Abstract
A meta-analysis of 150 research reports summarizing the results of multiple behavior domain interventions examined theoretical predictions about the effects of the included number of recommendations on behavioral and clinical change in the domains of smoking, diet, and physical activity. The meta-analysis yielded three main conclusions. First, there is a curvilinear relation between the number of behavioral recommendations and improvements in behavioral and clinical measures, with a moderate number of recommendations producing the highest level of change. A moderate number of recommendations is likely to be associated with stronger effects because the intervention ensures the necessary level of motivation to implement the recommended changes, thereby increasing compliance with the goals set by the intervention, without making the intervention excessively demanding. Second, this curve was more pronounced when samples were likely to have low motivation to change, such as when interventions were delivered to non-patient (vs. patient) populations, were implemented in non-clinic (vs. clinic) settings, used lay community (vs. expert) facilitators, and involved group (vs. individual) delivery formats. Finally, change in behavioral outcomes mediated the effects of number of recommended behaviors on clinical change. These findings provide important insights that can help guide the design of effective multiple behavior domain interventions.
Keywords: multiple behavior domain change, physical activity, diet, smoking cessation, lifestyle intervention, multi-domain intervention, multi-behavior intervention
Two alternative approaches have been used to prevent the cluster of diseases associated with smoking, poor diet, and physical inactivity: designing interventions to reduce each risk behavior as a separate entity with its unique set of determinants and methods of change (Nigg, Allegrante, & Ory, 2002), or embracing behavior co-occurrence by designing interventions that reduce the multiple behaviors associated with a disease or cluster of diseases (Fine, Philogene, Gramling, Coups, & Sinha, 2004; Klesges, Eck, Isbell, Fulliton, & Hanson, 1990; Pronk, et al., 2004). Multiple behavior domain interventions encourage change in two or more health behavior domains, such as diet and exercise, with the recommendations being delivered within a limited period of time (Goldstein, Whitlock, & DePue, 2004; Nigg, Allegrante, & Ory, 2002; Nigg & Long, 2012; Prochaska, Nigg, Spring, Velicer, & Prochaska, 2010; Prochaska & Prochaska, 2008). Few doubt that, if successful, multiple behavior domain interventions are a practical way of promoting health by adapting to the reality of the disease. Despite this appeal, however, cumulative efficacy data are limited, often based on a restricted set of studies (Smedley & Syme, 2000; Emmons, 2001), and the theoretical mechanisms underlying the efficacy of these programs are surprisingly unarticulated. One issue that is vital for the design of successful multiple behavior domain interventions is to determine the optimal number of behavioral recommendations to target. To close this critical gap in prevention science, we conducted a meta-analysis examining potential theoretical mechanisms driving the impact of differing numbers of lifestyle recommendations on behavioral and clinical change, and to determine whether these effects vary depending on conditions that may be associated with delivery to recipients with low motivation to change.
In this paper, we reviewed 150 research reports summarizing the results of interventions targeting change in the behavioral domains (broad risk factor being targeted) of diet, exercise, or smoking, to determine whether a higher number of behavior recommendations (the specific prescribed dietary, exercise, or smoking behaviors, such as engaging in moderate physical activity for 30-minutes on at least 5 days per week) results in healthier outcomes. There are at least two theoretical predictions for the influence of number of recommendations on behavioral and clinical change. On the one hand interventions may become more difficult to process when they include a greater number of recommended behaviors to change. Many decades ago, experimental research on memory processes demonstrated that upon intentional effort to remember multiple digits, humans can recall an average of seven (Miller, 1956; Shiffrin & Nosofsky, 1994). Just as more numbers overwhelm cognitive capacity and foster forgetting of all numbers in the sequence, how many behaviors can an intervention promote before its efficacy plateaus or plummets? How many recommended behaviors are too many given our self-control capacity?
On the other hand, interventions may be more interesting when they include more recommendations, increasing the probability of attracting attention and motivation to implement the recommended changes (e.g., Broadhurst, 1959; Hebb, 1955; Klein, 1982; Mendl, 1999; Teigen, 1994; Yerkes & Dodson, 1908). These predictions are consistent with Bandura's self-efficacy theory (1986, 1989, 1997, 2004) as well as Brehm's motivational intensity theory (Brehm & Self, 1989; Brehm, Wright, Solomon, Silka, & Greenberg, 1983), both of which assume that effort is greater for moderately difficult tasks, than for either easy or difficult ones (Brehm et al., 1983; Contrada et al., 1982; Light & Orbrist, 1980; Silvia, Jones, Kelly, & Zibae, 2011; Silvia, McCord, & Gendolla, 2010; Wright, Contrada, & Patane, 1986). If both motivation and capacity issues are implicated, one could expect an inverted U-type of effect in which a moderate number of recommendations is more effective at changing behavior than either a low or a high number of recommendations. That is, a moderate number of recommendations would be low enough to prevent disengagement while being high enough to ensure the necessary level of motivation and effort to maximize compliance and, ultimately, clinical change.
Health Change Following Multiple Behavior Domain Interventions
A common idea that often underlies the development of multiple behavior domain interventions is that if multiple behaviors contribute to a disease, they should all be targeted in a simultaneous prevention effort (Nigg et al., 2002; U.S. Department of Health and Human Services, 2000; Werch, Moore, DiClemente, Bledsoe, & Jobli, 2005). There is evidence suggesting that targeting multiple lifestyle changes is beneficial for change in clinical indicators of health. For instance, interventions promoting exercise and dietary changes have been shown to reduce the incidence of diabetes and other clinical outcomes related to diabetes (e.g., weight, glycaemia; Diabetes Prevention Program Research Group, 2002; Tuomilehto et al., 2001). Targeting multiple lifestyle domains in an intervention, such as diet and physical activity, can also have beneficial carryover effects on other behaviors that have not been systematically targeted by a behavioral recommendation. For example, intervening to increase fruit and vegetable intake and to decrease sedentary leisure screen time has been shown to produce a large and sustained decrease in saturated fat intake (Spring et al., 2012). Despite this intriguing evidence, prior research has not thoroughly examined whether single behavior domain interventions are similarly associated with improvements in untargeted behaviors. Due to this limitation, it remains unclear whether multiple behavior domain interventions promote improvement in multiple domains in a manner that does not happen spontaneously in single behavior domain interventions.
Although conclusions from prior reviews of multiple behavior domain interventions are far from being monolithic (see Table 1), they suggest that multiple behavior domain interventions are generally more effective than single behavior domain interventions. For example, a synthesis of multiple behavior domain interventions to reduce cardiovascular risk and disease found favorable effects on behavioral and clinical outcomes, particularly for recipients at high risk of illness (Ketola, Sipila, & Makela, 2000). A more recent review of interventions addressing prevention of cardiovascular disease suggested that multiple behavior domain interventions produced modest improvements in risk biomarkers (e.g., blood pressure, cholesterol) in the general population, and reduced cardiovascular events and total mortality among those with hypertension or diabetes (Ebrahim et al., 2011). Additionally, a promising meta-analysis of interventions for type-1 diabetes concluded that change is greater in programs targeting several behavior domains (i.e., exercise, diet, medication; d = 0.45) than in exercise-only programs (d = 0.03; Conn et al., 2008). Finally, a meta-analysis of smoking cessation and weight control programs concluded that, rather than being detrimental, jointly targeting smoking cessation and weight gain offers greater short-term benefits than targeting smoking cessation alone (Spring et al., 2009). Although this evidence speaks to the enhanced efficacy of multiple behavior domain interventions, the optimal number of behavioral recommendations to include in these interventions remains unclear.
Table 1.
Summary of Prior Meta-Analyses of Lifestyle Interventions.
| Authors, year | Sample | Type of design | Type of intervention (behaviors targeted) | Outcomes reported | Major finding |
|---|---|---|---|---|---|
|
Auer, Gaume, Rodondi, Cornuz, & Ghali (2008) Objective: To assess effects of in-hospital interventions targeting change in multiple cardiovascular risk factors. |
k = 26 n = 41,048 Population: mean age range = 42–76 years; hospitalized for acute coronary syndrome |
Experimental, RCTs + follow-up |
Intervention Groups: Smoking cessation, blood pressure, blood lipids, diet, weight, and physical activity (several combinations of two or more behaviors) Control Groups: No intervention |
Data reported are as RR with 95% CIs; between ( )number of trials where data are reported. All cause mortality (19) Short-term: RR = 0.78, 95% CI = 0.71, 0.86. Long-term: RR = 0.79, 95% CI = 0.85, 0.92. RR for all cause mortality was lower at 1-year a) in pre-post studies vs. clinical trials, b) interventions including provider-level and system-level components vs. interventions that only targeted patients, and c) in studies targeting an increase in medication usage. Readmission (11) RR = 0.59, 95% CI = 0.32, 1.07. Smoking cessation (13) Interventions showed evidence of increased smoking cessation rates (RR = 1.29, 95% CI = 1.02, 1.63). |
In-hospital multiple behavior domain interventions to reduce cardiovascular risk factors reduce mortality. However, this benefit was only statistically significant in pre-post studies. Interventions may be more effective when they target not only the patient, but also providers and the healthcare system. |
|
Benedict & Arterburn (2008) Objective: To assess effects of work-site based weight loss programs. |
k = 11 n = 2,502 Population: mean age range = 32–53 years |
RCTs, non-RCTs, uncontrolled case series |
Intervention Groups: Diet and/or exercise (8 targeted diet + exercise) Control Groups: No information provided |
Weight loss: In general, mean weight loss and changes in BMI were significantly greater in the IGs vs CGs. Serum lipids: 7 (of 11) studies reported modest improvements in serum lipids. Blood pressure (BP) 6 (of 11) studies reported modest improvements in systolic and/or diastolic BP. |
Multiple behavior domain work-site programs promote modest, short-term weight loss. |
|
Boulware, Gaumit, Frick, Minkovitz, Lawrence, & Powe (2001) Objective: To assess effects independent and interactive effects of three interventions (counseling, self-monitoring, structured, training courses) on BP control. |
k = 15 n = 4,072 Population: 53% male; age range = 50–65 years; 34% white |
Experimental |
Intervention Groups: Diet, exercise, smoking cessation Control Groups: Usual care |
Data reported as mean net changes. Counseling interventions: Significant BP improvement over usual care in 4 (of 15) studies. 3.2 mmHg improvement in diastolic BP (95% CI = 1.2, 5.3) and 11.1 mmHg improvement in systolic BP (95% CI = 4.1, 18.1) over usual care. Patient self-BP monitoring: Offered no significant improvement in BP over usual care in 1 (of 1) studies. Training courses: Counseling associated with stronger improvements (10 mmHg decrease in diastolic BP, 95% CI = 4.8, 15.6) than training courses in 1 (of 1) studies. Combined interventions: Significant reduction (4.7 mmHG, 95% CI 1.2, 8.2) was found in systolic BP in 2 (of 2) studies that compared counseling plus training to counseling alone; Combination offered no improvement to diastolic BP. In 1 (of 1) study, counseling plus training was associated 95% achieving hypertension control (95% CI = 87, 99), representing a statistically significant increase over training alone and counseling alone. |
Multiple behavior domain counseling interventions are associated with stronger improvements in blood pressure over usual care. Counseling interventions are also more effective than training courses. The addition of structured training courses to counseling interventions may enhance efficacy further. |
|
Conn et al. (2008) Objective: To assess effects of interventions to improve health behavior among adults with type-1 diabetes. |
k = 24; 11 (of 24) multiple behavior interventions n = 1,435 Population: 52% female; age range= 25–54 years; adults with type-1 diabetes |
Quasi-experimental, experimental |
Intervention: exercise, diet, medication (not all IGs targeted multiple behavior change) Control: Not all studies had control groups. When this was the case, pre- vs. post-test comparisons were made |
Data reported as standardized mean difference (Hedge's d) Glycosylated hemoglobin (HbA1c): The overall effect size for IGs was d = 0.26. Single vs. Multiple behavior intervention comparison: Interventions targeting multiple behaviors (diet, exercise, medication) were more effective than those targeting exercise alone (0.45 vs 0.03). |
Interventions for individuals with type-1 diabetes decrease HbA1c. Outcomes are maximized when interventions targeted multiple behaviors domains, rather than focusing on exercise alone. |
|
Ebrahim et al. (2011) Objective: To assess the effects of multiple behavior domain interventions addressing coronary heart disease (CHD) among adults. |
k = 55 n = 163,471 Population: Mean age = 50 years |
RCTs + minimum 6 month follow-up |
Intervention: diet, exercise, weight loss, salt intake, alcohol use, stress management, smoking cessation, adherence to medication (several combination of two or more behaviors) Control: no specific information reported |
Data reported are weighted mean difference between intervention and control (OR or RR with 95% CIs; between ( ) number of trials where data are reported. Total mortality (14) No strong evidence of reduction (RR: 1.00; 95% CI = 0.96, 1.05). A significant decrease seen in trials (6) where patients were recruited with hypertension or diabetes (RR= 0.78; 95% CI = 0.68, 0.89) and in trials where patients were prescribed medication (RR = 0.86; 95% CI = 0.78, 0.96). CHD mortality (11): OR = 0.99 (95% CI = 0.92, 1.07). Only one trial reported a significant decrease in stroke mortality but the pooled relative risk favored intervention (RR = 0.75; 95% CI = 0.60, 0.95). Fatal and non-fatal clinical events (9). A reduction in events was observed (RR = 0.84; 95% CI = 0.73, 0.98). Effect explained by inclusion of patients with hypertension or diabetes in whom the combined event relative risk was 0.71 (95% CI = 0.61, 0.83). Changing risk factors: Initial level and magnitude of risk factor reduction for diastolic BP (r = 0.73, p = .006), smoking (r = 0.63, p = .01), and cholesterol (r = 0.74, p = .004) indicated that samples with the highest baseline risk demonstrated greater change at follow-up. BP (48). Significant reduction in BP. The weighted mean difference between IGs and CGs was −2.71 mmHg (95% CI = −3.49, −1.93) for systolic BP and −2.13 mmHg (95% CI = −2.67, −1.58) for diastolic BP. Cholesterol (44) Small but highly significant decrease (OR = −0.07 mmol/L; 95% CI = −0.08, −0.06). Stronger effects in trials using antihypertensive and cholesterol lowering drugs (OR = −0.18 mmol/L; 95% CI = −0.22, −0.14). Smoking prevalence (20). Non-significant reduction in smoking prevalence (OR = 0.87; 95% CI = 0.75, 1.00). |
Multiple behavior domain interventions resulted in small reductions in risk factors, including: BP, cholesterol, and smoking. Studies with the highest baseline blood pressure, smoking, and cholesterol levels demonstrated larger decreases in these risk factors at follow up. Interventions using counseling and education aimed at behavior change do not reduce total or CHD mortality or clinical events in general populations, but may be effective in reducing mortality in high-risk hypertensive and diabetic populations. |
|
Ketola et al. (2000) Objective: To assess the effectiveness of lifestyle interventions addressing cardiovascular disease (CVD). |
k = 21 multiple behavior interventions n = 103,416 Population: Working-aged adults (18–65 years); 10 (of 21) multiple behavior interventions were secondary prevention studies |
RCTs + minimum 1 year follow-up |
Intervention Groups: Diet, smoking cessation, exercise, alcohol use, CVD medication (several combinations of two or more behaviors) Control Groups: No specific information reported |
Data reported as mean net changes for( ) number of trials where data are reported. Primary Prevention Studies: Morbidity and mortality: 2 (of 8) studies showed a significant effect on mortality, p < .05. None on morbidity, p > .05. BP: Clinically modest but non-significant improvement in systolic and diastolic BP, p > .05. Cholesterol: −0.36 mmol/L (IGs), p = .08. Weight loss: −0.9 kg (IGs) vs 1.2 kg (CGs), p = .023. Smoking: 2 (of 9) studies reported a significant improvement, p < .05 Alcohol use: 1 (of 1) reported non-significant effect, p > .05. Sodium excretion: Data not reported Exercise: 3 (of 4) studies showed significant effect, p < .05. Secondary Prevention Studies: Morbidity and mortality: 2 (of 5) studies showed a significant effect on mortality, p < .05. One showed a significant effect on CVD morbidity, p < .05. BP: Clinically modest but non-significant improvement in systolic and diastolic BP, p > .05. Cholesterol: −0.43 mmol/L (IGs) vs −.07 mmol/L (CGs), p =.007 Weight loss: −0.6 kg (IGs) vs 1.3 kg (CGs), p = .026. Smoking: 2 (of 7) studies showed a significant effect, p < .05 Alcohol use: 1 (of 3) reported a significant decrease; 37% (IGs) vs 5% (CGs), p = 02. Sodium excretion: 2 (of 4) studies reported significant decrease, p < .05. Exercise: 4 (of 10) studies showed significant improvement, p < .05. |
Multiple behavior domain interventions produced significant improvements in behavioral and clinical risk factors for CVD. Multiple behavior domain intervention outcomes optimized when used for secondary prevention, rather than primary prevention. |
|
Nigg & Long (2012) Objective: To assess effects of single vs. multiple behavior domain interventions in older adults. |
k = 18 n = 2,233 Population: mean age range = 60–79 years; more females than males; mainly non-Hispanic White |
RCTs |
Multiple health behavior change (MHBC): physical activity, diet, smoking cessation, alcohol use (several combinations of two or more behaviors) Single health behavior change (SHBC) interventions: physical activity, diet, smoking cessation, alcohol use (individually) |
SHBC interventions Physical activity studies: (12) Improvements were generally observed in physically activity level (at 6–12 months). Nutrition/weight loss studies: (2) IGs did better than CGs at follow-up (6 months), improving fruit and vegetable intake and adherence to dietary recommendations. Alcohol use studies: (2) IGs reduced their consumption of alcohol, up through 12 months post-intervention. MHBC interventions Physical activity & nutrition related studies: (2) In one study, fruit and vegetable consumption improved, physical activity decreased. In second study, weight loss behavior (meeting calorie and saturated fat goals) and physical activity improved. |
Effective SHBC interventions exist for older adults. Too few studies exist to make comparisons between the effectiveness of MHBC and SHBC interventions in older adults. More research is necessary to determine if older adults benefit from MHBC interventions. |
|
Norris et al. (2004) Objective: To assess effects of weight loss and weight control interventions in adults with type-2 diabetes. |
k = 22; 11 (of 22) multiple behavior interventions n = 4,659 Population: mean age = 55 years; adults with type-2 diabetes |
RCTs + minimum 1-year follow-up |
Intervention Groups: Diet, physical activity Control Groups: Usual care, diet or physical activity intervention differing from the IGs on some dimension (e.g., type of diet, methods of delivery) |
Data reported as mean net changes for( ) number of trials where data are reported. Weight change: (7) In control groups, weight change ranged from a gain of 2.1 kg (usual care) to a loss of 8.2 kg (diet intervention). In intervention groups, weight change ranged from a loss of .06 kg (diet intervention) to 14.5 kg (diet + physical activity + behavioral intervention). HbA1c: (6) Between-group changes (range −2.6%–1.0%) corresponded to changes in weight, and between-group pooled estimates were generally not significant. Systolic & Diastolic BP: (7) Between-group changes ranged from 1–4mmHG. Cholesterol: (13) Between-group changes ranged from −0.4 to −0.33mmol/L. |
Weight loss strategies involving dietary, physical activity, or behavior interventions are associated with small improvements in weight. Multiple behavior domain interventions appear effective for achieving weight loss in adults with type-2 diabetes. |
|
Spring et al. (2009) Objective: To assess effects of multiple behavior domain interventions to promote smoking cessation and weight control. |
k = 10 n = 2,233 Population: 93% female; age range = 18–70 years |
RTCs + minimum 1 month follow-up |
Intervention: smoking cessation + weight control (energy intake, energy expenditure, or attitudes about weight) Control: smoking cessation |
Data reported as OR with 95% CIs Smoking cessation Short-term: OR = 1.29, 95% CI = 1.01, 1.64, p = .041; Long-term: OR = 1.23, 95% CI = 0.85, 1.79; p = .27. Data reported as standardized mean difference (Hedge's g) Post-quit weight gain Short-term: g = −0.30, 95% CI = −0.57, −0.02, p =.035; Long-term: g = −0.17, 95% CI = −0.42, 0.07, p = 0.16. |
Smoking + weight control interventions increase smoking abstinence and decrease weight gain in the short-term (< 3 months) compared with smoking cessation interventions alone. No differences observed in the long-term (> 6 months). |
|
Ussher, Taylor, & Faulkner (2012) Objective: To assess effectiveness of exercise as an aid to smoking cessation. |
k = 15 n = 7,095 Population: Mean age range = 28–59; smokers or recent quitters |
RCTs + minimum 6 month follow-up |
Intervention: exercise + smoking cessation, or exercise alone Control: smoking cessation |
Smoking cessation (15) Short-term: Three studies reported significantly higher abstinence rates in IGs vs. CGs; Long-term: One study found significantly higher abstinence rates in IGs vs. CGs at the 3 month follow-up, and a marginally significant benefit for exercise at 12 month follow-up. One study found significantly higher abstinence rates in IGs vs. CGs at the 3 month follow-up, but not at the end of treatment or at the 12 month follow-up. Nicotine replacement therapy (NRT): (4) One study found higher abstinence rates at the end of treatment and at 12 months follow-up in the exercise + NRT group than in the CG. |
Only one study provided evidence that exercise aids smoking cessation in the long-term (> 6 months abstinence). Other studies were too small to exclude an intervention effect, or had exercise interventions that were not sufficiently intense. More research is necessary to determine if exercise is a beneficial aid to smoking cessation. |
Note. k = number of studies; OR = odds ratio; RR = relative risk, CI = confidence interval; IGs = intervention groups; CGs = control groups
Meta-Analyzing Optimal Recommendation Numbers Based on the Role of Motivation: The Inverted-U Prediction
What is problematic about past reviews of the multi-behavior domain intervention literature is their being based on a small number of reports (for similar points see Nigg & Long, 2012; Ussher, Taylor, & Faulkner, 2012) and not thoroughly considering the role of cognitive and motivational processes in intervention success. Brehm's motivational intensity theory (Brehm & Self, 1989; Brehm et al., 1983) assumes actions are costly and people invest only as much effort as is necessary to achieve a goal. According to this perspective, effort is determined by both the importance of a goal and the difficulty of achieving that goal. Whereas importance determines potential motivation (i.e., the amount of effort people are willing to put into attaining a particular goal), difficulty determines actual motivation (i.e., the amount of actual effort people put into reaching a goal). As easy tasks are perceived as attainable with minimal effort, the amount of effort put forth should be lower than for more difficult tasks, a prediction also possible from Bandura's (1977, 1986, 1997) conceptualization of moderate level goals as most motivating. Interventions recommending a greater number of behaviors are undoubtedly more demanding than single behavior interventions (Nigg & Long, 2012; Patterson, 2001) and, therefore, motivation and follow through should increase as the number of recommended changes increases. In other words, a greater number of recommendations may be associated with increased efficacy because intervention recipients may be further engaged with the intervention and put more effort into attaining the recommended changes than if a single behavior was recommended.
