Abstract
Background:
Poor screw-to-bone fixation is a clinical problem that can lead to screw loosening. Under-tapping (UT) the pedicle screw has been evaluated biomechanically in the past. The objective of the study was to determine if pedicle preparation with a sequential tapping technique will alter the screw-to-bone fixation strength using a stress relaxation testing loading protocol.
Materials and Methods:
Three thoracolumbar calf spines were instrumented with pedicle screws that were either probed, UT, standard-tapped (ST), or sequential tapped to prepare the pedicle screw track and a stress relaxation protocol was used to determine pull-out strength. The maximum torque required for pedicle screw insertion and pull-out strength was reported. A one-way ANOVA and Tukeys post-hoc test were used to determine statistical significance.
Results:
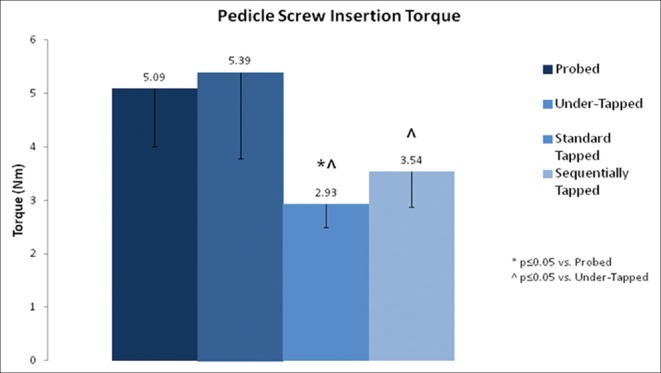
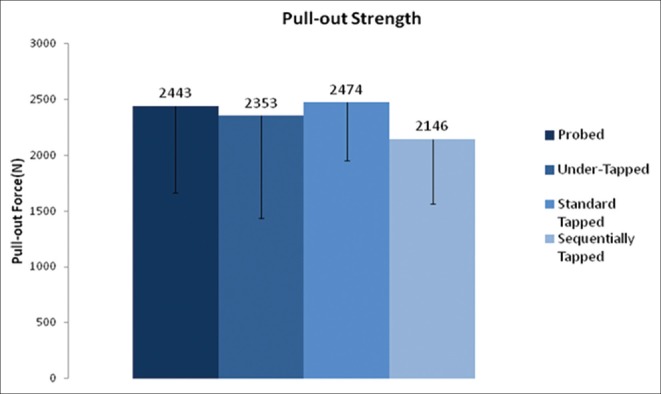
The pedicle screw insertion torques for the probed, UT, ST and sequentially tapped (SQT) techniques were 5.09 (±1.08) Nm, 5.39 (±1.61) Nm, 2.93 (±0.43) Nm, and 3.54 (±0.67) Nm, respectively. There is a significant difference between probed compared to ST (P ≤ 0.05), as well as UT compared to both ST and SQT (P ≤ 0.05). The pull-out strength for pedicle screws for the probed, UT, ST and SQT techniques was 2443 (±782) N, 2353(±918) N, 2474 (±521) N, and 2146 (±582) N, respectively, with no significant difference (P ≥ 0.05) between techniques.
Conclusions:
The ST technique resulted in the highest pull-out strength while the SQT technique resulted in the lowest. However, there was no significant difference in the pull-out strength for the various preparation techniques and there was no correlation between insertion torque and pull-out strength. This suggests that other factors such as bone density may have a greater influence on pull-out strength.
