütz M, Haas NP. Locked internal fixator: Sensitivity of screw/plate stability to the correct insertion angle of the screw. J Orthop Trauma. 2004;18:483–7. doi: 10.1097/00005131-200409000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Richard RD, Kubiak E, Horwitz DS. Techniques for the surgical treatment of distal tibia fractures. Orthop Clin North Am. 2014;45:295–312. doi: 10.1016/j.ocl.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 16.Blauth M, Bastian L, Krettek C, Knop C, Evans S. Surgical options for the treatment of severe tibial pilon fractures: A study of three techniques. J Orthop Trauma. 2001;15:153–60. doi: 10.1097/00005131-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Tornetta P, 3rd, Weiner L, Bergman M, Watnik N, Steuer J, Kelley M, et al. Pilon fractures: Treatment with combined internal and external fixation. J Orthop Trauma. 1993;7:489–96. doi: 10.1097/00005131-199312000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Pugh KJ, Wolinsky PR, McAndrew MP, Johnson KD. Tibial pilon fractures: A comparison of treatment methods. J Trauma. 1999;47:937–41. doi: 10.1097/00005373-199911000-00022. [DOI] [PubMed] [Google Scholar]
- 19.Wyrsch B, McFerran MA, McAndrew M, Limbird TJ, Harper MC, Johnson KD, et al. Operative treatment of fractures of the tibial plafond. A randomized, prospective study. J Bone Joint Surg Am. 1996;78:1646–57. doi: 10.2106/00004623-199611000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Lerner A, Stein H. Hybrid thin wire external fixation: An effective, minimally invasive, modular surgical tool for the stabilization of periarticular fractures. Orthopedics. 2004;27:59–62. doi: 10.3928/0147-7447-20040101-20. [DOI] [PubMed] [Google Scholar]
- 21.Wang D, Xiang JP, Chen XH, Zhu QT. A meta-analysis for postoperative complications in tibial plafond fracture: Open reduction and internal fixation versus limited internal fixation combined with external fixator. J Foot Ankle Surg. 2014 Aug 12; doi: 10.1053/j.jfas.2014.06.007. doi: 10.1053/j.jfas.2014.06007. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 22.Stein H, Lerner A. Is rigid fixation of the fibula indicated in tibial plafond fractures? Orthopedics. 2005;28:438. doi: 10.3928/0147-7447-20050501-04. [DOI] [PubMed] [Google Scholar]