Abstract
This article reports on the development of a manualized occupational therapy intervention for diabetes management. An initial theoretical framework and core content areas for a Stage 1 intervention manual were developed based on an in-depth needs assessment and review of existing literature. After evaluation by a panel of experts and completion of a feasibility study, the intervention was revised into a Stage 2 manual in preparation for a randomized study evaluating the intervention’s efficacy. In developing the initial manual, we delineated core theoretical principles to allow for flexible application and tailoring of the intervention’s content areas. Expert panel feedback and feasibility study results led to changes to the intervention structure and content as we developed the Stage 2 manual. Through describing this process, we illustrate the dynamic evolution of intervention manuals, which undergo revisions due to both theoretical and practical considerations at each stage of the research-to-clinical practice pipeline.
Keywords: feasibility studies, disease management, self-care
In the current health care climate that demands empirical evidence to support clinical practice, there has been a distinct movement toward enhancing the replicability of therapeutic interventions through the use of manuals, protocols, and other strategies to maintain intervention fidelity (Murphy & Gutman, 2012). Blanche, Fogelberg, Diaz, Carlson, and Clark (2011) argued that an “urgent need exists for occupational therapy researchers and practitioners to understand the role of manualized interventions in [research and] clinical practice” (p. 712). Although treatment manuals and other fidelity-monitoring strategies create a reproducible structure for intervention implementation, they have also been critiqued as minimizing the role of clinical reasoning, inhibiting therapist empathy, being inflexible, and being limited in their theoretical basis, which does not reflect the eclectic use of multiple theoretical frameworks in clinical practice (Blanche et al., 2011; Cukrowicz et al., 2011; Waller et al., 2013). In addition, there is not yet unequivocal evidence regarding the efficacy of manualized interventions; while many studies have shown superior therapeutic outcomes using manualized interventions as compared with non-manualized interventions (e.g., Cukrowicz et al., 2011; Robbins et al., 2011; Rossouw & Fonagy, 2012), others have found similar effects in manualized versus non-manualized interventions (e.g., Horigian et al., 2013).
Despite these potential limitations, intervention manuals remain necessary as a means to facilitate rigorous and systematic evaluation of therapeutic interventions, thereby providing evidence to justify our treatments to third-party payers and other stakeholders (Murphy & Gutman, 2012). In addition, they are a useful tool to translate effective intervention strategies across practice settings. As such, our challenge is to identify strategies to ameliorate the potential limitations of manualized interventions with respect to flexibility and therapeutic use of self.
A critical function of treatment manuals is to facilitate the translation of interventions from research into clinical practice. One model of manual development, outlined by Carroll and Nuro (2002), details the structure and function of treatment manuals at each stage of this research to practice intervention pipeline. Their approach recognizes that, while all treatment manuals should incorporate certain elements (such as intervention content, mode of delivery, dose, and setting of the intervention; Des Jarlais, Lyles, Crepaz, & TREND Group, 2004), a manual’s level of complexity evolves through various stages of the research process, with each stage incorporating greater complexity and a more explicit framework to guide clinical practice. Stage 1 manuals provide an initial specification of intervention techniques, goals, structure, format, and theoretical mechanisms, to guide pilot and feasibility studies. Stage 2 manuals, used in large-scale efficacy studies, add therapist selection, training, and supervision criteria; differences between the manualized intervention and other approaches; and processes to evaluate intervention fidelity. Stage 3 manuals, used to disseminate interventions shown to be successful in research settings into clinical practice, include all of the above, as well as strategies to tailor the intervention for different patient groups, settings, and formats.
In this article, we report on the process of developing a manualized occupational therapy intervention addressing diabetes management in young adults. We will describe our strategies for drafting a Stage 1 manual, implementing a feasibility study, and refining the intervention in a Stage 2 manual in preparation for a randomized study to evaluate the efficacy of the intervention. In describing this process, we aim to share with other clinicians and researchers our methods for developing intervention materials and strategies for addressing the potential drawbacks inherent to manualized interventions (such as a lack of flexibility and inattention to the client–therapist relationship).
