Abstract
Objective
The current study examined racial/ethnic differences in initial severity, session attendance, and counseling outcomes in a large and diverse sample of Asian American, Latino/a, and White student clients who utilized university counseling services between 2008 and 2012.
Method
We used archival data of 5,472 clients (62% female; M age = 23.1, SD = 4.3) who self-identified their race/ethnicity as being Asian American (38.9%), Latino/a (14.9%), or White (46.2%). Treatment engagement was measured by the number of counseling sessions attended; initial severity and treatment outcome were measured using the Outcome Questionnaire-45.
Results
Asian American clients, particularly Chinese, Filipino/a, Korean, and Vietnamese Americans, had greater initial severity compared to White clients. Asian Indian, Korean, and Vietnamese American clients used significantly fewer sessions of counseling than White clients after controlling for initial severity. All racial/ethnic minority groups continued to have clinically significant distress in certain areas (e.g., social role functioning) at counseling termination.
Conclusions
These findings highlight the need to devote greater attention to the counseling experiences of racial/ethnic minority clients, especially certain Asian American groups. Further research directions are provided.
Keywords: counseling outcome, utilization, college students, racial/ethnic minorities
University counseling centers are an important sector of mental health services delivery (Minami et al., 2009). Approximately half of young adults aged 18–25 are enrolled in higher education institutions (Snyder & Dillow, 2012). On average, 9% of students seek counseling each year (Gallagher, 2005), and these students often report high levels of depression and anxiety (Benton, Robertson, Tseng, Newton, & Benton, 2003) and have serious mental health needs. A report by the Center for Collegiate Mental Health (2014) showed that in 2012–2013, nearly one-third of counseling center clients (30.3%) reported that they seriously considered attempting suicide. In recent years, there has been a growing demand for university counseling services to address severe clinical issues (Benton et al., 2003), and popular press articles have also drawn attention to the increase in demand (e.g., Misner, 2014).
Treatments delivered in counseling centers are effective in reducing psychological distress (Minami et al., 2009; Snell, Mallinckrodt, Hill, & Lambert, 2001; Vonk & Thyer, 1999). Moreover, counseling services utilization is related to important academic outcomes (Choi, Buskey, & Johnson, 2010), including retention rates (Wilson, Mason, & Ewing, 1997). Examining the utilization and effectiveness of counseling services for racial/ethnic minority students is an important area of study as student bodies across U.S. college campuses are increasingly diversifying. In 1976, racial/ethnic minority students comprised only 15% of college enrollees, compared to 33% in 2010 (U.S. Department of Education, 2013). Identifying factors associated with treatment engagement, clinical characteristics, and treatment outcome will add to our understanding of the mental health needs of diverse students from historically underserved backgrounds.
Prior studies on the use of counseling services by racial/ethnic minority students have generally uncovered three patterns. First, racial/ethnic minority students, particularly Asian Americans, tend to report greater symptom severity at intake in comparison to White students (Kearney, Draper, & Baron, 2005; Krumrei, Newton, & Kim, 2010; Lockard, Hayes, Graceffo, & Locke, 2013). This is in contrast to epidemiological studies assessing prevalence rates of psychiatric disorders, which tend to find lower rates of diagnosable disorders among racial/ethnic minorities relative to White Americans (e.g., Chang, Chen, & Alegria, 2014). It is yet unclear whether this may be related to underreporting of symptoms in epidemiological studies or overreporting in individual studies, both of which may be related to cultural differences in symptom presentation. Notwithstanding this discrepancy, in counseling settings, racial/ethnic minority students have often self-reported greater levels of distress compared to White American students. This pattern has been fairly consistent across several reliable and valid measures, including the Outcome Questionnaire-45 (OQ-45; Lambert et al., 2004) and two versions of the Counseling Center Assessment of Psychological Symptoms (Locke et al., 2012), with few exceptions (e.g., Lambert et al., 2006).
In one investigation of student clients across 40 universities, Asian Americans reported the highest mean levels of psychological distress at intake as measured by the OQ-45, followed by Latino/as, African Americans, and Whites (Kearney et al., 2005). Accordingly, a higher percentage of the racial/ethnic minorities were considered to be in the clinical range at intake (65.7% of Asian Americans, 59.9% of Latino/as, and 55.2% of African Americans) in comparison to Whites (51.4%). Another investigation examined an aggregated sample of racial/ethnic minority students in comparison to White students across nine universities and found that racial/ethnic minority students reported significantly greater mood difficulties, interpersonal conflicts, and self-harm (Krumrei et al., 2010). Lockard and colleagues (2013) found that Asian American students indicated significantly higher levels of academic distress at intake compared to African American and White students.
Second, racial/ethnic minority students tend to underutilize counseling services in comparison to White students (Kearney et al., 2005). Kearney and colleagues’ investigation showed that Latino/a students utilized the fewest sessions of counseling (1.6 sessions), followed by Asian American (1.9 sessions), African American (2.2 sessions), and White students (3.5 sessions). These differences were statistically significant when comparing each of the racial/ethnic minority groups with White students, whereas the racial/ethnic minority groups did not differ with each other. Racial/ethnic minority students also tend to underutilize counseling services relative to their level of need (Eisenberg, Golberstein, & Gollust, 2007) although not relative to their campus representation (Hayes et al., 2011; Rosenthal & Wilson, 2008). Eisenberg and colleagues examined the likelihood of services use among students who perceived a need for mental health services and found that Asian/Pacific Islander students in particular were significantly less likely to use services (odds ratio = .22) relative to White students.
Third, evidence suggests that racial/ethnic minority students experience differential outcomes from counseling, though findings have been mixed. One investigation matched African American, Asian/Pacific Islander, Hispanic, and Native American clients to White control clients based on initial severity, gender, marital status, and age, and found no differences in treatment outcome (Lambert et al., 2006). Similarly, another study compared the mean change in distress from intake to termination, controlling for the number of sessions, and found that there were no racial/ethnic differences (Kearney et al., 2005). However, in both investigations, Asian American students began treatment in greater distress and remained in the clinical range at termination. Another study specifically examining academic distress showed that Asian American students reported significantly less change throughout treatment relative to White and Latino/a students (Lockard et al., 2013). Taken together, these studies suggest that counseling services may be less effective for racial/ethnic minority students, particularly Asian Americans, who tend to begin treatment with high symptom severity.
With growing mental health concerns on college campuses, alongside the increasing diversity of student bodies, there is a need to devote greater attention to the use and effectiveness of counseling services for racial/ethnic minority students. To this end, the current study used archival data from a university counseling center to further understand the use and effectiveness of counseling services across a large sample of Asian, Latino/a, and White American students. Asian Americans represent over 30 distinct cultural and ethnic groups (Liu, Murakami, Eap, & Hall, 2009), and similarly, Hispanic or Latino/a Americans have origins that represent more than 20 different Spanish-speaking countries (Lopez, Gonzalez-Barrera, & Cuddington, 2013). We focused on the six largest Asian American groups (i.e., Chinese, Filipino/a, Asian Indian, Vietnamese, Korean, and Japanese) and the largest Latino/a American group (i.e., Mexican) to examine racial/ethnic variations in initial severity, number of counseling sessions used, one-session attrition, and counseling outcomes. Our study is one of the few to examine these characteristics with data that are disaggregated by specific Asian and Latino/a American groups.
Method
Treatment Setting
We used archival data of clients who utilized Counseling and Psychological Services (hereafter referred to as CAPS) from a large, diverse public university located in the U.S. west coast. CAPS, located on the university campus, serves approximately 3,000 student clients each academic year, with over 16,000 clinical contacts annually. CAPS utilizes a brief therapy model, with long-term cases and more severe clinical needs typically referred to outside providers (an estimated 10% of clients yearly). CAPS regularly conducts student outreach through campus events and presentations. CAPS is accredited by the Association of Psychology Postdoctoral and Internship Centers as a postdoctoral fellowship training site. Provider characteristics are described below.