Despite potential advantages of ensuring the necessary level of motivation by targeting multiple behavior changes, a greater number of recommended behaviors may push the human limits of cognitive capacity and self-control (Baumeister, Heatherton, & Tice 1994; Muraven & Slessareva, 2003). Due to restrictions on attending to and implementing multiple recommended behavior changes (Meichenbaum & Turk, 1987; Ornstein et al., 1993), intervention efficacy may either plateau or decrease when more behavior changes are required. Outcome expectancies have been shown to play an important role in motivation (Bandura 1986, 1989, 1997; see Carver & Scheier, 1998; Duval & Silvia, 2002 for reviews on the issue), such that effort decreases when goals are perceived as unattainable. A high number of otherwise appropriate behavioral recommendations may overload the human limits of self-control, undermining self-regulation by leading to the perception that the goals are unattainable or inducing fatigue and resource depletion (Baumeister & Heatherton, 1996; Muraven, Tice, & Baumiester, 1998; Vohs & Heatherton, 2000), and potentially disengagement from the recommended behaviors. Therefore, a smaller number of recommendations may be more efficacious when capacity, instead of motivation, is taken into consideration.
Of course it is most likely that both of these two mechanisms contribute to behavior change. If this is the case, there may be an inverted U-type of effect with a moderate number of recommendations being more effective at changing behavioral, and ultimately clinical, outcomes than either a low or a high number of recommendations. That is, recommending a moderate number of behaviors may be most effective because the intervention ensures the necessary level of motivation to implement the recommended changes (e.g., Bandura 1986, 1989, 1997, 2004; Brehm & Self, 1989; Brehm et al., 1983; Wright, 1996), without making the intervention excessively demanding that engagement decreases (e.g., Baumeister & Heatherton, 1996; Muraven et al., 1998; Vohs & Heatherton, 2000). If both mechanisms co-exist, making more lifestyle recommendations may sometimes result in less behavior and clinical change.
Recipient Motivation to Change May Moderate the Curvature of the Association between Number of Recommendations and Resulting Change
If motivation drives the predicted curvilinear pattern of number of recommendations, delivery to samples that are likely to have low motivation to change may be adverse from the point of view of efficacy, except when the intervention can offset the potential impact of low motivation to change with increased motivation and engagement that may result when a moderate number of behaviors are recommended. As a result, conditions associated with delivery to samples with low motivation to change may show reduced efficacy when the number of recommendations is either low or high, and stronger effects when the number of recommendations is moderate and thus able to motivate the audience.
Modeling the efficacy of multiple behavior domain interventions with an eye on recipients' motivation to change suggests delivery to samples with low motivation to change will be associated with a stronger curvilinear effect of number of recommendations. Conditions that may be associated with delivery to samples with low motivation to change include delivery to non-patient populations, implementation at non-clinic settings, use of lay community facilitators, and group delivery formats. First, when interventions target non-patient populations or are delivered in non-clinic settings, they reach populations that are not already seeking out health care. Prior research suggests that individuals not currently experiencing a health condition may be less motivated, as evidenced by reduced intervention efficacy among lower risk populations (Ammerman, Lindquist, Lohr, & Hersey, 2002; Ebrahim et al., 2011; Hardcastle, Taylor, Bailey, Harley, & Haggar, 2013; Ketola et al., 2000; Corabian & Harstall, 2001; Norris, Englegau, & Narayan, 2001; Norris et al., 2002; Murchie et al., 2003). Furthermore, lay community facilitators are commonly viewed as an appropriate source of health information for populations not easily reached by health professionals, and thus offer a practical means to deliver interventions to audiences that are reluctant to access healthcare that must be captured through outreach efforts (Beck et al., 2013; Clements & Buczkiewicz, 1993; Deering et al., 2009; Enriquez, Farnan, & Neville, 2013; Jones, 1992; McClelland et al., 2002; Nies, Artinian, Schim, Wal, & Sherrick-Escamilla, 2004).1 Specifically, lay community facilitators may be selected for samples reluctant to participate because they can help to overcome barriers to healthcare access among marginalized groups (e.g., language/cultural differences, lack of public transportation, lack of health insurance coverage; Glenton et al., 2013; Karawalajtys et al., 2009; Nies et al.; Slutsky & Bryan-Stevens, 2001). Similarly, group delivery formats may be more likely to be used with audiences with low motivation to change, because this type of delivery format is better suited for the delivery of simple messages that are less tailored to the individual (Ayala, 2006; Greaves & Campbell, 2007; Renjilian et al., 2001; Wright, Sherriff, Dhaliwal, & Mamo, 2011). Group delivery formats may also be selected for samples with low motivation to change, because this delivery format offers potential benefits of social support and shared experiences (Deakin, McShane, Cade, & Williams, 2005; Paul-Ebhohimhen & Avenell, 2009; Skinner & van der Ven, 2005; Trento et al, 2002; Wilson et al., 1993; Wingham, Dalal, Sweeney, & Evans, 2006; Yalom, 1975) that may prove useful for prompting the desire to change in those not currently considering change.
The Present Meta-Analysis
In summary, the optimal number of behavioral recommendations to include in interventions targeting multiple behavior domains remains unclear, as do the mechanisms driving the impact of differing numbers of recommendations. Although prior reviews suggest that promoting change in multiple domains is more effective than targeting a single domain, none have precisely estimated the effects of interventions making varying numbers of behavioral recommendations (e.g., 2 vs. 5 recommendations) on change in behavioral and clinical measures. Moreover, no prior reviews have examined whether the effects of differing numbers of behavioral recommendations vary depending on conditions that are likely associated with delivery to samples with low motivation to change using a sufficiently large set of diverse studies. Gaining a thorough understanding of the effects of interventions making varying numbers of recommendations, particularly among audiences with low motivation to change, is critical to the development of a theory and a set of guidelines that inform the development of multiple behavior domain interventions.
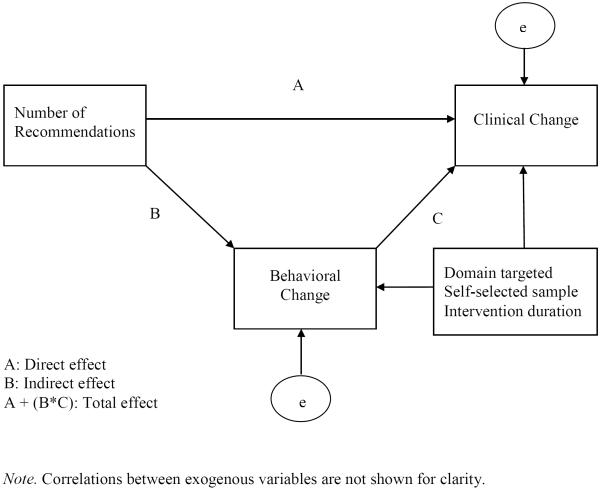
We included reports that summarized findings from interventions targeting change in the domains of smoking, diet, and exercise. As we were interested in examining change over time, reports were required to include a pretest assessment. Our search yielded 150 eligible reports, which provided approximately 93,600 participants. Analyses were conducted to examine the effects of number of lifestyle recommendations on change in behavioral and clinical measures with a sample of 216 intervention groups making multiple recommendations, 15 intervention groups recommending a single behavior, and 39 no-intervention control groups. Beyond considering the impact of differing numbers of recommendations on behavioral and clinical change, it is important to establish whether interventions also influence health behaviors not directly targeted by the intervention. Thus, we also assessed change in behavioral measures as a function of whether a behavior was either targeted or untargeted by the recommendation in interventions making a single recommendation. Finally, to gain an understanding of mechanisms through which multiple domain interventions produce change in clinical measures (e.g., blood pressure, BMI, cholesterol, percent with disease), this meta-analysis gauged whether the impact of an interventions' recommendations on change in clinical health outcomes is mediated by behavior change. As the accuracy of self-reported behavioral measures is often questioned, examination of this mediating mechanism will assist in determining whether the behavioral data included in our meta-analysis are valid and conducive to clinical change. We also conducted exploratory analyses to determine other factors that associated with increased efficacy in multiple domain interventions (e.g., active intervention, face-to face delivery).
Method
Review and Inclusion Criteria
We conducted a computerized search of MEDLINE and PsycInfo for reports published in English that were available by September 24, 2012 using a number of keywords for intervention. These search terms included Intervention, Health education, Persuasion, Recommendation, Treatment, Educational program, Rehabilitation, Counseling outcomes, Treatment outcomes, Treatment effectiveness evaluation, Treatment compliance, Health promotion, Behavior change, and Randomized trial. To identify interventions targeting multiple lifestyle behavior domains, these keywords were entered in combination with keywords for interventions promoting change in (a) diet, (b) exercise, and (c) smoking. To identify diet interventions, we used the keywords Binge eating, Body image, Body weight, Bulimia, Caloric intake, Craving, Diet, Dietary restraint, Eating behavior, Eating disorders, Fat intake, Food intake, Fruit intake, Metabolism disorders, Healthy nutrition, Obesity, Sugar intake, Vegetable intake, Weight control, Weight loss, and Healthy eating. Exercise interventions were searched using Aerobic exercise, Body image, Physical activity, Sport training, Strength training, Weight control, Weight loss, Lack of exercise, Walking, Gymnastics, Going to gym, Running, Biking, Work out, and Physical inactivity as keywords. To search for smoking interventions, we used the keywords Tobacco and Smoking. Next, we used additional strategies to search for published and unpublished work. Using the same keywords, we searched Proceedings and Papersfirst for conference titles. We also emailed the most published authors in our database to request their published and unpublished work. Finally, we examined the reference lists of prior reviews of multiple behavior domain interventions and the papers included in our database to identify other possible articles for inclusion. These additional search strategies did not result in the identification of any additional papers for inclusion although more materials were uncovered.
Once our search for relevant reports was complete, we used several eligibility criteria to select studies for inclusion. The eligibility criteria are explained below:
Presence of at least two groups. To be eligible, reports must include a control group. We considered control groups those that did not expose participants to any kind of intervention at the time of the study (e.g., wait list group, no-intervention group), an intervention group targeting change in a single behavior domain, or a usual care group. In addition, reports were required to include an intervention group targeting change in multiple behavior domains.
Presence of an intervention targeting more than one behavior domain. We included reports evaluating interventions promoting change in diet, exercise, or smoking. Given our interest in examining the effects of the number of recommendations in interventions promoting change in multiple lifestyle domains, only reports that included an intervention targeting at least two of these three domains were considered for inclusion. As multiple behavior domain interventions were the primary focus of this meta-analysis, we did not search for single behavior domain interventions in the domains of concern.
Presence of information to determine the number of behavioral recommendations in the intervention. We included reports that provided a description of the intervention that permitted determining the number of behavioral recommendations included in the intervention. Many control groups were excluded from our analyses because the description of the usual care group did not provide enough detail to code for number of behavioral recommendations (k = 96).
Presence of appropriate statistics. We only included studies that provided information that made it possible to calculate effect sizes representing change over time. Thus, reports without a pretest were excluded (n = 140). In some cases, supplementary information to calculate effect sizes was supplied by the authors of the synthesized reports.
Coding of Study Characteristics
Relevant characteristics of the reports, as well as the methods used in the studies, were coded by two independent raters, as described below. Intercoder coefficients (kappas for categorical variables and simple correlations for continuous variables) are summarized in Table 2. Disagreements between coders were resolved by discussion and further examination of the reports.
Table 2.
Descriptive Statistics
| Variable | Multiple behavior groups (k = 216) | Control groups (k = 54) |
|---|---|---|
| General characteristics of the reports | ||
| Publication year (r = 1) | ||
| M | 2002.24 | 2000.94 |
| Mdn | 2003 | 2002 |
| SD | 6.70 | 7.95 |
| k | 216 | 54 |
| Source type (κ = 1) | ||
| Journal article | 97.2(208) | 94.4(51) |
| Conference proceeding | 0.0(0) | 0.0(0) |
| Doctoral dissertation | 2.8(6) | 5.6(3) |
| Master's thesis | 0.0(0) | 0.0(0) |
| Academic affiliation (κ = .91) | ||
| University | 39.8(86) | 53.7(29) |
| College | 4.2(9) | 3.7(2) |
| Research center | 20.4(44) | 9.3(5) |
| Hospital or health center | 16.2(35) | 13.0(7) |
| Medical school | 15.3(33) | 18.5(10) |
| Other | 4.1(11) | 1.9(1) |
| Institutional area (κ = 1) | ||
| Psychology | 9.3(20) | 11.1(6) |
| Epidemiology | 4.6(10) | 0.0(0) |
| Community/Public health | 6.9(15) | 11.1(6) |
| Medicine | 58.8(127) | 59.3(32) |
| Education | 2.8(6) | 0.0(0) |
| Other | 4.2(9) | 13.0(7) |
| Not identified | 13.4(29) | 5.6(3) |
| Country (κ = 1) | ||
| United States | 48.2(104) | 38.9(21) |
| Finland | 6.0(13) | 5.7(3) |
| United Kingdom | 6.0(13) | 9.5(5) |
| Other | 39.8(112) | 45.9(33) |
| Language (U.S. only; κ = 1) | ||
| English | 100.0(216) | 100.0(54) |
|
| ||
| Types of intervention strategies | ||
| Passive strategies | ||
| Attitudinal arguments (κ = 1) | ||
| Yes | 32.4(70) | 6.7(1) |
| No | 67.6(146) | 93.3(14) |
| Normative arguments (κ = 1) | ||
| Yes | 6.5(14) | 0.0(0) |
| No | 93.5(202) | 100(15) |
| Control arguments (κ = .85) | ||
| Yes | 18.5(40) | 6.7(1) |
| No | 81.5(40) | 93.3(14) |
| Threat arguments (κ = 1) | ||
| Yes | 5.1(11) | 0.0(0) |
| No | 94.9(205) | 100(15) |
| Informational arguments (κ = 1) | ||
| Yes | 91.7(198) | 66.7(10) |
| No | 8.3(18) | 33.3(5) |
| Behavioral skills arguments (κ = 1) | ||
| Yes | 1.4(3) | 0.0(0) |
| No | 98.6(213) | 100(15) |
| Active strategies | ||
| Behavioral skills training (κ = 1) | ||
| Yes | 48.6(105) | 33.3(5) |
| No | 51.4(111) | 66.7(10) |
| Communication skills training (κ = 1) | ||
| Yes | 3.7(8) | 0.0(0) |
| No | 96.3(208) | 100(15) |
| Setting of goals or review of past goals (κ = 1) | ||
| Yes | 44.4(96) | 7.7(1) |
| No | 55.6(120) | 92.3(12) |
| Role playing exercises (κ = 1) | ||
| Yes | 4.2(9) | 0.0(0) |
| No | 95.8(207) | 100(15) |
| Teaches cues to engage in behavior (κ = 1) | ||
| Yes | 5.1(11) | 0.0(0) |
| No | 94.9(205) | 100(15) |
| Training on coping with barriers (κ = 1) | ||
| Yes | 18.1(39) | 6.7(1) |
| No | 81.9(177) | 93.3(14) |
| Relapse prevention training (κ = 1) | ||
| Yes | 7.9(17) | 13.3(2) |
| No | 92.1(199) | 86.7(13) |
| Relaxation training (κ = 1) | ||
| Yes | 10.2(22) | 0.0(0) |
| No | 89.8(194) | 100(15) |
| Time management training (κ = 1) | ||
| Yes | 3.7(8) | 0.0(0) |
| No | 96.3(208) | 100(15) |
| Teaches self-monitoring prompts (κ = 1) | ||
| Yes | 26.4(57) | 13.3(2) |
| No | 73.6(159) | 86.7(15) |
| Stress management skills training (κ = 1) | ||
| Yes | 13.4(29) | 0.0(0) |
| No | 86.6(187) | 100(15) |
| Strategies in both intervention types | ||
| Biological methods (κ = 1) | ||
| Yes | 14.4(31) | 13.3(2) |
| No | 85.6(185) | 86.7(13) |
| Behavioral contract (κ = 1) | ||
| Yes | 4.6(10) | 6.7(1) |
| No | 95.4(206) | 93.3(14) |
|
| ||
| Participant characteristics | ||
| Sample size (N) (r = 1) | ||
| Sum total | 73,858 | 19,709 |
| M | 341.94 | 364.98 |
| Mdn | 85.50 | 62.50 |
| SD | 1,125.39 | 960.84 |
| k | 216 | 54 |
| Age in years (r = 1) | ||
| M | 46.22 | 43.09 |
| Mdn | 50.00 | 44.10 |
| SD | 15.64 | 17.24 |
| k | 206 | 47 |
| % men (r = 1) | ||
| M | 46.58 | 47.07 |
| Mdn | 47.30 | 50.00 |
| SD | 31.30 | 34.61 |
| k | 213 | 53 |
| % women (r = 1) | ||
| M | 54.25 | 53.08 |
| Mdn | 52.70 | 50.00 |
| SD | 31.33 | 34.39 |
| k | 213 | 53 |
| % high school graduates (r = 1) | ||
| M | 46.48 | 43.63 |
| Mdn | 56.00 | 37.00 |
| SD | 35.72 | 38.63 |
| k | 87 | 23 |
| % with risk factor or health condition at pretest (r = 1) | ||
| M | 91.53 | 86.65 |
| Mdn | 100.00 | 100.00 |
| SD | 25.13 | 33.19 |
| k | 116 | 34 |
| Ethnic decent | ||
| % European (r = 1) | ||
| M | 62.99 | 71.25 |
| Mdn | 75.00 | 85.00 |
| SD | 36.55 | 31.47 |
| k | 203 | 51 |
| % African (r = 1) | ||
| M | 29.92 | 15.82 |
| Mdn | 4.35 | 2.00 |
| SD | 31.55 | 24.14 |
| k | 150 | 35 |
| % Latin American (r = 1) | ||
| M | 11.08 | 8.01 |
| Mdn | .00 | .00 |
| SD | 23.87 | 18.92 |
| k | 132 | 30 |
| % Asian (r = 1) | ||
| M | 18.21 | 14.97 |
| Mdn | 2.90 | 2.90 |
| SD | 35.45 | 30.73 |
| k | 134 | 36 |
| % North American Indian (r = 1) | ||
| M | 1.09 | .21 |
| Mdn | .00 | .00 |
| SD | 9.14 | .43 |
| k | 120 | 32 |
|
| ||
| Intervention set-up | ||
| Domains targeted | ||
| Diet (κ = 1) | ||
| Yes | 96.8(209) | 33.3(5) |
| No | 3.2(7) | 66.7(10) |
| Exercise (κ = 1) | ||
| Yes | 99.1(214) | 46.7(7) |
| No | .9(2) | 53.3(8) |
| Tobacco use (κ = 1) | ||
| Yes | 52.8(114) | 20.0(3) |
| No | 47.2(102) | 80.0(12) |
| Alcohol use (κ = 1) | ||
| Yes | 10.2(22) | 0.0(0) |
| No | 29.8(194) | 100.0(15) |
| Medication adherence (κ = 1) | ||
| Yes | 7.4(16) | 0.0(0) |
| No | 92.6(200) | 100.0(15) |
| Cancer screening (κ = 1) | ||
| Yes | 0.5(1) | 0.0(0) |
| No | 99.5(217) | 100.0(15) |
| Number of recommendations (r = 1) | ||
| M | 3.41 | 1.0 |
| Mdn | 3.00 | 1.0 |
| SD | .86 | 0.0 |
| k | 216 | 15 |
| Setting of exposure (κ = 1) | ||
| School | ||
| Yes | 7.9(17) | 13.3(2) |
| No | 92.1(199) | 86.7(13) |
| Clinic | ||
| Yes | 57.4(124) | 73.3(11) |
| No | 42.6(92) | 26.7(4) |
| Community (street, community center, bar) | ||
| Yes | 4.6(10) | 0.0(0) |
| No | 95.4(206) | 100.0(15) |
| Business | ||
| Yes | 8.3(18) | 0.0(0) |
| No | 91.7(198) | 100.0(15) |
| Mass media | ||
| Yes | 8.8(19) | 0.0(0) |
| No | 91.2(197) | 100.0(15) |
| Medium of delivery (κ = .97) | ||
| Face to face | ||
| Yes | 86.1(186) | 100.0(15) |
| No | 13.9(30) | 0.0(0) |
| Delivery format (κ = 1) | ||
| Groups | 20.4(44) | 33.3(5) |
| Individuals | 44.0(95) | 46.7(7) |
| Both | 35.6(77) | 20.0(3) |
| Facilitator (κ = .93) | ||
| Professional expert | 69.0(149) | 53.3(8) |
| Lay community member | 25.9(56) | 46.7(7) |
| Both | 5.1(11) | 0.0(0) |
| Culturally appropriate intervention (κ = .89) | ||
| Yes | 11.1(24) | 0.0(0) |
| No | 88.9(192) | 100.0(15) |
| Duration of intervention in hours (r = 1) | ||
| M | 18.46 | 25.78 |
| Mdn | 10.00 | 12.00 |
| SD | 22.83 | 31.06 |
| k | 158 | 9 |
|
| ||
| Research design and implementation | ||
| Random assignment to conditions (κ = .97) | ||
| Yes | 86.5(187) | 85.2(46) |
| No | 13.5(29) | 14.8(8) |
| Payment received (U.S. dollars; r = .93) | ||
| M | 55.00 | 23.75 |
| Mdn | 20.00 | 22.50 |
| SD | 146.44 | 27.50 |
| k | 23 | 4 |
| Days between intervention and posttest (r = .88) | ||
| M | 103.90 | 93.39 |
| Mdn | 28 | 14 |
| SD | 143.71 | 135.55 |
| k | 195 | 15 |
| Patient population (κ = 1) | ||
| Yes | 34.7(75) | 33.3(5) |
| No | 65.3(141) | 66.3(10) |
| Sample targeted by ethnicity (κ = 1) | ||
| Yes | 11.6(25) | 0.0(0) |
| No | 88.4(191) | 100.00(15) |
| Sample targeted by gender (κ = 1) | ||
| Yes | 26.9(58) | 46.7(7) |
| No | 73.1(158) | 53.3(8) |
| Self-selected sample (κ = 1) | ||
| Yes | 89.4(193) | 83.3(45) |
| No | 10.6(23) | 16.7(9) |
Note. k = number of cases. r = intercoder reliability for continuous variables. κ = intercoder reliability for categorical variables.
Description of the report
We coded studies for characteristics of the report, including the (a) publication year, (b) the first authors' institution (e.g., college, research center), (c) the first authors' institutional area (e.g., psychology, community/public health, medicine), (d) source type (e.g., journal article, unpublished dissertation or thesis, conference paper), (e) location of the intervention, and (f) language of the intervention.
Domains of behavior change and recommendations
Papers were also coded for whether they encouraged change in the primary domains of (a) diet, (b) exercise, and (c) smoking, as well as frequent secondary domains of (d) alcohol use, (e) medication adherence, and (f) cancer screening. Interventions that targeted change in more than one domain (e.g., exercise and diet) were classified as multiple behavior domain interventions, whereas those targeting change in a single domain (e.g., exercise) were considered single behavior domain interventions. Although the presence of an intervention targeting more than one behavior domain was a criterion for eligibility, this variable was not used in our count for number of behavior recommendations.
We coded interventions for number of behavioral recommendations by counting the total number of primary goals (e.g., reduce calories, increase fruit and vegetable intake, increase physical activity) that interventions were described as targeting. For example, the multiple behavior domain intervention in Ussher, West, McEwen, Taylor, and Steptoe (2003) was coded as presenting two recommendations because participants were instructed to engage in physical activity for 30-minutes or more on at least 5 days per week, and to stop smoking. In contrast, the control group in Spring et al. (2004) was coded as making one behavioral recommendation because participants were instructed to quit smoking. All primary goals were included in our count for number of behavioral recommendations, but more specific behavioral skills discussed as means to reaching those goals (e.g., monitoring urges, coping with temptation) were not counted because they are not reported in a reliable way. Although we coded for the inclusion of biological methods (e.g., nicotine replacement drugs), their presence was not counted as a behavioral recommendation, but rather as a biomedical strategy to reaching the recommended behavior. For interventions making a single behavioral recommendation, we also coded for whether the behavioral outcome measures were targeted by the recommendation (i.e., yes vs. no). For example, in an intervention that made a single behavioral recommendation to increase physical activity, measures assessing physical activity level were coded as targeted by the recommendation whereas any additional measures (e.g., measures assessing fruit and vegetable intake) were coded as untargeted.2
Facilitator characteristics
As some interventions used both types of sources, we coded whether the facilitator was a lay community member (i.e., yes vs. no) and whether the facilitator was a professional expert (i.e., yes vs. no). Lay community members included community leaders and peers, such as nonprofessional peer counselors. Professional experts included physicians, public health educators, nurses, dieticians, physical therapists, teachers, members of the research team, social workers, psychologists, counselors, and medical students. Of course, the two dummy codes for expertise and lay community membership were extremely highly correlated (r = −.89, p < .001). However, as some interventions included both types of facilitators, the correlation was not perfect and we used both indexes in analyses.
