Abstract
Depressive symptoms are common in individuals with multiple sclerosis (MS), and are frequently exacerbated by pain; however, spiritual well-being may allow persons with MS to more effectively cope with pain-related deficits in physical and role functioning. We explored the associations between spiritual well-being, pain interference and depressive symptoms, assessing each as a potential mediator, in eighty-one patients being treated for MS, who completed self-report measures: Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale, Pain Effects Scale, and Center for Epidemiologic Studies Depression Scale Revised. At the bivariate level, spiritual well-being and its subscale of meaning and peace were negatively associated with depression and pain interference. In mediation models, depression was not related to pain interference via spiritual well-being, or to spiritual well-being via pain interference. Pain interference was related to depression via spiritual well-being and meaning/peace, and to spiritual well-being and meaning/peace via depressive symptoms. Finally, spiritual well-being and meaning/peace were related to depression via pain interference, and to pain interference via depressive symptoms. For patients with MS, a multi-faceted approach to treatment that includes pain reduction and promotion of spiritual well-being may be beneficial, although amelioration of depression remains a critical task.
Keywords: Spiritual well-being, Pain interference, Depressive symptoms, Multiple sclerosis
Introduction
Multiple sclerosis (MS) is a chronic, neurological disorder for which there is no cure, and is estimated to affect between 250,000 and 400,000 individuals in the United States, and 2.1 million people worldwide (Devins & Shnek, 2000; Reingold, 2002). Typically, the disease is characterized by unpredictable periods of symptoms such as visual loss or numbness of the limbs, with intermittent periods of partial or full remission, occurring over one to two decades with constant progression and accumulated disability (McNulty et al., 2004). Many individuals with MS are faced with the prospect of enduring years of persisting and worsening symptoms, including pain and risk for depression and impairment in social, physical and psychological functioning (Osborne et al., 2006). Comorbid pain (affecting 44–80 % of MS patients) and depression (>50 % of MS patients) are common in patients with multiple sclerosis (Hirsh et al., 2009), with greater levels of pain severity and interference related to greater depressive symptoms (Arnett et al., 2008; Alschuler et al., 2013). Pain frequently disrupts the ability to engage in required daily routines and self-care (Osborne et al., 2006), contributes to poor quality of life (Ehde et al., 2003; Harris et al., 2003) and activity limitations (Hunfeld et al., 2001; Smith et al., 2001). Despite its neurological basis, pain is also associated with psychosocial factors (Gatchel et al., 2007).
One such factor, spiritual well-being, is defined as the benefits occurring from the “way individuals seek and express meaning and purpose and the way they experience their connectedness to the moment, to self, to others, to nature, and to the significant or sacred” (Puchalski et al., 2009), and is conceptualized as having two components: meaningfulness, or a sense of purpose in life, and faith, which refers to a sense of comfort in feeling connected with a higher power (Yanez et al., 2009). A growing body of research suggests that spiritual well-being is related to overall health (Bredle et al., 2011), decreased pain severity and better coping with chronic illness (Irvine et al., 2009; Keefe et al., 2001). The existential components of spiritual well-being (e.g., meaning and peace) are often more robustly associated with good health than traditional religious behaviors (e.g., attending church services) (Bekelman et al., 2007; Hirsch et al., 2014). Despite this, some conflicting results exist; for example, several previous studies have found no association between spiritual well-being and pain severity or interference, suggesting that other factors (e.g., variability in spiritual well-being and pain over time) may contribute to differences noted in their association (Mystakidou et al., 2007; Rippentrop et al., 2005).
It is clear that the interrelations between spirituality, pain and depression are complex, with often-contradictory findings and bi-directionality; however, the linkages between these variables have not been previously examined in patients with MS. In general, spiritual well-being is related to less perceived illness uncertainty and psychological distress (McNulty et al., 2004), as well as better coping and psychosocial adjustment (Irvine et al., 2009; McNulty et al., 2004), in patients with MS. However, previous research also indicates that pain is deleteriously associated with engagement in spiritual pursuits (i.e., negative effect of pain on ability to complete social routines; distraction) and is linked to depression risk (e.g., resulting from discomfort, isolation) (de Villiers et al., 2015; Dobratz, 2005). As well, depression is often linked to greater levels of pain (e.g., via catastrophizing, comorbid somatic symptoms) and less motivation or ability to engage in spiritual pursuits (Williams et al., 2003; Haythornthwaite et al., 1991).
Thus, the purpose of this study is to examine the interrelations between spiritual well-being, pain interference and depressive symptoms in persons with MS. We hypothesized that, at the bivariate level, spiritual well-being would be negatively, and pain interference positively, associated with depressive symptoms. In exploratory mediation models, we analyzed all potential associations between spiritual well-being, and its subscales, and depressive symptoms and pain interference, using each as a predictor, mediator and outcome variable, in turn.
