Abstract
Aim
To determine the incidence of out-of-hospital cardiac arrest (OHCA) fulfilling Utstein criteria in the Canton Ticino, Switzerland, the survival rate of OHCA patients and their neurological outcome.
Methods and results
All OHCAs treated in Canton Ticino between 1 January 2005 and 31 December 2014 were followed until either death or hospital discharge. The survival and neurological outcome of those OHCA fulfilling Utstein criteria are reported. A total of 3367 OHCAs occurred in the Canton Ticino over a 10-year period. Resuscitation was attempted in 2298 patients; of those 1492 (65%) were of presumed cardiac origin, 454 fulfilling the Utstein comparator criteria. About 69% [95% confidence interval (CI), 66.6–71.4%] of the patients had a bystander-witnessed arrest; a dispatched cardiopulmonary resuscitation (CPR) steadily and significantly increased from 2005 to 2014. Out-of-hospital cardiac arrest occurred prevalently home (67%), in men (71%) of a mean age of 71 ± 13 years. There were no statistically significant differences either in demographic characteristics of OHCA victims over these years or in presenting rhythm. There was a progressive increase in the survival at discharge from 15% in 2005 to 55% in 2014; overall 96% (95% CI, 93.3–99.9%) of the survivors had a good neurological outcome.
Conclusion
The significant increase in Utstein comparator survival rates and improved neurological outcome in OHCA victims in Canton Ticino are the result of an effective OHCA management programme which includes large-scale public education, a coordinated fast EMS response, high density of external defibrillators, and advances in clinical interventions for OHCAs.
Keywords: Out-of hospital cardiac arrest, Bystander resuscitation, Survival, Neurological outcome
What's new?
We report for the first time a systematic and conservative assessment of incidence of established OHCA in Switzerland resulting in 73 cases of OHCA per 100 000 per year.
Incidence of established OHCA remained stable over a 10-year observation period.
The incidence of emergency medical system treated bystander-witnessed OHCA with VF, in the decades >60 years, was two times that of the general population.
Analysis of standardized and homogeneous emergency medical protocols provides important data on the epidemiology of OHCA.
A major increase in survival rate after OHCA in Canton Ticino with particularly favourable neurological outcome due to a significant increase in the performance of first responder network, and due to improved pre- and in-hospital management.
Continued allocation of human and financial resources to further improve pre-, in-, and post-hospital survival and neurological outcome are greatly needed.
The clinical problem of OHCA needs to be studied on a population level to improve risk stratification beyond the current low ejection fraction recommendation.
Introduction
Incidence of out-of-hospital cardiac arrest (OHCA) attended by emergency medical service (EMS) in Europe is ∼86 per 100 000 person-year with significant geographical differences.1 Out-of-hospital cardiac arrest remains associated with very high morbidity and mortality,2 the latter ranging from 2.6 to 9.9%.3 It has been estimated that ∼10 000 people may suffer a sudden cardiac death in Switzerland.4 However, the real incidence of OHCA and survival rate in the country is currently unknown. Several initiatives have recently been undertaken in some Swiss cantons to raise awareness about OHCA, and to educate bystanders on cardiopulmonary resuscitation (CPR) and basic life support (BLS) manoeuvres. The lack of a federal OHCA registry does not permit the assessment of effectiveness of these initiatives.
In 2005 in Canton Ticino (the southernmost canton of Switzerland), a major restructuration of the OHCA management was undertaken. It included a significant change in the structure of EMS organizations, a facilitated access to cardiac catheterization laboratory and to intensive care unit at the regional heart centre. Moreover, a non-profit organization (Fondazione Ticino Cuore) was created to increase public awareness on OHCA, to promote bystander intervention, and to organize an efficient first responder network including engagement of trained lay people. Finally, there has been a systematic investment to increase year-after-year the density of public automated external defibrillators (PADs). On top of these activities, a prospectively designed web-based registry using international standards (Utstein nomenclature and outcome definition)5 was established, which serves as an observatory of the incidence and characteristics of OHCA on the territory and continuously monitors the survival rate and the neurological outcome of OHCA patients.