Delivery format
We coded whether interventions were delivered to individuals (i.e., yes vs. no) and groups (i.e., yes vs. no). Interventions were coded for the use of both formats because some interventions used both group and individual formats. The two dummy codes for delivery format were highly correlated (r = −.54, p < .001) and both indexes were used in analyses.
Other characteristics
We coded the demographic characteristics of the participants. To describe the characteristics of the sample, we recorded the (a) sample size, (b) percentage of males in each group, (c) lowest, highest and mean age, (d) percentage of participants of European, African, Latin, Asian, and Native American descent3, (e) percentage of participants who completed high school and mean years of education, and (f) percentage of participants with a health condition (e.g., diabetes, heart disease, and obesity).
We also coded for characteristics related to the intervention setup. We classified each intervention group according to (a) whether interventions included strategies that were active (e.g., behavioral skills training or client-tailored counseling components) or used only passive strategies (e.g., attitudinal arguments, informational arguments; see Albarracín et al., 2005), (b) interventions were also coded for whether they included biological methods, such as nicotine patches or drugs to reduce food cravings, or asked recipients to sign a behavioral contract for performance of the recommended behaviors, and these ratings were made independent of the classification of an intervention being more or less resource demanding as both types of interventions included these strategies, (c) the setting of exposure (i.e., clinic, school, community, mass media), and recoded this variable to provide an indicator clinic vs. non-clinic setting, (d) the form of media used to deliver the intervention (i.e., face-to-face interactions, video or audio taped materials), (e) whether the intervention was defined as culturally appropriate, (f) the location of recruitment (e.g., drug treatment facility, classroom, hospital), (g) the duration of the intervention in terms of total number of counseling contacts/visits, the length of each visit in minutes, and the number of days from the baseline until the end of the intervention.
Finally, we coded for factors related to the research design and implementation. We coded studies for (a) whether the design was within-subjects or whether the samples were different at pre- and posttest, (b) whether participants were randomly assigned to conditions, (c) the amount of money (in U.S. dollars) received in exchange for participation, (d) the mean and median number of days between the intervention and the posttest, (e) whether clinical outcomes were assessed objectively or relied on participant self-reports, (f) the specific sample to which the intervention was targeted (e.g., cardiac patients, hypertensive patients on medication, college students, smokers, obese adults), and recoded this variable to indicate whether the intervention targeted non-patient vs. patient populations, and (g) whether the intervention was targeted to a specific (h) ethnic or (i) gender group. We also coded for whether the sample was (j) self-selected, as indicated by whether participants took part in the study on a voluntary basis versus were more captive groups, such as participants in classrooms, inpatient hospitals, or prisons.
Retrieval of Effect Sizes
Effect sizes were calculated independently by two coders. When different effect sizes were calculated, a third researcher examined the effect size calculations and resolved the disagreement by discussion. For reports containing more than one measure of a construct of interest, we calculated effect sizes for each measure and the average effect size was used as the effect size for that particular variable (see B.T. Johnson, 1993). To indicate change in pretest to posttest measures, we used Becker's (1988) g, which was calculated by subtracting the mean at posttest from the mean at pretest and dividing the difference by the standard deviation of the pretest measure. Effect sizes were also calculated from exact reports of t tests, F ratios, proportions, p values, and confidence intervals. Depending upon the behaviors targeted in an intervention, we calculated effects sizes representing change in outcomes related to diet, exercise, and smoking, as well as additional outcomes related to alcohol use, medication adherence, cancer screening, and more general health outcomes. Effect sizes were always calculated as improvements from a health perspective (e.g., decrease in BMI, increase in fruit and vegetable intake). Outcomes were assessed using behavioral, clinical, and psychological measures, as described below.
Behavioral measures
The synthesized reports included a large variety of behavioral measures, which were used to calculate effect sizes reflecting improvements in health. The most frequent measures in the area of diet were energy intake (e.g., kcal/week, kcal/day, kj/day); carbohydrate, protein, fiber, fat, calcium, iron, vitamin, fruit, and vegetable (in milligrams, grams or servings) intake; number of meals per day; whether participants complied with the dietary recommendations; whether participants met daily guidelines for fruit and vegetable intake; whether participants checked their blood pressure in the past 12 months; presence of unhealthy eating; presence of overeating; and water intake. The most frequent behavioral measures in the exercise domain were whether participants exercised daily; weekly hours of physical activity; presence of occupational physical activity; whether participants reported regular physical activity; whether participants complied with exercise recommendations; whether participants were sedentary; whether participants reported high impact activity; presence of self-monitoring of pulse and blood pressure; presence of self-monitoring with pedometer (daily pace); time spent in physical activity; energy expenditure in physical activity (k/cal); and number of TV hours per day.
The most frequent behavioral measures in the smoking domain were whether participants currently smoked; and number of cigarettes per day (often via diaries).
There were also supplementary behavioral measures related to medication and screening in areas for diseases associated with diet, exercise, and smoking. These measures included never forgetting to take medication; forgetting to take medication; lack of adherence to the treatment plan; picking up medications; refilling medication; missing medication doses; using medication delivery methods; incorporating the medication regimen into one's daily life; and acquiring social support for adherence (e.g., involvement with friends, attending support groups, and community involvement). Moreover, some studies included such measures as whether participants had a PAP test within the past 2 years; whether participants had a mammogram within the past 2 years; whether participants had a lipid panel test; whether participants had a chest X-ray within the past year; whether participants had a dental cleaning within the last 6 months; and presence of other health seeking measures including specific lab tests within the past year.
Clinical measures
Among the many clinical measures used in the studies were body weight in kilograms; body mass index; hip size; waist size, hip/waist ratio; body fat measures; whether participants were overweight; whether participants were obese; systolic blood pressure; diastolic blood pressure; triglycerides level; HDL/LDL cholesterol; fasting blood glucose; results from other lab tests for diabetes; whether participants had diabetes; whether participants had metabolic syndrome; pulse; results from spirometer tests; results from VO2 Max tests; results from chest X-ray; whether participants had nicotine in blood; results from lab tests to confirm right dose of medication in blood; results from PAP reports; results from mammograms; results from dental records; and results from colonoscopy reports.
Psychological measures
Psychological measures present in the studies included beliefs about the benefits of a behavior for improving the desired clinical outcome (e.g., Physical activity is beneficial for lowering blood pressure; Burke, Giangiulio, Beilin, Houghton, & Millligan, 1999, p. 275); self-efficacy for performing the targeted behavior (e.g., How confident are you that you will be able to quit smoking for the next 3 months?; Kinnunen et al., 2008, p. 693); worry about weight (e.g., How concerned are you about gaining weight as a result of quitting?; Borrelli & Mermelstein, 1998; p. 622), and knowledge (e.g., ability to correctly identify LDL targets; Lichtman et al., 2003).
Analytic Strategy
We calculated weighted mean effect sizes to examine change over time for interventions making varying numbers of recommendations. Corrections for sample-size bias were performed to estimate the effect size of d. Hedges and Olkin's (1985) procedures were used to correct for sample size bias4, calculate weighted mean effect sizes (d), confidence intervals, and to estimate homogeneity statistics (Q), which test the hypothesis that the observed variance in effect sizes is no greater than that expected by sampling error alone. For between-subject designs, we calculated the variance of effect sizes following Hedges and Olkin's procedures. For within-subjects designs, we followed Morris' (2000) procedures to calculate the variance of effect sizes, and the correlation between the pre- and posttest measures was estimated at r = .50. Changing this correlation did not alter the pattern of findings. After computing effect sizes for each outcome measure, for each case we computed an average effect size indicating overall change, as well as average effect sizes for change in behavioral and clinical outcomes.
We performed analyses using fixed- and random-effects procedures. When conducting fixed-effects analyses, we weighted effect sizes using the inverse of the effect size's variance, which allowed effect sizes from studies with larger sample sizes to carry more weight than effect sizes from studies with smaller sample sizes.5 For random-effects models, we added a random variance component to the variance of each effect size, and recalculated the inverse variance prior to weighting the effects sizes. All analyses controlled for the effects of intervention duration by including this variable as a covariate in the model. In addition, as the type of strategies used in an intervention may vary as a function of the targeted domains, we controlled for whether studies targeted change in smoking, alcohol use, and medication adherence. Given that the majority of cases targeted change in exercise and diet (see Table 2), it was unnecessary to control for these domains in our analyses. We also controlled for whether the sample was self-selected, because self-selected samples were associated with stronger improvements in overall change than samples that were not self-selected, fixed-effects QB = 159.98, p < .001, k = 271.
Many of our analyses were conducted using analysis of variance (ANOVA) procedures. When conducting analyses, we entered the inverse of the variance of the effect size being predicted as a weight, and determined whether effects were significant by examining the significance of QB, which is a sum of squares analogous to an F ratio but distributed as a chi-square. QBs were obtained for the main effects of number of recommendations and intervention characteristics, the simple effects for intervention characteristics, and also for interaction terms between number of recommendations and intervention characteristics. After establishing the impact of differing numbers of recommendations, we conducted mediation analyses to identify the potential mechanism that accounts for the relation between number of recommendations and change in clinical outcomes. Specifically, we examined whether change in behavior following participation in a health promotion intervention mediates change in clinical indicators of health. Further details are provided as they become relevant.
Results
Sample of Interventions and Controls
We included 150 reports, which provided 216 intervention groups recommending multiple behaviors, 15 intervention groups recommending a single behavior, and 39 no-intervention control groups (e.g., waitlist, no treatment controls). Of the 150 reports, 50 provided a single data set, 80 provided two data sets, 16 provided three data sets, and 3 provided four data sets.6 Table 2 provides information about the included reports, and contains descriptions of the intervention participants, recommendations, strategies, and methods, with separate columns for multiple behavior intervention and control groups. As can be seen, most of the studies were published around 2003 and the median sample sizes were about 86 and 63 participants for multiple behavior intervention and control groups, respectively. Thirty-one countries were represented, with the majority of studies being conducted in the United States. Of the studies conducted in the U.S., 24 states were represented with California providing more groups than any other state.
As can be seen in Table 2, the majority of interventions included recommendations targeting change in exercise, dietary, or smoking behaviors. Interventions less frequently included recommendations targeting change in behaviors such as alcohol use, medication adherence, and cancer screening. Interventions recommending multiple behaviors included on average 3.41 (SD = 0.86, Range = 2–5) recommendations. With respect to the type of intervention to which recipients were exposed, 70% of groups were exposed to an intervention that involved more resource demanding strategies, whereas the remaining 30% of groups were exposed to interventions that relied solely on less resource demanding strategies. Strategies that were less resource demanding commonly included (a) informational statements about the targeted behaviors (79%), (b) arguments designed to induce a positive attitude toward the recommended behaviors (80%), and (c) arguments to enhance perceptions of control (13%). Fourteen percent of interventions included biological treatments (e.g., nicotine patches), and these types of treatments were administered in both types of interventions.
The papers we examined were diverse, in terms of the participants, intervention set-up, and research design and implementation. Samples comprised both females and males, and participants were on average middle age. On average, 67% of participants were of European decent, 45% of participants had completed high school, and 90% were described as having a risk factor, precursor to a health condition, or a health condition at pre-intervention. The samples included individuals at-risk or with a history of obesity, type-1 or type-2 diabetes, coronary heart disease, chronic kidney disease, congestive heart failure, hypertension, and high cholesterol, and 33% were described as a patient population at baseline. More interventions were delivered in clinics than in any other place, although interventions were also conducted in schools and in workplaces, as well as through the mass media. The majority of interventions were presented face-to-face (93%), exclusively used an individual delivery format in 45% of the cases, and exclusively used professional experts as facilitators in 61% of cases. On average, interventions lasted approximately 22 hours.
Finally, there was variability in research design and implementation across studies. All studies included pre- and posttest measures and the majority of the designs were within-subjects. However, some studies did use different participants at pre- and posttest. The assignment of participants to study condition was done at random in 87% of cases and participants were compensated on average U.S. $39.38. The mean length of time between the intervention and the posttest was slightly over three months for both interventions recommending a single behavior and those recommending multiple behaviors. Clinical outcomes were assessed objectively in the majority of cases (96%). The majority of interventions were targeted to a specific population, such as a population with a particular health condition or risk factor (e.g., women with coronary heart disease), and samples were frequently self-selected.
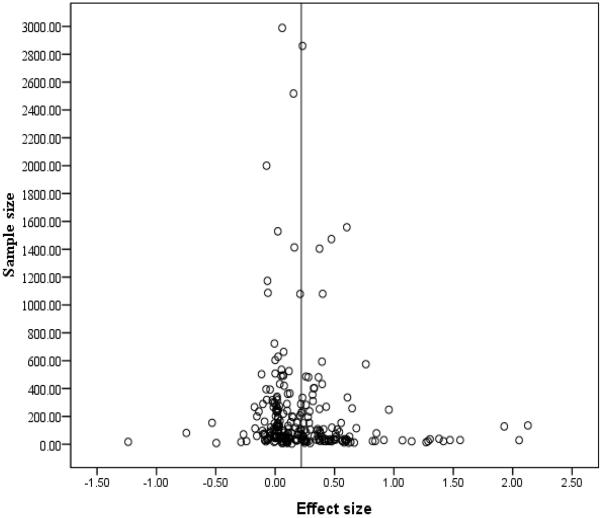
Average Intervention Effect Size
We first obtained a weighted-mean average of overall change and tested for variability among effect sizes in intervention groups recommending multiple behaviors, intervention groups recommending a single behavior, and control groups. For interventions recommending multiple behaviors, the average effects size was d = 0.17 (95% confidence interval [CI] = 0.16, 0.18; Q(216) for homogeneity = 2,829.83, p < .001) according to the fixed-effects model, and d = 0.23 (95% CI = 0.19, 0.26; Q(216) for homogeneity = 346.47, p < .001) according to the random-effects model. In interventions recommending a single behavior, the average effect size from the fixed-effects analysis was d = 0.07 (95% CI = 0.02, 0.13; Q(14) for homogeneity = 48.66, p < .001), and the average effect size from the random-effects analysis was d = 0.11 (95% CI = −0.04, 0.24; Q(14) for homogeneity = 11.06, p > .05). Finally, the average effect size for no-intervention control groups was d = 0.06 (95% CI = −0.01, 0.12; Q(38) for homogeneity = 267.48, p < .001) according to the fixed-effects model, and d = 0.04 (95% CI = −0.06, 0.13; Q(38) for homogeneity = 31.40, p > .05) according to the random-effects model. As most tests for homogeneity were statistically significant, indicating a large amount of variability between effect sizes, we examined whether our moderators accounted for a significant amount of this variability. We also conducted exploratory moderator analyses to identify other factors that likely influence efficacy in interventions recommending multiple behaviors.
Given that these initial analyses involved average effect sizes and that the number of measures contributing to our final effect size calculations differed across studies, we examined whether the number of measures included in an intervention varied as a function of number of recommendations. As interventions recommending a single behavior (Range 1–13, M = 5.93; SD = 4.20) included a comparable number of indicators as interventions making a moderate (Range 1–16, M = 4.71; SD = 3.01) and high (Range 1–16, M = 5.05; SD = 3.17) number of recommendations, F(2, 228) = 17.41, p > .05, it was unnecessary to control for the number of included measures in our analyses. This test provided reassurance for the use of average effect sizes in our final effect size calculations.
Furthermore, we compared the inclusion of clinical outcome measures across different intervention characteristics using chi-square tests. These analyses revealed that the inclusion of clinical measures was highly comparable across key intervention characteristics. Specifically, the inclusion of clinical measures was comparable for interventions recommending a single behavior (vs. multiple behaviors X2 (1, N = 231) = 0.10, p > .05), interventions delivered to non-patient populations (vs. patient populations, X2 (1, N = 231) = 0.77, p > .05), interventions implemented at non-clinic settings (vs. clinic settings, X2 (1, N = 231) = 1.19, p > .05), interventions implemented by community member (vs. non-community members, X2 (1, N = 231) = 1.88, p > .05), and interventions using group delivery formats (vs. individual delivery, X2 (1, N = 231) = 0.16, p > .05). Finally, we examined whether the effect of number of recommendations on overall change varied depending on whether papers included clinical outcomes and found no evidence of moderation, fixed-effects QB = 2.67, p > .05, k = 270. Together, these tests provided reassurance for the use of an indicator of overall change, combining behavioral and clinical effects, in our subsequent analyses.
Targeted Versus Untargeted Behavioral Change
We next explored whether change in behavioral measures was greater when outcomes were targeted in comparison to when outcomes were not targeted by a behavioral recommendation. To conduct these analyses, we examined whether interventions making a single behavior recommendation assessed change in behavioral outcomes untargeted by the recommendation, as this allowed for the comparison of change in targeted versus untargeted measures. Among interventions making a single behavior recommendation that included multiple behavioral measures (k = 5), we computed a weighted mean effect size for change in targeted and untargeted measures. Whether a measure was targeted by the recommendation in an intervention making a single behavioral recommendation significantly predicted overall change. The weighted mean effects sizes from the fixed-effects analyses suggested that compared to untargeted behaviors (d = 0.04 (95% CI = 0.01, 0.06), change was significantly greater in targeted behaviors (d = 0.33 (95% CI = 0.31, 0.36), fixed-effects QB = 4.99, p < .05, k = 5, and random-effects QB = 4.51, p < .05, k = 5.
Change as a Function of Number of Recommendations
Overall effects across interventions and control groups
More important than establishing that change is greater when outcomes are targeted by a recommendation is to determine the optimal number of recommendations to include in behavioral interventions. Thus, we then examined change in behavioral and clinical outcomes, as well as overall change across the average of all outcomes, as a function of number of recommendations. As some values for the number of recommended behaviors had a low frequency, we recoded number of recommendations prior to conducting these analyses (0 = 0 recommendations; k = 39, 1 = 1 recommendation; k = 15, 2 = 2-3 recommendations7; k = 110, 3 = 4 or more recommendations; k = 106). Moreover, when number of recommendations was left as a continuous variable some cells had a low frequency in our moderator analyses and the recoding corrected for this issue. In these analyses, interventions making 0 recommendations represent no-intervention control groups.
The weighted mean effect sizes and confidence intervals (CIs) from the fixed-effects analyses, along with QBs from the fixed- and random-effects analyses, appear in Table 3. As can be seen, a curvilinear relation exists between the number of behavioral recommendations and intervention effectiveness, and for all three outcomes stronger average improvements across outcomes were observed with interventions making 2-3 recommendations.8 However, a weaker effect was observed when change in clinical outcomes was considered. The stronger effect on average behavioral change is anticipated given that these outcomes are most proximal to the intervention and are likely to then drive clinical outcomes. Although interventions making multiple behavioral recommendations were in general more effective than interventions making a single recommendation, there is a limited benefit to increasing the number of recommendations in an intervention. In particular, our results indicate that interventions making a moderate number of recommendations are most efficacious, providing evidence that more lifestyle recommendations do not result in healthier outcomes.
Table 3.
Change as a Function of Number of Recommendations Controlling for Duration, Domain Targeted, and Self-Selected Sample.
| d (95% CI) | |||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Number of Recommendations | |||||||
|
|
|||||||
| Outcome | 0 | 1 | 2–3 | 4 or more | Fixed-effects QB | Random-effects QB | k |
| Behavioral | 0.05a(−0.07, 0.17) | 0.11b(−0.11, 0.33) | 0.29c(0.17, 0.41) | 0.14b(0.03, 0.25) | 300.09*** | 34.87*** | 205 |
| Clinical | 0.17a(0.04, 0.30) | 0.12a(−0.13, 0.36) | 0.27b(0.13, 0.40) | 0.22c(0.12, 0.33) | 32.56*** | 12.07** | 199 |
| Overall | 0.10a(0.01, 0.20) | 0.17b(−0.02, 0.36) | 0.33c(0.23, 0.43) | 0.19b(0.10, 0.27) | 282.94*** | 33.74*** | 270 |
Note. Change for intervention and control groups as a function of number of recommendations. CI = confidence interval. d = fixed-effects weighted means. QB = homogeneity coefficient for the difference across levels of a factor, distributed as a chi-square with degrees of freedom equal to the number of factor levels − 1. Within each row, ds with similar subscripts are not significantly different from one another.
p < .05,
p < .01,
p < .001.
Now, given that the number of outcomes assessed may vary depending on the number of recommendations included in an intervention, one could argue that smaller effect sizes may not necessarily equal less change. Specifically, our indicators of average change may not be ideal to capture improvements in interventions making varying numbers of recommendations. Given this possibility, we conducted additional analyses in which the dependent variables of behavioral, clinical, and overall change were computed by summing, rather than averaging, effect sizes. These analyses revealed a similar pattern of results for all three indicators of change, whereby interventions recommending a moderate number of behaviors were associated with stronger improvements. For example, the weighted mean effects sizes from the fixed-effects analyses suggested that overall change was significantly greater in interventions targeting 2-3 recommendations (d = 2.03 (95% CI = 1.12, 2.94) than in interventions making 0 (d = 0.61 (95% CI = −0.27, 1.51), 1 (d = 0.69 (95% CI = −0.54, 1.92), or 4 or more (d = 1.26 (95% CI = 0.54, 1.99) recommendations, respectively, fixed-effects QB = 551.56, p < .05, k = 270, and random-effects QB = 34.57, p < .05, k = 270. These additional analyses strengthen our conclusion that interventions making a moderate number of lifestyle recommendations are associated with stronger improvements than interventions making either high or low numbers of recommendations.
Intervention Duration
Given prior research suggesting that intervention intensity is related to intervention efficacy (e.g., Aguiar et al., 2014; Ebrahim et al., 2011; Ketola et al., 2000; McAlister et al., 2001), we examined whether duration interacted with number of behavioral recommendations to predict overall change. Our analyses revealed that interventions recommending a moderate number of recommendations were most effective (QB for main effect = 69.07, p < .001, k = 167) and that duration significantly interacted with number of recommendations (QB = 69.07, p < .001, k = 167). Interventions of shorter duration (1 SD below mean) were more effective when they recommended a single behavior (d = 0.24 (95% CI = −0.09, 0.57) than when they recommended a moderate (d = 0.12 (95% CI = 0.02, 0.23) or high (d = −0.03 (95% CI = −0.09, 0.07) number of behaviors. In contrast, interventions of average duration were more effective when they recommended a moderate number of behaviors (d = 0.20 (95% CI = 0.13, 0.28) than when they recommended a single (d = 0.11 (95% CI = −0.09, 0.33) or high (d = 0.02 (95% CI = −0.03, 0.07) number of behaviors. Similarly, interventions of longer duration (1 SD above mean) were more effective when they recommended a moderate number of behaviors (d = 0.28 (95% CI = 0.23, 0.37) than when they recommended a single (d = 0.00 (95% CI = −0.26, 0.263) or high (d = 0.07 (95% CI = 0.03, 0.11) number of behaviors.