Participants
Client characteristics
Between the study period of 7/1/2008 and 6/30/2012, 7,958 clients used 40,589 counseling sessions (M sessions = 5.2, SD = 5.6). The current study utilized data from 5,472 clients in the CAPS database who self-identified their race/ethnicity as Asian American (38.9%, n = 2,130), Latino/a (14.9%, n = 816), or White/Caucasian (46.2%, n = 2,526). Table 1 provides sample information by racial/ethnic group. Among Asian Americans, 39.1% identified as Chinese, 20.6% as Korean, 12.3% as Vietnamese, 11.2% as Asian Indian, 7.8% as Filipino/a, 3.6% as Japanese, and the remaining 5.2% either identified as ‘other Asian’ or were of multiple Asian ethnicities (e.g., Chinese and Vietnamese). Among Latino/as, 47.3% were Mexican, and specific ethnicities of the remaining 52.7% were not available. The majority of the clients were female (62.0%), with a mean age of 23.1 years (SD = 4.3). Overall, 27.6% of the sample had utilized CAPS in the past, and 11.6% indicated that they were currently taking prescribed psychiatric medications.
Table 1.
Client Characteristics by Race/Ethnicity
| Asian Indian | Chinese | Filipino/a | Japanese | Korean | Vietnamese | Other or multiple Asian | Mexican | Other Latino/a | White | All | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | 239 | 834 | 167 | 77 | 440 | 263 | 111 | 386 | 430 | 2,526 | 5,472 |
| M age (SD) | 21.9 (3.0) | 21.9 (2.9) | 22.3 (3.2) | 22.7 (3.9) | 22.1 (3.2) | 21.6 (3.1) | 21.2 (2.8) | 22.7 (4.7) | 23.0 (4.3) | 24.1 (4.9) | 23.1 (4.3) |
| % female | 59.4 | 64.7 | 60.5 | 68.8 | 63.1 | 64.3 | 70.3 | 67.4 | 67.4 | 58.6 | 62.0 |
| % class level | |||||||||||
| First-year | 6.7 | 9.3 | 5.4 | 9.1 | 7.7 | 9.5 | 11.7 | 10.9 | 9.3 | 6.9 | 8.0 |
| Sophomore | 10.5 | 12.3 | 9.0 | 13.0 | 16.4 | 16.7 | 13.5 | 15.8 | 13.0 | 8.6 | 11.3 |
| Junior | 25.1 | 27.9 | 23.4 | 27.3 | 23.7 | 23.2 | 27.0 | 24.9 | 26.3 | 20.1 | 23.1 |
| Senior | 38.1 | 34.3 | 51.5 | 31.2 | 41.0 | 40.3 | 41.4 | 34.5 | 33.7 | 28.6 | 33.1 |
| Graduate student | 14.2 | 11.8 | 5.4 | 15.6 | 8.9 | 3.4 | 3.6 | 9.8 | 14.4 | 29.1 | 19.0 |
| Other student | 5.4 | 4.4 | 5.3 | 3.9 | 2.3 | 6.9 | 2.8 | 4.1 | 3.3 | 6.7 | 5.3 |
| % international student | 9.2 | 11.3 | 1.2 | 24.7 | 12.5 | 1.5 | 12.5 | 0 | 4.9 | 2.9 | 5.3 |
| % first in family to attend college | 18.4 | 34.3 | 25.7 | 13.0 | 25.8 | 47.9 | 39.6 | 73.8 | 65.1 | 15.8 | 29.8 |
| % with documented disabilities | 0.7 | 1.8 | 0.5 | 0.1 | 0.5 | 7.3 | 10.5 | 14.7 | 13.0 | 9.0 | 3.2 |
| % currently on academic probation | 13.8 | 9.2 | 11.4 | 14.3 | 12.7 | 14.1 | 10.8 | 18.9 | 14.7 | 7.2 | 10.3 |
| % prior use of CAPS | 25.6 | 23.2 | 28.7 | 20.0 | 25.4 | 25.7 | 29.1 | 26.2 | 32.5 | 29.3 | 27.6 |
| % currently taking prescribed psychiatric meds | 8.0 | 6.0 | 8.4 | 10.7 | 6.6 | 4.2 | 4.5 | 8.3 | 7.5 | 17.2 | 11.6 |
| M sessions used (SD) | 3.6 (4.5) | 4.0 (4.0) | 4.1 (3.8) | 5.0 (5.5) | 3.8 (3.7) | 3.7 (3.5) | 3.8 (3.4) | 4.1 (3.6) | 4.4 (4.5) | 3.9 (3.6) | 4.0 (3.8) |
| % one-session attrition | 24.7 | 21.8 | 15.0 | 19.5 | 20.3 | 24.0 | 16.2 | 16.6 | 13.7 | 16.3 | 18.0 |
Notes. CAPS = Counseling and Psychological Services; meds = medications
Therapist characteristics
During 2008–2012, 66 therapists (68.2% female) treated clients in the database. Most were White (60.5%), and race/ethnicity of the remaining individuals included African American, Asian American, Latino/a, and multiracial (specific numbers are intentionally not reported to avoid identifying individuals). Half of the therapists were licensed doctoral-level clinical or counseling psychologists (50.0%), whereas the rest consisted of predoctoral interns, postdoctoral fellows, and psychiatrists who also provided psychotherapy to clients. In general, therapists used multiple theoretical orientations, including cognitive-behavioral, psychodynamic, interpersonal, humanistic, feminist, and multicultural approaches. More specific therapist data were intentionally not accessed and reported, as some of the authors are/were affiliated with CAPS and treated clients in the database.
Measures
Demographic and intake information
All clients completed a standard set of questions prior to their intake appointment, assessing (1) demographics, (2) presenting concerns, (3) level of impact (i.e., the extent to which concerns interfere with functional domains, such as academics), (4) mental health history (e.g., prior use of treatment), (5) alcohol and substance use/abuse history, (6) health and social issues (e.g., physical health, sleeping habits), and (7) family/cultural background (e.g., language spoken at home). For this study, we extracted client demographics, presenting concerns, and mental health history. Clients rank-ordered their top three concerns from a list of 52 concerns (e.g., “academic concerns,” “depression, sadness,” and “family problems”), with the option to select “other presenting concern” and give an open-ended response. From this list, we combined similar types of concerns (e.g., “intimate relationship concerns” and “family problems” were grouped as interpersonal concerns), yielding nine major presenting concerns (see Table 2). The mental health history portion of the intake questionnaire assessed any prior use of CAPS, any prior and/or current use of prescribed psychiatric medications, any prior and/or current self-injury without suicidal intent (e.g., “Have you purposely injured yourself without suicidal intent [e.g., cutting, hitting, burning, etc.]?”), and any prior, recent, and/or current thoughts of suicide (e.g., “In the last few days, have you had suicidalthoughts?”).
Table 2.
Percentage Distribution of Primary Presenting Concerns by Race/Ethnicity
| Asian Indian | Chinese | Filipino/a | Japanese | Korean | Vietnamese | Other or multiple Asian | Mexican | Other Latino/a | White | All | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | 238 | 822 | 166 | 76 | 435 | 261 | 111 | 386 | 427 | 2,506 | 5,428 |
| Academic issues | 23.8 | 20.3 | 19.2 | 18.2 | 22.1 | 24.7 | 18.9 | 18.4 | 23.5 | 14.3 | 18.1 |
| Adjustment | 1.3 | 1.8 | 1.2 | 0 | 1.1 | 0.8 | 1.8 | 2.6 | 1.9 | 2.0 | 1.8 |
| Anxiety | 13.4 | 11.4 | 12.6 | 16.9 | 16.6 | 11.0 | 14.4 | 14.8 | 13.6 | 18.9 | 16.1 |
| Depression | 19.2 | 19.1 | 18.0 | 18.2 | 20.5 | 22.1 | 17.1 | 18.7 | 19.1 | 19.0 | 19.2 |
| Identity issues | 5.4 | 7.9 | 7.8 | 5.2 | 5.9 | 4.2 | 9.0 | 5.2 | 5.2 | 5.0 | 5.7 |
| Interpersonal issues | 15.1 | 14.4 | 19.2 | 16.9 | 9.8 | 14.8 | 15.3 | 17.1 | 11.2 | 16.2 | 15.2 |
| Other mood symptoms | 4.6 | 6.2 | 5.4 | 5.2 | 4.6 | 4.6 | 6.3 | 3.1 | 6.0 | 5.0 | 5.2 |
| Stress | 3.8 | 4.3 | 4.2 | 0 | 4.1 | 3.8 | 0.9 | 5.2 | 4.2 | 4.7 | 4.4 |
| Substance issues | 1.7 | 0.5 | 0.6 | 3.9 | 2.1 | 0.8 | 0.9 | 1.6 | 1.2 | 1.4 | 1.3 |
Note. The two most common presenting concerns for each racial/ethnic group are depicted in bolded figures.