Currently, it is unknown whether these changes have resulted in significant improvements in both survival and neurological outcomes of bystander-witnessed OHCA with ventricular fibrillation (VF) (Utstein definition)5 in Canton Ticino, a topic addressed by this study.
Methods
Selection of participants and definitions
All individuals being older than 1 year who suffered in the Canton Ticino region from 1 January 2002 until 31 December 2014 an OHCA regardless of its aetiology have been included in this study. The capture of cardiac arrest cases was complete because the EMS system is activated for all emergencies concerning cardiac arrest, and the definition excludes cases with obvious late signs of death (e.g. rigor mortis) for which resuscitative efforts are not initiated or when a do-not-resuscitate order is in place. Out-of-hospital cardiac arrest was defined as cessation of cardiac mechanical activity that is confirmed by the absence of signs of circulation occurring outside of a hospital setting. Current analysis has been limited to those OHCAs who fulfilled Utstein criteria. All OHCA survivors were followed-up until discharge from the hospital. Survival rates were calculated at discharge from hospital, and at 1-year follow-up.
A bystander was defined as an individual who witnessed the collapse or who found the person unresponsive and activated the EMS system. Cerebral performance categories (CPCs, assessed during at the discharge and at 1-year follow-up) indicate neurological outcomes; CPCs of 1 (good) and 2 (moderate) were considered as favourable neurological outcomes in contrast to CPC 3 (severe cerebral disability) or CPC 4 (coma or vegetative state).6
The web-based registry
Although the cardiac arrest registry was established on 1 January 2002, consecutive and audited data have been entered starting on 1 January 2005. The web-based registry has the goal to monitor OHCA in Canton Ticino as well as to identify potential areas for improvement in cardiac and emergency care. It contains a record of every individual who presented a cardiac arrest regardless of aetiology, and includes patient' demographic data, comprehensive EMS-related data, detailed bystander and first responder activity including the use of automated external defibrillator (AED)/PAD as well as pre- and in-hospital treatment and outcome. Data are collected and stored following Good Clinical Practice Guidelines and the relevant legislation governing the use of patient data. The investigation complied with the Declaration of Helsinki's principles for physicians engaged in biomedical research involving human subjects and was approved by the appropriate ethics committee.
Management of emergency medical system in Canton Ticino, the Fondazione Ticino Cuore, and the first responder network
The Federazione Cantonale Ticinese Servizi Autoambulanze coordinates the entire EMS in Canton Ticino, a territory of more than 2.800 km² which presents significant geographic challenges (mountains, valleys, and lakes). The population of Canton Ticino is distributed in few urban areas with high population density, and a large number of rural areas unequally distributed over the territory. The Emergency Medical Dispatch (EMD) manages all emergencies based upon the medical priority dispatch system; in case of OHCA, a dispatched assisted triage and a dispatched life support are initiated. Emergency medical service personnel is trained according to International Liaison Committee on Resuscitation guidelines.7 Once the EMD dispatcher judges the OHCA scene secure, an alarm is issued and delivered to both professional (police and fire department—AED equipped) and laic first responders; the latter are guided to the OHCA location by messaging system which also indicates the location of a PAD. If the OHCA scene is not considered secure, then only professional first responders are alerted. The mission of the organization—Fondazione Ticino Cuore—has been outlined above.
Statistics
Data were imported from Microsoft Access into Stata 13.1 (StataCorp, College Station, TX, USA) and cleaned with back and forth checks with the registry data manager, before undergoing analysis. Continuous data were summarized as mean and standard deviation and median and quartiles, and categorical data as counts and percent. Death rates and binomial exact 95% confidence intervals (95% CIs) were computed. Patterns over years were assessed with the test for trend. All tests were two-sided and significance was set at 5%. To determine the yearly incidence of OHCA, i.e. number of new cases per unit of person-time at risk on every year, the yearly number of OHCAs was divided by the local population at risk during the same period.8 All OHCAs included also those who were declared dead in field, regardless of whether a resuscitation attempt was initiated.
