Abstract
Background
We assessed in-hospital mortality and utilization of invasive cardiac procedures following Acute Coronary Syndrome (ACS) admissions on the weekend versus weekdays over the past decade in the United States.
Methods
We used data from the Nationwide Inpatient Survey (2001–2011) to examine differences in all-cause in-hospital mortality between patients with a principal diagnosis of ACS admitted on a weekend versus a weekday. Adjusted and hierarchical logistic regression model analysis was then used to identify if weekend admission was associated with a decreased utilization of procedural interventions and increased subsequent complications as well.
Results
13,988,772 ACS admissions were identified. Adjusted mortality was higher for weekend admissions for Non-ST-Elevation Acute Coronary Syndromes [OR: 1.15, 95% CI, 1.14–1.16] and only somewhat higher for ST-Elevation Myocardial Infarction [OR: 1.03; 95% CI, 1.01–1.04]. Additionally, patients were significantly less likely to receive coronary revascularization intervention/therapy on their first day of admission [OR: 0.97, 95% CI: 0.96–0.98 and OR: 0.75, 95% CI: 0.75–0.75 for STEMI and NSTE-ACS respectively]. For ACS patients admitted during the weekend who underwent procedural interventions, in-hospital mortality and complications were higher as compared to patients undergoing the same procedures on weekdays.
Conclusion
For ACS patients, weekend admission is associated with higher mortality and lower utilization of invasive cardiac procedures, and those who did undergo these interventions had higher rates of mortality and complications than their weekday counterparts. This data leads to the possible conclusion that access to diagnostic/interventional procedures may be contingent upon the day of admission, which may impact mortality.
Introduction
Acute coronary syndrome (ACS) accounts for approximately 1.4 million hospital admissions per year in the United States[1]. With an annual incidence of approximately six cases per every 10,000 persons[2], ACS represents a common medical emergency that has shown marked improvement in morbidity and mortality when diagnostic procedures as well as percutaneous or thrombolytic therapies are initiated within an appropriate timeframe. Studies have consistently shown that timeliness of revascularization through percutaneous coronary intervention (PCI), and fibrinolytic therapy in the absence of contraindications and when PCI is not available, are the major prognostic factors in improving patient survival in ST-Elevation myocardial infarction (STEMI)[3–6]. Current guidelines dictate no more than a 90-minute window for the door-to-balloon time interval [6]. For this reason, patients with clinical suspicion of ACS are rapidly assessed to determine if they are suffering from acute ischemia. While STEMI patients have been clearly shown to benefit from early revascularization, patients with Non–ST-Elevation Acute Coronary Syndromes (NSTE-ACS) also derive a benefit. The current American College of Cardiology/American Heart Association (ACC/AHA) guidelines for the treatment of NSTE-ACS, endorse an early invasive approach, given the clinical benefit [7].
Although many hospitals provide emergency care on weekends, studies have shown that the level of expertise is reduced, and health care staff are significantly less accessible during weekends [8]. Consequently, patients presenting with time-sensitive medical emergencies such as intracerebral hemorrhage, ruptured aortic aneurysm and acutely decompensated heart failure on the weekend have shown increased mortality and poor outcomes [9–11]. Similarly, patients with acute myocardial infarction (MI) admitted during off-hours have been shown to have an increase in mortality, in addition to less usage of and increased time to invasive cardiac procedures [12, 13]. However, previous studies have been limited by either only including those suffering from ST-Elevation Myocardial Infarction (STEMI), a single component of ACS, or they have been limited by using a restricted regional cohort, such as data from a single state [14]. While the underlying cause of ACS dictates the appropriate intervention, and its timing, it is likely that those patients who present with ACS requiring revascularization are likely to have worse outcomes when admitted during the weekend, compared to those admitted during the weekdays.
In order to quantify the potential differences in admission timing outcomes, a direct comparison between patients admitted from Monday to Friday with those admitted on the weekend is necessary. Here eleven-year data abstracted from the 2001–2011 Nationwide Inpatient Sample (NIS) was used in order to compare outcomes of those admitted with a principal diagnosis of STEMI or NSTE-ACS on the weekends and weekdays. Additionally, the rates of procedural usage were compared, as were procedural complication rates.
Methods
Data Sources
We conducted a retrospective cohort study using the eleven-year data from Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project National Inpatient Sample (NIS) database. NIS is the largest publicly available all-payer inpatient care database, including discharge codes from more than 1,000 hospitals in 44 states. The NIS database was designed as a stratified, 20% representative sample of all nonfederal US hospitals, and is regularly used to identify national trends in healthcare utilization, charges, quality and outcomes.
Each hospitalization record includes patient-level characteristics such as discharge status, demographic information, length of stay, primary payer status, and clinical data coded using International Classification of Disease, Ninth Revision (ICD-9) diagnosis and procedure codes. The NIS database sample has been validated using Medicare inpatient claims for percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) [15]. Additionally, this database includes hospital-level characteristics such as the number of hospitals beds and hospital location as abstracted from the AHA Annual Survey of Hospitals. Similarly, NIS classifies hospitals with teaching affiliation if the hospitals are either accredited through the Accreditation Council for a Graduate Medical Education-approved residency program, are a member of the Council of Teaching Hospitals, or have a ratio of full-time equivalent interns and residents to beds of ≥0.25%.
Study Population
We included all patients aged ≥18 who were hospitalized with a primary diagnosis code of ACS (ICD-9 code 410, 411, and 413). The positive predictive value of ICD-9 codes for ACS has been validated in prior studies [16–18]. We limited the patient population to those with less than 7-day hospital stays, as patients with longer length of stays tend to have other complications and comorbidities not related to ACS. Lengthier hospital stays have been linked with less evidence-based care [19, 20]. Additionally, hospitals without the capability to perform ACS related procedures (e.g. Diagnostic Angiography, PCI, CABG) were excluded from the study. Finally, patients transferred to the hospital from a different acute care hospital, or from another type of health facility were also excluded, as this would in most cases delay the time to procedural intervention.
The patients were additionally stratified by the classification of their ACS. STEMI and NSTE-ACS were separated in order to examine the differences between both groups. This is distinction is important, as while STEMI patients should be, and are typically treated with urgent revascularization, the early invasive strategy has been less adopted in the treatment of NSTE-ACS [6, 7].
Independent Variables of Interest
As in previous studies, weekend admissions were defined as those occurring between 12:00 AM Saturday through 11:59 PM Sunday. [9, 21] All other admissions were considered to be weekday admissions. This is the definition used by NIS and cannot be modified. For those patients included in the study, their patient-level demographics (age, gender and race), primary payer status, and individual comorbid conditions were identified.
