Abstract
Background
Risk factors for alcohol problems (AP) include biological and environmental factors that are relevant across development. The pathways through which these factors are related, and how they lead to AP, are optimally considered in the context of a comprehensive developmental model.
Method
Using data from a prospectively assessed, population-based UK cohort, we constructed a structural equation model that integrated risk factors reflecting individual, family and peer/community-level constructs across childhood, adolescence and young adulthood. These variables were used to predict AP at the age of 20 years.
Results
The final model explained over 30% of the variance in liability to age 20 years AP. Most prominent in the model was an externalizing pathway to AP, with conduct problems, sensation seeking, AP at age 17.5 years and illicit substance use acting as robust predictors. In conjunction with these individual-level risk factors, familial AP, peer relationships and low parental monitoring also predicted AP. Internalizing problems were less consistently associated with AP. Some risk factors previously identified were not associated with AP in the context of this comprehensive model.
Conclusions
The etiology of young adult AP is complex, influenced by risk factors that manifest across development. The most prominent pathway to AP is via externalizing and related behaviors. These findings underscore the importance of jointly assessing both biologically influenced and environmental risk factors for AP in a developmental context.
Keywords: Alcohol problems, Avon Longitudinal Study of Parents and Children, development, externalizing pathways
Introduction
Alcohol use and problems are complex phenotypes that are influenced by both biological (e.g. genetic) and environmental factors (Goldman et al. 2005; Kendler et al. 2011b). Risk factors for the development of alcohol problems (AP) include exposures experienced during childhood, adolescence and adulthood (Prescott et al. 1997; Sher et al. 2005; Henkel, 2011); furthermore, factors at the level of the individual, the family and the peer/community environment are all relevant to risk. These factors are probably interrelated over development. Delineating the complex cascades of risk over time is critical to improving our understanding of the etiology of AP, as well as to refine programs aimed at education, prevention and early intervention.
Family history – a reflection for both genetic risk and familial–environmental risk – has been robustly associated with AP (Cloninger et al. 1981; Kendler et al. 2011b), as have childhood physical and/or sexual abuse and neglect (Kendler et al. 2000; Fergusson et al. 2013). The role of early socio-economic status (SES) is inconsistent (Hanson & Chen, 2007), potentially because the relationship might vary across different alcohol use outcomes (Kendler et al. 2014). Environmental risk factors for adolescent alcohol use include peer group deviance (Hoffmann & Bahr, 2014) and low parental monitoring (Dick et al. 2007).
Individual-level risk factors for AP have often been conceptualized as reflecting two major pathways: externalizing and internalizing (Cloninger et al. 1981; Babor et al. 1992; Del Boca & Hesselbrock, 1996; Windle & Scheidt, 2004). For example, Windle & Scheidt (2004) describe a ‘negative affect’ subtype and a ‘chronic/antisocial personality’ subtype, which are distinguished in part by their presentation of higher levels of anxiety and depression (the former subtype) v. higher levels of alcohol consumption and impairment, along with symptoms of adult antisocial behavior (the latter). The use of other substances, generally considered a manifestation of externalizing tendencies, has often been associated with AP (Babor et al. 1992; Blanco et al. 2013). This is probably due at least in part to genetic and/or environmental risk factors common to alcohol and other drug use (Kendler et al. 2011a; Wetherill et al. 2015). Personality and temperament are also indicators of risk (Sher et al. 2005): neuroticism (Prescott et al. 1997), impulsivity (McGue et al. 1997) and extraversion (Prescott et al. 1997; Kilbey et al. 1998) have all been associated with AP.
In the current study, we examine the effects of a wide variety of environmental, familial and individual-level factors on risk of early adult AP in a comprehensive longitudinal model. We utilize a large, prospectively assessed cohort from the UK where dense phenotypic information is available. Our design offers critical advantages over previous studies. While prior research has examined different aspects of the model described in the current study, few previous studies have had the opportunity to include such a wide range of potential risk/protective factors collected on a single sample. In many cases, we are also able to examine multiple measures of constructs potentially implicated in the etiology of AP, thereby determining if effects are time-specific. Another important advantage of our design is that participants are prospectively assessed, eliminating the possible risk of recall bias. Finally, the Avon Longitudinal Study of Parents and Children (ALSPAC) sample is community based, improving the likelihood of generalizability of findings, and the size of the study enables us to detect modest effect sizes, which is especially important in the context of a comprehensive model.
Method
Sample
ALSPAC is a cohort-based sample recruited in southwest England. ALSPAC recruited 14 541 pregnant women resident in Avon, UK with expected dates of delivery from 1 April 1991 to 31 December 1992; 14 541 is the initial number of pregnancies for which the mother enrolled in ALSPAC and had either returned at least one questionnaire or attended a ‘Children in Focus’ clinic by 19 July 1999. Of these initial pregnancies, there was a total of 14 676 fetuses, resulting in 14 062 live births and 13 988 children who were alive at 1 year of age. Subsequent phases of enrollment increased the sample size over time. The phases of enrollment are described in more detail in the cohort profile papers (Boyd et al. 2013; Fraser et al. 2013). For the current analyses, full or partial data were available for 9720 participants. The study website contains details of all the data that are available through a fully searchable data dictionary (http://www.bris.ac.uk/alspac/researchers/data-access/data-dictionary/). Ethical approval for the study was obtained from the ALSPAC Ethics and Law Committee and the Local Research Ethics Committees.
Measures
Other than sex, values for each predictor variable were sum scores derived from a series of individual items (see below and online Supplementary material). Where the focal individual provided non-missing responses for at least half of the items for a particular variable, a pro-rated score was calculated (exceptions noted in online Supplementary material). If necessary, variables were transformed to reduce skewness and were converted to Z-scores so that all were on a similar metric.
Outcome variables
The major outcome variable for these initial analyses was age 20 years AP, which was derived from 20 self-reported items regarding problematic alcohol use. These items and the approach to deriving scores have been previously described (Salvatore et al. 2014). Briefly, these items are from the Alcohol Use Disorders Identification Test (AUDIT), items aimed at assessing Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) alcohol dependence criteria, and additional items reflecting negative consequences due to drinking. Factor analysis in Mplus version 6.11 (Muthén & Muthén, 1998–2011) indicated that a single-factor model provided an adequate fit to the data (factor scores are provided in online Supplementary Table S1). Higher factor scores represent endorsement of a variety of alcohol-related behaviors that would be widely considered problematic, but which generally fall below diagnostic thresholds. Scores were square-root transformed and converted to Z-scores for use as outcome variables in the current analyses.