Although these findings suggest that the best strategy when implementing shorter interventions is to recommend a single behavior, interventions of average or longer duration appear to be associated with improved outcomes when a moderate number of behaviors are targeted. As such, allowing adequate time for implementation must be considered when designing interventions that recommend multiple behavior changes. As intervention efficacy varied as a function of intervention duration, we introduced this variable as a covariate in all analyses.
Behavior Change as a Mediator of the Influence of Recommendation Number on Clinical Change
Next, we conducted analyses to identify whether behavior change mediates the relation between number of recommendations and change in clinical outcomes. The generic mediation model (MacKinnon, Fairchild, & Fritz, 2007) is presented in Figure 1. In this model, number of recommendations was treated as a continuous variable, and was used to predict the behavioral change outcome mediator and the clinical change outcome directly. To estimate the model, we used Mplus, Version 5 (Muthén & Muthén, 2006), using maximum likelihood estimation and analyzed all cases even though missing values were present (Enders & Bandalos, 2001). We also weighted the effect sizes based on the reciprocal of the standard errors of the effect size estimates, as discussed earlier. We report the parameters for the path going from number of recommendations to clinical change (parameter A), the path going from the number of recommendations to behavioral change (parameter B), the path going from behavioral to clinical change (parameter C), and the percent of the total effect of recommendations on clinical change that is mediated, calculated from the analysis of the direct, indirect, and total effects (Streiner, 2005). We present unstandardized results to permit direct comparability of effect sizes (Greenland, Schlesselman, & Criqui, 1986), as well as the standardized results.
Figure 1.
Model to determine the mediating effects of change in behavioral outcomes on clinical change.
Given our theoretical predictions and our results suggesting that intervention efficacy begins to decrease when interventions recommend a large number of behaviors (see Table 3), our models included a quadratic term for number of recommendations. Prior to squaring the number of recommendations term, we centered this variable on the mean of the sample. When we included both the linear and quadratic components in our model, the direct effect of number of recommendations on behavioral change (linear term = 0.018, p > .05; quadratic term = −0.008, p > .05) and its indirect effect on clinical outcomes (linear term = 0.005, p > .05; quadratic term = −0.002, p > .05) were not significant. The lack of mediation when both the linear and quadratic terms were included in the model is likely due to multicollinearity, as indicated by the high correlation between the two variables (r = −.64, p < .001) and VIFs that are greater than two for both variables. Thus, we report results from our final model that included only the centered quadratic term for number of recommendations. This functional form of recommendations assumes that recommendations have differential impact on changes as they differ either higher or lower from the average value. If the coefficient of this variable is negative, interventions with either high or low number of recommendations are less effective in producing change in effect size outcomes than interventions with average values. If the coefficient of this variable is positive, interventions with either high or low number of recommendations are more effective in producing change in effect size outcomes than interventions with average values.
As can be seen in Table 4, the effect of number of recommendations on clinical change was mediated by change in behavioral outcomes. The direct effect of number of recommended behaviors was nonsignificant when we introduced behavioral change, suggesting that behavioral change was in fact a plausible mediator. The indirect effect of number of recommendations on clinical change was negative: departures from the average (moderate) number of recommended behaviors reduced behavioral effect sizes (see parameter B). Furthermore, behavioral effect sizes were positively related to larger clinical effect sizes (see parameter C), resulting in a negative indirect B*C effect. Importantly, as the direct effect of number of recommendations on clinical change was positive and about the same size as the negative indirect effect, these two countering balancing processes operated cumulatively to produce a near zero total effect. Thus, the percent mediated of the total effect was not a meaningful concept in this case. This type of compensating mediation was highlighted in early work on mediation and meta-analysis (Shadish, 1996, p. 56). In sum, our results suggested that behavioral change completely mediates the relation between quadratic recommendations and clinical change. In addition, as departures from the average number of recommendations had a negative effect on behavioral change, these findings are consistent with our hypothesis that more lifestyle recommendations do not always result in healthier outcomes.
Table 4.
Mediational Analysis of Centered Squared Form of Number of Recommendations.
| Mediator and Outcome | |||||
|---|---|---|---|---|---|
|
| |||||
| Mediator: Behavioral Change | Outcome: Clinical Change | ||||
|
| |||||
| Predictor | Direct Effect on Behavioral Change | Direct Effect on Clinical Change | Indirect Effect on Clinical Change | Total Effect on Clinical Change | % Indirect of Total |
| Quadratic Recommendation | −0.016*(−0.19) (B parameter) | 0.007(0.07) (A parameter) | −0.006*(−0.07) | 0.001(0.007) | See text |
| Number Behavioral Change | -- | 0.371*(0.35) (C parameter) | -- | -- | -- |
Note. Model is Mediation Figure 1 with adjustment variables noted there. k = 267 effect size records. Data are weighted. Entries are unstandardized coefficients with standardized coefficients in parentheses. R2 of behavioral change is .15. R2 of clinical change is .17.
p < .05
Effects of Number of Recommendations across Conditions of Varying Motivation to Change
Another goal of this meta-analysis was to test whether conditions related to implementation among intervention recipients with low motivation change moderates the effect of number of recommendations. One possible prediction is that among reluctant audiences, the intervention would have reduced effects, except when the intervention is sufficiently motivating to compensate for their lower levels of motivation. Given the similar effect of number of recommendations on behavioral and clinical change, we tested overall change as an outcome variable in ANOVAs weighted by the corresponding variance of the sample size, and our moderators as independent variables. All moderator analyses excluded control groups because there was no facilitator or delivery format to be coded (k = 39). Potential interactions can be examined from the QBs for the interactions between number of recommendations and intervention characteristics in Tables 5 and 6, complemented by the QBs for the simple effects. To further test our hypothesis regarding the effects of intervention conditions likely to be associated with recipients with low motivation to change, following significant interactions, we conducted follow-up analyses indicated with subscripts in Tables 5 and 6. Generally the results from fixed- and random-effects models demonstrated a similar pattern, although there were fewer significant interactions in our random-effects models. Thus, we focus on the results from fixed-effects models, which are more powerful and produce narrow confidence intervals (Rosenthal, 1995; Wang & Bushman, 1999).
Table 5.
Overall Change as a Function of Number of Recommendations and Intervention Characteristics-Univariate Analyses (k = 231).
| Number of Recommendations |
||||||
|---|---|---|---|---|---|---|
| d | QB | |||||
|
|
||||||
| 1 | 2–3 | 4 or more | Simple Effects | Main Effect | Interaction | |
| Non-patient population | -- | -- | -- | -- | 65.92*** | 12.55** |
| Yes (k = 151) | 0.08a | 0.34b | 0.17c | 189.17*** | -- | -- |
| No (k = 80) | 0.41d | 0.46d | 0.27e | 50.46*** | -- | -- |
| Non-Clinic Setting | -- | -- | -- | -- | 56.57*** | 13.49** |
| Yes (k = 96) | 0.03a | 0.30b | 0.13a | 132.26*** | -- | -- |
| No (k = 134) | 0.29b | 0.37c | 0.26b | 51.17*** | -- | -- |
| Community Member | -- | -- | -- | -- | 73.56*** | 186.74*** |
| Yes (k = 73) | 0.01a | 0.37b | 0.05a | 397.23*** | -- | -- |
| No (k = 158) | 0.36b | 0.34b | 0.28c | 12.83*** | -- | -- |
| Group Delivery | -- | -- | -- | -- | 58.03*** | 42.15*** |
| Yes (k = 118) | 0.09a | 0.39b | 0.18c | 200.20*** | -- | -- |
| No (k = 113) | 0.42b | 0.41b | 0.31d | 40.38*** | -- | -- |
Note. Change for intervention groups as a function of number of recommendations and intervention characteristics. Passive control groups (d = 0.15) were excluded. d = fixed-effects weighted means. Following the means, we present the QBs for each intervention characteristic alone and in interaction with the number of recommendation. QB for simple and main effects = homogeneity coefficient for the difference across levels of a factor, distributed as a chi-square with degrees of freedom equal to the number of factor levels − 1 degrees of freedom. QB for interaction = homogeneity coefficient for the interaction between factors, distributed as a chi-square with (number of levels of factor A − 1) × (number of levels of factor B − 1) degrees of freedom. ds with similar subscripts are not significantly different from one another.
p < .05,
p < .01,
p < .001
Table 6.
Overall Change as a Function of Number of Recommendations and Intervention Characteristics-Multivariate Analyses (k = 231).
| Number of Recommendations |
||||||
|---|---|---|---|---|---|---|
| d | QB | |||||
|
|
||||||
| 1 | 2–3 | 4 or more | Simple Effects | Main Effect | Interaction | |
| Non-patient population | -- | -- | -- | -- | 13.43** | 20 24*** |
| Yes (k = 151) | 0.10a | 0.34b | 0.18c | 135.98*** | -- | -- |
| No (k = 80) | 0.32b | 0.47d | 0.18c | 99.71*** | -- | -- |
| Non-Clinic Setting | -- | -- | -- | -- | 0.30 | 0.71 |
| Yes (k = 134) | 0.23a | 0.38b | 0.16a | 104.78*** | -- | -- |
| No (k = 97) | 0.20a | 0.43b | 0.20a | 146.72*** | -- | -- |
| Community Member | -- | -- | -- | -- | 23.37*** | 164.20*** |
| Yes (k = 73) | 0.06a | 0.45b | 0.08a | 293.06*** | -- | -- |
| No (k = 158) | 0.36c | 0.36c | 0.28d | 20.83*** | -- | -- |
| Group Delivery | -- | -- | -- | -- | 0.03 | 3.22 |
| Yes (k = 118) | 0.22a | 0.40b | 0.16c | 149.80*** | -- | -- |
| No (k = 113) | 0.20a | 0.41b | 0.20a | 108.27*** | -- | -- |
Note. Change for intervention groups as a function of number of recommendations and intervention characteristics. Passive control groups (d = 0.15) were excluded. d = fixed-effects weighted means. Following the means, we present the QBs for each intervention characteristic alone and in interaction with the number of recommendation. QB for simple and main effects = homogeneity coefficient for the difference across levels of a factor, distributed as a chi-square with degrees of freedom equal to the number of factor levels − 1 degrees of freedom. QB for interaction = homogeneity coefficient for the interaction between factors, distributed as a chi-square with (number of levels of factor A − 1) × (number of levels of factor B − 1) degrees of freedom. ds with similar subscripts are not significantly different from one another.
p < .05,
p < .01,
p < .001
The results from our univariate analyses examining the effects of our hypothesized moderators are presented in Table 5, and the results from our multivariate analysis, which takes into account potential intercorrelations among predictors, are presented in Table 6.9, 10 Only the interactions for delivery to non-patient populations and the use of lay community facilitators remained significant in our multivariate analysis. In this model, interventions delivered to non-patient populations (fixed-effects QB = 13.43, p < .01, k = 231) and the use of lay community facilitators (fixed-effects QB = 23.37, p < .001, k = 231) were associated with significantly reduced effects. Importantly, delivery to non-patient populations interacted with number of recommendations to predict overall change, fixed-effects QB = 20.24, p < .001, k = 231. Examination of the QBs for the simple effects indicated that the curvilinear type of effect of number of recommendations was stronger when interventions were delivered to non-patient populations. Interventions delivered to non-patient populations were associated with significantly reduced effects when both a single or high number of behaviors were recommended, whereas interventions delivered to patient populations were only associated with reduced effects when a high number of behaviors were delivered.
Similarly, facilitator expertise interacted with number of recommendations to predict overall change, fixed-effects QB = 164.20, p < .001, k = 231. Interventions implemented by lay community facilitators were most effective when they recommended a moderate number of behaviors, and significantly reduced effects were observed when lay community members recommended a low or high number of recommendations. In contrast, as indicated by the QB for the simple effects, the effect of number of recommendations for interventions implemented by noncommunity members was weaker, presumably because these interventions are likely to be implemented to recipients with higher motivation to change. These analyses support the hypothesis that interventions implemented to recipients that likely have low motivation to change are associated with significantly reduced effects, unless the intervention is sufficiently motivating to compensate for their lower levels of motivation.
Exploratory Analyses
We also conducted exploratory analyses to determine other factors that influence intervention efficacy in interventions making multiple recommendations. The results from our fixed-effects analyses of the effects of various intervention characteristics are presented in Table 7. These analyses showed that interventions making multiple recommendations were more effective when they were passive (vs. active; d. = 0.33 vs. d. = 0.20) and were presented using face-to-face interactions (vs. other presentation methods; d. = 0.29 vs. d. = 0.14). Moreover, interventions recommending multiple behaviors were more effective when interventions were described as culturally appropriate (vs. not described as culturally appropriate; d. = 0.35 vs. d. = 0.25), and targeted to a specific gender (vs. not targeted; d. = 0.36 vs. d. = 0.23) or ethnic group (vs. not targeted; d. = 0.33 vs. d. = 0.24). These analyses imply that interventions recommending multiple behaviors that rely solely on strategies that involve minimal involvement from intervention recipients (e.g., attitudinal arguments, normative arguments, informational arguments) or that are presented using face-to-face interactions enhance the ability of intervention recipients to implement multiple recommended changes, possibly because these characteristics decrease the difficulty of implementing and receiving an already demanding multi-behavior intervention. Moreover, tailoring the intervention to a particular target audience also appears to effectively enhance the efficacy of multiple behavior domain interventions.
Table 7.
Overall Change as a Function of Intervention Characteristics (k = 216).
| d. | ||||
|---|---|---|---|---|
|
| ||||
| Yes | No | Fixed-effects QB | Random-effects QB | |
| Active intervention | 0.20 | 0.33 | 140.01*** | .34 |
| Face-to-face delivery | 0.29 | 0.14 | 330.60*** | 7.00* |
| Culturally appropriate intervention | 0.35 | 0.25 | 17.28*** | 3.44 |
| Intervention targeted to specific gender | 0.36 | 0.23 | 121.83*** | 6.50* |
| Intervention targeted to specific ethnic group | 0.33 | 0.24 | 12.24*** | 1.21 |
Note. d. = fixed-effects weighted means. No-intervention control groups (k = 39, d. = .06, confidence interval = −0.01, 0.12) and groups making a single recommendation (k = 15, d. = .07, confidence interval = 0.02, 0.13) were excluded. All factors were dummy coded (characteristic present = 1; characteristic not present = 0). QB = homogeneity coefficient for the difference across levels of a factor, distributed as a chi-square with degrees of freedom equal to the number of factor levels − 1.
p < .05,
p < .01,
p < .001
Assessment of Publication and Eligibility Biases
Our effect sizes are displayed in a funnel plot in Figure 2. As publication practices and eligibility criteria determine the sample of reports that are included in a meta-analysis, we estimated potential biases by examining the funnel plot of effect sizes. If the effect sizes are unbiased, the plot takes the form of a funnel centered on the mean effect size, with greater variability among effect sizes based on smaller sample sizes than larger ones. A distortion in the shape of the funnel is an indicator of the presence of publication bias. For example, if the true effect size is zero and there is bias, the funnel plot has a hollow in the middle. If the true effect size is not zero, the plot tends to be asymmetrical, having a large and empty section where the estimates from studies with small sample sizes and small effect sizes would otherwise be located. Following these guidelines, examination of the plot in Figure 2 suggests no publication or selection bias in our meta-analysis.
Figure 2.
Funnel plot for overall change. Four effects with extremely large sample sizes were excluded to make the shape of the plot more apparent. These large sample groups had average effect sizes.
Discussion
The purpose of this meta-analysis was to examine the potential mechanism that drives the impact of the included number of behavioral recommendations on intervention efficacy. We found that interventions were most effective when they made a moderate number of recommendations, providing evidence that more lifestyle recommendations do not always equal healthier outcomes. A moderate number of lifestyle recommendations appears to be beneficial because it is low enough to prevent the intervention from becoming excessively demanding, while being high enough to ensure the necessary level of motivation to implement the recommended changes. Importantly, samples with low motivation to change benefited greatly from interventions recommending a moderate number of recommendations, suggesting that these interventions may be motivating enough to prompt the desire to change in audiences who are currently unmotivated to change.
Overview of Findings
This is the first meta-analysis to thoroughly examine the mechanism that accounts for the effect of differing number of recommendations on behavioral and clinical change, and to examine whether this relation varies as a function of recipients' motivation to change. Specifically, interventions encouraging change in lifestyle behaviors were most effective when they made a moderate number of recommendations, and efficacy began to decline when interventions recommended a low or high number of behaviors. The increased efficacy of interventions recommending multiple behavior changes relative those recommending a single behavior is consistent with prior meta-analyses that have concluded that stronger improvements in health outcomes are associated with participation in interventions targeting multiple behavior domains (Conn et al., 2008; Ebrahim et al., 2011; Ketola et al., 2000; Spring et al., 2009). We also examined differences in the amount of change depending on whether behaviors were targeted by a behavioral recommendation, and our findings suggested that changes in one health behavior may not spontaneously lead to changes in other, untargeted health behaviors. In addition, we considered the possibility that our indicators of average change were not ideal to capture improvements in interventions making varying numbers of recommendations. We, therefore, conducted analyses in which outcome variables were computed by summing, rather than averaging, effect sizes. These analyses revealed a similar pattern of results in which interventions recommending a moderate number of behaviors were associated with greater efficacy, and strengthen our conclusion that interventions making a high number of recommendations are associated with reduced effects due to increased demand. We also found that the effect of number of recommendations varied as a function intervention duration, with interventions recommending a moderate number of behaviors being most effective when they were of average or longer duration.
Beyond demonstrating the possible mechanism that accounts for the impact of various numbers of recommendations, we were also interested in the possible mechanisms through which interventions promote change in clinical outcomes. We demonstrated that interventions recommending a moderate number of behaviors were associated with stronger improvements in behavioral outcomes, and that change in behavioral outcomes mediated the effects of number of recommended behaviors on clinical change. Thus, our findings help to determine how behavioral recommendations impact clinical outcomes, the majority which were measured objectively, and highlight the value of self-reported behavioral measures (Schroder, Carey, & Vanable, 2003; Newell, Girgis, Sanson-Fisher, & Savolainen, 1999).
Importantly, our findings demonstrated that the curvilinear type of effect of number of recommendations varied as a function of recipients' motivation to change. However, when multivariate analysis was used to control for other predictors, only the interactions for delivery to non-patient populations and the use of lay community facilitator remained significant. These findings suggest that when recipients have low motivation to change, the intervention had significantly reduced effects except when the intervention was sufficiently motivating to compensate for the lower motivation level of the sample. Consistent with our hypothesis, audiences that are reluctant to change (i.e., as indicated by delivery to non-patient populations or the use of lay community facilitators) appear to benefit from interventions recommending a moderate number of recommendations. Once the target audience has been decided, our findings can guide selection of the most appropriate number of behaviors to target for optimal impact. Specifically, our results suggest that interventionists aiming to motivate reluctant audiences are more likely to succeed if they recommend a moderate number of behaviors, as these interventions may be most engaging to those with low motivation.
Our results also suggest that interventions with less difficult delivery (i.e., passive interventions, face-to-face presentation) or interventions tailored to specific target audiences enhanced the efficacy of interventions recommending multiple behavior changes. The impact of these various intervention characteristics highlights the importance of carefully considering how decisions about intervention design influence recipients' ability to pay attention to the content of a behavioral intervention and the impact this may have on intervention efficacy. The effectiveness of any intervention is dependent on exposure to and understanding of the program (McGuire, 1968; see Albarracín, 2002; Albarracín & Vargas, 2010; Wyer & Albarracín, 2005 for recent treatments of this issue). Additional research is necessary to understand the mechanisms that make some intervention characteristics more or less effective in multiple behavior domain interventions.
Theoretical Implications of Our Findings
Our meta-analysis has major theoretical implications for the mechanisms underlying the efficacy of multiple behavior domain intervention programs. Given the growing interest in the development of effective multiple behavior domain interventions, developing a theory that can both explain the mechanisms of multiple behavior domain change and guide implementation is of critical importance (Nigg et al., 2002). Although up to this point the majority of theorizing about behavior change has focused on the modification of behaviors in a single domain, our work sought to determine the optimal number of behaviors to target in a lifestyle behavior change intervention and tested whether motivation to change may moderate this relation.
Implications of number of recommendations
We proposed and tested the idea that a moderate number of recommendations would be associated with increased intervention efficacy with the assumption that these interventions would be challenging enough to increase motivation, without increasing difficulty to the extent that the intervention becomes too demanding and effort to implement the recommended changes decreases. Although our findings are consistent with prior theorizing on attention and self-control processes, as well as energerization theory (Brehm et al., 1983; Brehm & Self, 1989; Wright, 1996) and Bandura's self-efficacy theory (1986, 1989, 1997), they represent the first meta-analytic demonstration of the effects of motivational processes on multiple behavior change.
Various processes may underlie the enhanced efficacy of interventions recommending a moderate number of behaviors. In particular, our findings are consistent with a systems approach to behavior and the notion that a change in determinants of one behavior can lead to changes in other associated behaviors (Albarracín et al., 2008; Albarracín, Hepler, & Tannenbaum, 2011; Albarracín, Wang, & Leeper, 2009; Brent, 1978; Ford & Lerner, 1992; von Bertalanffy, 1968). For example, experiencing success in modifying one health behavior may increase self-efficacy to implement advocated changes in other recommended behavior changes that intervention recipients previously perceived as insurmountable (Emmons, Marcus, Linnan, Rossi, & Abrams, 1994; Prochaska, Spring, & Nigg, 2008). Similarly, learning a skill in one domain may map out onto other domains targeted in a multiple behavior domain intervention, thereby increasing problem solving capacity across the board (Botvin & Griffin, 2004; Griffin, Botvin, & Nichols. 2006; Noar, Chabot, & Zimmerman, 2008). Future research should examine whether multiple behavior domain interventions affect potential mediators of behavior change in this manner.
Our findings also suggest that recipients may feel overwhelmed when interventions attempt to modify too many behaviors (Meichenbaum & Turk, 1987; Ornstein et al., 1993), and that, after a certain point, recommending more behaviors becomes problematic and does not lead to healthier outcomes. Additional gains likely do not occur when interventions include a high number of recommendations due to limits on cognitive capacity and self-control (Baumeister et al., 1994; Muraven & Slessareva, 2003) that restrict the ability of recipients to implement multiple recommended actions. Consistent with these possibilities, our results demonstrated that interventions may become too difficult when a high number of behaviors are recommended, possibly leading to the perception that the goals set by the intervention are unattainable (e.g., Bandura, 1986, 1989, 1997, 2004; Carver & Scheier, 1998; see Duval & Silvia, 2001 for review on the issue) and disengagement from the intervention.
Implications of the influence of motivation to change
We also examined the possibility that intervention conditions that are likely associated with delivery to samples with low motivation to change would be associated with reduced effects, unless the intervention was sufficiently motivating to increase motivation and compliance. Overall, we found evidence that interventions delivered to reluctant audiences were associated with significantly reduced intervention effects, but only when a single or high number of behaviors were recommended. Our findings are consistent with prior research that suggests that the effectiveness of interventions depends on the intervention recipients' stage of change (see Albarracín, 2002; Albarracín et al., 2005; Bandura, 1997; Catania, Kegeles, & Coates, 1990; Noguchi, Albarracín, Durantini, & Glasman, 2007; Prochaska, DiClemente, & Norcross, 1992; Prochaska, Redding, Harlow, Rossi, & Velicer, 1994). Importantly, the results of our meta-analysis suggested that recipients are sensitive to the content of the intervention and that when interventions with a moderate number of recommendations are delivered to samples with low motivation to change, these interventions may be efficacious.
