Abstract
The current study extends the findings of Scogin et al. (2007) by exploring the role of social support in changes in quality of life resulting from home-delivered cognitive behavioral therapy (CBT). One hundred thirty-seven participants, characterized primarily as rural, low resource, and frail, were randomly assigned to either CBT or a minimal support control condition. Hierarchical regression revealed that positive change in satisfaction with social support was associated with improvement in quality of life beyond the effects of the CBT treatment. In addition, pretreatment satisfaction with social support, and change in satisfaction with social support moderated the effect of CBT on quality of life. These results suggest that bolstering social support concomitant to CBT may increase quality of life.
Keywords: cognitive behavioral therapy, older adults, quality of life, social support
As the present society ages and undergoes changes in social structure, such as a lower birth rate, urbanization, and a tendency for smaller family units, ever-greater focus will be needed on the unique psychological issues of older adults. Although social support and quality of life have received much attention in studies of the psychological issues of older adults, findings are yet to be extended to a variety of populations. This is particularly noteworthy given that social relations largely depend on the cultural background and structure of a society (Saito, Sagawa, & Kanagawa, 2005). Moreover, empirical studies of the psychological wellbeing of rural older adults are scarce. More research is needed to understand their unique psychological needs, particularly given that rural older adults often lack health care access. The current study explores the role of social support in overall quality of life in this underserved population.
Serving the mental health needs of rural older adults brings unique challenges. Williams and Cutchin (2002) outline several of these barriers to care, which include provider supply, distribution and availability of providers, provider recruitment and retention, and service access. Rural older adults are also faced with out-migration of young persons, leaving them more vulnerable to physical, mental, and economic issues (Rogers, 1999). Among rural older adults who do receive care, rural caregivers tend to be economically disadvantaged, have less education, and have poorer housing compared to their urban counterparts (Wang et al., 2005). Moreover, cultural shifts within rural communities along with the competing values of traditional and biomedical healing practices suggest that rural areas are as complex, diverse, and in need as urban areas (Williams & Cutchin, 2002). Given these complications, social support among rural older adults may take on added value in serving their psychological wellbeing.
Social support is broadly defined as the perceived availability of support, affection, and instrumental aid from significant social partners, including family members, close friends, neighbors, and coworkers (Antonucci, 1994; Cantor, 1979; Shumaker & Hill, 1991). Theoretical models of social support have emphasized that it helps to buffer stress and depression while enhancing an individual’s morale, health, and wellbeing (Berkman, 2000; Schaefer, Coyne, & Lazarus, 1981). According to Taylor (1999), social support may include emotional support (affection, acceptance, or approval), instrumental support (assistance with self-management or financial support for medications), informational support (providing education, advice, or information), and affirmational support (validating self-care-related behaviors and efforts).
Social support may be further broken down into self-reported social support frequency versus self-reported perceived social support (satisfaction with that support). These types of support are conceptually unique, given that, for example, one may have a large social network but be unhappy with the quality of that support (Beckner, Howard, Vella, & Mohr, 2010). Moreover, a meta-analysis of the relation between received and perceived social support revealed only a modest average correlation (Haber, Cohen, Lucas, & Baltes, 2007). Other studies have taken a more expansive view of perceived social support, encompassing one’s beliefs about types, amounts, and experiences of support (e.g., Richmond, Ross, & Egeland, 2007; Zhao et al., 2011), which may be distinctive from actual support provided. However, the current study takes a narrower conception of perceived social support with the aim of measuring its psychological benefits (i.e. satisfaction with support received), while frequency of support refers to the number and density of social contacts. This approach is due to the numerous studies that have found that satisfaction with social support may enhance wellbeing more so than frequency of social support received (e.g., Beedie & Kennedy, 2002; Rintala, Young, Hart, Clearman, & Fuhrer, 1992). According to Cohen and Willis (1985), this is because quality of social support enhances wellbeing through a perceived availability of interpersonal resources, particularly in stressful situations.
Quality of life evolved from the constructs of life satisfaction and subjective well-being (Frisch, 1994b), and it represents an individual’s subjective interpretation of the extent to which his or her most important needs, goals, and desires have been satisfied (Frisch, 1998). Quality of life theory integrates existing theories of depression with the subjective wellbeing literature (Frisch, Cornell, Villanueva, & Retzlaff, 1992; Lewinsohn, Redner, & Seeley, 1991), forming the unified construct of quality of life (Frisch, 1994b). The term “quality of life” may be used interchangeably with “life satisfaction,” (Frisch, Cornell, Villanueva, & Retzlaff, 1992) and both terms are components of the larger construct of subjective wellbeing or happiness (Andrews & Withey, 1976; Diener, 1984; Veenhoven, 1984). The current study uses the term “quality of life” and is conceptualized according to Frisch (1994b), encompassing health, psychological, economic, and social domains. An upward shift in life expectancy presents the need for more focus on quality of life, particularly because old age is often associated with health problems and irreversible decrease in functional capacity (Chalise, Saito, Takahashi, & Kai, 2007; Osborne, Hawthorne, Lew, & Gray, 2003).
Empirical studies of the relation between social support and quality of life in older adults suggest a positive relation across contexts. For example, Sherman et al. (2006) examined the role of health-related quality of life for 364 older adults with osteoarthritis, finding that perceived social support was positively related to baseline measures of quality of life. At 18-month follow-up, social support significantly predicted reduced depressive symptoms and increased life satisfaction (Sherman et al., 2006). More recently, Low, Molzahn, and Kalfoss (2008) explored the effects of health appraisal, morbidities, social support transitions (intimacy), and the environment on quality of life on older adults in Canada and Norway. In both samples, perceptions of available social support significantly predicted quality of life, with cognitive developmental transitions (behavioral adjustment to changing life conditions) mediating the effect (Low, Molzahn, & Kalfoss, 2008).