At its outset, the intervention we describe was conceptualized as an iteration of the occupational therapy intervention approach known as Lifestyle Redesign. This approach, previously used in two large-scale research programs, the Well Elderly and Pressure Ulcer Prevention Studies (Clark et al., 1997; Clark et al., 2012; Clark et al., 2014), also serves as the overarching intervention framework for an outpatient occupational therapy practice at the University of Southern California (USC Occupational Therapy Faculty Practice, n.d.). Lifestyle Redesign is characterized by three primary features. First, occupation is conceptualized as an emergent phenomenon: It cannot be fully understood by analyzing its individual elements (e.g., physical and cognitive requirements, physical environment, and sociocultural context) in a reductionist manner. Second, life history and personal themes of meaning, or the ways people understand and make sense of their lives, are incorporated into intervention goals and strategies, such that occupations that are most meaningful and relevant within a particular client’s life context are used therapeutically in the intervention. Finally, the intervention teaches occupational self-analysis, through providing clients with tools to examine their lifestyles and integrate sustainable, health-promoting changes into their everyday habits and routines (Jackson, Carlson, Mandel, Zemke, & Clark, 1998). The intervention we developed, called REAL: Resilient, Empowered, Active Living with Diabetes, was informed by these principles, research on efficacious diabetes self-management strategies, and our findings of an in-depth needs assessment among the target population (Pyatak, Florindez, & Weigensberg 2013; Pyatak, Florindez, Peters, & Weigensberg, 2014; Pyatak, Sequeira, Whittemore, Vigen, Peters, & Weigensberg, 2014).
Method
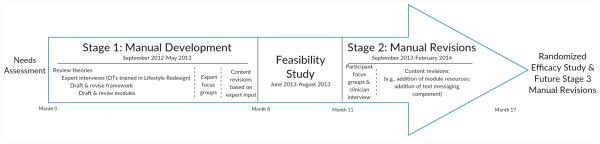
A timeline of all manual development activities is provided in Figure 1. Below, we detail the methods used for developing the Stage 1 manual, conducting a feasibility study, and completing revisions to create a Stage 2 manual for use in a randomized efficacy study.
Figure 1.
Timeline of Intervention Manual Development
Stage 1 Manual Development
Stage 1 intervention manual development incorporated three steps. First, we outlined a preliminary theoretical framework and intervention modules (content areas). The theoretical framework was developed through E.A.P.’s review of relevant health behavior theories, including social cognitive theory (Bandura, 1998), self-determination theory (Ryan & Deci, 2000), and the transtheoretical model (Prochaska, DiClemente, & Norcross, 1992), as well as interviews with four clinicians with experience implementing Lifestyle Redesign interventions. These clinicians had between 5 and 36 years of experience in a range of practice settings, including pediatric and adult physical rehabilitation, wellness and prevention, and chronic disease management. The content modules were informed by an extensive needs assessment conducted among the target population, the findings of which are outlined in Pyatak et al., 2013; Pyatak, Florindez, et al., 2014, and Pyatak, Sequeira, et al. 2014, and by E.A.P.’s review of existing interventions, including previous Lifestyle Redesign interventions (Blanche et al., 2011; Jackson et al., 1998) and the Stanford University Chronic Disease Self-Management Program and Diabetes Self-Management Program, two highly successful and widely disseminated manualized self-management interventions (K. Lorig, Ritter, Villa, & Armas, 2009; K. R. Lorig et al., 1999). An occupational therapy doctoral student (S.D.) then developed drafts of the theoretical framework and intervention modules, which were revised in an iterative process with feedback from E.A.P.
Next, the preliminary manual was reviewed during two focus groups, lasting approximately 2 hr each. A total of nine experts participated in the focus groups, including a pediatric and an adult endocrinologist, a health behavior researcher, a dietician, and five occupational therapists with experience delivering Lifestyle Redesign interventions with a variety of populations. Two of the above-identified experts were also certified diabetes educatorsâ. The sessions were led by E.A.P. and S.D. Focus group participants were asked for their input regarding the theoretical framework, the intervention’s structure and delivery (e.g., dose, frequency, setting), the planned assessment and goal-setting procedures, and the module content (including suggested goals and activities, participant handouts and resources, and therapist resources). A graduate research assistant took detailed notes during the meetings, which were also audio recorded for later review.
