Introduction
According to the UNAIDS 2009 AIDS Epidemic Update, HIV prevalence in the Democratic Republic of Congo (DRC) is lower overall than most African countries, with a rate of 1.3 percent in adults aged 15–49 compared to 5.2 percent in sub-Saharan Africa (UNAIDS 2008). However, as many as 94,000 people were estimated to be living with HIV/AIDS in the country in 2007, with women accounting for more than half of the adults estimated to be living with the virus (UNAIDS 2008). While HIV surveillance data in the DRC are limited, prevalence estimates have suggested much higher HIV rates in the eastern urban regions of the country (WHO 2005), as well as some higher rates in certain rural areas.
Spatial Patterns and Geographic Drivers of HIV Risk
Poverty and economic deprivation have been shown to be complex yet important factors related to HIV transmission, making the study of HIV and AIDS in Africa an area in need of collaboration between natural and social scientists, including geographers (Kalipeni 2007a). Geography plays an important role in HIV transmission in the Democratic Republic of Congo and other central African countries. While population centers in east Africa are highly interconnected and the HIV epidemic has grown rapidly in this region of the continent, the low prevalence of the virus in the Democratic Republic of Congo before and after the emergence of the pandemic may be a reflection of the difficulty in travel between major population centers in central Africa (Gray 2009). Although geographic factors are important indicators of HIV prevalence, there is little current research that uses spatial analytical techniques to study local heterogeneity of HIV prevalence rates in Africa. A 2002 review by Tanser and Leseuer of the application of Geographic Information Systems (GIS) to public health problems in Africa found only one study which incorporated GIS in analyzing factors related to HIV prevalence. This study (Tanser et al. 2000) found a significant correlation between HIV prevalence rates in South Africa and proximity of homesteads to primary or secondary roads using HIV data obtained from antenatal care clinics. Since 2002, the number of national-level studies using spatial analytical methodologies to study HIV prevalence has increased (Busgeeth and Rivett 2004, Chamla et al. 2007, Kalipeni and Zulu 2008, Vanmeulebrouk et al. 2008, Tanser et al. 2009); however, to date no detailed spatial studies have been published on HIV prevalence in the DRC.
Past studies of HIV transmission in African countries have shown prevalence to be associated with geographic factors including population mobility, migrant labor routes, and proximity to urban high-transmission areas (Serwadda et al. 1992, Amat-Roze 1993, Remy 1993, Arroyo et al. 2005, Arroyo et al. 2006, Coffee et al. 2005, Coffee et al. 2007, Karim 2009). Studies that map the geographic distribution of populations at greater risk of infection, such as non-circumcised males and commercial sex workers, have been important to our understanding spatial heterogeneity in rates of HIV prevalence (Obbo 1993, Webb 1994). Unfortunately, the lack of precise spatially-referenced data in many African countries often hinders detailed geographic studies of HIV prevalence.
Socio-behavioral Factors and HIV Risk
While poverty has been shown to be significantly related to risky sexual outcomes (Dodoo 2007; Kalipeni 2007b; Masanjala 2007), the urban poor have been found to be more likely to be infected with HIV than rural poor in African countries such as Kenya, due to a greater incidence of multiple sexual partnerships in impoverished urban areas. High unemployment, financial insecurity, unstable wages, and a social context which promotes prostitution may explain such disparities across economic classes (Dodoo 2007).
It cannot be ignored that the DRC has been in and out of war since the beginning of the HIV epidemic. Persistent conflict has led to the displacement of large numbers of refugees within central African countries, eliminating much of what little employment existed and placing an even greater demand on minimal health infrastructure. The combination of chaos, poverty, population displacement, and sexual violence would seem to provide a likely setting for high rates of HIV transmission; however, we have discussed that the prevalence of HIV in the DRC is low in comparison to most sub-Saharan African countries. Surprisingly, most studies to date have found little or no relationship between HIV and conflict. A 2007 Lancet review article (Spiegel, Bennedsen, Claass, et al. 2007) found no relationship between seroprevalence and conflict. In this review, 65 studies in seven countries compared HIV seroprevalence before and after conflict, and in conflict areas or refugee camps compared to peaceful neighboring areas. Another study found no effect of widespread rape on HIV prevalence. This study suggested that even when 15% of women were raped by assailants with high HIV prevalence, overall HIV seroprevalence would only increase by 0.023% (Anema, Joffres, Mills, & Spiegel 2008). However, two studies from the DRC suggest that violence is indeed associated with an increased HIV seroprevalence, with increased HIV prevalence found among refugees compared to the general population (Kim, Malele, Kaiser, et al. 2009; Mulanga, Bazepeo, Mwamba, et al. 2004).
Also relevant to this study is recent research indicating that in many African countries, HIV prevalence is higher in women than in men ((UNAIDS 2008; UNAIDS 2009); MacPhail et al. 2002; Glynn et al. 2001; Laga et al. 2001; Zierler and Krieger 1997; Berkley et al 1990). While it has been argued that gender norms and expectations have contributed to increased risk and societal vulnerability to HIV (Masanjala 2007), Glynn et al. (2001) found that the gender discrepancy in HIV existed in Kenyan and Zambian adults despite age at sexual debut being similar in both genders and number of sexual partners being higher in men in some cases. Furthermore, they found that prevalence was very high even among women reporting only one lifetime sexual partner and few instances of sexual intercourse. Therefore, it is possible that these seemingly important behavioral factors may not explain the differences between HIV prevalence in men and women.