The agency for healthcare research and quality Elixhauser adjustment scheme was used for the presence of 29 chronic comorbidities, including cardiovascular risk factors such as hyperlipidemia and hypertension, which are likely to have been present on admission and have been associated with increased in-hospital mortality. [22, 23] Additionally, we used All Patient refined Diagnosis Related Groups (APR-DRG) severity measure developed by 3M Health Information symptoms, as well as the number of chronic conditions, to identify if ACS patients admitted during the weekend were at a higher risk for mortality compared to those admitted during the weekdays.
3M developed APR-DRG methodology to allow large cohort analyses of outcomes for a given diagnostic group. [24] The APR-DRG scores use primary and secondary diagnosis, age, and preexisting medical conditions from discharge billing codes to rank the risk of mortality as low, medium, high, and extreme. This scoring system designed to specifically exclude codes reflecting in-hospital complications.
A chronic condition in NIS dataset is defined as a condition that lasts 12 months or longer and meets one or both of the following: (a) it places limitations on self-care, independent living, and social interactions; (b) it results in the need, for ongoing intervention with medical products, services, and special equipment [23]. Finally, we identified hospital characteristics, which included hospital bed-size (small, medium, or large) as assessed by the number of short-term acute-care beds, hospital location (rural or urban) and teaching affiliation.
Outcomes
The primary outcome of this study was in-hospital mortality among ACS patients admitted during the weekend as compared to the weekdays. Furthermore, differences in procedural usage and length of stay (LOS) between weekday and weekend ACS admissions were investigated. Finally, the differential usage of coronary revascularization intervention/therapy (Coronary angiography/PCI, thrombolytic therapy, and CABG) in ACS during weekday versus weekend admissions was evaluated, along with the effects on in-hospital mortality and major procedural complications (ICD-9 defined vascular, neurological, and mechanical complications; Appendix 1).
Appendix 1.
Percutaneous Coronary Intervention and Coronary Artery Bypass Graft Procedure Complications
| Procedure | ICD 9 Codes |
|---|---|
| PCI/Angiography | 997.1, 998, 998.1, 998.12, 998.11, E87.90, 459.0, 442.0, 442.3, 447.0, 444.22, 997.0, 997.00, 997.01, 997.02, 997.09, 996.62, 998.9, v15.08, 997.5 |
| CABG | 997.1, 998, 998.0, 998.1, 998.11, 998.12, 998.13, 997.0, 997.00, 997.01, 997.02, 997.09, 996, 996.0, 996.03, 996.1, 996.6, 996.61, 996.62, 996.72 |
| Thrombolytic Therapy | 997.0, 997.00, 997.01, 997.02, 997.09, 997.1, 998.11, 459.0 |
Note. Percutaneous Coronary Intervention, PCI; Coronary Artery Bypass Graft, CABG.
Statistical Analysis
For ACS patients admitted during the weekend and the weekdays, the admissions were compared based upon patient demographics, primary payer status, comorbidities, and previously identified hospital-level characteristics using chi-square tests for categorical variables and a two-sample t-test for continuous variables. Univariate logistic regression analysis was used to compare the mortality rates between weekend and weekday admissions. A separate multivariate logistic model was conducted based on adjustments for patient demographics, primary payer status, Elixhauser comorbidities, hospital bed-size, hospital location, and hospital teaching affiliation. Variables were additionally tested for mutlicollinearity through the use of two-way interaction terms. Interaction terms that were significant at p<0.05 have been included in the final model. The hospital ID was then added as random effect to eliminate the possibility that the weekend effect was limited to certain hospitals.
In separate unadjusted and adjusted multivariate models, logistic regression analysis was used to identify if weekend admissions were significantly associated with usage of coronary revascularization intervention/therapy (Coronary angiography/PCI, CABG, and thrombolytic therapy), usage of procedural interventions on the 1st day of admission, patient LOS>3 days, and survivor LOS>3 days. Unadjusted and adjusted logistic regression models were also used to identify if weekend admissions were significantly associated with increased mortality and complications in those ACS patients who received any of cardiac procedures. All statistical analysis was carried out using SAS 9.3, Cary, NC. The significance level was set at 0.05.
Results
Baseline characteristics of the cohort
From the sample of 426,949,182 hospital admissions between 2001 and 2011 in the NIS database, we identified 13,988,772 admissions with an ACS diagnosis of which 20.88% (2,921,589) were admitted during the weekend. Table 1 shows admission and patient characteristics of the total cohort of ACS patients, stratified by weekend versus weekday admission, and further stratification by STEMI and NSTE-ACS. The average age of the population was 65 ± 15 years, with 43.3% of the patients being female.
Table 1.
Baseline Comparison of Characteristics of Admitted Acute Coronary Syndrome Patients Stratified by Weekday vs. Weekend Admission
| STEMI | NSTE-ACS | |||||
|---|---|---|---|---|---|---|
| Weekday | Weekend | P | Weekday | Weekend | P | |
| Total (13988772) | 1447583 (73.44) | 523612 (26.56) | 9619600 (80.05) | 2397977 (19.95) | ||
| Age, mean (SD) | 63.32 (14.25) | 62.86 (14.50) | <0.0001 | 66.01 (14.61) | 66.99 (15.52) | <0.0001 |
| Male (%) | 66.60 | 67.00 | <0.0001 | 57.35 | 54.50 | <0.0001 |
| Race (%) | <0.0001 | <0.0001 | ||||
| White | 80.32 | 79.99 | 78.53 | 77.13 | ||
| Black | 6.99 | 7.45 | 9.51 | 10.90 | ||
| Hispanic | 6.98 | 6.89 | 7.10 | 7.38 | ||
| Asian | 1.98 | 2.08 | 1.65 | 1.63 | ||
| Native American | 0.41 | 0.40 | 0.47 | 0.49 | ||
| Other | 3.32 | 3.19 | 2.76 | 2.48 | ||
| Primary Payer (%) | <0.0001 | <0.0001 | ||||
| Medicare | 44.00 | 42.21 | 56.78 | 59.39 | ||
| Medicaid | 5.33 | 5.43 | 5.91 | 6.45 | ||
| Private | 39.55 | 40.93 | 30.10 | 26.07 | ||
| Self-pay | 7.20 | 7.47 | 4.16 | 5.03 | ||
| No Charge | 0.58 | 0.65 | 0.41 | 0.48 | ||
| Other | 3.35 | 3.30 | 2.64 | 2.58 | ||
| Location of hospital (%) | <0.0001 | <0.0001 | ||||
| Rural | 11.06 | 11.29 | 14.24 | 16.82 | ||
| Urban | 88.94 | 88.71 | 85.76 | 83.18 | ||
| Teaching status of hospital (%) | <0.0001 | <0.0001 | ||||
| Teaching | 46.41 | 45.22 | 43.69 | 38.59 | ||
| Nonteaching | 53.59 | 54.78 | 56.31 | 61.41 | ||
| Bed-size of hospital (%) | <0.0001 | <0.0001 | ||||
| Small | 9.00 | 8.80 | 10.42 | 11.34 | ||
| Medium | 23.25 | 23.61 | 23.70 | 25.33 | ||
| Large | 67.76 | 67.59 | 65.88 | 63.33 | ||
| AHRQ comorbidity measure (%) | ||||||
| Congestive heart failure | 1.59 | 1.42 | <.0001 | 2.75 | 3.44 | <.0001 |
| Chronic obstructive pulmonary disease | 13.72 | 13.31 | <.0001 | 17.17 | 19.00 | <.0001 |
| Depression | 4.16 | 4.11 | 0.1407 | 6.16 | 6.82 | <.0001 |
| Diabetes | 23.99 | 23.89 | 0.1572 | 31.41 | 32.13 | <.0001 |
| Hypertension | 55.29 | 54.88 | <.0001 | 64.10 | 63.07 | <.0001 |
| Fluid and electrolyte disorders | 10.19 | 11.11 | <.0001 | 9.37 | 12.97 | <.0001 |
| Morbid Obesity | 8.53 | 8.84 | <.0001 | 9.44 | 9.29 | <.0001 |
| Renal failure | 5.06 | 5.07 | 0.9563 | 8.02 | 10.03 | <.0001 |
| Valvular disease | 0.37 | 0.35 | 0.0386 | 1.09 | 1.31 | <.0001 |
| Hyperlipidemia | 48.74 | 48.78 | 0.5763 | 49.97 | 45.95 | <.0001 |
| Number of chronic conditions, mean (SD) | 5.85 (2.30) | 5.84 (2.26) | 0.3503 | 5.81 (2.71) | 6.31 (2.80) | <0.0001 |
P-values obtained from chi-square analyses for discrete variables, and Student t-test for continuous variables.