The research team, including E.A.P., S.D., a graduate research assistant, and two senior faculty mentors (one endocrinologist and one occupational therapist), subsequently reviewed these notes, categorized suggested revisions, and determined which to incorporate into the intervention. The major revisions at this stage included refining the study’s assessment tools, incorporating an iPad as an intervention resource to facilitate accessing websites and YouTube videos, and augmenting the intervention modules with information on specific content areas, such as diabetes and driving, how to utilize health insurance benefits, and emotional eating.
Feasibility Study
After completing the Phase 1 manual, a feasibility study was conducted to address the following aims: (a) evaluate the planned recruitment, assessment, and intervention procedures, and (b) evaluate the feasibility and acceptability of the intervention from the perspective of both the therapist and participants. The methods and results of the feasibility study are being reported in detail elsewhere (Carandang & Pyatak, 2015). In brief, eight participants aged 18 to 30 years, who had been diagnosed with either type 1 diabetes or type 2 diabetes for at least 1 year, were offered weekly occupational therapy sessions (median of 8 sessions; range = 7-12) over approximately 2 months guided by the Stage 1 manual. Because the target population was known to have poor clinic attendance, sessions were provided in participants’ homes or community settings. Participants completed pre- and post-intervention assessments, and were interviewed following study completion to solicit their views of the intervention and study procedures. The feasibility study was approved by the university’s Institutional Review Board, and all participants completed informed consent prior to engaging in study activities.
Stage 2 Manual Revisions
Following the feasibility study, further revisions were made to the intervention manual, based on three data sources: (a) interviews conducted with study participants and the treating occupational therapist, (b) treatment notes made by the occupational therapist, and (c) a log of potential revisions maintained by the research team during feasibility study implementation.
Post-intervention interviews were transcribed verbatim and entered into NVivo 10 for thematic analysis (Riessman, 2008). The coded data, along with the therapist’s treatment notes and the log of suggested revisions, were reviewed by the research team. A list of potential revisions was generated, and through discussion, the team came to consensus regarding a final set of revisions to make in the Stage 2 intervention manual. In addition to these changes, we incorporated elements into the Stage 2 manual that are not specified in a Stage 1 manual.
Results
Stage 1 Manual Development
As previously stated, the primary aims of a Stage 1 manual are the initial specification of techniques, goals, structure, format, and theoretical mechanisms of an intervention (Carroll & Nuro, 2002). In developing the Stage 1 REAL treatment manual, we aimed to address these goals while balancing the need for a well-characterized intervention with the flexibility that characterizes clinical practice. We adopted two strategies to address this challenge. First, the intervention’s theoretical framework was informed by a set of core principles derived from multiple theoretical perspectives, rather than a single theoretical lens. Second, the intervention’s structure and content were designed to be individually tailored; for example, therapists can modify the duration and frequency of sessions for each client, and do not need to deliver intervention content in a prescribed order. The intervention framework, structure, and content, as conceptualized in the Stage 1 manual, are described below.
REAL intervention framework
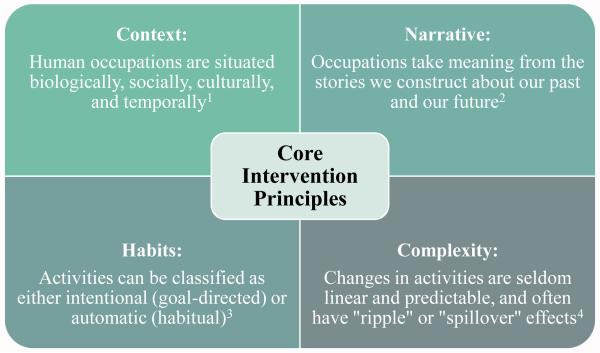
The core principles of the REAL intervention, along with clinical examples of their application in the feasibility study, are presented in Figure 2. We view these principles as creating the overarching theoretical framework of the intervention, which represents an adaptation of the original Lifestyle Redesign intervention approach. In crafting these principles that draw upon multiple theories, rather than basing the intervention on a singular theory, our aim was to develop a rich, yet flexible, theoretical basis for the intervention. We view these principles as tools to guide the intervention, with the expectation that certain principles are foregrounded, or recede into the background, depending on the clinical “puzzle” the therapist is trying to solve.
Figure 2. Core intervention principles for [redacted] intervention.