Results
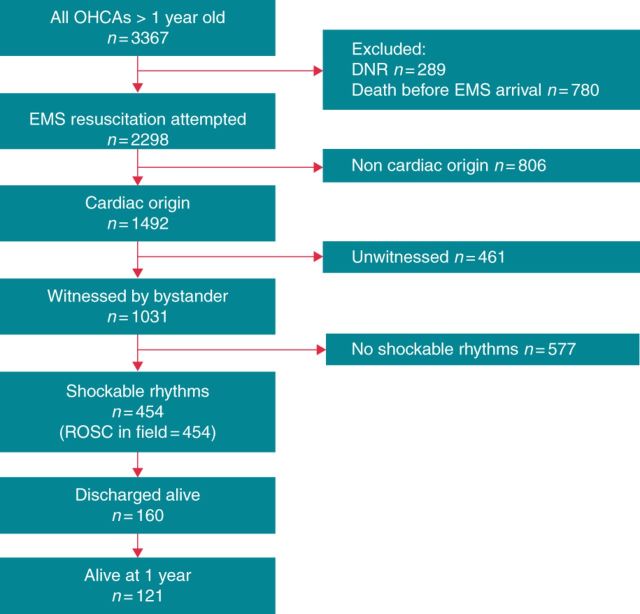
During the 10-year study period, a total of 3367 OHCAs occurred in the Canton Ticino. There was a negligible annual fluctuation in the absolute number of OHCA without significant change over time of the OHCA incidence (Table 1). The incidence of EMS-treated bystander-witnessed OHCA with VF in the decades >60 years was two times that of the general population (Table 1). Resuscitation was attempted in 2298 cases; of those 1492 (65%) were of presumed cardiac origin, and 454 fulfilled the Utstein comparator criteria (Figure 1). All patients who had a shockable rhythm as presenting event had a ROSC in field (Figure 1). Patients and resuscitation characteristics are shown in Table 2. Out-of-hospital cardiac arrest occurred prevalently home (67%), in men (71%) of a mean age of 71 ± 13 years. There were no statistically significant differences in demographic characteristics of OHCA victims over years as well as in the presenting rhythm.
Table 1.
Yearly incidence of OHCA (100 000 persons event/rate), EMS-attended OHCA, EMS-treated OHCA, EMS-treated OHCA of presumed cardiac aetiology, and EMS-treated OHCA with VF
| Resident population |
All-cause OHCAs | All-cause OHCAs incidence | EMS-treated OHCAs | EMS-treated OHCAs incidence | EMS-treated OHCAs of presumed cardiac aetiology | EMS-treated OHCAs of presumed cardiac aetiology incidence | EMS-treated OHCAs, bystander-witnessed with VF (Utstein comparator) | EMS-treated OHCAs, bystander-witnessed with VF (Utstein comparator) incidence | EMS-treated OHCAs (over 60 years), bystander-witnessed with VF | EMS-treated OHCAs (over 60 years), bystander-witnessed with VF incidence | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Over 60 years | n = 4320 | n = 2298 | n = 1492 | n = 454 | n = 261 | ||||||
| 2005 | 322.276 | 81.364 | 350 | 109 | 232 | 72 | 138 | 43 | 44 | 14 | 22 | 27 |
| 2006 | 324.851 | 83.577 | 326 | 100 | 222 | 68 | 149 | 46 | 47 | 14 | 26 | 31 |
| 2007 | 328.580 | 85.702 | 349 | 106 | 210 | 64 | 129 | 39 | 29 | 9 | 17 | 20 |
| 2008 | 332.736 | 87.674 | 300 | 90 | 206 | 62 | 143 | 43 | 43 | 13 | 25 | 29 |
| 2009 | 335.720 | 89.402 | 343 | 102 | 244 | 73 | 168 | 50 | 58 | 17 | 37 | 41 |
| 2010 | 333.753 | 89.522 | 360 | 108 | 241 | 72 | 164 | 49 | 44 | 13 | 31 | 35 |
| 2011 | 336.943 | 91.109 | 353 | 105 | 238 | 71 | 152 | 45 | 44 | 13 | 26 | 29 |
| 2012 | 341.652 | 92.770 | 331 | 97 | 238 | 70 | 145 | 42 | 50 | 15 | 28 | 30 |
| 2013 | 346.539 | 94.463 | 356 | 103 | 254 | 73 | 167 | 48 | 53 | 15 | 31 | 33 |
Resident population according to Swiss Federal Office of Statistics.8
Figure 1.