Keywords: Calf vertebral bodies, insertion torque, pull-out strength, stress relaxation, tapping technique
MeSh terms: Bone screws, pedicle, spinal fractures, fracture fixation, biomechanics
INTRODUCTION
Pedicle-based anchors are the most favored means of fixation in posterior spinal stabilization. The interface between the host bone and the pedicle screw presents an important variable in the construct stability. Different screw designs and adaptations such as dual outer diameter screws, expandable screws and cannulated screws supplemented with bone cement have been explored to increase fixation strength.1,2,3,4,5 However, a good technique for inserting the pedicle screws within the confines of the pedicle cannot be understated. Previous studies investigated different tapping techniques; however, no study has incorporated sequential tapping technique in calf specimen using a stress relaxation loading protocol, which reflects the screw failure more closely.6,7,8,9 The purpose of the study was to determine if pedicle preparation with different tapping techniques will alter the screw-to-bone fixation strength using a stress relaxation loading protocol.
MATERIALS AND METHODS
Specimen preparation and insertion techniques
Three thoracolumbar calf spines (T13-L5) were used to minimize the variability in bone mineral density and narrow the study to pedicle preparation technique. The specimens were cleaned of musculature and the posterior insertion points were stripped to the bone. A standard titanium 6.5 mm diameter 50 mm length pedicle screw (Globus Medical Inc.; Audubon, PA, USA) was used during testing and inserted to a depth of 40 mm. Screws were inserted along the midline of the long axis of the pedicle with minimal convergence.1 The said pedicle screw has a thread depth of 0.75 mm. The 5.5 mm and 6.5 mm taps had thread depths of 0.75 mm and 1 mm, respectively. All screw placements were confirmed with fluoroscopic imaging and a ball tip probe was used to verify that no pedicle breach occurred. The pedicle preparation techniques were applied as follows:
Probed (P) - An awl was used to perforate the cortex of the pedicle. A straight pedicle probe was then inserted to a depth of 40 mm to create a screw path. A 6.5 mm diameter 40 mm length pedicle screw was then inserted
Under-tapped (UT) - An awl was used to perforate the cortex of the pedicle and a straight probe was used to create a track 40 mm in depth. A 5.5 mm diameter tap was inserted 40 mm. A 6.5 mm diameter, 40 mm length screw was then inserted
Standard-tapped (ST) - An awl was used to perforate the cortex and a straight probe was inserted to a depth of 40 mm to create the track. A 6.5 mm tap was inserted to a depth of 40 mm. A 6.5 mm diameter, 40 mm length screw was then inserted
Sequentially tapped (SQT) - An awl was used to perforate the cortex and a straight probe was inserted to a 40 mm depth to clear a path. Taps were inserted to a depth of 40 mm in the following order: 4.5 mm, 5.5 mm and finally 6.5 mm diameter. A 6.5 mm diameter, 40 mm length screw was then inserted.
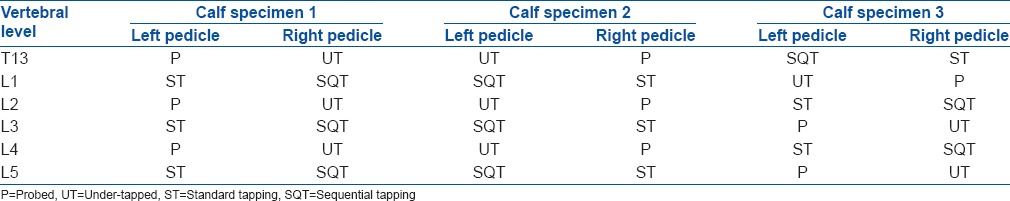
Table 1 lists the placement of each screw in the calf vertebral bodies. Similar results were expected between the probed and UT techniques as well as the ST and sequential tapping, thus the groups were were matched in the same vertebral body to reduce variability. Nine tests for each technique were used for the study for a total of 36 pull-out tests.
Table 1.
Pedicle screw path preparation techniques for each level by specimen
Testing setup
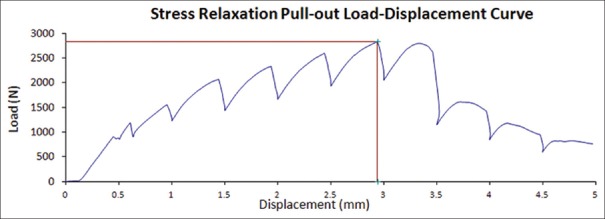
A stress relaxation loading protocol was used to more accurately simulate a physiological environment.8,10 A pull-out rate of 5 mm/min was applied. Furthermore, the tensile loading was paused for 1,000 s for every 0.5 mm of advancement.