1 Mc Leroy, et al. (1988); Strong, et al. (1999)
2 Clark (1993); Frank (2006); Mattingly (1998)
3 Scobbie, Dixon, and Wyke (2011); Wood, Quinn, and Kashy (2002)
4 Resnicow and Page (2008); Wilson, Holt, & Greenhalgh (2001)
The first principle concerns the context in which human behavior occurs. The connection between person, context, and occupation is embedded in the central tenets of our profession (American Occupational Therapy Association, 2014), and features prominently in much of the field’s theoretical work on occupation (e.g., Dickie, Cutchin, & Humphry, 2006; Kielhofner & Burke, 1980; Strong et al., 1999). The REAL intervention also draws on the social-ecological model of health behavior (McLeroy, Bibeau, Steckler, & Glanz, 1988) that we view as being highly complementary to the philosophy of occupational therapy, as well as a useful tool for communication and dissemination across disciplinary boundaries. Taken together, these theories provide a useful structure for understanding the interrelationships between individuals’ body structures and functions, and their social, cultural, and built environments, as they influence human occupations.
The second principle concerns the use of narrative in the context of occupational therapy intervention. Therapists use narrative to develop an understanding of the client’s life history, including their understanding of how diabetes fits into their overall life story, drawing on Mattingly’s (1998) work in clinical reasoning and Clark’s (1993) occupational storytelling and story making. In addition, therapists use narrative as a communication strategy, which has been shown to be an efficacious means of persuasion and conveying information in health care contexts (e.g., Lemal & Van den Bulck, 2010; Mishali, Sominsky, & Heymann, 2010).
The third principle concerns the distinction between goal-directed and habitual actions, and selection of appropriate intervention strategies for each mode of activity. Goal-directed actions occur when we explicitly aim to perform a given activity. In contrast, habitual actions are those we perform without conscious thought. Nearly half of our everyday activities are driven by habit (Wood, Quinn, & Kashy, 2002), and many of these activities are relevant to health. The REAL intervention draws on the emerging body of habit research to help clients develop and maintain healthful habits (such as taking medications) and break potentially harmful habits (such as excess sweetened beverage consumption).
The fourth principle concerns our understanding of individuals as complex systems. Complexity theory has been identified as particularly relevant to diabetes care, given that blood glucose control is “a classic example of a complex adaptive system” (Cooper & Geyer, 2009, p. 762). Complexity theory is highly congruent with the principles outlined above concerning context, narrative, and habits versus goal-directed activities. We therefore view complexity theory as an overarching principle, providing a coherent framework for the application of the previously described principles. Complexity theory aims to explain the behaviors of complex systems, which have emergent properties, such that the whole is greater than the sum of its parts. Complex systems tend to have overarching behavioral patterns and a capacity for self-organization, which at the level of an individual person, may be seen as analogous to habits and routines. This provides a framework for understanding an individual’s previous life experiences, shifting life context, and changes in their behavioral patterns over time, which may, in turn, provide clues regarding potentially effective intervention strategies (Resnicow & Page, 2008; Wilson, Holt, & Greenhalgh, 2001).
REAL intervention structure and content
The Stage 1 REAL manual was comprised of seven modular content areas, as outlined in Table 1. Module 1 focuses on introducing the intervention, assessment, and establishing goals. Modules 2 to 6 each address a specific content area relevant to diabetes management. Each module contains the following components: (a) a brief module-specific assessment, (b) suggested treatment goals and activities, (c) activity handouts and materials, and (d) a therapist reference guide for the module’s content. While the suggested goals and activities for each module provides a starting point for treatment planning, therapists have the latitude to implement individualized goals and activities in accordance with clients’ needs and interests, as long as they are consistent with the focus of the module and the intervention’s theoretical principles. Module 7 has a fixed format similar to Module 1, in which clients and therapists reflect on the client’s accomplishments, develop future goals, and identify community resources for continued diabetes support.
Table 1.