Psychological distress
Psychological distress was measured by the Outcome Questionnaire-45 (OQ-45; Lambert et al., 2004). The OQ-45 was designed to track a client’s progress throughout treatment and consists of 45 questions on a 5-point scale (0 = never, 1 = rarely, 2 = sometimes, 3 = frequently, 4 = almost always). Total scores range from 0–180, with higher scores indicating greater levels of distress. The 45 items can be divided into three subscales that measure Symptom Distress (SD; 25 items), the Quality of Interpersonal Relationships (IR; 11 items), and Social Role Functioning (SR; 9 items). SD assesses symptoms of stress and psychological distress, such as depressive and anxiety symptoms (e.g., “I feel worthless” and “I feel nervous”), as well as somatic symptoms (e.g., “I have headaches”). IR assesses complaints of loneliness, conflicts with others, and other relationship issues (e.g., “I am concerned about family troubles”). SR assesses the extent of difficulties and conflicts in social roles (e.g., “I feel stressed at work/school”). A score of 63+ on the total score indicates clinically significant distress, and a change of 14+ points during a subsequent administration indicates reliable improvement or deterioration, depending on the direction of change. For the SD subscale, a score of 36+ indicates clinical significance, with a change of 10+ points indicating reliable change. For the IR subscale, 15+ indicates clinical significance, and a 8+ point change indicates reliable change. For the SR subscale, 12+ indicates clinical significance, and a 7+ point change indicates reliable change. Lambert et al. (2004) reported an internal consistency of .93 and a 3-week test-retest reliability of .84. Total scores on the OQ-45 are highly correlated with other widely used measures of psychological symptoms including the SCL-90 (Derogatis, 1983) and the Beck Depression Inventory (Beck, Ward, Mendelson, Mock, & Erbaugh, 1961).
One study found that non-treatment-seeking Asian American students were more likely to score in the clinical range on the OQ-45 than their White American counterparts (Gregersen, Nebeker, Seely, & Lambert, 2004); a similar study could not be located for Latino/a students. Thus we acknowledge that there is a lack of research on the validity of the OQ-45 cutoff scores across racial/ethnic groups. Nonetheless, the OQ-45 has been used in published research with Asian American and Latino/a students and student clients (Gupta, Szymanski, & Leong, 2011; Kearney et al., 2005; Lambert et al., 2006). In the current study, Cronbach’s αs of all 45 items were .92 at intake and .94 at last measurement. For subscales, Cronbach’s αs at intake and last measurement, respectively, were as follows: .91 and .93 for SD; .72 and .76 for IR; and .67 and .69 for SR.
Treatment engagement
Treatment engagement was assessed by the number of counseling sessions attended by each client within a year (considered July 1 to June 30 of the following year). Clients who attended only a single session of counseling were considered as one-session attrition (Ibaraki & Hall, 2014).
Procedure
According to standard CAPS procedures, clients requested appointments in-person or via telephone. Prior to the initial appointment, clients received a secure email with instructions to complete the intake questionnaire and the OQ-45. The intake questionnaire was collected from each client on a yearly basis. That is, a client initially seen during 2008–2009 who returned for additional sessions during 2009–2010 recompleted the intake questionnaire. To avoid duplicity, we utilized data from each client’s first intake during 2008–2012. The OQ-45 was re-administered prior to the fourth, seventh, and last/termination sessions, for up to four measurements per client. All data were de-identified prior to any analyses. The university IRB exempted this archival study.
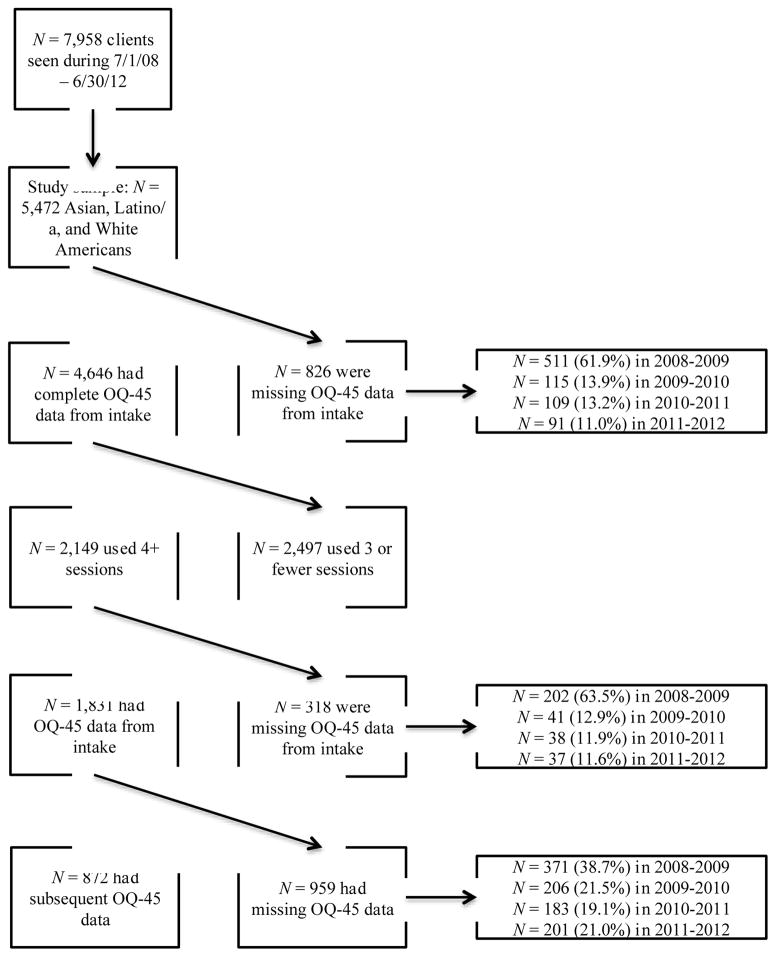
Handling of missing data on the OQ-45
Figure 1 provides a flowchart of the available and missing OQ-45 data. Intake OQ-45 scores were available for 84.9% of the sample, with no item-level missing data. Missing data for the remainder were likely due to a new electronic health record system implemented at CAPS in 2008–2009, as the majority of missing data was from clients seen during 2008–2009. Missing scores in subsequent years likely reflect routine client non-response (e.g., forgetfulness, refusal, time constraints). Given the aforementioned OQ-45 administration schedule, all clients who used 4+ sessions should have had a subsequent administration of the OQ-45. Among the 39.3% of clients who used 4+ sessions, 85.2% (n = 1,831) had OQ-45 data at intake. Among these individuals, 47.6% (n = 872) had a subsequent OQ-45 score. Similar to above, a sizable proportion of the missing subsequent OQ-45 data were from clients seen during 2008–2009. Among these 1,831 individuals, we compared those without and with missing data (n = 872 and n = 959, respectively). Chi-square tests and t-tests showed that these groups did not significantly differ on gender, race/ethnicity, age, and mean OQ-45 score at intake. The groups did, however, differ in the total number of sessions. On average, those without missing outcome data used an additional session (M = 7.6, SD = 4.0) than those with missing data (M = 6.6, SD = 4.0), t(1,829) = 5.03, p < .001. Clients who utilized more sessions likely received additional reminders to complete missed questionnaires.