Although age 20 years AP was the major outcome variable for our model, we also included age 17.5 years AP in our model, due to the strong association between AP across ages. We reasoned that risk factors relevant to age 17.5 years AP could potentially provide critical context in the multivariate model with age years 20 AP as the final outcome. In addition, this approach allowed us to test whether some risk factors were also important in late adolescence/early adulthood or if age 20 years AP would only be predicted by age 17.5 years AP. Thus, in univariate analyses with AP at age 17.5 or age 20 years as the outcome variable, we examined the effects of predictors described below.
Predictive variables
A broad range of potentially predictive factors, many of which were assessed at multiple ages, was tested for their association with age 17.5 or age 20 years AP in univariate models; these are listed here and in Table 1. Those variables included in the final model are also described in additional detail in the online Supplementary material. Early-life/exogenous factors included maternal and paternal alcohol consumption and AP; parental SES; and parental physical or emotional cruelty.
Table 1.
Variables tested for association with age 17.5 years or age 20 years alcohol problems
| Construct | Included in final model | Not included in final model | |
|---|---|---|---|
| Exogenous/early childhood | Sex | Maternal alcohol consumption (during/after pregnancy) | |
| Maternal alcohol problems | Partner alcohol consumptiona | ||
| Partner alcohol problems | Physical/emotional cruelty toward child | ||
| Parental SES | |||
| Individual level | SDQ at 11.7 years – conduct problems subscale | SDQ at 3.9 years – total score | Religious interest at 12.75 years |
| SDQ at 11.7 years – peer problems subscale | SDQ at 6.75 years – total score | MD symptoms at 12.5 years | |
| CD at 15.5 years | SDQ at 8.1 years – total score | MD symptoms at 13.5 years | |
| MD symptoms at 16.5 years | SDQ at 9.6 years – total score | MD symptoms at 17.5 years | |
| Extraversion at 13.5 years | SDQ at 11.7 years – total score (some subscales used) | Mood at 18 years | |
| Conscientiousness at 13.5 years | ADHD at 7.6 years | Neuroticism at 13.5 years | |
| Sensation seeking at 13.5 years | CD at 8.5 years | Openness at 13.5 years | |
| Sensation seeking at 18 years | CD at 12.5 years | Agreeableness at 13.5 years | |
| Illicit substance use at 17.5 years | CD at 13.9 years | SRE at 12.5 years | |
| Illicit substance use at 18 years | Antisocial behavior at 18 years | SRE at 13.5 years | |
| Antisocial behavior at 20 years | SRE at 17.5 years | ||
| Religious interest at 9.6 years | |||
| Peer/family/social environment | PGD at 12.5 years | PGD at 10.5 years | Bullying at 8.5 years |
| PGD at 17.5 years | PM at 11.6 years | Bullying at 10.5 years | |
| PM at 12.5 years | PM at 13.5 years | Bullying at 12.5 years | |
| SLE at 17.5 years | PM at 15.5 years | Bullying at 17.5 years | |
| SLE at 8.6 years | |||
SES, Socio-economic status; SDQ, Strengths and Difficulties Questionnaire; MD, major depression; CD, conduct disorder; ADHD, attention-deficit/hyperactivity disorder; SRE, Self-Reported Effects of Alcohol; PGD, peer group deviance; PM, parental monitoring; SLE, stressful life events.
‘Partner’ refers to the focal child’s mother’s partner. At the first Avon Longitudinal Study of Parents and Children assessment, the partner was the child’s father in >99% of cases.
Peer/family/social environmental factors tested were stressful life events, parental monitoring, bullying and peer group deviance. Individual-level predictive variables included scores on the Strengths and Difficulties Questionnaire (total and/or subscales; Goodman et al. 2000); symptoms of attention-deficit/hyperactivity disorder; symptoms of conduct disorder and antisocial behavior; religious interest; symptoms of major depression; personality constructs from the International Personality Item Pool (Ehrhart et al. 2008), which included openness, agreeableness, conscientiousness, neuroticism and extraversion; a modified version of Arnett’s Inventory of Sensation Seeking (Arnett, 1994); scores on the Self-Rating of the Effects of Alcohol (SRE) questionnaire (Schuckit et al. 1997); and illicit substance use.
Predictive variables were based on self-reports, maternal reports and maternal partner reports; as described in the online Supplementary material, the measures of parental AP were based on multiple reporters. Variables were prospectively assessed; see Table 1 for average age at assessment.
Statistical modeling
Predictive variables from the initial univariate analyses were retained for inclusion in the first iteration of the multivariable structural equation model if they were associated with the outcome at p < 0.05. In the multivariate model, variables were arranged as follows. Early-life/exogenous variables were ordered first (earliest) in the model. All other variables were placed in the model in order of their age of measurement. After the variable order was established, we constructed a saturated model where each upstream variable had paths to all downstream variables. We then sequentially pruned paths from the model as follows. First, starting from the top down, we removed all variables with p values greater than 0.5 (for the null hypothesis that the ‘true’ value of the path was zero). We then performed a second pass removing all with p values greater than 0.2. Similar iterations were performed of p values of 0.1, 0.05, and 0.01.
We next pruned based on standardized path coefficients to determine which paths to set to 0. First, we removed all paths with effect sizes less than 0.05. This was repeated using 0.06, and finally 0.071 (which corresponds to 0.5% of the variance) as minimum standardized path coefficients. Thus all paths that remain in the final model have p values less than 0.01 and contributed to at least 0.5% of the variance in the dependent variable. By using this approach we were able to obtain a final model that was simplified as much as possible without seriously degrading model fit or loss of explanatory power for the outcome variables of interest.
To deal with problems of missing data, models were fit with maximum likelihood. Thus we are operating under the assumption that missing values are missing at random. Under this assumption, we assume that missing values come from the same covariance matrix as the observed values so that missing values are ‘predictable’ (with a measurable level of uncertainty) from the observed variables for the proband.
Results
Model fitting
Model fitting resulted in a final model with acceptable fit (comparative fit index = 0.968, Tucker–Lewis index = 0.948) that explained 30.7% of the total variance of age 20 years AP, and 30.6% of the total variance of age 17.5 years AP. The model-fitting process resulted in the exclusion of many potential predictors, including parental cruelty, childhood physical abuse, scores on the SRE scale, and all but one measure of internalizing problems. Variables retained in the final model are described below and listed in Table 1, which also lists variables that did not meet inclusion criteria for the final model. Table 2 provides total and indirect effect sizes between each predictor and AP at age 17.5 and age 20 years. We focus on the association between risk factors and age 20 years AP below, as that was the primary outcome of interest.