Overview of intervention manual contents
| Module | Structure | Contents | Topics |
|---|---|---|---|
|
1. Setting
Goals |
Fixed |
|
|
|
2. Living
with Diabetes |
Tailored |
|
|
|
3. Access
and Advocacy |
|
||
|
4. Activity
and Health |
|
||
|
5. Social
Support |
|
||
|
6. Emotions
and Wellbeing |
|
||
|
7. Long-
term Health |
Fixed |
|
|
In the REAL feasibility study, the first and last modules were delivered in a standardized format with each client. Modules 2 to 6 were implemented flexibly, in accordance with clients’ individualized goals and diabetes care challenges. The module sequence, time spent on each module, and particular activities completed may vary according to each client’s needs. The total contact hours for each module, across all sessions, ranged from 4.8 hr (6.7% of total treatment time) for Module 3 to 27.8 hr (38.8% of total treatment time) for Module 2, with a median of 6.0 hr per module. Excluding the fixed modules administered in the first and last sessions, the number of sessions in which modules were discussed ranged from 19% (Module 6) to 78% (Module 2). A review of participants’ individualized treatment plans also illustrates the tailoring of the intervention. For example, Client 1 worked on Modules 2 and 3 for 6 sessions each, and Modules 4 to 6 for 1 session each; by contrast, Client 2 worked on Module 2 for 10 sessions, Module 5 for 7 sessions, Module 6 for 4 sessions, and Modules 3 and 4 for 1 session each.
Stage 2 Intervention Manual Revisions
Revisions to the REAL intervention manual were guided by findings from a feasibility study that aimed to “road test” the Stage 1 intervention manual and determine its strengths and areas for improvement. In addition, the revisions incorporated elements of a Stage 2 manual, as specified by Carroll and Nuro (2002), which were absent by design from the Stage 1 manual. An overview of the revisions undertaken in advancing from a Stage 1 to a Stage 2 manual is summarized below.
Revisions to REAL intervention structure
Because implementation of the feasibility study was limited by logistical constraints, the timing and duration of the intervention was identified by both participants and the therapist as a major limitation. Therefore, it was determined that the Phase 2 intervention would be implemented over 6 months, rather than 3 months as originally planned. In addition, due to feedback that the scheduling of sessions was overly restrictive, the therapist was given latitude to determine individualized treatment schedules for each participant, while maintaining the total intervention dose within a specific range of hours. Guidelines for intervention pacing, scheduling sessions, and summarizing intervention content were also incorporated based on the therapist and participant suggestions. In addition, the documentation forms were revised to facilitate easier charting and more comprehensive tracking of client goals. In the feasibility study, the therapist listed goals on each treatment note, which made it difficult to accurately and consistently track progress; the revised forms have a separate sheet for goal documentation and tracking. In addition, to simplify treatment notes, the most commonly used activities were converted to checklist form (with an “other” category to specify less common activities), which allowed for more efficient data entry.
Another significant revision to the REAL intervention structure involved the use of text messaging. Although this had not been specified as part of the Stage 1 protocol, it emerged spontaneously as a strategy viewed by both the therapist and participants as a useful and efficient way to reinforce intervention content between sessions. As such, a text messaging protocol was incorporated into the Stage 2 protocol to delineate appropriate uses of text messaging in the intervention.
Revisions to REAL intervention content
During the feasibility study, the treating therapist uncovered certain client concerns, such as the safety of getting tattoos, which had not arisen in the initial needs assessment but which fit within the scope of the intervention modules. In such cases, additional resources were identified or created to address those needs. The initial assessments completed in Module 1 were revised significantly in response to the therapist’s feedback. Certain assessment domains were added while others, which elicited information that could be obtained from other sources, were eliminated.
A number of suggested content revisions pertained to the therapist training materials. The feasibility study therapist identified a need to better understand “typical” diabetes care strategies among the target population. Therefore, four in-depth case studies, and several shorter vignettes, were incorporated into the therapist training. These case studies and vignettes were based on the actual diabetes care practices and life circumstances of needs assessment and feasibility study participants. Also, a bibliography of additional resources and readings were included in the therapist’s reference guide to address more obscure diabetes care issues that may arise with clients.