The gender disparity in HIV prevalence in many African countries is likely due in greater part, then, to biological factors such as the greater ease with which HIV is spread from men to women than vice versa, especially during cases of forced sex or first female intercourse. Greater prevalence of other sexually transmitted diseases such as the herpes simplex in women may further increase their biological risk of HIV infection (Glynn et al. 2001, Laga et al. 2001). It has been argued, however, that this vulnerability to infection is worsened for women by social inequalities (Kalipeni 2007a; Kalipeni 2008)
Gaps in Recent Literature
HIV prevalence in the DRC and many other African countries has often been estimated using blood samples drawn from pregnant women in antenatal clinics. While these data have been shown to provide proximate estimates of prevalence in the overall population of women and men (Pisani et al. 2000), there are obvious limitations in that these samples do not include women who are either not pregnant or do not attend antenatal care clinics, nor do they include men. Furthermore, pregnant women have been found to be at increased risk for new HIV infection (Gray et al. 2005), and knowledge of HIV status may also reduce a woman’s fertility choices. Another important limitation to sentinel surveillance systems for HIV is that almost no information is collected about the demographic or behavioral characteristics of the individual women, nor is the geographic location of their place of residence. While broad regional estimates of prevalence may be possible from this type of data, its limitations present important obstacles when attempting to analyze the socio-demographic, behavioral and geographic determinants of HIV infection.
The current study used a 2007 population-based household survey of the DRC to examine the individual and community-level factors that increase an individual’s risk for HIV infection. Geographic coordinates of the survey communities were used to map prevalence of HIV infection in the country and compute rates for areas surrounding an individual’s community, as well as to explore a number of additional geographic variables thought to be related to HIV risk. These were explored in conjunction with several demographic and behavioral characteristics extracted from the survey. Improved surveillance systems in the DRC and other African countries have the potential to greatly enhance understanding of the determinants of HIV infection as well as the spatial patterns of prevalence, therefore contributing to improved allocation of public health resources in the future.
Data and Methods
The 2007 DRC Demographic Health Surveillance (DHS) survey was a population-based, nationally representative survey linking individual HIV test results to that individual’s responses to an array of socio-demographic and behavioral characteristics. With the exception of Kinshasa which is the country’s densely-populated capital, each of the country’s eleven provinces was divided into three strata: major cities, towns, and rural areas, with a total of 34 enumeration areas created. The basis for these areas was the 1984 DRC census which contained a complete list of neighborhoods in the major cities and towns, along with territories and chiefdoms in rural areas. Neighborhoods were selected from cities and towns, and villages were selected from territories or chiefdoms. Within these neighborhoods or villages, households were then selected. The population sampling scheme did not exclude those areas heavily plagued by conflict; however, it must be considered that conflict does affect short-term migration patterns and the sampling scheme could not account for changes in the underlying population distribution since the 1984 census.
In total, nine thousand households in 300 communities (neighborhoods or villages) were targeted for the 2007 DRC. DHS (3,690 in urban areas and 5,310 in rural areas). Of these 9,000 households, 99.3% were successfully identified and interviewed. This included 4,757 men aged 15–49 years, all of whom were tested for infection with HIV, as well as 9,995 women aged 15–49 years, half of whom were tested for HIV. Of the nearly 9,000 individuals tested for HIV, 1.3 % were found to be HIV-positive, with 0.9 % of men testing positive and nearly double the proportion in women at 1.6 (Demographic and Health Surveys, 2008).
Geographic coordinates of the 300 community centroids (mean centers) were also collected. For privacy purposes, these geographic coordinates were randomly displaced by 5 km in rural areas and 2 km in urban areas. The number of respondents in each community ranged from 14 to 53 individuals, with an average of 30 individuals per community. The proportion of HIV-positive individuals was computed for men, women, and both genders combined for each community taking the sampling weights of the survey into account. Using the geographic coordinates of the communities, “hotspots”, or communities with HIV prevalence which is higher than would be expected from a random disease distribution, were detected using a Poisson-based spatial scan statistic that adjusts for the underlying populations in each survey community using SatScan v8.0.1 (Kulldorff 1997, 2006). This spatial scan statistic looks for these “hotspots” by taking into consideration the rates of nearby clusters across multiple spatial scales, minimizing the potential for error resulting from the small sample sizes within each individual cluster of households. It must be noted, however, that in areas of the country where the survey communities were farther apart from one another, the spatial scan statistic may be less robust.
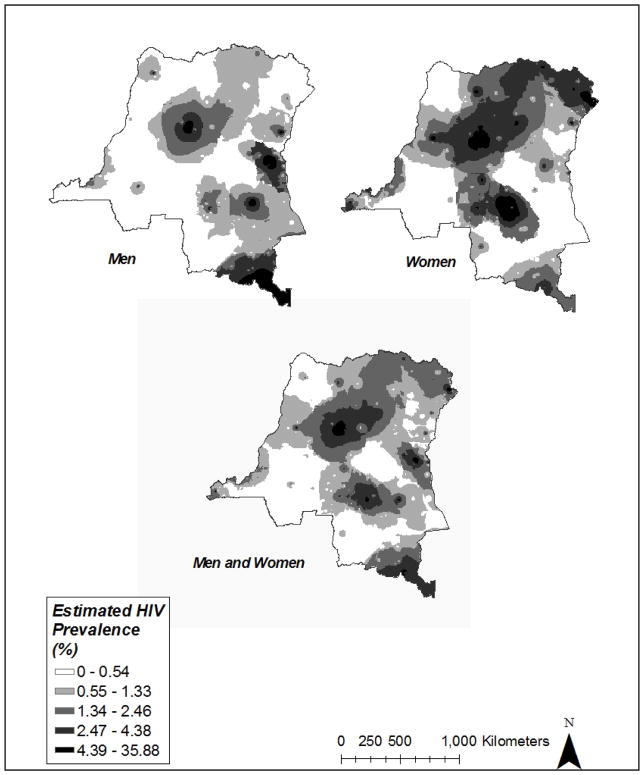
A visualization of the spatial patterns of HIV prevalence in the DRC was created by computing smoothed surfaces of prevalence for men, women, and both genders combined using inverse distance weighting (IDW) in the GIS software ArcGIS 9.3 (ESRI, Redlands CA). IDW uses nearby values to predict those in unmeasured locations. In this procedure, known values closest to the unmeasured location have greater influence on the interpolated values than those farther away. The estimated prevalence in a minimum of 2 and a maximum of 15 of the nearest communities were used to interpolate prevalence for each unmeasured 1 km-by-1 km cell in the resulting surfaces. As subsequently discussed in further detail, these smoothed surfaces were also used to create regional-level HIV prevalence predictor variables to be included in individual-level multivariate statistical models of HIV risk.