Table 2.
Standardized total and indirect effects on age 17.5 years and age 20 years APa
| Age 17.5 years (maximum n = 3422) |
Age 20 years (maximum n = 3598) |
|||||
|---|---|---|---|---|---|---|
| Predictor variable | n | Total standardized effect |
Indirect standardized effect |
Total standardized effect |
Indirect standardized effect |
Primary mediation paths for age 20 years AP |
| Sex | 8121 | 0.046 | 0.046 | 0.082 | 0.082 | SS 13 years 6 months, SS 18 years |
| Parental SES | 8121 | −0.024 | −0.024 | 0.138 | −0.003 | – |
| Paternal AP | 8121 | 0.099 | 0 | 0.115 | 0.044 | AP 17 years 6 months |
| Maternal AP | 8121 | 0.022 | 0.022 | 0.013 | 0.013 | – |
| Conduct problems 11 years 8 months | 6598 | 0.045 | 0.045 | 0.031 | 0.031 | – |
| Good peer relationships 11 years 8 months | 6602 | 0.101 | 0.014 | 0.047 | 0.047 | AP 17 years 6 months |
| Low parental monitoring 12 years months | 4882 | 0.13 | 0.13 | 0.090 | 0.090 | SS 13 years 6 months, SS 18 years |
| PGD 12 years 8 months | 5781 | 0.161 | 0.161 | 0.098 | 0.098 | CD – AP 17 years 6 months, PGD 17 years 6 months – AP 17 years 6 months |
| Extraversion 13 years months | 5283 | 0.128 | 0.044 | 0.078 | 0.078 | AP 17 years 6 months |
| Low conscientiousness 13 years 6 months | 5264 | 0.097 | 0.097 | 0.065 | 0.065 | SS 13 years 6 months, SS 18 years |
| SS 13 years 6 months | 5281 | 0.102 | 0.102 | 0.130 | 0.130 | SS 18 years |
| CD 15 years 6 months | 4707 | 0.286 | 0.15 | 0.146 | 0.146 | AP 17 years 6 months, PGD17 years 6 months – AP 17 years 6 months |
| Major depression symptoms 16 years 6 months | 4534 | 0.066 | 0.066 | 0.035 | 0.035 | PGD17 years 6 months – AP 17 years 6 months |
| PGD 17 years 6 months | 3310 | 0.341 | 0.12 | 0.187 | 0.187 | AP 17 years 6 months, ISU 17 years 6 months – AP 17 years 6 months |
| Stressful life events 17 years 6 months | 3947 | 0.108 | 0.025 | 0.055 | 0.055 | AP 17 years 6 months |
| ISU 17 years 6 months | 3591 | 0.254 | n/a | 0.185 | 0.185 | AP 17 years 6 months, ISU 18 years |
| AP 17 years 6 months | 3422 | n/a | n/a | 0.442 | 0.027 | SS 18 years |
| SS 18 years | 2954 | n/a | n/a | 0.161 | 0.009 | ISU 18 years |
| ISU 18 years | 3018 | n/a | n/a | 0.096 | – | n.a. |
AP, Alcohol problems; SS, sensation seeking; SES, socio-economic status; PGD, peer group deviance; CD, conduct disorder; ISU, illicit substance use; n.a., not applicable.
Where appropriate, the most pronounced mediation paths between predictors and age 20 years AP are described.
Early-life predictors
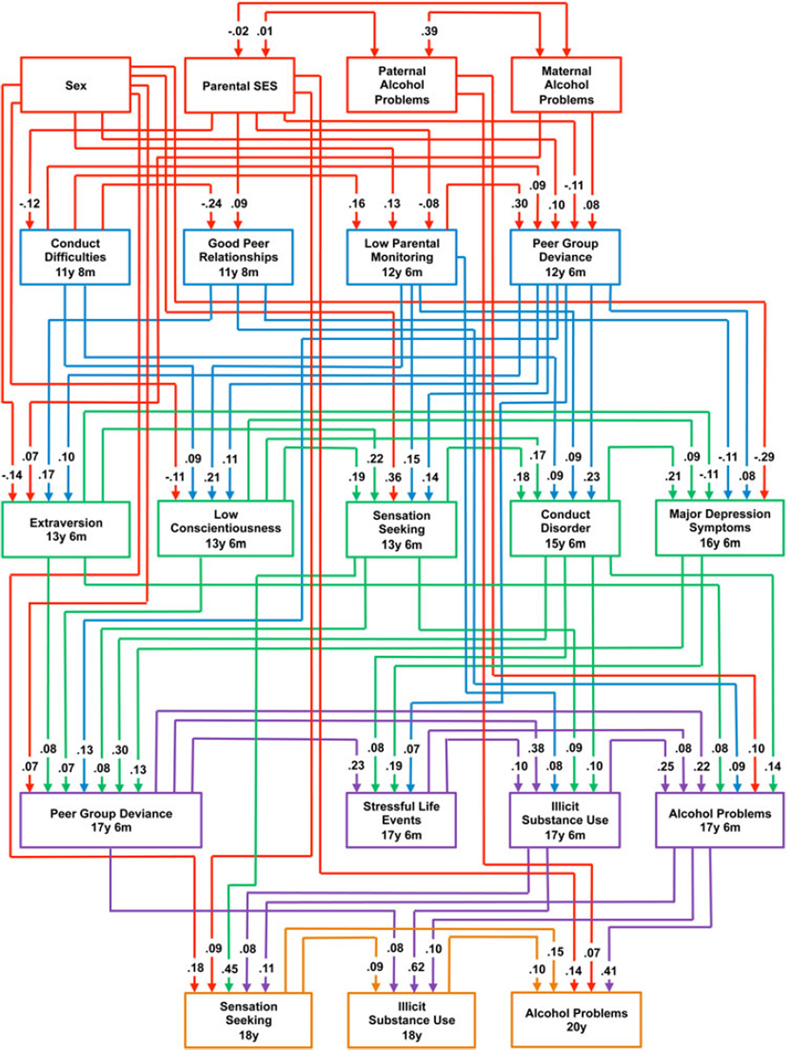
Four exogenous or early-life predictors (sex, parental SES, paternal AP and maternal AP) remained in the final model (Fig. 1). Of these, paternal AP and parental SES had direct effects on AP at age 20 years, which accounted for 62% and 98% of their total effect sizes, respectively (Table 2). Men were more likely to have AP than women, as were participants with higher parental SES.