Methods
Participants in this IRB-approved study were volunteers recruited from an outpatient, university hospital-based, MS clinic. Informed consent was obtained by trained research staff, and participants completed questionnaires in written format, in a private assessment room. Our sample consisted of 81 participants, ages 30–75 years old (M = 51.12; SD = 9.6), with more women (n = 64; 83 %) than men. The self-reported race of our sample was primarily White (91.4 %; N = 74), with 4.9 % Other (N = 4), 2.5 % Multiracial (N = 2), and 1.3 % Black (N = 1). Participants reported a mean education level of 15.44 years (SD = 2.6). Approximately 59 % (58.8 %; N = 47.63) reported current engagement in religious practice. Most participants were married (60.5 %), 14.8 % divorced, 11.1 % single and never married, 6.2 % widowed, 2.5 % legally separated, and 4.9 % with no reported marital status.
Measures
The Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale (FACIT-Sp) (Peterman et al., 2002), was developed to assess the spiritual well-being of patients with chronic illness, and includes two subscales: The Meaning and Peace subscale (Mean = 21.24; SD = 7.06), which measures feelings of inner peace and meaning (8 items; e.g., “I feel a sense of purpose in my life”), and the Faith subscale (Mean = 8.74, SD = 4.60), which measures sense of strength and comfort from one's beliefs (4 items; e.g., “I find strength in my faith or spiritual beliefs”). Items are rated on a 5-point Likert scale ranging from 0 (not at all) to 5 (very much), with higher scores indicating greater spiritual well-being (Total Range = 0–40; faith subscale = 0–20; meaning and peace subscale = 0–40). In a series of two studies, among patients with cancer, the FACIT-SP demonstrated good internal consistency for the total score (α = .87; .86), meaning and peace subscale (α = .81; .81), and faith subscale (α = .88; .86) (Peterman et al., 2002). In our sample, alpha coefficients were as follows: total score (α = .88), meaning and peace subscale (α = .91), and faith subscale (α = .84).
Pain interference, or the effect of pain on behavior and mood, was measured by the Pain Effects Scale (PES), which consists of 6 items, and is part of the Multiple Sclerosis Quality of Life Inventory (MSQLI) (Ritvo et al., 1997). Participants indicated the degree to which pain interfered with their mood, ability to walk or move around, sleep, normal work, recreational activities, and enjoyment in life, on a 5-point Likert scale ranging from 1 (not at all) to 5 = (to an extreme degree); higher scores indicate greater impact of pain interference (range = 6–30). Among MS patients, the PES has demonstrated excellent internal consistency (α = .92) (Osborne et al., 2006), which was reflected in the current sample (α = .94).
The Center for Epidemiologic Studies Depression Scale (CES-D-R 20) was used to assess presence and severity of depressive symptoms (Radloff, 1977). Items (N = 20) are rated on a 4-point Likert scale ranging from 0 (rarely or none of the time) to 3 (most or all of the time), with higher scores indicating greater depressive symptoms (range = 0–60). The CES-D-R 20 has excellent internal reliability (α = .90) among patients with MS (Verdier-Taillefer et al., 2001), as it did in the current study (α = .91).
Statistical analyses
Bivariate analyses
Pearson's product-moment correlations were used to examine zero-order associations between spiritual well-being, the faith subscale, the meaning and peace subscale, pain interference, and depressive symptoms; no correlation exceeded the cut-off recommended for multicollinearity (r > .80) (Katz, 2006), except for the relation between spiritual well-being and the meaning and peace subscale which, in mediation models, were assessed independently.
Mediation analyses
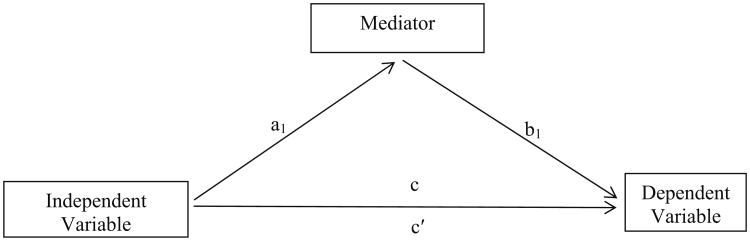
Multivariate mediation analyses were conducted, consistent with Preacher and Hayes (2008a), which allow for one independent variable (IV), one dependent variable (DV), and more than one mediator variable. We examined the relation between spiritual well-being, and its subscales, and depression via pain interference; for subscale analyses, the spiritual well-being subscale not entered as the IV was covaried (see Fig. 1). We also examined the following models: relation between spiritual well-being and pain interference via depression; relation between depression and pain interference via spiritual well-being; between depression and spiritual well-being via pain interference; between pain interference and depression via spiritual well-being; and, finally, between pain interference and spiritual well-being via depression. There are several potential pathways of significance in a mediation model. The total effect, or (c) pathway, signifies the direct relationship between the IV and DV without controlling for possible MVs. A direct effect, or the (c′) pathway, refers to the relation between the IV and DV after controlling for the possible effects of a MV. A total indirect effect (ab) refers to the role of all potential MVs on the association between an IV and a DV. Finally a specific indirect effect refers to the role of a particular MV(s) in the relationship between an IV and a DV. When there is a reduction in significance from the total to direct effects (c to c′), mediation is said to occur, with these common terms often applied: partial mediation (coefficient remains significant) and full mediation (coefficient is reduced to non-significance).
Fig. 1.