Flowchart of patients' inclusion.
Table 2.
Baseline and operational characteristics for patients with presumed cardiac cause of OHCA
| Characteristics | Year |
P-value | n (%) | Missing data (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2005–14 | |||
| OHCA, n (%) | 138 (61) | 149 (67) | 129 (61) | 143 (69) | 168 (69) | 164 (68) | 152 (64) | 145 (61) | 167 (66) | 137 (68) | 1492 (65) | 0.0 | |
| Age, years mean ± SD | 70 ± 12 | 68 ± 14 | 70 ± 12 | 72 ± 14 | 70 ± 13 | 72 ± 14 | 72 ± 14 | 71 ± 14 | 73 ± 13 | 69 ± 15 | 0.03 | 1489 | 1 |
| Men, n (%) | 96 (69) | 112 (67) | 90 (70) | 99 (70) | 116 (69) | 123 (75) | 109 (72) | 107 (74) | 118 (71) | 111 (81) | 0.17 | 970 (71) | 0.1 |
| Cardiac arrest in private home, n (%) | 103 (74) | 99 (66) | 89 (69) | 83 (58) | 102 (61) | 111 (68) | 113 (74) | 100 (69) | 114 (68) | 87 (63) | 0.75 | 1001 (67) | 0.0 |
| Bystander-witnessed arrest, n (%) | 105 (76) | 107 (72) | 83 (64) | 101 (71) | 115 (68) | 101 (61) | 111 (73) | 100 (69) | 121 (72) | 93 (70) | 0.53 | 1037 (69) | 0.0 |
| Bystander CPR performed, n (%) | 47 (38) | 82 (55) | 64 (50) | 84 (58) | 85 (54) | 84 (55) | 84 (60) | 85 (62) | 106 (63) | 93 (70) | 0.00 | 814 (57) | 0.1 |
| Shockable heart rhythm, n (%) | 44 (32) | 47 (31) | 29 (24) | 43 (31) | 58 (34) | 44 (29) | 44 (29) | 50 (35) | 53 (32) | 42 (31) | 0.46 | 454 (30) | 0.0 |
| AED use, n (%) | N.A. | N.A. | N.A. | 5 (11) | 7 (12) | 9 (20) | 10 (23) | 16 (32) | 12 (23) | 9 (21) | 0.90 | 68 (15) | 0.0 |
| Time to BLS, median (IQR) (min) | N.A. | 1.0 [0.9–3.0] | 2.0 [0.9–6.0] | 2.9 [1.0–5.9] | 3.3 [1.3–5.5] | 2.6 [1.1–5.7] | 1.9 [0.9–4.7] | 3.1 [1.4–5.5] | 2.1 [1.0–5.8] | 3.3 [1.6–4.9] | 0.00 | 243 | 47.0 |
| Time to EMS arrival on scene, median (IQR) (min) | 9.5 [7.4–14.0] | 11.0 [9.0–13.0] | 11.0 [8.0–16.0] | 10.9 [7.9–14.0] | 10.6 [7.9–13.8] | 10.7 [7.9–14.2] | 10.6 [7.7–13.5] | 9.7 [7.1–13.8] | 9.8 [7.8–14.1] | 9.9 [7.3–11.8] | 0.47 | 453 | 0.5 |
| Survival, n (%) | |||||||||||||
| On arrival at hospital | 21 (47) | 27 (57) | 17 (58) | 27 (63) | 31 (53) | 23 (52) | 26 (59) | 30 (60) | 31 (58) | 30 (71) | 0.11 | 263 (56) | 0.0 |
| At discharge | 7 (15) | 13 (27) | 10 (34) | 16 (37) | 21 (36) | 16 (36) | 14 (32) | 18 (36) | 22 (41) | 23 (55) | 0.00 | 160 (35) | 0.0 |
| 1 year | 5 (11) | 12 (25) | 9 (31) | 10 (23) | 17 (29) | 16 (36) | 14 (32) | 18 (36) | 20 (38) | N.A. | 0.11 | 121 (24) | 14 |
Times refer to bystander-witnessed OHCAs with first rhythm shockable; Survival refers to those patients with presumed cardiac aetiology as assessed by EMS, witnessed by a bystander layperson and having as presenting cardiac rhythm a VF or pulseless ventricular tachycardia (Utstein comparator).
