Abstract
Background and Objective:
The present study retrospectively analyzed the data of 213 patients who underwent laparoscopic ureterolithotomy.
Methods:
We retrospectively analyzed the data of 213 patients, in whom we performed conventional laparoscopic ureterolithotomy from April 2006 and January 2015 based on the diagnosis of an upper or middle ureteral stone. Patients with large ureteral stones (>15 mm) or a history of failed shock-wave lithotripsy or ureteroscopy were included in the study. Although the retroperitoneal approach was preferred for 170 patients, the transperitoneal approach was used in the remaining 43 patients.
Results:
The mean patient age was 39.3 ± 12.0 years (range, 18–73). The study population was composed of 78 (26.7%) female and 135 (63.3%) male patients. The mean stone size was 19.7 ± 2.5 mm. The mean operative time was 80.9 ± 10.9 minutes, and the mean blood loss was 63.3 ± 12.7 mL. Intraoperative insertion of a double-J catheter was performed in 76 patients. The overall stone-free rate was 99%. No major complication was observed in any patient. However, conversion to open surgery was necessary in 1 patient.
Conclusion:
With high success and low complication rates, laparoscopic ureterolithotomy is an effective and reliable method that ensures quick recovery and may be the first treatment option for patients with large, impacted ureteral stones, as well as for those with a history of failed primary treatment.
Keywords: Laparoscopy, Retroperitoneal, Transperitoneal, Ureterolithotomy
INTRODUCTION
Shock wave lithotripsy (SWL) and ureteroscopy (URS) are the most commonly preferred methods for the treatment of ureteral stones.1 However, their use for large upper and middle ureteral stones remains controversial.2 Particularly with impacted stones, the success rate of SWL and URS diminishes, and when the stone size exceeds 1 cm, SWL efficacy decreases to from 84 to 42%.3 Although 7% of the ureteral stones treated with endourological methods require repeated treatment, 1% –10% of such patients may need open surgery.4 Open surgery has the advantage of a high success rate in one session for such complicated patients. Because open surgery increases the length of hospital stay and requires additional analgesic treatment for the patient, laparoscopic ureterolithotomy (LU) has recently become an alternative management method. It has been proposed that the success rate of LU is similar to that of open surgery and that it is superior to open surgery in reduced analgesic requirement, hospital stay, recovery, and cosmetic outcome.5–7
In this study, we analyzed the outcomes of LUs performed in our clinic in patients with upper or middle ureteral stones.
METHODS
Study Design
This study was performed with the approval of the Ethics Committee of Bakirkoy Research and Training Hospital. We retrospectively analyzed the data of 213 patients who underwent conventional LU for upper or middle ureteral stones from April 2006 through January 2015 in our clinic. Patients treated with single-port surgery were not included in the study. The indications for LU were a stone >15 mm in diameter or a history of failed SWL or URS. All procedures were performed by an experienced laparoscopic surgeon. All patients were followed up for at least 3 months.
Preoperative Evaluation
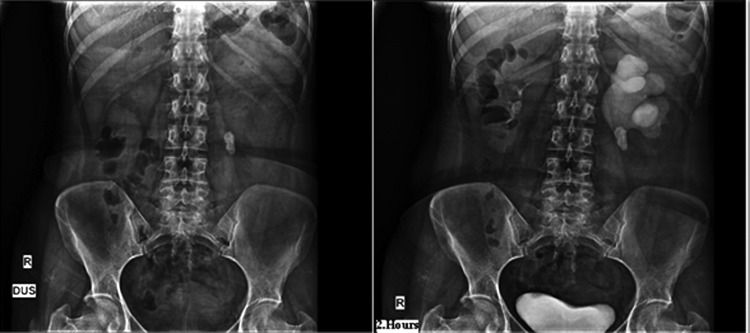
The preoperative evaluation included a detailed history, urinalysis, urine culture, complete blood count, and biochemical analysis of serum, coagulation tests, and intravenous pyelography, computed tomography, or both. Stone size was measured by using the longest axis of stone viewed on preoperative imaging (Figure 1).
Figure 1.
Preoperative images.
Positive urine cultures were adequately treated with appropriate antibiotics before surgery. Urinary drainage was performed through either a double-J (D-J) catheter or a nephrostomy tube in patients who had symptoms of sepsis, acute renal failure, severe hydronephrosis, and severe pain in the preoperative period.
Operative Technique
Even though we preferred the retroperitoneal approach in our clinic for LU, we used the transperitoneal approach in patients with a nephrostomy tube or a history of open retroperitoneal surgery.