Illustration of indirect effects models for multivariable mediation. Note: a = direct effect of IV on mediator; b = direct effect of mediator on DV; c = total effect (IV affects DV without accounting for mediator); c′ = direct effect (IV affects DV when accounting for mediator); ab = total indirect effect (IV affects DV through mediator). Adapted from Preacher and Hayes (2008a)
Compared to Baron and Kenny's (1986) approach to mediation analysis, Preacher and Hayes' (2008a) mediation techniques use bootstrap resampling to calculate more accurate analysis of indirect effects (Hayes, 2009; Preacher & Hayes, 2008b). Bootstrapping resampling provides an estimate of indirect effects and empirical approximations of the sampling distribution of an indirect effect, by resampling a study sample k times (at least 5000 times; in the current study, 10,000 iterations) and generating confidence intervals (CI's), that permit inferences about the size of the indirect effect (Hayes, 2009); when CI's do not cross zero, the model is deemed significant. The techniques can be used on non-normally distributed data, and allow for indirect effects without the presence of direct effects. Also, the bootstrapping method permits the detection of effects even when the sample size is small (Preacher & Hayes, 2008a). In all models, age and sex were included as covariates, and the alpha (Type I error) level was set at p <.05. Effect sizes (percent mediation) are reported (Preacher & Kelly, 2011).
Results
In bivariate analyses, there was partial support for our hypotheses (see Table 1). Spiritual well-being (r = −.52, p <.001), its subscale of peace/meaning (r = −.60, p <.05) and pain interference (r = .54, p < .001) were associated with depressive symptoms; the faith subscale was not correlated with depressive symptoms. Spiritual well-being (r = .54, p < .001), and meaning/peacefulness (r = .54, p < .001), were related to pain interference, but faith was not. Spiritual wellbeing, as well as the subscale of meaning and peace, were not related to participation in religious activities; however, the faith subscale was related to engagement in religious activities (r = .36, p < .001).
Table 1. Means, standard deviations, and correlations.
| Variable | M | SD | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|
| 1. Spiritual well-being | 29.69 | 9.89 | – | |||
| 2. Meaning and peace | 21.25 | 7.06 | .91** | – | ||
| 3. Faith | 8.74 | 4.60 | .76** | .40** | – | |
| 4. Pain Interference | 13.64 | 7.06 | −.36** | −.42** | −.13 | – |
| 5. Depressive symptoms | 15.93 | 11.79 | −.52** | −.60* | −.21 | .54** |
Spiritual Well-Being, Meaning and Peace, Faith = Functional Assessment of Chronic Illness Therapy—Spiritual Well-Being Scale (FACIT-Sp); Pain Interference = Pain Effects Scale (PES); and Depressive Symptoms = Center for Epidemiologic Studies Depression Scale (CES-D-R 20)
p ≤ .05;
p ≤ .01
In mediation models, we first examined the relation of spiritual well-being to depression via pain interference (see Fig. 1). Significant total and direct effects for spiritual well-being (c = − 0.67, p <.0000; c′ = −0.49, p = .0002) and the meaning and peace subscale (c = −1.04, p <.0000; c′ = −0.78, p = .0000) on depressive symptoms were observed; although the total indirect effect for the faith subscale was not significant [Percent Mediation effect size (Pm) = .35], there was an initial direct effect between faith and depression (c = −.73, p = .03). The indirect effect of spiritual well-being on depressive symptoms through pain interference was statistically significant (ab = −0.18, CI = −0.37 to −0.05; Pm = .27). Greater spiritual well-being was associated with less perceived pain inference (a = −0.27, p = .0005) which, in turn, was associated with fewer depressive symptoms (b = 0.68, p = .0008). The indirect effect of the meaning and peace subscale on depressive symptoms through pain interference was also significant (ab = −0.26, CI = −0.57 to −0.06; Pm = .25). Greater meaning and peace was associated with lower levels of perceived pain inference (a = −0.42, p = .0002) which, in turn, was associated with less depressive symptoms (b = 0.62, p = .002).
We also examined the effect of spiritual well-being on pain interference via depressive symptoms. Significant total, but not direct, effects for spiritual well-being (c = −0.27, p <.0005; c′ = −0.11, p = .20) and the meaning and peace subscale (c = −0.42, p <.0002; c′ = −0.16, p = .20) on pain interference were observed, indicating full mediation. The indirect effect of spiritual well-being on pain interference through depressive symptoms was statistically significant (ab = −0.16, CI = −0.27 to −0.07; Pm = .60). Greater spiritual well-being was associated with fewer depressive symptoms (a = −0.67, p < .0000) and, in turn, to less pain interference (b = 0.24, p = .0008). The indirect effect of the meaning and peace subscale on pain interference via depressive symptoms was also significant (ab = −0.42, CI = −0.63 to −0.21; Pm = .61). Greater meaning and peace was associated with less depression (a = −1.04, p <.0000) which, in turn, was related to less pain interference (b = 0.25, p = .002). Although the total and direct effects of the faith subscale on pain interference were not significant, an indirect only effect was indicated; that is, no initial relation exists between faith and pain interference, but this association manifests only via the impact of faith on depressive symptoms (ab = −.21, CI = −.45 to −.04). Faith was negatively related to depressive symptoms (a = −0.73, p < .05), although depressive symptoms were, in turn, consistently related to greater pain interference (b = .29, p < .001).