Incorporation of Stage 2 manual elements
In advancing from a Stage 1 to a Stage 2 manual, Carroll and Nuro (2002) suggest that additional intervention parameters be specified regarding therapist selection, training, and supervision; differences between the intervention and other treatments; and processes to evaluate intervention fidelity. Several revisions to the REAL intervention manual were undertaken to achieve these goals. First, while we had already specified therapist selection and training standards, we provided additional details regarding training objectives and recognized continuing education providers. Second, to address fidelity monitoring, therapist documentation forms were revised to include reporting on key aspects of the intervention, and a fidelity checklist was developed to facilitate evaluation of therapy sessions. Finally, we clarified key differences and similarities with other interventions, including other diabetes education programs and occupational therapy interventions using the Lifestyle Redesign approach. With respect to diabetes education programs, a key similarity is our focus on diabetes self-management behaviors as targets of the intervention. A key difference is our emphasis on integrating these behaviors into everyday occupations and routines, rather than teaching self-management knowledge and skills. With respect to other Lifestyle Redesign interventions, this intervention is similar in its emphasis on everyday habits and routines, but differs in its delivery mechanism and tailoring of content to a particular developmental stage.
Conclusion
The purpose of this article was to illustrate the process of development, feasibility testing, and revision of an occupational therapy intervention manual. Although we drew upon our research team’s experiences developing an intervention targeting diabetes management, this process could be applied to any clinical problem in occupational therapy practice.
Intervention development is inherently an iterative process that draws on one’s experiential knowledge and clinical reasoning, the needs and concerns of a particular population, and information from the research literature. Viewing a clinical problem through each of these lenses provides insight regarding a theoretical framework from which to approach the problem, and practical considerations for intervention delivery and dissemination, both of which must be revisited at each stage of manual development. For example, from a theoretical standpoint, clinic-based group meetings may have been an ideal strategy for implementing our intervention, because of the opportunity for group problem-solving and social support. However, the target population’s low clinic attendance and low uptake of a previous clinic-based group intervention (Weigensberg et al., 2014) guided our decision to provide the intervention in participants’ homes, to ensure delivery of an adequate treatment dose to accurately assess the intervention’s effect. Although this strategy is appropriate for efficacy research (in which an ideal form of an intervention is tested under tightly controlled conditions), these considerations must be revisited if the intervention is to be translated into broad application. For example, our pilot test of a text messaging component in the Stage 2 manual may pave the way toward a future mobile health implementation of the intervention. This is just one illustration of how theoretical and practical trade-offs are navigated, and how these factors may be weighed differently depending on the stage of intervention development.
Limitations
Although this study reports on the development and manualization of an evidence-based intervention, research evaluating the efficacy of this intervention is still underway. Therefore, some of the intervention strategies outlined in this article may need to be revisited if the intervention is shown not to be efficacious. Furthermore, as previously discussed, the intervention in its current form is relatively resource intensive, and would not be feasible to deliver in most practice settings. If the intervention demonstrates efficacy, further development will be necessary to translate the intervention principles and strategies into a Stage 3 intervention manual that is practical and cost-effective to deliver on a broader scale.
In summary, intervention manuals are a critical tool for developing the evidence base for occupational therapy clinical practice. Developing intervention manuals is an iterative process, with their form and purpose differing depending on the stage of the research-to-clinical practice pipeline. Developing a flexible intervention framework allows manuals to navigate the competing demands of defining core intervention elements and allowing for clinical judgment.
Acknowledgment
The authors thank Marc Weigensberg, MD, Anne Peters, MD, CDE, and Florence Clark, PhD, OTR/L, FAOTA for their mentorship in completing this project.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: National Institute of Diabetes and Digestive and Kidney Diseases (Grant/Award 1K01DK099202-01A1) and National Center for Advancing Translational Sciences (Grant/Award KL2RR031991).