Figure 1.
Flowchart Depicting Proportion of Available and Missing Data on the Outcome Questionnaire-45 (OQ-45)
In assessing treatment outcomes using OQ-45 scores, we assumed that data were missing completely at random or missing at random (Schlomer, Bauman, & Card, 2010). We discounted the possibility of missing not at random because there was no relation between initial OQ-45 score and missingness on the subsequent OQ-45 score (p = .98). We handled missing data using multiple imputation, which is an appropriate method for large survey studies (Sinharay, Stern, & Russell, 2001). We used auxiliary variables because over 50% of our treatment outcome data were missing. Auxiliary variables, which are used in the imputation model but not the analysis model, can improve the prediction of missing values as they may be correlated with variables with missing data (Schlomer et al., 2010). We included five auxiliary variables that may be related to psychological distress severity, including current use of psychiatric medications, prior and current self-injury, and prior and current suicidal thoughts. We created 10 imputed datasets (Schafer & Graham, 2002) to estimate subsequent OQ-45 scores of all individuals who used 4+ sessions of counseling and had an OQ-45 score at intake. This method allowed for the use of all available data (n = 1,831), rather than being limited to only data from clients who provided both an intake score and a subsequent score on the OQ-45 (n = 872).
Results
Presenting Concerns
Table 2 shows the percentage distribution of presenting concerns across racial/ethnic groups, with the top two presenting concerns shown in bolded figures. Across all racial/ethnic minority groups, academic issues and depression were most frequently reported, whereas depression and anxiety were most frequently reported for White clients. For Filipino/a clients, interpersonal issues was also a top presenting concern alongside academic issues, and for Japanese clients, interpersonal issues and anxiety were equally reported as the second most common presenting concern.
Initial Severity
Table 3 displays data on clinical severity. Across all clients, 36.1% reported ever having had thoughts of self-injury, and 13.0% reported recent suicidal thoughts. We used chi-square tests to examine group differences in the proportion of clients who reported ever having thoughts of self-injury and recent thoughts of suicide. Using a significant p-value of .005 to correct for multiple tests (i.e., .05 / 9 comparisons), we found that Chinese, Filipino/a, and Korean clients were significantly more likely to report ever having had thoughts of self-injury, relative to White clients, all ps < .001. A significantly greater proportion of Asian Indian, Chinese, Filipino/a, Korean, and other or multiple Asian clients reported recent thoughts of suicide compared to White clients, all ps < .005.
Table 3.
Clinical Severity at Intake by Race/Ethnicity
| Asian Indian | Chinese | Filipino/a | Japanese | Korean | Vietnamese | Other or multiple Asian | Mexican | Other Latino/a | White | All | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| % reporting ever having thoughts of self-injury | 32.4 | 39.7* | 49.7* | 42.7 | 44.1* | 41.4 | 45.5 | 30.6 | 34.7 | 32.9 | 36.1 |
| % reporting recent suicidal thoughts | 15.5* | 16.7* | 17.4* | 17.3 | 21.0* | 14.6 | 18.2* | 10.9 | 12.9 | 9.6 | 13.0 |
| n | 206 | 724 | 145 | 68 | 375 | 232 | 91 | 336 | 362 | 2,107 | 4,646 |
| M distress (OQ-45 score) at intake (SD) | 70.5 (21.5) | 72.5* (20.8) | 74.9* (20.3) | 73.5 (24.4) | 77.8* (22.2) | 73.3* (22.6) | 70.5 (22.4) | 67.8 (22.4) | 70.1 (21.7) | 66.9 (21.1) | 69.8 (21.7) |
| % in clinical range | 63.6 | 69.5* | 75.9* | 58.8 | 77.3* | 67.7 | 64.8 | 61.9 | 62.4 | 57.7 | 63.3 |
Notes.
indicates statistically significant difference compared to Whites at p < .005 to correct for multiple tests;
OQ-45 = Outcome Questionnaire-45.
Table 3 also shows initial distress scores and percentage of clients considered in the clinical range (i.e., OQ-45 score of 63+) by race/ethnicity. We conducted a one-way analysis of variance (ANOVA) examining racial/ethnic differences in initial distress, as measured by total OQ-45 scores. Results indicated a statistically significant difference in overall distress, F(9, 4,636) = 13.65, p < .001, partial η2 = .026. Although sample sizes varied across groups, Levene’s test did not indicate unequal variances (F = 1.19, p = .30). Using a corrected p-value of .005, post-hoc tests (Tukey) showed that relative to White clients, Chinese (p < .001), Filipino/a (p < .001), Korean (p < .001), and Vietnamese (p = .001) clients had significantly greater levels of distress at intake. Korean clients, who had the highest mean distress score at intake, had significantly greater distress when compared with Chinese (p = .004), Asian Indian (p = .003), Mexican (p < .001), and other Latino/a (p < .001) clients.
A chi-square test revealed significant overall differences in the proportion of clients considered to be in the clinical range at intake, χ2 (9, N = 4,646) = 84.82, p < .001, Cramer’s V = .14. As shown on Table 3, Korean clients had the highest proportion in the clinical range, whereas White clients had the lowest. Individual chi-square tests showed that a significantly greater proportion of Chinese, Filipino/a, and Korean clients were in the clinical range at intake, compared to White clients.
Session Attendance and One-Session Attrition
On average, clients attended 4.0 sessions (SD = 3.8, median = 3, mode = 1). A one-way ANOVA testing racial/ethnic differences in session attendance was not significant, F(9, 5,462) = 1.79, p = .07. We conducted a multiple regression analysis to control for initial severity, in which racial/ethnic groups were entered as binary independent variables, and Whites were the reference group. When controlling for initial distress severity, Asian Indian (B (SE) = −.68 (.26), β = −.04, p = .009), Korean (B (SE) = −.50 (.20), β = −.04, p = .014), and Vietnamese (B (SE) = −.50 (.25), β = −.03, p = .044) clients attended significantly fewer sessions of counseling, whereas Japanese clients (B (SE) = 1.12 (.44), β = .04, p = .011) attended significantly greater sessions.
Across all clients, 18.0% (n = 987) attended only one session. A chi-square test revealed significant differences in one-session attrition, χ2 (9, N = 5,472) = 35.20, p < .001, Cramer’s V = .08, which was relatively high for Asian Indian, Vietnamese, Chinese, Korean, and Japanese clients, and relatively low for Mexican, White, other or multiple Asian, and other Latino/a clients (Table 1). We conducted a logistic regression analysis, controlling for initial severity, to examine likelihood of one-session attrition across groups. In reference to White clients, Asian Indian (odds ratio [OR] = 1.75, 95% CI [1.25, 2.46], p < .001), Chinese (OR = 1.51, 95% CI [1.22, 1.86], p < .001), and Korean clients (OR = 1.42, 95% CI [1.08, 1.89], p < .001) were more likely to terminate treatment after one session. Odds ratios of all other racial/ethnic groups were not significant compared to Whites. Moreover, post-hoc tests showed that initial severity did not moderate the association between race/ethnicity and one-session attrition.
Counseling Outcomes
We examined the subset of clients who provided an OQ-45 score at intake and used at least four sessions (n = 1,831) to sufficiently measure clinical change. Table 4 provides subsample characteristics in terms of gender and age, and a summary of OQ-45 scores across intake and last administration. As indicated by asterisks on Table 4, all groups at intake were clinically significant in overall distress, symptom distress (SD), interpersonal relations (IR), and social role functioning (SR). At last measurement, all groups except Whites had clinically significant distress in certain areas. Korean Americans continued to have clinically significant distress in all areas, and Asian Indian, Chinese, Filipino/a, and Vietnamese Americans had clinically significant distress in all areas except IR. Although Japanese, other or multiple Asians, Mexicans, and other Latino/as were no longer clinically significant in terms of overall distress, they remained clinically significant in SR.
