Abstract
Background
Prompt recognition of acute myocardial infarction (AMI) symptoms and timely care-seeking behavior are critical to optimize acute medical therapies. Relatively little is known about the symptom presentation and care-seeking experiences of women aged ≤55 years with AMI, a group shown to have increased mortality risk as compared with similarly aged men. Understanding symptom recognition and experiences engaging the healthcare system may provide opportunities to reduce delays and improve acute care for this population.
Methods and Results
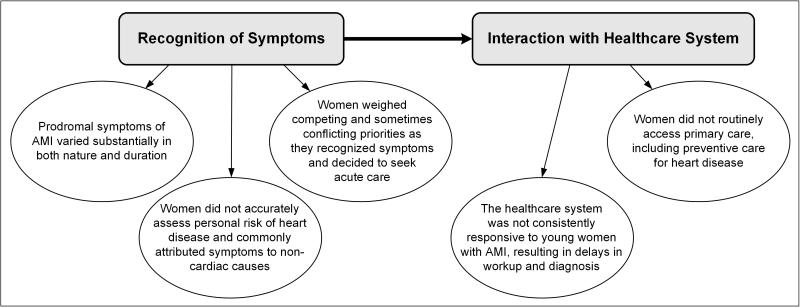
We conducted a qualitative study using in-depth interviews with 30 women (aged 30-55 years) hospitalized with AMI to explore their experiences with prodromal symptoms and their decision-making process to seek medical care. Five themes characterized their experiences: 1) prodromal symptoms varied substantially in both nature and duration; 2) they inaccurately assessed personal risk of heart disease and commonly attributed symptoms to non-cardiac causes; 3) competing and conflicting priorities influenced decisions about seeking acute care; 4) the healthcare system was not consistently responsive to them, resulting in delays in workup and diagnosis; and 5) they did not routinely access primary care, including preventive care for heart disease.
Conclusions
Participants did not accurately assess their cardiovascular risk, reported poor preventive health behaviors, and delayed seeking care for symptoms, suggesting that differences in both prevention and acute care may be contributing to young women's elevated AMI mortality relative to men. Identifying factors that promote better cardiovascular knowledge, improved preventive health care, and prompt care-seeking behaviors represent important targets for this population.
Keywords: women, myocardial infarction, symptoms, qualitative research
Over 15,000 U.S. women aged <55 years die each year from heart disease, ranking it among the leading causes of death in this age group.1 Young women have twice the risk of dying during a hospitalization for an acute myocardial infarction (AMI), as compared with similarly aged men.2,3 Moreover, among those who survive, the subsequent mortality risk for women is about 50% higher than the risk for men.4 Though the absolute difference in mortality outcomes between men and women has been decreasing over time, women aged <55 years remain at increased risk for death.5 The causal factors for this excess risk remain unknown.
Delays in both recognizing symptoms of AMI and seeking medical care for symptoms may contribute to poorer outcomes for women.6 Evidence derived from older populations of individuals with AMI reveals that women delay longer than men and often attribute symptoms to non-cardiac conditions.7-12 Comparable studies have not been conducted to describe the perceptions and actions of women younger than 55 years experiencing AMI symptoms. Discord between actual and perceived symptoms of heart disease may contribute to delays in care-seeking behavior.7,8,13 Describing the clinical presentation of AMI symptoms from the perspective of these women, particularly in terms of their internal decision process to act on symptoms, may provide valuable insights into factors that influence prompt care-seeking behaviors. We know little about young women's perceptions of the care that they received when presenting with symptoms of AMI. Understanding healthcare interactions from their perspective may provide insights into opportunities to improve the early detection and treatment of this high risk, but relatively poorly described, population for whom AMI is a leading cause of death.
To address these gaps in knowledge, we interviewed women 55 years of age or younger who were recently hospitalized with AMI to describe their experiences, including symptom recognition, responses to symptoms, and interactions with primary and acute healthcare systems. We sought to identify factors that may contribute to delays in recognizing symptoms of heart disease and engaging the healthcare system.
Methods
Study Design and Sample
We conducted a qualitative study of women aged ≤55 years enrolled in the Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients’ Health Status (TRIUMPH) study, a multicenter observational registry of >4,300 patients hospitalized with AMI.14 We chose a qualitative approach because we were interested in capturing essential aspects of a phenomenon that is difficult to measure quantitatively,15 that is, the individual perspectives and experiences of this younger cohort of women diagnosed with AMI. Such methods are increasingly recognized as providing unique and valuable contributions to cardiovascular disease outcomes and health services research.16 We used a grounded theory approach to guide our study, deriving explanations or theories inductively from the data.17
We selected a sample of ‘information-rich’ participants18 who were uniquely able to provide insights of central importance to the study's purpose (also known as purposeful sampling). We contacted eligible TRIUMPH participants by mail with an introductory letter explaining the purpose of the study and inviting their participation. We conducted in-depth interviews via telephone within 2 weeks of TRIUMPH study enrollment between 10/2006 and 5/2007. The final sample size was determined by the criterion of theoretical saturation, or the point at which no novel concepts emerged from successive interviews.19 Saturation was achieved upon completion of 30 participant interviews; the last few interviews provided no new information, thus confirming saturation.