Other longitudinal studies have examined trajectories of quality of life among older adults. In one such study of older adults in Britain, Zaninotto, Falaschetti, and Sacker (2009) gathered data from 11,392 individuals in three waves across a four-year period to examine age trajectories in quality of life. They found that fewer numbers of friends and lower perceived social support predicted lower quality of life in older adults, concluding that younger old adults can be prepared for further aging by increasing social support and engaging in the wider community while they are able. In another study of British older adults, Netuveli, Wiggins, Hildon, Montgomery, and Blane (2006) found that quality of life in older adults could be improved by changes in various psychosocial factors, including improving trusting relationships with family, increasing contact with friends, and living in socially supportive neighborhoods.
Studies of social support and quality of life pertaining to rural older adults are scarce. In one of the only studies of this population, Theeke, Goins, Moore, and Campbell (2012) examined the relation between loneliness, depression, perceived social support, and quality of life in older chronically ill Appalachians. Theeke et al. found that self-identification of loneliness correlated with lower quality of life and social support, concluding that the low emotional support inherent in loneliness leads to reduced overall wellbeing. The authors also noted that the participants of this study reported relatively high quality of life scores in the face of loneliness, poverty, and chronic illness, suggesting the possibility of lower life or cultural expectations among this population.
Despite the numerous studies linking social support with quality of life, empirical research is limited regarding the role of social support in psychotherapy’s impact on quality of life, particularly as it pertains to rural older adults. Moreover, studies of quality of life have been inconsistent in how it is measured, with many focusing on health quality of life. The current study addresses the need for more research with overall quality of life as an outcome, which may yield different findings. This study may also aid in understanding the underlying mechanisms of psychotherapy that enhance quality of life, which may in turn benefit underserved populations whose primary resource may be their social support. Although some studies suggest that satisfaction with social support positively predicts better outcome for depression (e.g., George, Blazer, Hughes, & Fowler, 1989; Nasser & Overholser, 2005) and that CBT increases quality of life (e.g., Scogin et al., 2007), little research exists regarding the influence of social support on psychotherapy outcome. Among the very few such studies to date, Beckner, Howard, Vella, and Mohr (2010) explored the role of baseline levels of received and satisfaction with social support in treatment outcome in telephone-administered CBT (T-CBT) compared to telephone-administered emotion-focused therapy (T-EFT) among multiple sclerosis patients. The authors found that individuals with higher levels of received social support and greater satisfaction with such support showed greater reduction in depressive symptoms when enrolled in T-CBT compared with T-EFT. They theorized that those with high social support may have more emotional resources to take on the challenging tasks of CBT, including doing homework, testing out new behaviors, and developing new skills.
Findings were similar in a study of the role of caregiver participation among Parkinson’s disease patients receiving CBT for depression. In this study, Dobkin et al. (2012) found that caregiver participation predicted response to treatment. Although the presence of a caregiver is not directly comparable to the multifaceted nature of social support,, patients’ benefits from the assistance of a caregiver suggest an important role of social support as an addition to CBT.
Based on the potential of social support to enhance the benefits of CBT, along with established links between social support and quality of life in a variety of contexts, it appears that social support enhances CBT’s positive impact on quality of life. This effect is likely to occur for satisfaction with social support, and less so for frequency of social support. Moreover, account should be taken of changes in social support during the course of CBT treatment. For instance, levels of social support may change between pretreatment and posttreatment. Given that pre- and posttreatment social support data were available, the current study will examine the impact of pretreatment social support, as well as change in social support between pre- and posttreatment. As such, the following hypotheses will be tested in a sample of rural older adults:
H1: Satisfaction with social support will predict improvement in quality of life in rural older adults receiving CBT.
H2: Frequency of social support will not predict improvement in quality of life in rural older adults receiving CBT.
H3: Positive change in satisfaction with social support from pretreatment to posttreatment will predict improvement in quality of life in rural older adults receiving CBT.
Method
The current study is a secondary analysis of data collected from the Scogin et al. (2007) study that assessed the efficacy of home-delivered CBT in improving the quality of life in rural older adults (see Scogin et al. for additional details regarding methods and primary treatment outcomes). Participants were randomized into a CBT or minimal support condition (MSC) and were assessed at baseline (Time 1), midtreatment, immediately posttreatment (Time 2), and follow-up. Although data were collected on client social support, the original study did not conduct analysis of this variable.
Participants
Participants were recruited through advertisements, public and private home health-care agencies, senior centers, church organizations, hospitals with associated home health-care groups, and service providers such as physicians and pharmacists. Participant inclusion criteria were as follows: (a) age of 65 years or older, (b) a T score of 55 or lower on the Quality of Life Inventory (QOLI; Frisch, 1992), (c) a T score of greater than 45 on the Global Severity Index (GSI) of the Symptoms Checklist-90-Revised (SCL-90-R; Derogatis, Rickels, & Rock, 1976) using non-patient adult norms, and (d) residence outside the cities of Tuscaloosa (AL) and Montgomery (AL).
The following were exclusion criteria: (a) self-reported history of bipolar disorder, schizophrenia, or current substance abuse; (b) receiving psychotherapy currently; or (c) significant cognitive impairment indicated by a score of 23 or less (16 or less for those with less than a ninth-grade education) on the MMSE (Folstein, Folstein, & McHugh 1975).