Table 4.
Client Characteristics, Session Count, and Counseling Outcome (OQ-45 scores) of Clients Using 4+ Sessions by Race/Ethnicity
| Asian Indian | Chinese | Filipino/a | Japanese | Korean | Vietnamese | Other or multiple Asian | Mexican | Other Latino/a | White | All | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | 61 | 283 | 55 | 32 | 134 | 83 | 37 | 140 | 153 | 853 | 1,831 |
| M age | 21.5 (2.3) | 21.8 (2.9) | 21.9 (2.7) | 22.4 (4.0) | 22.4 (3.3) | 21.1 (2.3) | 21.2 (2.0) | 22.8 (5.1) | 23.3 (4.3) | 24.4 (5.0) | 23.2 (4.4) |
| % female | 59.0 | 64.0 | 58.2 | 75.0 | 64.2 | 62.7 | 78.4 | 62.9 | 67.3 | 58.9 | 61.9 |
| M sessions (SD) | 7.0 (3.6) | 7.5 (4.5) | 7.4 (3.9) | 9.3 (6.3) | 7.2 (3.4) | 6.9 (3.8) | 6.8 (3.7) | 6.9 (3.6) | 7.1 (4.6) | 6.9 (3.8) | 7.1 (4.0) |
| Intake OQ-45 | |||||||||||
| Total | 75.8* | 75.5* | 77.3* | 80.6* | 83.5* | 79.7* | 75.6* | 71.3* | 73.7* | 69.0* | 72.9* |
| SD | 45.2* | 43.7* | 45.3* | 47.5* | 49.6* | 47.2* | 44.1* | 41.4* | 42.8* | 40.1* | 42.6* |
| IR | 15.9* | 16.4* | 16.3* | 16.5* | 17.6* | 16.8* | 15.9* | 15.5* | 16.2* | 15.1* | 15.8* |
| SR | 14.8* | 15.3* | 15.6* | 16.5* | 16.4* | 15.7* | 15.5* | 14.5* | 14.7* | 13.7* | 14.5* |
| Last OQ-45 | |||||||||||
| Total | 64.9* | 64.0* | 64.5* | 61.0 | 71.7* | 66.3* | 62.1 | 58.8 | 59.8 | 59.4 | 61.7 |
| SD | 37.7* | 36.6* | 37.1* | 35.3 | 41.9* | 38.4* | 36.1* | 33.6 | 33.7 | 34.2 | 35.5 |
| IR | 14.5 | 14.4 | 14.4 | 13.4 | 15.9* | 14.5 | 13.1 | 12.8 | 13.5 | 13.3 | 13.7 |
| SR | 12.7* | 13.0* | 13.0* | 12.4* | 13.9* | 13.5* | 12.8* | 12.4* | 12.6* | 11.9 | 12.5 |
| Change in OQ-45 | |||||||||||
| Total | 10.9 | 11.5 | 12.8 | 19.6** | 11.8 | 13.4 | 13.5 | 12.5 | 13.9 | 9.6 | 11.2 |
| SD | 7.5 | 7.1 | 8.2 | 12.2** | 7.7 | 8.8 | 8.0 | 7.8 | 9.1 | 5.9 | 7.1 |
| IR | 1.4 | 2.0 | 1.9 | 3.1 | 1.7 | 2.3 | 2.8 | 2.7 | 2.7 | 1.8 | 2.1 |
| SR | 2.1 | 2.3 | 2.6 | 4.1 | 2.5 | 2.2 | 2.7 | 2.1 | 2.1 | 1.8 | 2.0 |
Notes.
indicates clinical significance;
indicates reliable change;
SD = Symptom Distress subscale; IR = Interpersonal Relations subscale; SR = Social Role subscale
Table 4 also shows the change in distress between first and last measurement of the OQ-45 across racial/ethnic groups. Paired-sample t-tests showed that these change scores were significant for all groups (all ps < .001). However, the only change scores that met criterion for reliable improvement established by Lambert et al. (2006) were for Japanese clients in the areas of overall distress and SD. We conducted a multiple regression analysis predicting change in total distress scores from the intake measurement to the last measurement. We controlled for the intake distress severity and the number of sessions, and race/ethnicity were entered as binary independent variables, with Whites as the reference group. The results showed that only Japanese clients had significantly lower distress after counseling (B = −10.29, SE = 4.38, β = −.06, p = .019). Although White clients were no longer considered to have clinically significant distress, their change in distress did not warrant reliable improvement. All clients experienced improvement from utilizing at least four sessions of counseling, but most did not warrant clinically significant, reliable improvement.
Discussion
Our investigation nuances the general pattern of finding that Asian American clients tend to have greater initial severity at the outset of counseling than their non-Asian American counterparts (e.g., Durvasula & Sue, 1996; Kearney et al., 2005). In this study, Chinese, Filipino/a, Korean, and Vietnamese American clients reported greater levels of psychological distress compared to White clients. Of these groups, Korean Americans reported the greatest levels of distress. A previous study investigating depressive symptom severity among non-treatment-seeking college students showed that Korean Americans reported more severe depressive symptoms compared to Chinese Americans and Whites (Young, Fang, & Zisook, 2010). Factors such as acculturative stress and cultural value orientations have been considered to be salient to the mental health of Korean Americans. One study showed that cultural value orientation, such as perceived parental traditionalism, was associated with depressive symptoms for Korean American students (Aldwin & Greenberger, 1987). Historically, Korean Americans are one of the newest groups of Asian American immigrants in the U.S., and this may contribute to many Korean American student clients experiencing conflicts in cultural values between themselves and their parents, which may contribute to greater mental health problems (Hovey, Kim, & Seligman, 2006).
Greater severity of distress among certain Asian American students is important given the patterns of presenting concerns, as many cited academic issues as a primary reason for seeking counseling. An earlier study reported that educational concerns were the most common presenting problems among Asian American students seeking counseling, versus interpersonal or emotional concerns among White American students (Tracey, Leong, & Glidden, 1986). For many Asian Americans, psychological distress or depressive symptoms may result in part from high academic pressures from their families and cultures of origin (Lee et al., 2009). One study found that Asian American students worried more frequently about academic issues than White American students, and this difference was explained by perceptions of living up to parental expectations of academic performance (Saw, Berenbaum, & Okazaki, 2013). These pressures may reflect another area of family cultural conflict, which has been found to be a predictor of mental health services use in a population-based study of Asian Americans (Chang, Natsuaki, & Chen, 2013). Educational achievement tends to be highly valued among many Asian Americans (Sue & Okazaki, 2009), and these academic-related pressures appear to have negative mental health consequences for many Asian Americans.
Academic issues were also a major concern for Latino/a clients. The majority of Mexicans (74%) and non-Mexican Latino/as (65%) reported that they were the first in their immediate family to attend college. The experience of being a first generation college student may contribute to psychological symptoms because of the pressures and stressors associated with navigating an unfamiliar educational system with limited social and financial resources (Castillo et al., 2015). That Latino/as have been historically underrepresented in higher education settings may also contribute to stress and/or distress. For example, one study conducted in a diverse public university found that Latino/a students reported relatively high levels of depressive symptoms, and in particular, the stress related to minority status contributed to these symptoms (Arbona & Jimenez, 2014). Research on youth have shown that college-aspiring Latino/a youth reported greater symptoms of depression and distress compared to their non-college-aspiring counterparts, whereas the relationship was reversed for Black and White youth (Turcios-Cotto & Milan, 2013). These prior findings support results of the current study that academic concerns are prominent among Latino/a students seeking counseling.
