To the Editor:
Urinary incontinence (UI) and heart failure (HF) are both prevalent conditions having significant impact on quality of life (1). Little information is available about HF patients seeking help for UI despite evidence that both conditions can be managed through intervention from a health care worker (1). The purpose of this study was to identify factors associated with help-seeking for UI in adults with HF.
Secondary analyses were conducted using a dataset from a survey exploring prevalence and correlates of UI and other urinary symptoms conducted with HF patients from 2005 to 2007 (2). Participants were recruited from one in-patient HF unit and two ambulatory HF clinics. The study was approved by the University of North Carolina, Presbyterian, and Carolina Health Systems Institutional Review Boards.
An affirmative response to a survey question, “Have you reported your urinary leakage or overactive bladder to your doctor or nurse?” defined help-seeking behavior for these analyses. The 7-item Incontinence Impact Questionnaire (IIQ) and the 6-item Urogenital Distress Inventory (UDI) were used to evaluate the impact of incontinence on quality of life and assess bother experienced from symptoms, respectively. Statistical analyses were performed using SAS, version 9.2 (SAS Institute, Inc., Cary, NC).
One hundred and thirty-four patients (45%) in this sample reported UI. Proportionally more women (p<.001), out-patients (p<.001), people who self-reported poor health (p=.002), and people reporting more than two urinary symptoms (p<.001) also reported being incontinent. Of the 134 incontinent HF patients, only forty-five (34%) reported UI to a health care professional.
Twenty-two percent of incontinent respondents reported they had talked to other people about incontinence, 13% reported they had asked for more information about incontinence, and 30% had read articles about UI in popular magazines. Each of these variables was significantly associated with help-seeking (χ2 = (1, N=134) = 18.3, p<.001; χ2 = (1, N=134) = 20.1, p<.001; χ2 = (1, N=134) = 5.3, p=.022, respectively). The majority of respondents (69%) responded they were interested in learning more about urinary leakage.
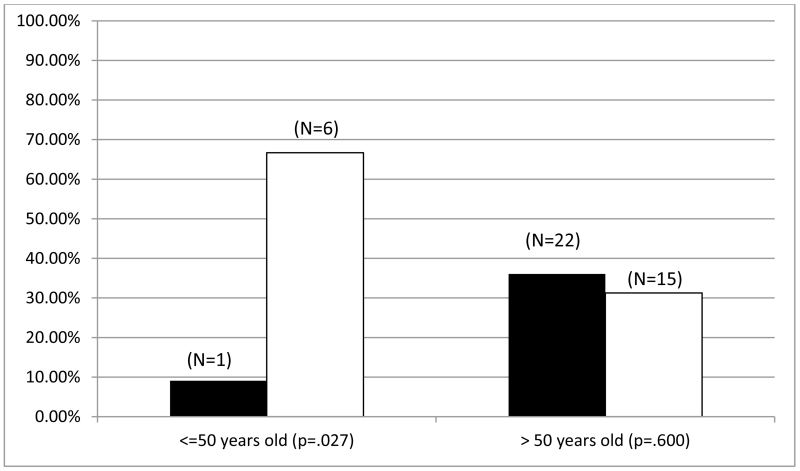
Logistic regression was used for multivariate analyses. One unit increase of UDI-6 was associated with 17% increase of the likelihood of seeking help (β = .172, se=.059, p =.004); Odds Ratio 1.2 (95% CI 1.1 to 1.3). There was significant interaction between age and gender on help-seeking behavior (p=.027) (see Figure 1). Men younger than 50 years of age were more likely to seek help for incontinence than women (67% versus 9%, p=.027). After the age of 50, the proportion of men and women seeking help was similar (31% versus 36%, p= .600).
Figure 1.
Help-seeking for UI by Sex and Age Group
 Women Seeking Help
Women Seeking Help
 Men Seeking Help
Men Seeking Help
UDI-6 score was associated with help-seeking, which suggests that bothersomeness and impact on quality of life may be important factors in the decision to seek help. Despite the low proportion of patients reporting UI, many engaged in behaviors to get information about UI or stated they would like to learn more about UI. These responses indicate HF patients have interest in knowing more about UI, perhaps to decrease the impact of UI on their lives.