We have previously described the retroperitoneal LU technique in detail with its modifications.4,8
To avoid stone migration, we used a Babcock clamp to grab the ureter proximal to the stone and performed all dissection cranially to caudally.
Ureterotomy was performed with a cold knife or a fine electrocautery hook, set at the lowest power setting.
When stones migrated into the kidney during manipulation or were present in the same-side kidney, they were taken into a basket catheter by entering through the working port with a flexible cystoscope (Karl Storz, Tuttlingen, Germany). Stones that were not small enough to pass through the lumen of the ureter were removed after being fragmented via laser lithotripsy (Figure 2).
Figure 2.
Preoperative and peroperative images of the patient who had ipsilateral ureteral and renal stones. (A) Preoperative CT imaging. (B) Flexible cystoscope introduced through an available working port. (C) Renal stones were removed with a nitinol basket.
A D-J stent was not routinely applied, but was used only in cases of ureteral mucosa inflammation as a result of long-term irritation of impacted stones.
Postoperative Period
All patients were mobilized and returned to oral feeding on the evening of the day of surgery. On the postoperative first day, an abdominal radiograph was performed to check for the presence of a residual stone and the condition of the D-J catheter. The drain was withdrawn on the second postoperative day if the drainage level fell below 50 mL. Postoperative analgesia was not a routine procedure; however, diclofenac sodium (75 mg intramuscularly) and/or paracetamol (500 mg orally) were administered if analgesia was necessary. Postoperative analgesic use and visual analog scale (VAS) for pain were evaluated on the day of surgery and on the first postoperative day. The D-J catheter was removed under local anesthesia between the second and fourth postoperative weeks. Serum creatinine and urine tests were carried out in the first postoperative month, and intravenous urography was performed in the third postoperative month.
Demographic data, stone characteristics, and intraoperative and postoperative data were recorded. Complications were classified according to the modified Clavien classification system.9
Statistical Analysis
The Number Cruncher Statistical System 2007 (Kaysville, UT, USA) was used for statistical analysis. Descriptive statistics (mean, standard deviation, median, frequency, and ratio) were used for evaluation of the study data. The independent samples t test was used for intergroup comparison of normally distributed random variables, and the Mann-Whitney U test was applied for nonnormally distributed variables. The qualitative data were compared by the Pearson χ2 test and the Fisher's exact test. P < .05 was considered statistically significant.
RESULTS
The mean patient age was 39.3 ± 12.0 years, with a range between 16 and 67 years. There were 135 (63.3%) male and 78 (26.7%) female patients in the study. Stones were located in the right side in 134 (62.9%) patients, and were located in the left side in 79 (37.1%) patients. Of the 213 patients, 178 (83.5%) had upper ureteral stones, and 35 (16.%) had middle stones. Thirteen of the patients had undergone unsuccessful URS, and 26 had unsuccessful SWL. LU was performed on 174 patients with the primary indication of stone size >15 mm. The size of the stones varied from 12 to 25 mm among the patients; the mean stone size was 19.7 ± 2.5 mm. The retroperitoneal approach was used in 170 (79.8%) patients, the transperitoneal approach was used in the remaining 43 (20.2%). In the transperitoneal group, 32 of the 43 patients had a nephrostomy catheter. Urinary drainage rate was significantly higher in the transperitoneal group (P < .01). Eleven patients had a history of open retroperitoneal surgery. Moreover, 13 patients who had a history of open abdominal surgery were treated with the retroperitoneal approach. There were significant differences among groups regarding the mean age (P < .01): the transperitoneal group was significantly older. No statistically significant difference was found between groups regarding gender distribution (P > .05). The body mass index measurements, stone size, stone location, failed SWL rate, and failed URS rate did not reveal any significant difference between groups (P > .05). The demographic and clinical characteristics of the patients are presented in Table 1.
Table 1.
Demographic Data
| Retroperitoneal (n = 170) | Transperitoneal (n = 43) | P | |
|---|---|---|---|
| Mean age (y) | 37.1 ± 11.9 | 43.3 ± 11.0 | .002a,* |
| Sex (M/F) | 113/57 | 30/13 | .681b |
| BMI (kg/m2) | 24.9 ± 2.2 | 25.0 ± 1.5 | .764a |
| Stone size (mm) | 19.6 ± 2.6 | 19.9 ± 2.2 | .497a |
| Stone side (R/L) | 91/79 | 23/20 | .996b |
| Failed SWL (n) | 21 | 5 | .897b |
| Failed URS (n) | 11 | 2 | .999c |
| Preoperative urinary drainage (nephrostomy/D-J) | 7 | 32 | .001b,* |
Independent-samples test.
