Abstract
An estimated 200 million children worldwide fail to meet their development potential due to poverty, poor health, and unstimulating environments. Missing developmental milestones has lasting effects on adult human capital. Africa has a large burden of risk factors for poor child development. The objective of this paper is to identify scope for improvement at the country level in three domains – nutrition, environment, and maternal-child interactions. We used nationally-representative data from large-scale surveys, data repositories, and country reports from 2000–2014. Overall, there was heterogeneity in performance across domains, suggesting that each country faces distinct challenges in addressing risk factors for poor child development. Data were lacking for many indicators, especially in the maternal-child interaction domain. There is a clear need to improve routine collection of high-quality, country-level indicators relevant to child development to assess risk and track progress.
Keywords: Child Development, Human Capital, Africa
INTRODUCTION
As the world has seen large reductions in child mortality over the last decades, there has been increasing focus on improving child development. An estimated 200 million children worldwide fail to meet their development potential due to poverty, poor health, and unstimulating environments. The 2007 and 2011 Lancet series on child development identified major risks for poor child development.(1,2) These risks include intrauterine growth restriction (IUGR), stunting, iodine deficiency, iron-deficiency anemia, malaria, lead exposure, HIV, maternal depression, and inadequate cognitive stimulation. Additionally, maternal education and breastfeeding were identified as protective factors.
Africa has a high burden of risk factors for poor child development. Fifteen of the top 24 countries with the highest burden of stunting worldwide are in sub-Saharan Africa.(3) An estimated 40% of the population, including 58 million school-aged children, have inadequate iodine intakes.(4) In 2010, Tanzania, Uganda, Mozambique and Côte d’Ivoire accounted for an estimated 47% of malaria cases worldwide.(5) Many of these risk factors are inter-related, and the accumulation of risk can lead to long term and enduring impacts on child development. Early life is critical because perturbations during this period of rapid brain development can lead to enduring changes to the brain’s structural and functional capacity.(6) Failure to meet developmental milestones during this critical window has lasting effects throughout the life course, including school achievement, adult earnings, and intergenerational transmission of poverty.(7,8)
The objective of this paper is to identify scope for improvement by classifying countries across levels of risk factors for poor child development and coverage of interventions addressing these risk factors. Identifying high-performing countries allows us to estimate the potential impact of health interventions in sub-Saharan Africa if all countries were to achieve the level of the high performing countries. High performers also serve as a model of positive deviance for the region.
METHODS
Domains of Interest
We focus on the risk factors identified in the Walker et al. Lancet series on child development which are modifiable through maternal, child, or household-level interventions and for which there are nationally-representative indicators.(1,2) The risk factors and interventions influencing cognitive development in children can be divided into three domains: nutrition, environment, and maternal-child interactions.
Nutrition
Major nutritional risk factors for poor child development include IUGR, stunting, iodine deficiency, and iron-deficiency anemia. Low birthweight, a proxy for IUGR, is associated with poor cognitive development.(9–13) Stunting at age two or three has been associated with school attainment, dropout, and later life cognitive deficits.(1) Iodine deficiency is the main cause of preventable mental impairment in childhood.(14) Severe iodine deficiency during pregnancy can lead to cretinism; however, even sub-clinical deficiencies are associated with intellectual impairment and neurological abnormalities.(15) Iron is essential for both mental and physical development. Iron-deficiency anemia may result in impaired motor development, coordination, and scholastic achievement in young children.
Balanced energy and protein supplementation to underweight women, micronutrient supplementation, and intermittent preventive treatment in malaria endemic areas have been shown to increase birthweight, reduce incidence of low birthweight, and/or reduce risk of a small-for-gestational-age baby.(16) A wide range of interventions have demonstrated efficacy in reducing stunting, including complementary feeding education, food supplementation in food insecure populations, preventive zinc supplementation, hygiene interventions that reduce incidence of diarrhea, and deworming in populations with a high burden of intestinal helminthiasis.(16,17) Estimates suggest that existing interventions designed to improve nutrition and related disease could reduce stunting at age 36 months by 36%.(16)
Mass fortification of foodstuffs can address iodine and iron deficiencies. The Iodine Global Network and WHO recommend universal salt iodization to prevent and treat iodine deficiency disorders.(18) Salt iodization decreases the risk of iodine deficiency in children by 41%, improves cognitive function, reduces risk of low intelligence, and improves IQ.(19,20) While iron supplementation can treat and prevent iron deficiency, due to the potential for increased risk of death with malaria infection, it is recommended only for non-malarial areas.(16) Because iron levels in fortified grains are far lower than those of iron supplements, grain fortification is considered an alternative intervention to address iron deficiency. Mass fortification of foodstuffs with iron is estimated to reduce the odds of iron-deficiency anemia in children by 28%.(16)
Breastfeeding is a protective factor for child development. Breastfeeding could benefit child development through improved nutrition, reduced infant morbidity, or mother-child interactions.(1) Studies have shown a small but detectable effect of breastfeeding on child cognition, with larger effects among babies with low birthweight and with longer duration of exclusive breastfeeding.(21–23) Antenatal breastfeeding education and support improve breastfeeding outcomes, including exclusive breastfeeding.(24) Universal implementation of educational and promotional strategies for breastfeeding are estimated to increase exclusive breastfeeding until one month by 30% and from one to five months by 90%.(17)
Environment
Malaria, lead exposure, and HIV are major environmental risk factors for poor child development. In severe or cerebral malaria, organisms can directly damage the brain and central nervous system, causing neurological impairment.(25–27) Malaria infection can indirectly lead to poor child development outcomes through poor nutrition, decreased exploration of the environment, and decreased physical activity.(1) To address the burden of malaria, the Global Malaria Action Plan recommends preventive and therapeutic interventions such as long-lasting insecticide-treated nets (ITN), indoor residual spraying (IRS) with insecticide, and artemisinin-based combination therapies.(5)
Lead is a neurotoxin which has been associated with decreased intelligence and impaired neurobehavioral development.(27) No safe blood lead threshold has been identified with respect to infant and child neurodevelopment.(28) Even at levels below those considered toxic, lead exposure is associated with 2–5 point decreases in IQ.(29) Because leaded fuel has been a major source of lead exposure worldwide, shifting to unleaded fuel is primary intervention to address toxic lead exposure.
HIV-affected children are at increased risk for poor health and development outcomes.(30) Two systematic reviews found delays in all domains of cognitive development in both children infected with HIV and those affected by HIV.(28,29) The WHO recommends ARV for pregnant women with HIV to reduce mother-to-child-transmission (MTCT).(30) Without treatment, approximately a third of infants born to HIV-infected mothers will be infected during pregnancy, birth, or breastfeeding.(31)
Maternal-Child Interactions
Poor maternal mental health is associated with poor child growth and development.(32) It is thought that depressed women interact differently with their children than mothers without depression, leading to poorer cognitive, social-emotional, and behavioral outcomes.(33) A 2006 systematic review of studies from 41 countries worldwide found the reported prevalence of post-partum depression (PPD) ranged from 0% to more than 73%.(33,34) Interventions to address PPD include antidepressants, psychotherapy, support, or a combination of these treatments.(34)
Environments with inadequate stimulation and few opportunities for learning are associated with poor cognitive development outcomes.(1) Studies report higher cognitive function when children are given stimulating environments, with positive effects that are evident for years after the intervention.(35–37) Additionally, maternal education is associated with higher child development. Better-educated women are more likely to delay pregnancy until after adolescence, leading to better birth and early life outcomes in their offspring; conversely, children of young mothers are more likely to suffer from low birthweight, under-nutrition, and poor physical and cognitive development.(38) Interventions to address low maternal education include universal primary/secondary schooling and delaying marriage, as girls who marry early often abandon formal education and become pregnant.(38)
Data Sources and Analyses
To examine the prevalence of risk factors affecting child cognitive development and the prevalence of development-sensitive interventions, we used national-level data from 51 countries in sub-Saharan Africa from large-scale national surveys including Demographic and Health Surveys, Multiple Indicator Cluster Surveys, Malaria Indicator Surveys, and AIDS Indicator Surveys. We also used data repositories including the WHO’s Vitamin and Mineral Nutrition Information System, the Iodine Global Network, and the Food Fortification Initiative. Country reports from UNAIDS, UNICEF, World Bank, and the WHO provided supplementary data. For interventions without data on national coverage, we have used estimates from the literature to determine the expected reductions in the level of the risk factor(s) if the interventions were widely available. Indicator definitions and sources can be found in Table 1. Only estimates from 2000 or later were included.
Table 1.
Risk indicators, definitions, and sources, by domain
| Risk | Risk Indicator | Definition | Sources |
|---|---|---|---|
| Nutrition domain | |||
|
Intrauterine growth restriction |
Low birthweight | Percentage of babies with birth weights < 2,500 g among children born in the five years prior to the survey and who had recorded birthweights. |
DHS, MICS, UNICEF |
| Stunting | Stunting among children under five years |
Percentage of children under five years with height-for-age less than ≤ −2 SD from median height-for-age of WHO international reference population. |
DHS, MICS, UNICEF |
| Iodine deficiency | Population-level iodine deficiency |
Percentage of the population with urinary iodine excretion (UIE) less than 100 µg/L. |
IGN |
| Household coverage of iodized salt |
Percentage of household with iodized salt among households with salt and where salt was tested. |
DHS, IGN, MICS, UNICEF |
|
|
Iron-deficiency anemia |
Children aged 6–59 months with any anemia |
Percentage of children aged 6–59 months with hemoglobin less than 11g/dL, adjusted for altitude using CDC standards. |
DHS, MICS, MIS, VMNIS |
| Children aged 6–59 months with severe anemia |
Percentage of children aged 6–59 months with hemoglobin less than 7g/dL, adjusted for altitude using CDC standards. |
DHS, MICS, MIS, and VMNIS |
|
| Fortification legislation |
Mandatory: Legislation has the effect of mandating fortification of one or more type of wheat flour, maize flour, and/or rice with at least iron. Planning: There is written evidence that the government is acting to prepare, draft, and/or move legislation for mandatory fortification. Voluntary: At least 50 % of the industrially-milled wheat or maize flour or rice produced in the country is being fortified through voluntary efforts. None: None of the above. |
FFI | |
|
Exclusive breastfeeding |
Exclusive breastfeeding | Percentage of children under two years who received only breastmilk (including breastmilk that has been expressed or from a wet nurse) and nothing else, except for ORS, medicines, and vitamins and minerals before 6 months of age. |
DHS, MICS, UNICEF |
| Environment domain | |||
| Malaria | Children aged 6–59 months testing positive for malaria |
Percentage of children aged 6–59 months with a positive rapid malaria diagnostic test. |
DHS, MIS |
| Indoor residual spraying (IRS) |
Percentage of households that had rooms sprayed with insecticide of residual action (IRS) during the 12 months preceding the survey. |
DHS, MIS | |
| Children under five years sleeping under a treated bed net (ITN) |
Percentage of children under five years who slept under an insecticide-treated bed net the night before the survey. An insecticide-treated net (ITN) is 1) a factory-treated net that does not require any further treatment, 2) a pretreated net obtained within the past 12 months, or 3) a net that has been soaked with insecticide within the past 12 months. |
DHS, MICS, MIS | |
| Children under five years with fever receiving anti- malarial drugs |
Percentage of children under five years who were ill with fever in the two weeks prior to the survey and received any appropriate (locally defined) antimalarial drugs. |
DHS, MICS, MIS, UNICEF |
|
| HIV | Prevalence of HIV among adults aged 15–49 years |
The estimated number of adults aged 15–49 years with HIV infection, whether or not they have developed symptoms of AIDS, expressed as per cent of total population in that age group. |
AIS, DHS, UNAIDS, WHO |
| Prevalence of HIV among pregnant women |
(WHO) - Percentage of blood samples taken from pregnant women aged 15–24 years who test positive for HIV during ‘unlinked anonymous sentinel surveillance’ at selected antenatal clinics. |
AIS, DHS, WHO | |
|
(DHS/AIS) - Percentage of blood samples taken from women aged 15–49 years who test positive for HIV during survey and who self-report pregnancy expressed as per cent of total female population in that age group. |
|||
| Pregnant women with HIV receiving ARVs to prevent MTCT |
Estimated percentage of pregnant women with HIV who received the most effective antiretroviral regimens as recommended by WHO (i.e. excluding single-dose nevirapine) during the past 12 months to reduce mother-to-child transmission. |
WHO | |
| Mother-child interaction domain | |||
| Maternal depression | Post-partum depression | Maternal post-partum depression as defined in each individual study | Various. See table for studies |
|
Inadequate cognitive stimulation |
Learning materials at home (Books) |
Percentage of households with children under five years with three or more children’s books |
MICS, UNICEF |
| Learning materials at home (Playthings) |
Percentage of households with children under five years with two or more types of playthings. |
MICS, UNICEF | |
| Children left in inadequate care |
Percentage of children under five years left alone or left in the care of other children under the age of 10 years for more than one hour at least once during the week prior to the survey. |
MICS, UNICEF | |
| Attendance in early childhood education |
Percentage of children under five years attending early childhood education. | MICS, UNICEF | |
| Maternal education | No schooling | Percentage of surveyed women aged 15–49 years with no school attendance or completion. |
AIS/MIS, DHS, EMIP, MICS |
| Secondary school complete | Percentage of surveyed women aged 15–49 years with secondary school as the highest level of schooling completed. |
DHS, MICS, MIS | |
| Marriage by age 15 | Percentage of women aged 15–49 years who were married by age 15 years. | UNICEF | |
Note: AIS = AIDS Indicator Survey; DHS = Demographic Health Survey; EMIP = Education Measurement Information and Practice; FFI = Food Fortification Initiative; IGN = Iodine Global Network; MICS = Multiple Indicator Cluster Survey; MIS = Malaria Indicator Survey; VMNIS = Vitamin and Mineral Nutrition Information System.