Note. ST-elevation myocardial infarction, Non-ST-elevation Acute Coronary Syndrome, NSTE-ACS.
There were some differences between the two cohorts; ACS patients were more likely to be admitted to nonteaching hospitals during the weekdays (p<0.0001). In contrast to STEMI patients, NSTE-ACS patients admitted on the weekend had higher number of chronic conditions, and an overall higher risk of mortality (p< 0.0001). In addition, STEMI patients were more likely to be admitted during weekend in contrast to NSTE-ACS patients who had more weekday admissions.
Overall Mortality in ACS Admitted Weekday vs Weekend Patients
The unadjusted in-hospital mortality odds ratios (OR) were 1.04 (95% CI, 1.03–1.05) and 1.43 (95% CI, 1.42–1.44) for weekend admissions of STEMI and NSTE-ACS patients respectively. This increase in mortality for weekend admissions remained significant after the multivariable logistics regression model (OR, 1.03; 95% CI, 1.01–1.04 for STEMI and OR, 1.15; 95% CI, 1.14–1.16 for NSTE-ACS) (Table 2). Within this model, the hospital-level characteristic of teaching affiliation was associated with an increase in mortality for weekend admitted ACS patients (OR, 1.11; 95% CI, 1.09–1.12 and 1.06; 95% CI, 1.05–1.07 for STEMI and NSTE-ACS respectively). The ORs for mortality remained unchanged, even in the hierarchical logistic regression model, where we used hospital ID as the random-effect variable, suggesting that hospitals do not differ statistically in their higher weekend mortality, after accounting for all the covariates.
Table 2.
Multivariate Analysis of Predictors of Mortality among Hospitalized Patients with Acute Coronary Syndrome
| STEMI | NSTE-ACS | |||
|---|---|---|---|---|
| Odds Ratio (95% CI) | P-Value | Odds Ratio (95% CI) | P-Value | |
| Weekend* | 1.03 (1.01–1.04) | <.0001 | 1.15 (1.14–1.16) | <.0001 |
| Age | 1.053 (1.053–1.054) | <.0001 | 1.053 (1.053–1.054) | <.0001 |
| Male | 0.78 (0.77–0.79) | <.0001 | 1.03 (1.02–1.04) | <.0001 |
| Race | ||||
| White | Reference | Reference | ||
| Black | 1.05 (1.02–1.08) | <.0001 | 1.03 (1.02–1.05) | <.0001 |
| Hispanic | 1.09 (1.06–1.12) | <.0001 | 0.99 (0.97–1.01) | 0.4916 |
| Asian | 1.22 (1.16–1.27) | <.0001 | 1.12 (1.09–1.15) | <.0001 |
| Native American | 0.85 (0.74–0.96) | 0.0136 | 1.09 (1.02–1.16) | 0.0087 |
| Other | 1.08 (1.04–1.13) | 0.0001 | 1.01 (0.98–1.03) | 0.4506 |
| Primary Payer (%) | ||||
| Medicare | Reference | Reference | ||
| Medicaid | 1.14 (1.10–1.19) | <.0001 | 1.21 (1.18–1.24) | <.0001 |
| Private | 0.71 (0.69–0.72) | <.0001 | 0.93 (0.92–0.94) | <.0001 |
| Self-pay | 1.18 (1.14–1.22) | <.0001 | 1.60 (1.56–1.65) | <.0001 |
| No Charge | 0.84 (0.75–0.95) | 0.0046 | 1.03 (0.94–1.13) | 0.4757 |
| Other | 0.91 (0.86–0.96) | 0.0008 | 1.46 (1.41–1.50) | <.0001 |
| Location of Hospital (%) | ||||
| Urban | Reference | Reference | ||
| Rural | 0.83 (0.81–0.85) | <.0001 | 0.94 (0.93–0.96) | <.0001 |
| Teaching status of hospital (%) | ||||
| Nonteaching | Reference | Reference | ||
| Teaching | 1.11 (1.09–1.12) | <.0001 | 1.06 (1.05–1.07) | <.0001 |
| Bedsize of hospital (%) | ||||
| Large | Reference | Reference | ||
| Medium | 0.90 (0.88–0.92) | <.0001 | 0.96 (0.95–0.97) | <.0001 |
| Small | 0.80 (0.78–0.82) | <.0001 | 0.88 (0.87–0.90) | <.0001 |
Adjusted for Age, Sex, Race, Year of admission, Elixhauser comorbidities, Primary Payer, Hospital Location, Hospital Teaching Status, Hospital Bed-size, and Total Hospital Admissions
Note. ST-elevation myocardial infarction, Non-ST-elevation Acute Coronary Syndrome, NSTE-ACS.