Data Collection and Measures
In-depth interviews elicited individual patient perceptions and experiences through open, non-directive questions. The interviews began with a broad ‘grand tour’20 question: “Let's start by having you tell me about your health just before your recent hospitalization.” We used standard open-ended probes to encourage women to increase the breadth or depth of responses and to clarify statements.18 Consistent with the grounded theory approach,17 data collection and analysis steps were iterative in nature, and our interview guide evolved as interviews and analysis progressed in order to ensure the questions were exploring all emerging themes (Supplement).
A member of the research team (BG) with training in medical anthropology and extensive experience in qualitative interviewing conducted the telephone interviews. Interviews were 30-45 minutes in length, with an average length of 28 minutes. All interviews were audiotaped and transcribed by a member of the research team. A second research team member reviewed every 5 transcripts to verify the accuracy of the transcriptions. To further describe the sample, we extracted data on selected sociodemographic and clinical characteristics from each participant's TRIUMPH record. Institutional Review Board approval was obtained at each institution participating in the parent TRIUMPH study, and patients provided informed consent for their study participation in TRIUMPH and in the qualitative sub-study.
Data Analysis
We analyzed data from the transcribed interviews by classifying specific quotes from participants with codes (tags or labels assigning meaning to segments of text) developed iteratively to reflect the data. We created an initial code structure after in-depth review of the first few transcripts, and as additional transcripts were reviewed, we ‘constantly compared’ sections with previously coded transcripts to ensure consistent assignment of codes to similar data. We continued the process of refining codes, and describing the properties and dimensions of each, until no new concepts emerged in subsequent transcripts. As is recommended for qualitative research,21 members of our analysis team represented diverse backgrounds, including cardiovascular epidemiology, public health, health services research, and qualitative methodology. All 30 transcripts were initially coded independently by 2 team members (JL and EW) and at least one other team member (LC and NA). Independent codes were discussed in group sessions, with differences reconciled through negotiated consensus. This process generated a set of 10 primary codes and subcodes that captured major concepts in the data. The full study team reviewed the code structure for logic, breadth, and clarity twice during the analysis. Using the coded data and following established approaches to thematic development,22 we summarized the key themes and recurrent concepts that describe both the symptom experiences of women aged ≤55 years with AMI and these women's interactions with the healthcare system. This process is commonly referred to as the constant comparative method.17 We used ATLAS.ti software to facilitate data organization and retrieval.
Results
Patient Characteristics
Our sample included 30 women with a mean age of 47 years (range 30-55; Table 1). The majority of these women were white (60%), 47% were married, and 27% had a high school-level education or below. Nearly half (47%) reported full- or part-time work outside the home, 53% had health insurance, and 37% reported difficulties in accessing health care. Five themes characterized the experiences of these women with AMI in recognizing and responding to their symptoms (Figure).
Table 1.
Participant Characteristics (n=30)
| Sociodemographic, n (%) | |
| Age, mean, years (range) | 47.9 (30-55) |
| Race | |
| White | 18 (60) |
| Black | 8 (27) |
| Other | 4 (13) |
| Education ≥12 years* | 22 (73) |
| Marital status* | |
| Married | 14 (47) |
| Divorced/separated/widowed | 8 (27) |
| Single (never married) | 6 (20) |
| Working full- or part-time* | 14 (47) |
| Difficulty getting health care: extremely/moderately/somewhat* | 11 (37) |
| No health insurance* | 12 (40) |
| Avoided health care due to cost in the past year* | 11 (37) |
| General monthly finances | |
| Some money left over | 9 (30) |
| Just enough to make ends meet | 8 (27) |
| Not enough to make ends meet | 11 (37) |
| Medical History/Comorbid Conditions, n (%) | |
| Dyslipidemia | 12 (40) |
| Hypertension | 20 (67) |
| Smoking | |
| Within past month | 16 (53) |
| >1 month to 1 year ago | 2 (7) |
| Non-smoker | 12 (40) |
| Diabetes | 8 (27) |
| Prior angina | 1 (3) |
| Prior myocardial infarction | 1 (3) |
| Family history of heart disease | 20 (67) |
| Family history of diabetes | 16 (53) |
| Depression requiring treatment | 3 (10) |
Missing data for 2 participants.
Figure.
Five Themes Characterizing the Recognition and Response to Symptoms of Young Women Aged ≤55 years with Acute Myocardial Infarction
Theme 1: Prodromal symptoms of AMI varied substantially in both nature and duration
Participants in this sample described highly diverse prodromal symptoms of AMI that varied in both duration of onset and clinical presentation. Although they reported a range of symptoms, from discomfort or pain (e.g., chest, neck, jaw) to more general symptoms (e.g., sweating, anxiety, fatigue, dizziness), the vast majority reported chest pain (Table 2). Some women experienced a rapid onset of severe pain that appeared “out of the blue”. As one participant described:
“I got up...and I walked one dog at a time. It was a very easy walk, nothin’ any different than any other day...I'd come in for the fourth dog, and that's when it just hit me. My chest just started hurtin’ real bad. It was like a cinder block in the center of my chest. I had radiating burning in both armpits, like acid was in my blood...and it shot down both arms and out both fingertips...I'd had the excruciating pain in my chest for a good 35 minutes solid. You know, hyperventilating, hot sweat, and I knew it was definitely something with my heart.” (Patient #23, white, age 49)
Table 2.