For each risk factor/intervention, we ranked countries by prevalence, divided them into quintiles, and assigned point values based on quintile. For risk factors, we assigned 1 point if in the highest quintile and 5 points if in the lowest quintile. For interventions, we assigned 5 points if in the highest quintile and 1 point if in the lowest quintile. For iron fortification legislation, we assigned points as follows: 1 for ‘no legislation’, 2 for ‘planning legislation’, 3 for ‘voluntary fortification’, and 4 for ‘mandatory fortification’. Countries for which data were not available were assigned the mean score of available indicators within the same domain. We then summed risk factor/intervention scores within the nutrition and environment domains, excluding countries who were missing >75% of indicators within a domain. Because all countries in sub-Saharan Africa have converted to unleaded fuel, lead exposure was not included in the calculation of environment domain scores. As sixty-seven percent of countries were missing more than half of the mother-child interaction indicators, we did not calculate a domain score and instead discuss country performance qualitatively by risk factor/intervention.
RESULTS
Nutrition
IUGR/Low Birthweight
Nutrition domain indicators are presented in Table 2. Of the 45 countries with data, prevalence of low birthweight (< 2,500 g) ranged from 5.6% in Kenya to 34.7% in Mauritania. Eighteen countries had low birthweight prevalence < 10%. Among the countries with high burden of low birthweight, Mali, Senegal, Comoros, Chad, had low birthweight prevalence of 15–20%. We identified no data on national-level coverage of interventions to specifically address birthweight.
Table 2.
Nutrition domain – prevalence of low birthweight, stunting, iodine deficiency, iron-deficiency anemia, and exclusive breastfeeding indicators, by country
| Country | Low birthweight, (%) |
Stunting among children < 5 years, (%) |
Population with UIE < 100 µg/L, (%) |
Households with iodized salt, (%) |
Children 6– 59 months with any anemia (Hb < 11 g/dL), (%) |
Children 6–59 months with severe anemia (Hb < 7 g/dL), (%) |
Iron fortification legislation |
Grain | Exclusive breastfeeding, (%) |
|---|---|---|---|---|---|---|---|---|---|
| Angola | 12 (UNICEF 2012) |
29 (UNICEF 2012) |
92.0 (IGN 2012) |
44.7 (IGN 2012) |
57.2 (MIS 2006/07) |
1.3 (MIS 2006/07) |
None | - | 11.0 (UNICEF 2012) |
| Benin | 12.7 (DHS 2011/12) |
44.6 (UNICEF 2012) |
12.5 (IGN 2012) |
92.2 (DHS 2011/12) |
58.3 (DHS 2011/12) |
3.0 (DHS 2011/12) |
Mandatory | Wheat | 32.5 (DHS 2011/12) |
| Botswana | 13 (UNICEF 2012) |
31.4 (UNICEF 2012) |
15.0 (IGN 2012) |
65.2 (IGN 2012) |
- | - | Planning | Wheat | 20.0 (UNICEF 2012) |
| Burkina Faso |
13.9 (DHS 2010) |
20.3 (DHS 2010) |
47.1 (IGN 2012) |
95.9 (MICS 2010) |
87.9 (MICS 2010) |
11.3 (MICS 2010) |
Mandatory | Wheat | 38.2 (DHS 2010) |
| Burundi | 10.7 (DHS 2010) |
57.7 (DHS 2010) |
60.5 (IGN 2012) |
96.1 (DHS 2010) |
44.5 (DHS 2010) |
1.0 (DHS 2010) |
Planning | Rice | 69.3 (DHS 2010) |
| Cape Verde | 6 (UNICEF 2012) |
- | 43.2 (IGN 2012) |
74.8 (IGN 2012) |
52.1 (DHS 2005) |
1.7 (DHS 2005) |
Mandatory | Wheat | 28 (DHS 2005) |
| Cameroon | 7.6 (DHS 2010) |
30.0 (DHS 2010) |
29.6 (IGN 2012) |
90.9 (MICS 2011) |
60.3 (MICS 2011) |
1.7 (MICS 2011) |
Mandatory | Wheat | 20.0 (DHS 2010) |
| Central African Republic |
13.7 (UNICEF 2012) |
40.7 (UNICEF 2012) |
87.0 (IGN 2012) |
64.5 (IGN 2012) |
- | - | None | - | 34.3 (UNICEF 2012) |
| Chad | 19.9 (UNICEF 2012) |
40.9 (DHS 2004) |
29.4 (IGN 2012) |
56* (DHS 2004) |
- | - | None | - | 3.4 (UNICEF 2012) |
| Comoros | 16.2 (MICS 2012) |
30.1 (MICS 2012) |
- | 91.0 (MICS 2012) |
- | - | None | - | 12.0 (MICS 2012) |
| Congo (Brazzaville) |
10.0 (DHS 2011/12) |
24.4 (DHS 2011/12) |
- | 99.5 (DHS 2011/12) |
66.7 (DHS 2011/12) |
1.0 (DHS 2011/12) |
Mandatory | Wheat | 21.0 (DHS 2011/12) |
| Congo (DR) | 7.1 (DHS 2013/14) |
42.7 (DHS 2013/14) |
1.5 (IGN 2012) |
92.4 (DHS 2013/14) |
59.8 (DHS 2013/14) |
3.1 (DHS 2013/14) |
Voluntary | Wheat | 48.0 (DHS 2013/14) |
| Côte d’Ivoire | 14.2 (DHS 2011/12) |
29.8 (DHS 2011/12) |
27.6 (IGN 2012) |
91.6 (DHS 2011/12) |
74.8 (DHS 2011/12) |
3.3 (DHS 2011/12) |
Mandatory | Wheat | 12.1 (DHS 2011/12) |
| Djibouti | 10 (UNICEF 2012) |
30.8 (UNICEF 2012) |
- | 0.4 (IGN 2012) |
- | - | Mandatory | Wheat | 1.0 (UNICEF 2012) |
| Equatorial Guinea |
11.7 (DHS 2011) |
26.2 (DHS 2011) |
- | 33.3 (IGN 2012) |
67.1 (DHS 2011) |
4.0 (DHS 2011) |
None | - | 7.0 (DHS 2011) |
| Eritrea | 14 (UNICEF 2012) |
37.6 (DHS 2002) |
25.3 (IGN 2012) |
68* (DHS 2002) |
- | - | None | - | 52.0 (DHS 2002) |
| Ethiopia | 10.8 (DHS 2011) |
44.4 (DHS 2011) |
83.0 (IGN 2012) |
15.4 (DHS 2011) |
44.2 (DHS 2011) |
2.5 (DHS 2011) |
Planning | Wheat | 52.0 (DHS 2011) |
| Gabon | 14.0 (DHS 2012) |
16.5 (DHS 2012) |
30.5 (IGN 2012) |
97.6 (DHS 2012) |
60.2 (DHS 2012) |
2.1 (DHS 2012) |
None | - | 20.0 (DHS 2011) |
| The Gambia | 10.2 (UNICEF 2012) |
24.5 (DHS 2013) |
87.0 (IGN 2012) |
22 (IGN 2012) |
72.8 (DHS 2013) |
1.8 (DHS 2013) |
Voluntary | Wheat | 46.8 (DHS 2013) |
| Ghana | 10.7 (MICS 2011) |
22.7 (MICS 2011) |
71.0 (IGN 2012) |
38.2* (MICS 2011) |
57.0 (MICS 2011) |
2.6 (MICS 2011) |
Mandatory | Wheat | 45.7 (MICS 2011) |
| Guinea | 8.6 (DHS 2012) |
31.2 (DHS 2012) |
32.4 (IGN 2012) |
64.4 (DHS 2012) |
76.6 (DHS 2012) |
7.6 (DHS 2012) |
Mandatory | Wheat | 20.5 (DHS 2012) |
| Guinea- Bissau |
11 (UNICEF 2012) |
32.2 (UNICEF 2012) |
- | 11.7 (IGN 2012) |
- | - | None | - | 38.3 (UNICEF 2012) |
| Kenya | 5.6 (DHS 2008/09) |
35.3 (DHS 2008/09) |
36.8 (IGN 2012) |
97.6* (DHS 2008/09) |
26.5 (MIS 2010) |
- | Mandatory | Wheat, maize |
31.9 (DHS 2008/09) |
| Lesotho | 9.3 (DHS 2009) |
39.2 (DHS 2009) |
21.5 (IGN 2012) |
84.4* (DHS 2009) |
47.1 (2009 DHS) |
1.3 (DHS 2009) |
Planning | Wheat | 53.5 (DHS 2009) |
| Liberia | 9.7 (DHS 2013) |
31.6 (DHS 2013) |
12.6 (IGN 2012) |
98.5 (DHS 2013) |
- | - | Mandatory | Wheat | 55.2 (DHS 2013) |
| Madagascar | 12.7 (DHS 2008/09) |
50.1 (DHS 2008/09) |
- | 52.6* (DHS 2008/09) |
51.0 (MIS 2013) |
1.4 (MIS 2013) |
None | - | 50.7 (DHS 2008/09) |
| Malawi | 12.3 (DHS 2010) |
47.1 (DHS 2010) |
35.0 (IGN 2012) |
97.2 (DHS 2010) |
62.5 (DHS 2010) |
3.1 (DHS 2010) |
Planning | Wheat, maize |
71.4 (DHS 2010) |
| Mali | 15.5 (DHS 2012/13) |
38.3 (DHS 2012/13) |
68.3 (IGN 2012) |
94.7 (DHS 2011/12) |
81.7 (DHS 2012/13) |
9.3 (DHS 2012/13) |
Mandatory | Wheat | 32.9 (DHS 2012/13) |
| Mauritania | 34.7 (UNICEF 2012) |
34.5 (DHS 2000/01) |
17.5 (IGN 2012) |
22.6 (IGN 2012) |
- | - | Mandatory | Wheat | - |
| Mauritius | 14 (UNICEF 2012) |
- | 4.4 (IGN 2012) |
0 (IGN 2012) |
- | - | None | - | 21.0 (UNICEF 2012) |
| Mozambique | 14.1 (DHS 2011) |
42.6 (DHS 2011) |
68.1 (IGN 2012) |
44.8 (DHS 2011) |
68.7 (DHS 2011) |
4.0 (DHS 2011) |
Planning | Wheat | 42.8 (DHS 2011) |
| Namibia | 13.0 (DHS 2013) |
23.8 (DHS 2013) |
28.7 (IGN 2012) |
76.2 (DHS 2013) |
47.5 (DHS 2013) |
0.8 (DHS 2013) |
Voluntary | Wheat, maize |
48.5 (DHS 2013) |
| Niger | 11.8 (DHS 2012) |
43.9 (DHS 2012) |
4.4 (IGN 2012) |
58.5 (DHS 2012) |
73.4 (DHS 2012) |
2.9 (DHS 2012) |
Mandatory | Wheat | 28.2 (DHS 2012) |
| Nigeria | 8.1 (DHS 2013) |
36.8 (DHS 2013) |
40.4 (IGN 2012) |
51.5 (IGN 2012) |
- | - | Mandatory | Wheat, maize |
17.4 (DHS 2013) |
| Réunion | - | - | - | - | - | - | - | - | - |
| Rwanda | 6.2 (DHS 2010) |
44.2 (DHS 2010) |
0.0 (IGN 2012) |
99.3 (DHS 2010) |
38.1 (DHS 2010) |
0.5 (DHS 2010) |
Mandatory | Wheat, maize |
84.9 (DHS 2010) |
| Sao Tome and Principe |
8.5 (DHS 2008/09) |
29.3 (DHS 2008/09) |
- | 85.6* (DHS 2008/09) |
62.2 (DHS 2008/09) |
1.3 (DHS 2008/09) |
None | - | 51.4 (DHS 2008/09) |
| Senegal | 15.9 (MICS 2010/11) |
18.7 (DHS 2012/13) |
47.8 (IGN 2012) |
47.0* (MICS 2010/11) |
71.2 (DHS 2012/13) |
4.0 (DHS 2012/13) |
Mandatory | Wheat | 37.5 (DHS 2012/13) |
| Seychelles | - | - | - | - | - | - | None | - | - |
| Sierra Leone | 7.1 (DHS 2013) |
37.9 (DHS 2013) |
- | 80.2 (DHS 2013) |
79.9 (DHS 2013) |
6.0 (DHS 2013) |
Mandatory | Wheat | 32.0 (DHS 2013) |
| Somalia | - | 42 (UNICEF 2012) |
10.0 (IGN 2012) |
1.2 (IGN 2012) |
- | - | None | - | 9 (UNICEF 2012) |
| South Africa | 8.0 (DHS 2003) |
27.4 (DHS 2003) |
19.2 (IGN 2012) |
- | - | - | Mandatory | Wheat, maize |
8.3 (DHS 2003) |
| South Sudan | - | - | - | - | - | - | - | - | - |
| Sudan | - | - | 70.8 (IGN 2012) |
11.0 (IGN 2007) |
- | - | None | - | - |
| Swaziland | 7.8 (DHS 2006/07) |
28.9 (DHS 2006/07) |
41.4 (IGN 2012) |
79.9* (DHS 2006/07) |
41.8 (DHS 2006/07) |
0.8 (DHS 2006/07) |
None | - | 32.3 (DHS 2006/07) |
| Tanzania | 6.9 (DHS 2010) |
42.0 (DHS 2010) |
25.0 (IGN 2012) |
58.5* (DHS 2010) |
58.6 (DHS 2010) |
1.9 (DHS 2010) |
Mandatory | Wheat, maize |
49.8 (DHS 2010) |
| Togo | 11.1 (UNICEF 2012) |
27.4 (DHS 2013/14) |
6.2 (IGN 2012) |
31.5 (IGN 2012) |
70.0 (DHS 2013/14) |
2.4 (DHS 2013/14) |
Mandatory | Wheat | 57.4 (DHS 2013/14) |
| Uganda | 10.2 (DHS 2011) |
33.4 (DHS 2011) |
3.9 (IGN 2012) |
99.0 (DHS 2011) |
49.3 (DHS 2011) |
1.5 (DHS 2011) |
Mandatory | Wheat, maize |
63.2 (DHS 2011) |
| Western Sahara |
- | - | - | - | - | - | - | - | - |
| Zambia | 9.3 (DHS 2007) |
45.4 (DHS 2007) |
14.0 (IGN 2012) |
77.4 (IGN 2012) |
52.9 (VMNIS 2003) |
- | None | - | 60.9 (DHS 2007) |
| Zimbabwe | 9.5 (DHS 2010/11) |
32.0 (DHS 2010/11) |
14.8 (IGN 2012) |
94.0 (DHS 2010/11) |
56.3 (DHS 2010/11) |
0.9 (DHS 2010/11) |
None | - | 31.4 (DHS 2010/11) |
Note: *Salt iodized above minimum recommendation (>15ppm)
Stunting
Of 44 countries with data on stunting (HAZ ≤ −2 SD) among children under five years, prevalence ranged from 16.5% in Gabon to 57.7% in Burundi. Only Senegal and Gabon had stunting prevalence < 20%.(39) We identified no data on national-level coverage of interventions to specifically address stunting.