Our next series of models examined the relation between pain interference and depression via spiritual well-being, and between pain interference and spiritual well-being via depressive symptoms. A significant total and direct effect for pain interference on depression was observed, via spiritual well-being (c = 0.99, p < .0000; c′ = 0.68, p = .0008) and the meaning and peace subscale (c = 1.01, p <.0000; c′ = 0.63, p < .01). The indirect effect of pain interference on depression through spiritual well-being was statistically significant (ab = 0.31, CI = 0.13–0.64; Pm = .32). Greater pain interference was related to less spiritual well-being (a = −0.64, p = .0005) which, in turn, was associated with fewer depressive symptoms (b = −.48, p = .0002). The indirect effect of pain interference on depression via the meaning and peace subscale was also significant (ab = 0.38, CI = 0.18–0.73; Pm = .38). Greater pain interference was related to less meaning and peace (a = −0.49, p = .0002) which, in turn, was related to more depressive symptoms (b = −.78, p = .0000). Analyses examining the faith subscale were not significant (Pm = .06).
A significant total effect for pain interference on spiritual well-being was observed (c = −0.64, p < .0005), but this reduced in significance with the inclusion of depression as a mediator, indicating full mediation (c′ = −0.25, p = .19). The indirect effect of pain interference on spiritual well-being via depression was statistically significant (ab = −0.40, CI = −0.68 to −0.22; Pm = .62). Greater pain interference was related to more depression (a = 0.99, p = .0000) which, in turn, was related to less spiritual well-being (b = −.40, p = .0002).
A significant total effect of pain interference on the meaning and peace subscale was also significant (c = −0.49, p = .0002), but this was reduced to non-significance with the inclusion of depressive symptoms (c′ = −0.17, p = .19), indicating full mediation. The indirect effect of pain interference on meaning/peace was significant (ab = −0.32, CI = −0.53 to −0.18; Pm = .66); greater pain interference was related to more depressive symptoms (a = 1.01, p = .0000) which, in turn, was related to less meaning and peace (b = −.31, p = .0000). Analyses examining depression as a mediator of the linkage between pain interference and faith were not significant (Pm = .69).
Finally, we examined a series of models of the association between depression and pain interference via spiritual well-being, and of the relation between depression and spiritual well-being via pain interference, finding that neither model was significant for mediation effects.
Discussion
In support of our hypotheses, at the bivariate level, we found a significant, negative association between spiritual well-being, and its subscale of meaning and peace, and depressive symptoms, and a significant positive association between pain interference and depressive symptoms. In exploratory mediation models examining all potential associations between spiritual well-being, pain interference and depressive symptoms, we found the following associations in order of robustness (Pm): (1) pain interference was related to peace/meaning and spiritual well-being via depression; (2) spiritual well-being and meaning/peace was related to pain interference via depression; (3) pain interference was related to depression via spiritual well-being and meaning/peace; and, (4) spiritual well-being and meaning/peace were related to depression via pain interference. The faith subscale was not a significant mediator in any of the model series.
Our results support the notion that the relations between spiritual well-being, pain interference and depression are complex, and are multi-directional in nature. The relation between pain interference and spiritual well-being via depression, which was our most robust finding, is an association that is often overlooked in the literature; however, a growing body of work suggests that, in addition to contributing to reduced motivation to engage in religious/spiritual pursuits, depression may also result in “spiritual disconnection,” and feelings of anger toward God or feeling unloved by God (Sorajjakool et al., 2008; Koenig, 2007).
Alternatively, we also found that pain interference is related to depression via spiritual well-being, providing insight into a potential mechanism of action for the pain-depression linkage. In yet another relatively unexplored area of research, preliminary findings suggest that, health stressors such as pain, chronic illness and terminal illness can challenge (e.g., questioning suffering; doubting God's existence) and/or distract from (e.g., discomfort; inability to participate) expression of religious and spiritual beliefs, or engagement in spiritual activities (Dobratz, 2005; de Villiers et al., 2015). In a reciprocal manner, patients with MS who experience pain-related disruptions to daily activities may experience depression as a result of reduced ability to engage in spiritual or personally-meaningful pursuits and, as well, the pain-related depressive symptoms experienced by these individuals may reduce efficacy and motivation to fulfill spiritual needs.
We also found that spiritual well-being, overall, but primarily carried by the weight of meaningfulness/peace-fulness, was related to less pain interference via depressive symptoms, which was our second most-robust finding, and that spiritual well-being was related to less depressive symptoms via pain interference. Faith was not significantly associated with pain interference or depression, across most analyses. This pattern of associations is consistent with prior research indicating the benefits of existential spirituality for physical and mental health (Koenig et al., 2001), but is in contrast to findings suggesting that ritualistic religious activities promote wellbeing (Yanez et al., 2009). Indeed, at the bivariate level, we found that faith was related to increased levels of pain and poorer spiritual well-being. It may be that, for patients with MS or others with chronic illness, faith-based activities, which are often socially-involved and based outside of the home, may be difficult to engage in.