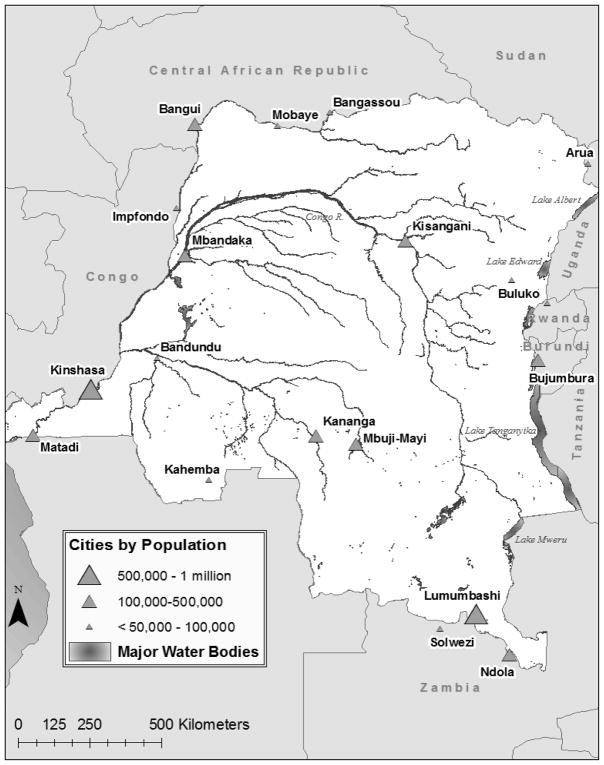
Figure 1 is provided as a reference to the study area, showing cities in and near the DRC as well as major rivers and inland water bodies. GIS layers for water bodies and roads were obtained from the Digital Chart of the World (DCW) (ESRI 1991) and used to compute the distance from the community centroid to the nearest primary or secondary road, nearest river or major water body, and nearest city in kilometers. These geographic indicators serve as measures of proximity to trade and migratory routes. It must be noted that while the DCW dataset is the most recent data available for determining the locations of roads, it is likely that in the face of economic collapse many of the roads have changed or disappeared since 1991.
Figure 1.
Map of the DRC, including major water bodies and cities within 25 km.
A geographic database of armed conflict and refugee camp locational data was also compiled. The Armed Conflict Locational Event Dataset (ACLED) includes locations, dates, and additional characteristics of individual battle events in states affected with civil war (Raleigh & Hegre 2005). The current dataset covers eight conflict areas in West and Central Africa including the DRC and surrounding countries from 1960 through 2006. We computed the number of conflict events within several distance buffers of the community centroids (10, 25, and 100 km), aggregating events temporally into two categories: (1) all events between 1960 and 2006, and (2) only those events occurring within ten years of the survey year (since 1997). The locations of current refugee camps in the DRC and all surrounding countries were also obtained from the United Nations Human Rights Council. The distance of a community centroid to a refugee camp was computed, as well as the density of camps within the three different distance buffers.
Additional geographic indicator variables computed for this study included the average HIV prevalence and population per square kilometer within 10-, 25- and 100-kilometer buffers around each survey community. These were computed using the interpolated surfaces described above and a DRC population density grid (SEDAC 2008).
Both the female and male questionnaires asked detailed questions regarding socio-demographic characteristics, sexual activity and risk behaviors associated with HIV/AIDS. Items related to the age, gender, education, wealth, sexual behaviors and rural or urban residence of the respondents were extracted from the survey and examined in conjunction with the computed geographic indicator variables for their relationship to HIV risk in DRC individuals.
The socio-demographic, behavioral and geographic indicators described above were entered into three multivariate logistic regression models using Stata v. 10 (StataCorp LP, College Station TX), including separate models for men and women as well as a model for both genders combined. Correction for unobserved random errors at the community level was included as part of all three models. The dependent variable in all models was the individual’s HIV status, and independent variables initially entered into the models included the respondent’s age, gender (combined model only), education in single years, total number of lifetime sex partners, the distance of the respondent’s community to the nearest road, water body, and city, the population density and HIV prevalence within the 10-, 25-, and 100-km buffers, the described conflict-related variables, and whether the respondent resides in a rural or urban community. Although the DHS survey provided many behavioral variables of interest, due to the low prevalence of HIV in both men and women in the DRC, only very simple statistical models with a small number of parameters could be used to predict risk for infection and the variables described above were considered to be the most important to enter into our models. The best-fitting model for the entire survey population as well as each gendered subset was selected using Akaike’s Information Criterion (AIC), a goodness-of-fit statistic which favors parsimony by making a tradeoff between the precision and complexity of each model (Burnham and Anderson 2002).