Symptoms Reported by Participants (n=30)
| Discomfort or Pain, n (%) | |
| Chest (including pressure and heaviness) | 28 (93) |
| Arms/hands | 20 (67) |
| Back | 11 (37) |
| Jaw | 8 (27) |
| Shoulders/shoulder blades | 8 (27) |
| Neck | 4 (13) |
| Legs | 3 (10) |
| Throat | 2 (7) |
| General Symptoms, n (%) | |
| Shortness of breath/dyspnea | 17 (57) |
| Fatigue/exhausted | 11 (37) |
| Indigestion/heartburn | 10 (33) |
| Nausea/vomiting | 9 (30) |
| Anxiety/anxious/stress/emotional | 9 (30) |
| Sweating/diaphoresis | 7 (23) |
| Hot/flushed | 4 (13) |
| Dizziness/lightheadedness/fainting | 3 (10) |
| Weakness | 3 (10) |
| Headache | 2 (7) |
| Loss of motor function | 2 (7) |
| Palpitations/heart racing | 1 (3) |
Other women reported more nuanced and subtle symptoms, feeling like “something was off”. These symptoms would pass or recur and build over days, weeks, and even months prior to the AMI event. One woman recalled that she had experienced specific symptoms repeatedly during the past several years, both at work and at home:
“It was just another normal night...And I was just layin’ in the bed and noticed that my head was sweatin’ and I had to throw up. Went into the bathroom and did that. Came back and my hand started tinglin’. My left arm started to hurt. It went up underneath my armpit and up into my jaw. And what I didn't realize at the time is I've had these same symptoms probably five times in the past 5 years. It would just happen out of nowhere. I had a couple of ‘em while I was at work. And the other two, the other two or three were probably at night here at the house.” (Patient #27, white, age 47)
Theme 2: Women aged ≤55 years with AMI did not accurately assess personal risk of heart disease and commonly attributed symptoms to non-cardiac causes
When asked to reflect on their health prior to their AMI, participants acknowledged that they had not recognized their personal risk of heart disease. This lack of awareness occurred even among women who had a family history of heart disease or multiple known risk factors:
“...We have a lot of heart disease in our family. My father died of a heart attack. My grandfather died of a heart attack, on both sides...I have a physical every year. I have a mammogram every year...I just never put it all together. I didn't even think about them all dyin’ of a heart attack until I was sittin’ there goin’ over the history with them at the hospital...and my mom, she made the first statement, we have a lot of that in our family. And I was like, oh God, I guess we do.” (Patient #22, white, age 47)
Participants did not consider heart disease as the potential underlying cause of common symptoms such as muscle pain, indigestion, or fatigue. Some women perceived this disconnect as a consequence of their young age while others reported that their concern for a chronic health condition precluded considering the possibility of heart disease:
“I had no idea that it would be heart related. I thought it was totally related to my diabetes, ‘cause I had taken my blood sugar and it was way, sky high. And that's what I was relating it to...And my blood pressure being so high...it runs in my family...my father had heart problems at 45...so I've been aware of the problem. But not thinking it was gonna happen myself...because basically I've been diabetic for 32 years.” (Patient #12, white, age 53)
Misattribution of symptoms to other causes was also reinforced by influential external sources, including health professionals and the popular media. Women described having symptoms that differed significantly from their expectations of AMI as portrayed by the media, noting theirs was “not a Hollywood heart attack”:
“The [doctor's] words to me were acid reflux mimics a heart attack. That's exactly what they told me. They said acid reflux has the same signs as a heart attack with the pain in the chest, the jaw...And then throughout, until this last time, anytime that it happened, [I] thought, okay, acid reflux.” (Patient #21, white, age 51)
Everything I'd heard was...if you have pain shooting down, radiating down your left arm...And I didn't know that it could involve your jaw and stuff...I didn't have any of the typical heart attack symptoms that you always hear about on TV and the ER hospital shows...if you're taught that watching television all the time, then that's what you come to expect, and then when you're really having a heart attack, you're going, “Well, no that's not a heart attack because that's not the way it was on ER.” (Patient #5, white/black, age 49)
Theme 3: Women aged ≤55 years with AMI weighed competing and sometimes conflicting priorities as they recognized symptoms and decided to seek acute care
Women reported processing multiple considerations as they appraised their symptoms and tried to decide when and how to respond. They attributed their hesitation to initiate emergency care to a range of complex factors, some of which were unrelated to their personal health. Family and work responsibilities, as well as concerns about how family members would respond to their change in health status, persisted even as they experienced escalating symptoms:
“I said, ‘I really just don't feel good.’ But no, I didn't say, ‘I'm having chest pains.’ I probably had too much to do. I know I had too much to do to be wimpy about being sick. I have always been like that...I have worked through fevers. I have worked through the flu. Just feeling like I've got to get the job done. You'd think I was President of the United States. You know, we run households. We work businesses...We mop the floor. I stay up ‘till two or three o'clock in morning...to make it all happen.” (Patient #9, white, age 47)
Participants described feeling anxious about what would happen if they initiated a false alarm. A recurrent theme was a fear of being perceived as hypochondriacal if they were in fact not having a heart attack. One participant described a sense of relief when the nurse confirmed she had had an AMI:
“I felt so stupid laying in the ER...the nurse comes in and goes, ‘all your lab work, everything looks great’...and I burst into tears like I'm so embarrassed...The nurse comes in about 20 minutes later and goes, ‘we need to move you to ICU...you've had a heart attack.’ But it was a sense of relief...I was tryin’ to justify it. I was mortified...I felt like, oh my gosh, what are these people in the ER thinking of me? That here I am, a CRNA [Certified Registered Nurse Anesthetist], and I'm so stupid, you know, like a hypochondriac...I thought there's no possible way I can be having a heart attack...I've just skied six days, hard, no chest pain, I exercise, I'm healthy as a horse...and I'm not gonna go in and be embarrassed by having them tell me it was a gas bubble.” (Patient #13, white, age 47)