Measures
Background information
This included age, sex, race, marital status, education, income, and subjective financial burden. For the current study, age, race, sex, education, and income were tested for their ability to predict positive change in quality of life.
Quality of life
To measure self-reported overall quality of life, the Quality of Life Inventory (QOLI; Frisch, 1992) was used. The QOLI contains sixteen domains of assessment: health, self-regard, philosophy of life, standard of living, work, recreation, learning, creativity, helping, love relationship, friendships, relationships with children, relationships with relatives, home, neighborhood, and community. A 3-point Likert scale is used to rate the importance of each domain, and a 6-point Likert scale is used to rate satisfaction with the domain. The cross-product is then summed, and this score is converted to T scores based on adult, community-dwelling norms. Cronbach’s alpha in the normative study was .79 (Frisch, 1992) and .70 in the current study at Time 1. The mean score for the sample at Time 1 was 42.5 (SD = 9.0). In the current study, the dependent variable consisted of QOLI change scores. These scores were created by subtracting Time 1 QOLI scores from Time 2 (posttreatment) scores. The mean QOLI change score was 4.6 (SD = 10.7).
Social support
The satisfaction and frequency of social support variables were created from the overall social support scale in the original study (Scogin et al., 2007). These measures consist of multiple dimensions and were based on a measure of social support developed for the Resources for Enhancing Alzheimer’s Caregiver Health I (REACH I) project (Wisniewski et al., 2003). It includes the 4-item Krause (1995) measure of negative interactions (e.g., “How often have others taken advantage of you?”), 10 items based on questions from the Lubben Social Network Index (Lubben, 1988) asking about help received (e.g., “How often has someone helped you with shopping?”), and 13 items measuring satisfaction with tangible, emotional, and informational support received (Krause, 1995; Krause & Markides, 1990). Tangible items included “In the past month, how often has someone pitched in to help do something that needed to get done, such as household chores or yard work?” Emotional items included “In the past month, how often has someone listened to you talk about your private feelings?” Informational items included “In the past month, how often has someone made a difficult situation clearer and easier to understand?”
Drawing from the above scale, the satisfaction with social support scale consisted of items chosen based on the participant’s subjective perception of the quality of his or her social support, rather than the quantity. Examples of items include “Overall, how satisfied have you been in the last month with the help you have received from friends, neighbors, or family members?” and “In the past month, how satisfied have you been with the support received during difficult times, comforting from others, how others have listened, and interest and concern from others?” The range of the satisfaction with social support scale is 0 to 37, and the Cronbach’s alpha value for the sample is .75. The mean score for the sample at Time 1 was 23.0 (SD = 6.4).
Frequency of social support consisted of items measuring the quantitative extent to which persons receive social support. Examples of items include “How often do you see or hear from the person with whom you have the most contact?” and “In the past month, how often was someone physically there with you in a stressful situation?” The range of the frequency of social support scale is 0 to 47, and the Cronbach’s alpha value for the sample is .76. The mean score for the sample at Time 1 was 21.8 (SD = 8.1).
Finally, change scores in satisfaction with and frequency of social support were also created. These scores represent change in social support from Time 1 assessment to Time 2 assessment. Scores were created by subtracting Time 1 social support scores from Time 2 scores. The mean change score for satisfaction with social support was 1.2 (SD = 4.9), and the mean change score for frequency of social support was 1.3 (SD = 6.8).
Procedure
Participants were randomized to CBT or the minimal support condition (MSC). Randomization involved stratifying participants based on two variables: site location (rural Tuscaloosa or rural Montgomery) and race (African American or Caucasian). “Rural” was defined as residence outside of city limits. Among the four groups, a random number table determined assignment to CBT or the MSC. At the time of the baseline assessment, research assistants were blind to participant assignment.
After randomization, participants in the CBT condition were assessed on outcome variables at midtreatment and immediately posttreatment (Time 2). Participants assigned to the MSC were assessed a second time approximately three months after randomization. Thus, the controlled comparison was between the Time 1 and Time 2 assessments for the two conditions. After the Time 2 assessment, MSC participants received CBT as described above. Finally, all participants were assessed again six months following the CBT intervention. For participants who did not complete the study, data from their most recent assessment were carried forward for subsequent assessments.
Treatment
Therapists consisted of five licensed Masters of Social Work (MSW) clinical social workers (two African Americans and three Caucasians) without prior CBT experience. The principal investigator conducted training of the therapists, which consisted of four sessions that included 12 hours of didactic instruction and 12 hours of experiential training. Feedback was provided until therapists were competent based on the Cognitive Therapy Scale (CTS; Young & Beck, 1980), and weekly supervision was conducted with the therapists.
CBT
Treatment was based on the manual by Thompson, Gallagher-Thompson, and Dick (1995) for the delivery of CBT to older adults and consisted of 16 sessions. The first month of treatment consisted of twice-weekly sessions, followed by weekly sessions during the remainder of the treatment. The essential components of the treatment were activity scheduling, identifying and changing unhelpful thoughts, relaxation, and assertiveness. In accordance with the manual by Thompson et al., treatment included modifications of traditional CBT to apply to older adults, such as providing in-session cue cards as memory aids, reducing the pace of the intervention process, and simplification of homework assignments. The average number of sessions was 11.7, and the average time to complete treatment was 5.3 months.
MSC
In this condition, participants received weekly telephone calls from the project staff. These calls lasted for three months and served both as a means to monitor participants for deteriorating mental health and as an incentive to continue in the project. No CBT techniques were administered.