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- American Occupational Therapy Association Occupational therapy practice framework: Domain and process. American Journal of Occupational Therapy. (3rd) 2014;68(Suppl. 1):S1–S48. [PubMed] [Google Scholar]
- Bandura A. Health promotion from the perspective of social cognitive theory. Psychology & Health. 1998;13:623–649. [Google Scholar]
- Blanche EI, Fogelberg D, Diaz J, Carlson M, Clark F. Manualization of occupational therapy interventions: Illustrations from the pressure ulcer prevention research program. American Journal of Occupational Therapy. 2011;65:711–719. doi: 10.5014/ajot.2011.001172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carandang K, Pyatak EA. Feasibility of a manualized diabetes management occupational therapy intervention. Manuscript in preparation. 2015 doi: 10.5014/ajot.2018.021790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Nuro K. One size cannot fit all: A stage model for psychotherapy manual development. Clinical Psychology: Science and Practice. 2002;9:396–406. [Google Scholar]
- Clark F. Occupation embedded in a real life: Interweaving occupational science and occupational therapy. American Journal of Occupational Therapy. 1993;47:1067–1078. doi: 10.5014/ajot.47.12.1067. [DOI] [PubMed] [Google Scholar]
- Clark F, Azen SP, Zemke R, Jackson J, Carlson M, Mandel D, Lipson L. Occupational therapy for independent-living older adults—A randomized controlled trial. Journal of the American Medical Association. 1997;278:1321–1326. [PubMed] [Google Scholar]
- Clark F, Jackson J, Carlson M, Chou CP, Cherry BJ, Jordan-Marsh M, Azen SP. Effectiveness of a lifestyle intervention in promoting the well-being of independently living older people: Results of the Well Elderly 2 Randomised Controlled Trial. Journal of Epidemiology & Community Health. 2012;66:782–790. doi: 10.1136/jech.2009.099754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark F, Pyatak E, Carlson M, Blanche E, Vigen C, Hay J, PUPS Study Group Implementing trials of complex interventions in community settings: The USC-Rancho Los Amigos Pressure Ulcer Prevention Study (PUPS) Clinical Trials. 2014;11:218–229. doi: 10.1177/1740774514521904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HC, Geyer R. What can complexity do for diabetes management? Linking theory to practice. Journal of Evaluation in Clinical Practice. 2009;15:761–765. doi: 10.1111/j.1365-2753.2009.01229.x. [DOI] [PubMed] [Google Scholar]
- Cukrowicz KC, Timmons KA, Sawyer K, Caron KM, Gummelt HD, Joiner TE. Improved treatment outcome associated with the shift to empirically supported treatments in an outpatient clinic is maintained over a ten-year period. Professional Psychology: Research and Practice. 2011;42:145–152. [Google Scholar]
- Des Jarlais D, Lyles C, Crepaz N, TREND Group Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: The TREND statement. American Journal of Public Health. 2004;94:361–366. doi: 10.2105/ajph.94.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickie V, Cutchin M, Humphry R. Occupation as transactional experience: A critique of individualism in occupational science. Journal of Occupational Science. 2006;13:83–93. [Google Scholar]
- Frank A. Health stories as connectors and subjectifiers. Health. 2006;10:421–440. doi: 10.1177/1363459306067312. [DOI] [PubMed] [Google Scholar]
- Horigian V, Weems C, Robbins M, Feaster D, Ucha J, Miller M, Werstlein R. Reductions in anxiety and depression symptoms in youth receiving substance use treatment. The American Journal on Addictions. 2013;22:329–337. doi: 10.1111/j.1521-0391.2013.12031.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson J, Carlson M, Mandel D, Zemke R, Clark F. Occupation in lifestyle redesign: The Well Elderly Study Occupational Therapy Program. American Journal of Occupational Therapy. 1998;52:326–336. doi: 10.5014/ajot.52.5.326. [DOI] [PubMed] [Google Scholar]
- Kielhofner G, Burke JP. A model of human occupation, Part 1: Conceptual framework and content. American Journal of Occupational Therapy. 1980;34:572–581. doi: 10.5014/ajot.34.9.572. [DOI] [PubMed] [Google Scholar]
- Lemal M, Van den Bulck J. Testing the effectiveness of a skin cancer narrative in promoting positive health behavior: A pilot study. Preventive Medicine. 2010;51:178–181. doi: 10.1016/j.ypmed.2010.04.019. [DOI] [PubMed] [Google Scholar]
- Lorig K, Ritter PL, Villa FJ, Armas J. Community-based peer-led diabetes self-management: A randomized trial. The Diabetes Educator. 2009;35:641–651. doi: 10.1177/0145721709335006. [DOI] [PubMed] [Google Scholar]