Public Health Implications of Our Findings
This meta-analysis has relevance to the way multiple behavior domain interventions are designed and implemented. To begin with, although there are benefits to designing interventions that promote change across multiple domains, cognitive ability and outcome expectancies may place limits on the number of recommendations that can be successfully delivered and adopted. Readers may be interested in estimating how large a change in specific health outcomes might result from varying numbers of recommendations. To this end, we applied the average effect sizes for behavioral and clinical change presented in Table 3 to national averages of health statistics obtained from the National Health and Nutrition Examination Survey (National Center for Health Statistics, 2011). Given an average daily energy intake for men of 2110 kcal, a d. of 0.11 for single behavior interventions implies a 172.67 kcal reduction, a d. of 0.29 implies a 764.10 kcal reduction for interventions recommending a moderate number of behaviors, and a d. of 0.14 implies a 368.88 kcal reduction for interventions making a high number of recommendations. Results are similar when change in energy intake for females was considered (national average = 1,811 kcal), with estimated 154.69 kcal, 407.82 kcal, and 196.87 kcal reductions following participation in interventions recommending change in a single, moderate, and high number of behaviors, respectively. As the national average for cholesterol is 196 mg/dL, a d. of 0.12 for clinical change in single behavior interventions implies a 6.43 reduction in cholesterol, a d. of 0.27 implies a 14.46 mg/dL reduction in cholesterol when interventions recommend a moderate number of behaviors, and a d. of 0.22 implies a 11.78 mg/dL reduction in cholesterol for interventions the recommend change in a large number of behaviors. Similarly, as the national average for BMI for men is 28.6, estimated reductions in BMI of 1.17, 2.63, and 2.15 can be expected following participation in interventions recommending change in a single, moderate, and high number of recommendations, respectively. These estimated values demonstrate the benefit of recommending a moderate number of behaviors, and demonstrate that more lifestyle recommendations do not always result in healthier outcomes. A moderate number of recommendations may be associated with increased efficacy because these interventions are challenging enough to keep receipts interested and engaged, thereby ensuring the necessary level of motivation, while at the same time not being so challenging that recipients perceive the intervention as too difficult and reduce the amount of effort they put into reaching the health goals set by the health promotion program.
Our findings also indicate that once a sample with low motivation to change has been selected, unless appropriate decisions are made about the number of behaviors to recommend, interventions will be associated with reduced effects. However, our findings can help guide the design of the most appropriate intervention. First, particularly when interventions target change in samples with low motivation, the implementation of an intervention that recommends a moderate number of behaviors should be favored wherever possible. Second, samples with greater motivation to change also appear to benefit from interventions that recommend a moderate number of behaviors. However, as the curvilinear relation was weaker for samples with higher motivation, there may be greater flexibility in the selection of the optimal number of behaviors to target. That is, other relevant information could be used to decide the number of behaviors to target in interventions delivered to samples with higher motivation, such as the resources for intervention implementation, recipient factors (e.g., demographic characteristics), or the behaviors that are targeted in the intervention.
Duration of the intervention should be taken into account when selecting the number of recommendations to target. Interventions of average or longer duration were associated with greater improvements in health outcomes when a moderate number of recommendations were made. In contrast, it appears beneficial to recommend a single behavior in interventions of shorter duration. These findings suggest that it is unlikely that an intervention will succeed if adequate time is not provided to ensure that all components are implemented. In addition, given their overall greater efficacy, the best advice may be to design interventions that recommend a moderate number of behaviors that are of a sufficient duration to ensure success. The use of mobile technologies that can assist in intervention implementation may be one method for increasing the intensity of an intervention when resources to deliver an intervention with a high number of face-to-face interactions is lacking.
Limitations of This Meta-Analysis and Future Directions
The current meta-analysis has several limitations that are important to discuss. These limitations are related to coding for number of recommendations, inability to directly assess motivation to change, the correlational nature of the results, the validity of self-report measures, the inability to explore the content of the recommendations, and the generalizability of our findings.
Number of recommendations
We operationalized number of recommendations as the total number goals, or broad behavioral categories, targeted in an intervention. Although we coded for specific strategies discussed as means to reaching those goals, as well as the inclusion of biological methods, these were not included in our count of number of recommendations. Other options for coding the number of behavioral recommendations are of course possible. For example, all interventions involving behavioral-skills training by definition target multiple behaviors, and interventions targeting a single behavior domain, such as smoking cessation, likely include recommendations to assist recipients in quitting their smoking behavior (e.g., monitoring urges, coping with temptation). The challenge of operationalizing number of recommendations is further complicated by the fact that papers vary in the extent to which interventions are described in detail. Coding number of recommendations by counting only primary goals set by the intervention likely resulted in a more consistent coding of number of recommendations across studies. At a minimum, papers likely report the primary goals of an intervention, whereas specific details on the strategies recommended to assist intervention recipients in modifying the recommended behaviors may vary greatly across papers. Nonetheless, it is important to acknowledge that interventions often recommend a number of strategies as a means to reach the primary goals set by the intervention. Future research should examine whether the curvilinear relation between number of recommendations and intervention efficacy replicates using more precise methods of counting behavioral recommendations.
Motivation to change
In this meta-analysis we assumed that specific intervention conditions (e.g., the use of lay community facilitators, delivery to non-patients populations) would be associated with intervention delivery to samples with low motivation to change. Unfortunately, because the research included in our meta-analysis did not measure motivation, it was not possible to verify whether our hypothesized moderators were indeed associated with lower initial levels of motivation to change. In the future, research should include measures of motivation to better understand the mechanism through which recommendations influence intervention efficacy. Moreover, future research should consider whether other aspects of multiple behavior domain interventions, such as the strategies used to promote behavior change, can increase motivation, and ultimately behavioral and clinical change, among samples with low motivation. Given disparities associated with many health conditions, future research must further examine the reduced efficacy of interventions delivered by lay community facilitators, which are commonly used in the delivery of interventions to marginalized groups. Interventions delivered by lay community facilitators cover a broad range of interventions that differ in terms of the level of training provided, the responsibility and latitude of facilitators in intervention delivery, and the extent to which implementation is monitored (Glenton et al., 2013; Nies et al., 2004). Closer examination of these various factors may increase our understanding of factors associated with the increased success of interventions implemented by lay community facilitators.
Intervention complexity
Up to this point, research examining the effect of the included number of recommendations on intervention efficacy has been limited. Determining the optimal number of behaviors to target became the focus of our meta-analysis, and our findings contribute broadly to our understanding of multiple behavior domain change. However, multiple behavior domain interventions are by their very nature complex interventions that seek to modify an important set of health behaviors in several different domains (Goldstein et al., 2004; Nigg et al., 2002; Nigg & Long, 2012; Prochaska et al., 2010). Evidence suggests that combining different types of behavioral recommendations impacts intervention efficacy. For example, there is evidence that reducing a behavior that acts as a barrier to a consequent behavior promotes the consequent behavior (e.g., reducing substance use influences medication adherence; Ingersoll et al., 2011; Parson, Golub, Rosof, & Holder, 2007). However, one important question for future research is whether the effect of number of recommendations varies across interventions targeting different combinations of behavioral domains (e.g., interventions targeting diet and exercise vs. interventions targeting diet and smoking), as well as interventions within a single domain. The behavior domains combined in an intervention will impact the outcomes used to assess the intervention and the strategies used to modify health behaviors, as well as other factors related to participant characteristics and the setting of delivery. Given the differences that exist between intervention recommending different combinations of behaviors, it will be important to determine whether the curvilinear pattern of number of recommendations replicates for interventions targeting different combinations of health behaviors.
Correlational nature of our results
As noted, a limitation of this meta-analysis is the correlational nature of the analyses we reported. Assignment to intervention and control groups in the papers we included was often conducted at random. However, the specific characteristics of an intervention and the participants particular researchers chose to study are subject to their preferences and may covary with other study characteristics. Although the various controls included in our models help to rule out spurious findings, other co-associations cannot be completely ruled out. When all is said and done, however, our conclusions represent important insights into the effectiveness of multiple behavior domain interventions, and fill important gaps in our knowledge of multiple behavior change processes.
Inaccuracy of self-report
Another limitation of this meta-analysis is related to potential inaccuracies in self-reported behavior. Various factors are known to influence the accuracy of self-report data, including (a) the length of the time interval respondents are asked to recall behaviors (Newell et al., 1999; Schroeder et al., 2003), (b) lack of knowledge to answer questions correctly (Newell et al., 1999), and (c) demand characteristics inherent in survey situations (Beach & Mayer, 1990; Furnham, 1986). Although prior research calls into question the accuracy of self-report data, it is important to note that many of the studies included in our meta-analysis reported data on objectively measured clinical biomarkers, as well as self-reported behavioral outcomes. Importantly, the convergence between our findings about the effect of number of recommendations on behavioral and clinical biomarker change and our finding that behavioral change mediated clinical change suggest that our findings reflect more than self-report bias.
Content of recommendation
Unfortunately, we could not examine how specific recommendation content, such as the framing of the recommendation, influenced change in health outcomes because few papers provided such detailed descriptions of behavioral recommendations. Gain framed messages emphasize the benefits of engaging in a behavior, whereas loss framed messages highlight the consequences of failing to engage in a behavior. Prior research has indicated that loss-framed messages most effectively promote detection behaviors (e.g., mammography), and that gain-framed messages more effectively promote prevention behaviors (e.g., physical activity; Banks et al., 1995; Latimer et al., 2008; Rothman & Salovey, 1997; Rothman, Salovey, Antone, Keough, & Martin, 1993). Given the effects that framing of recommendations can have on health decisions, we hope it will be possible to examine the influence of message framing in multiple behavior domain interventions in the future.
Potential sleeper effects
Although an important objective of this meta-analysis was to examine factors that influence the efficacy of multiple behavior domain intervention, we only considered outcomes at the immediate follow-up point. Future research should examine the possibility of sleeper effects (see Kumkale & Albarracín, 2004), given that some outcomes may change over longer periods of time. For example, more resource demanding interventions may be overwhelming in the beginning but become more effective over time. Understanding such long-term effects will be important to develop a more comprehensive understanding of the mechanisms whereby multiple behavior interventions exert their effects.
Generalizability to the study sample and to the population of all possible studies
Our paper presents the largest meta-analysis of interventions promoting change in multiple lifestyle behaviors. As such, our findings are likely to be most generalizable to date. In particular, the mean comparisons suggest that interventions are most effective when they attempt to modify a moderate number of behaviors. Moreover, our findings suggest that the curvilinear relation becomes stronger when intervention characteristics increase difficulty of intervention delivery and processing. However, our findings for the effects of intervention characteristics were obtained with fixed-effects models. Although the pattern of findings presented in Table 5 and 6 replicated using random-effects models, the number of significant effects declined. In the future, a meta-analysis with a sufficiently large number of effect sizes may allow for the estimation of population variance and establish the tenability of the findings in the broader universe of all possible studies.
Closing note
Our meta-analysis clearly shows that decisions about the number of recommendations to include in an intervention have important implications for intervention efficacy. We demonstrated that intervention outcomes were maximized when a moderate number of lifestyle behaviors were recommended, suggesting this amount is low enough to prevent a reduction in cognitive ability while being high enough to ensure the necessary level of motivation to maximize behavioral and clinical change. Our findings are consistent with various motivational models (Bandura, 1986, 1989, 1997; Brehm & Self, 1989; Brehm et al., 1983), and suggest that recommending a moderate number of behaviors is associated with stronger improvements because these interventions are challenging and motivating without becoming overwhelming, and potentially reducing the amount of effort recipients' put forth to implementing the recommended changes. Our findings also suggest that decisions about the number of behaviors to target has important consequences for the efficacy of behavior change interventions for reluctant audiences, such that recommending a moderate number of behaviors appears particularly beneficial when intervention recipients have low motivation to change. We hope that the results from this work will contribute to the development of a theory of multiple behavior domain change and provide guidelines for intervention implementation to make multiple behavior domain change programs more effective.
Acknowledgments
This research was supported by Grants R01 MH094241 (Dolores Albarracin) and HL075451 (Bonnie Spring) from the National Institutes of Health.
Footnotes
Perceived similarity between facilitators and recipients is orthogonal to expertise and contributes favorably to efficacy (Durantini et al., 2006). Perceived similarity was not examined in the current meta-analysis.
It was not possible to examine targeted vs. untargeted change interventions making multiple recommendations as all measures were targeted by the recommendations included in the intervention.
When ethnicity data were not reported and countries were highly ethnically homogeneous (e.g., the Netherlands, Italy), we obtained the information from population reports from those countries.
When the N at the pretest differed from the N at the posttest, the smaller N was used.
The distribution of weights was skewed due to sixteen cases with large weights. To correct for this, we curved weights over 999 to fit between the range of 1,000–2,000. Because results were similar regardless of whether we used the original or curved weights, we present only results from analyses using the curved weights.
Data set refers to the number of conditions that each paper contributed to the final database.
We analyzed whether differences existed in the efficacy of interventions we coded as making a moderate number of recommendations. Our analyses revealed that there was not a significant difference in overall (QB = 0.25, p > .05, k = 110), behavioral (QB = 0.01, p > .05, k = 76), or clinical (QB = 2.67, p > .05, k = 78) change for interventions making two versus three behavioral recommendations.
Due to the small number of cases that assessed clinical outcomes using self-report measures (k = 7), it was not possible to determine if the effect of number of recommendations differed depending upon whether clinical outcomes were measured objectively. When we removed cases where clinical outcomes relied on self-report from our analysis, the overall pattern of results remained the same (QB = 32.63, p < .05, k = 192). Because results were similar, we retained these cases in our analyses.
We analyzed whether professional expertise moderated the influence of numbers of recommendations on overall change. Our results replicated and the interaction between number of recommendations and expertise was significant, Fixed effects QB = 276.25, p < .001, k = 231.
We analyzed whether the use of individual delivery formats moderated the influence of numbers of recommendations on overall change. Our results replicated and the interaction between number of recommendations and expertise was significant, Fixed effects QB = 40.86, p < .001, k = 231.
References
References marked with an asterisk indicate studies included in the meta-analysis. The in-text citations to studies selected for meta-analysis are not preceded by asterisks.
- Aguiar EJ, Morgan PJ, Collins CE, Plotnikoff R, Callister R. Efficacy of interventions that include diet, aerobic and resistance training components for type 2 diabetes prevention: A systematic review with meta-analysis. The International Journal of Behavioral Nutrition and Physical Acitivity. 2014;11:2. doi: 10.1186/1479-5868-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracín D. Cognition in persuasion: An analysis of information processing in response to persuasive communications. In: Zanna MP, editor. Advances in experimental social psychology. Vol. 34. Academic Press; San Diego, CA: 2002. pp. 61–130. [Google Scholar]
- Albarracín D, Gillette J, Earl A, Glasman LR, Durantini MR, Ho MH. A test of major assumptions about behavior change: A comprehensive look at HIV prevention interventions since the beginning of the epidemic. Psychological Bulletin. 2005;131:856–897. doi: 10.1037/0033-2909.131.6.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracín D, Handley IM, Noguchi K, McCulloch KC, Li H, Leeper J, Earl A. Increasing and decreasing motor and cognitive output: A model of general action and inaction goals. Journal of Personality and Social Psychology. 2008;95:510–523. doi: 10.1037/a0012833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracín D, Hepler JJ, Tannenbaum MB. General action and inaction goals: Their behavioral, cognitive, and affective origins and influences. Current Directions in Psychological Science. 2011;20:119–123. doi: 10.1177/0963721411402666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracín D, Vargas P. Attitude formation and change: From biology to social responses to persuasion intent. In: Fiske S, Gilbert D, editors. Handbook of Social Psychology. 5th ed John Wiley & Sons, Inc; Hoboken, NJ: 2010. pp. 394–427. [Google Scholar]
- Albarracín D, Wang W, Leeper J. Immediate increase in food intake following exercise messages. Obesity. 2009;17:1451–1452. doi: 10.1038/oby.2009.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albrecht A, Marcus B, Roberts M, Forman D, Parisi A. Effect of smoking cessation on exercise performance in female smokers participating in exercise training. American Journal of Cardiology. 1998;82:950–95. doi: 10.1016/s0002-9149(98)00511-6. [DOI] [PubMed] [Google Scholar]
- Allen J, Blumenthal R, Margolis S, Young D, Miller E, Kelly K. Nurse case management of hypercholesterolemia in patients with coronary heart disease: Results of a randomized clinical trial. American Heart Journal. 2002;144:678–86. doi: 10.1067/mhj.2002.124837. [DOI] [PubMed] [Google Scholar]
- Ammerman AS, Lindquist CH, Lohr KN, Hersey J. The efficacy of behavioral interventions to modify dietary fat and fruit and vegetable intake: A review of the evidence. Preventive Medicine. 2002;35:25–41. doi: 10.1006/pmed.2002.1028. [DOI] [PubMed] [Google Scholar]
- Anderson D, Mizzari K, Kain V. The effects of a multimodal intervention trial to promote lifestyle factors associated with the prevention of cardiovascular disease in menopausal and postmenopausal Australian women. Health Care for Women International. 2006;27:238–253. doi: 10.1080/07399330500506543. [DOI] [PubMed] [Google Scholar]
- Atlantis E, Chow C, Kirby A, Singh M. Worksite intervention effects on physical health: A randomized controlled trial. Health Promotion International. 2006;21:191–200. doi: 10.1093/heapro/dal012. [DOI] [PubMed] [Google Scholar]
- Auer R, Gaume J, Rodondi N, Cornuz J, Ghali WA. Efficacy of in-hospital multidimensional interventions of secondary prevention after acute coronary syndrome: A systematic review and meta-analysis. Preventive Cardiology. 2008;117:3109–3117. doi: 10.1161/CIRCULATIONAHA.107.748095. [DOI] [PubMed] [Google Scholar]
- Ayala GX. An experimental evaluation of group versus computer-based intervention to improve food portion size estimation skills. Health Education Research. 2006;21:1133–145. doi: 10.1093/her/cyh049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babamoto K, Sew K, Camilleri A, Karlan V, Catalasan J, Morisky D. Improving diabetes care and health measures among Hispanics using community health workers; Results from a randomized controlled trial. Health Education & Behavior. 2009;36:113–126. doi: 10.1177/1090198108325911. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Prentice Hall. Bandura; Englewood Cliffs, NJ: 1986. 1997. [Google Scholar]