Statistical Analyses
Hierarchical multiple regression analysis was used to test whether social support uniquely predicted increase in quality of life beyond the effects of the CBT treatment. Social support x treatment group interaction terms were also entered to test for the potential moderating role of social support in CBT’s effect on quality of life change. Finally, as an exploratory analysis, change in social support was tested as a mediator of the relation between CBT and increased quality of life. All analyses used a critical alpha level of .05 for determining statistical significance, and exact levels are reported unless they are less than .001. To maximize statistical power, dropout participant social support and quality of life data were carried forward from their last completed data point to posttreatment.
Results
Descriptive Analyses
The sample consisted of 137 participants, with 71 individuals in the treatment group and 66 in the MSC group. At Time 2 the sample consisted of 51 individuals in the treatment group and 50 in the MSC group. The treatment group consisted of 87.3% females, and the MSC group consisted of 75.8% females. In terms of race, the treatment group was 57.7% African American and 42.3% Caucasian, and the MSC group was 59.1% African American and 40.9% Caucasian. The mean age was 75.2 (SD = 7.0) for the treatment group and 76.3 (SD = 7.9) for the MSC group. The mean level of education was 9.8 years (SD = 4.1) for the treatment group and 9.3 years (SD = 3.5) for the MSC group. See Table 1 for descriptive characteristics.
Table 1.
Participant Characteristics
| Variable | All (n = 137) | Treatment (n = 71) | MSC (n = 66) | |||
|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |
| Age | 75.7 | 7.4 | 75.2 | 7.0 | 76.3 | 7.9 |
| Education | 9.5 | 3.8 | 9.8 | 4.1 | 9.3 | 3.5 |
| Frequencies | Frequencies | Frequencies | ||||
| Sex | ||||||
| Male | 25 (18.2 %) | 9 (12.7%) | 16 (24.2%) | |||
| Female | 112 (81.8%) | 62 (87.3%) | 50 (75.8%) | |||
| Race/Ethnicity | ||||||
| African-American | 80 (58.4%) | 41 (57.7%) | 39 (59.1%) | |||
| Caucasian | 57 (41.6%) | 30 (42.3%) | 27 (40.9%) | |||
| Annual Income | ||||||
| < $5,000 | 3 (2.2%) | 0 (0%) | 3 (4.5%) | |||
| $5,000 - $9,999 | 58 (42.3%) | 27 (38.0%) | 31 (47.0%) | |||
| $10,000 - $14,999 | 27 (19.7%) | 16 (22.5%) | 11 (16.7%) | |||
| $15,000 - $19,999 | 9 (6.6%) | 5 (7.0%) | 4 (6.1%) | |||
| $20,000 - $29,999 | 6 (4.4%) | 2 (2.8%) | 4 (6.1%) | |||
| $30,000 - $39,999 | 1 (.7%) | 1 (1.4%) | 0 (0%) | |||
| $40,000 - $49,999 | 2 (1.5%) | 2 (2.8%) | 0 (0%) | |||
| $50,000 - $59,999 | 0 (0%) | 0 (0%) | 0 (0%) | |||
| $60,000 - $69,999 | 1 (.7%) | 0 (0%) | 1 (1.5%) | |||
| $70,000 or more | 1 (.7%) | 1 (1.4%) | 0 (0%) | |||
Note. Forty-one participants did not provide age, 1 participant did not provide education data, and 29 participants did not provide income data.
Treatment Results
Test for differential outcomes by location
To test for the possibility of differential levels of social support or quality of life change by treatment location, independent samples t-tests were performed between the rural Montgomery and rural Tuscaloosa participants. There were no significant differences in satisfaction with or frequency of social support, as well as quality of life change scores.
Control Variables
Simple linear regression was used to test the predictive ability of age, race, sex, education, and income on the dependent variable of improvement in quality of life. None of these variables significantly predicted the dependent variable and were excluded from further statistical analysis.
Social support
Hierarchical regression analysis was used to examine the effects of social support on positive quality of life change. Separate equations were used for each measure of social support. The main effects of pretreatment satisfaction and frequency of social support were nonsignificant (see Table 2 for effects of pretreatment social support). As such, H1 was not supported, whereas H2 was supported. In support of H3, change in satisfaction with social support significantly predicted the dependent variable, explaining 5.3% of the variance (β = .25, p = .003). See Table 3 for effects of change in social support.
Table 2.
Hierarchical Multiple Regression Analyses Predicting Increase in Quality of Life from Pretreatment Social Support
| Type of Social Support | ||||
|---|---|---|---|---|
| Satisfaction | Frequency | |||
| Predictor | ΔR2 | β | ΔR2 | β |
| Step 1 | ||||
| Group | .07** | .26** | .07** | .26** |
| Step 2 | ||||
| Social Support | .00 | .00 | .01 | .10 |
| Step 3 | ||||
| Social Support × Group | .04* | −.19* | .02 | .13 |
Note. Group variable indicates effect of treatment group.
p < .05;
p < .01
Table 3.
Hierarchical Multiple Regression Analyses Predicting Increase in Quality of Life from Change in Social Support
| Type of Social Support | ||||
|---|---|---|---|---|
| Satisfaction | Frequency | |||
| Predictor | ΔR2 | β | ΔR2 | β |
| Step 1 | ||||
| Group | .07** | .21* | .07** | .22* |
| Step 2 | ||||
| Social Support | .05** | .25** | .03 | .17 |
| Step 3 | ||||
| Social Support × Group | .03* | .19* | .01 | .12 |
Note. Group variable indicates effect of treatment group.
p < .05;
p < .01
Social support was also tested as a moderator of the CBT treatment on quality of life. Pretreatment satisfaction with social support was found to moderate the effect of treatment (β = −.19, p = .03; see Table 2). Finally, change in satisfaction with social support was found to moderate the effect of treatment (β = .19, p = .03; see Table 3.