Our findings also indicate that UI may be more bothersome to younger men than younger women. Older men had a rate similar to older women in seeking help. It may be that with age people learn to adjust to being incontinent or consider it a part of growing older. Other researchers found a similar relationship between age and sex and help-seeking (3). Li et al. (2007) suggested that younger women may be less likely to seek help due to the availability of coping strategies, such as pads designed for the containment of urine or menstrual flow. Convenient methods to manage UI may be less known, less available, or less acceptable to younger men, which may promote early help-seeking from health care providers. Similarly, women may be more likely to view UI as a personal problem and therefore be less likely to seek help, while men may seek help, fearing that a serious medical problem may underlie their UI (3). It is widely believed that UI is a normal part of the aging process (4). When this belief is held by both health care professionals and patients, both may be unlikely to discuss the problem. Evidence suggests young women (from 45 to 54 years old) would seek help if they believed UI was related to a health condition (5). Screening for UI and its impact on quality of life at hospital admission, during hospitalization, and at clinical visits for all HF patients could begin the processes of education and intervening to improve continence and manage urinary symptoms.
ACKNOWLEDGMENTS
We acknowledge support from the University of North Carolina Center for Aging and Health and the American Federation for Aging Research. We also acknowledge support from the University of North Carolina School of Nursing, particularly John Carlson, MS, Research Associate Professor, for his invaluable statistical consultation.
Funding Sources
Detrol Clinical Research Program, 2005-2007
MSTAR, 2011 American Federation for Aging Research
Sponsor’s Role: None.
Footnotes
Conflict of Interest: Dr. Mary H. Palmer declared a conflict of interest.
Conflict of Interest Disclosures:
| Elements of Financial/Personal Conflicts |
Kaleigh Lindeman | Yin Li | Mary H. Palmer | |||
|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | |
|
Employment or Affiliation |
x | x | x | |||
| Grants/Funds | x | x | x | |||
| Honoraria | x | x | x | |||
| Speaker Forum | x | x | x | |||
| Consultant | x | x | x | |||
| Stocks | x | x | x | |||
| Royalties | x | x | x | |||
| Expert Testimony | x | x | x | |||
| Board Member | x | x | x | |||
| Patents | x | x | x | |||
| Personal Relationship | x | x | x | |||
Author Contributions:
Kaleigh Lindeman: Conception of study; preparation and review of manuscript; final approval of manuscript;
Yin Li: Data management, analysis and interpretation of data; manuscript preparation and review; final approval of manuscript;
Mary H. Palmer: Conception and design of the study; data analyses and interpretation; preparation and review of manuscript; final approval of manuscript;
REFERENCES
- 1.Lee PG, Cigolle C, Blaum C. The co-occurrence of chronic diseases and geriatric syndromes: the health and retirement study. J Am Geriatr Soc. 2009;57(3):511–516. doi: 10.1111/j.1532-5415.2008.02150.x. [DOI] [PubMed] [Google Scholar]
- 2.Palmer MH, Hardin SR, Behrend C, et al. Urinary incontinence and overactive bladder in patients with heart failure. J Urol. 2009;182(1):196–202. doi: 10.1016/j.juro.2009.02.115. [DOI] [PubMed] [Google Scholar]
- 3.Li Y, Cai X, Glance LG, et al. Gender differences in healthcare-seeking behavior for urinary incontinence and the impact of socioeconomic status: a study of the Medicare managed care population. Med Care. 2007;45(11):1116–1122. doi: 10.1097/MLR.0b013e31812da820. [DOI] [PubMed] [Google Scholar]
- 4.Tannenbaum C, Drali R, Holroyd-Leduc J, et al. Lessons learned: Impact of a continence promotion activity for older community-dwelling women. Neurourol Urodyn. 2010;29(4):540–544. doi: 10.1002/nau.20800. [DOI] [PubMed] [Google Scholar]
- 5.Margalith I, Gillon G, Gordon D. Urinary incontinence in women under 65: quality of life, stress related to incontinence and patterns of seeking health care. Quality of Life research. 2004;13(8):1381–1390. doi: 10.1023/B:QURE.0000040794.77438.cf. [DOI] [PubMed] [Google Scholar]