Exclusive Breastfeeding
Of 45 countries with data on exclusive breastfeeding among children under six months, prevalence ranged from 1% in Djibouti to 84.9% in Rwanda. Only 12 countries had exclusive breastfeeding prevalence ≥50%. We identified no data on national-level coverage of interventions to specifically address exclusive breastfeeding.
Iodine Deficiency
Among the 39 countries with data, the prevalence of iodine deficiency (urinary iodine excretion [UIE] < 100 µ/l) ranged from 0% in Rwanda to 92% in Angola. Of the 40 countries with data on median population urinary iodine excretion, eight countries were considered iodine insufficient (data not presented). Of the 46 countries with data, the proportion of households with iodized salt ranged from 0.4% in Djibouti to > 99% in DR Congo, Uganda, and Rwanda. In sixteen countries, ≥ 90% of households had iodized salt. In fourteen countries, ≤ 50% of households had iodized salt.
Iron-deficiency Anemia
Of the 33 countries with data on anemia (hemoglobin [Hb] <11 g/dL) among children aged 6–59 months, prevalence ranged from 26.5% in Kenya to 87.9% in Burkina Faso. Twenty-five countries had anemia prevalence ≥50%. The highest levels of anemia were clustered in West Africa. Even among the countries with the lowest burden of anemia, none had prevalence <25%. Of the 31 countries with data on severe anemia (Hb <7 g/dL) among children aged 6–59 months, prevalence ranged from 0.5% in Rwanda to 11.3% in Burkina Faso.
Twenty-one countries had mandatory fortification of grains with at least iron. Three countries had voluntary iron fortification of grains, and six countries were planning fortification. Most countries fortified wheat; however, eight countries fortified both wheat and maize. Burundi was planning rice fortification. Sixteen countries had no fortification legislation.
Nutrition Domain
The nutrition domain score is presented in Fig 1. Réunion, South Sudan, Western Sahara, and Seychelles were missing more than 75% of the nutrition domain indicators and were excluded from the domain score. Of 39 possible points in the domain, scores ranged from eight in Sudan to 35 in Rwanda.
Figure 1.
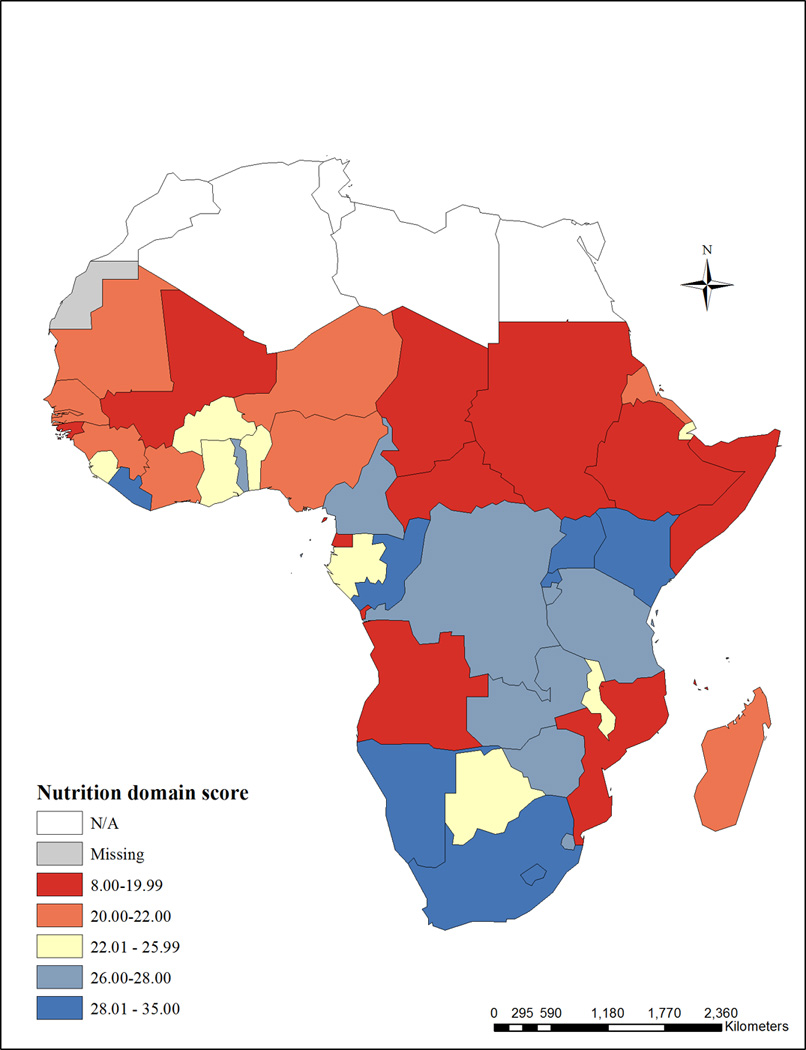
Nutrition domain score - The nutrition domain score includes the following indicators: low birthweight, stunting among children under five years, population-level iodine deficiency, household coverage of iodized salt, children aged 6–59 months with any anemia, children aged 6–59 months with severe anemia, legislation on iron fortification of grains, and exclusive breastfeeding. Réunion, South Sudan, Western Sahara, and Seychelles were missing more than 75% of the nutrition domain indicators and were excluded from the score.
Environment
Malaria
Environment domain indicators are presented in Table 3. Of 17 countries with data on malaria prevalence among children aged 6–59 months, prevalence ranged from 2.3% in The Gambia to 65.9% in Burkina Faso. In Kenya, 12.3% of children aged 3–59 months tested positive for malaria.(40) Of 38 countries with data on children under five years sleeping under an ITN, prevalence ranged from 0.6% in Swaziland to 74.1% in Rwanda. In seven countries, < 50% of children under five years slept under an ITN. Of 28 countries with data on household IRS, prevalence ranged from 0.3% in Burundi to 39.2% in Equatorial Guinea. Of 43 countries with data on children under five years with fever who received anti-malarial drugs, prevalence ranged from 0.6% in Swaziland to 65% in Sudan.
Table 3.
Environment domain – prevalence of indicators for malaria and HIV-affected children, by country
| Country | Children 6–59 months testing positive for malaria, (%) |
Households with indoor residual spraying, (%) |
Children < 5 years ill with fever receiving antimalarial drugs, (%) |
Children < 5 years sleeping under an ITN, (%) |
HIV prevalence among adults aged 15–49 years, (%) |
HIV prevalence among pregnant women, (%) |
Pregnant women with HIV receiving ARVs to prevent MTCT, (%) |
|---|---|---|---|---|---|---|---|
| Angola | 10.1 (MIS 2011) |
7.0 (MIS 2011) |
28.3 (MIS 2011) |
25.9 (MIS 2011) |
2.3 (UNAIDS 2012) |
- | 16 (WHO 2011) |
| Benin | 28.4 (DHS 2011/12) |
6.0 (DHS 2011/12) |
38.4 (DHS 2011/12) |
69.7 (DHS 2011/12) |
2.2 (UNAIDS 2012) |
0.9 (DHS 2011/12) |
30 (WHO 2011) |
| Botswana | - | - | - | - | 21.9 (WHO 2013) |
- | 94 (WHO 2011) |
| Burkina Faso | 65.9 (DHS 2010) |
0.9 (DHS 2010) |
31.5 (DHS 2010) |
47.4 (DHS 2010) |
1.0 (UNAIDS 2012) |
0.83 (DHS 2010) |
46 (WHO 2011) |
| Burundi | - | 0.3 (DHS 2010) |
17.2 (DHS 2010) |
45.3* (DHS 2010) |
1.3 (UNAIDS 2012) |
2.0 (DHS 2010) |
52 (WHO 2011) |
| Cameroon | 30.0 (DHS 2010) |
2.3 (DHS 2010) |
23.1 (DHS 2010) |
21.0 (DHS 2010) |
4.5 (UNAIDS 2012) |
5.6 (DHS 2010) |
53 (WHO 2011) |
| Cape Verde | - | - | - | - | 0.2 (UNAIDS 2012) |
- | - |
| Central African Republic |
- | - | 31.8 (UNICEF 2010) |
36.4 (UNICEF 2012) |
4.9 (MICS 2010) |
4.5 (MICS 2010) |
48 (WHO 2011) |
| Chad | - | - | 35.7 (UNICEF 2010) |
9.8 (UNICEF 2012) |
2.5 (WHO 2013) |
- | 11 (WHO 2011) |
| Comoros | - | 4.3 (MICS 2012) |
26.7 (MICS 2012) |
41.4 (MICS 2012) |
2.1 (UNAIDS 2012) |
- | 0 (WHO 2011) |
| Congo (Brazzaville) |
- | - | 25.0 (DHS 2011/12) |
26.3* (DHS 2011/12) |
2.8 (UNAIDS 2012) |
3.7 (AIS 2009) |
6 (WHO 2011) |
| Congo (DR) | 30.8 (DHS 2013/14) |
- | 29.2 (DHS 2013/14) |
55.8 (DHS 2013/14) |
1.2 (DHS 2013/14) |
0.6 (DHS 2013/14) |
- |
| Côte d’Ivoire | 41.5 (DHS 2011/12) |
1.5 (DHS 2011/12) |
17.5 (DHS 2011/12) |
37.2 (DHS 2011/12) |
3.7 (DHS 2011/12) |
2.7 (DHS 2011/12) |
68 (WHO 2011) |
| Djibouti | - | - | 0.9 (UNICEF 2009) |
19.9 (UNICEF 2012) |
0.9 (WHO 2013) |
- | 14 (WHO 2011) |
| Equatorial Guinea |
47.8 (DHS 2011) |
39.2 (DHS 2011) |
33.2 (DHS 2011) |
23.0 (DHS 2011) |
6.2 (DHS 2011) |
2.4 (DHS 2011) |
- |
| Eritrea | - | - | 3.6 (DHS 2002) |
4.2 (DHS 2002) |
0.6 (WHO 2013) |
- | 0 (WHO 2011) |
| Ethiopia | - | - | 3.6 (DHS 2011) |
30.1 (UNICEF 2012) |
1.3 (UNAIDS 2012) |
0.8 (DHS 2011) |
24 (WHO 2011) |
| Gabon | - | 4.2 (DHS 2012) |
25.9 (DHS 2012) |
38.8 (DHS 2012) |
4.0 (UNAIDS 2012) |
5.2 (DHS 2012) |
48 (WHO 2011) |
| The Gambia | 2.3 (DHS 2013) |
30.4 (DHS 2013) |
6.7 (DHS 2013) |
47.2 (DHS 2013) |
1.2 (WHO 2013) |
- | - |
| Ghana | 47.5 (MICS 2011) |
- | 52.6 (MICS 2011) |
39.0 (MICS 2011) |
1.3 (WHO 2013) |
- | 75 (WHO 2011) |
| Guinea | 46.9 (DHS 2012) |
1.7 (DHS 2012) |
28.1 (DHS 2012) |
26.1 (DHS 2012) |
1.7 (UNAIDS 2012) |
1.7 (DHS 2012) |
40 (WHO 2011) |
| Guinea-Bissau | - | - | 51.2 (UNICEF 2010) |
35.5 (UNICEF 2012) |
3.7 (WHO 2013) |
- | 32 (WHO 2011) |
| Kenya | - | 10.8 (MIS 2010) |