Higher levels of psychological distress have been associated with greater mental health help-seeking stigma for Asian and Latino/a American students (Cheng, Kwan, & Sevig, 2013). Thus these clients may have reported academic issues as a primary reason for counseling to circumvent the stigma associated with help-seeking. Prior findings demonstrate that explicit discussion of academic concerns in counseling sessions is related to greater session attendance for racial/ethnic minorities, particularly for Asian Americans (Ibaraki & Hall, 2014). Moreover, counseling is effective in reducing academic-related distress (Lockard et al., 2012). An implication from the current and previous findings may be that counselors should directly address academic concerns, particularly at the outset of treatment, as a mechanism to demonstrate the utility of seeking counseling for problems related to academics and the emotional concerns that may coincide with academic difficulties. This may also serve to validate the presenting concerns of many clients, which in turn, may reduce the stigma associated with mental health problems and increase session attendance.
We found that Asian Indian, Korean, and Vietnamese American clients used significantly fewer sessions of counseling when adjusting for initial severity. Furthermore, Asian Indian, Chinese, and Korean American clients were significantly more likely to terminate treatment after one session compared to White clients. In contrast to previous results (Kearney et al., 2005), Latino/a clients did not show patterns of one session attrition. Premature termination has been a longstanding mental health disparity that has affected Asian Americans as a group (Sue et al., 2012). Thus it is unlikely that these clients terminated treatment because they successfully met their treatment goals. Although it is possible that these clients found help elsewhere (e.g., family or friends, other campus resources), this is also less likely given that racial/ethnic minorities tend to seek formal mental health services after utilizing informal sources of help (Cabassa & Zayas, 2007). Clients may have also been referred to outside providers, though we were unable to explore this possibility with the current data.
In greater likelihood, clients may have dropped out of treatment because they felt that it was not immediately helpful in addressing their problems. This is congruent to Sue and Zane’s (1987) recommendation that clinicians offer an immediate benefit (e.g., normalization, validation) to enhance perceptions of therapy credibility for culturally diverse clients. Among Asian Indians, for example, scholars have suggested that reframing mental health symptoms as reactions to interpersonal issues is one way to promote help-seeking in a culturally congruent manner (Leung, Cheung, & Tsui, 2012). In our study, Asian Indian clients had the highest rates of one-session attrition. This may be in part due to a lack of match on pre-therapy expectations, which are known to influence outcomes (Constantino, Arnkoff, Glass, Ametrano, & Smith, 2011), with actual experiences (Goldfried, 2012). For example, Asian Americans have the tendency to avoid negative thinking and not excessively dwell on distressing thoughts (Leong & Lau, 2001). This is counter to the process of active self-disclosure and discussion of distressing thoughts and feelings, particularly in the initial phases of therapy. Furthermore, mismatches on expectations about treatment, such as therapist directiveness, may also contribute to the perception that treatment was not helpful (Wong, Beutler, & Zane, 2007).
Therapist effects may also account for premature termination from counseling (Owen, Imel, Adelson, & Rodolfa, 2012). It has been suggested for some time that racial/ethnic matching of client and therapist may be conducive to greater engagement and better outcome (Sue, Fujino, Hu, Takeuchi, & Zane, 1991), though meta-analytic findings have not supported this notion (Cabral & Smith, 2011; Maramba & Hall, 2002). A study conducted in a university counseling center found that regardless of racial/ethnic match, therapists varied in their effectiveness with racial/ethnic minority clients, such that some therapists were more effective in reducing symptoms among White clients, whereas others were more effective in reducing symptoms among racial/ethnic minority clients (Hayes, Owen, & Bieschke, 2014). The study of therapist effects on client outcomes was beyond the scope of this study, but this is an important area of research that has implications in multicultural training of therapists.
At counseling termination, all racial/ethnic groups, with the exception of Whites, continued to be clinically significant in certain areas of distress. Korean Americans continued to have clinically significant distress in all areas measured by the OQ-45. We do note that the OQ-45 subscales are highly correlated with one another (Mueller, Lambert, & Burlingame, 1998), which suggests that for Korean Americans, high overall distress also impacted interpersonal relationships and social functioning. Asian Indian, Chinese, Filipino/a, and Vietnamese Americans had clinically significant distress in all areas except interpersonal relations. This might tentatively demonstrate the effectiveness of counseling in reducing interpersonal problems that cause distress. Japanese American clients appeared to reliably improve in terms of overall distress and symptom distress, but interpretations should be made cautiously given the small sample size of Japanese clients.
Research on the dose-response relationship might help explain why most groups did not reliably improve from counseling (Draper, Jennings, Baron, Erdur, & Shankar, 2002). One study determined that 14 sessions of counseling were needed for 51% of clients to meet criteria for clinically significant change (Wolgast, Lambert, & Puschner, 2003). However, most counseling clients do not remain in treatment for that duration, and university counseling centers largely offer short-term approaches. The mean number of sessions across all clients in the current study was considerably lower than what necessitates clinically significant change; however, utilizing even two sessions of counseling has been associated with improvement (Minami et al., 2009). Our findings suggest the need for future research in reducing one-session attrition and examining the dose-response relationship for racial/ethnic minority counseling clients.
We acknowledge limitations to our study. We note that research on the cross-cultural validity of the OQ-45 is not yet available. However, Asian American groups did report greater severity of mental health problems from other indicators (e.g., self-injury, suicidal ideation), which parallel the patterns of findings from the OQ-45. Furthermore, academic issues were a primary concern for many racial/ethnic minority students seeking counseling, but the OQ-45 does not explicitly measure academic-related distress. In recent years, CAPS has implemented the use of the Counseling Center Assessment of Psychological Symptoms-34 (Locke et al., 2012), which measures academic distress and has been found to be cross-culturally valid for Asian American and Latino/a students and student clients (Center for Collegiate Mental Health, 2014). There was a high amount of missing data on the OQ-45, which we statistically mitigated, but this raises questions about other systemic reasons contributing to missing data. We also note that the outcome variable reflected the last available measurement of the OQ-45 for clients who used 4+ sessions, which may not have perfectly corresponded to the actual termination session.
Another limitation is that we did not have information on cultural variables, such as acculturation or ethnic identity, which may have been informative in understanding within-group variations. We also did not have data on the reason for termination (e.g., therapist-client mutual termination or client “no show” to follow-up appointments). These limitations reflect the constraints of many counseling centers on the ability to conduct systematic research in a setting where clinical care is the priority. The varied sample sizes of racial/ethnic groups may have reduced the power needed to detect effects in some cases. We nonetheless deemed it meaningful to include these smaller groups (e.g., Japanese Americans) given the lack of ethnic specific extant data. Our findings may be more statistically stable when examining greater than four years of data, allowing a larger sample size of certain groups. Despite this concern, the overall sample size and diversity was a particular strength, and these results may generalize to other university counseling centers with similar characteristics.
The findings have implications for outreach, provision of counseling, and research. The pattern of findings for Asian American students (i.e., high levels of initial distress but less engagement in treatment) strongly suggests that this clientele has great clinical needs but may not find specialized office-centric mental health services to be a viable means for addressing these needs. Despite disaggregating by specific Asian ethnic groups, the findings showed that these problems were largely shared across Asian ethnic groups. As Kazdin and Blase (2011) have noted, there is an urgent need for innovative approaches to provide mental health services to those who clearly need such services but fail to receive or use them. For racial/ethnic minority students, web-based interventions may be especially useful in circumventing the stigma associated with mental health problems by providing psychoeducational information in a more accessible yet private context. Another avenue may be to leverage peers as resources through peer mentoring programs and student organizations that are culturally focused. This type of outreach may be especially helpful for Latino/a students who are often first-generation college students. They may thus benefit from developing a network of peers focused on providing resources and social support. Web-based outreach programs could be used to increase the mental health literacy of college students in general, to become more knowledgeable about mental health issues, learn about effective self-help methods, and gain more information on available campus-based resources. These types of programs can also provide psychoeducation in terms of what to expect from treatment, which may help increase the likelihood that clients will stay long enough to receive the minimum dosage level needed to benefit from mental health care. Therapists who work with racial/ethnic minority clients may need to assess client expectations in terms of what he/she expects from the therapist and adapt their methods to meet clients’ needs. It is clear that university counseling services are pivotal in delivering direly needed mental health care on college campuses. Our study has identified specific areas that are particularly important to the provision of effective mental health care for racial/ethnic minority students.