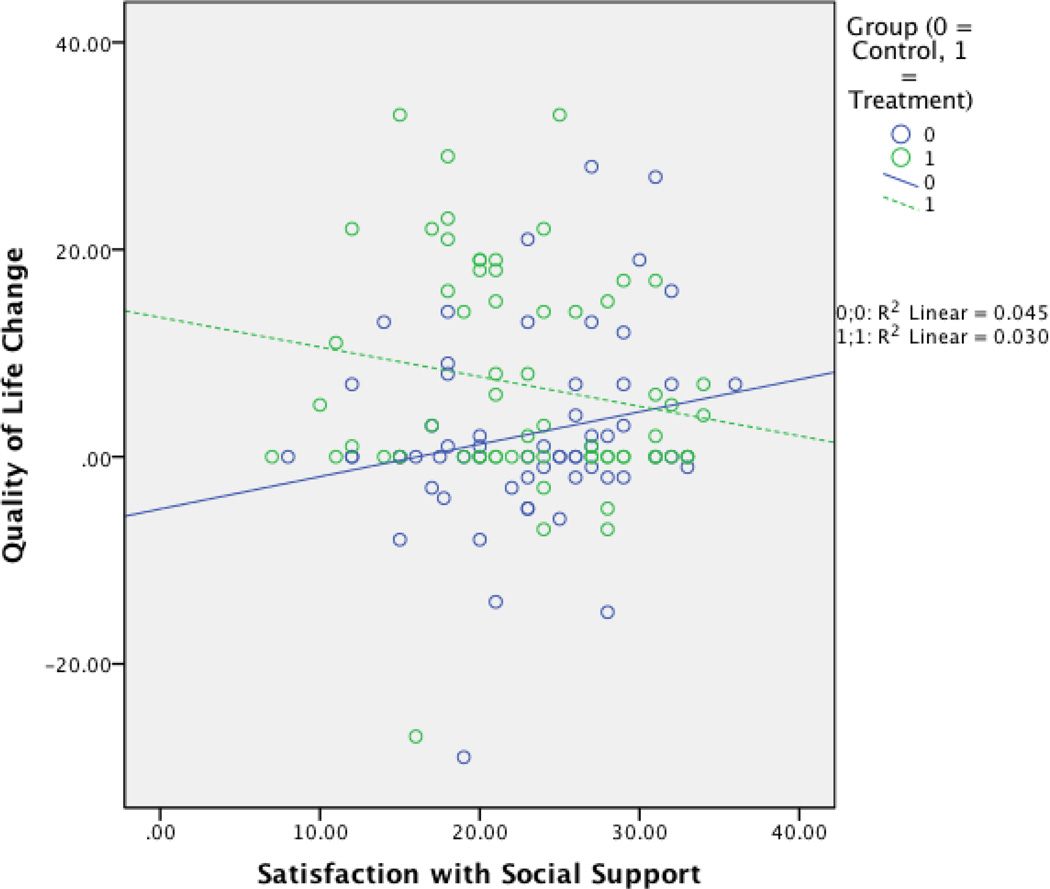
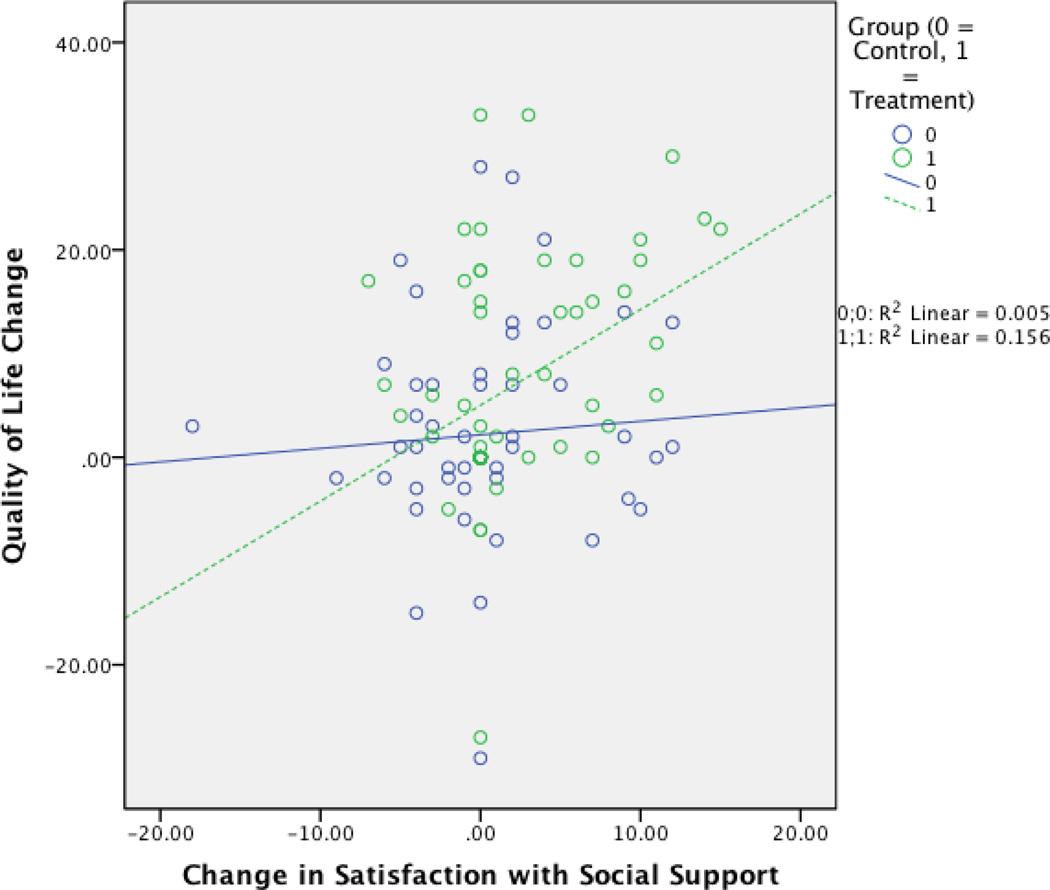
The moderating effects of social support are also depicted in the scatterplots (Figures 1 – 2). As depicted in Figure 1, as pretreatment satisfaction with social support increases, quality of life change scores increase for the control group but decrease for the treatment group. In Figure 2, as change in satisfaction with social support increases, quality of life change scores increase for both groups, but more so for the treatment group. Participants receiving CBT maximized their gains in quality life with increased social support.