35.1 (MIS 2010) |
42.2 (MIS 2010) |
6.1 (UNAIDS 2012) |
8.3 (DHS 2008/09) |
67 (WHO 2011) |
| Lesotho | - | - | - | - | 23.1 (UNAID 2012) |
17.9 (DHS 2009) |
62 (WHO 2011) |
| Liberia | 44.7 (MIS 2011) |
10.7 (DHS 2013) |
55.7 (DHS 2013) |
38.1 (DHS 2013) |
2.1 (DHS 2013) |
4.6 (DHS 2013) |
59 (WHO 2011) |
| Madagascar | 10.0 (MIS 2013) |
28.2 (MIS 2013) |
11.3 (MIS 2013) |
61.5* (MIS 2013) |
0.4 (WHO 2013) |
- | - |
| Malawi | 43.4 (MIS 2012) |
8.5 (MIS 2012) |
32.5 (MIS 2012) |
56.0 (MIS 2012) |
10.8 (UNAIDS 2012) |
8.8 (DHS 2010) |
53 (WHO 2011) |
| Mali | - | 6.2 (DHS 2012/13) |
22.5 (DHS 2012/13) |
69.0 (DHS 2012/13) |
1.1 (DHS 2012/13) |
- | - |
| Mauritania | - | - | 33.4 (EMIP 2003/04) |
2.1¥ (EMIP 2003/04) |
0.4 (UNAIDS 2012) |
- | - |
| Mauritius | - | - | - | - | 1.1 (WHO 2013) |
- | - |
| Mozambique | 38.3 (DHS 2011) |
18.5 (DHS 2011) |
29.9 (DHS 2011) |
35.7 (DHS 2011) |
10.8 (WHO 2013) |
- | 51 (WHO 2011) |
| Namibia | - | 15.5 (DHS 2013) |
8.4 (DHS 2013) |
5.6 (DHS 2013) |
14.3 (DHS 2013) |
12.8 (DHS 2013) |
85 (WHO 2011) |
| Niger | - | 0.5 (DHS 2012) |
19.2 (DHS 2012) |
20.1 (DHS 2012) |
0.5 (UNAIDS 2012) |
0.2 (DHS 2012) |
- |
| Nigeria | - | 1.7 (DHS 2013) |
32.7 (DHS 2013) |
16.6 (DHS 2013) |
3.2 (WHO 2013) |
- | 18 (WHO 2011) |
| Réunion | - | - | - | - | - | - | - |
| Rwanda | - | 10.3 (MIS 2013) |
12.0 (MIS 2013) |
74.1 (MIS 2013) |
2.9 (WHO 2013) |
- | 56 (WHO 2011) |
| Sao Tome and Principe |
- | - | 8.4 (DHS 2008/09) |
56.0 (DHS 2008/09) |
1.0 (UNAIDS 2012) |
1.5 (DHS 2008/09) |
- |
| Senegal | - | 11.6 (DHS 2012/13) |
6.2 (DHS 2012/13) |
45.8 (DHS 2012/13) |
0.5 (UNAIDS 2012) |
1.5 (MICS 2010/11) |
- |
| Seychelles | - | - | - | - | - | - | - |
| Sierra Leone | 46.2 (MIS 2013) |
5.8 (MIS 2013) |
44.1 (MIS 2013) |
45.0 (MIS 2013) |
1.5 (DHS 2013) |
1.1 (DHS 2013) |
74 (WHO 2011) |
| Somalia | - | - | 7.9 (UNICEF 2012) |
11.4 (UNICEF 2012) |
0.5 (WHO 2013) |
- | - |
| South Africa | - | - | - | - | 19.1 (WHO 2013) |
- | 95 (WHO 2011) |
| South Sudan | - | - | 51.2 (UNICEF 2010) |
- | 2.2 (WHO 2013) |
- | 6 (WHO 2011) |
| Sudan | - | - | 65.0 (UNICEF 2010) |
0.2 (WHO 2013) |
- | 3 (WHO 2011) |
|
| Swaziland | - | 11.8 (DHS 2006/07) |
0.6 (DHS 2006/07) |
0.6 (DHS 2006/07) |
27.4 (WHO 2013) |
37.7 (DHS 2006/07) |
95 (WHO 2011) |
| Tanzania | 9.2 (AIS/MIS 2011/12) |
13.9 (AIS/MIS 2011/12) |
53.7 (AIS/MIS 2011/12) |
72.0 (AIS/MIS 2011/12) |
5.1 (UNAIDS 2012) |
3.2 (AIS/MIS 2011/12) |
74 (WHO 2011) |
| Togo | - | - | 19.9 (DHS 2013/14) |
42.9 (DHS 2013/14) |
2.3 (WHO 2013) |
- | 61 (WHO 2011) |
| Uganda | - | 7.2 (DHS 2011) |
64.5 (DHS 2011) |
42.8 (DHS 2011) |
7.4 (WHO 2013) |
- | 50 (WHO 2011) |
| Western Sahara | - | - | - | - | - | - | - |
| Zambia | - | 15.6 (DHS 2007) |
38.4 (DHS 2007) |
28.5 (DHS 2007) |
12.7 (UNAIDS 2012) |
11.6 (DHS 2007) |
86 (WHO 2011) |
| Zimbabwe | - | 17.0 (DHS 2010/11) |
2.3 (DHS 2010/11) |
9.7 (DHS 2010/11) |
15.0 (WHO 2013) |
11.9 (DHS 2010/11) |
54 (WHO 2011) |
Note: * ITN with long acting insecticide;
ITN treated less than six months before the survey.
Lead Exposure
To our knowledge, there are no nationally representative estimates of blood lead levels in sub-Saharan Africa. Available studies are not representative of sub-Saharan Africa as a whole, but they provide some information about lead exposure in the sub-continent prior to the shift to unleaded fuel. One study from South Africa found that 15–30% of children in urban areas had blood lead levels >25 µg/dL.(41) A study of school children in Ghana found average blood lead levels of 28–32 µg/dL.(42) Blood lead levels >10 µg/dL are generally considered toxic.(43) Over the last 15 years, governments in Africa have implemented strategies to shift to alternate fuel additives such as ethanol or MTBE. As of April 2014, all countries in sub-Saharan Africa had shifted to unleaded fuel.(44)
HIV-affected Children
Of 48 countries with data, prevalence of HIV among adults aged 15–49 years ranged from 0.2% in Sudan and Cape Verde to 27.4% in Swaziland. Countries with the highest adult prevalence of HIV were clustered in southern Africa where nine countries had prevalence >10%. Among the 22 countries with data, the prevalence of HIV among pregnant women ranged from 0.2% in Niger to 37.7% in Swaziland. In Botswana, UNAIDS estimated that 10.2% of women seroconvert during pregnancy.(45) The proportion of pregnant women with HIV receiving ARVs ranged from 0.5% in Comoros and Eritrea to ≥95% in South Africa and Swaziland.
Environment Domain
The environment domain score category is presented in Fig 2. Cape Verde, Mauritius, Réunion, Seychelles, and Western Sahara were missing more than 75% of the environment domain indicators and were excluded from the domain score. Of 35 possible points in the environment domain, scores ranged from 14 in Eritrea, Lesotho, and Nigeria to 30 in Madagascar.
Figure 2.
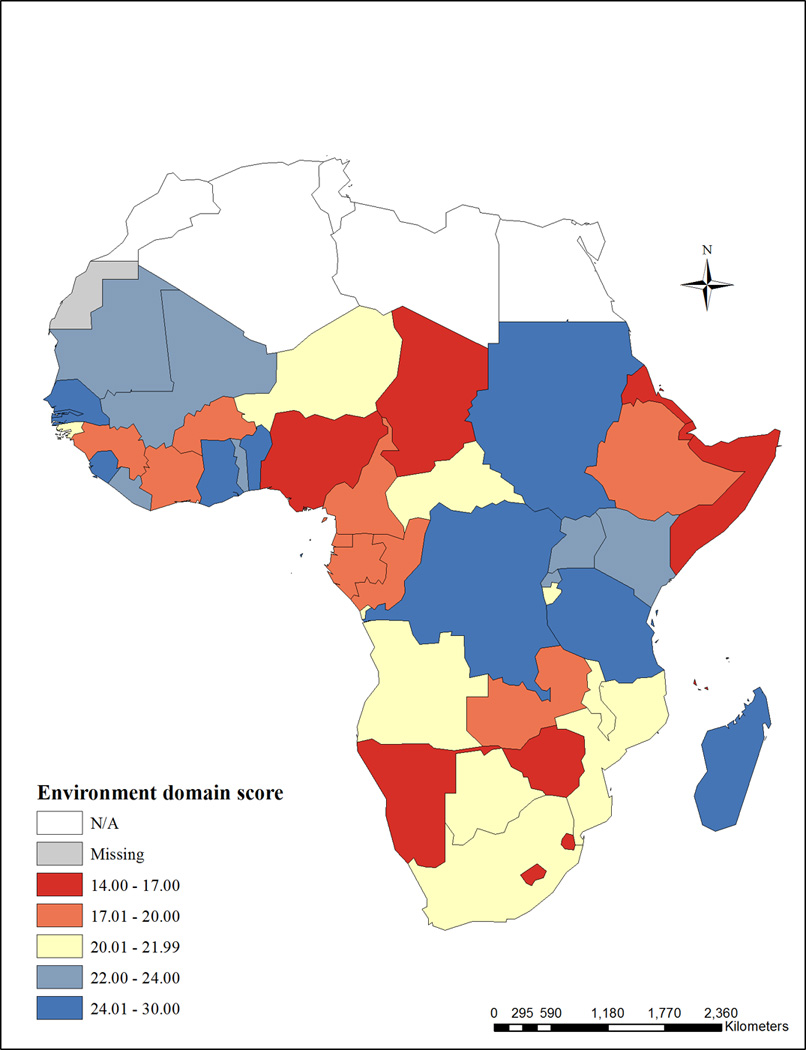
Environment domain score - The environment domain score includes the following indicators: children aged 6–59 months testing positive for malaria, household indoor residual spraying, children under five years sleeping under a treated bed net, children under five years ill with fever receiving anti-malarial drugs, prevalence of HIV among adults aged 15–49 years, prevalence of HIV among pregnant women, pregnant women with HIV receiving ARVs to prevent MTCT. Cape Verde, Mauritius, Réunion, Seychelles, and Western Sahara were missing more than 75% of the environment domain indicators and were excluded from the domain score.
Maternal-Child Interaction
Maternal Depression
Maternal depression indicators are presented in Table 4. To our knowledge, no nationally representative estimates of PPD are available for any sub-Saharan African countries; however, a national survey in Namibia found that 12.7% of women aged 15–49 years reported having general depression.(46) Studies of non-nationally representative samples provide some evidence of the PPD burden. A systematic review of maternal wellbeing in Africa found 11.3% prevalence of depression during pregnancy and 18.3% prevalence in the postpartum period.(47) Studies from Nigeria found PPD prevalence ranging from 4–30%.(48–51) In South Africa, studies found a PPD prevalence of 8–37%.(52,53) Studies in Ethiopia, the Gambia, and Uganda reported PPD prevalence ranging from 3–17%.(54–56) With limited health resources in many sub-Saharan African countries, psychological support and treatment for pregnant women and new mothers with depression is likely to be rare; however, we identified no data on national-level coverage of interventions to address maternal depression.
Table 4.