Pearson χ2 test.
Fisher's exact test.
P < .01.
The mean operative time was 80.9 ± 10.9 minutes, whereas the mean blood loss was 63.3 ± 12.7 mL. Intraoperative insertion of the D-J cather was performed in 76 patients. The procedure was converted to open surgery in one (1%) patient because of an aberrant vessel. In another patient, the ureteral stone migrated to the kidney and a D-J stent was placed, and the stone was removed in 3 SWL sessions. After that surgery, we used flexible cystoscopy through a working port and removed the stones with a basket catheter in the other 23 patients: 4 had stone migration into the kidney and 19 had kidney stones in addition to ureteral stones. The stones were removed after fragmentation via laser lithotripsy in 4 patients owing to large stone size. The overall stone-free rate was calculated at 99%.
The stone-free rate did not differ among groups (P > .05). Operative time was found to be significantly longer in the transperitoneal group (P < .01). Moreover, the number of patients requiring D-J stenting was significantly higher in the transperitoneal group (P < .01). In addition, length of hospital stay and time to return to daily activities were significantly longer in the cases of transperitoneal surgery (P < .01). VAS scores were higher in the transperitoneal group compared with those in the retroperitoneal group on the day of surgery and first postoperative days (P < .01). Table 2 presents detailed information regarding the intraoperative and postoperative data.
Table 2.
Operative and Postoperative Data
| Retroperitoneal (n = 170) | Transperitoneal (n = 43) | P | |
|---|---|---|---|
| Stone-free rate, n (%) | 169 (99.4) | 43 (100) | .999a |
| Operative time (min) | 78.3 ± 10.0 | 91.1 ± 7.8 | .001b,* |
| D-J stenting, n (%) | 50 (29.4) | 26 (60.5) | .001c,* |
| Hospitalization mean ± SD | 2.8 ± 1.3 | 3.5 ± 1.2 | .001d,* |
| Return to daily activities (d) mean ± SD | 9.5 ± 1.1 | 12.2 ± 1.9 | .001b,* |
| VAS 0 mean ± SD | 6.0 ± 0.8 | 7.5 ± 0.9 | .001d,* |
| VAS 1 mean ± SD | 4.5 ± 0.7 | 6.0 ± 1.1 | .001d,** |
Data are the mean [plus/minus] SD, unless otherwise stated
Fisher's exact test.
Independent-samples test.
Pearson χ2 test.
Mann-Whitney U test.
P < .01
P < .05.
None of the patients needed blood transfusion. Gonadal vein injury was controlled with an endoclip in 4 patients. In 4 retroperitoneal cases, inadvertent peritoneotomy was observed and treated through enlargement of the peritoneal tear to equalize the pressure in 2 compartments. Prolonged urine drainage was observed in 10 patients after surgery. Although the drainage stopped on the fifth postoperative day in 7 patients, 3 patients required D-J stenting. Subcutaneous emphysema developed in 2 patients and recovered spontaneously within 24 hours. Antibiotic therapy was administered to 4 patients with postoperative fever and 1 patient with port-site infection. Ileus, which was resolved with conservative treatment, was observed in seven patients. No ureteral stricture was encountered during follow-up.
Although no significant difference was observed between groups regarding complications (P > .05), only the ileus rate was significantly higher in the transperitoneal group (P < .01). Detailed information on complications is given in Table 3.
Table 3.
Complications
| Retroperitoneal (n = 170) | Transperitoneal (n = 43) | P | |
|---|---|---|---|
| Open conversion | 1 | 0 | .999 |
| Urinary leakage | 9 | 1 | .691 |
| Postoperative D-J stent placement | 3 | 0 | .350 |
| Subcutaneous emphysema | 2 | 0 | 1.000 |
| Ileus | 1 | 6 | .001* |
| Peritoneal tear | 4 | 0 | .585 |
| Gonadal vein injury | 3 | 1 | 1.000 |
| Postoperative fever | 2 | 2 | .182 |
| Port site infection | 1 | 0 | 1.000 |
Fisher's exact test.
P < .01.