Fig. 1.
Final full model with standardized path estimates. Variables and their corresponding paths are color-coded by approximate developmental time-frame. SES, Socio-economic status; y, years; m, months.
Other variables measured prior to the age of 13 years that remained in the final model were conduct problems, positive peer relationships, low parental monitoring and peer deviance. Positive peer relationships were associated with greater AP; higher levels of conduct problems and peer deviance, and lower levels of parental monitoring predicted higher levels of AP. The effect size of this early measure of conduct problems, an individual-level factor, was lower than those of the familial/peer environment measures.
In mid-adolescence (ages 13–16.5 years), only individual-level variables were predictive of AP in the final model. The personality constructs of extraversion and low conscientiousness, sensation seeking, and symptoms of major depression and conduct disorder were all positively associated with AP.
In late adolescence (age 17.5 years and older), both individual-level and environmental variables were predictive of age 20 years AP. Peer group deviance and stressful life events were positively associated with the outcome, with the former having a reasonably large effect size. Age 17.5 years AP and illicit substance use also predicted age 20 years AP. As expected, the former was by far the strongest predictor in the model: it had the highest effect size of any predictor, and only 6% of the effect was indirect. Finally, two individual-level variables assessed at age 18 years, sensation seeking and illicit substance use, were associated with age 20 years AP.
As shown in Table 2, nearly all variables’ effects were mediated to some extent. Indeed, only five (of 19) predictors in the final model had a direct effect on age 20 years AP: higher parental SES, paternal AP, age 17.5 years AP, and age 18 years sensation seeking and illicit substance use (only direct effects were possible for the last two). Primary mediators included conduct problems, peer group deviance and the predictors most temporally proximal to age 20 years AP.
Discussion
This report describes a comprehensive developmental model delineating the complex pathways leading to early adult AP. Our use of a large, longitudinal population-based cohort, densely assessed across 20 years for a broad range of risk factors, represents a substantial advance over previous studies that have been limited by sample size, scope and/or reliance on retrospective reporting. Our results provide important insight to the contextual effects of environmental and individual risk factors for AP. The final model accounted for over 30% of the variance in age 20 years AP, a figure comparable with several previous studies of older adults (Dubow et al. 2008; Pitkanen et al. 2008; Kendler et al. 2011b), and higher than a model of adult alcohol consumption in a British sample (Maggs et al. 2008). Below, we detail our most noteworthy findings.
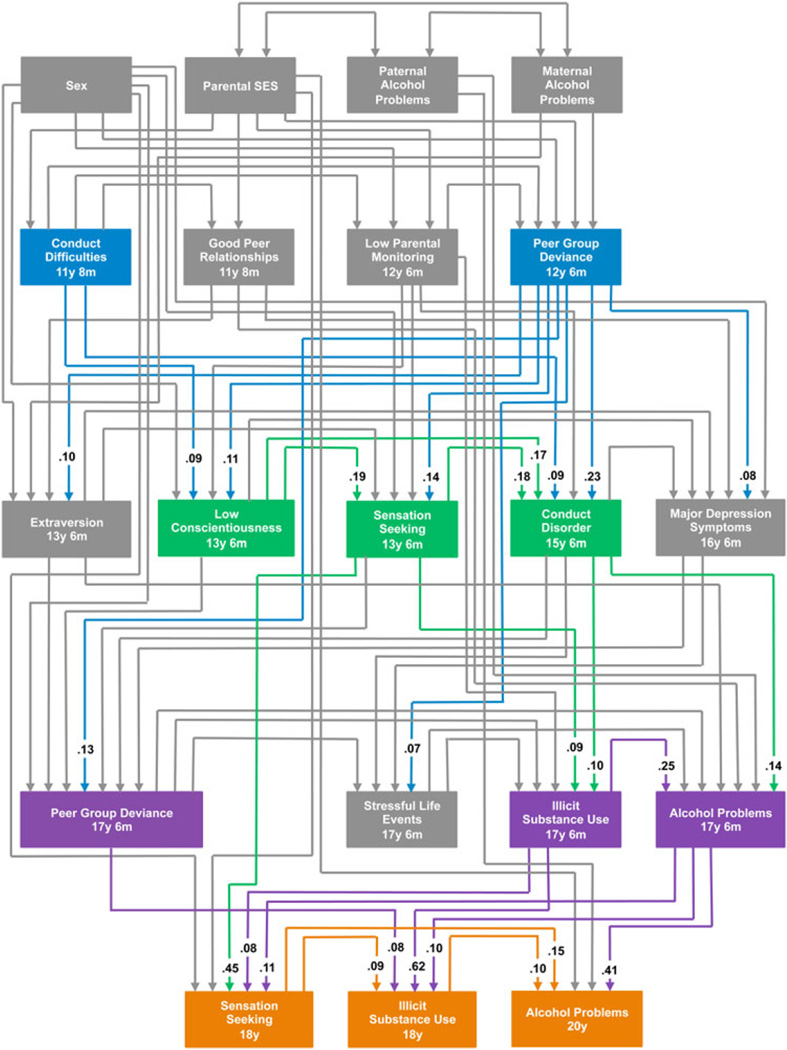
First, we found strong evidence of a developmental externalizing pathway to AP (Fig. 2), beginning in early adolescence with conduct difficulties at age 11 years 8 months and peer deviance at 12.5 years. This continues into the mid- to late-teen years as exemplified by low conscientiousness (age 13.5 years), sensation seeking (ages 13.5 and 18 years), subsequent conduct problems (age 15.5 years), and substance use (ages 17.5 and 18 years). In addition, conduct problems and sensation seeking are prominent mediators of many other predictors. These results are consistent with prior reports of associations between externalizing problems and alcohol use/AP (Hesselbrock & Hesselbrock, 2006; Fergusson et al. 2007; Pardini et al. 2007; Zucker, 2008; Whelan et al. 2014), including in some (but not all; Copeland et al. 2012) samples that have been longitudinally assessed (McGue & Iacono, 2008; Hicks et al. 2014), and studies that have used the current sample (Heron et al. 2013; Kendler et al. 2013). These individual-level externalizing problems mediate, and are mediated by, low parental monitoring and peer group deviance, similar to previous reports (Patterson et al. 1989; Steinberg et al. 1994; Hussong, 2002; Nash et al. 2005). Critically, we provide evidence that this externalizing pathway is robust to the inclusion of a wide variety of other risk factors, thereby demonstrating its unique predictive ability.