- Bandura A. Perceived self-efficacy in the exercise of control over AIDS infection. In: Mayes VM, Albee GW, Schneider SF, editors. Primary prevention of AIDS: Psychological approaches. Sage; London: 1989. pp. 128–141. [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. Freeman; New York: 1997. [Google Scholar]
- Badura A. Health promotion by social cognitive means. Health Education & Behavior. 2004;31:143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Banks SM, Salovey P, Greener S, Rothman AJ, Moyer A, Beauvais J, Epel E. The effects of message framing on mammography utilization. Health Psychology. 1995;14:178–184. doi: 10.1037//0278-6133.14.2.178. [DOI] [PubMed] [Google Scholar]
- Baranowski T, Baranowski J, Cullen K, Thompson DI, Nicklas T, Zakeri IF, Rochon J. The fun, food, and fitness project (FFFP): The Baylor Gems Pilot Study. Ethnicity and Disease. 2003;13(Supplement 1):30–39. [PubMed] [Google Scholar]
- Bauer RL, Heller RF, Challah S. United Kingdom heart disease prevention project: 12-year follow-up of risk factors. American Journal of Epidemiology. 1985;121:563–569. doi: 10.1093/oxfordjournals.aje.a114034. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, Heatherton TF. Self-regulation failure: An overview. Psychological Inquiry. 1996;7:1–15. [Google Scholar]
- Baumeister RF, Heatherton TF, Tice DM. Losing control: How and why people fail at self-regulation. Academic Press; San Diego, California: 1994. [Google Scholar]
- Bayne-Smith M, Fardy PS, Azzollini A, Magel J, Schmitz KH, Agin D. Improvements in heart health behaviors and reduction in coronary artery disease risk factors in urban teenaged girls through a school-based intervention: The PATH program. American Journal of Public Health. 2004;94:1538–1543. doi: 10.2105/ajph.94.9.1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach DL, Mayer JA. The effects of social demand on breast self-examination self- report. Journal of Behavioral Medicine. 1990;13:195–205. doi: 10.1007/BF00844999. [DOI] [PubMed] [Google Scholar]
- Beck C, Fausett JK, Krukowski RA, Cornell CE, Prewitt TE, Lensing S, West DS. A randomized trial of a community-based cognitive intervention for obese senior adults. Journal of Aging and Health. 2013;25(1):97–118. doi: 10.1177/0898264312467374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker BJ. Synthesizing standardized mean-change measures. British Journal of Mathematical & Statistical Psychology. 1988;41:257–278. [Google Scholar]
- Becker DM, Yanek LR, Johnson WR, Garret D, Moy TF, Reynolds SS, Becker LC. Impact of a community-based multiple risk factor intervention on cardiovascular risk in black families with a history of premature coronary disease. Circulation. 2005;111:1298–1304. doi: 10.1161/01.CIR.0000157734.97351.B2. [DOI] [PubMed] [Google Scholar]
- Benedict MA, Arterburn D. Worksite-based weight loss programs: A systematic review of recent literature. American Journal of Health Promotion. 2008;22:408–416. doi: 10.4278/ajhp.22.6.408. [DOI] [PubMed] [Google Scholar]
- Bennett G, Herring S, Puleo E, Stein E, Emmons K, Gillman M. Web-based weight loss in primary care: A randomized controlled trial. Obesity. 2010;18:308–313. doi: 10.1038/oby.2009.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrelli B, Mermelstein R. The role of weight concern and self-efficacy in smoking cessation and weight gain among smokers in a clinic-based cessation program. Addictive Behaviors. 1998;23:609–622. doi: 10.1016/s0306-4603(98)00014-8. [DOI] [PubMed] [Google Scholar]
- Boulware LE, Gaumit GL, Frick KD, Minkovitz CS, Lawrence RS, Powe MR. An evidence based review of patient-centered behavioural interventions for hypertension. American Journal of Preventive Medicine. 2001;21:221–232. doi: 10.1016/s0749-3797(01)00356-7. [DOI] [PubMed] [Google Scholar]
- Botvin GJ, Griffin KW. Life skills training: Empirical findings and future directions. Journal of Primary Prevention. 2004;25:211–232. [Google Scholar]
- Brehm JW, Self E. The intensity of motivation. Annual Review of Psychology. 1989;40:109–131. doi: 10.1146/annurev.ps.40.020189.000545. [DOI] [PubMed] [Google Scholar]
- Brehm JW, Wright RA, Solomon S, Silka L, Greenberg J. Perceived difficulty, energization, and the magnitude of goal valence. Journal of Experimental Social Psychology. 1983;19:21–48. [Google Scholar]
- Broadhurst PL. The interaction of task difficulty and motivation: The Yerkes-Dodson law revived. Acta Psychologica. 1959;16:321–338. [Google Scholar]
- Brent SP. Prigogine's model for self-organization in non-equilibrium systems: Its relevance for developmental psychology. Human Development. 1978;21:374–387. [Google Scholar]
- Bruckert E, Giral P, Paillard F, Ferrieres J, Schlienger JL, Renucci JF, Chadarevian R, on behalf of the PEGASE group Effect of an educational program (PEGASE) on cardiovascular risk in hypercholesterolaemic patients. Cardiovascular Drug Therapy. 2008;22:495–505. doi: 10.1007/s10557-008-6137-4. [DOI] [PubMed] [Google Scholar]
- Burke V, Beilin L, Cutt HE, Mansour J, Mori T. Moderators and mediators of behaviour change in a lifestyle program for treated hypertensives: A randomized controlled trial (ADAPT) Health Education Research. 2008;23:583–591. doi: 10.1093/her/cym047. [DOI] [PubMed] [Google Scholar]
- Burke V, Beilin LJ, Cutt HE, Mansour J, Williams A, Mori TA. A lifestyle program for treated hypertensives improved health-related behaviors and cardiovascular risk factors: A randomized controlled trial. Journal of Clinical Epidemiology. 2007;60:133–141. doi: 10.1016/j.jclinepi.2006.05.012. [DOI] [PubMed] [Google Scholar]
- Burke V, Beilin LJ, Cutt HE, Mansour J, Wilson A, Mori TA. Effects of a lifestyle programme on ambulatory blood pressure and drug dosage in treated hypertensive patients: A randomized controlled trial. Journal of Hypertension. 2005;23:1241–1249. doi: 10.1097/01.hjh.0000170388.61579.4f. [DOI] [PubMed] [Google Scholar]
- Burke V, Giangiulio N, Gillam HF, Beilin LJ, Houghton S, Milligan RAK. Health promotion in couples adapting to a shared lifestyle. Health Education Research. 1999;14:269–288. doi: 10.1093/her/14.2.269. [DOI] [PubMed] [Google Scholar]
- Cakir H, Pinar R. Randomized controlled trial on lifestyle modification in hypertensive patients. Western Journal of Nursing Research. 2006;28:190–209. doi: 10.1177/0193945905283367. [DOI] [PubMed] [Google Scholar]
- Cambien F, Richard JL, Ducimetiere P, Warnet JM, Kahn J. The Paris cardiovascular risk factor prevention trial: Effects of two years of intervention in a population of young men. Journal of Epidemiology & Community Health. 1981;35:91–97. doi: 10.1136/jech.35.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell MK, Tessaro I, DeVellis B, Benedict S, Kelsey K, Belton L, Sanhueza A. Effects of a tailored health promotion program for female blue-collar workers: Health works for women. Preventive Medicine. 2002;34:313–323. doi: 10.1006/pmed.2001.0988. [DOI] [PubMed] [Google Scholar]
- Campbell NC, Ritchie LD, Thain J, Deans HG, Rawles JM, Squair JL. Secondary prevention in coronary heart disease: A randomized trial of nurse led clinics in primary care. Heart. 1998;80:447–452. doi: 10.1136/hrt.80.5.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, Scheier MF. On the self-regulation of behavior. Cambridge University Press; New York: 1998. [Google Scholar]
- Catania JA, Kegeles SM, Coates TJ. Towards an understanding of risk behavior: An AIDS risk reduction model (ARRM) Health Education Quarterly. 1990;17:53–72. doi: 10.1177/109019819001700107. [DOI] [PubMed] [Google Scholar]
- Christian J, Bessesen D, Byers T, Christian K, Goldstein M, Bock B. Clinic-based support to help overweight patients with type 2 diabetes increase physical activity and lose weight. Archives of Internal Medicine. 2008;168:141–146. doi: 10.1001/archinternmed.2007.13. [DOI] [PubMed] [Google Scholar]
- Clements L, Buczkiewicz M. Approaches to peer led health education: A guide for youth workers. Health Education Authority; London: 1993. [Google Scholar]
- Conn VS, Hafdahl AR, LeMaster JW, Ruppar TM, Cochran JE, Nielsen PJ. Meta-analysis of health behavior change interventions in Type 1 Diabetes. American Journal of Health Behavior. 2008;32:315–329. doi: 10.5555/ajhb.2008.32.3.315. [DOI] [PubMed] [Google Scholar]
- Contrada RJ, Glass DC, Krakoff LR, Krantz DS, Kehoe K, Isecke W, Collins C, Elting E. Effects of control over aversivc stimulation and Type A behavior on cardiovascular and plasma catecholamine responses. Psychophysiology. 1982;19:408–419. doi: 10.1111/j.1469-8986.1982.tb02496.x. [DOI] [PubMed] [Google Scholar]
- Corabian P, Harstall C. Patient diabetes education in the management of adult type-2 diabetes. Alberta Heritage Foundation for Medical Research; Edmonton, Alberta, Canada: 2001. [Google Scholar]
- Cupples ME, McKnight A. Randomized controlled trial of health promotion in general practice for patients at high cardiovascular risk. British Medical Journal. 1994;309:993–996. doi: 10.1136/bmj.309.6960.993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasgupta K, Grover S, Da Costa D, Lowensteyn I, Yale JF, Rahme E. Impact of modified glucose target and exercise interventions on vascular risk factors. Diabetes Research and Clinical Practice. 2006;72:53–60. doi: 10.1016/j.diabres.2005.09.010. [DOI] [PubMed] [Google Scholar]
- Davies MJ, Heller S, Skinner TC, Campbell MJ, Carey ME, Cradock S, Khunti K. Effectiveness of the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: Cluster randomised controlled trial. BMJ: British Medical Journal. 2008;336:491. doi: 10.1136/bmj.39474.922025.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deakin T, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database of Systematic Reviews (CD003417) 2005 doi: 10.1002/14651858.CD003417.pub2. Retrieved from http://proxy.library.upenn.edu:2170/doi/10.1002/14651858.CD003417.pub2/pdf. [DOI] [PubMed]
- DeBar L, Ritenbaugh C, Aickin M, Orwoll E, Elliot D, Dickerson J, Irving LM. A health plan-based lifestyle intervention increases bone mineral density in adolescent girls. Archives of Pediatrics and Adolescent Medicine. 2006;160:1269–1277. doi: 10.1001/archpedi.160.12.1269. [DOI] [PubMed] [Google Scholar]
- DeBusk R, Houston-Miller N, Superko R, Dennis C, Thomas RJ, Lew HT, Taylor CB. A case-management system for coronary risk factor modification after acute myocardial infarction. Annals of Internal Medicine. 1994;120:721–729. doi: 10.7326/0003-4819-120-9-199405010-00001. [DOI] [PubMed] [Google Scholar]
- Deering KN, Shannon K, Sinclair H, Parsad D, Gilbert E, Tyndall MW. Piloting a peer-driven intervention model to increase access and adherence to ART and HIV care among street-entrenched HIV-positive women in Vancouver. AIDS Patient Care STDs. 2009;23:603–609. doi: 10.1089/apc.2009.0022. [DOI] [PubMed] [Google Scholar]
- Delaney EK, Murchie P, Lee AJ, Ritchie LD, Campbell NC. Secondary prevention clinics for coronary heart disease: A 10-year follow-up of a randomized controlled trial in primary care. Heart. 2008;94:1419–1423. doi: 10.1136/hrt.2007.126144. [DOI] [PubMed] [Google Scholar]
- de Vries H, Kremers SPJ, Smeets T, Brug J, Eijmael K. The effectiveness of tailored feedback and action plans in an intervention addressing multiple health behaviors. American Journal of Health Promotion. 2008;22:417–425. doi: 10.4278/ajhp.22.6.417. [DOI] [PubMed] [Google Scholar]
- Diabetes Prevention Program Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or Metformin. New England Journal of Medicine. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dove J. Effects of a multi-component school-based intervention on health markers, body composition, physical fitness, and psychological measures in overweight and obese adolescent females. Dissertation Abstracts International. 2010;69:2620. UMI No. 3316066. [Google Scholar]
- Doyle A, Goldschmidt A, Huang C, Winzelberg AJ, Taylor CB, Wilfley DE. Reduction of overweight and eating disorder symptoms via the internet in adolescents: A randomized controlled trial. Journal of Adolescent Health. 2008;43:172–179. doi: 10.1016/j.jadohealth.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duff E, Simpson SH, Whittle S, Bailey EY, López SA, Wilks R. Impact on blood pressure control of a six-month intervention project. West Indian Medical Journal. 2000;49:307–311. [PubMed] [Google Scholar]
- Durantini MR, Albarracín D, Mitchell AL, Earl AN, Gillette JC. Conceptualizing the influence of social agents of behavior change: A meta-analysis of the effectiveness of HIV-prevention interventionists for different groups. Psychological Bulletin. 2006;132:212–248. doi: 10.1037/0033-2909.132.2.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duval TS, Silvia PJ. Self-awareness, probability of improvement, and the self-serving bias. Journal of Personality and Social Psychology. 2002;82:49–61. doi: 10.1037//0022-3514.82.1.49. [DOI] [PubMed] [Google Scholar]
- Ebrahim S, Taylor F, Ward K, Beswick A, Burke M, Davey Smith G. Multiple risk factor interventions for primary prevention of coronary heart disease. Cochrane Database of Systematic Reviews. 2011;1 doi: 10.1002/14651858.CD001561.pub3. CD001561.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elmer P, Obarzanek E, Vollmer W, Simons-Morton D, Stevens VJ, Young DR, Apple LJ. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Annals of Internal Medicine. 2006;144:485–495. doi: 10.7326/0003-4819-144-7-200604040-00007. [DOI] [PubMed] [Google Scholar]
- Emmons KM. Behavioral and social science contributions to the health of adults in the United States. In: Smedley BD, Syme SL, editors. Promoting health: Intervention strategies from social and behavioral research. National Academy Press; Washington, DC: 2001. pp. 254–231. [Google Scholar]
- Emmons KM, Marcus BH, Linnan L, Rossi JS, Abrams DB. Mechanisms in multiple risk factor interventions: Smoking, physical activity, and dietary fat intake among manufacturing workers. Preventive Medicine. 1994;23:481–489. doi: 10.1006/pmed.1994.1066. [DOI] [PubMed] [Google Scholar]
- Enders C, Bandalos D. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling. 2001;8:430–457. [Google Scholar]
- Enriquez M, Farnan R, Neville S. What experienced HIV-infected lay peer educators working in midwestern U.S. HIV medical care settings think about their role and contributions to patient care. AIDS Patient Care and STDs. 2013;27:474–480. doi: 10.1089/apc.2013.0021. [DOI] [PubMed] [Google Scholar]
- Erfurt JC, Foote A, Heirich MA. Worksite wellness programs: Incremental comparison of screening and referral alone, health education, follow-up counseling, and plant organization. American Journal of Health Promotion. 1991;5:438–448. doi: 10.4278/0890-1171-5.6.438. [DOI] [PubMed] [Google Scholar]
- Estabrooks PA, Smith-Ray RL. Piloting a behavioral intervention delivered through interactive voice response telephone messages to promote weight loss in a pre-diabetic population. Patient Education and Counseling. 2008;72:34–41. doi: 10.1016/j.pec.2008.01.007. [DOI] [PubMed] [Google Scholar]
- Ferré R, Plana N, Merino J, Aragonés G, Girona J, Heras M, Masana L. Effects of therapeutic lifestyle changes on peripheral artery tonometry in patients with abdominal obesity. Nutrition, Metabolism & Cardiovascular Diseases. 2010;22:95–102. doi: 10.1016/j.numecd.2010.04.008. [DOI] [PubMed] [Google Scholar]
- Fine LJ, Philogene GS, Gramling R, Coups EJ, Sinha S. Prevalence of multiple chronic disease risk factors: 2001 national health interview survey. American Journal of Preventive Medicine. 2004;27:18–24. doi: 10.1016/j.amepre.2004.04.017. [DOI] [PubMed] [Google Scholar]
- Fogelholm M, Kukkonen-Harjula K, Nenonen A, Pasanen M. Effects of walking training on weight maintenance after a very-low-energy diet in pre-menopausal obese women. Archives of Internal Medicine. 2000;40:2177–2184. doi: 10.1001/archinte.160.14.2177. [DOI] [PubMed] [Google Scholar]
- Ford DH, Lerner RM. Developmental systems theory: An integrative approach. Sage; Newbury Park, CA: 1992. [Google Scholar]
- Fouad M, Kiefe C, Bartolucci A, Burst N, Ulene V, Harvey M. A hypertension control program tailored to unskilled and minority workers. Ethnicity & Disease. 1997;7:191–199. [PubMed] [Google Scholar]
- Frank E, Elon L, Hertzberg V. A quantitative assessment of a 4-year intervention that improved patient counseling through improving medical student health. Medscape General Medicine. 2007;9:58. [PMC free article] [PubMed] [Google Scholar]
- Friedman DB, Williams AN, Levine BD. Compliance and efficacy of cardiac rehabilitation and risk factor modification in the medically indigent. The American Journal of Cardiology. 1997;79:281–285. doi: 10.1016/s0002-9149(96)00748-5. [DOI] [PubMed] [Google Scholar]
- Furnham A. Response bias, social desirability and dissimulation. Personality and Individual Differences. 1986;7:385–400. [Google Scholar]
- Gabriele J. Effects of nondirective and directive support on weight loss in an e-counseling intervention. 2008. Retrieved from Dissertation Abstracts International. (UMI No. 3332093) [Google Scholar]
- Gaede P, Beck M, Vedel P, Pedersen O. Limited impact of lifestyle education in patients with Type 2 diabetes mellitus and microalbuminuria: Results from a randomized intervention study. Diabetic Medicine. 2001;18:104–108. doi: 10.1046/j.1464-5491.2001.00444.x. [DOI] [PubMed] [Google Scholar]
- Geliebter A, Maher M, Gerace L, Gutin B, Heymsfield S, Hashim S. Effects of strength or aerobic training on body composition, resting metabolic rate, and peak oxygen consumption in obese dieting subjects. American Journal of Clinical Nutrition. 1997;66:557–563. doi: 10.1093/ajcn/66.3.557. [DOI] [PubMed] [Google Scholar]
- Giannuzzi P, Temporelli P, Marchioli R, Maggioni AP, Balestroni G, Ceci V, Vanuzzo D. Global secondary prevention strategies to limit event recurrence after myocardial infarction. Archives of Internal Medicine. 2008;168:2194–2204. doi: 10.1001/archinte.168.20.2194. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Toobert DJ, Hampson SE, Brown JE, Lewinsohn PM, Donnelly J. Improving self-care among older patients with the Type II diabetes: The “sixty something……” study. Patient Education & Counseling. 1992;19:61–74. doi: 10.1016/0738-3991(92)90102-o. [DOI] [PubMed] [Google Scholar]
- Glenton C, Colvin CJ, Carlsen B, Swartz A, Lewin S, oyes J, Rasidian A. Barriers and facilitators to the implementation of lay health worker programmes to improve maternal and child health: Qualitative evidence synthesis (Review) Cochrane Database of Systematic Reviews. 2013;10 doi: 10.1002/14651858.CD010414.pub2. CD010414.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goetzel R, Baker K, Short ME, Pei X, Ozminkowski RJ, Wang S, Wilson MG. First year results of an obesity prevention program at the Dow Chemical Company. Journal of Occupational and Environmental Medicine. 2009;51:125–138. doi: 10.1097/JOM.0b013e3181954b03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein MG, Whitlock EP, DePue J. Multiple behavior risk factor interventions in primary care: Summary of research evidence. American Jounral of Preventive Medicine. 2004;27:61–79. doi: 10.1016/j.amepre.2004.04.023. [DOI] [PubMed] [Google Scholar]
- Goodman RM, Wheeler FC, Lee PR. Evaluation of the heart to heart project: Lessons from a community-based chronic disease prevention project. American Journal of Health Promotion. 1995;9:443–445. doi: 10.4278/0890-1171-9.6.443. [DOI] [PubMed] [Google Scholar]
- Gordon NF, English CD, Contractor A, Salmon R, Leighton RF, Franklin BA, Haskell WL. Effectiveness of three models for comprehensive cardiovascular disease risk reduction. The American Journal of Cardiology. 2002;89:1263–1268. doi: 10.1016/s0002-9149(02)02323-8. [DOI] [PubMed] [Google Scholar]
- Gräfner L, Heinrich J, Knappe J, Holtz H. Atherosclerosis precursors in schoolchildren. Results of a two-year intervention study. Cor et Vasa. 1987;29:421–427. [PubMed] [Google Scholar]
- Greaves CJ, Campbell JL. Supporting self-care in general practice. British Journal of General Practice. 2007;57:814–821. [PMC free article] [PubMed] [Google Scholar]
- Greenland S, Schlesselman JJ, Criqui M. The fallacy of employing standardized regression coefficients and correlations as measures of effect. American Journal of Epidemiology. 1986;123:203–208. doi: 10.1093/oxfordjournals.aje.a114229. [DOI] [PubMed] [Google Scholar]
- Griffin KW, Botvin GJ, Nichols TR. Effects of a school-based drug abuse prevention program for adolescents on HIV risk behavior in young adulthood. Prevention Science. 2006;7:103–112. doi: 10.1007/s11121-006-0025-6. [DOI] [PubMed] [Google Scholar]
- Hanssen TA, Nordrehaug JE, Eide GE, Hanestad BR. Improving outcomes after myocardial infarction: A randomized controlled trial evaluating effects of a telephone follow-up intervention. European Journal of Cardiovascular Prevention & Rehabilitation. 2007;14:429–437. doi: 10.1097/HJR.0b013e32801da123. [DOI] [PubMed] [Google Scholar]
- Hanssen TA, Nordrehaug JE, Eide GE, Hanestad BR. Does a telephone follow-up intervention for patients discharged with acute myocardial infarction have long-term effect on health-related quality of life? A randomized controlled trial. Journal of Clinical Nursing. 2009;18:1334–1345. doi: 10.1111/j.1365-2702.2008.02654.x. [DOI] [PubMed] [Google Scholar]
- Hardcastle SJ, Taylor AH, Bailey MP, Harley RA, Haggar MS. Effectiveness of a motivational interviewing intervention on weight loss, physical activity and cardiovascular disease risk factors: A randomised controlled trial with a 12-month post-intervention follow-up. The International Journal of Behavioral Nutrition and Physical Activity. 2013;10:40. doi: 10.1186/1479-5868-10-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison MB, Browne GB, Roberts J, Tugwell P, Gafni A, Graham ID. Quality of life of individuals with heart failure. A randomized trial of the effectiveness of two models of hospital-to-home transition. Medical Care. 2002;40:271–282. doi: 10.1097/00005650-200204000-00003. [DOI] [PubMed] [Google Scholar]
- Haskell WL, Alderman EL, Fair JM, Maron DJ, Mackey SF, Superko HR, Krauss RM. Effects of intensive multiple risk factor reduction on coronary atherosclerosis and clinic cardiac events in men and women with coronary artery disease. Circulation. 1994;89:975–990. doi: 10.1161/01.cir.89.3.975. [DOI] [PubMed] [Google Scholar]
- Hebb DO. Drives and the CNS. Psychological Review. 1955;62:243–254. doi: 10.1037/h0041823. [DOI] [PubMed] [Google Scholar]
- Hedges LV, Olkin I. Statistical methods for meta-analysis. Academic Press; Orlando, FL: 1985. [Google Scholar]
- Heirich MA, Foote A, Erfurt JC. Work-site physical fitness programs: Comparing the impact of different program designs on cardiovascular risks. Journal of Occupational Medicine. 1993;35:510–517. [PubMed] [Google Scholar]
- Hill MN, Bone LR, Hilton SC, Roary MC, Kelen GD, Levine DM. A clinical trial to improve high blood pressure care in young urban black men. The American journal of Hypertension. 1999;12:548–554. doi: 10.1016/s0895-7061(99)00007-2. [DOI] [PubMed] [Google Scholar]
- Hivert M, Langlois M, Bèrard P, Cuerrier J, Carpentier A. Prevention of weight gain in young adults through a seminar-based intervention program. International Journal of Obesity. 2007;31:1262–1269. doi: 10.1038/sj.ijo.0803572. [DOI] [PubMed] [Google Scholar]