Results
Spatial Patterns in DRC HIV Prevalence
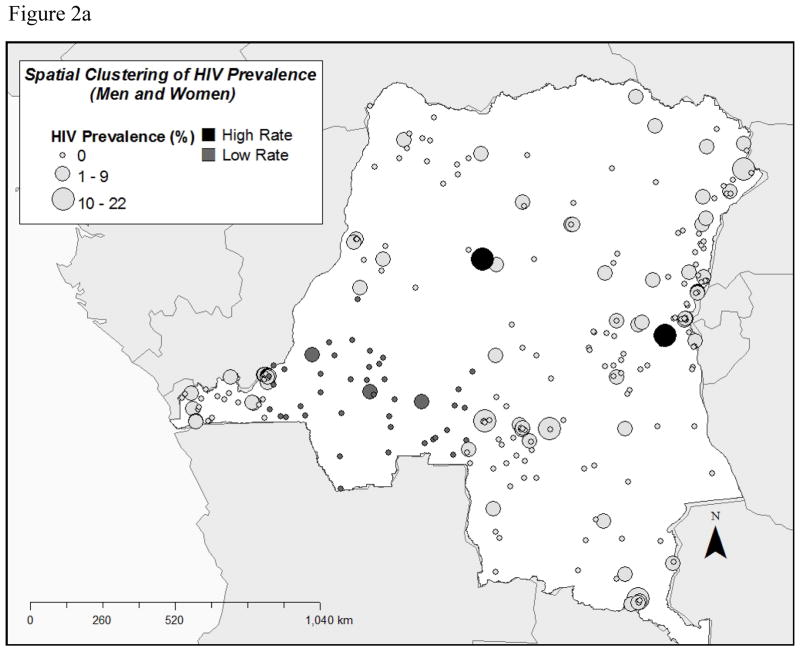
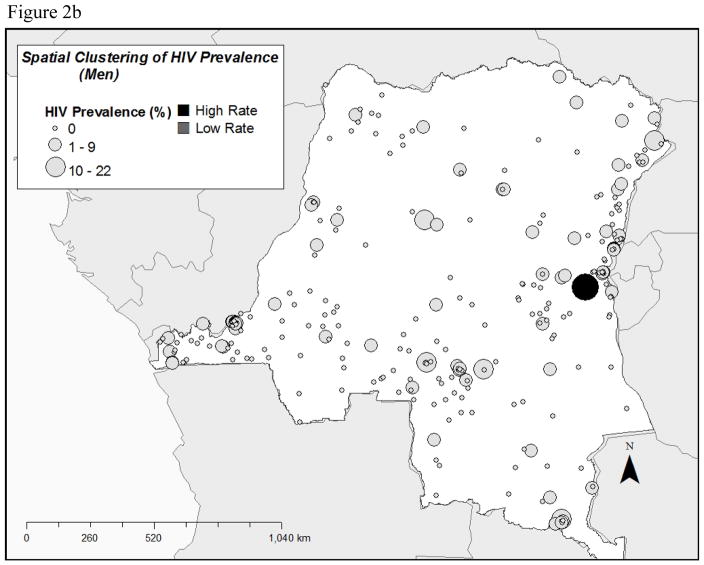
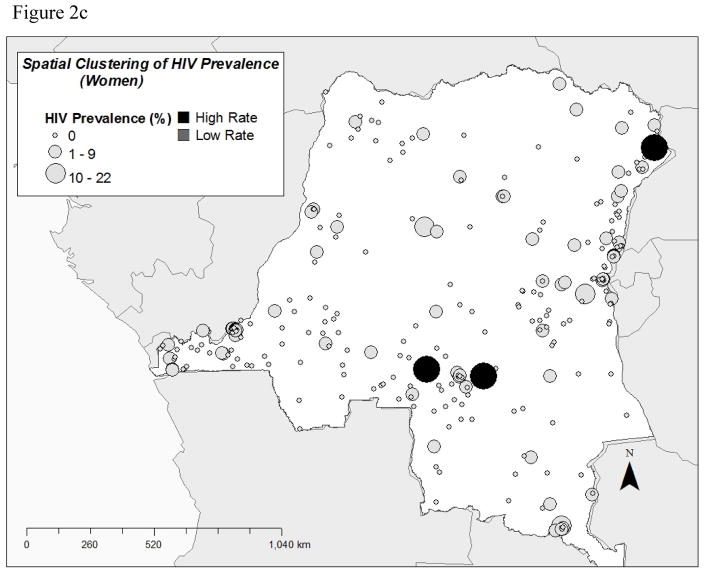
Figures 2a through 2c display the results of the Kulldorff spatial scan statistic for HIV prevalence in all survey respondents, as well as for each gender separately. Each circle represents a community centroid and is sized according to the HIV prevalence of the community. As mentioned above, the spatial scan statistic takes into account the prevalence in neighboring communities as well. Areas found to have rates that are significantly higher than would be expected from a random distribution are shown along with those whose rates are significantly lower than would be expected. Overall, lower rates tend to be found in the southwest portion of the country, while higher rates are found in the north and west of the country as seen in Figure 2a. Figure 2b indicates that the high rate found in Kivu is likely accounted for by high prevalence of male HIV infection, while Figure 2c indicates that higher than expected rates of female infection are found further to the north as well as to the south of this male HIV hotspot.
Figure 2.