Fig. 2.
Variables falling under the rubric of ‘externalizing’ are highlighted (with other variables in gray), along with the corresponding path estimates, to illustrate the externalizing pathway from early adolescence to age 20 years alcohol problems. SES, Socio-economic status; y, years; m, months.
Second, we observe a strong, and almost entirely direct, relationship between AP at age 17.5 years and age 20 years. Thus, understanding risk for late adolescent AP is quite informative for predicting risk for age 20 years AP. However, it is not sufficient: not only do factors assessed at age 18 years (sensation seeking and illicit substance use) have substantial effects on age 20 years AP, but some earlier risk factors’ primary mediation paths do not principally involve age 17.5 years AP. This demonstrates that, despite the fact that adolescent AP is considered a robust risk factor for problems in adulthood (McCambridge et al. 2011), the developmental pathways leading to AP extend beyond late adolescence. This finding has potential implications for prevention efforts, in that it reveals that preventing problems at the age of 17.5 years does not entirely mitigate risk for later problems.
Third, we demonstrate that effects of sex and the early-life influences of parental SES and paternal AP are persistent, making an impact on early adult AP via both direct and indirect paths. We conducted post-hoc multi-group analyses to further investigate the potential effect of sex. In those analyses, the sexes were modeled separately and we tested whether parameter estimates differed significantly across sex; results indicated that they did not. Thus although males are more likely to develop AP, our results suggest that pathways to AP are consistent across the sexes. A previous study using this sample reported a complex relationship between parental SES and alcohol outcomes at the ages of 16 and 18 years (Kendler et al. 2014); the current results, in which the direction and magnitude of effect differ for age 18 years and age 20 years AP, further confirm that the association is nuanced. Previous work suggests that higher parental SES confers easier access to alcohol among adolescents, thereby acting as a risk factor for misuse (Richter et al. 2006; Humensky, 2010), though not all studies support this hypothesis (Lowry et al. 1996; Lemstra et al. 2008).
Maternal AP are a much less robust risk factor than paternal problems. Findings from previous studies have been inconsistent with respect to the impact of paternal v. maternal drinking problems (e.g. Bohman et al. 1981; Cloninger et al. 1981). In less extensive models examining the relationship between parental and offspring AP in the current sample, parent-specific effects were less discrepant (Kendler et al. 2013), raising the possibility that the true effects of parental AP must be considered through the lens of comprehensive developmental models such as that described here. These results warrant follow-up.
Fourth, despite previous reports of an ‘internalizing subtype’ of AP (Del Boca & Hesselbrock, 1996; Hesselbrock & Hesselbrock, 2006), we found only modest evidence of such a pathway. Despite the examination of multiple measures of internalizing symptoms, across various ages, only age 16 years 6 months symptoms of major depression was retained in the final model. Previous studies of the ALSPAC sample have demonstrated a positive relationship between internalizing problems and alcohol misuse (Edwards et al. 2014), but those effects apparently diminish in the context of externalizing-related predictors. Studies in other samples have also demonstrated more extensive positive relationships between various manifestations of internalizing problems and AP (Prescott et al. 1997; Kendler et al. 2011b; Mezquita et al. 2014). Notably, those studies have focused on samples that are generally older than the ALSPAC sample, which might contribute to the observed inconsistencies.
Additional risk factors were peripheral to the central externalizing pathway to AP. Positive peer relationships, assessed at age 11.7 years, could confer risk by increasing exposure or access to alcohol, given that alcohol use during this period frequently occurs within the context of peer groups (Hussong, 2000, 2002). Similarly, the positive association between extraversion and AP could be related to peer interactions, as has been demonstrated in previous research (Knyazev, 2004). We also note that stressful life events, which were assessed at age 17.5 years, were predictive of AP. The events included in this scale range from a death in the family to academic problems to problems with parents; future analyses might examine whether specific events are riskier or whether the accumulation of stressors is more important, regardless of the nature of those events.
Finally, we note that a number of previously implicated AP risk factors were not supported in the current model. Childhood abuse and neglect were insufficiently predictive of AP to warrant inclusion in the final model, contrary to previous studies’ reports of their relationship with AP (Herrenkohl et al. 2013; La Flair et al. 2013; Mezquita et al. 2014; Potthast et al. 2014). We also found no support for a unique relationship between scores on the SRE scale and AP, despite evidence that SRE scores are related to earlier drinking measures and peer drinking in this sample (Schuckit et al. 2008a, b). Furthermore, in many cases only one assessment of a given risk factor was included in the final model – e.g. conduct disorder at 15.5 years was included, but not at the ages of 8.5, 12.5 or 13.9 years (see Table 1). Similarly, antisocial behavior at ages 18 and 20 years was not included in the final model. These exclusions are possibly due to the close relationships among these variables and those that were included in the final model (e.g. conduct problems, low conscientiousness, sensation seeking, illicit drug use), largely rendering the excluded variables redundant.
Limitations
The findings reported here should be considered in light of several limitations. First, the ALSPAC sample is relatively young and not yet through the risk period for the development of AP. Some individuals will develop such problems later in life via pathways distinct from those observed here. Indeed, the internalizing subtype of AP probably has a later onset (Del Boca & Hesselbrock, 1996), potentially explaining why support for an internalizing pathway to AP was limited in this young sample. Accordingly, later waves of data collection may reveal other diverse pathways of risk. In addition, drinking behaviors could differ between US and UK populations, particularly given the earlier legal drinking age in the UK; thus these results warrant replication in a US sample.
In some cases, our modeling approach was limited by the availability of variables at different ages. For example, personality characteristics are evident prior to the available measure at age 13.5 years, and might actually influence conduct difficulties at age 11.7 years. Furthermore, our model-trimming approach involved excluding measures based on their predictive power, rather than on the age at assessment. Thus, although symptoms of major depression were assessed at age 12.5 years, they did not strongly predict risk until later in adolescence, so only the later measure was retained. We do not intend to imply that the risk pathway cannot begin prior to the appearance of each factor in the final model. Despite these idiosyncrasies of model fitting, a shift in ordering of these factors in the model would be unlikely to dramatically make an impact on the substantive findings of the study, i.e. an externalizing pathway to AP would probably remain evident.