Figure 1 shows the test setup. An MTS Mini Bionix III (MTS Corporation, Minneapolis, MN, USA) test machine was used to perform all pull-out tests. A load cell to measure the applied tensile force is located at the bottom of the test machine. Above the load cell is a universal joint to allow rotation so that the axis of the screw remains aligned with the actuator. The universal joint is threaded on both ends and positioned between the load cell and stand. The specimen is secured to the stand with U clamps to prevent translation and rotation. The pull-out fixture slides under the head of the screw and the actuator of the machine applies a vertically positive displacement. The test specimen was positioned so that the path of the screw was on the same axis as the pull-out fixture and actuator.
Figure 1.
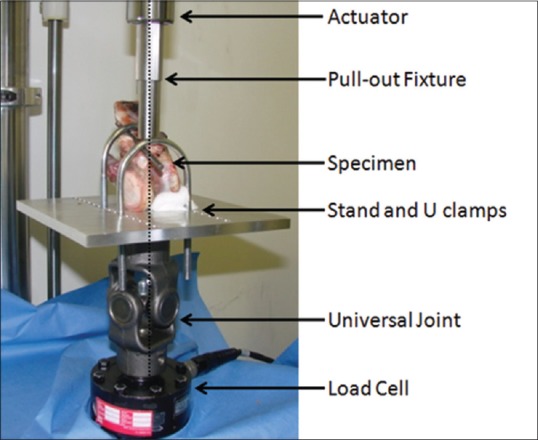
Testing setup in the MTS test machine
Measured parameters
Insertion torques were recorded for all groups using a Multitorq (CDI Torque Products; City of Industry, CA, USA) torque and data collection system [Figure 2]. The maximum torque required for pedicle screw insertion was reported. The pull-out strength of the pedicle screws was defined as the point, in the load-displacement graph, at which the force peaked and then decreased sharply with increasing displacement. A one-way ANOVA and Tukeys post-hoc test were used to determine the significance.
Figure 2.
Torque meter used to measure insertion torques of pedicle screws
Pull-out strength is defined as the maximum point in the load-displacement curve. Insertion torque is the largest value recorded by the sensor during pedicle screw insertion. Screw failure is when the load-displacement curve declined.
RESULTS
Figure 3 shows the insertion torques based on the track preparation technique. The pedicle screw insertion torques for the probed, UT, ST and SQT techniques were 5.09 (±1.08) Nm, 5.39 (±1.61) Nm, 2.93 (±0.43) Nm, and 3.54 (±0.67) Nm, respectively. There is a significant difference between probed compared to ST (P ≤ 0.05), as well as UT compared to both ST and SQT (P ≤ 0.05). Figure 4 is a representative load displacement graph. The pull-out strength for pedicle screws for the probed, UT, ST, and SQT techniques was 2443 (±782) N, 2353 (±918) N, 2474 (±521) N, and 2146 (±582) N, respectively, with no significant difference (P ≥ 0.05) between techniques [Figure 5].
Figure 3.
A bar diagram showing insertion torque of the pedicle screw relative to track preparation technique
Figure 4.
A typical load-displacement graph using the stress relaxation protocol. The graph shows a decrease in load during the hold phase. The peaks of the graph are similar to a standard load-displacement curve
Figure 5.