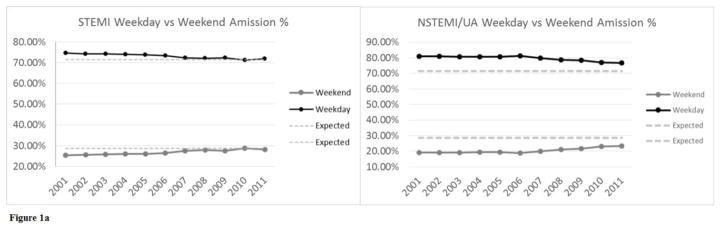
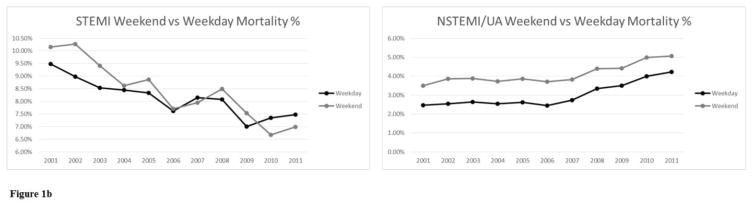
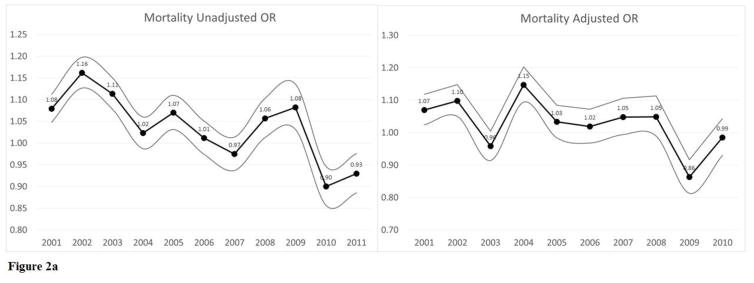
Interaction terms with weekend admission were tested to determine if the weekend admission association with in-hospital mortality differed over subgroups, including gender, race, year of admission, and comorbidities. Interaction terms were significant for “year of admission” (p-value for interaction < 0.0001). The association of weekend admission with in-hospital mortality statistically significantly differed in patients in different years between 2001 and 2011 (Fig 1 and 2). OR for adjusted in-hospital mortality for patients with STEMI were only significant for those admitted in 2002, 2003, 2005, and 2010. However, all OR for adjusted in-hospital mortality were statistically significant for patients admitted with NSTE-ACS, except for those admitted in 2009. Before 2007, NSTE-ACS patients admitted during weekends, had 16–24% higher chance of mortality compare to those admitted during weekdays. After 2007, the odds of in-hospital mortality for patients with NSTE-ACS fluctuated between 3% and 10% (Figure 2).
Figure 1.
Figure la. Percentage of weekend admissions between 2001 and 2011.
Figure lb. Percentage of weekend in hospital mortalities between 2001 and 2011.
Figure 2.
Figure 2a. Odds Ratio of weekend admissions in-hospital mortalities between 2001 and 2011 among patients with STEMI.
Figure 2b. Odds Ratio of weekend admissions in-hospital mortalities between 2001 and 2011 among patients with NSTE-ACS.
Usage of Procedural Intervention
Table 3 shows a significantly increased proportion of patients with NSTE-ACS admitted on a weekday as compared to a weekend, received some procedural intervention. After adjustment for potential confounders, the weekend admitted patients remained significantly less likely to undergo coronary angiography, PCI, or CABG (OR: 0.75, 95% CI: 0.75–0.75). The likelihood that a weekend admitted ACS patient underwent any procedure (cardiac or non-cardiac) was even less probable when restricting the use of any therapeutic intervention to the 1st day of admission for both STEMI and NSTE-ACS patients (OR, 0.58; 95% CI, 0.58–0.59 for STEMI, and 95% CI, 0.42–0.42 for NSTE-ACS). The odds of being hospitalized for more than 3 days was 1.58 times greater for NSTE-ACS patients admitted during a weekend. After adjustment for covariates, this association remained statistically significant (OR: 1.45, 95% CI: 1.44–1.46). Likewise, the unadjusted OR of a STEMI patient being hospitalized for more than 3 days was 1.25 (95% CI: 1.24–1.26). After adjustment, weekend admitted patients remained significantly more likely to stay in the hospital longer than 3 days (OR: 1.24, 95% CI: 1.22–1.25). Similarly, LOS>3 days in both STEMI and NSTE-ACS survivors was increased for weekend admitted patients (OR: 1.30, 95% CI: 1.29–1.32 and OR, 1.49; 95% CI, 1.48–1.50 for STEMI and NSTE-ACS respectively).
Table 3.
Weekend Admission’s association with Acute Coronary Syndrome Patient’s Procedural Usage and Length of Stay
| Weekday | Weekend | Unadjusted OR | Adjusted OR | |
|---|---|---|---|---|
| Cardiac procedure as the 1st procedure, after admission* | ||||
| STEMI | 46.47% | 47.62% | 1.05 (1.04–1.05) † | 0.97 (0.96–0.98) † |
| NSTE-ACS | 37.03% | 30.32% | 0.74 (0.74–0.75) † | 0.753 (0.750–0.756) † |
| Any procedure on 1st Day of Admission | ||||
| STEMI | 92.66% | 88.32% | 0.60 (0.59–0.61) † | 0.58 (0.58–0.59) † |
| NSTE-ACS | 86.23% | 73.46% | 0.44 (0.44–0.45) † | 0.42 (0.42–0.42) † |
| Length of Stay>3 days | ||||
| STEMI | 44.31% | 49.92% | 1.25 (1.24–1.26) † | 1.24 (1.22–1.25) † |
| NSTE-ACS | 33.48% | 44.35% | 1.58 (1.58–1.59) † | 1.45 (1.44–1.46) † |
| Length of Stay> 3 days in survivors | ||||
| STEMI | 46.24% | 52.93% | 1.31 (1.30–1.32) † | 1.30 (1.29–1.32) † |
| NSTE-ACS | 33.44% | 44.89% | 1.62 (1.62–1.63) † | 1.49 (1.48–1.50) † |
Adjusted for Age, Sex, Race, Year of admission, Elixhauser comorbidities, Primary Payer, Hospital Location, Hospital Teaching Status, Hospital Bed-size, and Total Hospital Admissions
Includes percutaneous coronary intervention, coronary artery bypass graft, and angiography.
p<0.05
Note. Odds Ratio, OR; ST-elevation myocardial infarction, STEMI; Non- ST-elevation Acute Coronary Syndrome, NSTE-ACS.