Mother-child interaction domain – prevalence of maternal depression, by country
| Country | Postpartum depression, (%) |
|---|---|
| Ethiopia |
Median 5 months postpartum 12% (CPRS) 17% (EPDS ≥5) (Hanlon et al. 2008) |
| The Gambia | <6 months postpartum 6.9% (PSE ICD-10) |
|
6–18 months postpartum 3.2% (PSE ICD-10) (Coleman et al. 2006) |
|
| Nigeria |
4–6 weeks postpartum 23.0 (EPDS ≥12) 17.5 (ICD-10) (Owoeye et al. 2006) |
|
6 weeks postpartum 14.6 (SCID-NP ≥9) (Adewuya et al. 2005) |
|
|
18.6 (EPDS ≥9) (Abiodun 2006) |
|
|
12.0 (difficult delivery) (Zung’s SRDS ≥45) 9.6 (unassisted vaginal delivery) (Zung’s SRDS ≥45) (Fatoye et al. 2006) |
|
|
6–8 weeks postpartum 29.8 (caesaran section) (BDI ≥10) 4.2 (normal delivery) (BDI ≥10) (Ukpong and Owolabi 2006) |
|
| South Africa |
6 weeks postpartum 36.9 (EPDS ≥12) 7.8 (DSM IV) (Lawrie et al. 1998) |
|
8 weeks postpartum 34.7 (DSM IV) (Cooper et al. 1999) 34.7 (SCID DSM-IV) (Tomlinson et al. 2005) |
|
| Uganda |
6–15 weeks postpartum 10.0 (SPI ICD-8) (Cox 1983) |
BDI = Beck’s Depression Inventory; CPRS = Comprehensive Psychopathological Rating Scale; EPDS = Edinburgh Postnatal Depression Scale; PSE = Present State Examination; SCID = Structured Clinical Interview for DSM-III-R; SPI = Standardized Psychiatric Interview; SRDS = Self Rating Depression Scale.
Inadequate Cognitive Stimulation
Indicators for inadequate cognitive stimulation are presented in Table 5. Among the 12 countries with data on households with children under five years with three or more children’s books, prevalence ranged from 0.4% in Mali to 14.7% in Djibouti. In four countries, < 1% of households had three or more children’s books. Of 13 countries with data, the proportion of households with two or more playthings ranged from 23.7% in Djibouti to 68.6% in Swaziland. Among the 12 countries with data on children left in inadequate care, prevalence ranged from 11.8% in Djibouti to 60.7% in CAR. Of 20 countries with data, the prevalence of children under five years attending early childhood education ranged from 2.2% in Burkina Faso to 68.2% in Ghana. Prevalence of attendance varied greatly by household wealth with children from the richest 20% of households having substantially higher attendance relative to children from the poorest 20% of households (data not presented).
Table 5.
Mother-child interaction domain – prevalence of cognitive stimulation and maternal education indicators, by country
| Country | Attendance in early childhood education, (%) |
Households with 3+ children’s books, (%) |
Households with 2+ playthings, (%) |
Children left in inadequate care, (%) |
No Schooling, (%) | Completed secondary school, (%) |
Marriage by age 15 (%) |
|---|---|---|---|---|---|---|---|
| Angola | - | - | - | - | 24.6 (MIS 2011) |
- | - |
| Benin | - | - | - | - | 59.5 (DHS 2011/12) |
2.3 (DHS 2011/12) |
7.9 (UNICEF 2012) |
| Botswana | 17.8 (UNICEF 2012) |
- | - | - | - | - | - |
| Burkina Faso | 2.2 (UNICEF 2012) |
- | - | - | 73.9 (MICS 2010) |
0.5 (MICS 2010) |
10.2 (UNICEF 2012) |
| Burundi | 4.7 (UNICEF 2012) |
- | - | - | 44.8 (DHS 2010) |
- | 2.5 (UNICEF 2012) |
| Cameroon | - | - | - | - | 20.0 (MICS 2011) |
2.0 (MICS 2011) |
13.4 (UNICEF 2012) |
| Cape Verde | - | - | - | - | 5.6 | - | 2.8 (UNICEF 2012) |
| Central African Republic |
5.0 (UNICEF 2012) |
0.7 (UNICEF 2012) |
48.5 (UNICEF 2012) |
60.7 (UNICEF 2012) |
- | - | 29.1 (UNICEF 2012) |
| Chad | 4.7 (UNICEF 2012) |
0.5 (UNICEF 2012) |
43.1 (UNICEF 2012) |
- | 74.8 (DHS 2004) |
3.7 (DHS 2004) |
29.0 (UNICEF 2012) |
| Comoros | - | - | - | - | 31.0 (MICS 2012) |
6.2 (MICS 2012) |
- |
| Congo (Brazzaville) |
- | - | - | - | 5.8 (DHS 2011/12) |
4.9 (DHS 2011/12) |
6.7 (UNICEF 2012) |
| Congo (DR) | 4.9 (UNICEF 2012) |
0.6 (UNICEF 2012) |
29 (UNICEF 2012) |
- | 15.4 (DHS 2013/14) |
8.5 (DHS 2013/14) |
9.3 (UNICEF 2012) |
| Côte d’Ivoire | 4.5 (UNICEF 2012) |
4.8 (UNICEF 2012) |
38.7 (UNICEF 2012) |
58.8 (UNICEF 2012) |
53.2 (DHS 2011/12) |
2.8 (DHS 2011/12) |
9.8 (UNICEF 2012) |
| Djibouti | 13.5 (UNICEF 2012) |
14.7 (UNICEF 2012) |
23.7 (UNICEF 2012) |
11.8 (UNICEF 2012) |
- | - | 1.8 (UNICEF 2012) |
| Equatorial Guinea | - | - | - | - | 7.8 (DHS 2011) |
6.4 (DHS 2011) |
- |
| Eritrea | - | - | - | - | 50.1 (DHS 2002) |
6.4 (DHS 2002) |
19.6 (UNICEF 2012) |
| Ethiopia | - | - | - | - | 50.8 (DHS 2011) |
0.9 (DHS 2011) |
16.3 (UNICEF 2012) |
| Gabon | - | - | - | - | 4.4 (DHS 2012) |
3.2 (DHS 2012) |
5.6 (UNICEF 2012) |
| The Gambia | 18.1 (UNICEF 2012) |
1.2 (UNICEF 2012) |
42 (UNICEF 2012) |
20.6 (UNICEF 2012) |
46.5 (DHS 2013) |
- | 7.3 (UNICEF 2012) |
| Ghana | 68.2 (MICS 2011) |
6.2 (MICS 2011) |
41.1 (MICS 2011) |
20.7 (MICS 2011) |
21.1 (DHS 2008) |
10.1 (DHS 2008) |
5.0 (UNICEF 2012) |
| Guinea | - | - | - | - | 67.0 (DHS 2012) |
1.5 (DHS 2012) |
19.8 (UNICEF 2012) |
| Guinea-Bissau | 9.9 (UNICEF 2012) |
- | - | - | - | - | 6.5 (UNICEF 2012) |
| Kenya | - | - | - | - | 15.0 (MIS 2010) |
13.4 (MIS 2010) |
6.2 (UNICEF 2012) |
| Lesotho | - | - | - | - | 1.2 (DHS 2009) |
8.0 (DHS 2009) |
2.3 (UNICEF 2012) |
| Liberia | - | - | - | - | 33.2 (DHS 2013) |
6.0(DHS 2013) | 10.8 (UNICEF 2012) |
| Madagascar | - | - | - | - | 20.7 (MIS 2013) |
2.3 (MIS 2013) |
14.4 (UNICEF 2012) |
| Malawi | - | - | - | - | 18.2 (MIS 2012) |
6.2 (MIS 2012) |
11.7 (UNICEF 2012) |
| Mali | 10.1 (UNICEF 2012) |
0.4 (UNICEF 2012) |
40 (UNICEF 2012) |
32.8 (UNICEF 2012) |
75.8 (DHS 2012/13) |
0.8 (DHS 2012/13) |
14.5 (UNICEF 2012) |
| Mauritania | 13.6 (UNICEF 2012) |
- | 40.1 (UNICEF 2012) |
26.1 (UNICEF 2012) |
26.9 (EMIP 2003/04) |
- | 14.2 (UNICEF 2012) |
| Mauritius | - | - | - | - | - | - | - |
| Mozambique | - | 2.8 (UNICEF 2012) |
- | 32.5 (UNICEF 2012) |
31.2 (DHS 2011) |
2.3 (DHS 2011) |
14.3 (UNICEF 2012) |
| Namibia | - | - | - | - | 4.6 (DHS 2013) |
17.8 (DHS 2013) |
2.4 (UNICEF 2012) |
| Niger | - | - | - | - | 80.0 (DHS 2012) |
0.3 (DHS 2012) |
36.1 (UNICEF 2012) |
| Nigeria | 42.6 (UNICEF 2012) |
6.0 (UNICEF 2012) |
38.1 (UNICEF 2012) |
39.9 (UNICEF 2012) |
37.8 (DHS 2013) |
18.3 (DHS 2013) |
19.6 (UNICEF 2012) |
| Réunion | - | - | - | - | - | - | - |
| Rwanda | - | - | - | - | 13.8 (MIS 2013) |
4.3 (MIS 2013) |
0.8 (UNICEF 2012) |
| Sao Tome and Principe |
27.4 (UNICEF 2012) |
- | - | - | 5.9 (DHS 2008/09) |
0.5 (DHS 2008/09) |
5.0 (UNICEF 2012) |
| Senegal | 21.6 (UNICEF 2012) |
- | - | - | 54.8 (DHS 2012/13) |
0.6 (MICS 2010/11) |
12.0 (UNICEF 2012) |
| Seychelles | - | - | - | - | - | - | - |
| Sierra Leone | 13.9 (UNICEF 2012) |
2.1 (UNICEF 2012) |
34.6 (UNICEF 2012) |
32.4 (UNICEF 2012) |
55.8 (DHS 2013) |
4.7 (DHS 2013) |
17.7 (UNICEF 2012) |
| Somalia | 2.3 (UNICEF 2012) |
- | - | - | - | - | 8.4 (UNICEF 2012) |
| South Africa | - | - | - | - | 12.2 (DHS 2003) |
- | 0.8 (UNICEF 2012) |
| South Sudan | - | - | - | - | - | - | - |
| Sudan | - | - | - | - | - | - | - |
| Swaziland | 33 (UNICEF 2012) |
3.8 (UNICEF 2012) |
68.6 (UNICEF 2012) |
14.9 (UNICEF 2012) |
8.1 (DHS 2006/07) |
- | 0.7 (UNICEF 2012) |
| Tanzania | - | - | - | - | 17.8 (AIS/MIS 2011/12) |
0.3 (AIS/MIS 2011/12) |
6.6 (UNICEF 2012) |
| Togo | 28.8 (UNICEF 2012) |
1.5 (UNICEF 2012) |
31.2 (UNICEF 2012) |
41.3 (UNICEF 2012) |
31.8 (DHS 2013/14) |
- | 5.8 (UNICEF 2012) |
| Uganda | - | - | - | - | 12.9 (DHS 2011) |
1.3 (DHS 2011) |
9.9 (UNICEF 2012) |
| Western Sahara | - | - | - | - | - | - | - |
| Zambia | - | - | - | - | 10.4 (DHS 2007) |
5.4 (DHS 2007) |
8.5 (UNICEF 2008–12) |
| Zimbabwe | - | - | - | - | 2.3 (DHS 2010/11) |
1.5 (DHS 2010/11) |
9.3 (UNICEF 2012) |
Maternal Education
Indicators for maternal education are presented in Table 5. Of 40 countries with data, the proportion of women aged 15–49 years with no schooling ranged from 1.2% in Lesotho to 80% in Niger. Among the 32 countries with data on secondary school completion among women aged 15–49 years, prevalence ranged from 0.3% in Tanzania and Niger to 18.3% in Nigeria. Categories for female school completion are presented in Fig 3. Of 41 countries with data, the proportion of women aged 15–49 years who were married by age 15 ranged from 0.7% in Swaziland to 36.1% in Niger. Categories for early marriage are presented in Fig 4.
Figure 3.
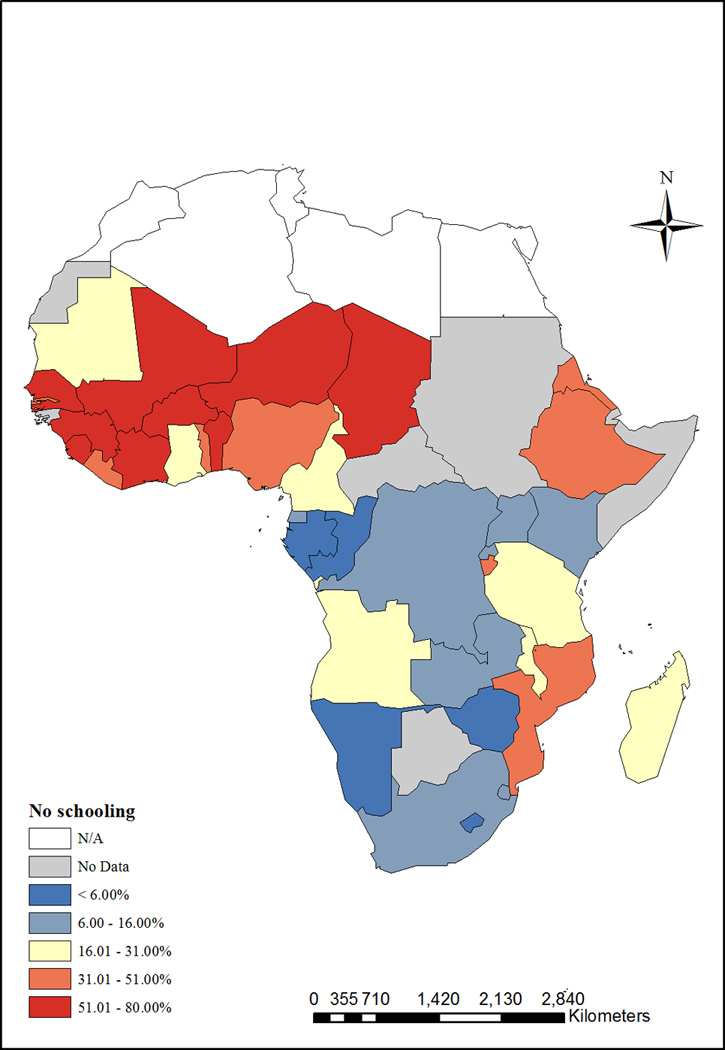
Maternal education (maternal-child interaction domain) - Women aged 15–49 years with no schooling (%), and women aged 15–49 years with secondary school completion (%).