Witnessed status, bystander resuscitation attempt, role of first responders, and automated external defibrillator use
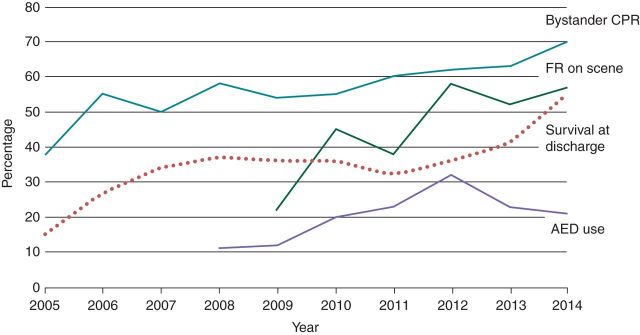
Altogether, 69% (95% CI, 66.6–71.4%) of the patients had a bystander-witnessed arrest; this proportion was stable over time (Table 2). Throughout the study period, a BLS or a dispatched CPR steadily and significantly increased (Table 2). A layperson or a professional first responder was on scene in 29% of time within 7 min from the alarm call, thus replacing or supporting the bystander-initiated CPR (Figure 2). Subsequently with the introduction of a telephone-based messaging system (SMS) activated by the EMS dispatcher, there was a progressive increase in the number of laic first responders who responded to the SMS (Figure 2), and reached the scene within 3 min from message.
Figure 2.
Pre-hospital resuscitation activities (first responders on scene, bystander-performed CPR, and AED use) and survival rate at hospital discharge (dotted line). Data for bystander-performed CPR have been collected starting in 2009; data on the use of AED have been collected starting in 2008.
Survival and 1-year neurological outcome
Before 2010, all OHCAs were referred to the nearest hospital, with a subsequent transfer to a tertiary level hospital (Fondazione Cardiocentro Ticino) for OHCAs of cardiac origin. Starting in 2011, all OHCAs of presumed cardiac origin were directly transferred to the tertiary care centre, in which primary coronary revascularization and therapeutic hypothermia was immediately available. There was a progressive increase in the proportion of patients achieving survival at discharge from 15% in 2005 to 55% in 2014 (Table 2). The improvement in survival rate was still significant when 1-year survival was assessed (Table 2). Altogether, 96% (95% CI, 93.3–99.9%) of the survivors had a good neurological outcome (Table 3). Implantation of a cardioverter-defibrillator which may include cardiac resynchronization therapy was indicated in 116 patients whose OHCA was not related to a myocardial ischaemic event.
Table 3.
Distribution of CPC scores among surviving patients per year
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | P-value | 2005–14 | Missing data (%) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CPC 1–2 score, n (%) | 5 (100) | 11 (92) | 8 (89) | 10 (100) | 16 (94) | 15 (94) | 14 (100) | 18 (100) | 18 (100) | N.A. | 0.14 | 115 (96) | 0 |
| CPC 3–4 score, n (%) | 0 | 1 (8) | 1 (11) | 0 | 1 (6) | 1 (6) | 0 | 0 | 0 | N.A. | 0.14 | 4 (4) | 0 |
Discussion
This study reports a major increase in survival rate after OHCA in Canton Ticino with particularly favourable neurological outcome due to a significant increase in the performance of first responder network, and due to improved pre- and in-hospital management. It is evident that there is much value in utilizing a registry to provide evidence of effectiveness; it also provides invaluable information to identify areas for improvement in the chain of survival. Notably, our experience may possible serve as an OHCA management model to other Swiss Cantons.