FIGURE 1.
Scatterplot illustrating the moderating effect of pretreatment satisfaction with social support on treatment group’s relation to positive quality of life change.
FIGURE 2.
Scatterplot illustrating the moderating effect of change in satisfaction with social support on treatment group’s relation to positive quality of life change.
Finally, change in social support was tested as a mediator of the relation between CBT and quality of life change. However, both satisfaction with social support and frequency of social support were nonsignificant as mediators.
Discussion
This study explored the potential of social support to uniquely improve quality of life in the context of receiving CBT. Regression analysis revealed that change in satisfaction with social support explained positive change in quality of life over and above the effects of being in the CBT treatment group. Moreover, social support was found to moderate CBT’s effect on quality of life improvement. These findings attest to the importance of social support in persons receiving CBT. Specifically, rural older adults with increased social support during the course of CBT treatment appear to have increased wellbeing, over and above the effects of the CBT itself. The findings are also consistent with the wealth of literature establishing the link between social support and quality of life. Although the current study conceptualized quality of life across multiple domains, results are consistent with many earlier studies focusing on health quality of life (e.g., Sherman et al., 2006).
Increases in social support as predictors of increased quality of life raise important possibilities about the role of social support during the course of CBT. For example, a greater amount of social support at posttreatment would suggest a greater impact of social support in the latter part of treatment. Indeed, change in satisfaction with social support was found to predict increase in quality of life. The moderating role of change in satisfaction with social support in the current study may be understood in terms of social support enhancing the effects of CBT. Clients gain skills in activity scheduling, relaxation, and changing unhelpful thoughts during the course of treatment, but it may take time for clients to become open to and grasp these skills. Toward the latter part of treatment, social contacts may facilitate the acceptance, practice, and inculcation of these skills.
The current study’s findings are consistent with the moderating role of social support in telephone-administered CBT’s effectiveness in reducing depression in patients with multiple sclerosis (Beckner, Howard, Vella, & Mohr, 2010), as well as the role of caregiver participation in predicting treatment response to CBT for depression among Parkinson’s patients (Dobkin et al., 2012). According to Beckner and colleagues, those with high social support have the emotional resources to take on the challenging tasks of CBT, in which they have more empathic people to turn to, are less reliant on the therapist, and have greater emotional resources to perform the tasks of CBT. Moreover, high social support may be a marker for certain skills or traits that facilitate improvement in CBT, such as feelings of encouragement, greater openness to trying new behaviors, and more cognitive resources for acquiring new skills (Beckner et al., 2010).
The nature of the moderating role of pretreatment satisfaction with social support was unexpected. Specifically, individuals with lower pretreatment satisfaction with social support enjoyed greater gains in quality of life resulting from CBT. This may be explained by the beneficial role of increase in social support during the course of CBT. For example, those with low pretreatment social support may typically have more to gain in this area, which in turn results in greater positive change in quality of life at posttreatment. This is underscored by the current study’s findings of change in satisfaction with social support moderating the role of CBT in improving quality of life.
The findings of the current study have important implications for the role of social support in CBT treatment programs, particularly for rural older adults who may lack resources other than social support. Social support both enhances the effects of CBT on quality of life, as well as improving individuals’ quality of life over and above the effects of CBT. Thus, persons undergoing CBT who have poor social support stand much to gain by enhancing the quality of their social networks. Therapists would do well to emphasize the value of social support in increasing one’s subjective wellbeing. They may also provide clients with skills to ask for help when needed, reduce interpersonal conflicts, alter negative perceptions of others, and increase the quality of their interactions with people who are close to them. Future research should investigate whether the impact of social support is specific to CBT or whether these results will generalize to any treatment in improving the quality of life of rural older adults.
Findings of this study also provide preliminary support for supplementing individually administered CBT with a standardized educational intervention for caregivers of older adults. According to Dobkin and colleagues (2012), the skills-based nature of CBT, its focus on specific thoughts and behaviors, and the use of homework and practice may make CBT especially well suited for the inclusion of caregivers in the treatment of older adults.
Study Limitations
This study has several limitations. Given that the sample consisted of rural older adults, results may not generalize to other populations. The sample was also overwhelmingly female, making it difficult to fully assess the role of sex in social support. Moreover, as with most correlational research, it is difficult to know the nature of causality. While it appears that social support predicts higher quality of life, it could be that both social support and quality of life are influenced by other variables not tested. Additionally, carrying forward dropout data to maximize statistical power may have attenuated the predictive power of the independent variable on the dependent variable. Finally, four of the sixteen dimensions of quality of life (love relationships, friendships, relationships with children, and relationships with relatives) may conceptually overlap with social support, in which case social support may not necessarily benefit the nonsocial aspects of quality of life.