Mortality and Complications with Procedural Use
A larger percentage of ACS patients admitted on the weekdays underwent cardiac procedural interventions as the first procedure after admission (37.03% vs 30.32%, p<0.0001) compared to patients admitted during the weekend. Among patients who underwent ACS related interventions, the OR for unadjusted in-hospital mortality was increased for weekend admitted individuals, compared to weekday admitted counterparts (Table 4). After adjustment, the increase in mortality for both STEMI and NSTE-ACS remained significant for those undergoing PCI (OR 1.09, 95% CI 1.08–1.09 and 1.38, 95% CI 1.29–1.47 respectively). However, after adjustment, the increased in-hospital mortality in CABG was only statistically significant for NSTE-ACS patients (OR 3.09, 95% CI 2.84–3.37). Similarly, ACS patients admitted during the weekend were more likely to have complications after receiving PCI and CABG when compared to weekday admitted patients.
Table 4.
Mortality and Complications in Weekend Admitted vs Weekday Admitted ACS Patients Receiving Invasive Coronary Interventions
| STEMI | NSTE-ACS | |||
|---|---|---|---|---|
| Unadjusted OR | Adjusted OR | Unadjusted OR | Adjusted OR | |
| Mortality | ||||
| Thrombolytic Therapy | 0.98 (0.89–1.07) | 1.13 (1.13–1.14) † | - | - |
| PCI | 1.07 (1.03–1.11) † | 1.091 (1.090–1.092) † | 1.76 (1.67–1.87) † | 1.38 (1.30–1.48) † |
| CABG | 1.15 (1.06–1.24) † | 1.06 (0.95–1.19) † | 3.09 (2.91–3.28) † | 3.10 (2.85–3.37) † |
| Complications | ||||
| Thrombolytic Therapy | 1.96 (1.35–2.85) † | 2.23 (1.30–3.81) † | - | - |
| PCI | 1.03 (1.00–1.05) † | 1.05 (1.02–1.08) † | 1.07 (1.04–1.09) † | 1.07 (1.04–1.10) † |
| CABG | 1.07 (0.99–1.16) | 1.12 (1.01–1.25) † | 1.05 (1.00–1.10) † | 1.04 (0.97–1.11) |
p<0.05
Adjusted for Age, Sex, Race, Year of admission, Elixhauser comorbidities, Primary Payer, Hospital Location, Hospital Teaching Status, Hospital Bed-size, and Total Hospital Admissions
Note. Odds Ratio, OR; ST-elevation myocardial infarction, STEMI; Non- ST-elevation Acute Coronary Syndrome, NSTE-ACS; Percutaneous Coronary Intervention, PCI; Coronary Artery Bypass Graft, CABG.
Discussion
Using nationally representative data, we have shown that in-hospital mortality of patients with the principal diagnosis of NSTE-ACS was significantly higher if patients were admitted on a weekend compared to a weekday. For patients with a diagnosis of STEMI, this number, although statistically significant, is not nearly as dramatic as those patients with NSTE-ACS likely as a result of STEMI activation teams and more timely weekend interventions. These effects persisted independently of demographic characteristics, hospital characteristics, year of admission, and a wide-range of comorbid conditions.
Our results are consistent with previous studies, suggesting that outcomes are worse if patients with time-sensitive medical conditions are admitted over the weekend.[9–11] This study demonstrates the phenomena in a large, nationally representative dataset. Additionally, the increase in in-hospital mortality is demonstrated not only in the larger group of patients presenting with the overarching diagnosis of ACS, but is then stratified by the major components of ACS (STEMI, NSTE-ACS). Prior studies have studied only “Acute MI” which can be confusing and exclude some components of ACS. [25] The current ACC/AHA guidelines for treatment of NSTE-ACS suggest an “early invasive strategy”, as a Class I recommendation for initially stabilized patients, in addition to patients at high risk of clinical events (class IA), with refractory angina, and those with electrical or hemodynamic insufficiency (class IB).[7] This strategy promotes the expedited use of procedural intervention within 24 hours in order to risk stratify and treat patients with ACS, which, results in lower rates of recurrent UA, recurrent rehospitalization, MI, and death [26, 27]. Hence, inclusion of UA and NSTEMI under the umbrella of ACS in this study is important to determine if these patients admitted on the weekend are receiving appropriate guideline driven therapy, in addition to those patients who present with a STEMI.
As has been shown in previous studies, this analysis revealed that invasive cardiac procedures (coronary angiography, PCI, and CABG) are significantly less likely to be performed on weekend admitted patients. [12] This observation is perhaps related to the diminished number of staff qualified to perform invasive cardiac procedures on the weekends. [8, 28, 29] In turn, this lack of timely procedural intervention and less weekend post-procedural monitoring may increase the risk of mortality found in those ACS patients who underwent a procedure on the weekend, as compared to those who underwent weekday procedures. The observed effect persisted even after adjustment for demographics characteristics, hospital characteristics, and a wide-range of comorbidities in the studied patients. ACS patients who underwent PCI or CABG were more likely to experience severe vascular, neurological, and mechanical complications when admitted during the weekend.
These findings suggest not only a deficiency in access to life-saving procedures, but also reduced quality of care in those who receive such procedures during the weekend. Prior investigations have implied a decreased staff and increased physician per patient responsibility during the weekend as possible explanations for the decreased intensity and quality of care. [11, 30–33] It is possible that the increased mortality observed for ACS patients during the weekend is due to a combination of a lower rate of invasive interventions, and reduced hospital resources (human and mechanical) resulting in less intensive medical care after such procedures.
Another plausible interpretation for these findings is a selection bias, it is possible that the in hospital mortality increase may be due to a skewed population of severely ill patients admitted to the hospital on weekends. It could be argued that only patients with more advanced or symptomatic disease states, and those that delayed medical care to avoid missing work, would present to emergency rooms on weekends, while patients with less acute disease may delay the admission to the next working day. The significantly higher chance of mortality (APR-DRG score) among weekend admissions (17.27% vs 24.33%, P < .0001) may support this interpretation. Additionally, in this cohort, weekend admissions represented only 21% of all admissions, instead of two out of seven (28.5%), and ACS patients admitted on the weekend had higher number of chronic conditions. However, the decrease in admissions can be explained by the lack of patients being seen in weekday clinics being admitted, and by that logic, some patients who may have been appropriate for outpatient care are admitted on the weekends, which would screw the results in the opposite direction. Finally, sicker patients coming to the ER on the weekend would not explain the decreased rate of procedural intervention. Logically, such are patients would be very likely to require coronary revascularization. Additionally, there is no data to suggest that the patients who present to the ER on weekends tend to be a patient population with more medical comorbidities.
Although multivariable adjustment was implemented to adjust for baseline differences, if such a selection bias does exist, Mondays should be associated with the highest total number of admissions, highest number of patients with less severe disease and consequently the lowest death rate of the week. Unfortunately, we didn’t have the details of weekdays in our dataset to address this issue, and even in this view of the matter, this explanation, as discussed, cannot justify the significant decrease rate of ACS related procedures and procedures performed on the first day of admission, among weekend admitted individuals.