- Horlick L, Cameron R, Firor W, Bhalerao U, Baltzan R. The effects of education and group discussion in the post myocardial infarction patient. Journal of Psychosomatic Research. 1984;28:485–492. doi: 10.1016/0022-3999(84)90082-5. [DOI] [PubMed] [Google Scholar]
- Huang SH, Weng KP, Hsieh KS, Ou SF, Lin CC, Chien KJ, Ho TY. Effects of a classroom-based weight-control intervention on cardiovascular disease in elementary-school obese children. Acta Paediatrica Taiwanica. 2006;48:201–206. [PubMed] [Google Scholar]
- Hughes A, Stewart L, Chapple J, McColl JH, Donaldson MDC, Kelnar CJH, Reilly JJ. Randomized, controlled trial of a best-practice individualized behavioral program for treatment of childhood overweight: Scottish Childhood Overweight Treatment Trial (SCOTT) Pediatrics. 2008;121:539–546. doi: 10.1542/peds.2007-1786. [DOI] [PubMed] [Google Scholar]
- Hunter M, O'Dea I. An evaluation of a health education intervention for mid-aged women: Five year follow-up of effects upon knowledge, impact of menopause and health. Patient Education and Counseling. 1999;38:249–255. doi: 10.1016/s0738-3991(98)00143-8. [DOI] [PubMed] [Google Scholar]
- Hunter C, Peterson A, Alvarez L, Poston WC, Brundige AR, Haddock CK, Foreyt JP. Weight management using the internet: A randomized controlled trial. American Journal of Preventive Medicine. 2008;34:119–126. doi: 10.1016/j.amepre.2007.09.026. [DOI] [PubMed] [Google Scholar]
- Hussien S. Retrieved from Dissertation Abstracts International. 2007. Impact of a culturally-sensitive lifestyle intervention on reducing risk factors for type 2 diabetes in Arab Canadian Muslim women. (UMI No. 304760536) [Google Scholar]
- Hyman DJ, Pavlik VN, Taylor WC, Goodrick GK, Moye L. Simultaneous vs. sequential counseling or multiple behavior change. Archives of Internal Medicine. 2007;167:1152–1158. doi: 10.1001/archinte.167.11.1152. [DOI] [PubMed] [Google Scholar]
- Ingersoll KS, Farrell-Carnahon L, Cohen-Flipic J, Heckman CJ, Ceperich SD, Hettema J, Marzani-Nissen G. Drug & Alcohol Dependence. 2011;116:177–187. doi: 10.1016/j.drugalcdep.2010.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iso H, Takashi S, Yokota K, Sankai T, Jacobs D, Komachi Y. Community-based education classes for hypertension control: A 1.5-year randomized controlled trial. Hypertension. 1996;27:968–974. doi: 10.1161/01.hyp.27.4.968. [DOI] [PubMed] [Google Scholar]
- Jacobs N, Clays E, De Bacquer D, De Backer G, Dendale P, Thijs H, Claes N. Effect of a tailored behavior change program on a composite lifestyle change score: A randomized controlled trial. Health Education Research. 2011;26:886–895. doi: 10.1093/her/cyr046. [DOI] [PubMed] [Google Scholar]
- Jacobs N, De Bourdeaudhuij ID, Thijs H, Dendale P, Claes N. Effect of a cardiovascular program on health behavior and BMI in highly educated adults: A randomized controlled trial. Patient Education and Counseling. 2011;85:122–126. doi: 10.1016/j.pec.2010.08.024. [DOI] [PubMed] [Google Scholar]
- Jatuporn S, Sangwatanaroj S, Saengsiri A, Rattanapruks S, Srimahachota S, Uthayachalerm W, Tosukhowong P. Short term-effect of an intensive lifestyle modification program on lipid peroxidation and antioxidant systems in patients with coronary artery disease. Clinical Hemorheology and Microcirculation. 2003;29:429–436. [PubMed] [Google Scholar]
- Jeong HS, Chae JS, Moon JS, Yoo YS. An individualized teaching program for atherosclerotic risk factor reduction in patients with myocardial infarction. Yonsei Medical Journal. 2001;43:93–100. doi: 10.3349/ymj.2002.43.1.93. [DOI] [PubMed] [Google Scholar]
- Jiang X, Sit JW, Wong TKS. A nurse-led cardiac rehabilitation program improves health behaviors and cardiac physiological risk parameters: Evidence from Chengdu, China. Journal of Clinical Nursing. 2007;16:1886–1897. doi: 10.1111/j.1365-2702.2007.01838.x. [DOI] [PubMed] [Google Scholar]
- Johnson BT. DSTAT 1.10: Software for the meta-analytic review of research literatures. Erlbaum; Hillsdale, NJ: 1993. [Google Scholar]
- Jolly K, Bradley F, Sharp S, Smith H, Thompson S, Kimmonth AL, Mant D. Randomized controlled trial of follow up care in general practice of patients with myocardial infarction and angina: Final results of the Southampton heart integrated care project (SHIP) British Medical Journal. 1999;318:706–711. doi: 10.1136/bmj.318.7185.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones M. It pays to use peer educators. Education and Health. 1992;10:49–54. [Google Scholar]
- Kallio V, Hamalainen H, Hakkila J, Luurila OJ. Reduction in sudden deaths by a multifactorial intervention programme alters acute myocardial infarction. The Lancet. 1979;2:1091–1094. doi: 10.1016/s0140-6736(79)92502-9. [DOI] [PubMed] [Google Scholar]
- Karawalajtys T, McDonough B, Hall H, Guirguis-Younger M, Chambers LW, Kaczorowski J, Hutchinson B. Development of the volunteer peer education role in a community Cardiovascular Health Awareness Program (CHAP): A process evaluation in two communities. Journal of Community Health. 2009;34:336–345. doi: 10.1007/s10900-009-9149-5. [DOI] [PubMed] [Google Scholar]
- Kelishadi R, Sarrafzadegan N, Sadri G, Pashmi R, Mohammadifard N, Tavasoli A, Bahonar A. Short-term results of a community-based program on promoting healthy lifestyle for prevention and control of chronic diseases in a developing country setting: Isfahan healthy heart program, Asia-Pacific. Journal of Public Health. 2011;23:518–533. doi: 10.1177/1010539509348241. [DOI] [PubMed] [Google Scholar]
- Ketola E, Makela M, Klockars M. Individualized multi-factorial lifestyle intervention trial for high-risk cardiovascular patients in primary care. British Journal of General Practice. 2001;51:291–294. [PMC free article] [PubMed] [Google Scholar]
- Ketola E, Sipila R, Makela M. Effectiveness of individual lifestyle interventions in reducing cardiovascular disease and risk factors. Annals Medicine. 2000;32:239–251. doi: 10.3109/07853890009011767. [DOI] [PubMed] [Google Scholar]
- Keyserling T, Hodge C, Jilcott S, Johnston LF, Garcia BA, Gizlice Z, Ammerman AS. Randomized trial of a clinic-based, community-supported, lifestyle intervention to improve physical activity and diet: The North Carolina enhanced WISEWOMAN project. Preventive Medicine. 2008;46:499–510. doi: 10.1016/j.ypmed.2008.02.011. [DOI] [PubMed] [Google Scholar]
- Keyserling T, Samuel-Hodge C, Ammerman A, Ainsworth BE, Henriquez-Roldan CF, Elasy TA, Bangdiwala SI. A randomized trial of an intervention to improve self-care behaviors of African-American women with type 2 diabetes: Impact on physical activity. Diabetes Care. 2002;25:1576–1583. doi: 10.2337/diacare.25.9.1576. [DOI] [PubMed] [Google Scholar]
- Killen JD, Robinson TN, Telch MJ, Saylor KE, Maron DJ, Rich T, Bryson S. The Stanford adolescent heart health program. Health Education Quarterly. 1989;16:263–283. doi: 10.1177/109019818901600210. [DOI] [PubMed] [Google Scholar]
- Kinnunen T, Leeman R, Korhonen T, Quiles ZN, Terwal DM, Garvey AJ, Hartley HL. Exercise as an adjunct to nicotine gum, in treating tobacco dependence among women. Nicotine & Tobacco Research. 2008;10:689–703. doi: 10.1080/14622200801979043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein SB. Motivation: Biosocial approaches. McGraw-Hill; New York, NY: 1982. [Google Scholar]
- Klesges RC, Eck LH, Isbell TR, Fulliton W, Hanson CL. Smoking status: Effects on the dietary intake, physical activity, and body fat of adult men. American Journal of Clinical Nutrition. 1990;51:784–789. doi: 10.1093/ajcn/51.5.784. [DOI] [PubMed] [Google Scholar]
- Knutsen S, Knutsen R. The Tromso Survey: The family intervention study: The effect of intervention on some coronary risk factors and dietary habits, a 6-year follow-up. Preventive Medicine. 1991;20:197–212. doi: 10.1016/0091-7435(91)90020-5. [DOI] [PubMed] [Google Scholar]
- Krasnoff JB, Vintro AQ, Ascher NL, Bass NM, Paul SM, Dodd MJ, Painter PL. A randomized trial of exercise and dietary counseling after liver transplantation. American Journal of Transplantation. 2006;6:1896–1905. doi: 10.1111/j.1600-6143.2006.01391.x. [DOI] [PubMed] [Google Scholar]
- Kuller LH, Kinzel LS, Pettee KK, Kriska AM, Simkin-Silverman L, Conroy MB, Johnson BD. Lifestyle intervention and coronary heart disease risk factor changes over 18 months in postmenopausal women: The women on the move through activity and nutrition (WOMAN Study) clinical trial. Journal of Women Health. 2006;18:962–974. doi: 10.1089/jwh.2006.15.962. [DOI] [PubMed] [Google Scholar]
- Kumkale GT, Albarracín D. The sleeper effect in persuasion: A meta-analysis. Psychological Bulletin. 2004;130:143–172. doi: 10.1037/0033-2909.130.1.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kypri K, McAnally H. Randomized controlled trial of a web-based primary care intervention for multiple health risk behaviors. Preventive Medicine. 2005;41:761–766. doi: 10.1016/j.ypmed.2005.07.010. [DOI] [PubMed] [Google Scholar]
- Lalonde L, Gray-Donald K, Lowensteyn I, Marchand S, Dorais M, Michaels G, Grover SA. Comparing the benefits of diet and exercise in the treatment of dyslipidemia. Preventive Medicine. 2002;35:16–24. doi: 10.1006/pmed.2002.1052. [DOI] [PubMed] [Google Scholar]
- Latimer AE, Rivers SR, Rench TA, Katulak NA, Hicks A, Hodorowski JK, Salovey P. A field experiment testing the utility of regulatory fit messages for promoting physical activity. Journal of Experimental Social Psychology. 2008;44:826–832. doi: 10.1016/j.jesp.2007.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lear SA, Spinelli JJ, Linden W, Brozic A, Kiess M, Frohlich JJ, Ignaszewski A. The Extensive Lifestyle Management Intervention (ELMI) after cardiac rehabilitation: A 4-year randomized controlled trial. American Heart Journal. 2006;152:333–339. doi: 10.1016/j.ahj.2005.12.023. [DOI] [PubMed] [Google Scholar]
- Leighton R, Repka F, Birk T, Lynch DJ, Bingle JF, Gohara AF, Walsh E. The Toledo exercise and diet study. Archives of Internal Medicine. 1990;150:1016–1020. [PubMed] [Google Scholar]
- Lichtman J, Amatruda J, Yaari S, Cheng S, Smith GL, Mattera JA, Krumholz HM. Clinical trial of an educational intervention to achieve recommended cholesterol levels in patients with coronary artery disease. American Heart Journal. 2003;147:522–528. doi: 10.1016/j.ahj.2003.06.003. [DOI] [PubMed] [Google Scholar]
- Light KL, Obrist PA. Cardiovascular response to stress: Effects of the opportunity to avoid shock, shock experience, and performance feedback. Psychophysiology. 1980;17:243–252. doi: 10.1111/j.1469-8986.1980.tb00143.x. [DOI] [PubMed] [Google Scholar]
- Lin H, Tsai Y, Lin P, Tsay P. Effects of a therapeutic lifestyle-change programme on cardiac risk factors after coronary artery bypass graft. Journal of Clinical Nursing. 2010;19:60–68. doi: 10.1111/j.1365-2702.2009.02980.x. [DOI] [PubMed] [Google Scholar]
- Lin PH, Appel LJ, Funk K, Craddick S, Chen C, Elmer P, Champagne C. The PREMIER intervention helps participants follow the dietary approaches to stop hypertension dietary pattern and the current dietary reference intakes recommendations. Journal of the American Dietetic Association. 2007;107:1541–1551. doi: 10.1016/j.jada.2007.06.019. [DOI] [PubMed] [Google Scholar]
- Lindsay S, Bellaby P, Smith S, Baker R. Enabling healthy choices: is ICT the highway to health improvement? Health. 2008;12:313–331. doi: 10.1177/1363459308090051. [DOI] [PubMed] [Google Scholar]
- Lindsay S, Smith S, Bellaby P, Baker R. The health impact of an online heart disease support group: A comparison of moderated versus un-moderated support. Health Education Research. 2009;24:646–654. doi: 10.1093/her/cyp001. [DOI] [PubMed] [Google Scholar]
- Lindstrom J, Eriksson JG, Valle TT, Aunola S, Cepaitis Z, Hakumaki H, Tuomilheto J. Prevention of diabetes mellitus in subjects with impaired glucose tolerance in the Finnish diabetes prevention study: Results from a randomized clinical trial. Journal of American Society of Nephrology. 2003;14(Suppl. 2):108–113. doi: 10.1097/01.asn.0000070157.96264.13. [DOI] [PubMed] [Google Scholar]
- Lindstrom J, Louheranta A, Mannelin M, Rastas M, Eriksson J, Uusitupa M, Tuomilheto J, Finnish Diabetes Prevention Study Group The Finnish Diabetes Prevention Study (DPS): Lifestyle intervention and 3 year results on diet and physical activity. Diabetes Care. 2003;26:3230–3236. doi: 10.2337/diacare.26.12.3230. [DOI] [PubMed] [Google Scholar]
- Lisspers J, Hofman-Bang C, Ryden L, Sundin O, Öhman A, Nygren A. Long-term effects of lifestyle behavior change in coronary artery disease: Effects on recurrent coronary events after percutaneous coronary intervention. Health Psychology. 2005;24:41–48. doi: 10.1037/0278-6133.24.1.41. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manios Y, Moschonis G, Koutsikas K, Papoutsou S, Petraki I, Bellou E, Tanagra S. Changes in body composition following a dietary and lifestyle intervention trial: The postmenopausal health study. Maturitas. 2008;62:58–65. doi: 10.1016/j.maturitas.2008.11.005. [DOI] [PubMed] [Google Scholar]
- McAlister F, Lawson F, Teo K, Armstrong P. Randomized trials of secondary prevention programmes in coronary heart disease: A systematic review. British Medical Journal. 2001;323:957–962. doi: 10.1136/bmj.323.7319.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClelland JW, Irving LM, Mitchell RE, Bearson LB, Webber KH. Extending the reach of nutrition education for older adults: Feasibility of a train-the-trainer approach in congregate nutrition sites. Journal of Nutrition Education and Behavior. 2002;34(S1):48–52. doi: 10.1016/s1499-4046(06)60311-4. [DOI] [PubMed] [Google Scholar]
- McGillion MH, Watt-Watson J, Stevens B, LeFort SM, Coyte P, Graham A. Randomized controlled trial of a psychoeducation program for the self-management of chronic cardiac pain. Journal of Pain and Symptom Management. 2008;36:126–140. doi: 10.1016/j.jpainsymman.2007.09.015. [DOI] [PubMed] [Google Scholar]
- McGuire WJ. Personality and attitude change. In: Greenwald AG, Brock TC, Ostrom TM, editors. Psychological foundation of attitudes. Vol. 3. Academic Press; San Diego, CA: 1968. pp. 171–196. [Google Scholar]
- Mendl M. Performing under pressure: Stress and cognitive function. Applied Animal Behavior Science. 1999;65:221–244. [Google Scholar]
- Meichenbaum D, Turk DC. Facilitating treatment adherence: A practitioner's guidebook. Plenum Press; New York, NY: 1987. [Google Scholar]
- Miettinen TA, Huttunen JK, Naukkarinen V, Strandberg T, Mattila S, Kumlin T, Sarna S. Multifactorial primary prevention of cardiovascular diseases in middle-aged men: Risk factor changes, incidence, and mortality. Journal of the American Medical Association. 1985;254:2097–2102. [PubMed] [Google Scholar]
- Miller GA. The magical number seven, plus or minus two: Some limits on our capacity for processing information. Psychological Review. 1956;63:81–97. [PubMed] [Google Scholar]
- Mittag O, China C, Hoberg E, Juers E, Kolenda KD, Richardt GA, Raspe H. Outcomes of cardiac rehabilitation with versus without a follow-up intervention rendered by telephone (Luebeck follow-up trial): Overall and gender-specific affects. International Journal of Rehabilitation Research Issue. 2006;29:295–302. doi: 10.1097/MRR.0b013e328010ba9a. [DOI] [PubMed] [Google Scholar]
- Morey M, Snyder D, Sloane R, Cohen H, Peterson B, Hartman T, Denmark-Wahnefried W. Effects of home-based diet and exercise on functional outcomes among older, overweight long-term cancer survivors. The Journal of American Medical Association. 2009;301:1883–1991. doi: 10.1001/jama.2009.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris SB. Distribution of the standardized mean change effect size for meta-analysis on repeated measures. British Journal of Mathematical & Statistical Psychology. 2000;53:17–29. doi: 10.1348/000711000159150. [DOI] [PubMed] [Google Scholar]
- Morrison N. Group cognitive therapy: treatment of choice or suboptimal option? Behavioral and Cognitive Psychotherapy. 2001;29:311–332. [Google Scholar]
- Mosca L, Christian A, Mochari-Greenberger H, Kligfield P, Smith S. A randomized clinical trial of secondary prevention among women hospitalized with coronary heart disease. Journal of Women's Health. 2010;19:195–202. doi: 10.1089/jwh.2009.1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moy F, Sallam AA, Wong M. The results of a worksite health promotion program in Kuala Lumpur, Malaysia. Health Promotion International. 2006;22:301–310. doi: 10.1093/heapro/dal031. [DOI] [PubMed] [Google Scholar]
- Muraven M, Slessareva E. Mechanisms of self-control failure: Motivation and limited resources. Personality and Social Psychology Bulletin. 2003;29:894–906. doi: 10.1177/0146167203029007008. [DOI] [PubMed] [Google Scholar]
- Muraven M, Tice DM, Baumeister RF. Self-control as a limited resource: Regulatory depletion patterns. Journal of Personality and Social Psychology. 1998;74:774–789. doi: 10.1037//0022-3514.74.3.774. [DOI] [PubMed] [Google Scholar]
- Murchie P, Campbell NC, Ritchie LD, Simpson JA, Thain J. Secondary prevention clinics for coronary heart disease: Four year follow up of a randomized controlled trial in primary care. British Medical Journal. 2003;326:84.. doi: 10.1136/bmj.326.7380.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L, Muthén B. Mplus user's guide. Muthen & Muthen; Los Angeles, CA: 2006. [Google Scholar]
- Muto T, Yamauchi K. Evaluation of a multi-component workplace health promotion program conducted in Japan for improving employee's cardiovascular disease risk factors. Preventive Medicine. 2001;33:571–577. doi: 10.1006/pmed.2001.0923. [DOI] [PubMed] [Google Scholar]
- Nader P, Sallis J, Patterson T, Abramson IS, Rupp JW, Senn KL, Vega WA. A family approach to cardiovascular risk reduction: Results from the San Diego Family Health Project. Health Education Quarterly. 1989;16:229–244. doi: 10.1177/109019818901600207. [DOI] [PubMed] [Google Scholar]
- Nader PR, Stone EJ, Lytle LA, Perry CL, Osganian SK, Kelder S, Luepker RV. Three-year maintenance of improved diet and physical activity. Archives of Pediatrics & Adolescent Medicine. 1999;153:695–704. doi: 10.1001/archpedi.153.7.695. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics National Health and Nutrition Examination Survey Data. Hyattsville, 2007–2010 data. 2011 Retrieved from http://www.cdc.gov/nchs/hus/contents2011.htm#071.
- Newell SA, Girgis A, Sanson-Fisher R, Savolainen NJ. The accuracy of self-reported health behaviors and risk factors relating to cancer and cardiovascular disease in the general population: A critical review. American Journal of Preventive Medicine. 1999;17:211–229. doi: 10.1016/s0749-3797(99)00069-0. [DOI] [PubMed] [Google Scholar]
- Niaura R, Marcuss B, Albrecht A, Thompson P, Abrams D. Exercise, smoking cessation, and short-term changes in serum lipids in women: A preliminary investigation. Medicine & Science in Sport & Exercise. 1998;30:1414–1418. doi: 10.1097/00005768-199809000-00010. [DOI] [PubMed] [Google Scholar]
- Nies MA, Artinian NT, Schim SM, Wal JSV, Sherrick-Escamilla S. Effects of lay health educator interventions on activity, diet, and health risks in an urban mexican american community. The Journal of Primary Prevention. 2004;25:441–455. [Google Scholar]
- Nigg C, Allegrante JP, Ory M. Theory-comparison and multiple-behavior research: Common themes advancing health behavior research. Health Education Research. 2002;17:670–679. doi: 10.1093/her/17.5.670. [DOI] [PubMed] [Google Scholar]
- Nigg CR, Long CR. A systematic review of single health behavior change interventions vs. multiple behavior change interventions among older adults. Translational Behavioral Medicine. 2012;2:163–179. doi: 10.1007/s13142-012-0130-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsson PM, Klasson EB, Nyberg P. Life-style intervention at the worksite-Reduction of cardiovascular risk factors in a randomized study. Scandinavian Journal of Work Environment Health. 2001;27:57–62. doi: 10.5271/sjweh.587. [DOI] [PubMed] [Google Scholar]
- Nishtar S, Badar A, Kamal MU, Iqbal A, Bajwa R, Shah T, Rahim E. The Heartfile Lodhran CVD prevention Project-- end of Project evaluation. Promotion & Education. 2007;14:17–27. [PubMed] [Google Scholar]
- Noar SM, Chabot M, Zimmerman RS. Applying health behavior change theory to multiple behavior change: Considerations and approaches. Preventive Medicine. 2008;46:275–280. doi: 10.1016/j.ypmed.2007.08.001. [DOI] [PubMed] [Google Scholar]
- Noguchi K, Albarracín D, Durantini M, Glasman L. Who participates in which health promotion programs? A meta-analysis of motivations underlying enrollment and retention in HIV prevention interventions. Psychological Bulletin. 2007;133:955–975. doi: 10.1037/0033-2909.133.6.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordmann A, Heilmbauer I, Walker T, Martina B, Battegay E. A case-management program of medium intensity does not improve cardiovascular risk factor control in coronary artery disease patients: The Heartcare I trial. The American Journal of Medicine. 2001;110:543–550. doi: 10.1016/s0002-9343(01)00682-9. [DOI] [PubMed] [Google Scholar]
- Norris SL, Nichols PJ, Caspersen CJ, Glasgow RE, Engelgau MM, Jack L, Jr., McCulloch D. Increasing diabetes self-management education in community settings: A systematic review. American Journal of Preventive Medicine. 2002;22:39–66. doi: 10.1016/s0749-3797(02)00424-5. [DOI] [PubMed] [Google Scholar]
- Norris SL, Engelgau MM, Narayan KMV. Effectiveness of self-management training in type-2 diabetes: A systematic review of randomized controlled trials. Diabetes Care. 2001;24:561–587. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- Norris SL, Zhang X, Avenall A, Gregg E, Bowman B, Serdula M, Lau J. Long-term effectiveness of lifestyle and behavioral weight loss interventions in adults with type 2 diabetes: A meta-analysis. The American Journal of Medicine. 2004;117:762–774. doi: 10.1016/j.amjmed.2004.05.024. [DOI] [PubMed] [Google Scholar]
- Oenema A, Brug J, Dijkstra A, de Weerdt I, de Vries H. Efficacy and use of an internet-delivered computer-tailored lifestyle intervention, targeting saturated fat intake, physical activity and smoking cessation: A randomized controlled trial. Annals of Behavioral Medicine. 2008;35:125–135. doi: 10.1007/s12160-008-9023-1. [DOI] [PubMed] [Google Scholar]
- Oh E, Hyun S, Kim S, Bang SY, Chu S,H, Jeon JY, Kang MS. A randomized controlled trial of therapeutic life style modification in rural women with metabolic syndrome: A pilot study. Metabolism Clinical and Experimental. 2008;57:255–251. doi: 10.1016/j.metabol.2007.09.009. [DOI] [PubMed] [Google Scholar]
- Olvera N, Bush JA, Sharma S, Knox B, Scherer R, Butte N. BOUNCE: A community-based mother-daughter healthy lifestyle intervention for low-income Latino families. Childhood Obesity. 2010;18(Suppl. 1):102–104. doi: 10.1038/oby.2009.439. [DOI] [PubMed] [Google Scholar]
- Ornish D, Brown SE, Scherwitz LW, Billings JH, Armstrong WT, Ports TA, Gould KL. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart trial. Lancet. 1990;336:129–133. doi: 10.1016/0140-6736(90)91656-u. [DOI] [PubMed] [Google Scholar]
- Ornstein SM, Musham C, Reid A, Jenkins RG, Zemp LD, Garr DR. Barriers to adherence to preventive services reminder letters: The patient's perspective. Journal of Family Practice. 1993;36:195–200. [PubMed] [Google Scholar]