The higher incidence of OHCA of presumed cardiac origin in Canton Ticino compared with other European countries (Denmark: 52%)9 or cities (e.g. London: 44%; Vienna: 48.5%)10,11 may be related to a higher proportion of bystander-witnessed cardiac arrest and/or to demographic differences. Differently from Wissenberg et al.9 and Margey et al.12 but in agreement with Martens et al.,13 we did not notice a measurable reduction in either absolute number of OHCAs or its incidence. This may result from a parallel increase of incidence of OHCA in the persons aged over 60, a population segment that has been rapidly growth in Canton Ticino over the last decade.
Differently from recent reports,14 the proportion of bystander CPR in Canton Ticino was already relatively high in the early years of the registry and continued to increase over time. Moreover, the first responder network progressively increased its performance as indicated by the presence of a first responder within a few minutes from the alarm who started CPR and/or used AED. Differently from other international realities, in Canton Ticino the first responder network includes a very large group of laypersons well trained to perform CPR and to use PAD/AED, and operates next to the more traditional first responder network made by police or fire department officers. The prompt availability of a first responder, especially in a geographically challenging territory such as Canton Ticino, increases the likelihood of performing CPR in an adequate manner, and provides physical and psychological support to the OHCA bystander and to relatives of OHCA victim until ambulance arrival.15 In line with other reports,16 we observed that an early-performed CPR increased hospital arrival survival.
The strong relationship between CPR training and increase in resuscitation attempts by bystanders has been well documented in several previous studies,17,18 and is confirmed by our data. The large temporal increase in rates of bystander CPR is attributable to a number of factors including an overall increased level of attention to resuscitation by general population triggered by large-scale awareness campaigns, as well as the offer of CPR training programme to adults and to teenagers as part of their school education. Altogether, they have contributed to changes in attitude to start CPR in Canton Ticino, and to the growth in the number of volunteers who are part of the first responder network observed in our study.
Certainly, early use of a defibrillator by bystanders is positively associated with an increased survival.18,19 Public automated external defibrillators have been proved effective if they are placed in strategic locations;20 currently the PAD density in Canton Ticino is ∼256 PADs per 100 000 inhabitants. On the other hand, and consistent with other experiences,10,11 nearly three-fourths of the OHCAs occurred in private homes, a factor which is commonly considered a limitation of the efficacy of a PADs programme. In spite of this, we noticed a higher rate of defibrillation by bystanders or by first responders in Canton Ticino compared with other European countries.21,22 A possible explanation is the fact that both laic and professional first responders are carrying a private AED or are able to quickly geo-locate a PAD by using a mobile application developed by us.
Finally, post-resuscitation care of OHCA victims is of equal importance compared with pre-hospital activities in improving outcome. Over the years, there has been a significant evolution in post-resuscitation care, which nowadays includes early access to primary coronary revascularization,23 therapeutic hypothermia,23 and comprehensive heart failure management.24 All these interventions have contributed to an improved survival and neurological outcome by limiting the severity of ischaemic myocardial and brain damage as clearly demonstrated by the progressive reduction of our in-hospital mortality and massive improvement of cerebral performance at discharge. Moreover, the subsequent implantation of a cardioverter-defibrillator and cardiac resynchronization therapy whenever indicated according to guidelines of the European Society of Cardiology24,25 may have further contributed to significantly reduce the risk of recurrence of a fatal event during the follow-up.
Conclusions
The significant increase in survival rates and improved neurological outcome in bystander-witnessed OHCA with VF (Utstein definition) in Canton Ticino represent good evidence that a coordinated fast EMS response along with an efficient first responder network, high density of PADs/AEDs, and advances in clinical interventions for OHCAs are all essential elements for success. Our data do not allow to provide any firm conclusion as to which specific factors have contributed most to the increase in survival.