Figure 4.
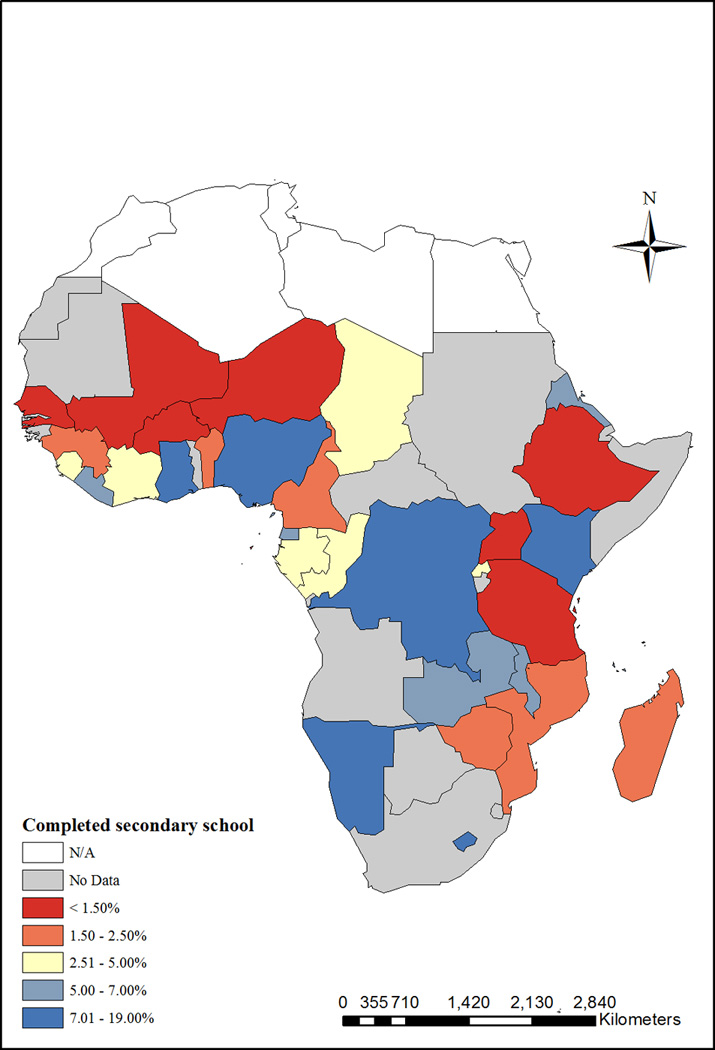
Early marriage (maternal-child interaction domain) - Marriage by age 15 among women aged 15–49 years (%).
Maternal-Child Domain
Because 67% of countries were missing more than half of the maternal-child interaction indicators and eight countries were missing more than 75% of the indicators, we did not calculate a maternal-child interaction domain score.
DISCUSSION
There is a clear need to improve routine collection of high quality, country-level indicators relevant to child development. Data were lacking for many indicators, especially in the maternal-child interaction domain where two-thirds of countries were missing more than half of the indicators. In addition to making risk estimation difficult, the lack of data can hamper efforts to monitor progress. For example, monitoring low birthweight has been challenging due to poor coverage of weighing at birth.(3) Less than 30% of births in Ethiopia, Liberia, Mali, Niger, Nigeria, and Sierra Leone had recorded birthweight, so the reported prevalence of low birthweight in these countries may not be representative of the true burden. If governments are committed to improving child development outcomes, greater effort should be made to design new or improve existing data collection systems.
Nutrition
Given adequate health care and nutrition, low and middle income countries can substantially reduce the burden of low birthweight. Tanzania, Rwanda, Cape Verde, and Kenya had low birthweight prevalence similar to the European average of 6.9%.(57) These levels could be due to policy interventions, including improved antenatal care and food security for pregnant women in Kenya; however, the findings could also be related to other factors including the proportion of babies with recorded birthweights or changes in the prevalence of attended births.(58) Despite successes in minimizing low birthweight in parts of sub-Saharan Africa, the continent still faces a high burden of stunting. Even the best performing countries had under-five stunting prevalence of 16–28%, far exceeding the expected 2.5% observed in cohorts of children growing in accordance with WHO growth standards. Economic development, improved water and sanitation, and sustained inputs into early child growth are likely drivers of the lower levels of stunting in the best performing countries, but it is not clear why some countries with growth-sensitive programming fail to meet growth benchmarks. If the countries with the highest burdens of stunting (48–58% prevalence) could reduce prevalence to levels seen in the best performing countries, the effect on child development could be far reaching.
Since the 1990s, many countries have made substantial improvements in iodization. Governments of major salt producing countries, in partnership with salt producers and organizations like UNICEF and the Micronutrient Initiative, have launched iodization initiatives.(59) There have been major successes; DR Congo had been severely iodine deficient and has achieved sufficiency for 98.5% of the population.(60) In the last decade, however, progress on salt iodization has slowed, due to technical challenges of reaching small salt producers, poor quality control of salt iodization, difficulties in enforcing iodized salt legislation, and waning interest by governments.(61) Despite sufficiency at the national level, sub-groups such as women of reproductive age and children may be at high risk for deficiency – especially those with increased iodine requirements, in whom salt iodization alone may not be adequate.(19) In these sub-groups, additional supplementation might be needed to ensure improved cognitive outcomes.(62,63) Routine monitoring of iodine levels in these high risk groups could help ensure adequacy.
Many countries have a substantial burden of anemia. Addressing iron deficiency in sub-Saharan Africa is complicated by endemic malaria. Mass fortification of grains with iron is presumed to have lower risk relative to iron supplementation, but the effect of fortification initiatives on iron deficiency burden at the population level is unclear. The countries with the highest burden of both severe and total anemia are those with mandatory fortification legislation. While fortified staple foods can reach broad parts of the population, the effectiveness of fortification in reducing iron-deficiency could be limited by choice of fortification vehicle, the type and concentration of fortificant, and other factors. Studies have shown that in the absence of enforcement and quality assurance mechanisms, fortification legislation does not necessarily lead to the desired health outcomes.(64) Worldwide, about half of anemia is due to iron deficiency, so persistence of anemia despite fortification could also be due to factors other than iron such as infection, parasites, or other nutrient deficiencies.(65)
Overall, there was a wide range of performance in nutrition indicators. No countries were consistently high or low performing, suggesting that each country faces its own unique challenges. For example, Rwanda had one of the lowest burdens of low birthweight (6.2%) but one of the highest burdens of stunting (44.2%). The major protective nutrition factor examined, exclusive breastfeeding, had very variable coverage with prevalence ranging from 1% in Djibouti to 84.9% in Rwanda, with 12 countries having prevalence ≥50%. We were unable to identify data on interventions to specifically address IUGR, stunting, and exclusive breastfeeding, so it is unclear how programs designed to affect these risks, if present, might be affecting child development. Again, this underlines the need to improve routine collection of high quality, country-level indicators relevant to child development.
Environment
The shift from leaded to unleaded fuel represents a major success and highlights the important role of government and public policy in leading public health initiatives. In the 1990s, the lead content of gasoline in Africa was the highest in the world.(66) Sudan became the first country in sub-Saharan Africa to switch to unleaded gas in 2000.(67) Regional fuel exporters helped accelerate the shift away from leaded fuel. Cameroon, which exports to CAR, Chad, and Equatorial Guinea, stopped distributing leaded gas in November 2005. South Africa stopped leaded fuel by 2006, affecting smaller importing countries nearby.(67) While fuel is no longer a source of lead exposure in sub-Saharan Africa, children are still exposed through house paint, home-based lead works, burning refuse, polluted waters, and contaminated foods.(41,66,68,69) Studies in Nigeria and South Africa have documented the effects of mining on blood lead levels in both adults and children.(68,69) These sources of lead exposure remain potential threats to child development and should be addressed.
Despite endemicity of malaria and the threat it poses to child development, only 16 countries had estimates of malaria prevalence. Countries with high coverage of malaria prevention interventions tended to also have low prevalence of malaria. Tanzania had the second highest prevalence of children under five years sleeping under ITN and the second lowest burden of malaria among children aged 6–59 months. Madagascar and the Gambia had among the highest proportion of households with IRS and among the lowest malaria burdens. For malaria treatment, however, only one high burden country, Equatorial Guinea, also had a high proportion of children under five years ill with fever receiving anti-malarial drugs. Overall, the reach of malaria interventions was low. The best performing countries had 50–75% of children under five years sleeping under ITN, 40–65% of children under five years ill with fever receiving anti-malarial drugs, and only 16–40% of households with IRS. Countries will have to maintain prevention and treatment efforts to achieve lasting reductions in malaria and influence cognitive development outcomes in children.
More than any other risk factor we analyzed, HIV was the most highly clustered by region. Countries with the highest adult prevalence of HIV were all located in southern Africa. Countries with the highest adult prevalence of HIV also had the highest prevalence of HIV among pregnant women. Generally, ARV receipt tracks with the HIV burden of pregnant women. Five of the six countries with the lowest proportion of pregnant women with HIV receiving ARVs do not have data on prevalence of HIV among pregnant women; however, prevalence of HIV among adults 15–49 years in these countries was <3%, suggesting prevalence of HIV burden among pregnant women might be low and therefore not a health priority given resource constraints.
Despite the health resources devoted to HIV in sub-Saharan Africa, we were not able to directly identify the number of HIV-affected children and instead relied on proxy measures. Countries, especially those with high burdens of HIV, should invest in improved data collection of indicators relevant to HIV-affected children. With the exception of Botswana, South Africa, Swaziland, and Zimbabwe, population-based surveys have typically excluded children and adolescents for measures of HIV prevalence, so the burden of HIV is not clear in this age group. Evidence from acute care settings suggest that children and adolescents are presenting for care for HIV-related illness; however, planning for testing and treatment have not tended to focus on this age group.(70–72) Interventions targeted to adults might not address the unique needs of HIV-affected children such as school disruption or psychological distress from loss of a caregiver. Many long-term cohort studies on the effects of HIV and child outcomes have been focused on North American or European populations and might not be applicable to children in the context of Africa.(73,74) Understanding key factors associated with resilience in this population is imperative to developing interventions to mitigate risks of HIV exposure in children.
There was a wide range of performance in the environment indicators. Indicators in the environment domain provide the most evidence for effective interventions by governments and other supporting agencies. All countries in sub-Saharan Africa have phased out leaded fuel. This is an example of evidence-driven policy change with wide reaching population health benefits. Countries with high coverage of interventions to prevent malaria also had low malaria prevalence, and countries with the highest burden of HIV among pregnant women also had the highest ARV receipt.
Maternal-Child Interactions
Despite the high global prevalence of PPD, relatively little is known about maternal depression in sub-Saharan Africa. We were unable to identify nationally representative estimates for either maternal depression or treatment. Studies from non-nationally representative samples suggest the burden is high but variable across and within countries. With limited health resources, psychological support for pregnant women and new mothers is likely rare. Early identification of maternal depression both during pregnancy and in the postpartum period coupled with effective treatment could greatly reduce the effects of depression on child development.(53) More research is needed on both the burden of maternal depression in sub-Saharan Africa and the role of poverty, violence, and societal stress on maternal depression and child development after which the best methods of screening for and treating maternal depression can be identified.
Very little data were available to assess the burden of inadequate cognitive stimulation. Fewer than 14 countries reported data on learning materials in the home or children left in inadequate care. Only 20 countries reported data on early childhood education. The proportion of households with ≥3 children’s books was low (0.4%-14.7%) while the proportion of households with ≥2 playthings was substantially higher (23.7%-68.6%). Even where available, these are imperfect measures of home environment because they do not account for parental or familial involvement despite lack of material learning objects. Attendance in early childhood education was highly variable across countries and by household wealth. Instituting universal early childhood education could help address low attendance as well as the wealth gap in attendance.