Women discussed relying on strategies for self-care to treat their symptoms until they reached a threshold they could no longer tolerate. These women's often prolonged efforts at self-care were supported by prior experiences with similar symptoms and, in some instances, were reinforced by others present at the time of presentation:
“I went to the emergency room and they had told me...that I had acid reflux. They gave me something called the GI cocktail. It calmed it. I stayed there about four and a half, maybe five hours I came home, they gave me a pain pill Vicodin. And told me to continue to take the Prevacid that the other doctor had prescribed for me and to take the Vicodin if I had any pain...that Thursday I was fine up until about six fifteen in the evening...and that's when the pain hit me...I took a Pepcid AC and it didn't do anything...the longer I waited the worse the pain was getting, so I...had someone to take me to the hospital.” (Patient #4, white, age 45)
In recounting the AMI event, participants consistently noted the involvement of others in both the assessment of symptoms and decisions about responding. Corroboration that the symptoms were consistent with AMI prompted action and instilled confidence to engage the system. Other women reported delegating the decision to take action to others:
“I wouldn't [have] even known...once I told [my niece], I'm getting a pain in my jaw and then I just started...a dry heave. And she was tellin’ me, ‘That's not acid reflux. You're havin’ a heart attack.’ So I'm like, alrighty then.” (Patient #21, white, age 51)
Although most women described a process of weighing various factors as they decided whether to seek medical attention, several participants recognized that they were experiencing symptoms of heart attack and were proactive in seeking care:
“That was my biggest thing is that I was real nauseated, but when I started feeling my hand tingle and my arm kind of go to sleep and my ear hurt and my jaw hurt, I said, I've heard all of those symptoms, and those are all classic symptoms of heart problems, so I thought, well, I'd be a fool not to check it out.” (Patient #15, white/Hispanic/Latino, age 53)
Theme 4: The healthcare system was not consistently responsive to these younger women with AMI, resulting in delays in workup and diagnosis
Participants described encounters with the healthcare system (primary care and emergency health services) during symptom presentation in which they did not receive a prompt or complete workup for their AMI symptoms or a formal diagnosis. Such encounters occurred with presentation of both typical and atypical acute symptoms:
“I remember callin’ a doctor and tellin’ him I was having these chest pains and all that stuff, and they just scheduled a regular appointment for me...I would not know that I'm havin’ a heart attack...I would consider that your [the doctor's] responsibility...they should of pushed me in faster...It was like a 5 day wait ‘til I got into the doctor.” (Patient #22, white, age 47)
“I think the Friday before I had the heart attack...I had the heart attack on the Sunday...I went to the doctor because I had pains in my legs and my ankles were swollen and my hands were swollen. And I was just tired all the time and he felt my leg and thought it was a shin splint and then he put me on a new blood pressure medication. He said my blood pressure was up. And then that Sunday I had a heart attack.” (Patient #2, white, age 48)
In some instances, the initial evaluation was negative for heart conditions and multiple interactions were required to make a diagnosis of AMI, sometimes within a short timeframe:
“At first it was just pain in my shoulders and I thought maybe I had slept wrong. But then when the heart palpitations started coming...then I got concerned and then I went to the hospital...then they said, well, they didn't find anything life threatening anyway, which kind of upset me. They did the EKG. They didn't find anything. They did the CAT scan on my chest. They didn't find anything. It wasn't until I went back on the 31st that they had found anything.” (Patient #11, white/black, age 31)
Theme 5: Women aged ≤55 with AMI did not routinely access primary care, including preventive care for heart disease
Although interviews focused on acute care interactions, we also asked participants about their prior experiences with the primary healthcare system. Women described limited and sporadic connections with primary care for general health maintenance and the prevention of heart disease. Reasons for this disengagement were both internally and externally motivated. Internal factors included anxiety about being perceived as complaining about minor concerns, determination to “power through” illness, preferences for self-care, and work and family demands taking priority:
“...my mom is kind of a hypochondriac...and my sister and I have dealt with this for years...we are so afraid that we will be that way that we just kind of...And that was what I kept thinking in the back of my mind is, if it's really, really bad, my body would be telling me more than just this...I just didn't want to be one of those people who just, oh, I've got a pain, and run to the doctor. And that was part of my denial.” (Patient #18, white, age 45)
“I'm terrible about procrastinating. And I see it's a bad thing to do. But that's me. You know, I'm tryin’ to be as honest as I can. And that's about the best I can tell you...I did have health insurance when I worked over at the assisted living place. I just never took the time. I was working about 16 hours a day over there, too, and it's kind of hard to find time to go to the doctor and sleep and work.” (Patient #25, white, age 54)
External influences that prevented women from obtaining routine primary care included prior negative experiences with healthcare providers (e.g., poor physician-patient relationships, feeling rebuffed or treated with disrespect, being denied care). Although some women reported that lack of insurance precluded routine and preventive care, no women indicated that financial factors prevented them from seeking emergent care for AMI:
“Usually I feel kind of embarrassed...I can't go and get the proper care like I want because of my financial conditions. And then maybe some things, I could be more comfortable talking to a lady doctor than a man...I get nervous when I try to explain the condition...I just be glad to, if I could see a doctor, I don't want to be choosy. Basically I don't have the correct funds or anything, so I just, whatever doctor that will see me, I just let it go at that.” (Patient #8, white/black/Native American, age 53)
In contrast, two participants described proactively seeking routine care to monitor their risk factors for heart disease:
“I have such a strong parental history of it [heart disease]...So they actually watched me quite carefully to make sure that after I hit 40, that I wasn't severely overweight, that I didn't seem to have tachycardia, that I didn't have shortness of breath...It wasn't being ignored.” (Patient #24, white, age 48)
“...I had just moved to [city, state] and I had a doctor, because of my high cholesterol, just kind of wanted to do a stress test. So they did that where they induce the heart attack...But my heart was fine...And then I had moved here and I found a new doctor and probably less than a year ago, he did a sonogram of my heart. And found nothing. Because again, I go in and my cholesterol is always so high, it scares the doctors...but he said, oh, you're fine, and I said okay. I am one not to run to the doctor for everything. But when I feel like that my body's just not right then I definitely go.” (Patient #28, white, age 53)
Discussion
Several recurrent themes characterized the experiences of the young women in our study (aged 30-55 years) as they recognized and responded to their AMI symptoms. Participants reported highly nuanced symptoms that did not cohere with the representation of heart attacks common in the lay media or with their understanding of current scientific evidence from healthcare providers. The women commonly attributed symptoms to non-cardiac causes and dismissed personal risk factors including family history of heart disease. The lack of responsiveness of the healthcare system further complicated both preventive care and acute treatment of these young women with AMI.
The presence of atypical AMI symptoms in women may contribute to delays in care-seeking behavior. Prior studies of older populations suggest that women may experience a range of prodromal and acute symptoms,11,23-25 and they may have more atypical symptoms than men.10,26-30 In general, these studies found that even though the vast majority of patients present with the hallmark symptom of chest pain, women were less likely to experience chest pain and more likely to present with other symptoms, such as pain or discomfort in the back, jaw, or throat as well as headache, nausea, and coughing. Reports from the National Registry of Myocardial Infarction31 and a Canadian cohort of patients aged ≤55 years with acute coronary syndrome32 support these patterns. Although >80% of patients younger than 55 years in these studies presented with chest pain, the young women were more likely to present without chest pain than the men. Our study participants described diverse prodromal symptoms of AMI that predominantly included chest pain but also included atypical and diffuse symptoms. Recognizing prodromal symptoms is important, as they were associated with acute symptoms and subsequent cardiac events in prior studies.24,33,34 In many instances, our participants described attributing symptoms to non-cardiac causes due to their nature and duration, in part because of a lack of public media examples that depict atypical symptoms, particularly among younger women. Stereotypic depiction of heart attack symptoms based on common profiles among men may lead women to characterize atypical symptom as non-cardiac in origin. Misattribution of cardiac symptoms to non-cardiac causes may warrant particular attention in younger populations (e.g., those aged ≤55 years) that may be even less likely to attribute aberrant symptoms to the risk of heart disease.
Participants in our study reported that preventive cardiac care was not a priority due to a variety of competing demands and circumstances. The perception of several women that preventive cardiac care was not a priority due to current age may warrant special attention in this population. Studies examining the prevalence of multiple risk factors have generally shown that 50% to 60% of AMI patients present with at least two factors, and 20% to 30% present with at least three.35,36 A more recent study reported prevalence rates among women aged <55 years with AMI of 70% to 80% for two or more risk factors and 44% to 54% for three or more factors.37 Many of our participants discussed a strong family history of heart disease and discussed their own risk factors for heart disease, but they did not connect these to their own cardiac risk. The misperception that young women with a strong family history of cardiac disease and the presence of traditional cardiovascular risk factors are not likely to have heart disease because of their age indicates a critical need to develop targeted educational campaigns for these women to prioritize their own health in terms of managing traditional risk factors, particularly within the context of familial history.
Women tend to delay longer in seeking prompt care than men;38 however, the paucity of qualitative research about premonitory and acute symptoms and their role on care-seeking behavior, especially among younger age groups, represents a notable gap in the literature.31 Consistent with findings derived from older populations, our patients aged 30-55 years with AMI reported lack of awareness of personal risk, misattribution of symptoms, waiting for symptoms to worsen, and self-medicating as factors contributing to delays.6,12,39-45 Participants also cited competing family and work responsibilities as causes for delay, which may represent additional domains that are unique to this younger population.
Concerns about inappropriately engaging the healthcare system and wanting external corroboration of symptoms prior to taking action have been shown in older populations.12 Such concerns may be further heightened in younger women as cardiac events are less common, and many participants in our study cited their age as a reason they did not think they were at risk for heart disease. Identifying strategies to empower women to recognize prodromal symptoms and seek care without stigma or perceived judgment may be particularly critical for young women at increased risk for heart disease.