Having a sense of meaning and purposefulness in the context of chronic illness may help to counteract the negative emotional states, such as hopelessness and helplessness, that often accompany pain-related disability and which may contribute to depressive symptoms (O'Connor et al., 2008; Tan et al., 2008; McNulty et al., 2004; Johnson et al., 2011). For example, individuals with greater spiritual well-being may believe that their pain is part of a “larger plan” or a “test of faith,” and a common spiritual coping mechanism is to release or “turn over” a stressor, such as pain, to a higher power (Bussing et al., 2009; Glover-Graf et al., 2007). Spiritual contemplative practices such as prayer, meditation and mindfulness may also promote acceptance and management of the emotional components of pain (Wachholtz et al., 2007; Morone et al., 2008).
In our study, contrary to some previous research (Baetz & Bowen, 2008), the relationship between faith and depressive symptoms was not statistically significant, perhaps due to limited power as a result of small sample size. It may also be that the faith-based component of spiritual well-being, assessed by items regarding finding strength or comfort in faith or spiritual beliefs, and the relation between illness and the strengthening of faith or spiritual beliefs, is more aligned with formal religious beliefs and practices (e.g., church attendance, prayer) which often, in the abstract, are unrelated to health outcomes (Bekelman et al., 2007). On the other hand, attempting to find peace of mind, harmony and meaning, or extracting a purpose from one's experience of pain-induced limitations, may evoke more effective and adaptive forms of cognitive, emotional and behavioral coping (Mohr et al., 1999).
In addition to our specific patterns of results, it is important to consider our findings within the context of the extant, and often-mixed, literature on the association between spirituality and pain (Rippentrop et al., 2005; Baetz & Bowen, 2008). In our sample of patients with MS, we found an essentially reciprocal relationship between pain interference and spiritual well-being via the common factor of depression. In contrast, depression, as an independent variable, was not significantly related to pain interference (via spiritual well-being) or spiritual well-being (via pain interference). In simplified terms, depression, in isolation, may not exacerbate pain interference enough to disturb spiritual well-being and, similarly, may not impair spiritual well-being to the extent that psychological distress occurs. Yet, depressive symptoms appear to play a critical role in the linkage between pain and spiritual well-being, and between spiritual well-being and pain interference. Intuitively, and in support of spirituality-based protective theories, we found that spiritual well-being and, in particular, meaningfulness and peacefulness, were related to less depression and, in turn, to less pain interference. Our finding suggests a basic association between spiritual well-being and lower levels of pain that might be routed through psychopathology, solidifying the need for a psychosocial approach to the treatment of pain. On the other hand, we found that pain is directly related to mood dysfunction and, in turn, to reduced spiritual well-being; thus, initial treatment of pain may be necessary to facilitate the ability to engage in activities that promote psychological and spiritual well-being (Pakenham, 2008). Future prospective research, both mechanistic and interventive, is necessary to better understand the temporal relations between spiritual well-being, pain and depression, and to determine the best therapeutic approaches (e.g., focus on pain reduction versus promotion of spiritual well-being, or a multi-focused strategy) for improving health-related quality of life in patients with chronic illness.
Limitations
Given the cross-sectional design, causal inference is not permitted and bi-directionality is a possibility, which we examined. Additionally, pain interference was only a partial mediator. Presumably there are other psychosocial or biological factors, including severity of pain, not available for examination in this secondary analysis, that also affect the relation between spiritual well-being and depression (Mofidi et al., 2007). One such factor is cognitive decline, which is an insidious contributor to decreased well-being and functionality in patients with MS, and for which we did not have available data. Given that meaning-making and purposefulness are predicated on cognitive-emotional ability (Wilson et al., 2013), and considering that persons with MS may have impairments to emotional reactivity, decision making and abstract reasoning, future research should consider the impact of cognitive decline on the ability to engage in, and benefit from, meaning-making activities and spiritual coping (Kleeberg et al., 2004; Rogers & Panegyres, 2007). Finally, our small sample primarily included patients with relapsing-remitting MS, which may limit generalizability to patients with progressive MS. Small sample size may have also contributed to underpowered statistical analyses. Prospective research with larger and more diverse samples, and which assesses a wider array of potential mediating factors, is needed.
Our findings may also have clinical implications for therapeutics research. Interventions that aim to promote spiritual well-being, particularly the search for meaning and purpose, may beneficially influence the perception of pain-related impairment and depressive symptoms. Spiritual well-being may aid in coping with the effects of pain by allowing a reframing of the pain-related experience and by promoting problem solving and goal-motivation (Keefe et al., 2001; Baetz & Bowen, 2008; Simoni & Ortiz, 2003). A sense of meaningfulness and peace may help to promote acceptance of pain interference (Braams et al., 2012), or distract from a focus on bodily pain and its consequent limitations, thereby increasing pain tolerance (Wachholtz et al., 2007). Interventions such as spiritual or mindfulness meditation may facilitate reflection on meaning and purpose in life, and are related to increased pain tolerance, positive mood and better health-related quality of life (Delaney et al., 2011; Wachholtz & Pargament, 2005). Furthermore, a brief spiritual well-being intervention—the Short-Term Life Review, which permits patients to create a narrative about proud and important roles, events, and memories in life, is noted to increase spiritual well-being and decrease depressive symptoms (Ando et al., 2010), and could be readily implemented in treatment settings. Research on the effects of meaning-oriented interventions that is designed to uncover mechanisms of action would be useful.