It is likely that uniform health care access over the weekend may lead to equal mortality rates on the weekends and weekdays. However, this is not an easy problem to eradicate, given the structure of group call, the increased reliance of academic hospitals on lower level residents over the weekend and inability to adequately staff angiography suites and operating rooms over the weekends. Currently, private health care institutions, whether using a foundation or group model, typically have a weekend call system that limits the number of sub-specialists available. [30] Considering the limited access to consulting physicians over the weekend, primary physicians may not have the access to procedural expertise that is needed particularly in ACS. An additional barrier in the private sector is the staffing of angiography suites and operating rooms over the weekends. [30] While weekday staff is scheduled and available, weekend staff may be sparser or offsite, and may need to be called in. Studies have shown, if weekend staff is available, many hospitals, particularly in rural areas, will limit the activation of a cardiac catheterization lab only for patients presenting with STEMI, despite the indications in NSTEMI and UA patients. [30] However, continuous onsite physician and staff coverage of angiography suites and operating rooms over the weekends is prohibitively expensive for many institutions. Finally, in the case of academic centers, data has shown that there are a limited number of typically less experienced residents who are on call over the weekend, particularly as work hour restrictions tighten, and quite frequently there is less intense attending level supervision.[34] Likewise, It has been shown that with the new restrictions, interns are doing more work than ever before.[34] This may be a possible explanation for the increase in mortality seen particularly in academic centers.
Our analysis showed a decrease in the disparity between the OR of mortality for weekend versus weekday admitted patients with STEMI and NSTE-ACS in the past decade (Figure 2). For STEMI patients, the OR of 1.07 (95% CI: 1.02–1.11) in 2002 decreased to OR of 0.99 (95% CI: 0.93–1.04) in 2011. In NSTE-ACS patients, the higher odds of mortality during weekends (OR: 1.21, 95% CI: 1.17–1.24) in 2002 decreased to 1.09 (95% CI: 1.06–1.12) in 2011. These findings can reflect recent improvement in the management of patients with AMI in the United States. Previous studies confirmed reduction in mortality and LOS of patients, mainly attributed to readily accessible diagnostic facilities, and growing physician awareness of the current guidelines. [35, 36]
Another possible explanation for the decrease in “weekend effect” in the last decade could be the increase in weekend admissions rates for both STEMI and NSTE-ACS patients. While only 18.98% of NSTE-ACS patients admitted during weekend in 2001, 23.29% of those patients were admitted on weekends in 2011, which is closer to 28.5% expected rate. For STEMI patients, weekend admission rate was 25.36% in 2001, which almost reached the two out of seven (28.5%) expected rate in 2011.
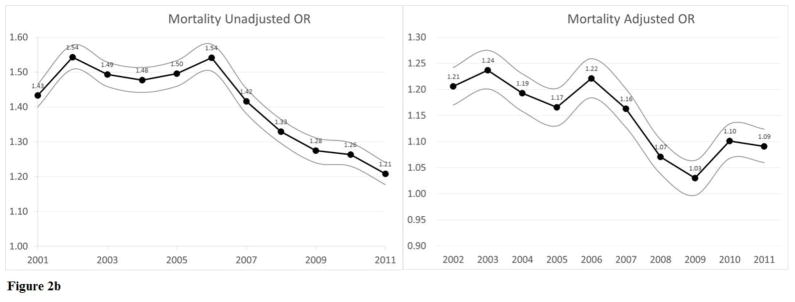
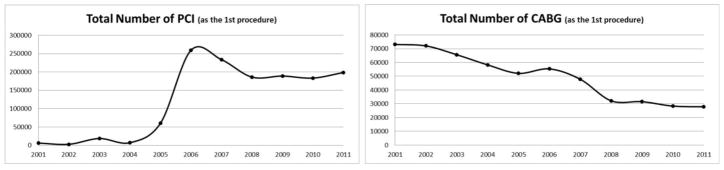
Finally, the advantages of an early invasive strategy have been consistently shown in meta-analysis of randomized trials, especially in the setting of NSTEMI. [26, 37] In our sample, the total number of PCIs performed as the 1st procedure after admission increased dramatically after 2006 (Figure 3). In weekend admitted NSTE-ACS patients, utilization of PCI on the day of admission increased from 18.5% in 2001 to 25.6% in 2011 (p<0.001). Adoption of guidelines recommending shorter door to balloon times, as well as designation of hospitals being STEMI centers largely contribute on recent improvement in the management STEMI patients in the United States. [35, 36]
Figure 3.
Total number of PCI and CABG performed between 2001 and 2011 among patients with STEMI and NSTE-ACS.
Our study has several limitations. The study population was identified on the basis of ICD-9 codes reflective of ACS. While these ICD-9 codes have been validated in prior studies [16–18, 38], it is possible that coding practices may vary among hospitals, although coding is unlikely to differ between weekday and weekend admission in a specific hospital. Another possible limitation is the fact that we were unable to consider some of the unmeasured confounders in ACS presentation when accounting for weekend versus weekday in-hospital mortality, procedure usage, and procedure complication outcomes. Although our findings were adjusted for important covariates, we did not have access to data including time to hospital presentation, emergency room waiting time, MI type and location, infarct size, left ventricular ejection fraction on admission and achievement of anticoagulation targets. Additionally, in the NIS dataset, weekend admissions are considered as only those occurring from midnight Friday to midnight Sunday. This coding misclassifies other time periods or “off hours” such as evenings, holidays and late Friday night, which are similar to weekend hours in term of reduced staffing and physician coverage. However, this would bias the results toward the null. Furthermore, stratifying for intensive care admission in our analysis was not possible, as adherence to guidelines and outcomes may be influenced by the severity of the disease presentation. Finally, our results are only reflective of in-hospital mortality, despite a large portion of mortality occurring in the post-discharge period and upon hospital readmission. Given the large population of patients covered in our sample size, some differences, while statistically significant, may not be clinically noteworthy.
In conclusion, despite these limitations, this study extends previous studies findings regarding the weekend admission effect on mortality for ACS patients, and provides new information on the nationwide trends in procedural utilization on the weekends and in NSTE-ACS. For patients with myocardial infarction, admission on weekends is associated with higher mortality in NSTE-ACS. Although, statistically significant, for STEMI admitted patients, admission on weekends was not associated with such a dramatic significant difference in mortality. Our findings suggest that the higher mortality on weekends in NSTE-ACS patients is mediated in part by the lower rate of invasive procedures. The widespread adoption of guidelines recommending prompt PCI with shorter door to balloon times, regardless of the day of the week, contributes largely to the absence of “weekend effect” in STEMI patients. We speculate that increase rates of coronary revascularization procedures, more liberal use of primary PCI, and better-quality care on weekends could improve the outcome of NSTE-ACS patients.