A bar diagram showing the pull-out strength of the pedicle screws with respect to the hole preparation technique. The pull-out strength for the probed, under-tapped, standard-tapped, and sequentially tapping techniques was 2443 (±782) N, 2353 (±918) N, 2474 (±521) N, and 2146 (±582) N, respectively, with no significant difference (P ≥ 0.05) between techniques
DISCUSSION
Correlation between pedicle screw insertion techniques and increased strength has been examined previously. Chatzistergos et al. tested different tapping techniques in solid rigid polyurethane foam and found that UT increases the pull-out strength of pedicle screws.6 Pfeiffer et al., found no increase in screw pull-out strength between tapping and no tapping.11 Defino et al. performed a similar study using different mediums including calf vertebral bodies, and pull-out strength increased with UT and decreased with reinsertion of the screws.12 In addition, insertion torque also decreased but it did not correlate to reduced pull-out strength.12,13 Insertion torque and ultimate pull-out strength are not affected by either probing or tapping the pedicle screw path.14 The same conclusion was found by another independent group, using human vertebra, where the average pull-out strength differed by < 2%.7 After performing a multiple regression analysis on factors affecting screw-to-bone interface it was found that pedicle bone mineral, insertion torque, and in situ stiffness were the best predictors of screw pull-out force.15 Finally, Kuklo and Lehman found an increased insertion torque with UT but not a definitive positive correlation between bone quality and insertion torque.16 In the present study, potential bias based on bone density is minimized by restricting testing to three calf spines and distributing different pedicle preparation techniques equally among them.
Inceoglu et al. studied pull-out strength in human and calf vertebral bodies, using a stress relaxation protocol.8,10 The stress relaxation protocol used the same pull-out rate and paused for 1,000 s every 0.5 mm of displacement.8,10 Stress relaxation significantly decreased the pull-out strength of pedicle screws in both human and calf bone, compared to the standard testing method.8,10 Another study performed by the same researchers found no significant correlation between pull-out strength and insertion torque.17 Similarly, Kwok et al. determined that “insertion torque is not a reliable predictor of pull-out strength in cadaveric bone.”3 In contrast, Zdeblick et al. concluded that insertion torque is a good predictor of bone to metal interface failure.14
Polymethylmethacrylate cement augmentation, with either prefilled or cement injected cannulated screws, significantly increases screw-to-bone strength compared to no augmentation.2,18 Cement augmentation comes with the risk of leakage into the spinal canal and surrounding area of the vertebral body. Revising a screw with previous cement augmentation is fraught with intra-operative technical difficulties. Previous biomechanical testing has shown increased bone-to-screw interface strength when UT and no difference between drilled and probed trajectories.7,9 Silva et al. investigated the effect of hole preparation using sheep specimens and found that a pilot diameter smaller than the internal diameter of the screw significantly increased the insertion pull-out strength immediately and 8 months postimplantation.9 Other axial pull-out tests report screw insertion torques and pull-out strength similar to our results.7,9,10,12,17 The present study shows that even though, there were significant differences between insertion torques, pedicle screws based on the technique, these differences did not correlate to increased pull-out strength. Based on these findings, the authors do not support the routine use of sequential tapping. UT improves the insertion torque marginally, though the pull-out strength is not affected significantly and is our preferred practice.
The authors of this study believe that stress relaxation protocol replicates the in vivo environment of pedicle screw loosening better than a traditional load-to-failure test. Screw loosening occurs over a period of time postoperatively and thus holding the actuator in between displacements more accurately represents the clinical scenario. Screw failure normally occurs with multiple loads applied over time. The load-displacement curve shows a decrease in load during the hold phase which better simulates a physiological environment. Another possible explanation for the relationship between insertion torque and pull-out strength is alignment of the threads of the pedicle screws with the thread cuts made by the taps. Results showed that the ST screws had the highest pull-out strength, supporting the theory that the pedicle screw threads fell in line with the cuts made by the tap.