Summary and Conclusions
By enhancing social support, clients are able to get more from CBT treatment, possibly through greater emotional resources and more opportunities to practice new skills. This is consistent with the finding that clients benefitted from increases in social support during the course of treatment, in which clients became increasingly equipped to enact newly learned behaviors and ways of thinking. Based on this study’s findings, therapists conducting CBT for rural older adults would do well to encourage clients to maximize their treatment gains by extending and enriching their social support.
ACKNOWLEDGMENT
Allan Kaufman provided valuable assistance in collecting data for this article.
FUNDING
This research was supported by National Institute on Aging Grant AG16311.
Footnotes
Color versions of one or more of the figures in the article can be found online at www.tandfonline.com/wcli.
References
- Andrews FM, Withey SB. Social indicators of well being: American's perceptions of life quality. New York: Plenum Press; 1976. [Google Scholar]
- Antonucci TC. A life-span view of women's social relations. In: Turner B, Troll LE, Turner B, Troll LE, editors. Women growing older: Psychological perspectives. Thousand Oaks, CA US: Sage Publications, Inc; 1994. pp. 239–269. [Google Scholar]
- Beckner V, Howard I, Vella L, Mohr DC. Telephone-administered psychotherapy for depression in MS patients: Moderating role of social support. Journal of Behavioral Medicine. 2010;33(1):47–59. doi: 10.1007/s10865-009-9235-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beedie A, Kennedy P. Quality of social support predicts hopelessness and depression post spinal cord injury. Journal of Clinical Psychology in Medical Settings. 2002;9(3):227–234. [Google Scholar]
- Berkman LF. Social support, social networks, social cohesion and health. Social Work in Health Care. 2000;31(2):3–14. doi: 10.1300/J010v31n02_02. [DOI] [PubMed] [Google Scholar]
- Cantor MH. Neighbors and friends: An overlooked resource in the informal support system. Research On Aging. 1979;1(4):434–463. [Google Scholar]
- Chalise H, Saito T, Takahashi M, Kai I. Relationship specialization amongst sources and receivers of social support and its correlations with loneliness and subjective well-being: A cross sectional study of Nepalese older adults. Archives Of Gerontology and Geriatrics. 2007;44(3):299–314. doi: 10.1016/j.archger.2006.07.001. [DOI] [PubMed] [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98(2):310–357. [PubMed] [Google Scholar]
- Derogatis LR, Rickels K, Rock AF. The SCL-90 and the MMPI: A step in the validation of a new self-report scale. British Journal of Psychiatry. 1976;128:280–289. doi: 10.1192/bjp.128.3.280. [DOI] [PubMed] [Google Scholar]
- Diener E. Subjective well-being. Psychological Bulletin. 1984;95:542–575. [PubMed] [Google Scholar]
- Dobkin RD, Rubino J, Allen LA, Friedman J, Gara MA, Mark MH, Menza M. Predictors of treatment response to cognitive-behavioral therapy for depression in Parkinson's disease. Journal of Consulting and Clinical Psychology. 2012;80(4):694–699. doi: 10.1037/a0027695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatry Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Frisch MB. Quality of life therapy and assessment in health care. Clinical Psychology: Science And Practice. 1998;5(1):19–40. [Google Scholar]
- Frisch MB. Test manual and treatment guide for the QOLI (Quality of Life Inventory) Minneapolis, MN: Pearson Assessments (formerly NCS Assessments; 1994b. [Google Scholar]
- Frisch MB. Use of the Quality of Life Inventory in problem assessment and treatment planning for cognitive therapy of depression. In: Freeman A, Dattilio FM, editors. Comprehensive casebook of cognitive therapy. New York: Plenum; 1992. pp. 27–52. [Google Scholar]
- Frisch MB, Cornell J, Villanueva M, Retzlaff PJ. Clinical validation of the Quality of Life Inventory: A measure of life satisfaction for use in treatment planning and outcome assessment. Psychological Assessment. 1992;4(1):92–101. [Google Scholar]
- George LK, Blazer DG, Hughes DC, Fowler N. Social support and the outcome of major depression. British Journal of Psychiatry. 1989;154:478–485. doi: 10.1192/bjp.154.4.478. [DOI] [PubMed] [Google Scholar]
- Haber MG, Cohen JL, Lucas T, Baltes BB. The relationship between self-reported received and perceived social support: A meta-analytic review. American Journal of Community Psychology. 2007;39(1–2):133–144. doi: 10.1007/s10464-007-9100-9. [DOI] [PubMed] [Google Scholar]
- Krause N. Negative interaction and satisfaction with social support among older adults. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 1995;50B:59–73. doi: 10.1093/geronb/50b.2.p59. [DOI] [PubMed] [Google Scholar]
- Krause N, Markides KS. Measuring social support among older adults. The International Journal of Aging & Human Development. 1990;30(1):37–53. doi: 10.2190/CY26-XCKW-WY1V-VGK3. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Redner JE, Seeley JR. The relationship between life satisfaction and psychosocial variables: New perspectives. In: Strack F, Argyle M, Schwarz N, Strack F, Argyle M, Schwarz N, editors. Subjective well-being: An interdisciplinary perspective. Elmsford, NY US: Pergamon Press; 1991. pp. 141–169. [Google Scholar]