Our AP outcome is not a diagnostic measure. However, age 20 years AP is strongly correlated with age 20 years alcohol dependence symptom count (r = 0.65, p < 0.0001) and with an age 20 years alcohol dependence diagnosis (r = 0.46, p < 0.001), suggesting that our measure of AP is a useful indicator of clinical risk. Attrition in the ALSPAC sample is of some concern, though we have made an effort to address this by using maximum likelihood in our modeling. In addition, we conducted tests to determine whether parameter estimates changed substantially if individuals were weighted based on parental SES (which was predictive of attrition), and found only minimal shifts, with increases in effect size being more common than decreases. Thus, we are confident that the biases in results reported due to attrition are modest. Finally, different approaches to modeling are possible and could lead to varying conclusions. For example, we tested related predictors (e.g. conduct problems/ antisocial behavior) independently rather than as trajectories, in part due to inconsistencies in assessment items over time. In addition, our structural equation model assumes that the predictor variables act additively and linearly in their impact on AP, which in some cases may be unrealistic.
Conclusions
In summary, using a prospective sample densely assessed from birth to the age of 20 years, our comprehensive developmental model indicates that factors at the level of the family environment, social environment and individual combine to influence risk to early adult AP. Early-life factors, such as parental AP and SES, have long-lasting effects on AP. In early adolescence, an externalizing pathway to AP is initiated, which involves conduct problems, association with deviant peers, sensation seeking and illicit substance use. The lack of evidence for several previously implicated risk factors merits additional study in the current sample as well as replication in other samples using comparable methods.
The multifactorial nature of these predictors, and in particular the predictive utility of extrinsic factors such as parental SES and peer group deviance, indicates that reductive biological models will fail to sufficiently explain developmental risk for AP. Rather, consistent with findings from twin and family studies indicating that approximately half the variance in AP is due to genetic factors (Verhulst et al. 2015), the model described here provides support for the importance of both biologically influenced, individual-level factors (e.g. personality constructs, psychopathology) and environmental factors, which affect risk through complex and intertwined relationships. To further understand the etiology of AP, both domains must be considered jointly.
Supplementary Material
Acknowledgments
This research was specifically funded by the National Institutes of Health – National Institute on Alcohol Abuse and Alcoholism (A.C.E., AA021399; K.S.K, AA018333, 1P50AA022537 and R37AA011408). The UK Medical Research Council and the Wellcome Trust (grant reference 092731) and the University of Bristol provide core support for ALSPAC. This publication is the work of the authors and A.C.E. will serve as guarantor for the contents of this paper.
We are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses.
Footnotes
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S0033291715002457
Declaration of Interest
None.
References
- Arnett J. Sensation seeking – a new conceptualization and a new scale. Personality and Individual Differences. 1994;16:289–296. [Google Scholar]
- Babor TF, Hofmann M, DelBoca FK, Hesselbrock V, Meyer RE, Dolinsky ZS, Rounsaville B. Types of alcoholics, I. Evidence for an empirically derived typology based on indicators of vulnerability and severity. Archives of General Psychiatry. 1992;49:599–608. doi: 10.1001/archpsyc.1992.01820080007002. [DOI] [PubMed] [Google Scholar]
- Blanco C, Krueger RF, Hasin DS, Liu SM, Wang S, Kerridge BT, Saha T, Olfson M. Mapping common psychiatric disorders: structure and predictive validity in the national epidemiologic survey on alcohol and related conditions. JAMA Psychiatry. 2013;70:199–208. doi: 10.1001/jamapsychiatry.2013.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohman M, Sigvardsson S, Cloninger CR. Maternal inheritance of alcohol abuse. Cross-fostering analysis of adopted women. Archives of General Psychiatry. 1981;38:965–969. doi: 10.1001/archpsyc.1981.01780340017001. [DOI] [PubMed] [Google Scholar]
- Boyd A, Golding J, Macleod J, Lawlor DA, Fraser A, Henderson J, Molloy L, Ness A, Ring S, Davey Smith G. Cohort profile: the ‘children of the 90s’ – the index offspring of the Avon Longitudinal Study of Parents and Children. International Journal of Epidemiology. 2013;42:111–127. doi: 10.1093/ije/dys064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloninger CR, Bohman M, Sigvardsson S. Inheritance of alcohol abuse. Cross-fostering analysis of adopted men. Archives of General Psychiatry. 1981;38:861–868. doi: 10.1001/archpsyc.1981.01780330019001. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Angold A, Shanahan L, Dreyfuss J, Dlamini I, Costello EJ. Predicting persistent alcohol problems: a prospective analysis from the Great Smoky Mountain Study. Psychological Medicine. 2012;42:1925–1935. doi: 10.1017/S0033291711002790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Boca FK, Hesselbrock V. Gender and alcoholic subtypes. Alcohol Health and Research World. 1996;20:56–62. [PMC free article] [PubMed] [Google Scholar]
- Dick DM, Pagan JL, Viken R, Purcell S, Kaprio J, Pulkkinen L, Rose RJ. Changing environmental influences on substance use across development. Twin Research and Human Genetics. 2007;10:315–326. doi: 10.1375/twin.10.2.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubow EF, Boxer P, Huesmann LR. Childhood and adolescent predictors of early and middle adulthood alcohol use and problem drinking: the Columbia County Longitudinal Study. Addiction. 2008;103(Suppl. 1):36–47. doi: 10.1111/j.1360-0443.2008.02175.x. [DOI] [PubMed] [Google Scholar]