Pedicle screw fixation to bone is a clinically important variable in any posterior spinal construct. It is a significant challenge in the older patient and patients with a suboptimal bone density due to co morbidities. Previous solutions include modifications in screw design, screw trajectory and cement augmentation. The current study investigates the role of the tapping techniques on pull-out strength using a stress relaxation loading protocol. Sequential tapping increased the screw path diameter stepwise and in theory allowing for better screw-to-bone interface. Due to specimen translating in the fixture, loading not being applied along the axis of the screw and software problems, certain specimens were excluded from the study. The number of specimens reported for the probed, UT, ST, and SQT groups was 5, 7, 6 and 6 respectively. Due to the matching the groups in the pedicles and the consistency in calf bone quality, there were enough samples to quantify a trend and larger sample size is not expected to alter the conclusions of the study. Previous biomechanical testing using calf vertebral bodies, where dual energy X-ray absorptiometry scans were performed, conclude that the quality of calf bone is comparable to healthy human vertebral bone.4,5,19,20 Lei and Wu tested 100 calf vertebral bodies reported bone mineral density to range from 1.341 to 2.634 g/cm2 (mean 1.822; standard deviation, 0.385) with no significant differences in bone quality between groups (P > 0.05).4 From this large sample size testing, it is reasonable to assume that bone quality was similar between groups.
The screw insertion torque significantly increased based on the pedicle preparation technique used being highest for UT. However, there was no significant difference in pull-out strength for the various preparation techniques. This suggests that other factors such as may have a greater influence on pull-out strength.
Financial support and sponsorship
Provided by Globus Medical Inc., Pennsylvania, United States.
Conflicts of interest
M.M., K.S., B.B., and S.K., are paid employees of Globus Medical Inc., Pennsylvania, United States.
REFERENCES
- 1.Barber JW, Boden SD, Ganey T, Hutton WC. Biomechanical study of lumbar pedicle screws: Does convergence affect axial pullout strength? J Spinal Disord. 1998;11:215–20. [PubMed] [Google Scholar]
- 2.Chao KH, Lai YS, Chen WC, Chang CM, McClean CJ, Fan CY, et al. Biomechanical analysis of different types of pedicle screw augmentation: A cadaveric and synthetic bone sample study of instrumented vertebral specimens. Med Eng Phys. 2013;35:1506–12. doi: 10.1016/j.medengphy.2013.04.007. [DOI] [PubMed] [Google Scholar]
- 3.Kwok AW, Finkelstein JA, Woodside T, Hearn TC, Hu RW. Insertional torque and pull-out strengths of conical and cylindrical pedicle screws in cadaveric bone. Spine (Phila Pa 1976) 1996;21:2429–34. doi: 10.1097/00007632-199611010-00004. [DOI] [PubMed] [Google Scholar]
- 4.Lei W, Wu Z. Biomechanical evaluation of an expansive pedicle screw in calf vertebrae. Eur Spine J. 2006;15:321–6. doi: 10.1007/s00586-004-0867-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lill CA, Schneider E, Goldhahn J, Haslemann A, Zeifang F. Mechanical performance of cylindrical and dual core pedicle screws in calf and human vertebrae. Arch Orthop Trauma Surg. 2006;126:686–94. doi: 10.1007/s00402-006-0186-6. [DOI] [PubMed] [Google Scholar]
- 6.Chatzistergos PE, Sapkas G, Kourkoulis SK. The influence of the insertion technique on the pullout force of pedicle screws: An experimental study. Spine (Phila Pa 1976) 2010;35:E332–7. doi: 10.1097/BRS.0b013e3181ba0b0c. [DOI] [PubMed] [Google Scholar]