Conclusion
In our sample of patients with MS, the capacity to find meaning and purpose was associated with less pain interference and less severe depressive symptoms. This cross-sectional study suggests that the capacity to find meaning and purpose is associated with decreased pain interference and decreased depression severity. Prospective studies are needed, including intervention research. Clinical interventions which increase meaningfulness and purpose in life may allow patients with multiple sclerosis to overcome some of the perceived deficits associated with pain, thereby reducing depressive symptoms.
Footnotes
Conflict of interest Sheri A. Nsamenang, Jameson K. Hirsch, Raluca Topciu, Andrew D. Goodman and Paul R. Duberstein declare that they have no conflict of interest.
Compliance with ethical standards: Human and animal rights and Informed consent All procedures followed were in accordance with ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
References
- Alschuler KN, Ehde DM, Jensen MP. The cooccurrence of pain and depression in adults with multiple sclerosis. Rehabilitation Psychology. 2013;58:217–221. doi: 10.1037/a0032008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ando M, Morita T, Akechi T. Factors in the short-term life review that affect spiritual well-being in terminally ill cancer patients. Journal of Hospice and Palliative Nursing. 2010;12:305–311. http://journals.lww.com/jhpn/pages/default.aspx. [Google Scholar]
- Arnett PA, Barwick FH, Beeney JE. Depression in multiple sclerosis: Review and theoretical proposal. Journal of the International Neuropsychological Society. 2008;14:691–724. doi: 10.1017/S1355617708081174. [DOI] [PubMed] [Google Scholar]
- Baetz M, Bowen R. Chronic pain and fatigue: Associations with religion and spirituality. Pain Research and Management. 2008;13:383–388. doi: 10.1155/2008/263751. http://www.ncbi.nlm.nih.gov/pmc/journals/531/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bekelman DB, Dy SM, Becker DM, Wittstein IS, Hendricks DE, Yamashita TE, Gottlieb SH. Spiritual well-being and depression in patients with heart failure. Journal of General Internal Medicine. 2007;22:470–477. doi: 10.1007/s11606-006-0044-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braams BR, Blechert J, Boden M, Gross JJ. The effects of acceptance and suppression on anticipation and receipt of painful stimulation. Journal of Behavior Therapy and Experimental Psychiatry. 2012;43:1014–1018. doi: 10.1016/j.jbtep.2012.04.001. [DOI] [PubMed] [Google Scholar]
- Bredle JM, Salsman JM, Debb SM, Arnold BJ, Cella D. Spiritual well-being as a component of health related quality of life: The Functional Assessment of Chronic Illness Therapy Spiritual Well-Being Scale. Religions. 2011;2:77–94. doi: 10.3390/rel2010077. [DOI] [Google Scholar]
- Bussing A, Michalsen A, Balzat HJ, Grunther RA, Ostermann T, Neugebauer EA, Matthiessen PF. Are spirituality and religiosity resources for patients with chronic pain conditions? Pain Medicine. 2009;10:327–339. doi: 10.1111/j.1526-4637.2009.00572.x. [DOI] [PubMed] [Google Scholar]
- de Villiers M, Maree JE, van Belkum C. The influence of chronic pain on the daily lives of underprivileged South Africans. Pain Management Nursing. 2015;16(2):96–104. doi: 10.1016/j.pmn.2014.05.001. [DOI] [PubMed] [Google Scholar]
- Delaney C, Barrere C, Helming M. The influence of a spirituality-based intervention on quality of life, depression, and anxiety in community-dwelling adults with cardiovascular disease: A pilot study. Journal of Holistic Nursing. 2011;29:21–32. doi: 10.1177/0898010110378356. [DOI] [PubMed] [Google Scholar]
- Devins GM, Shnek ZM. Multiple sclerosis. In: Frank RG, Elliott TR, editors. Handbook of rehabilitation psychology. Washington, DC: American Psychological Association; 2000. pp. 163–184. [Google Scholar]
- Dobratz MC. A comparative study of life-closing spirituality in home hospice patients. Research and Theory for Nursing Practice. 2005;19(3):243–256. doi: 10.1891/rtnp.2005.19.3.243. [DOI] [PubMed] [Google Scholar]
- Ehde DM, Gibbons LE, Chwastiak L, Bombardier CH, Sullivan MD, Kraft GH. Chronic pain in a large community sample of persons with multiple sclerosis. Multiple Sclerosis. 2003;9:605–611. doi: 10.1191/1352458503ms939oa. [DOI] [PubMed] [Google Scholar]
- Gatchel RJ, Peng Y, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychological Bulletin. 2007;133:581–624. doi: 10.1037/0033-2909.133.4.581. [DOI] [PubMed] [Google Scholar]
- Glover-Graf N, Marini I, Baker J, Buck T. Religious and spiritual beliefs and practices of persons with chronic pain. Rehabilitation Counseling Bulletin. 2007;51:21–33. doi: 10.1177/00343552070510010501. [DOI] [Google Scholar]