- Lorig KR, Sobel DS, Stewart AL, Brown BW, Jr., Bandura A, Ritter P, Holman HR. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: A randomized trial. Medical Care. 1999;37:5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- Mattingly C. Healing dramas and clinical plots: The narrative structure of experience. Cambridge University Press; Cambridge, UK: 1998. [Google Scholar]
- McLeroy K, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Education Quarterly. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- Mishali M, Sominsky L, Heymann A. Reducing resistance to diabetes treatment using short narrative interventions. Family Practice. 2010;27:192–197. doi: 10.1093/fampra/cmp091. [DOI] [PubMed] [Google Scholar]
- Murphy S, Gutman S. Intervention fidelity: A necessary aspect of intervention effectiveness studies. American Journal of Occupational Therapy. 2012;66:387–388. doi: 10.5014/ajot.2010.005405. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC, Norcross JC. search of how people change: Applications to addictive behaviors. American Psychologist. 1992;47:1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- Pyatak EA, Florindez D, Peters AL, Weigensberg MJ. "We are all gonna get diabetic these days": the impact of a living legacy of type 2 diabetes on Hispanic young adults' diabetes care. The Diabetes Educator. 2014;40:648–658. doi: 10.1177/0145721714535994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyatak EA, Florindez D, Weigensberg MJ. Adherence decision making in the everyday lives of emerging adults with type 1 diabetes. Patient Preference and Adherence. 2013;7:709–718. doi: 10.2147/PPA.S47577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyatak EA, Sequeira PA, Whittemore R, Vigen CP, Peters AL, Weigensberg MJ. Challenges contributing to disrupted transition from paediatric to adult diabetes care in young adults with Type 1 diabetes. Diabetic Medicine. 2014;31:1615–1624. doi: 10.1111/dme.12485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnicow K, Page S. Embracing chaos and complexity: A quantum change for public health. American Journal of Public Health. 2008;98:1382–1389. doi: 10.2105/AJPH.2007.129460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riessman CK. Narrative methods for the human sciences. SAGE; Thousand Oaks, CA: 2008. [Google Scholar]
- Robbins MS, Feaster DJ, Horigian VE, Rohrbaugh M, Shoham V, Bachrach K, Szapocznik J. Brief strategic family therapy versus treatment as usual: Results of a multisite randomized trial for substance using adolescents. Journal of Consulting and Clinical Psychology. 2011;79:713–727. doi: 10.1037/a0025477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossouw T, Fonagy P. Mentalization-based treatment for self-harm in adolescents: A randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry. 2012;51:1304–1313. doi: 10.1016/j.jaac.2012.09.018. [DOI] [PubMed] [Google Scholar]
- Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist. 2000;55:68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- Scobbie L, Dixon D, Wyke S. Goal setting and action planning in the rehabilitation setting: Development of a theoretically informed practice framework. Clinical Rehabilitation. 2011;25:468–482. doi: 10.1177/0269215510389198. [DOI] [PubMed] [Google Scholar]
- Strong S, Rigby P, Stewart D, Law M, Letts L, Cooper B. Application of the Person-Environment-Occupation Model: A practical tool. Canadian Journal of Occupational Therapy. 1999;66:122–133. doi: 10.1177/000841749906600304. [DOI] [PubMed] [Google Scholar]
- USC Occupational Therapy Faculty Practice. (n.d.). Retrieved from http://ot.usc.edu/patient-care/faculty-practice. [Google Scholar]
- Waller G, Mountford VA, Tatham M, Turner H, Gabriel C, Webber R. Attitudes towards psychotherapy manuals among clinicians treating eating disorders. Behaviour Research and Therapy. 2013;51:840–844. doi: 10.1016/j.brat.2013.10.004. [DOI] [PubMed] [Google Scholar]
- Weigensberg M, Pyatak E, Florindez D, Sequeira P, Spruijt-Metz D, Juarez M, Peters A. Diabetes Empowerment Council (DEC): Development and pilot testing of an innovative mind-body group intervention for young adults with type 1 diabetes. Journal of Alternative and Complementary Medicine. 2014;20:A69. [Google Scholar]
- Wilson T, Holt T, Greenhalgh T. Complexity and clinical care. British Medical Journal. 2001;323:685–688. doi: 10.1136/bmj.323.7314.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood W, Quinn J, Kashy D. Habits in everyday life: Thought, emotion, and action. Journal of Personality and Social Psychology. 2002;83:1281–1297. [PubMed] [Google Scholar]