Finally, our findings can help individual physicians, hospitals, and policy makers to be aware and more considerate of an approximate 15% increased likelihood mortality for those NSTE-ACS patients admitted during the weekend regardless of the cause.
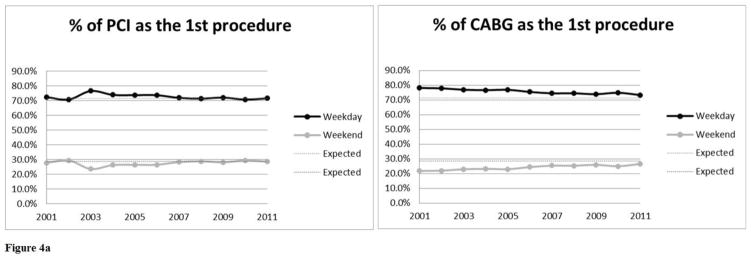
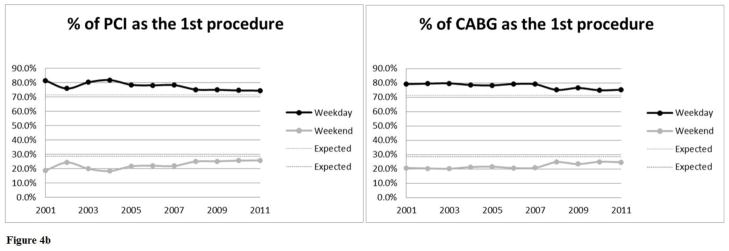
Figure 4.
Figure 4a. Percentage of PCI and CABG performed on weekdays and weekend in patients with STEMI between 2001 and 2011.
Figure 4b. Percentage of PCI and CABG performed on weekdays and weekend in patients with NSTE-ACS between 2001 and 2011.
Footnotes
Relations with Industry: None
Financial Support: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kumar A, Cannon CP. Acute coronary syndromes: diagnosis and management, part I. Mayo Clinic proceedings. 2009;84:917–38. doi: 10.4065/84.10.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sarkees ML, Bavry AA. Acute coronary syndrome (unstable angina and non-ST elevation MI) BMJ clinical evidence. 2009;2009 [PMC free article] [PubMed] [Google Scholar]
- 3.Berger PB, Ellis SG, Holmes DR, Jr, Granger CB, Criger DA, Betriu A, et al. Relationship between delay in performing direct coronary angioplasty and early clinical outcome in patients with acute myocardial infarction: results from the global use of strategies to open occluded arteries in Acute Coronary Syndromes (GUSTO-IIb) trial. Circulation. 1999;100:14–20. doi: 10.1161/01.cir.100.1.14. [DOI] [PubMed] [Google Scholar]
- 4.Cannon CP, Gibson CM, Lambrew CT, Shoultz DA, Levy D, French WJ, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. Jama. 2000;283:2941–7. doi: 10.1001/jama.283.22.2941. [DOI] [PubMed] [Google Scholar]
- 5.McNamara RL, Wang Y, Herrin J, Curtis JP, Bradley EH, Magid DJ, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. Journal of the American College of Cardiology. 2006;47:2180–6. doi: 10.1016/j.jacc.2005.12.072. [DOI] [PubMed] [Google Scholar]
- 6.O’Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the American College of Emergency Physicians and Society for Cardiovascular Angiography and Interventions. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions. 2013;82:E1–27. doi: 10.1002/ccd.24776. [DOI] [PubMed] [Google Scholar]
- 7.Amsterdam EA, Wenger NK, Brindis RG, Casey DE, Jr, Ganiats TG, Holmes DR, Jr, et al. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2014;64:e139–228. doi: 10.1016/j.jacc.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 8.Angus DC, Shorr AF, White A, Dremsizov TT, Schmitz RJ, Kelley MA, et al. Critical care delivery in the United States: distribution of services and compliance with Leapfrog recommendations. Critical care medicine. 2006;34:1016–24. doi: 10.1097/01.CCM.0000206105.05626.15. [DOI] [PubMed] [Google Scholar]
- 9.Crowley RW, Yeoh HK, Stukenborg GJ, Medel R, Kassell NF, Dumont AS. Influence of weekend hospital admission on short-term mortality after intracerebral hemorrhage. Stroke; a journal of cerebral circulation. 2009;40:2387–92. doi: 10.1161/STROKEAHA.108.546572. [DOI] [PubMed] [Google Scholar]
- 10.Groves EM, Khoshchehreh M, Le C, Malik S. Effects of weekend admission on the outcomes and management of ruptured aortic aneurysms. Journal of vascular surgery. 2014;60:318–24. doi: 10.1016/j.jvs.2014.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Horwich TB, Hernandez AF, Liang L, Albert NM, Labresh KA, Yancy CW, et al. Weekend hospital admission and discharge for heart failure: association with quality of care and clinical outcomes. American heart journal. 2009;158:451–8. doi: 10.1016/j.ahj.2009.06.025. [DOI] [PubMed] [Google Scholar]
- 12.Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE, et al. Weekend versus weekday admission and mortality from myocardial infarction. The New England journal of medicine. 2007;356:1099–109. doi: 10.1056/NEJMoa063355. [DOI] [PubMed] [Google Scholar]
- 13.Magid DJ, Wang Y, Herrin J, McNamara RL, Bradley EH, Curtis JP, et al. Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. Jama. 2005;294:803–12. doi: 10.1001/jama.294.7.803. [DOI] [PubMed] [Google Scholar]
- 14.Khoshchehreh M, Mirnateghi N, Malik S. The Weekend Effect: Does the Type of Myocardial Infarction Impact Management and Outcomes? Journal of the American College of Cardiology. 2015;66:593–4. doi: 10.1016/j.jacc.2015.01.069. [DOI] [PubMed] [Google Scholar]
- 15.Epstein AJ, Polsky D, Yang F, Yang L, Groeneveld PW. Coronary revascularization trends in the United States, 2001–2008. Jama. 2011;305:1769–76. doi: 10.1001/jama.2011.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Coady SA, Sorlie PD, Cooper LS, Folsom AR, Rosamond WD, Conwill DE. Validation of death certificate diagnosis for coronary heart disease: the Atherosclerosis Risk in Communities (ARIC) Study. Journal of clinical epidemiology. 2001;54:40–50. doi: 10.1016/s0895-4356(00)00272-9. [DOI] [PubMed] [Google Scholar]
- 17.McAlpine R, Pringle S, Pringle T, Lorimer R, MacDonald TM. A study to determine the sensitivity and specificity of hospital discharge diagnosis data used in the MICA study. Pharmacoepidemiology and drug safety. 1998;7:311–8. doi: 10.1002/(SICI)1099-1557(199809/10)7:5<311::AID-PDS371>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 18.Varas-Lorenzo C, Castellsague J, Stang MR, Tomas L, Aguado J, Perez-Gutthann S. Positive predictive value of ICD-9 codes 410 and 411 in the identification of cases of acute coronary syndromes in the Saskatchewan Hospital automated database. Pharmacoepidemiology and drug safety. 2008;17:842–52. doi: 10.1002/pds.1619. [DOI] [PubMed] [Google Scholar]