Finally, the healthcare system faces particular challenges in diagnosing women with AMI, even when women present in a timely manner.12 The decreased probability of having an AMI at a younger age (e.g., ≤55 years) likely contributes to initial triage strategies to attribute symptoms to non-cardiac conditions. Our participants described delays that occurred for both typical and atypical symptoms as well as delays within the physician's office and the emergency department. Consistent with our results, a prior qualitative study of AMI patients noted that a 56-year-old woman presenting with symptoms was told that she was too young to be experiencing a heart attack.46 A number of our participants discussed having inconclusive results for cardiac diagnostic tests in the acute setting, only to return with an AMI within a short period of time. Atypical AMI presentation in young women, in terms of diagnostic test results, warrants further research attention, as it may contribute to delays in the diagnosis and receipt of care.
Although our work provides important and novel insights into the experiences of young women with AMI, there are several limitations. Participants were selected from an ongoing observational study. Although TRIUMPH participants were enrolled from diverse clinical centers across the country, results from our interviews may not reflect the experiences of women treated at other clinical centers. Not all contacted participants agreed to enroll; reasons for non-participation included no response to telephone contacts (N=9), inability to contact due to changes in living locations (N=1), and patients being rehospitalized or too ill at the time of contact (N=3). However, basic demographic characteristics were comparable between those participants identified and those successfully interviewed. Recall bias is possible as we interviewed participants after their AMI hospitalizations. We tried to minimize this bias by conducting interviews within 2 weeks of the AMI and by using probing techniques to recall a spectrum of factors associated with participants’ experiences and delays. In addition, we used several recommended strategies20 to ensure data reliability, including consistent use of the discussion guide, audio-taping interviews, independent transcript preparation, standardized coding and analysis of the data using software, and maintenance of materials necessary to achieve auditability.47
Given that AMI is a leading cause of death among young women, generating hypotheses about potential factors that shape these women's care-seeking behaviors is essential for the development of targeted interventions to improve prompt patient presentation and timely, accurate AMI diagnosis. Results from this qualitative study provide novel insights about perceptions and gaps in action for women aged ≤55 years, and they have informed the development of a quantitative instrument to assess aspects of symptom recognition and perceived delays in a large, prospective study of young patients with AMI.48 Identifying opportunities to improve the detection of symptoms and receipt of timely acute care represents an important target for healthcare providers and researchers seeking to improve outcomes for young women with AMI.
Supplementary Material
Acknowledgments
Sources of Funding
The study was funded by the Fannie E. Rippel Foundation and grants R01 HL081153 and P50 HL077113 from the National Heart, Lung, and Blood Institute.
Footnotes
Disclosures
None.
References
- 1.National Center for Health Statistics . Health, United States, 2012: With Special Feature on Emergency Care. Hyattsville, MD: 2012. [PubMed] [Google Scholar]
- 2.Vaccarino V, Horwitz RI, Meehan TP, Petrillo MK, Radford MJ, Krumholz HM. Sex differences in mortality after myocardial infarction: Evidence for a sex-age interaction. Arch Intern Med. 1998;158:2054–2062. doi: 10.1001/archinte.158.18.2054. [DOI] [PubMed] [Google Scholar]
- 3.Vaccarino V, Parsons L, Every NR, Barron HV, Krumholz HM. Sex-based differences in early mortality after myocardial infarction. National Registry of Myocardial Infarction 2 participants. N Engl J Med. 1999;341:217–225. doi: 10.1056/NEJM199907223410401. [DOI] [PubMed] [Google Scholar]
- 4.Vaccarino V, Krumholz HM, Yarzebski J, Gore JM, Goldberg RJ. Sex differences in 2-year mortality after hospital discharge for myocardial infarction. Ann Intern Med. 2001;134:173–181. doi: 10.7326/0003-4819-134-3-200102060-00007. [DOI] [PubMed] [Google Scholar]
- 5.Vaccarino V, Parsons L, Peterson ED, Rogers WJ, Kiefe CI, Canto J. Sex differences in mortality after acute myocardial infarction: Changes from 1994 to 2006. Arch Intern Med. 2009;169:1767–1774. doi: 10.1001/archinternmed.2009.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DeVon HA, Saban KL, Garrett DK. Recognizing and responding to symptoms of acute coronary syndromes and stroke in women. J Obstet Gynecol Neonatal Nurs. 2011;40:372–382. doi: 10.1111/j.1552-6909.2011.01241.x. [DOI] [PubMed] [Google Scholar]