DISCUSSION
The first retroperitoneal ureterolithotomy was performed in 1979 by Wickham10, and the first transperitoneal ureterolithotomy was performed in 1992 by Raboy et al.11 In several studies LU showed a >95% success rate in the treatment of large ureter stones.11,12 According to the European Association of Urology guidelines on urolithiasis, large impacted ureteral stones, failure of minimally invasive procedures, different operative requirements for a concurrent indication, and technological deficiency are considered to be indications for performing LU.13
Ko et al14 compared LU with rigid ureteroscopy as the primary treatment modality for large upper ureteral stones and found the stone-free rate after a single session to be significantly higher in the LU group (93% vs 68%). Neto et al2 compared laparoscopy, SWL, and rigid URS and found success rates of 93, 35, and 62%, respectively. They also reported a lower need for additional procedures in the laparoscopy group. Ozturk et al15 reported that laparoscopy, SWL, and flexible URS had 81, and 79% success rates, respectively regarding treatment of large ureteral stones. These results may prove that LU is associated with higher success rates and lower requirement for auxiliary procedures. LU has been proposed as the primary treatment method for larger ureteral stones, especially in developing countries, where endourological technologies are expensive.16,17
Our previous study, in which a single surgeon's 6-year experience was reported, compared flexible URS and URS for upper ureteral stones >15 mm. The success rate was higher in the laparoscopy group (100% vs 87%). Although laparoscopy cases did not require additional intervention, 11 patients who underwent ureteroscopy required an additional procedure.8 In this series of 213 cases, the overall success rate was 99%. In one of our early cases, the stone migrated into the kidney. We could not reach the stone, so a D-J catheter was inserted and the stone was removed subsequently during multiple SWL sessions. After that patient, we had 23 patients—4 with stone migration into the kidney and 19 with kidney stones besides ureteral stones—who underwent flexible cystoscopy through a working port stone removal.
In this series, only 1 patient needed conversion to open surgery because of an aberrant vessel. However, compared with several series that reported open conversion rates, our series resulted in lower conversion rates.18,19
LU can be performed with the transperitoneal or retroperitoneal approach. The transperitoneal approach is advantageous because it provides a wider working space, better visibility, and better identifiable anatomical landmarks.18 The major disadvantage of the retroperitoneal approach is the limited working space. Conversely, there is no need for colon mobilization and, the risk for visceral organ injury is lower in the retroperitoneal approach. In addition, the risk for contamination of the peritoneal cavity caused by postoperative urinary leakage and the rate of postoperative ileus are lower in this approach.6,21 Postoperative recovery time is shorter in the retroperitoneal approach.22 Because of all of these, we prefer taking the retroperitoneal approach. Nevertheless, it may be difficult to perform retroperitoneal LU in the patients with a nephrostomy tube or those with a history of open retroperitoneal surgery.23 In these patients, we prefer the transperitoneal approach. In this series, we observed that both approaches provided high stone-free rates, but the retroperitoneal approach seems superior because of shorter operative time and faster postoperative recovery.
Urinary leakage is one of the most important complications of the procedure. However, morbidity does not increase as long as the urine is drained and remains noninfected. There is great debate on ureteral stenting and suturing. Kijvikai and Patcharatrakul12 emphasized suturing of the ureter to be an essential stage of the procedure. Bellman and Smith24, conversely, reported no need for incision suturing as long as the incision is small and the preoperative urine is sterile. Karami et al25 compared the patients with a D-J stent with those without a D-J stent, and reported that the presence of the D-J stent significantly decreased complication rates without increasing operative time. Therefore, stent placement was recommended for those patients without them. Alternatively, Hammady et al26 compared the outcomes of patients with stents versus no stents and reported lower analgesic requirement, shorter operative time, and lower cost—in favor of stenting. Kijvikai and Patcharatrakul12 recommended stenting only for prolonged impacted ureteral stones and for patients who could not receive ureteral sutures because of chronic inflammation of the ureteral mucosa. The ureter was closed with sutures in all of our cases. We placed D-J stents only in the presence of impacted stones or intensive inflammation of the ureter wall.
Ureteral stricture is a major complication of LU. In the review by Nouira et al,27 the rate of ureteral stricture was found to be 2.5%. In the present series, ureteral stricture was not detected in any of the patients through intravenous pyelography follow-ups after 3 months. The etiology of postoperative ureteral stricture is not clearly known. The correlation of the development of ureteral stricture with dilation–closure of the ureter is questionable. Nouira et al27 argued that a cold knife should be used to make an incision in the ureter to prevent ureteral stricture. Gaur et al28 indicated in their large series that ureter incision with an electric hook in cutting mode would be easier and safer to perform. Harewood et al18 claimed that the use of diathermy hook electrode is a reliable method for opening the ureter. We used a cold knife for our first cases, but then began using a monopolar hook for incision in light of the data provided by the aforementioned series.