- Harris S, Morley S, Barton SB. Role loss and emotional adjustment in chronic pain. Pain. 2003;105:363–370. doi: 10.1016/S0304-3959(03)00251-3. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76:408–420. doi: 10.1080/03637750903310360. [DOI] [Google Scholar]
- Haythornthwaite JA, Sieber WJ, Kerns RD. Depression and the chronic pain experience. Pain. 1991;46(2):177–184. doi: 10.1016/0304-3959(91)90073-7. [DOI] [PubMed] [Google Scholar]
- Hirsch J, Webb J, Kaslow N. Daily hassles and suicidal behavior in African American, female suicide attempters: Moderating effect of spiritual well-being. Mental Health, Religion and Culture. 2014;17:529–541. doi: 10.1080/13674676.2013.858682. [DOI] [Google Scholar]
- Hirsh AT, Turner AP, Ehde DM, Haselkorn JK. Prevalence and impact of pain in multiple sclerosis: Physical and psychologic contributors. Archives of Physical Medicine and Rehabilitation. 2009;90:646–651. doi: 10.1016/j.apmr.2008.10.019. http://www.archives-pmr.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunfeld JM, Perquin CW, Duivenvoorden HJ, Hazebroek-Kampschreur AM, Passchier J, van Suijlekom-Smit LA, van der Wouden JC. Chronic pain and its impact on quality of life in adolescents and their families. Journal of Pediatric Psychology. 2001;26:145–153. doi: 10.1093/jpepsy/26.3.145. [DOI] [PubMed] [Google Scholar]
- Irvine HH, Davidson CC, Hoy KK, Lowe-Strong AA. Psychosocial adjustment to multiple sclerosis: Exploration of identity redefinition. Disability and Rehabilitation. 2009;31:599–606. doi: 10.1080/09638280802243286. http://informahealthcare.com/loi/dre. [DOI] [PubMed] [Google Scholar]
- Johnson KS, Tulsky JA, Hays JC, Arnold RM, Olsen MK, Lindquist JH, Steinhauser KE. Which domains of spirituality are associated with anxiety and depression in patients with advanced illness? Journal of General Internal Medicine. 2011;26:751–758. doi: 10.1007/s11606-011-1656-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz MH. Multivariable analysis: A practical guide for clinicians. New York, NY: Cambridge University; 2006. [Google Scholar]
- Keefe F, Affleck G, Lefebvre J, Underwood L, Caldwell D, Drew J, et al. Living with rheumatoid arthritis: The role of daily spirituality and daily religious and spiritual coping. Journal of Pain. 2001;2:101–110. doi: 10.1054/jpai.2001.19296. http://www.jpain.org/ [DOI] [PubMed] [Google Scholar]
- Kleeberg J, Bruggimann L, Annoni J, van Melle G, Bogous-slavsky J, Schluep M. Altered decision-making in multiple sclerosis: A sign of impaired emotional reactivity? Annals of Neurology. 2004;56:787–795. doi: 10.1002/ana.20277. [DOI] [PubMed] [Google Scholar]
- Koenig HG. Religion and depression in older medical inpatients. The American Journal of Geriatric Psychiatry. 2007;15(4):282–291. doi: 10.1097/01.JGP.0000246875.93674.0c. [DOI] [PubMed] [Google Scholar]
- Koenig HG, McCullough ME, Larson DB. Handbook of religion and health. New York, NY: Oxford University Press; 2001. [Google Scholar]
- McNulty K, Livneh H, Wilson LM. Perceived uncertainty, spiritual well-being, and psychosocial adaptation in individuals with multiple sclerosis. Rehabilitation Psychology. 2004;49:91–99. doi: 10.1037/0090-5550.49.2.91. [DOI] [Google Scholar]
- Mofidi M, DeVellis RF, DeVellis BM, Blazer DG, Panter AT, Jordan JM. The relationship between spirituality and depressive symptoms: Testing psychosocial mechanisms. Journal of Nervous and Mental Disease. 2007;195:681–688. doi: 10.1097/NMD.0b013e31811f4038. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Dick LP, Russo D, Pinn J, Boudewyn AC, Likosky W, Goodkin DE. The psychosocial impact of multiple sclerosis: Exploring the patient's perspective. Health Psychology. 1999;18:376–382. doi: 10.1037//0278-6133.18.4.376. [DOI] [PubMed] [Google Scholar]
- Morone N, Greco C, Weiner D. Mindfulness meditation for the treatment of chronic low back pain in older adults: A randomized controlled pilot study. Pain. 2008;134:310–319. doi: 10.1016/j.pain.2007.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mystakidou K, Tsilika E, Parpa E, Pathiaki M, Patiraki E, Galanos A, Vlahos L. Exploring the relationships between depression, hopelessness, cognitive status, pain, and spirituality in patients with advanced cancer. Archives of Psychiatric Nursing. 2007;21:150–161. doi: 10.1016/j.apnu.2007.02.002. [DOI] [PubMed] [Google Scholar]
- O'Connor AB, Herrmann DN, Markman JD, Dworkin RH. Pain associated with multiple sclerosis: Systematic review and proposed classification. Pain. 2008;137:96–111. doi: 10.1016/j.pain.2007.08.024. [DOI] [PubMed] [Google Scholar]
- Osborne TL, Turner AP, Williams RM, Bowen JD, Hatzakis M, Rodriguez A, Haselkorn JK. Correlates of pain interference in multiple sclerosis. Rehabilitation Psychology. 2006;51:166–174. doi: 10.1037/0090-5550.51.2.166. [DOI] [Google Scholar]