References
- Aldwin C, Greenberger E. Cultural differences in the predictors of depression. American Journal of Community Psychology. 1987;15(6):789–813. doi: 10.1007/BF00919803. [DOI] [PubMed] [Google Scholar]
- Arbona C, Jimenez C. Minority stress, ethnic identity, and depression among Latino/a college students. Journal of Counseling Psychology. 2014;61(1):162–168. doi: 10.1037/a0034914. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Benton SA, Robertson JM, Tseng WC, Newton FB, Benton SL. Changes in counseling center client problems across 13 years. Professional Psychology: Research and Practice. 2003;34(1):66–72. doi: 10.1037/0735-7028.34.1.66. [DOI] [Google Scholar]
- Cabassa LJ, Zayas LH. Latino immigrants’ intentions to seek depression care. American Journal of Orthopsychiatry. 2007;77(2):231–242. doi: 10.1037/0002-9432.77.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabral RR, Smith TB. Racial/ethnic matching of clients and therapists in mental health services: A meta-analytic review of preferences, perceptions, and outcomes. Journal of Counseling Psychology. 2011;58(4):537–554. doi: 10.1037/a0025266. [DOI] [PubMed] [Google Scholar]
- Castillo LG, Navarro RL, Walker JEOY, Schwartz SJ, Zamboanga BL, Whitbourne SK, Caraway SJ. Gender matters: The influence of acculturation and acculturative stress on Latino college student depressive symptomatology. Journal of Latina/o Psychology. 2015;3(1):40–55. doi: 10.1037/lat0000030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Collegiate Mental Health. 2013 Annual Report. 2014 Jan; Publication No. STA 14-43. Retrieved from http://sites.psu.edu/ccmh/wp-content/uploads/sites/3058/2014/05/2013_CCMH_Report1.pdf.
- Chang J, Chen CN, Alegría M. Contextualizing social support: Pathways to help seeking in Latinos, Asian Americans, and Whites. Journal of Social and Clinical Psychology. 2014;33(1):1–24. doi: 10.1521/jscp.2014.33.1.1. [DOI] [Google Scholar]
- Chang J, Natsuaki MN, Chen CN. The importance of family factors and generation status: Mental health service use among Latino and Asian Americans. Cultural Diversity and Ethnic Minority Psychology. 2013;19(3):236–247. doi: 10.1037/a0032901. [DOI] [PubMed] [Google Scholar]
- Cheng HL, Kwan KLK, Sevig T. Racial and ethnic minority college students’ stigma associated with seeking psychological help: Examining psychocultural correlates. Journal of Counseling Psychology. 2013;60(1):98–111. doi: 10.1037/a0031169. [DOI] [PubMed] [Google Scholar]
- Choi KH, Buskey W, Johnson B. Evaluation of counseling outcomes at a university counseling center: The impact of clinically significant change on problem resolution and academic functioning. Journal of Counseling Psychology. 2010;57(3):297–303. doi: 10.1037/a0020029. [DOI] [PubMed] [Google Scholar]
- Constantino MJ, Arnkoff DB, Glass CR, Ametrano RM, Smith JZ. Expectations. Journal of Clinical Psychology. 2011;67(2):184–192. doi: 10.1002/jclp.20754. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. SCL-90-R Revised Manual. Baltimore, MD: Johns Hopkins School of Medicine; 1983. [Google Scholar]
- Draper MR, Jennings J, Baron A, Erdur O, Shankar L. Time-limited counseling outcome in a nationwide college counseling center sample. Journal of College Counseling. 2002;5(1):26. doi: 10.1002/j.2161-1882.2002.tb00204.x. [DOI] [Google Scholar]
- Durvasula R, Sue S. Severity of disturbance among Asian American outpatients. Cultural Diversity and Mental Health. 1996;2(1):43–51. doi: 10.1037/1099-9809.2.1.43. [DOI] [PubMed] [Google Scholar]
- Eisenberg D, Golberstein E, Gollust SE. Help-seeking and access to mental health care in a university student population. Medical Care. 2007;45(7):594–601. doi: 10.1097/MLR.0b013e31803bb4c1. [DOI] [PubMed] [Google Scholar]
- Gallagher RP. National survey of counseling center directors. The International Association of Counseling Services, Inc; 2005. Monograph Series Number 8O. Retrieved from http://www.collegecounseling.org/pdf/2005_survey.pdf. [Google Scholar]
- Goldfried MR. On entering and remaining in psychotherapy. Clinical Psychology: Science and Practice. 2012;19(2):125–128. doi: 10.1111/j.1468-2850.2012.01278.x. [DOI] [Google Scholar]
- Gregersen AT, Nebeker RS, Seely KL, Lambert MJ. Social validation of the Outcome Questionnaire-45: An assessment of Asian and Pacific Islander college students. Journal of Multicultural Counseling and Development. 2004;32(4):194–205. doi: 10.1002/j.2161-1912.2004.tb00627.x. [DOI] [Google Scholar]
- Gupta A, Szymanski DM, Leong FTL. The “model minority myth”: Internalized racialism of positive stereotypes as correlates of psychological distress, and attitudes toward help-seeking. Asian American Journal of Psychology. 2011;2(2):101–114. doi: 10.1037/a0024183. [DOI] [Google Scholar]
- Hayes JA, Owen J, Bieschke KJ. Therapist differences in symptom change with racial/ethnic minority clients. Psychotherapy. 2014 doi: 10.1037/a0037957. [DOI] [PubMed] [Google Scholar]
- Hayes JA, Youn SJ, Castonguay LG, Locke BD, McAleavey AA, Nordberg S. Rates and predictors of counseling center use among college students of color. Journal of College Counseling. 2011;14(2):105–116. doi: 10.1002/j.2161-1882.2011.tb00266.x. [DOI] [Google Scholar]
- Hovey JD, Kim SE, Seligman LD. The influences of cultural values, ethnic identity, and language use on the mental health of Korean American college students. The Journal of Psychology. 2006;140(5):499–511. doi: 10.3200/JRLP.140.5.499-511. [DOI] [PubMed] [Google Scholar]
- Ibaraki AY, Hall GCN. The components of cultural match in psychotherapy. Journal of Social and Clinical Psychology. 2014;33(10):936–953. doi: 10.1521/jscp.2014.33.10.936. [DOI] [Google Scholar]
- Kazdin AE, Blase SL. Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspectives on Psychological Science. 2011;6(1):21–37. doi: 10.1177/1745691610393527. [DOI] [PubMed] [Google Scholar]
- Kearney LK, Draper M, Barón A. Counseling utilization by ethnic minority college students. Cultural Diversity and Ethnic Minority Psychology. 2005;11(3):272–285. doi: 10.1037/1099-9809.11.3.272. [DOI] [PubMed] [Google Scholar]
- Krumrei EJ, Newton FB, Kim E. A multi-institution look at college students seeking counseling: Nature and severity of concerns. Journal of College Student Psychotherapy. 2010;24(4):261–283. doi: 10.1080/87568225.2010.509223. [DOI] [Google Scholar]
- Lambert MJ, Morton JJ, Hatfield D, Harmon C, Hamilton S, Reid RC, et al. Administration and scoring manual for the OQ-45.2 (Outcome Questionnaire) Stevenson, MD: American Professional Credentialing Services; 2004. [Google Scholar]
- Lambert MJ, Smart DW, Campbell MP, Hawkins EJ, Harmon C, Slade KL. Psychotherapy outcome, as measured by the OQ-45, in African American, Asian/Pacific Islander, Latino/a, and Native American clients compared with matched Caucasian clients. Journal of College Student Psychotherapy. 2006;20(4):17–29. doi: 10.1300/J035v20n0403. [DOI] [Google Scholar]