- 7.Albarran JW, Clarke BA, Crawford J. 'It was not chest pain really, I can't explain it!' An exploratory study on the nature of symptoms experienced by women during their myocardial infarction. J Clin Nurs. 2007;16:1292–1301. doi: 10.1111/j.1365-2702.2007.01777.x. [DOI] [PubMed] [Google Scholar]
- 8.King KB, McGuire MA. Symptom presentation and time to seek care in women and men with acute myocardial infarction. Heart Lung. 2007;36:235–243. doi: 10.1016/j.hrtlng.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 9.Richards HM, Reid ME, Watt GC. Why do men and women respond differently to chest pain? A qualitative study. J Am Med Womens Assoc. 2002;57:79–81. [PubMed] [Google Scholar]
- 10.Lovlien M, Schei B, Hole T. Women with myocardial infarction are less likely than men to experience chest symptoms. Scand Cardiovasc J. 2006;40:342–347. doi: 10.1080/14017430600913199. [DOI] [PubMed] [Google Scholar]
- 11.McSweeney JC. Women's narratives: Evolving symptoms of myocardial infarction. J Women Aging. 1998;10:67–83. doi: 10.1300/J074v10n02_06. [DOI] [PubMed] [Google Scholar]
- 12.McSweeney JC, Lefler LL, Crowder BF. What's wrong with me? Women's coronary heart disease diagnostic experiences. Prog Cardiovasc Nurs. 2005;20:48–57. doi: 10.1111/j.0889-7204.2005.04447.x. [DOI] [PubMed] [Google Scholar]
- 13.Lockyer L. Women's interpretation of their coronary heart disease symptoms. Eur J Cardiovasc Nurs. 2005;4:29–35. doi: 10.1016/j.ejcnurse.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 14.Arnold SV, Chan PS, Jones PG, Decker C, Buchanan DM, Krumholz HM, Ho PM, Spertus JA, for the Cardiovascular Outcomes Research Consortium Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients' Health Status (TRIUMPH): Design and rationale of a prospective multicenter registry. Circ Cardiovasc Qual Outcomes. 2011;4:467–476. doi: 10.1161/CIRCOUTCOMES.110.960468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pope C, Mays N. Reaching the parts other methods cannot reach: An introduction to qualitative methods in health and health services research. BMJ. 1995;311:42–45. doi: 10.1136/bmj.311.6996.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Curry LA, Nembhard IM, Bradley EH. Qualitative and mixed methods provide unique contributions to outcomes research. Circulation. 2009;119:1442–1452. doi: 10.1161/CIRCULATIONAHA.107.742775. [DOI] [PubMed] [Google Scholar]
- 17.Glaser BG, Strauss AL. The Discovery of Grounded Theory; Strategies for Qualitative Research. Aldine Pub. Co.; Chicago: 1967. [Google Scholar]
- 18.Patton MQ. Qualitative Research and Evaluation Methods. Sage Publications; Thousand Oaks, CA: 2002. [Google Scholar]
- 19.Morse JM. The significance of saturation. Qual Health Res. 1995;5:147–149. [Google Scholar]
- 20.Crabtree BF, Miller WL. Doing Qualitative Research. 2nd ed. Sage Publications; Thousand Oaks: 1999. [Google Scholar]
- 21.Mays N, Pope C. Rigour and qualitative research. BMJ. 1995;311:109–112. doi: 10.1136/bmj.311.6997.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: Developing taxonomy, themes, and theory. Health Serv Res. 2007;42:1758–1772. doi: 10.1111/j.1475-6773.2006.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McSweeney JC, Cody M, Crane PB. Do you know them when you see them? Women's prodromal and acute symptoms of myocardial infarction. J Cardiovasc Nurs. 2001;15:26–38. doi: 10.1097/00005082-200104000-00003. [DOI] [PubMed] [Google Scholar]
- 24.McSweeney JC, Cody M, O'Sullivan P, Elberson K, Moser DK, Garvin BJ. Women's early warning symptoms of acute myocardial infarction. Circulation. 2003;108:2619–2623. doi: 10.1161/01.CIR.0000097116.29625.7C. [DOI] [PubMed] [Google Scholar]
- 25.McSweeney JC, Crane PB. Challenging the rules: Women's prodromal and acute symptoms of myocardial infarction. Res Nurs Health. 2000;23:135–146. doi: 10.1002/(sici)1098-240x(200004)23:2<135::aid-nur6>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 26.Arslanian-Engoren C, Patel A, Fang J, Armstrong D, Kline-Rogers E, Duvernoy CS, Eagle KA. Symptoms of men and women presenting with acute coronary syndromes. Am J Cardiol. 2006;98:1177–1181. doi: 10.1016/j.amjcard.2006.05.049. [DOI] [PubMed] [Google Scholar]
- 27.Chen W, Woods SL, Wilkie DJ, Puntillo KA. Gender differences in symptom experiences of patients with acute coronary syndromes. J Pain Symptom Manage. 2005;30:553–562. doi: 10.1016/j.jpainsymman.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 28.Culic V, Eterovic D, Miric D, Silic N. Symptom presentation of acute myocardial infarction: Influence of sex, age, and risk factors. Am Heart J. 2002;144:1012–1017. doi: 10.1067/mhj.2002.125625. [DOI] [PubMed] [Google Scholar]
- 29.Goldberg R, Goff D, Cooper L, Luepker R, Zapka J, Bittner V, Osganian S, Lessard D, Cornell C, Meshack A, Mann C, Gilliland J, Feldman H. Age and sex differences in presentation of symptoms among patients with acute coronary disease: The REACT trial. Rapid Early Action for Coronary Treatment. Coron Artery Dis. 2000;11:399–407. doi: 10.1097/00019501-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Meischke H, Larsen MP, Eisenberg MS. Gender differences in reported symptoms for acute myocardial infarction: Impact on prehospital delay time interval. Am J Emerg Med. 1998;16:363–366. doi: 10.1016/s0735-6757(98)90128-0. [DOI] [PubMed] [Google Scholar]