- 19.Martin-Sanchez FJ, Carbajosa V, Llorens P, Herrero P, Jacob J, Perez-Dura MJ, et al. Prolonged hospitalization in patients admitted for acute heart failure in the short stay unit (EPICA-UCE study): study of associated factors. Medicina clinica. 2014;143:245–51. doi: 10.1016/j.medcli.2013.06.028. [DOI] [PubMed] [Google Scholar]
- 20.Vavalle JP, Lopes RD, Chen AY, Newby LK, Wang TY, Shah BR, et al. Hospital length of stay in patients with non-ST-segment elevation myocardial infarction. The American journal of medicine. 2012;125:1085–94. doi: 10.1016/j.amjmed.2012.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nanchal R, Kumar G, Taneja A, Patel J, Deshmukh A, Tarima S, et al. Pulmonary embolism: the weekend effect. Chest. 2012;142:690–6. doi: 10.1378/chest.11-2663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Medical care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 23.van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Medical care. 2009;47:626–33. doi: 10.1097/MLR.0b013e31819432e5. [DOI] [PubMed] [Google Scholar]
- 24.Iezzoni LI, Ash AS, Shwartz M, Daley J, Hughes JS, Mackiernan YD. Predicting who dies depends on how severity is measured: implications for evaluating patient outcomes. Annals of internal medicine. 1995;123:763–70. doi: 10.7326/0003-4819-123-10-199511150-00004. [DOI] [PubMed] [Google Scholar]
- 25.Kumar G, Deshmukh A, Sakhuja A, Taneja A, Kumar N, Jacobs E, et al. Acute myocardial infarction: a national analysis of the weekend effect over time. Journal of the American College of Cardiology. 2015;65:217–8. doi: 10.1016/j.jacc.2014.09.083. [DOI] [PubMed] [Google Scholar]
- 26.Bavry AA, Kumbhani DJ, Rassi AN, Bhatt DL, Askari AT. Benefit of early invasive therapy in acute coronary syndromes: a meta-analysis of contemporary randomized clinical trials. Journal of the American College of Cardiology. 2006;48:1319–25. doi: 10.1016/j.jacc.2006.06.050. [DOI] [PubMed] [Google Scholar]
- 27.Hoenig MR, Aroney CN, Scott IA. Early invasive versus conservative strategies for unstable angina and non-ST elevation myocardial infarction in the stent era. The Cochrane database of systematic reviews. 2010:CD004815. doi: 10.1002/14651858.CD004815.pub3. [DOI] [PubMed] [Google Scholar]
- 28.Czaplinski C, Diers D. The effect of staff nursing on length of stay and mortality. Medical care. 1998;36:1626–38. doi: 10.1097/00005650-199812000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Deshmukh A, Pant S, Kumar G, Bursac Z, Paydak H, Mehta JL. Comparison of outcomes of weekend versus weekday admissions for atrial fibrillation. The American journal of cardiology. 2012;110:208–11. doi: 10.1016/j.amjcard.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 30.Marco J, Barba R, Plaza S, Losa JE, Canora J, Zapatero A. Analysis of the mortality of patients admitted to internal medicine wards over the weekend. American journal of medical quality : the official journal of the American College of Medical Quality. 2010;25:312–8. doi: 10.1177/1062860610366031. [DOI] [PubMed] [Google Scholar]
- 31.Peberdy MA, Ornato JP, Larkin GL, Braithwaite RS, Kashner TM, Carey SM, et al. Survival from inhospital cardiac arrest during nights and weekends. Jama. 2008;299:785–92. doi: 10.1001/jama.299.7.785. [DOI] [PubMed] [Google Scholar]
- 32.Schilling PL, Campbell DA, Jr, Englesbe MJ, Davis MM. A comparison of in-hospital mortality risk conferred by high hospital occupancy, differences in nurse staffing levels, weekend admission, and seasonal influenza. Medical care. 2010;48:224–32. doi: 10.1097/MLR.0b013e3181c162c0. [DOI] [PubMed] [Google Scholar]
- 33.Shaheen AA, Kaplan GG, Myers RP. Weekend versus weekday admission and mortality from gastrointestinal hemorrhage caused by peptic ulcer disease. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2009;7:303–10. doi: 10.1016/j.cgh.2008.08.033. [DOI] [PubMed] [Google Scholar]
- 34.Theobald CN, Stover DG, Choma NN, Hathaway J, Green JK, Peterson NB, et al. The effect of reducing maximum shift lengths to 16 hours on internal medicine interns’ educational opportunities. Academic medicine : journal of the Association of American Medical Colleges. 2013;88:512–8. doi: 10.1097/ACM.0b013e318285800f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Masoudi FA, Foody JM, Havranek EP, Wang Y, Radford MJ, Allman RM, et al. Trends in acute myocardial infarction in 4 US states between 1992 and 2001: clinical characteristics, quality of care, and outcomes. Circulation. 2006;114:2806–14. doi: 10.1161/CIRCULATIONAHA.106.611707. [DOI] [PubMed] [Google Scholar]
- 36.O’Flaherty M, Huffman MD, Capewell S. Declining trends in acute myocardial infarction attack and mortality rates, celebrating progress and ensuring future success. Heart. 2015 doi: 10.1136/heartjnl-2015-307868. [DOI] [PubMed] [Google Scholar]
- 37.Mehta SR, Cannon CP, Fox KA, Wallentin L, Boden WE, Spacek R, et al. Routine vs selective invasive strategies in patients with acute coronary syndromes: a collaborative meta-analysis of randomized trials. Jama. 2005;293:2908–17. doi: 10.1001/jama.293.23.2908. [DOI] [PubMed] [Google Scholar]
- 38.Goraya TY, Jacobsen SJ, Pellikka PA, Miller TD, Khan A, Weston SA, et al. Prognostic value of treadmill exercise testing in elderly persons. Annals of internal medicine. 2000;132:862–70. doi: 10.7326/0003-4819-132-11-200006060-00003. [DOI] [PubMed] [Google Scholar]