- Pakenham K. Making sense of illness or disability: The nature of sense making in multiple sclerosis (MS) Journal of Health Psychology. 2008;13:93–105. doi: 10.1177/1359105307084315. http://hpq.sagepub.com/ [DOI] [PubMed] [Google Scholar]
- Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: The Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale (FACIT-Sp) Annals of Behavioral Medicine. 2002;24:49–58. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008a;40:879–891. doi: 10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- Preacher K, Hayes A. Contemporary approaches to assessing mediation in communication research. In: Hayes AF, Slater MD, Snyder LB, editors. The Sage sourcebook of advanced data analysis methods for communication research. Thousand Oaks, CA: Sage Publications; 2008b. pp. 13–54. [Google Scholar]
- Preacher K, Kelly K. Effect size measures for mediation models: Quantitative strategies for communicating indirect effects. Psychological Methods. 2011;16:93–115. doi: 10.1037/a0022658. [DOI] [PubMed] [Google Scholar]
- Puchalski C, Ferrell B, Virani R, Otis-Green S, Baird P, Bull J, et al. Improving the quality of spiritual care as a dimension of palliative care: The report of the consensus conference. Journal of Palliative Medicine. 2009;12:885–904. doi: 10.1089/jpm.2009.0142. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Reingold S. Prevalence estimates for MS in the United States and evidence of an increasing trend for women. Neurology. 2002;59:294. doi: 10.1212/wnl.59.2.294. http://www.neurology.org/ [DOI] [PubMed] [Google Scholar]
- Rippentrop A, Altmaier EM, Chen JJ, Found EM, Keffala VJ. The relationship between religion/spirituality and physical health, mental health, and pain in a chronic pain population. Pain. 2005;116:311–321. doi: 10.1016/j.pain.2005.05.008. [DOI] [PubMed] [Google Scholar]
- Ritvo PG, Fischer JS, Miller DM, Andrews H, Paty DW, LaRocca NG. Multiple Sclerosis Quality of Life Inventory: A user's manual. New York: National Multiple Sclerosis Society; 1997. [DOI] [PubMed] [Google Scholar]
- Rogers J, Panegyres P. Cognitive impairment in multiple sclerosis: Evidence-based analysis and recommendations. Journal of Clinical Neuroscience. 2007;14:919–927. doi: 10.1016/j.jocn.2007.02.006. [DOI] [PubMed] [Google Scholar]
- Simoni JM, Ortiz MZ. Mediational models of spirituality and depressive symptomatology among HIV-positive Puerto Rican women. Cultural Diversity and Ethnic Minority Psychology. 2003;9:3–15. doi: 10.1037/1099-9809.9.1.3. [DOI] [PubMed] [Google Scholar]
- Smith BH, Elliott AM, Chambers W, Smith W, Hannaford PC, Penny K. The impact of chronic pain in the community. Family Practice. 2001;18:292–299. doi: 10.1093/fampra/18.3.292. [DOI] [PubMed] [Google Scholar]
- Sorajjakool S, Aja V, Chilson B, Ramírez-Johnson J, Earll A. Disconnection, depression, and spirituality: A study of the role of spirituality and meaning in the lives of individuals with severe depression. Pastoral Psychology. 2008;56(5):521–532. [Google Scholar]
- Tan G, Jensen MP, Thornby J, Sloan PA. Negative emotions, pain, and functioning. Psychological Services. 2008;5:26–35. doi: 10.1037/1541-1559.5.1.26. [DOI] [Google Scholar]
- Verdier-Taillefer MH, Gourlet VV, Fuhrer RR, Alpérovitch AA. Psychometric properties of the Center for Epidemiologic Studies-Depression Scale in multiple sclerosis. Neuroepidemiology. 2001;20:262–267. doi: 10.1159/000054800. [DOI] [PubMed] [Google Scholar]
- Wachholtz A, Pargament K. Is spirituality a critical ingredient of meditation? Comparing the effects of spiritual meditation, secular meditation, and relaxation on spiritual, psychological, cardiac, and pain outcomes. Journal of Behavioral Medicine. 2005;28:369–384. doi: 10.1007/s10865-005-9008-5. [DOI] [PubMed] [Google Scholar]
- Wachholtz A, Pearce M, Koenig H. Exploring the relationship between spirituality, coping, and pain. Journal of Behavioral Medicine. 2007;30:311–318. doi: 10.1007/s10865-007-9114-7. [DOI] [PubMed] [Google Scholar]
- Williams LS, Jones WJ, Shen J, Robinson RL, Weinberger M, Kroenke K. Prevalence and impact of depression and pain in neurology outpatients. Journal of Neurology, Neurosurgery & Psychiatry. 2003;74(11):1587–1589. doi: 10.1136/jnnp.74.11.1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson RS, Boyle PA, Segawa E, Yu L, Begeny CT, Anagnos SE, Bennett DA. The influence of cognitive decline on well-being in old age. Psychology and Aging. 2013;28:304–313. doi: 10.1037/a0031196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanez B, Edmondson D, Stanton AL, Park CL, Kwan L, Ganz PA, Blank TO. Facets of spirituality as predictors of adjustment to cancer: Relative contributions of having faith and finding meaning. Journal of Consulting and Clinical Psychology. 2009;77:730–741. doi: 10.1037/a0015820. [DOI] [PMC free article] [PubMed] [Google Scholar]