- 31.Canto JG, Rogers WJ, Goldberg RJ, Peterson ED, Wenger NK, Vaccarino V, Kiefe CI, Frederick PD, Sopko G, Zheng ZJ. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. JAMA. 2012;307:813–822. doi: 10.1001/jama.2012.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Khan NA, Daskalopoulou SS, Karp I, Eisenberg MJ, Pelletier R, Tsadok MA, Dasqupta K, Norris CM, Pilote L, GENESIS PRAXY Team Sex differences in acute coronary syndrome symptom presentation in young patients. JAMA Intern Med. 2013;173:1863–1871. doi: 10.1001/jamainternmed.2013.10149. [DOI] [PubMed] [Google Scholar]
- 33.McSweeney J, Cleves MA, Fischer EP, Moser DK, Wei J, Pettey C, Rojo MO, Armbya N. Predicting coronary heart disease events in women: A longitudinal cohort study. J Cardiovasc Nurs. 2014;29:482–492. doi: 10.1097/JCN.0b013e3182a409cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O'Keefe-McCarthy S, Ready L. Impact of prodromal symptoms on future adverse cardiac-related events: A systematic review. J Cardiovasc Nurs. doi: 10.1097/JCN.0000000000000207. Epub ahead of print November 21, 2014; doi: 101097/JCN.0000000000000207. [DOI] [PubMed] [Google Scholar]
- 35.Gerber Y, Weston SA, Killian JM, Jacobsen SJ, Roger VL. Sex and classic risk factors after myocardial infarction: A community study. Am Heart J. 2006;152:461–468. doi: 10.1016/j.ahj.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 36.Canto JG, Kiefe CI, Rogers WJ, Peterson ED, Frederick PD, French WJ, Gibson CM, Pollack CV, Jr., Ornato JP, Zalenski RJ, Penney J, Tiefenbrunn AJ, Greenland P. Number of coronary heart disease risk factors and mortality in patients with first myocardial infarction. JAMA. 2011;306:2120–2127. doi: 10.1001/jama.2011.1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Leifheit-Limson EC, Spertus JA, Reid KJ, Jones SB, Vaccarino V, Krumholz HM, Lichtman JH. Prevalence of traditional cardiac risk factors and secondary prevention among patients hospitalized for acute myocardial infarction (AMI): Variation by age, sex, and race. J Womens Health (Larchmt) 2013;22:659–666. doi: 10.1089/jwh.2012.3962. [DOI] [PubMed] [Google Scholar]
- 38.Nguyen HL, Gore JM, Saczynski JS, Yarzebski J, Reed G, Spencer FA, Goldberg RJ. Age and sex differences and 20-year trends (1986 to 2005) in prehospital delay in patients hospitalized with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2010;3:590–598. doi: 10.1161/CIRCOUTCOMES.110.957878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mochari-Greenberger H, Miller KL, Mosca L. Racial/ethnic and age differences in women's awareness of heart disease. J Womens Health (Larchmt) 2012;21:476–480. doi: 10.1089/jwh.2011.3428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moser DK, Kimble LP, Alberts MJ, Alonzo A, Croft JB, Dracup K, Evenson KR, Go AS, Hand MM, Kothari RU, Mensah GA, Morris DL, Pancioli AM, Riegel B, Zerwic JJ. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: A scientific statement from the American Heart Association Council on Cardiovascular Nursing and Stroke Council. Circulation. 2006;114:168–182. doi: 10.1161/CIRCULATIONAHA.106.176040. [DOI] [PubMed] [Google Scholar]
- 41.Arslanian-Engoren C. Treatment-seeking decisions of women with acute myocardial infarction. Women Health. 2005;42:53–70. doi: 10.1300/j013v42n02_04. [DOI] [PubMed] [Google Scholar]
- 42.Banks AD, Dracup K. Factors associated with prolonged prehospital delay of African Americans with acute myocardial infarction. Am J Crit Care. 2006;15:149–157. [PubMed] [Google Scholar]
- 43.Harralson TL. Factors influencing delay in seeking treatment for acute ischemic symptoms among lower income, urban women. Heart Lung. 2007;36:96–104. doi: 10.1016/j.hrtlng.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 44.Moser DK, McKinley S, Dracup K, Chung ML. Gender differences in reasons patients delay in seeking treatment for acute myocardial infarction symptoms. Patient Educ Couns. 2005;56:45–54. doi: 10.1016/j.pec.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 45.Rosenfeld AG, Lindauer A, Darney BG. Understanding treatment-seeking delay in women with acute myocardial infarction: Descriptions of decision-making patterns. Am J Crit Care. 2005;14:285–293. [PubMed] [Google Scholar]
- 46.Schoenberg NE, Peters JC, Drew EM. Unraveling the mysteries of timing: Women's perceptions about time to treatment for cardiac symptoms. Soc Sci Med. 2003;56:271–284. doi: 10.1016/s0277-9536(02)00026-6. [DOI] [PubMed] [Google Scholar]
- 47.Sandelowski M. The problem of rigor in qualitative research. ANS Adv Nurs Sci. 1986;8:27–37. doi: 10.1097/00012272-198604000-00005. [DOI] [PubMed] [Google Scholar]
- 48.Lichtman JH, Lorenze NP, D'Onofrio G, Spertus JA, Lindau ST, Morgan TM, Herrin J, Bueno H, Mattera JA, Ridker PM, Krumholz HM. Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients (VIRGO) study design. Circ Cardiovasc Qual Outcomes. 2010;3:684–693. doi: 10.1161/CIRCOUTCOMES.109.928713. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.