- Low G, Molzahn AE, Kalfoss M. Quality of life of older adults in Canada and Norway: Examining the Iowa model. Western Journal of Nursing Research. 2008;30(4):458–476. doi: 10.1177/0193945907305675. [DOI] [PubMed] [Google Scholar]
- Lubben JE. Assessing social networks among elderly populations. Journal of Family and Community Health. 1988;11:42–52. [Google Scholar]
- Nasser EH, Overholser JC. Recovery from major depression: The role of support from family, friends, and spiritual beliefs. Acta Psychiatrica Scandinavica. 2005;111(2):125–132. doi: 10.1111/j.1600-0447.2004.00423.x. [DOI] [PubMed] [Google Scholar]
- Netuveli G, Wiggins RD, Hildon Z, Montgomery SM, Blane D. Quality of life at older ages: Evidence from the English longitudinal study of aging (wave 1) Journal of Epidemiology and Community Health. 2006;60(4):357–363. doi: 10.1136/jech.2005.040071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborne RH, Hawthorne G, Lew EA, Gray LC. Quality of life assessment in the community-dwelling elderly: Validation of the assessment of quality of life (AQoL) instrument and comparison with the SF-36. Journal of Clinical Epidemiology. 2003;56:138–147. doi: 10.1016/s0895-4356(02)00601-7. [DOI] [PubMed] [Google Scholar]
- Richmond CM, Ross NA, Egeland GM. Social support and thriving health: A new approach to understanding the health of indigenous Canadians. American Journal of Public Health. 2007;97(10):1827–1833. doi: 10.2105/AJPH.2006.096917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rintala DH, Young ME, Hart KA, Clearman RR, Fuhrer MJ. Social support and the well-being of persons with spinal cord injury living in the community. Rehabilitation Psychology. 1992;37(3):155–163. [Google Scholar]
- Rogers CC. Growth of the oldest old population and future implications for rural areas. Rural Development Pespectives. 1999;14:22–26. [Google Scholar]
- Saito E, Sagawa Y, Kanagawa K. Social support as a predictor of health status among older adults living alone in Japan. Nursing & Health Sciences. 2005;7(1):29–36. doi: 10.1111/j.1442-2018.2005.00220.x. [DOI] [PubMed] [Google Scholar]
- Schaefer C, Coyne JC, Lazarus RS. The health-related functions of social support. Journal of Behavioral Medicine. 1981;4(4):381–406. doi: 10.1007/BF00846149. [DOI] [PubMed] [Google Scholar]
- Scogin F, Morthland M, Kaufman A, Burgio L, Chaplin W, Kong G. Improving quality of life in diverse rural older adults: A randomized trial of a psychological treatment. Psychology and Aging. 2007;22(4):657–665. doi: 10.1037/0882-7974.22.4.657. [DOI] [PubMed] [Google Scholar]
- Sherman AM, Shumaker SA, Rejeski W, Morgan T, Applegate WB, Ettinger W. Social support, social integration, and health-related quality of life over time: Results from the Fitness and Arthritis in Seniors Trial (FAST) Psychology & Health. 2006;21(4):463–480. [Google Scholar]
- Shumaker SA, Hill D. Gender differences in social support and physical health. Health Psychology. 1991;10(2):102–111. doi: 10.1037//0278-6133.10.2.102. [DOI] [PubMed] [Google Scholar]
- Taylor SE. Health psychology. 4th ed. New York, NY US: McGraw-Hill; 1999. [Google Scholar]
- Theeke L, Goins R, Moore J, Campbell H. Loneliness, depression, social support, and quality of life in chronically ill Appalachians. Journal of Psychology: Interdisciplinary and Applied. 2012;146(1–2):155–171. doi: 10.1080/00223980.2011.609571. [DOI] [PubMed] [Google Scholar]
- Thompson LW, Gallagher-Thompson D, Dick LP. Cognitive-behavioral therapy for late life depression: A therapist manual. Palo Alto, CA: Older Adult and Family Center, Veterans Affairs Palo Alto Health Care System; 1995. [Google Scholar]
- Veenhoven R. Conditions of happiness. Boston: Reidel; 1984. [Google Scholar]
- Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve month use of mental health services in the United States: Results from the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- Williams A, Cutchin M. The rural context of health care provision. Journal of Interprofessional Care. 2002;16(2):107–115. doi: 10.1080/13561820220124120. [DOI] [PubMed] [Google Scholar]
- Wisniewski SR, Belle SH, Coon DW, Marcus SM, Ory MG, Burgio LD, et al. The Resources for Enhancing Alzheimer’s Caregiver Health (REACH): Project design and baseline characteristics. Psychology and Aging. 2003;18:375–384. doi: 10.1037/0882-7974.18.3.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young J, Beck AT. Cognitive Therapy Scale: Rating manual. Philadelphia: University of Pennsylvania; 1980. Unpublished manuscript. [Google Scholar]
- Zaninotto P, Falaschetti E, Sacker A. Age trajectories of quality of life among older adults: Results from the English longitudinal study of ageing. Quality Of Life Research: An International Journal Of Quality Of Life Aspects Of Treatment, Care & Rehabilitation. 2009;18(10):1301–1309. doi: 10.1007/s11136-009-9543-6. [DOI] [PubMed] [Google Scholar]
- Zhao G, Li X, Fang X, Zhao J, Hong Y, Lin X, Stanton B. Functions and sources of perceived social support among children affected by HIV/AIDS in China. AIDS Care. 2011;23(6):671–679. doi: 10.1080/09540121.2010.525619. [DOI] [PMC free article] [PubMed] [Google Scholar]