Funding
This work was been in part supported by a research grant by Swiss Heart Foundation ‘An analysis of incidence and outcome of out-of-hospital cardiac arrest in Canton Tcino over the past decade (TIRECA study)’. An unrestricted grant to Fondazione Ticino Cuore has been given by each of the following institutions or companies: Biotronik GmbH (Zug, Switzerland), Ente Ospedaliero Cantonale (Lugano, Switerland), Federazione Cantonale Ticinese Servizi Autoambulanze (Breganzona, Switzerland), Fondazione Cardiocentro Ticino (Lugano, Switzerland), Fondazione Cecilia Augusta (Lugano, Switzerland), Fondazione Fidinam (Lugano, Switzerland), Fondazione Ing. Pasquale Lucchini (Lugano, Switzerland), Boston Scientific (Solothurn, Switzerland), Medtronic Foundation (Minneapolis, USA), St. Jude Medical (Zurich, Switzerland), REGA (Zurich, Switzerland), Philips AG (Zurich, Switzerland), Swiss Heart Foundation (Bern, Lugano), SuVA (Luzern, Switzerland). Funding to pay the Open Access publication charges for this article was provided by Fondazione Ticino Cuore.
Conflict of interest: A.A. receives consulting fees or honoraria from Medtronic, Inc., Sorin Group, Abbott, Biologics Delivery Systems, Cordis Corporation (a J&J company), DC Devices Incorporated; the other co-authors have no disclosures.
Acknowledgements
The authors wish to acknowledge all rescue crews, all members of the local EMD Ticino Soccorso and EMSs, every first responder who on daily basis offers his or her time and help to save a life, to the Ministry of Health and to the Ministry of Education of Repubblica and Canton Ticino for their respective support to conduct educational activities in the schools, to the trainers, and to all past and present sponsors who generously have supported the project.
References
- 1. Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation 2010;81:1479–87. [DOI] [PubMed] [Google Scholar]
- 2. Ewy GA, Sanders AB. Alternative approach to improving survival of patients with out-of-hospital primary cardiac arrest. J Am Coll Cardiol 2013;61:113–8. [DOI] [PubMed] [Google Scholar]
- 3. Gräsner JT, Böttiger BW, Bossaert L; European Registry of Cardiac Arrest (EuReCa) ONE Steering Committee; EuReCa ONE Study Management Team. EuReCa ONE - ONE month - ONE Europe - ONE goal. Resuscitation 2014;85:1307–8. [DOI] [PubMed] [Google Scholar]
- 4. Katz E, Metzger JT, Sierro C, Mischler C, Fishman D, Kappenberg L. Sudden cardiac death: epidemiology and modern therapy. Rev Med Suisse 2007;3:302–7. [PubMed] [Google Scholar]
- 5. Cummins R, Chamberlain D, Abramson N, Allen M, Baskett P, Becker L, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the ‘Utstein style’. Prepared by a Task Force of Representatives from the European Resuscitation Council, American Heart Association, Heart and Stroke Foundation of Canada. Resuscitation 1991;22:1–26. [PubMed] [Google Scholar]
- 6. Safar P. Cerebral resuscitation after cardiac arrest: research initiatives and future directions. Ann Emerg Med 1993;22:324–49. [DOI] [PubMed] [Google Scholar]
- 7. Consensus 2010 documents http://www.ilcor.org/consensus-2010/costr-2010-documents (2 February 2015, date last accessed).
- 8. Summary Vital Statistics in Ticino. Swiss Federal Statistics Office website: www.statistics.admin.ch (15 November 2014, date last accessed).