Figure 2a. Results of the Kulldorff spatial scan statistic for HIV prevalence in DRC men and women.
Figure 2b. Results of the Kulldorff spatial scan statistic for HIV prevalence in DRC men.
Figure 2c. Results of the Kulldorff spatial scan statistic for HIV prevalence in DRC women.
Figure 3 reinforces the impression of the differences in the spatial patterns between male and female HIV prevalence in the DRC. While overall, the southwest and northeast regions of the country exhibit low HIV prevalence, areas of high prevalence are not identical for men and women. While there tends to be higher infection amongst women in the upper northeast corner of the country, this is an overall low-prevalence region for men. On the contrary, the southernmost tip of the country near Lubumbashi is an area of high prevalence for men, while similar high rates are not seen for women. Overall, heterogeneity in prevalence for the entire population, as well as for men and women separately, can be seen upon examination of these interpolated surfaces, with estimated rates as high as 30.5 percent in some areas as compared to the country’s overall HIV prevalence of less than 2 percent. Such patterns indicate that some factor or set of factors is contributing to increased risk in certain parts of the country.
Figure 3.
Interpolated surfaces of HIV prevalence in the DRC.
Multivariate Analyses
Five variables were retained in both the overall and female-only models, while only three variables were retained in the male-only model after selection using the AIC criterion (Table 1). In all models, individual HIV outcome is the dependent variable. No relationship was found in any of our models between HIV status and education, population density, urban versus rural place of residence, or conflict or refugee camp density. When men and women were considered together, age, the total number of lifetime sexual partners, and HIV prevalence within 25 kilometers of one’s community were all positive predictors of HIV infection, while distance to a city was a negative predictor of infection. Men were also 71 percent less likely than women to be infected with HIV in the DRC.
Table 1.
Parameter estimates for the variables retained in the logistic regression models explaining individual HIV in men and women.
| Parameter | Men | Women | Men and Women |
|---|---|---|---|
| Age | 0.042*** | 0.020* | |
| Wealth index (1–5) | 0.370** | ||
| Total lifetime no. of sexual partners | 0.016* | 0.034* | 0.015* |
| Distance to a city (km) | −0.005*** | −0.004*** | |
| Distance to a water body (km) | 0.117* | ||
| HIV prevalence within 25 km of community (%) | 0.491*** | 0.370*** | 0.430*** |
| Male | N/A | N/A | −0.710** |
|
| |||
| Number of Observations | 3325 | 3849 | 7174 |
| Log Likelihood | −172.5 | −309.3 | −490.7 |
| AIC | 351.0 | 628.6 | 991.4 |
=p<.001
=p<.01
=p<.05
Considered separately, the model results for both men and women indicate that an individual’s total number of lifetime sexual partners as well as the HIV prevalence within 25 kilometers of his or her community were both positively associated with the probability of being infected with HIV, with the total number of lifetime sexual partners further showing a correlation of more than double the magnitude with women’s HIV prevalence than men’s. In women, age and distance to a river or water body were also positively associated with HIV infection, while distance to a city was negatively associated. In men, wealth was positively associated with HIV infection, while it was not an important factor in a woman’s likelihood of being infected with HIV.
Conclusions and Discussion
This study has shown the importance of considering socio-demographic, behavioral and geographic factors in conjunction when determining individuals’ risk for HIV infection in the DRC. Individual characteristics and sexual behaviors including age, gender, wealth and number of sexual partners are shown to be associated with increased risk for HIV infection. Most notably, our findings in the DRC are concurrent with recent literature highlighted in the background section of this paper citing that women are significantly more likely to become infected with HIV in many sub-Saharan African countries. We also noted in our results that the total number of lifetime sexual partners showed a correlation of more than double the magnitude with women’s HIV prevalence than men’s, supporting the literature discussed in the background section of this paper which suggests women may be biologically at greater risk for HIV infection than men. The significant positive relationship between age and HIV status in the women-only and overall models indicates that exposure time is important in terms of the likelihood of becoming infected with the virus. The greater significance and magnitude of the relationship with this variable in the women-only model may be related to more lifetime exposure to partner violence with increasing age (Maman 2002). Our results also indicate that wealth shows no relationship in our overall or women-only models; however, a significant positive relationship was found between wealth and men’s HIV status, likely due to increased travel and extramarital sex in wealthier men (Gillespie 2007; Kimuna 2005).
It is also notable that the prevalence of HIV within 25 kilometers of an individual’s community is highly significant in all three models. The greater significance of the 25-kilometer buffer of HIV prevalence in comparison to the 100-km buffers is unsurprising in that people in the DRC are likely partaking in sexual intercourse with people who live closer to them rather than farther away. While small sample sizes within community household clusters may have lead to exaggerated rates in certain areas, a particularly high HIV prevalence in one 25 km area is not likely to have a significant impact in a model in which persons are grouped into 300 clusters.
While living in an urban community itself is not a significant contributor to any of the three models, the negative association found with the geographic variable (distance to a city) in the overall and women-only models indicates that even individuals who do not live in urban areas may be exposed to higher risk for HIV infection if they live close to these urban areas and their associated high-risk sexual networks. It is not clear why this variable is not significant when men’s HIV status is modeled alone, but its significance in the women-only and overall model indicates that access to or living in cities places DRC individuals at a greater risk for HIV transmission.