- Edwards AC, Joinson C, Dick DM, Kendler KS, Macleod J, Munafo M, Hickman M, Lewis G, Heron J. The association between depressive symptoms from early to late adolescence and later use and harmful use of alcohol. European Child and Adolescent Psychiatry. 2014;23:1219–1230. doi: 10.1007/s00787-014-0600-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrhart KH, Roesch SC, Ehrhart MG, Kilian B. A test of the factor structure equivalence of the 50-item IPIP Five-factor model measure across gender and ethnic groups. Journal of Personality Assessment. 2008;90:507–516. doi: 10.1080/00223890802248869. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM. Conduct and attentional problems in childhood and adolescence and later substance use, abuse and dependence: results of a 25-year longitudinal study. Drug and Alcohol Dependence. 2007;88(Suppl. 1):S14–S26. doi: 10.1016/j.drugalcdep.2006.12.011. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, McLeod GF, Horwood LJ. Childhood sexual abuse and adult developmental outcomes: findings from a 30-year longitudinal study in New Zealand. Child Abuse and Neglect. 2013;37:664–674. doi: 10.1016/j.chiabu.2013.03.013. [DOI] [PubMed] [Google Scholar]
- Fraser A, Macdonald-Wallis C, Tilling K, Boyd A, Golding J, Davey Smith G, Henderson J, Macleod J, Molloy L, Ness A, Ring S, Nelson SM, Lawlor DA. Cohort profile: the Avon Longitudinal Study of Parents and Children: ALSPAC mothers cohort. International Journal of Epidemiology. 2013;42:97–110. doi: 10.1093/ije/dys066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman D, Oroszi G, Ducci F. The genetics of addictions: uncovering the genes. Nature Reviews: Genetics. 2005;6:521–532. doi: 10.1038/nrg1635. [DOI] [PubMed] [Google Scholar]
- Goodman R, Ford T, Simmons H, Gatward R, Meltzer H. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. British Journal of Psychiatry. 2000;177:534–539. doi: 10.1192/bjp.177.6.534. [DOI] [PubMed] [Google Scholar]
- Hanson MD, Chen E. Socioeconomic status and health behaviors in adolescence: a review of the literature. Journal of Behavioral Medicine. 2007;30:263–285. doi: 10.1007/s10865-007-9098-3. [DOI] [PubMed] [Google Scholar]
- Henkel D. Unemployment and substance use: a review of the literature (1990–2010) Current Drug Abuse Reviews. 2011;4:4–27. doi: 10.2174/1874473711104010004. [DOI] [PubMed] [Google Scholar]
- Heron J, Maughan B, Dick DM, Kendler KS, Lewis G, Macleod J, Munafo M, Hickman M. Conduct problem trajectories and alcohol use and misuse in mid to late adolescence. Drug and Alcohol Dependence. 2013;133:100–107. doi: 10.1016/j.drugalcdep.2013.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrenkohl TI, Hong S, Klika JB, Herrenkohl RC, Russo MJ. Developmental impacts of child abuse and neglect related to adult mental health, substance use, and physical health. Journal of Family Violence. 2013;28 doi: 10.1007/s10896-012-9474-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesselbrock VM, Hesselbrock MN. Are there empirically supported and clinically useful subtypes of alcohol dependence? Addiction. 2006;101(Suppl. 1):97–103. doi: 10.1111/j.1360-0443.2006.01596.x. [DOI] [PubMed] [Google Scholar]
- Hicks BM, Iacono WG, McGue M. Identifying childhood characteristics that underlie premorbid risk for substance use disorders: socialization and boldness. Development and Psychopathology. 2014;26:141–157. doi: 10.1017/S0954579413000862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann JP, Bahr SJ. Parenting style, religiosity, peer alcohol use, and adolescent heavy drinking. Journal of Studies on Alcohol and Drugs. 2014;75:222–227. doi: 10.15288/jsad.2014.75.222. [DOI] [PubMed] [Google Scholar]
- Humensky JL. Are adolescents with high socioeconomic status more likely to engage in alcohol and illicit drug use in early adulthood? Substance Abuse Treatment, Prevention, and Policy. 2010;5:19. doi: 10.1186/1747-597X-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM. The settings of adolescent alcohol and drug use. Journal of Youth and Adolescence. 2000;29:107–119. [Google Scholar]
- Hussong AM. Differentiating peer contexts and risk for adolescent substance use. Journal of Youth and Adolescence. 2002;31:207–220. [Google Scholar]
- Kendler KS, Aggen SH, Knudsen GP, Roysamb E, Neale MC, Reichborn-Kjennerud T. The structure of genetic and environmental risk factors for syndromal and subsyndromal common DSM-IV Axis I and all Axis II disorders. American Journal of Psychiatry. 2011a;168:29–39. doi: 10.1176/appi.ajp.2010.10030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Bulik CM, Silberg J, Hettema JM, Myers J, Prescott CA. Childhood sexual abuse and adult psychiatric and substance use disorders in women: an epidemiological and cotwin control analysis. Archives of General Psychiatry. 2000;57:953–959. doi: 10.1001/archpsyc.57.10.953. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Edwards A, Hickman M, Heron J, Macleod J, Lewis G, Dick DM. Dimensions of parental alcohol use/problems and offspring temperament, externalizing behaviors, and alcohol use/problems. Alcoholism, Clinical and Experimental Research. 2013;37:2118–2127. doi: 10.1111/acer.12196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Hickman M, Heron J, Macleod J, Lewis G, Dick DM. Socioeconomic status and alcohol-related behaviors in mid- to late adolescence in the Avon Longitudinal Study of Parents and Children. Journal of Studies on Alcohol and Drugs. 2014;75:541–545. doi: 10.15288/jsad.2014.75.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for alcohol use disorders in men. Twin Research and Human Genetics. 2011b;14:1–15. doi: 10.1375/twin.14.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilbey MM, Downey K, Breslau N. Predicting the emergence and persistence of alcohol dependence in young adults: the role of expectancy and other risk factors. Experimental and Clinical Psychopharmacology. 1998;6:149–156. doi: 10.1037//1064-1297.6.2.149. [DOI] [PubMed] [Google Scholar]
- Knyazev GG. Behavioural activation as predictor of substance use: mediating and moderating role of attitudes and social relationships. Drug and Alcohol Dependence. 2004;75:309–321. doi: 10.1016/j.drugalcdep.2004.03.007. [DOI] [PubMed] [Google Scholar]
- La Flair LN, Reboussin BA, Storr CL, Letourneau E, Green KM, Mojtabai R, Pacek LR, Alvanzo AA, Cullen B, Crum RM. Childhood abuse and neglect and transitions in stages of alcohol involvement among women: a latent transition analysis approach. Drug and Alcohol Dependence. 2013;132:491–498. doi: 10.1016/j.drugalcdep.2013.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemstra M, Bennett NR, Neudorf C, Kunst A, Nannapaneni U, Warren LM, Kershaw T, Scott CR. A meta-analysis of marijuana and alcohol use by socio-economic status in adolescents aged 10–15 years. Canadian Journal of Public Health. Revue Canadienne de Santé Publique. 2008;99:172–177. doi: 10.1007/BF03405467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowry R, Kann L, Collins JL, Kolbe LJ. The effect of socioeconomic status on chronic disease risk behaviors among US adolescents. JAMA. 1996;276:792–797. [PubMed] [Google Scholar]