Maternal education is associated with higher child development. Closing gender gaps in education has been slow in West and Central Africa – especially for completion of secondary schooling.(38) In all countries with data, the proportion of women completing secondary school was low. Completion rates in the best performing countries were only 7–18%. Generally, the countries with the lowest levels of maternal education also had the highest prevalence of child marriage. Parenting by age 15 years might also be an important proxy for a mother’s ability to complete secondary school; however, no national-level data were available for this indicator. Strengthening universal primary and secondary education and delaying marriage and first pregnancy until after adolescence could lead to reduced prevalence of low birthweight and better early life growth and child development.
Consistency across Domains
Most countries had mixed performance on indicators. For example, Namibia was in the best category for nutrition but the worst category for environment. Sao Tome and Principe was the only country to score in the best category in both the nutrition and environment domains. Only Chad performed poorly across indicators with the worst category in the nutrition and environment domains and the worst categories for maternal education and child marriage. This finding suggests that each country faces distinct challenges in addressing risk factors for poor child development. Variation could be due to differing country-level priorities as reflected in policies and funding.
Strengths and Limitations
In this paper, we focus on modifiable risk factors that can be addressed through household, mother and/or child-level interventions and for which nationally-representative indicators were available. Additionally, we have included three initiatives for which national policy-level intervention have been or would be required: shifting to unleaded fuels, salt iodization, and iron fortification of grains. While potentially important contributors, we did not review interventions addressing the underlying causes of poor child development including poverty or macro-system risk such as societal violence. Similarly, we have not focused on potential or suspected risks to child development, such as diarrhea, low essential fatty acid intake, or maternal pre-conceptual nutrition, due to limited and/or inconsistent findings.
A main limitation in this study was the lack of data on risks and interventions. In an attempt to include as many risk factors as possible in our analyses, we used proxy measures for some indicators, such as low birthweight for IUGR and anemia for iron deficiency. Additionally, we chose to weight all indicators within each domain equally. While it is unlikely that all elements are of equal importance to child development, there was insufficient evidence to support differential weighting. We excluded countries missing more than 75% of indicators from domain scores. The cut point is arbitrary; however, we wanted to include as many countries as possible while maintaining meaningful score values. Despite these limitations, the domain scores allow for general understanding of performance within and across domains. Due to an overall lack of national-level data on many of the maternal-child interaction indicators, we were unable to calculate a domain score. Subsequently, we were unable to calculate total scores over the three domains making it more difficult to assess overall performance.
Estimates for impact of interventions were largely based on the findings of the Lancet maternal and child under-nutrition series. Their models were based on 36 countries most affected by the burden of under-nutrition – not all of which were in sub-Saharan Africa. Conflict, population displacement, and other factors could influence impact of interventions on child development outcomes in the region. Thus, the interventions could be more or less effective within the sub-Saharan African context. Additionally, synergy among interventions could improve outcomes disproportionately relative to single interventions.
As the world has seen large reductions in child mortality over the last decades, there has been increasing focus on improving child development. Africa has a high burden of risk factors for poor child development with high rates of stunting, malaria, and HIV. Most countries had mixed performance across domains, and only Chad had overall poor performance. This finding suggests that each country faces its own unique challenges in addressing risk factors for child development. A major issue in the development agenda is a lack of data on many indicators, especially those related to mother-child interaction. There is a clear need to improve routine collection of high-quality, country-level indicators relevant to child development to assess risk and track progress. Thus, greater effort should be placed to design new or improve existing data collection systems.
Supplementary Material
Acknowledgments
None.
Financial Support: This research was supported in part by Laney Graduate School, Emory University.
Footnotes
Author Contributions: NDF and ADS conceived the original study idea, formulated the research question, and designed the study. NDF conducted all analyses and wrote the initial manuscript draft. Both authors interpreted findings, contributed to the intellectual content of the work, and edited subsequent drafts.
Ethical Standards: This study does not constitute human subjects research.
Conflicts of Interest: None.
REFERENCES
- 1.Walker SP, Wachs TD, Gardner JM, Lozoff B, Wasserman GA, Pollitt E, et al. Child development: risk factors for adverse outcomes in developing countries. Lancet. 2007 Jan 13;369(9556):145–157. doi: 10.1016/S0140-6736(07)60076-2. [DOI] [PubMed] [Google Scholar]
- 2.Walker SP, Wachs TD, Grantham-McGregor S, Black MM, Nelson CA, Huffman SL, et al. Inequality in early childhood: risk and protective factors for early child development. Lancet. 2011 Oct 8;378(9799):1325–1338. doi: 10.1016/S0140-6736(11)60555-2. [DOI] [PubMed] [Google Scholar]
- 3.UNICEF. Improving child nutrition: the achievable imperative for global progress. 2013. [Google Scholar]
- 4.Andersson M, Karumbunathan V, Zimmermann MB. Global iodine status in 2011 and trends over the past decade. J Nutr. 2012 Apr;142(4):744–750. doi: 10.3945/jn.111.149393. [DOI] [PubMed] [Google Scholar]
- 5.Roll Back Malaria Partnership. Eliminating Malaria: Learning From the Past, Looking Ahead [Internet] World Health Organization; 2011. [cited 2015 Jan 15]. Available from: http://www.rbm.who.int/ProgressImpactSeries/docs/report9-en.pdf. [Google Scholar]
- 6.Grantham-McGregor S, Cheung YB, Cueto S, Glewwe P, Richter L, Strupp B, et al. Developmental potential in the first 5 years for children in developing countries. Lancet. 2007 Jan 6;369(9555):60–70. doi: 10.1016/S0140-6736(07)60032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Engle PL, Black MM, Behrman JR, Cabral de Mello M, Gertler PJ, Kapiriri L, et al. Strategies to avoid the loss of developmental potential in more than 200 million children in the developing world. Lancet. 2007 Jan 20;369(9557):229–242. doi: 10.1016/S0140-6736(07)60112-3. [DOI] [PubMed] [Google Scholar]
- 8.Engle PL, Fernald LCH, Alderman H, Behrman J, O’Gara C, Yousafzai A, et al. Strategies for reducing inequalities and improving developmental outcomes for young children in low-income and middle-income countries. Lancet. 2011 Oct 8;378(9799):1339–1353. doi: 10.1016/S0140-6736(11)60889-1. [DOI] [PubMed] [Google Scholar]
- 9.Lee PA, Houk CPW. Cognitive and psychosocial development concerns in children born small for gestational age. Pediatr Endocrinol Rev PER. 2012 Jan;10(2):209–216. [PubMed] [Google Scholar]
- 10.de Kieviet JF, Zoetebier L, van Elburg RM, Vermeulen RJ, Oosterlaan J. Brain development of very preterm and very low-birthweight children in childhood and adolescence: a meta-analysis. Dev Med Child Neurol. 2012 Apr;54(4):313–323. doi: 10.1111/j.1469-8749.2011.04216.x. [DOI] [PubMed] [Google Scholar]
- 11.Gorman KS, Pollitt E. Relationship between weight and body proportionality at birth, growth during the first year of life, and cognitive development at 36, 48, and 60 months. Infant Behav Dev. 1992 Jul;15(3):279–296. [Google Scholar]
- 12.Villar J, Smeriglio V, Martorell R, Brown CH, Klein RE. Heterogeneous growth and mental development of intrauterine growth-retarded infants during the first 3 years of life. Pediatrics. 1984 Nov;74(5):783–791. [PubMed] [Google Scholar]
- 13.Liu X, Sun Z, Neiderhiser JM, Uchiyama M, Okawa M. Low birth weight, developmental milestones, and behavioral problems in Chinese children and adolescents. Psychiatry Res. 2001 Mar 25;101(2):115–129. doi: 10.1016/s0165-1781(00)00244-4. [DOI] [PubMed] [Google Scholar]
- 14.Zimmermann MB. The Effects of Iodine Deficiency in Pregnancy and Infancy. Paediatr Perinat Epidemiol. 2012 Jul 1;26:108–117. doi: 10.1111/j.1365-3016.2012.01275.x. [DOI] [PubMed] [Google Scholar]
- 15.Haddow JE, Palomaki GE, Allan WC, Williams JR, Knight GJ, Gagnon J, et al. Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child. N Engl J Med. 1999 Aug 19;341(8):549–555. doi: 10.1056/NEJM199908193410801. [DOI] [PubMed] [Google Scholar]
- 16.Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K, Giugliani E, et al. What works? Interventions for maternal and child undernutrition and survival. The Lancet. 2008 Feb 8;371(9610):417–440. doi: 10.1016/S0140-6736(07)61693-6. [DOI] [PubMed] [Google Scholar]
- 17.Bhutta ZA, Das JK, Rizvi A, Gaffey MF, Walker N, Horton S, et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? The Lancet. 2013 Aug 9;382(9890):452–477. doi: 10.1016/S0140-6736(13)60996-4. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. Assessment of iodine deficiency disorders and monitoring their elimination [Internet] WHO; [cited 2015 Jan 22]. Available from: http://www.who.int/nutrition/publications/micronutrients/iodine_deficiency/9789241595827/en/ [Google Scholar]
- 19.Wu T, Liu GJ, Li P, Clar C. Iodised salt for preventing iodine deficiency disorders. Cochrane Database Syst Rev. 2002;(3):CD003204. doi: 10.1002/14651858.CD003204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aburto NJ, Abudou M, Candeias V, Wu T. Effect and safety of salt iodization to prevent iodine deficiency disorders: a systematic review with meta-analyses [Internet] Geneva: World Health Organization; 2014. [cited 2015 May 19]. Available from: http://apps.who.int/iris/bitstream/10665/148175/1/9789241508285_eng.pdf. [Google Scholar]
- 21.Horwood LJ, Fergusson DM. Breastfeeding and later cognitive and academic outcomes. Pediatrics. 1998 Jan;101(1):E9. doi: 10.1542/peds.101.1.e9. [DOI] [PubMed] [Google Scholar]
- 22.Jain A, Concato J, Leventhal JM. How good is the evidence linking breastfeeding and intelligence? Pediatrics. 2002 Jun;109(6):1044–1053. doi: 10.1542/peds.109.6.1044. [DOI] [PubMed] [Google Scholar]
- 23.Daniels MC, Adair LS. Breast-feeding influences cognitive development in Filipino children. J Nutr. 2005 Nov;135(11):2589–2595. doi: 10.1093/jn/135.11.2589. [DOI] [PubMed] [Google Scholar]
- 24.Imdad A, Yakoob MY, Bhutta ZA. Effect of breastfeeding promotion interventions on breastfeeding rates, with special focus on developing countries. BMC Public Health. 2011 Apr 13;11(Suppl 3):S24. doi: 10.1186/1471-2458-11-S3-S24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Idro R, Carter JA, Fegan G, Neville BGR, Newton CRJC. Risk factors for persisting neurological and cognitive impairments following cerebral malaria. Arch Dis Child. 2006 Feb;91(2):142–148. doi: 10.1136/adc.2005.077784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holding PA, Stevenson J, Peshu N, Marsh K. Cognitive sequelae of severe malaria with impaired consciousness. Trans R Soc Trop Med Hyg. 1999 Oct;93(5):529–534. doi: 10.1016/s0035-9203(99)90368-1. [DOI] [PubMed] [Google Scholar]
- 27.Boivin MJ. Effects of early cerebral malaria on cognitive ability in Senegalese children. J Dev Behav Pediatr JDBP. 2002 Oct;23(5):353–364. doi: 10.1097/00004703-200210000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Sherr L, Mueller J, Varrall R. A systematic review of cognitive development and child human immunodeficiency virus infection. Psychol Health Med. 2009 Aug;14(4):387–404. doi: 10.1080/13548500903012897. [DOI] [PubMed] [Google Scholar]