Nouira et al27 stated that too-tight sutures may create ischemia on the wall, resulting in ureteral strictures, and argued that the main goal of the suturing method should be to ensure water resistance and approximation of the ureter ends to facilitate healing. Nevertheless, Kijvikai and Patcharatrakul12 did not encounter ureteral stricture during their 6-month follow-up in their cases with watertight suturing. Mitchinson and Bird29 suggested that prolonged urinary leakage may result in retroperitoneal fibrosis and ureteral strictures. Because of the increased visibility provided by laparoscopy, we can approximate the mucosal edges during ureteral suturing in a more accomplished fashion. We believe that, in this way, we may decrease both the urinary leakage and stricture rates.
Owing to these findings, including the high prevalence of urolithiasis in Turkey, with our clinic's position as the reference center, social factors, and patient preference, we frequently perform LU. To our knowledge, this is one of the largest series in literature of a single-surgeon experience on laparoscopic ureterolithotomy. The retrospective nature of the study and short-term follow-up are the limitations of the study.
CONCLUSION
Even though SWL and URS are considered to be the first-line treatment options for ureteral stones, retroperitoneal or transperitoneal LU can be established as an effective and reliable method, particularly in cases with large impacted stones and failure of the first-line treatments.
Contributor Information
Selçuk Şahin, Department of Urology, Bakirkoy Dr. Sadi Konuk Training and Research Hospital, Istanbul, Turkey..
Bekir Aras, Department of Urology, Dumlupinar University, Kutahya, Turkey..
Mithat Ekşi, Department of Urology, Bakirkoy Dr. Sadi Konuk Training and Research Hospital, Istanbul, Turkey..
Nevzat Can Şener, Department of Urology, Adana Numune Training and Research Hospital, Adana, Turkey..
Volkan Tugču, Department of Urology, Bakirkoy Dr. Sadi Konuk Training and Research Hospital, Istanbul, Turkey..
References
- 1. Segura JW, Preminger GM, Assimos DG, et al. Ureteral stones clinical guidelines panel summary report on the management of ureteral calculi. J Urol. 1997;158:1915–1921. [DOI] [PubMed] [Google Scholar]
- 2. Lopes Neto AC, Korkes F, et al. Prospective randomized study of treatment of large proximal ureteral stones: extracorporeal shock wave lithotripsy versus ureterolithotripsy versus laparoscopy. J Urol. 2012;187:164–168. [DOI] [PubMed] [Google Scholar]
- 3. Park H, Park M, Park T. Two-year experience with ureteral stones: extracorporeal shockwave lithotripsy v ureteroscopic manipulation. J Endourol. 1998;12:501–504. [DOI] [PubMed] [Google Scholar]
- 4. El-Moula MG, Abdallah A, El-Anany F, et al. Laparoscopic ureterolithotomy: our experience with 74 cases. Int J Urol. 2008;15:593–597. [DOI] [PubMed] [Google Scholar]
- 5. Soares RS, Romanelli P, Sandoval MA, et al. Retroperitoneoscopy for treatment of renal and ureteral stones. Int Braz J Urol. 2005;31:111–116. [DOI] [PubMed] [Google Scholar]
- 6. Feyaerts A, Rietbergen J, Navarra S, et al. Laparoscopic ureterolithotomy for ureteral calculi. Eur Urol. 2001;40:609–613. [DOI] [PubMed] [Google Scholar]
- 7. El-Feel A, Abouel-Fettouh H, Abdel-Hakim AM, et al. Laparoscopic transperitoneal ureterolithotomy. J Endourol. 2007;21:50–54. [DOI] [PubMed] [Google Scholar]
- 8. Tugcu V, Resorlu B, Sahin S, et al. Flexible ureteroscopy versus retroperitoneal laparoscopic ureterolithotomy for the treatment of proximal ureteral stones >15 mm: a single surgeon experience. Urol Int. 2016;96:77–82. [DOI] [PubMed] [Google Scholar]
- 9. Tefekli A, Karadag MA, Tepeler K, et al. Classifications of percutaneous nephrolithotomy complications using the modified Clavien grading system: looking for a standard. Eur Urol. 2008;53:184–190. [DOI] [PubMed] [Google Scholar]