- Ostbye T, Krause KM, Lovelady CA, Morey MC, Bastian LA, Peterson BL, McBride CM. Active mothers postpartum: A randomized controlled weight-loss intervention trial. American Journal of Preventive Medicine. 2009;37:173–180. doi: 10.1016/j.amepre.2009.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Golub SA, Rosof E, Holder C. Motivational interviewing and cognitive-behavioral intervention to promote HIV medication adherence among hazardous drinkers: A randomized control trial. Journal of Acquired Immune Deficiency Syndrome. 2007;46:443–450. doi: 10.1097/qai.0b013e318158a461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick K, Calfas KJ, Norman GJ, Zabinski MF, Sallis JF, Rupp J, Cella J. Randomized controlled trial of a primary care and home-based intervention for physical activity and nutrition behaviors. Journal of Pediatrics and Adolescent Medicine. 2006;160:128–136. doi: 10.1001/archpedi.160.2.128. [DOI] [PubMed] [Google Scholar]
- Patterson R. Changing patient behavior: Improving outcomes in health and disease management. Jossey-Bass; San Francisco, CA: 2001. [Google Scholar]
- Paul-Ebhohimhen V, Avenell A. A systematic review of the effectiveness of group versus individual treatments for adult obesity. Obesity Facts. 2009;2:17–24. doi: 10.1159/000186144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philis-Tsimikas A, Walker C, Rivard L, Talavera G, Reimann JO, Salman M, Araujo R. Improvement in diabetes care of underinsured patients enrolled in Project Dulce: A community based, culturally appropriate, nurse case management and peer education diabetes care model. Diabetes Care. 2004;27:110–115. doi: 10.2337/diacare.27.1.110. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: Application to addictive behaviors. American Psychologist. 1992;47:1002–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- Prochaska JJ, Nigg CR, Spring B, Velicer WF, Prochaska JM. The benefits and challenges of multiple behavior change in research an practice. Preventive Medicine. 2010;50:26–29. doi: 10.1016/j.ypmed.2009.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JJ, Prochaska JM. Multiple risk behavior change: What most individuals need. In: Okene J, Reikert K, Shumaker S, editors. The Handbook of Health Behavior Change. 3rd ed. Springfield Publishers; New York, NY: 2008. pp. 287–305. [Google Scholar]
- Prochaska JO, Redding CA, Harlow LL, Rossi JS, Velicer WF. The transtheoretical model of change and HIV prevention: A review. Health Education Quarterly. 1994;21:471–486. doi: 10.1177/109019819402100410. [DOI] [PubMed] [Google Scholar]
- Prochaska JJ, Spring B, Nigg CR. Multiple health behavior change research: An introduction and overview. Preventive Medicine. 2008;46:181–188. doi: 10.1016/j.ypmed.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronk NP, Anderson LH, Crain AL, Martinson BC, O'Connor PJ, Sherwood NE, Whitebird RR. Meeting recommendations for multiple healthy lifestyle factors. Prevalence, clustering, and predictors among adolescent, adult, and senior health plan members. American Journal of Preventive Medicine. 2004;27:25–33. doi: 10.1016/j.amepre.2004.04.022. [DOI] [PubMed] [Google Scholar]
- Proper KI, Hildebrandt VH, Van der Beek AJ, Twisk JWR, Van Mechelen W. Effect of individual counseling on physical activity fitness and health: A randomized controlled trial in a workplace setting. American Journal of Preventive Medicine. 2003;24:218–226. doi: 10.1016/s0749-3797(02)00645-1. [DOI] [PubMed] [Google Scholar]
- Renjilian DA, Perri MG, Nezu AM, McKelvey WF, Shermer RL, Anton SD. Individual versus group therapy for obesity: Effects of matching participants to their treatmetn preferences. Journal of Consulting & Clinical Psychology. 2001;69:717–721. [PubMed] [Google Scholar]
- Rosenthal R. Writing meta-analytic reviews. Psychological Bulletin. 1995;118:183–192. [Google Scholar]
- Rothman AJ, Salovey P. Shaping perceptions to motivate healthy behavior: The role of message framing. Psychological Bulletin. 1997;121:3–19. doi: 10.1037/0033-2909.121.1.3. [DOI] [PubMed] [Google Scholar]
- Rothman AJ, Salovey P, Antone C, Keough K, Martin C. The influence of message framing on intentions to perform health behaviors. Journal of Experimental Social Psychology. 1993;29:408–433. [Google Scholar]
- Sacco WP, Malone JI, Morrison AD, Friedman A, Wells K. Effect of a brief, regular telephone intervention by paraprofessionals for type 2 diabetes. Journal of Behavioral Medicine. 2009;32:349–359. doi: 10.1007/s10865-009-9209-4. [DOI] [PubMed] [Google Scholar]
- Salminen M, Vahlberg T, Ojanlatva, A. Kivela S. Effects of a controlled family-based health education/counseling intervention. American Journal of Health Behavior. 2005;29:395–406. doi: 10.5555/ajhb.2005.29.5.395. [DOI] [PubMed] [Google Scholar]
- Sarrafzadegan N, Kelishadi R, Esmaillzadeh A, Mohammadifard N, Rabiei K, Roohafza H, Malekafzali H. Do lifestyle interventions work in developing countries? Findings from the Isfahan Healthy Heart Program in the Islamic Republic of Iran. Bulletin of World Health Organization. 2009;87:39–50. doi: 10.2471/BLT.07.049841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savoye M, Shaw M, Dziura J, Tamborlane W, Guandalini C, Burgert TS, Caprio S. Effects of a weight management program on body composition and metabolic parameters in overweight children: A randomized controlled trial. The Journal of the American Medical Association. 2007;297:2697–2704. doi: 10.1001/jama.297.24.2697. [DOI] [PubMed] [Google Scholar]
- Schroder KE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: 1. Item content, scaling, and data analytical options. Annals of Behavioral Medicine. 2003;26:76–103. doi: 10.1207/s15324796abm2602_02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shadish WR. Meta-analysis and the exploration of causal mediating processes: A primer of examples, methods, and issues. Psychological Methods. 1996;1:47–65. [Google Scholar]
- Sherwin R. Sudden death in men with increased risk of myocardial infarction. Drugs. 1984;28:46–53. doi: 10.2165/00003495-198400281-00005. [DOI] [PubMed] [Google Scholar]
- Shibayama T, Kobayashi K, Takano A, Kadowaki T, Kazuma K. Effectiveness of lifestyle counseling by certified expert nurse of Japan for non-insulin-treated diabetic outpatients: A 1-year randomized controlled trial. Diabetes Research and Clinical Practice. 2007;76:265–268. doi: 10.1016/j.diabres.2006.09.017. [DOI] [PubMed] [Google Scholar]
- Shiffrin RM, Nosofsky RM. Seven plus or minus two: A commentary on capacity limitations. Psychological Review. 1994;101:357–361. doi: 10.1037/0033-295x.101.2.357. [DOI] [PubMed] [Google Scholar]
- Silvia PJ, Jones HC, Kelly CS, Zibae A. Trait self-focused attention, task difficulty, and effort-related cardiocascular reactivity. International Journal of Psychophysiology. 2011;79:335–340. doi: 10.1016/j.ijpsycho.2010.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silvia PJ, McCord DM, Gendolla GHE. Self-focused attention, performance expectancies, and the intensity of effort: Do people try harder for harder goals? Motivation & Emotion. 2010;34:363–370. [Google Scholar]
- Simkin-Silverman L, Wing RR, Hansen DH, Klem ML, Pasagian-Macaulay AP, Meilahn EN, Kuller LH. Prevention of Cardiovascular risk factor elevations, in healthy premenopausal women. Preventive Medicine. 1995;24:509–517. doi: 10.1006/pmed.1995.1081. [DOI] [PubMed] [Google Scholar]
- Simkin-Silverman LR, Wing RR, Boraz MA, Meilahn EN, Kuller LH. Maintenance of cardiovascular risk factor changes among middle-aged women in a lifestyle intervention trial. Women's Health: Research On Gender Behavior. 1998;4:255–271. [PubMed] [Google Scholar]
- Singh RB, Sharma VK, Rastogi SS, Singh NK. In patients with mild hypertension, do exercise and a gradual rather then abrupt increase in fatty acid and salt intake cause fewer rises in cardiovascular risk factors? Clinical Nutrition. 1992;11:309–314. doi: 10.1016/0261-5614(92)90009-f. [DOI] [PubMed] [Google Scholar]
- Skinner TC, van der Ven N. Psychological group interventions in diabetes care. In: Snoek FJ, Skinner TC, editors. Psychology in diabetes care. John Wiley & Sons, Ltd; Hoboken, NJ: 2005. pp. 141–169. [Google Scholar]
- Slutsky P, Bryan-Stevens T. Developing a comprehensive community based asthma education and training program. Pediatric Nursing. 2001;27:449–458. [PubMed] [Google Scholar]
- Smedley BD, Syme SL. Promoting Health: Intervention Strategies from Social and Behavioral Research. National Academy Press; Washington, DC: 2000. [PubMed] [Google Scholar]
- Smith L. Support for Healthy Eating and Exercise (SHEE) Dissertation Abstracts International. 2007;69:4445. UMI No.3315760. [Google Scholar]
- Song KJ. The effects of self-efficacy promoting cardiac rehabilitation program on self-efficacy, health behavior, and quality of life. Journal of Korean Academy of Nursing. 2003;33:510–518. doi: 10.4040/jkan.2003.33.4.510. [DOI] [PubMed] [Google Scholar]
- Spring B, Doran N, Pagoto S, Schneider K, Pingitore R, Hedeker D. Randomized controlled trial for behavioral smoking and weight control treatment: Effect of concurrent versus sequential intervention. Journal of Consulting and Clinical Psychology. 2004;72:785–796. doi: 10.1037/0022-006X.72.5.785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spring B, Howe D, Berendsen M, McFadden G, Hitchcock K, Rademaker AW, Hitsman B. Behavioral intervention to promote smoking cessation and prevent weight gain: A systematic review and meta-analysis. Addiction. 2009;104:1472–1486. doi: 10.1111/j.1360-0443.2009.02610.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spring B, Schneider K, McFadden HG, Vaughn J, Kozak AT, Smith M, Lloyd-Jones DM. Multiple behavior change in diet and activity: A randomized controlled trial using mobile technology. Archives of Internal Medicine. 2012;172(10):789–796. doi: 10.1001/archinternmed.2012.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stamler R, Stamler J, Gosch F, Civinelli J, Fishman J, McKeever P, Dyer AR. Primary prevention of hypertension by nutritional-hygienic means: Final report of a randomized, controlled trial. Journal of the American Medical Association. 1989;262:1801–1807. [PubMed] [Google Scholar]
- Steptoe A, Doherty S, Rink E, Kerry S, Kendrick T, Hilton S. Behavioral counseling in general practice for the promotion of healthy behavior among adults at increased risk of coronary heart disease: Randomized trial. British Medical Journal. 1999;319:943–948. doi: 10.1136/bmj.319.7215.943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Kerry S, Rink E, Hilton S. The impact of behavioral counseling on stage of change in fat intake, physical activity, and cigarette smoking in adults at increased risk of coronary heart disease. American Journal of Public Health. 2001;91:265–269. doi: 10.2105/ajph.91.2.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Rink E, Phil M, Kerry S. Psychosocial predictors of changes in physical activity in overweight sedentary adults following counseling in primary care. Preventive Medicine. 2000;31:183–194. doi: 10.1006/pmed.2000.0688. [DOI] [PubMed] [Google Scholar]
- Storro O, Oien T, Dotterud C, Jenssen JA, Johnsen R. A primary health-care intervention on pre- and postnatal risk factor behavior to prevent childhood allergy. The prevention of allergy among children in Trondheim (PACT) study. BMC Public Health. 2010;10:443. doi: 10.1186/1471-2458-10-443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strandberg TE, Salomaa VV, Naukkarinen VA, Vanhanen HT, Sarna SJ, Miettinen TA. Long-term mortality after 5-year multi-factorial primary prevention of cardiovascular diseases. Journal of the American Medical Association. 1991;266:1225–1229. [PubMed] [Google Scholar]
- Streiner DI. Finding our way: An introduction to path analysis. Canadian Journal of Psychiatry. 2005;50:115–122. doi: 10.1177/070674370505000207. [DOI] [PubMed] [Google Scholar]
- Sun J, Wang Y, Chen X, Chen Y, Feng Y, Zhang X, Mustad VA. An integrated intervention program to control diabetes in overweight Chinese women and men with type 2 diabetes. Asia Pacific Journal of Clinical Nutrition. 2008;17:514–524. [PubMed] [Google Scholar]
- Svetkey L, Pollak K, Yancy W, Dolor RJ, Batch BC, Samsa G, Lin PH. Hypertension Improvement Project (HIP): Randomized trial of quality improvement for physicians and lifestyle modification for patients. Hypertension. 2009;54:1226–1233. doi: 10.1161/HYPERTENSIONAHA.109.134874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talvi AI, Jarvisalo JO, Knuts LR. A health promotion program for oil refinery employees: Changes of health promotion needs observed at three years. Occupational Medicine. 1999;49:93–101. doi: 10.1093/occmed/49.2.93. [DOI] [PubMed] [Google Scholar]
- Teigen KH. Yerkes-Dodson: A law for all seasons. Theory & Psychology. 1994;4:525–547. [Google Scholar]
- Thompson D, Baranowski T, Cullen K, Watson K, Liu Y, Canada A, Zakeri I. Food, fun, and fitness internet program for girls: Pilot evaluation of an e-Health youth Obesity prevention program examining predictors of obesity. Preventive Medicine. 2008;47:494–497. doi: 10.1016/j.ypmed.2008.07.014. [DOI] [PubMed] [Google Scholar]
- Toobert DJ, Glasgow RE, Radcliffe JL. Physiologic and related behavioral outcomes from the women's lifestyle heart trial. Annals of Behavioral Medicine. 2000;22:1–9. doi: 10.1007/BF02895162. [DOI] [PubMed] [Google Scholar]
- Toobert DJ, Glasgow RE, Strycker LA, Barrera M, Ritzwoller DP, Weidner G. Long-term effects of the Mediterranean lifestyle program: A randomized clinical trial for postmenopausal women with type 2 diabetes. International Journal of Nutrition and and Physical Activity. 2007;4:1–12. doi: 10.1186/1479-5868-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trento M, Passera P, Tomalino M, Pagnozzi F, Pomero F, Vaccari P, Porta M. Therapeutic group education in the follow-up of patients with non-insulin treated, non-insulin dependent diabetes mellitus. Diabetes, Nutrition & Metabolism. 1998;11:212–216. [Google Scholar]
- Trento M, Passera P, Bajardi M, Tomalino M, Grassi G, Borgo E, Porta M. Lifestyle intervention by group care preventsdeterioration of Type II diabetes: A 4-year randomized controlled clinical trial. Diabetologia. 2002;45:1231–1231. doi: 10.1007/s00125-002-0904-8. [DOI] [PubMed] [Google Scholar]
- Tudor-Smith C, Nutbeam D, Moore L, Catford J. Effects of the Heartbeat Wales program over five years on behavioral risks for cardiovascular disease: Quasi-experimental comparison of results from Wales and a matched reference area. British Medical Journal. 1998;316:818–822. doi: 10.1136/bmj.316.7134.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuomilehto J, Lindstrom J, Eriksson JG, Hamalainen H, IIanne-Parikka P, Keinanen-Kiukaanniemi S, Uusitupa M. Prevention of type-2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. New England Journal of Medicine. 2001;344:1343–1350. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . Healthy People 2010. DHHS; Washington, DC: 2000. [Google Scholar]
- Ussher M, Taylor, Faulkner G. Exercise interventions for smoking cessation. Cochrane Database of Systematic Reviews. 2012;1 doi: 10.1002/14651858.CD002295.pub4. CD002295.pub4. [DOI] [PubMed] [Google Scholar]
- Ussher M, West R, McEwen A, Taylor A, Steptoe A. Efficacy of exercise counseling as an aid for smoking cessation: A randomized controlled trial. Addiction. 2003;98:523–532. doi: 10.1046/j.1360-0443.2003.00346.x. [DOI] [PubMed] [Google Scholar]
- Ussher M, West R, McEwen A, Taylor A, Steptoe A. Randomized controlled trial of physical activity counseling as an aid to smoking cessation: 12 month follow-up. Addictive Behaviors. 2007;32:3060–3064. doi: 10.1016/j.addbeh.2007.04.009. [DOI] [PubMed] [Google Scholar]
- Vale MJ, Jelinek MV, Best JD, Dart AM, Grigg LE, Hare DL, McNeil JJ, on behalf of the COACH Study Group Coaching patients on achieving cardiovascular health (COACH): A multicenter randomized trial in patients with coronary heart disease. Archives of Internal Medicine. 2003;163:2775–2783. doi: 10.1001/archinte.163.22.2775. [DOI] [PubMed] [Google Scholar]
- Van Elderen T, Maes S, Seegers G, Kragten H, Relik-Van Wely L. Effects of a post-hospitalization group health education program for patients with coronary heart disease. Psychology and Health. 1994;9:317–330. doi: 10.1080/08870449408407490. [DOI] [PubMed] [Google Scholar]
- Van Elderen-van Kemenade T, Maes S, van den Broek Y. Effects of a health education program with telephone follow-up during cardiac rehabilitation. British Journal of Clinical Psychology. 1994;33:367–378. doi: 10.1111/j.2044-8260.1994.tb01133.x. [DOI] [PubMed] [Google Scholar]
- Vanninen E, Uusitupa M, Siitonen O, Laitine J, Lansimies E. Habitual physical activity, aerobic capacity and metabolic control in patients with newly-diagnosed Type 2 (non-insulin-dependent) diabetes mellitus: Effect of 1-year diet and exercise intervention. Diabetologia. 1992;35:340–346. doi: 10.1007/BF00401201. [DOI] [PubMed] [Google Scholar]
- van Zuilen A, Blankestijn P, van Buren M, ten Dam M, Kaasjager K, Ligtenberg G, Wetzels JF, on behalf of the MASTERPLAN study group Nurse practitioners improve quality of care in chronic kidney disease: two-year results of a randomised study. The Netherlands Journal of Medicine. 2011;69:517–524. [PubMed] [Google Scholar]
- Vestfold Healthcare Study Group Influence on lifestyle measures and five-year coronary risk by a comprehensive lifestyle intervention program in patients with coronary heart disease. European Journal of Cardiovascular Prevention and Rehabilitation. 2003;10:429–437. doi: 10.1097/01.hjr.0000107024.38316.6a. [DOI] [PubMed] [Google Scholar]
- Vohs KD, Heatherton TF. Self-regulatory failure: A resource-depletion approach. Psychological Science. 2000;11:249–254. doi: 10.1111/1467-9280.00250. [DOI] [PubMed] [Google Scholar]
- von Bertalanffy L. General systems theory. Braziller; New York, NY: 1968. [Google Scholar]
- von Gruenigen VE, Courneya KS, Gibbons HE, Kavanagh MB, Waggoner SE, Lerner E. Feasibility and effectiveness of a lifestyle intervention program in obese endometrial cancer patients: A randomized trial. Gynecologic Oncology. 2008;109:19–26. doi: 10.1016/j.ygyno.2007.12.026. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Berkowitz R,I, Womble LG, Sarwer DB, Phelan S, Cato RK, Stunkard AJ. Randomized trial of lifestyle modification and pharmacotherapy for obesity. The New England Journal of Medicine. 2005;353:2111–2120. doi: 10.1056/NEJMoa050156. [DOI] [PubMed] [Google Scholar]
- Wang MC, Bushman BJ. Integrating results through meta-analytic review using SAS software. SAS Institute Inc; Cary, NC: 1999. [Google Scholar]
- Watanabe M, Okayama A, Shimamoto K, Ueshima H. Short term effectiveness of an individual counseling program for impaired fasting glucose and mild type 2 diabetes in Japan: A multi-center randomized control trial. Asia Pacific Journal of Clinical Nutrition. 2007;16:489–497. [PubMed] [Google Scholar]
- Watkins LL, Sherwood A, Feinglos M, Hinderliter A, Babyak M, Gullette E, Blumenthal JA. Effects of exercise and weight loss on cardiac risk factors associated with syndrome X. Archives of Internal Medicine. 2003;163:1889–1895. doi: 10.1001/archinte.163.16.1889. [DOI] [PubMed] [Google Scholar]
- Werch C, Moore MJ, DiClemente CC, Bledsoe R, Jobli E. A multihealth behavior intervention integrating physical activity and substance use prevention for adolescents. Prevention Science. 2005;6:213–226. doi: 10.1007/s11121-005-0012-3. [DOI] [PubMed] [Google Scholar]
- White N, Carnahan J, Nuget CA, Iwaoka T, Dodson MA. Management of obese patients with Diabetes Mellitus: Comparison of advice education with group management. Diabetes Care. 1986;9:490–496. doi: 10.2337/diacare.9.5.490. [DOI] [PubMed] [Google Scholar]
- Wilhelmsen L, Berglund G, Elmfeldt D, Tibblin G, Wedel H, Pennert K, Werko L. The multifactor primary prevention trial in Goteborg, Sweden. European Heart Journal. 1986;7:279–288. doi: 10.1093/oxfordjournals.eurheartj.a062065. [DOI] [PubMed] [Google Scholar]
- Will J, Massoudi B, Mokdad A, Ford ES, Rosamond W, Stoddard AM, Sorensen G. Reducing risk for cardiovascular disease in uninsured women: Combined results from two WISEWOMAN projects. Journal of American Medical Women's Association. 2001;56:161–165. [PubMed] [Google Scholar]
- Williamson DA, Martin PD, White MA, Newton R, Walden H, York-Crowe E, Ryan D. Efficacy of an internet-based behavioral weight loss program for overweight adolescent African-American girls. Eating and Weight Disorders. 2005;10:193–203. doi: 10.1007/BF03327547. [DOI] [PubMed] [Google Scholar]
- Wilson SR, Scamagas P, German DF, Hughes GW, Lulla S, Coss S, Stancavage FB. A controlled trial of two forms of self-management education for adults with asthma. American Journal of Medicine. 1993;94:564–576. doi: 10.1016/0002-9343(93)90206-5. [DOI] [PubMed] [Google Scholar]
- Wingham J, Dalal HM, Sweeney KG, Evans PH. Listening to patients: Choice in cardiac rehabilitation. European Journal of Cardiovascular Nursing. 2006;5:289–294. doi: 10.1016/j.ejcnurse.2006.02.002. [DOI] [PubMed] [Google Scholar]
- Wister A, Loewen N, Kennedy-Symonds H, McGowan B, McCoy B, Singer J. One-year follow-up of a therapeutic lifestyle intervention targeting cardiovascular disease risk. Canadian Medical Association Journal. 2007;177:859–865. doi: 10.1503/cmaj.061059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witmer JM, Hensel M, Holck PS, Ammerman A, Will J. Heart disease prevention for Alaska native women: A review of pilot study finding. Journal of Women Health. 2004;13:569–578. doi: 10.1089/1540999041280981. [DOI] [PubMed] [Google Scholar]
- Woollard J, Beilin L, Lord T, Puddey I, MacAdam D, Rouse I. A controlled trial of nurse counseling on lifestyle change for hypertensives treated in general practice: Preliminary results. Clinical and Experimental Pharmacology and Physiology. 1995;22:466–468. doi: 10.1111/j.1440-1681.1995.tb02046.x. [DOI] [PubMed] [Google Scholar]
- Wright RA. Brehm's theory of motivation as a model of effort and cardiovascular response. In: Gollwitzer PM, Bargh JA, editors. The psychology of action: Linking cognition and motivation to behavior. Guilford; New York: 1996. pp. 424–453. [Google Scholar]
- Wright JL, Sherriff JL, Dhaliwal SS, Mamo JCL. Tailored, iterative, printed dietary feedback is as effective as group education in improving dietary behaviours: Results from a randomised control trial in middle-aged adults with cardiovascular risk factors. The International Journal of Behavioral Nutrition and Physical Activity. 2011;8(43) doi: 10.1186/1479-5868-8-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright RA, Contrada RJ, Patane MJ. Task difficulty, cardiovascular response, and the magnitude of goal valence. Journal of Personality and Social Psychology. 1986;51:837–843. doi: 10.1037//0022-3514.51.4.837. [DOI] [PubMed] [Google Scholar]
- Writing group of the PREMIER collaborative research group Effects of comprehensive lifestyle modification on blood pressure control: Main results of the PREMIER clinical trial. The Journal of American Medical Association. 2003;289:2083–2093. doi: 10.1001/jama.289.16.2083. [DOI] [PubMed] [Google Scholar]
- Wyer RS, Albarracín D. Belief Formation, Organization, and Change: Cognitive and Motivational Influences. In: Albarracín D, Johnson BT, Zanna MP, editors. Handbook of attitudes. Lawrence Erlbaum; Hillsdale, NJ: 2005. pp. 273–322. [Google Scholar]
- Wylie-Rosett J, Swencionis C, Ginsberg M, Cimino C, Wassertheil-Smoller S, Caban A, Lewis J. Computerized weight loss intervention optimizes staff time: The clinical and cost results of a controlled clinical trial. Journal of the American Diabetic Association. 2001;101:1155–1162. doi: 10.1016/s0002-8223(01)00284-x. [DOI] [PubMed] [Google Scholar]
- Yalom ID. The theory and practice for group psychotherapy. Basic Books; New York, NY: 1975. [Google Scholar]
- Yerkes RM, Dodson JD. The relation of strength of stimulus to rapidity of habit-formation. Journal of Comparative Neurology and Psychology. 1908;18:459–482. [Google Scholar]