When controlling for other factors, the average population density near an individual’s community and distance to roads are not shown to be significant, and the distance to the nearest river is shown to be positively associated with female HIV prevalence, which is contrary to the expected relationship. A large portion of the DRC is without primary or secondary roads, particularly in the central part of the country where the Congo River Basin lies. The terrain and climate of the basin present severe barriers to road construction, and persistent economic mismanagement and domestic conflict has led to serious underinvestment in transportation for many years, with only 2,250 km of paved roads, few of which remain in good condition (Gauthier and Guepin 2006). In contrast, the DRC has thousands of kilometers of navigable waterways, and thus water transport has traditionally been the primary means of moving about the country. Therefore, it is surprising that the distance to a river is not negatively associated with HIV infection overall or in men, and furthermore that it is positively associated with HIV infection in women, as access to transportation routes would likely increase one’s exposure to trade and migratory routes as well as facilitate access to high-risk urban areas. Further information about the navigability of the rivers in the DCW dataset would be necessary in order to fully assess this relationship.
A finding meriting further study is the relationship between conflict and HIV prevalence in the DRC. While the current study found no relationship between proximity to or density of conflict events within several distances, either since 1960 or since 1997, or the proximity to or density of current refugee camps, patterns of migration between neighboring countries and high-conflict regions would be necessary in order to confirm our findings that conflict does not seem to affect HIV prevalence in the DRC. A limitation of the current study also lies in the fact that no information about personal experience of violence, especially rape, was available and should be addressed in order to confirm our findings. It is also possible that population movement from conflict plays an important role in the spatial distribution of HIV clades, or subtypes, found across the country (Laga, Matendo, & Buve 2008), even if it does not affect overall HIV prevalence. This is a question that also merits further research.
The geographic pattern of prevalence estimated using the DHS survey results confirms the 2005 WHO estimates from antenatal clinic data that higher HIV prevalence exists in the eastern parts of the DRC. However, much more locally heterogeneous patterns are found in this study by using a population-based survey and spatial statistical techniques, and most importantly the differences in the locations of high-prevalence areas for men and women are highlighted. Having access to counseling, testing services and treatment facilities is essential for controlling HIV incidence. Understanding the geographic distribution of prevalence may be of great importance when determining where to locate these services. In particular, our study findings show that targeting interventions and sentinel surveillance sites may be most effective if they were to be implemented in the north eastern border of the Orientale province, the eastern border of Kivu, and the southeast corner of Equateur. High rates in the southern portions of Kasai-Occidental and Kasai-Oriental as well as in the southern tip of the Katanga province near Lubumbashi should also be considered for sentinel surveillance.
To date, this is the largest study examining factors associated with increased risk for HIV infection in the DRC. A better understanding of the geographic distribution of HIV-infected populations is essential in assessing the magnitude of the epidemic in certain parts of the DRC and for allocating better treatment and support services to those who are infected. This study has exhibited the potential for using spatial methods in conjunction with population-based surveys in order to help predict HIV prevalence based on known socio-demographic, behavioral and geographic factors associated with risk. While the region of residence was included in the DHS survey, using region as a predictor in the analysis would not have allowed such a fine scale computation of geographic variables which were built into the GIS according to communities rather than large-scale regions. Modeling the spatial distribution of HIV prevalence at the local scale allows for the exploration of sub-regional heterogeneity in the DRC, an important step towards efficient intervention planning.
Contributor Information
JP Messina, Department of Zoology, University of Oxford.
M Emch, Department of Geography, Department of Epidemiology, Carolina Population Center, University of North Carolina at Chapel Hill.
J Muwonga, Ministry of Health, Democratic Republic of Congo.
K Mwandagalirwa, Kinshasa School of Public Health, University of Kinshasa.
SB Edidi, Ministry of Health, Democratic Republic of Congo.
N Mama, Ministry of Health, Democratic Republic of Congo.
A Okenge, Ministry of Health, Democratic Republic of Congo.
SM Taylor, Department of Epidemiology, University of North Carolina at Chapel Hill.
SR Meshnick, Department of Epidemiology, University of North Carolina at Chapel Hill.
References
- Amat-Roze JM. Geographic inequalities in HIV infection and AIDS in sub- Saharan Africa. Social Science & Medicine (1982) 1993;36(10):1247–1256. doi: 10.1016/0277-9536(93)90214-o. [DOI] [PubMed] [Google Scholar]