- 29.Sherr L, Croome N, Parra Castaneda K, Bradshaw K, Herrero Romero R. Developmental challenges in HIV infected children—An updated systematic review. Child Youth Serv Rev. 2014 Oct;45:74–89. [Google Scholar]
- 30.World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection [Internet] Geneva: World Health Organization; 2013. Jun, [cited 2015 May 15]. Available from: http://www.who.int/hiv/pub/guidelines/arv2013/download/en/ [Google Scholar]
- 31.De Cock KM, Fowler MG, Mercier E, de Vincenzi I, Saba J, Hoff E, et al. Prevention of mother-to-child HIV transmission in resource-poor countries: translating research into policy and practice. JAMA. 2000 Mar 1;283(9):1175–1182. doi: 10.1001/jama.283.9.1175. [DOI] [PubMed] [Google Scholar]
- 32.Wachs TD, Black MM, Engle PL. Maternal Depression: A Global Threat to Children’s Health, Development, and Behavior and to Human Rights. Child Dev Perspect. 2009;3:51–59. [Google Scholar]
- 33.Halbreich U, Karkun S. Cross-cultural and social diversity of prevalence of postpartum depression and depressive symptoms. J Affect Disord. 2006 Apr;91(2–3):97–111. doi: 10.1016/j.jad.2005.12.051. [DOI] [PubMed] [Google Scholar]
- 34.Leahy-Warren P, McCarthy G. Postnatal depression: prevalence, mothers’ perspectives, and treatments. Arch Psychiatr Nurs. 2007 Apr;21(2):91–100. doi: 10.1016/j.apnu.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 35.Magwaza AS, Edwards SD. An Evaluation of an Integrated Parent-Effectiveness Training and Children’s Enrichment Programme for Disadvantaged Families. South Afr J Psychol. 1991 Mar 1;21(1):21–25. [Google Scholar]
- 36.Kagitcibasi C, Sunar D, Bekman S. Long-term effects of early intervention: Turkish low-income mothers and children. J Appl Dev Psychol. 2001 Jul;22(4):333–361. [Google Scholar]
- 37.Eickmann SH, Lima ACV, Guerra MQ, Lima MC, Lira PIC, Huttly SRA, et al. Improved cognitive and motor development in a community-based intervention of psychosocial stimulation in northeast Brazil. Dev Med Child Neurol. 2003 Aug;45(8):536–541. doi: 10.1017/s0012162203000987. [DOI] [PubMed] [Google Scholar]
- 38.UNICEF. The State of the World’s Children 2012 [Internet] New York: UNICEF; 2012. [cited 2015 May 18]. Available from: http://www.unicef.org/sowc09/docs/SOWC09-FullReport-EN.pdf. [Google Scholar]
- 39.World Health Organization, UNICEF, the World Bank. Joint child malnutrition estimates - Levels and trends [Internet] [cited 2015 Feb 16];Global Database on Child Growth and Malnutrition. 2014 Available from: http://www.who.int/nutgrowthdb/estimates2013/en/
- 40.Division of Malaria Control [Ministry of Public Health and Sanitation], Kenya National Bureau of Statistics, ICF Macro. 2010 Kenya Malaria Indicator Survey [Internet] Nairobi, Kenya: DOMC, KNBS, and ICF Macro; 2011. [cited 2015 Jan 29]. Available from: http://dhsprogram.com/pubs/pdf/MIS7/MIS7.pdf. [Google Scholar]
- 41.Nriagu J. Toxic metal pollution in Africa. Sci Total Environ. 1992;121:1–37. doi: 10.1016/0048-9697(92)90304-b. [DOI] [PubMed] [Google Scholar]
- 42.Golow A, Kwaansa-Ansah E. Comparisons of lead and zinc levels in the hair of pupils from four towns in Jumasi municipal area of Ghana. Bull Environ Contam Toxicol. 1994;53:325–331. doi: 10.1007/BF00197221. [DOI] [PubMed] [Google Scholar]
- 43.Advisory Committee on Childhood Lead Poisoning Prevention. Low Level Lead Exposure Harms Children: A Renewed Call for Primary Prevention [Internet] Atlanta, GA: Centers for Disease Control and Prevention; 2012. [cited 2015 Mar 3]. Available from: http://www.cdc.gov/nceh/lead/acclpp/final_document_030712.pdf. [Google Scholar]
- 44.The Partnership for Clean Fuels and Vehicles. An Overview of the Partnership for Clean Fuels and Vehicles (PCFV) [Internet] United Nations Environment Programme; 2014. [cited 2015 Jan 15]. Available from: http://www.unep.org/Transport/New/PCFV/pdf/PCFV-Brochure-April2014_combined.pdf. [Google Scholar]
- 45.National AIDS Coordinating Agency Republic of Botswana, UNAIDS. Botswana 2013 global AIDS response report: progress report of the national response to the 2011 declaration of commitments on HIV and AIDS [Internet] Republic of Botswana: National AIDS Coordinating Agency; 2014. Mar, [Accessed 18 January 2015]. Available from: http://www.unaids.org/sites/default/files/en/dataanalysis/knowyourresponse/countryprogressreports/2014countries/BWA_narrative_report_2014.pdf. [Google Scholar]
- 46.The Namibia Ministry of Health and Social Services (MoHSS), ICF International. The Namibia Demographic and Health Survey 2013 [Internet] Windhoek, Namibia, and Rockville, Maryland, USA: MoHSS and ICF International; 2014. [cited 2015 Jan 30]. Available from: http://dhsprogram.com/pubs/pdf/FR298/FR298.pdf. [Google Scholar]
- 47.Sawyer A, Ayers S, Smith H. Pre- and postnatal psychological wellbeing in Africa: a systematic review. J Affect Disord. 2010 Jun;123(1–3):17–29. doi: 10.1016/j.jad.2009.06.027. [DOI] [PubMed] [Google Scholar]
- 48.Fatoye FO, Oladimeji BY, Adeyemi AB. Difficult delivery and some selected factors as predictors of early postpartum psychological symptoms among Nigerian women. J Psychosom Res. 2006 Mar;60(3):299–301. doi: 10.1016/j.jpsychores.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 49.Adewuya AO, Ola BO, Aloba OO, Mapayi BM, Okeniyi JAO. Impact of postnatal depression on infants’ growth in Nigeria. J Affect Disord. 2008 May;108(1–2):191–193. doi: 10.1016/j.jad.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 50.Owoeye AO, Aina OF, Morakinyo O. Risk factors of postpartum depression and EPDS scores in a group of Nigerian women. Trop Doct. 2006 Apr;36(2):100–103. doi: 10.1258/004947506776593341. [DOI] [PubMed] [Google Scholar]
- 51.Ukpong DI, Owolabi AT. Postpartum emotional distress: a controlled study of Nigerian women after caesarean childbirth. J Obstet Gynaecol J Inst Obstet Gynaecol. 2006 Feb;26(2):127–129. doi: 10.1080/01443610500443386. [DOI] [PubMed] [Google Scholar]
- 52.Lawrie TA, Hofmeyr GJ, de Jager M, Berk M. Validation of the Edinburgh Postnatal Depression Scale on a cohort of South African women. South Afr Med J Suid-Afr Tydskr Vir Geneeskd. 1998 Oct;88(10):1340–1344. [PubMed] [Google Scholar]
- 53.Cooper PJ, Tomlinson M, Swartz L, Woolgar M, Murray L, Molteno C. Post-partum depression and the mother-infant relationship in a South African peri-urban settlement. Br J Psychiatry J Ment Sci. 1999 Dec;175:554–558. doi: 10.1192/bjp.175.6.554. [DOI] [PubMed] [Google Scholar]
- 54.Hanlon C, Medhin G, Alem A, Araya M, Abdulahi A, Hughes M, et al. Detecting perinatal common mental disorders in Ethiopia: validation of the self-reporting questionnaire and Edinburgh Postnatal Depression Scale. J Affect Disord. 2008 Jun;108(3):251–262. doi: 10.1016/j.jad.2007.10.023. [DOI] [PubMed] [Google Scholar]
- 55.Coleman R, Morison L, Paine K, Powell RA, Walraven G. Women’s reproductive health and depression: a community survey in the Gambia, West Africa. Soc Psychiatry Psychiatr Epidemiol. 2006 Sep;41(9):720–727. doi: 10.1007/s00127-006-0085-8. [DOI] [PubMed] [Google Scholar]
- 56.Cox JL. Postnatal depression: a comparison of African and Scottish women. Soc Psychiatry Sozialpsychiatrie Psychiatr Soc. 1983;18(1):25–28. doi: 10.1007/BF00583384. [DOI] [PubMed] [Google Scholar]
- 57.OECD. Health at a Glance: Europe 2012 [Internet] Paris: OECD Publishing; 2012. [cited 2015 May 19]. Available from: http://www.oecd-ilibrary.org.proxy.library.emory.edu/social-issues-migration-health/health-at-a-glance-europe-2012_9789264183896-en. [Google Scholar]
- 58.Ministry of Public Health and Sanitation (Republic of Tanzania) National Nutrition Action Plan (2012–2017) [Internet] Ministry of Public Health and Sanitation; 2013. [cited 2015 Jul 15]. Available from: http://scalingupnutrition.org/wp-content/uploads/2013/10/Kenya-National-Nutrition-Action-Plan-2012-2017-final.pdf. [Google Scholar]
- 59.Micronutrient Initiative. The Micronutrient Initiative in Africa [Internet] Micronutrient Initiative; 2015. [cited 2015 Mar 2]. Available from: http://www.micronutrient.org/english/view.asp?x=547. [Google Scholar]
- 60.Iodine Global Network. Global Iodine Nutrition Scorecard for 2012 [Internet] Iodine Global Network; 2013. [cited 2015 Mar 2]. Available from: http://www.ign.org/cm_data/Scorecard_IGN_website_02_03_2015.pdf. [Google Scholar]
- 61.Pearce EN, Andersson M, Zimmermann MB. Global Iodine Nutrition: Where Do We Stand in 2013? Thyroid. 2013 May 1;23(5):523–528. doi: 10.1089/thy.2013.0128. [DOI] [PubMed] [Google Scholar]
- 62.Cao XY, Jiang XM, Dou ZH, Rakeman MA, Zhang ML, O’Donnell K, et al. Timing of vulnerability of the brain to iodine deficiency in endemic cretinism. N Engl J Med. 1994 Dec 29;331(26):1739–1744. doi: 10.1056/NEJM199412293312603. [DOI] [PubMed] [Google Scholar]
- 63.Qian M, Wang D, Watkins WE, Gebski V, Yan YQ, Li M, et al. The effects of iodine on intelligence in children: a meta-analysis of studies conducted in China. Asia Pac J Clin Nutr. 2005;14(1):32–42. [PubMed] [Google Scholar]
- 64.van den Wijngaart A, Begin F, Codling K, Randall P, Johnson QW. Regulatory monitoring systems of fortified salt and wheat flour in selected ASEAN countries. Food Nutr Bull. 2013 Jun;34(10):102S–111S. doi: 10.1177/15648265130342S112. [DOI] [PubMed] [Google Scholar]
- 65.United Nations Children’s Fund Micronutrient Initiative (UNICEF/MI) Vitamin and Mineral Deficiency. A Global Progress Report. Ottawa: 2004. [Google Scholar]
- 66.Nriagu JO, Blankson ML, Ocran K. Childhood lead poisoning in Africa: a growing public health problem. Sci Total Environ. 1996 Mar 15;181(2):93–100. doi: 10.1016/0048-9697(95)04954-1. [DOI] [PubMed] [Google Scholar]
- 67.Lacey M. Belatedly, Africa Is Converting to Lead-Free Gasoline. [cited 2015 Jan 15];The New York Times [Internet] 2004 Oct 31; Available from: http://www.nytimes.com/2004/10/31/international/africa/31kenya.html.
- 68.Nriagu J, Oleru NT, Cudjoe C, Chine A. Lead poisoning of children in Africa, III. Kaduna, Nigeria. Sci Total Environ. 1997 Apr 30;197(1–3):13–19. doi: 10.1016/s0048-9697(96)05408-3. [DOI] [PubMed] [Google Scholar]
- 69.Nriagu J, Jinabhai CC, Naidoo R, Coutsoudis A. Lead poisoning of children in Africa, II. Kwazulu/Natal, South Africa. Sci Total Environ. 1997 Apr 30;197(1–3):1–11. doi: 10.1016/s0048-9697(96)05407-1. [DOI] [PubMed] [Google Scholar]
- 70.Ferrand RA, Corbett EL, Wood R, Hargrove J, Ndhlovu CE, Cowan FM, et al. AIDS among older children and adolescents in Southern Africa: projecting the time course and magnitude of the epidemic. AIDS Lond Engl. 2009 Sep 24;23(15):2039–2046. doi: 10.1097/QAD.0b013e32833016ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ferrand RA, Bandason T, Musvaire P, Larke N, Nathoo K, Mujuru H, et al. Causes of Acute Hospitalization in Adolescence: Burden and Spectrum of HIV-Related Morbidity in a Country with an Early-Onset and Severe HIV Epidemic: A Prospective Survey. PLoS Med. 2010 Feb 2;7(2):e1000178. doi: 10.1371/journal.pmed.1000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Walker AS, Mulenga V, Sinyinza F, Lishimpi K, Nunn A, Chintu C, et al. Determinants of survival without antiretroviral therapy after infancy in HIV-1-infected Zambian children in the CHAP Trial. J Acquir Immune Defic Syndr 1999. 2006 Aug 15;42(5):637–645. doi: 10.1097/01.qai.0000226334.34717.dc. [DOI] [PubMed] [Google Scholar]
- 73.Rice ML, Zeldow B, Siberry GK, Purswani M, Malee K, Hoffman HJ, et al. Evaluation of risk for late language emergence after in utero antiretroviral drug exposure in HIV-exposed uninfected infants. Pediatr Infect Dis J. 2013 Oct;32(10):e406–e413. doi: 10.1097/INF.0b013e31829b80ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gadow KD, Angelidou K, Chernoff M, Williams PL, Heston J, Hodge J, et al. Longitudinal study of emerging mental health concerns in youth perinatally infected with HIV and peer comparisons. J Dev Behav Pediatr JDBP. 2012 Jul;33(6):456–468. doi: 10.1097/DBP.0b013e31825b8482. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