- 10. Wickham JEA. (ed). The surgical treatment of renal lithiasis. In: Urinary Calculus Disease. New York: Churchill Livingstone; 1979:145–198. [Google Scholar]
- 11. Raboy A, Ferzli GS, Laffreda R, et al. Laparoscopic ureterolithotomy. Urology. 1992;39:223–225. [DOI] [PubMed] [Google Scholar]
- 12. Kijvikai K, Patcharatrakul S. Laparoscopic ureterolithotomy: its role and some controversial technical considerations. Int J Urol. 2006;13:206–210. [DOI] [PubMed] [Google Scholar]
- 13. Turk C, Knoll T, Petrik A, et al. EAU guidelines on urolithiasis. Vienna, Austria: European Association of Urology; 2011. [Google Scholar]
- 14. Ko YH, Kang SG, Park JY, et al. Laparoscopic ureterolithotomy as a primary modality for large proximal ureteral calculi: comparison to rigid ureteroscopic pneumatic lithotripsy. J Laparoendosc Adv Surg Tech A. 2011;21:7–13. [DOI] [PubMed] [Google Scholar]
- 15. Ozturk U, Sener NC, Goktug G, et al. The comparison of laparoscopy, shock wave lithotripsy and retrograde intrarenal surgery for large proximal ureteral stones. Can Urol Assoc J. 2013;7:E673–E676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gaur DD, Agarwal DK, Purohit KC, et al. Retroperitoneal laparoscopic pyelolithotomy. J Urol. 1994;151:927–929. [DOI] [PubMed] [Google Scholar]
- 17. Nualyong C, Taweemonkongsap T. Laparoscopic ureterolithotomy for upper ureteric calculi. J Med Assoc Thai. 1999;82:1028–1033. [PubMed] [Google Scholar]
- 18. Harewood LM, Webb DR, Pope AJ. Laparoscopic ureterolithotomy: the results of an initial series, and an evaluation of its role in the management of ureteric calculi. Br J Urol. 1994;74:170–176. [DOI] [PubMed] [Google Scholar]
- 19. Keeley FX, Gialas I, Pillai M, et al. Laparoscopic ureterolithotomy: the Edinburgh experience. BJU Int. 1999;84:765–769. [DOI] [PubMed] [Google Scholar]
- 20. Müslümanoglu AY, Karadag M, Tefekli AH, et al. When is open ureterolithotomy indicated for the treatment of ureteral stones? Int J Urol. 2006;13:1385–1388. [DOI] [PubMed] [Google Scholar]
- 21. Gaur DD, Rathi SS, Ravandale AV, et al. A single centre experience of retroperitoneoscopy using the balloon technique. BJU Int. 2001;87:602–606. [DOI] [PubMed] [Google Scholar]
- 22. Rofeim O, Yohannes P, Badlani G. Does laparoscopic ureterolithotomy replace shock-wave lithotripsy or ureteroscopy for ureteral stones? Curr Opin Urol. 2001;11:287–291. [DOI] [PubMed] [Google Scholar]
- 23. Bose TK, Shaw RE. Transperitoneal ureterolithotomy. Br J Urol. 1975;47:613. [DOI] [PubMed] [Google Scholar]
- 24. Bellman GC, Smith AD. Special considerations in the technique of laparoscopic ureterolithotomy. J Urol. 1994;151:146–149. [DOI] [PubMed] [Google Scholar]
- 25. Karami H, Javanmard B, Hasanzadeh-Hadah A, et al. Is it necessary to place a Double J catheter after laparoscopic ureterolithotomy? A four-year experience. J Endourol. 2012;26:1183–1186. [DOI] [PubMed] [Google Scholar]
- 26. Hammady A, Gamal WM, Zaki M, et al. Evaluation of ureteral stent placement after retroperitoneal laparoscopic ureterolithotomy for upper ureteral stone: randomized controlled study. J Endourol. 2011;25:825–830. [DOI] [PubMed] [Google Scholar]
- 27. Nouira Y, Kallel Y, Binous MY, et al. Laparoscopic retroperitoneal ureterolithotomy: initial experience and review of literature. J Endourol. 2004;18:557–561. [DOI] [PubMed] [Google Scholar]
- 28. Gaur DD, Trivedi S, Prabhudesai MR, et al. Laparoscopic ureterolithotomy: technical considerations and long-term follow-up. BJU Int. 2002;89:339–343. [DOI] [PubMed] [Google Scholar]
- 29. Mitchinson MJ, Bird DR. Urinary leakage and retroperitoneal fibrosis. J Urol. 1971;105:56–58. [DOI] [PubMed] [Google Scholar]