- Anema A, Joffres MR, Mills E, Spiegel PB. Widespread rape does not directly appear to increase the overall HIV prevalence in conflict-affected countries: So now what? Emerging Themes in Epidemiology. 2008;5:11. doi: 10.1186/1742-7622-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arroyo MA, Hoelscher M, Sateren W, Samky E, Maboko L, Hoffmann O, et al. HIV-1 diversity and prevalence differ between urban and rural areas in the Mbeya region of Tanzania. AIDS (London, England) 2005;19(14):1517–1524. doi: 10.1097/01.aids.0000183515.14642.76. [DOI] [PubMed] [Google Scholar]
- Arroyo MA, Sateren WB, Serwadda D, Gray RH, Wawer MJ, Sewankambo NK, et al. Higher HIV-1 incidence and genetic complexity along main roads in Rakai district, Uganda. Journal of Acquired Immune Deficiency Syndromes (1999) 2006;43(4):440–445. doi: 10.1097/01.qai.0000243053.80945.f0. [DOI] [PubMed] [Google Scholar]
- Berkley S. AIDS and HIV infection in Uganda-are more women infected than men? AIDS (London) 1990;4(12):1237. doi: 10.1097/00002030-199012000-00009. [DOI] [PubMed] [Google Scholar]
- Burnham KP, Anderson DR. Model selection and multimodel inference: A practical information-theoretic approach. New York, NY: Springer Publishing; 2002. [Google Scholar]
- Busgeeth K, Rivett U. The use of a spatial information system in the management of HIV/AIDS in South Africa. International Journal of Health Geographics. 2004;3(1):13. doi: 10.1186/1476-072X-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamla DD, Olu O, Wanyana J, Natseri N, Mukooyo E, Okware S, et al. Geographical information system and access to HIV testing, treatment and prevention of mother-to-child transmission in conflict affected northern Uganda. Conflict and Health. 2007;1:12. doi: 10.1186/1752-1505-1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffee M, Lurie MN, Garnett GP. Modelling the impact of migration on the HIV epidemic in South Africa. AIDS (London, England) 2007;21(3):343–350. doi: 10.1097/QAD.0b013e328011dac9. [DOI] [PubMed] [Google Scholar]
- Coffee MP, Garnett GP, Mlilo M, Voeten HA, Chandiwana S, Gregson S. Patterns of movement and risk of HIV infection in rural Zimbabwe. The Journal of Infectious Diseases. 2005;191(Suppl 1):S159–67. doi: 10.1086/425270. [DOI] [PubMed] [Google Scholar]
- Demographic and Health Surveys. Democratic Republic of Congo – HIV Fact Sheet. 2008 Retrieved from ( http://www.measuredhs.com/pubs)
- Dodoo F. Urban–rural differences in the socioeconomic deprivation–Sexual behavior link in Kenya. Social Science & Medicine (1982) 2007;64(5):1019–1031. doi: 10.1016/j.socscimed.2006.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ESRI. Environmental Systems Research Institute Digital Chart of the World data set. 1991 Retrieved from ( http://www.esri.com/data/data-maps/index.html)
- Gauthier JM, Guepin L. [accessed 4/30/2009];DRC Snapshot – Roads in the DRC. 2006 Retreived from UN Joint Logistics Centre ( http://www.unjlc.org/drc)
- Gillespie SS. Is poverty or wealth driving HIV transmission? AIDS (London) 2007;21(suppl 7):S5–S16. doi: 10.1097/01.aids.0000300531.74730.72. [DOI] [PubMed] [Google Scholar]
- Glynn JR. Why do young women have a much higher prevalence of HIV than young men? A study in Kisumu, Kenya and Ndola, Zambia. AIDS (London) 2001;15:S51. doi: 10.1097/00002030-200108004-00006. [DOI] [PubMed] [Google Scholar]
- Gray RH, Li X, Kigozi G, Serwadda D, Brahmbhatt H, Wabwire-Mangen F, et al. Increased risk of incident HIV during pregnancy in Rakai, Uganda: A prospective study. Lancet. 2005;366(9492):1182–1188. doi: 10.1016/S0140-6736(05)67481-8. [DOI] [PubMed] [Google Scholar]
- Gray RR. Spatial phylodynamics of HIV-1 epidemic emergence in east Africa. AIDS (London) 2009;23(14):F9–F17. doi: 10.1097/QAD.0b013e32832faf61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalipeni E. HIV/AIDS, gender, agency and empowerment issues in Africa. Social Science & Medicine (1982) 2007a;64(5):1015–1018. doi: 10.1016/j.socscimed.2006.10.010. [DOI] [PubMed] [Google Scholar]
- Kalipeni E. Concern and practice among men about HIV/AIDS in low socioeconomic income areas of Lilongwe, Malawi. Social Science & Medicine (1982) 2007b;64(5):1116–1127. doi: 10.1016/j.socscimed.2006.10.013. [DOI] [PubMed] [Google Scholar]
- Kalipeni EE. HIV/AIDS in women: Stigma and gender empowerment in Africa. Future HIV Therapy. 2008;2(2):147–153. [Google Scholar]
- Karim SS. Commentary: Spatial clustering of HIV infection: Providing clues for effective HIV prevention. International Journal of Epidemiology. 2009 doi: 10.1093/ije/dyp201. [DOI] [PubMed] [Google Scholar]
- Kim AA, Malele F, Kaiser R, Mama N, Kinkela T, Mantshumba JC, et al. HIV infection among internally displaced women and women residing in river populations along the congo river, democratic republic of congo. [Electronic version] AIDS and Behavior. 2009;13(5):914–920. doi: 10.1007/s10461-009-9536-z. [DOI] [PubMed] [Google Scholar]
- Kimuna SR. Wealth and extramarital sex among men in zambia. [Electronic version] International Family Planning Perspectives. 2005;31(2):83. doi: 10.1363/3108305. [DOI] [PubMed] [Google Scholar]
- Kulldorff M. A spatial scan statistic, Communications in Statistics: Theory and Methods. 1997;26(1997):1481–1496. [Google Scholar]
- Kulldorff M. SaTScan user guide for version 7.0. 2006;(2006) Retrieved from ( http://www.satscan.org/techdoc.html)
- Laga M. To stem HIV in Africa, prevent transmission to young women. AIDS (London) 2001;15(7):931. doi: 10.1097/00002030-200105040-00014. [DOI] [PubMed] [Google Scholar]