- Lee S, Juon HS, Martinez G, Hsu CE, Robinson ES, Bawa J, Ma GX. Model minority at risk: Expressed needs of mental health by Asian American young adults. Journal of Community Health. 2009;34(2):144–152. doi: 10.1007/s10900-008-9137-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leong FTL, Lau ASL. Barriers to providing effective mental health services to Asian Americans. Mental Health Services Research. 2001;3(4):201–214. doi: 10.1023/A:1013177014788. [DOI] [PubMed] [Google Scholar]
- Liu CH, Murakami J, Eap S, Hall GCN. Who are Asian Americans? An overview of history, immigration, and communities. In: Tewari N, Alvarez AN, editors. Asian American psychology: Current perspectives. New York, NY: Lawrence Erlbaum Associates; 2009. pp. 1–29. [Google Scholar]
- Lockard AJ, Hayes JA, Graceffo JM, Locke BD. Effective counseling for racial/ethnic minority clients: Examining changes using a practice research network. Journal of College Counseling. 2013;16(3):243–257. doi: 10.1002/j.2161-1882.2013.00040.x. [DOI] [Google Scholar]
- Locke BD, McAleavey AA, Zhao Y, Lei PW, Hayes JA, Castonguay LG, Lin YC. Development and initial validation of the counseling center assessment of psychological symptoms-34. Measurement and Evaluation in Counseling and Development. 2012;45(3):151–169. doi: 10.1177/0748175611432642. [DOI] [Google Scholar]
- Lopez MH, Gonzalez-Barrera A, Cuddington D. Diverse origins: The nation’s 14 largest Hispanic-origin groups. Washington, DC: Pew Research Center; 2013. Retrieved from http://www.pewhispanic.org/files/2013/06/summary_report_final.pdf. [Google Scholar]
- Maramba GG, Hall GCN. Meta-analyses of ethnic match as a predictor of dropout, utilization, and level of functioning. Cultural Diversity and Ethnic Minority Psychology. 2002;8(3):290–297. doi: 10.1037/1099-9809.8.3.290. [DOI] [PubMed] [Google Scholar]
- Minami T, Davies DR, Tierney SC, Bettmann JE, McAward SM, Averill LA, Wampold BE. Preliminary evidence on the effectiveness of psychological treatments delivered at a university counseling center. Journal of Counseling Psychology. 2009;56(2):309–320. doi: 10.1037/a0015398. [DOI] [Google Scholar]
- Misner J. Seeking help at a campus counseling center? Take a number. The Chronicle of Higher Education. 2014 Oct 10; Retrieved from http://chronicle.come/article/Seeking-Help-at-a-Campus/149321/
- Mueller RM, Lambert MJ, Burlingame GM. Construct validity of the Outcome Questionnaire: A confirmatory factor analysis. Journal of Personality Assessment. 1998;70(2):248–262. doi: 10.1207/s15327752jpa7002_5. [DOI] [Google Scholar]
- Owen J, Imel Z, Adelson J, Rodolfa E. “No-show”: Therapist racial/ethnic disparities in client unilateral termination. Journal of Counseling Psychology. 2012;59(2):314–320. doi: 10.1037/a0027091. [DOI] [PubMed] [Google Scholar]
- Rosenthal B, Wilson WC. Mental health services: Use and disparity among diverse college students. Journal of American College Health. 2008;57(1):61. doi: 10.3200/JACH.57.1.61-68. [DOI] [PubMed] [Google Scholar]
- Saw A, Berenbaum H, Okazaki S. Influences of personal standards and perceived parental expectations on worry for Asian American and White American college students. Anxiety, Stress, and Coping. 2013;26(2):187–202. doi: 10.1080/10615806.2012.668536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7(2):147–177. doi: 10.1037/1082-989X.7.2.147. [DOI] [PubMed] [Google Scholar]
- Schlomer GL, Bauman S, Card NA. Best practices for missing data management in counseling psychology. Journal of Counseling Psychology. 2010;57(1):1–10. doi: 10.1037/a0018082. [DOI] [PubMed] [Google Scholar]
- Sinharay S, Stern HS, Russell D. The use of multiple imputation for the analysis of missing data. Psychological Methods. 2001;6(4):317–329. doi: 10.1037/1082-989X.6.4.317. [DOI] [PubMed] [Google Scholar]
- Snell MN, Mallinckrodt B, Hill RD, Lambert MJ. Predicting counseling center clients’ response to counseling: A 1-year follow-up. Journal of Counseling Psychology. 2001;48(4):463–473. doi: 10.1037/0022-0167.48.4.463. [DOI] [Google Scholar]
- Snyder TD, Dillow SA. Digest of education statistics 2011. Washington, DC: U.S. Department of Education; 2012. (No. NCES 2012-001) Retrieved from http://nces.ed.gov/pubs2012/2012001_0.pdf. [Google Scholar]
- Sue S, Cheng JKY, Saad CS, Chu JP. Asian American mental health: A call to action. American Psychologist. 2012;67(7):532–544. doi: 10.1037/a0028900. [DOI] [PubMed] [Google Scholar]
- Sue S, Fujino DC, Hu L, Takeuchi DT, Zane NWS. Community mental health services for ethnic minority groups: A test of the cultural responsiveness hypothesis. Journal of Consulting and Clinical Psychology. 1991;59(4):533–540. doi: 10.1037/0022-006X.59.4.533. [DOI] [PubMed] [Google Scholar]
- Sue S, Okazaki S. Asian-American educational achievements: A phenomenon in search of an explanation. Asian American Journal of Psychology. 2009;S(1):45–55. doi: 10.1037/1948-1985.S.1.45. [DOI] [PubMed] [Google Scholar]
- Sue S, Zane N. The role of culture and cultural techniques in psychotherapy: A critique and reformulation. American Psychologist. 1987;42(1):37–45. doi: 10.1037/0003-066X.42.1.37. [DOI] [PubMed] [Google Scholar]
- Tracey TJ, Leong FT, Glidden C. Help seeking and problem perception among Asian Americans. Journal of Counseling Psychology. 1986;33(3):331–336. doi: 10.1037/0022-0167.33.3.331. [DOI] [Google Scholar]
- Turcios-Cotto VY, Milan S. Racial/ethnic differences in the educational expectations of adolescents: Does pursuing higher education mean something different to Latino students compared to White and Black students? Journal of Youth and Adolescence. 2012;42(9):1399–1412. doi: 10.1007/s10964-012-9845-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Education, National Center for Education Statistics. Digest of education statistics. 2013. NCES 2014-015. [Google Scholar]
- Vonk ME, Thyer BA. Evaluating the effectiveness of short-term treatment at a university counseling center. Journal of Clinical Psychology. 1999;55(9):1095–1106. doi: 10.1002/(SICI)1097-4679(199909)55:9<1095::AID-JCLP7>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- Wilson SB, Mason TW, Ewing MJM. Evaluating the impact of receiving university-based counseling services on student retention. Journal of Counseling Psychology. 1997;44(3):316–320. doi: 10.1037/0022-0167.44.3.316. [DOI] [Google Scholar]
- Wolgast BM, Lambert MJ, Puschner B. The dose-response relationship at a college counseling center: Implications for setting session limits. Journal of College Student Psychotherapy. 2003;18(2):15–29. doi: 10.1300/J035v18n02_03. [DOI] [Google Scholar]
- Wong EC, Beutler LE, Zane NW. Using mediators and moderators to test assumptions underlying culturally sensitive therapies: An exploratory example. Cultural Diversity and Ethnic Minority Psychology. 2007;13(2):169–177. doi: 10.1037/1099-9809.13.2.169. [DOI] [PubMed] [Google Scholar]
- Young CB, Fang DZ, Zisook S. Depression in Asian–American and Caucasian undergraduate students. Journal of Affective Disorders. 2010;125(1–3):379–382. doi: 10.1016/j.jad.2010.02.124. [DOI] [PubMed] [Google Scholar]