- Maggs JL, Patrick ME, Feinstein L. Childhood and adolescent predictors of alcohol use and problems in adolescence and adulthood in the National Child Development Study. Addiction. 2008;103(Suppl. 1):7–22. doi: 10.1111/j.1360-0443.2008.02173.x. [DOI] [PubMed] [Google Scholar]
- McCambridge J, McAlaney J, Rowe R. Adult consequences of late adolescent alcohol consumption: a systematic review of cohort studies. PLoS Medicine. 2011;8:e1000413. doi: 10.1371/journal.pmed.1000413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGue M, Iacono WG. The adolescent origins of substance use disorders. International Journal of Methods in Psychiatric Research. 2008;17(Suppl. 1):S30–S38. doi: 10.1002/mpr.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGue M, Slutske W, Taylor J, Iacono WG. Personality and substance use disorders: I. Effects of gender and alcoholism subtype. Alcoholism, Clinical and Experimental Research. 1997;21:513–520. [PubMed] [Google Scholar]
- Mezquita L, Ibanez MI, Moya J, Villa H, Ortet G. A longitudinal examination of different etiological pathways to alcohol use and misuse. Alcoholism, Clinical and Experimental Research. 2014;38:1770–1779. doi: 10.1111/acer.12419. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 6th. Los Angeles, CA: Muthén & Muthén; 1998–2011. [Google Scholar]
- Nash SG, McQueen A, Bray JH. Pathways to adolescent alcohol use: family environment, peer influence, and parental expectations. Journal of Adolescent Health. 2005;37:19–28. doi: 10.1016/j.jadohealth.2004.06.004. [DOI] [PubMed] [Google Scholar]
- Pardini D, White HR, Stouthamer-Loeber M. Early adolescent psychopathology as a predictor of alcohol use disorders by young adulthood. Drug and Alcohol Dependence. 2007;88(Suppl. 1):S38–S49. doi: 10.1016/j.drugalcdep.2006.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson GR, DeBaryshe BD, Ramsey E. A developmental perspective on antisocial behavior. American Psychologist. 1989;44:329–335. doi: 10.1037//0003-066x.44.2.329. [DOI] [PubMed] [Google Scholar]
- Pitkanen T, Kokko K, Lyyra AL, Pulkkinen L. A developmental approach to alcohol drinking behaviour in adulthood: a follow-up study from age 8 to age 42. Addiction. 2008;103(Suppl. 1):48–68. doi: 10.1111/j.1360-0443.2008.02176.x. [DOI] [PubMed] [Google Scholar]
- Potthast N, Neuner F, Catani C. The contribution of emotional maltreatment to alcohol dependence in a treatment-seeking sample. Addictive Behaviors. 2014;39:949–958. doi: 10.1016/j.addbeh.2014.01.015. [DOI] [PubMed] [Google Scholar]
- Prescott CA, Neale MC, Corey LA, Kendler KS. Predictors of problem drinking and alcohol dependence in a population-based sample of female twins. Journal of Studies on Alcohol. 1997;58:167–181. doi: 10.15288/jsa.1997.58.167. [DOI] [PubMed] [Google Scholar]
- Richter M, Leppin A, Nic Gabhainn S. The relationship between parental socio-economic status and episodes of drunkenness among adolescents: findings from a cross-national survey. BMC Public Health. 2006;6:289. doi: 10.1186/1471-2458-6-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvatore J, Aliev F, Edwards A, Evans D, Macleod J, Hickman M, Lewis G, Kendler K, Loukola A, Korhonen T, Latvala A, Rose R, Kaprio J, Dick D. Polygenic scores predict alcohol problems in an independent sample and show moderation by the environment. Genes. 2014;5:330–346. doi: 10.3390/genes5020330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuckit MA, Smith TL, Tipp JE. The Self-Rating of the Effects of Alcohol (SRE) form as a retrospective measure of the risk for alcoholism. Addiction. 1997;92:979–988. [PubMed] [Google Scholar]
- Schuckit MA, Smith TL, Trim R, Heron J, Horwood J, Davis JM, Hibbeln JR Team AS. The performance of elements of a ‘level of response to alcohol’-based model of drinking behaviors in 13-year-olds. Addiction. 2008a;103:1786–1792. doi: 10.1111/j.1360-0443.2008.02325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuckit MA, Smith TL, Trim RS, Heron J, Horwood J, Davis J, Hibbeln J Team AS. The Self-Rating of the Effects Of Alcohol Questionnaire as a predictor of alcohol-related outcomes in 12-year-old subjects. Alcohol and Alcoholism. 2008b;43:641–646. doi: 10.1093/alcalc/agn077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher KJ, Grekin ER, Williams NA. The development of alcohol use disorders. Annual Review of Clinical Psychology. 2005;1:493–523. doi: 10.1146/annurev.clinpsy.1.102803.144107. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Fletcher A, Darling N. Parental monitoring and peer influences on adolescent substance use. Pediatrics. 1994;93:1060–1064. [PubMed] [Google Scholar]
- Verhulst B, Neale MC, Kendler KS. The heritability of alcohol use disorders: a meta-analysis of twin and adoption studies. Psychological Medicine. 2015;45:1061–1072. doi: 10.1017/S0033291714002165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetherill L, Agrawal A, Kapoor M, Bertelsen S, Bierut LJ, Brooks A, Dick D, Hesselbrock M, Hesselbrock V, Koller DL, Le N, Nurnberger JI, Jr, Salvatore JE, Schuckit M, Tischfield JA, Wang JC, Xuei X, Edenberg HJ, Porjesz B, Bucholz K, Goate AM, Foroud T. Association of substance dependence phenotypes in the COGA sample. Addiction Biology. 2015;20:617–627. doi: 10.1111/adb.12153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whelan R, Watts R, Orr CA, Althoff RR, Artiges E, Banaschewski T, Barker GJ, Bokde AL, Buchel C, Carvalho FM, Conrod PJ, Flor H, Fauth-Buhler M, Frouin V, Gallinat J, Gan G, Gowland P, Heinz A, Ittermann B, Lawrence C, Mann K, Martinot JL, Nees F, Ortiz N, Paillere-Martinot ML, Paus T, Pausova Z, Rietschel M, Robbins TW, Smolka MN, Strohle A, Schumann G, Garavan H IMAGEN Consortium. Neuropsychosocial profiles of current and future adolescent alcohol misusers. Nature. 2014;512:185–189. doi: 10.1038/nature13402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windle M, Scheidt DM. Alcoholic subtypes: are two sufficient? Addiction. 2004;99:1508–1519. doi: 10.1111/j.1360-0443.2004.00878.x. [DOI] [PubMed] [Google Scholar]
- Zucker RA. Anticipating problem alcohol use developmentally from childhood into middle adulthood: what have we learned? Addiction. 2008;103(Suppl. 1):100–108. doi: 10.1111/j.1360-0443.2008.02179.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.