- Laga M, Matendo R, Buve A. Chapter 11: The situation in the cradle of AIDS: Congo and central africa. In: Celentano D, Beyrer C, editors. Public health aspects of HIV/AIDS in low and middle income countries. New York: Springer; 2008. p. 196. [Google Scholar]
- MacPhail CC. Relative risk of HIV infection among young men and women in a South African township. International Journal of STD & AIDS. 2002;13(5):331–342. doi: 10.1258/0956462021925162. [DOI] [PubMed] [Google Scholar]
- Maman SS. HIV-positive women report more lifetime partner violence: Findings from a voluntary counseling and testing clinic in Dar es Salaam, Tanzania. American Journal of Public Health (1971) 2002;92(8):1331–1337. doi: 10.2105/ajph.92.8.1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masanjala W. The poverty-HIV/AIDS nexus in Africa: A livelihood approach. Social Science & Medicine (1982) 2007;64(5):1032–1041. doi: 10.1016/j.socscimed.2006.10.009. [DOI] [PubMed] [Google Scholar]
- Mokili J, Korber B. The spread of HIV in Africa. Journal of Neurovirology. 2005;11(Suppl 1):66–75. [PubMed] [Google Scholar]
- Mulanga C, Bazepeo SE, Mwamba JK, Butel C, Tshimpaka JW, Kashi M, et al. Political and socioeconomic instability: How does it affect HIV? A case study in the Democratic Republic of Congo. AIDS (London, England) 2004;18(5):832–834. doi: 10.1097/00002030-200403260-00024. [DOI] [PubMed] [Google Scholar]
- Obbo C. HIV transmission through social and geographic networks in Uganda. Social Science & Medicine (1982) 1993;36(7):949–955. doi: 10.1016/0277-9536(93)90086-j. [DOI] [PubMed] [Google Scholar]
- Pisani E, Schwartländer B, Cherney S, Winter A. Report on the global HIV/AIDS epidemic – June 2000. Joint United Nations Programme on HIV/AIDS (UNAIDS) 2000 [Google Scholar]
- Raleigh C, Hegre H. Introducing ACLED: An armed conflict location and event dataset. Disaggregating the study of civil war and transnational violence; San Diego, CA. 2005. [Google Scholar]
- Remy G. Geographic distribution of HIV-1 infection in central Africa: remarkable discontinuities. Annales De La Societe Belge De Medecine Tropicale. 1993;73(2):127–142. [PubMed] [Google Scholar]
- Serwadda D, Wawer MJ, Musgrave SD, Sewankambo NK, Kaplan JE, Gray RH. HIV risk factors in three geographic strata of rural Rakai district, Uganda. AIDS (London, England) 1992;6(9):983–989. doi: 10.1097/00002030-199209000-00012. [DOI] [PubMed] [Google Scholar]
- Siegfried N, Clarke M, Volmink J. Randomised controlled trials in africa of HIV and AIDS: Descriptive study and spatial distribution. BMJ (Clinical Research Ed) 2005;331(7519):742. doi: 10.1136/bmj.331.7519.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Socioeconomic Data and Applications Center (SEDAC) Gridded Population of the World data set. 2008 Retrieved from ( http://sedac.ciesin.columbia.edu/gpw/)
- Sokal DC, Buzingo T, Nitunga N, Kadende P, Standaert B. Geographic and temporal stability of HIV seroprevalence among pregnant women in Bujumbura, Burundi. AIDS (London, England) 1993;7(11):1481–1484. doi: 10.1097/00002030-199311000-00012. [DOI] [PubMed] [Google Scholar]
- Spiegel PB, Bennedsen AR, Claass J, Bruns L, Patterson N, Yiweza D, et al. Prevalence of HIV infection in conflict-affected and displaced people in seven sub-Saharan African countries: A systematic review. Lancet. 2007;369(9580):2187–2195. doi: 10.1016/S0140-6736(07)61015-0. [DOI] [PubMed] [Google Scholar]
- Tanser F. Methodology for optimising location of new primary health care facilities in rural communities: A case study in KwaZulu-natal, South Africa. Journal of Epidemiology and Community Health. 2006;60(10):846–850. doi: 10.1136/jech.2005.043265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanser F, Barnighausen T, Cooke GS, Newell ML. Localized spatial clustering of HIV infections in a widely disseminated rural South African epidemic. International Journal of Epidemiology. 2009 doi: 10.1093/ije/dyp148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanser F, Gijsbertsen B, Herbst K. Modelling and understanding primary health care accessibility and utilization in rural South Africa: An exploration using a geographical information system. Social Science & Medicine (1982) 2006;63(3):691–705. doi: 10.1016/j.socscimed.2006.01.015. [DOI] [PubMed] [Google Scholar]
- Tanser F, Lesueur D, Solarsh G, Wilkinson D. HIV heterogeneity and proximity of homestead to roads in rural South Africa: An exploration using a geographical information system. Tropical Medicine & International Health : TM & IH. 2000;5(1):40–46. doi: 10.1046/j.1365-3156.2000.00513.x. [DOI] [PubMed] [Google Scholar]
- Tanser FC, Le Sueur D. The application of geographical information systems to important public health problems in Africa. International Journal of Health Geographics. 2002;1(1):4. doi: 10.1186/1476-072X-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. 2009 AIDS epidemic update. 2009 Retrieved from ( http://www.unaids.org/en/knowledgecentre/resources/publications)
- UNAIDS. 2008 report on the global AIDS epidemic. 2008 Retrieved from ( http://www.unaids.org/en/knowledgecentre/resources/publications)
- Vanmeulebrouk B, Rivett U, Ricketts A, Loudon M. Open source GIS for HIV/AIDS management. International Journal of Health Geographics. 2008;7:53. doi: 10.1186/1476-072X-7-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb D. Mapping the AIDS pandemic: Geographical progression of HIV in South Africa 1990–93. Nursing RSA = Verpleging RSA. 1994;9(9):20–21. [PubMed] [Google Scholar]
- World Health Organization. Democratic Republic of the Congo: Summary Country Profile for HIV/AIDS Treatment Scale-Up. 2005 Retreived from ( http://www.who.int/publications)