- 7.George DC, Krag MH, Johnson CC, Van Hal ME, Haugh LD, Grobler LJ. Hole preparation techniques for transpedicle screws. Effect on pull-out strength from human cadaveric vertebrae. Spine (Phila Pa 1976) 1991;16:181–4. [PubMed] [Google Scholar]
- 8.Inceoglu S, Akbay A, McLain RF. Stress relaxation at the bone-pedicle screw interface in human bone. Spine (Phila Pa 1976. 2006;31:1321–6. doi: 10.1097/01.brs.0000218478.70656.63. [DOI] [PubMed] [Google Scholar]
- 9.Silva P, Rosa RC, Shimano AC, Defino HL. Effect of pilot hole on biomechanical and in vivo pedicle screw-bone interface. Eur Spine J. 2013;22:1829–36. doi: 10.1007/s00586-013-2810-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Inceoglu S, McLain RF, Cayli S, Kilincer C, Ferrara L. Stress relaxation of bone significantly affects the pull-out behavior of pedicle screws. J Orthop Res. 2004;22:1243–7. doi: 10.1016/j.orthres.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 11.Pfeiffer FM, Abernathie DL, Smith DE. A comparison of pullout strength for pedicle screws of different designs: A study using tapped and untapped pilot holes. Spine (Phila Pa 1976) 2006;31:E867–70. doi: 10.1097/01.brs.0000244658.35865.59. [DOI] [PubMed] [Google Scholar]
- 12.Defino HL, Rosa RC, Silva P, Shimano AC, Volpon JB, de Paula FJ, et al. The effect of repetitive pilot-hole use on the insertion torque and pullout strength of vertebral system screws. Spine (Phila Pa 1976) 2009;34:871–6. doi: 10.1097/BRS.0b013e31819e3556. [DOI] [PubMed] [Google Scholar]
- 13.Ricci WM, Tornetta P, 3rd, Petteys T, Gerlach D, Cartner J, Walker Z, et al. A comparison of screw insertion torque and pullout strength. J Orthop Trauma. 2010;24:374–8. doi: 10.1097/BOT.0b013e3181c4a655. [DOI] [PubMed] [Google Scholar]
- 14.Zdeblick TA, Kunz DN, Cooke ME, McCabe R. Pedicle screw pullout strength. Correlation with insertional torque. Spine (Phila Pa 1976) 1993;18:1673–6. doi: 10.1097/00007632-199309000-00016. [DOI] [PubMed] [Google Scholar]
- 15.Myers BS, Belmont PJ, Jr, Richardson WJ, Yu JR, Harper KD, Nightingale RW. The role of imaging and in situ biomechanical testing in assessing pedicle screw pull-out strength. Spine (Phila Pa 1976) 1996;21:1962–8. doi: 10.1097/00007632-199609010-00004. [DOI] [PubMed] [Google Scholar]
- 16.Kuklo TR, Lehman RA., Jr Effect of various tapping diameters on insertion of thoracic pedicle screws: A biomechanical analysis. Spine (Phila Pa 1976) 2003;28:2066–71. doi: 10.1097/01.BRS.0000084665.31967.02. [DOI] [PubMed] [Google Scholar]
- 17.Inceoglu S, Ferrara L, McLain RF. Pedicle screw fixation strength: Pullout versus insertional torque. Spine J. 2004;4:513–8. doi: 10.1016/j.spinee.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 18.Kuhns CA, Reiter M, Pfeiffer F, Choma TJ. Surgical strategies to improve fixation in the osteoporotic spine: The effects of tapping, cement augmentation, and screw trajectory. Global Spine J. 2014;4:47–54. doi: 10.1055/s-0033-1361588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Akbay A, Bozkurt G, Ilgaz O, Palaoglu S, Akalan N, Benzel EC. A demineralized calf vertebra model as an alternative to classic osteoporotic vertebra models for pedicle screw pullout studies. Eur Spine J. 2008;17:468–73. doi: 10.1007/s00586-007-0545-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seller K, Wahl D, Wild A, Krauspe R, Schneider E, Linke B. Pullout strength of anterior spinal instrumentation: A product comparison of seven screws in calf vertebral bodies. Eur Spine J. 2007;16:1047–54. doi: 10.1007/s00586-007-0307-0. [DOI] [PMC free article] [PubMed] [Google Scholar]