- 9. Wissenberg M, Lippert FK, Folke F, Weeke P, Hansen CM, Christensen EF, et al. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA 2013;310:1377–84. [DOI] [PubMed] [Google Scholar]
- 10. Nürnberger A, Sterz F, Malzer R, Warenits A, Girsa M, Stöckl M, et al. Out of hospital cardiac arrest in Vienna: incidence and outcome. Resuscitation 2013;84:42–7. [DOI] [PubMed] [Google Scholar]
- 11. Fothergill RT, Watson LR, Chamberlain D, Virdi GK, Moore FP, Whitbread M. Increases in survival from out-of-hospital cardiac arrest: a five year study. Resuscitation 2013;84:1089–92. [DOI] [PubMed] [Google Scholar]
- 12. Margey R, Browne L, Murphy E, O'Reilly M, Mahon N, Blake G, et al. The Dublin cardiac arrest registry: temporal improvement in survival from out-of-hospital cardiac arrest reflects improved pre-hospital emergency care. Europace 2011;13:1157–65. [DOI] [PubMed] [Google Scholar]
- 13. Martens E, Sinner MF, Siebermair J, Raufhake C, Beckmann B, Veith S, et al. Incidence of sudden cardiac death in Germany, results from an emergency medical service registry in Lower Saxony. Europace 2014;16:1752–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kitamura T, Iwami T, Kawamura T, Nitta M, Nagao K, Nonogi K, et al. Japanese Circulation Society Resuscitation Science Study Group. Nationwide improvements in survival from out-of-hospital cardiac arrest in Japan. Circulation 2012;126:2834–43. [DOI] [PubMed] [Google Scholar]
- 15. Pekevski J. First responders and psychological first aid. J Emerg Manag 2013;11:39–48. [DOI] [PubMed] [Google Scholar]
- 16. McNally B, Robb R, Mehta M, Vellano K, Valderrama AL, Yoon PW, et al. ; Centers for Disease Control and Prevention. Out-of-hospital cardiac arrest surveillance—Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005—December 31, 2010. MMWR Surveill Summ 2011;60:1–19. [PubMed] [Google Scholar]
- 17. Cobb LA, Fahrenbruch CE, Walsh TR, Copass MK, Olsufka M, Breskin M, et al. Influence of cardiopulmonary resuscitation prior to defibrillation in patients with out-of hospital ventricular fibrillation. JAMA 1999;281:1182–8. [DOI] [PubMed] [Google Scholar]
- 18. Hüpfl M, Selig HF, Nagele P. Chest-compression-only versus standard cardiopulmonary resuscitation: a meta-analysis. Lancet 2010;376:1552–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mitani Y, Ohta K, Yodoya N, Otsuki S, Ohashi H, Sawada H, et al. Public access defibrillation improved the outcome after out-of-hospital cardiac arrest in school-age children: a nationwide, population-based, Utstein registry study in Japan. Europace 2013;15:1259–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sanna T, La Torre G, de Waure C, Scapigliati A, Ricciardi W, Dello Russo A, et al. Cardiopulmonary resuscitation alone vs. cardiopulmonary resuscitation plus automated external defibrillator use by non-healthcare professionals: a meta-analysis on 1583 cases of out-of-hospital cardiac arrest. Resuscitation 2008;76:226–32. [DOI] [PubMed] [Google Scholar]
- 21. Murakami Y, Iwami T, Kitamura T, Nishiyama C, Nishiuchi T, Hayashi Y, et al. ; Utstein Osaka Project. Outcomes of out-of-hospital cardiac arrest by public location in the public-access defibrillation era. J Am Heart Assoc 2014;3:e000533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Blom MT, Beesems SG, Homma PC, Zijlstra JA, Hulleman M, van Hoeijen DA, et al. Improved survival after out-of-hospital cardiac arrest and use of automated external defibrillators. Circulation 2014;130:1868–75. [DOI] [PubMed] [Google Scholar]
- 23. Callawaya CW, Schmickerb RH, Brown SP, Albrichc JM, Andrusiek DL, Aufderheide TP, et al. Early coronary angiography and induced hypothermia are associated with survival and functional recovery after out-of-hospital cardiac arrest. Resuscitation 2014;85:657–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 2012;33:1787–847. [DOI] [PubMed] [Google Scholar]
- 25. Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, Boriani G, Breithardt OA, et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Europace 2013;15:1070–118. [DOI] [PubMed] [Google Scholar]