Abstract
The Western Australian (WA) ‘LiveLighter’ (LL) mass media campaign ran during June–August and September–October 2012. The principal campaign ad graphically depicts visceral fat of an overweight individual (‘why’ change message), whereas supporting ads demonstrate simple changes to increase activity and eat healthier (‘how’ to change message). Cross-sectional surveys among population samples aged 25–49 were undertaken pre-campaign (N = 2012) and following the two media waves (N = 2005 and N = 2009) in the intervention (WA) and comparison state (Victoria) to estimate the population impact of LL. Campaign awareness was 54% after the first media wave and overweight adults were more likely to recall LL and perceive it as personally relevant. Recall was also higher among parents, but equal between socio-economic groups. The ‘why’ message about health-harms of overweight rated higher than ‘how’ messages about lifestyle change, on perceived message effectiveness which is predictive of health-related intention and behaviour change. State-by-time interactions showed population-level increases in self-referent thoughts about the health-harms of overweight (P < 0.05) and physical activity intentions (P < 0.05). Endorsement of stereotypes of overweight individuals did not increase after LL aired. LL was associated with some population-level improvements in proximal and intermediate markers of campaign impact. However, sustained campaign activity will be needed to impact behaviour.
Introduction
The World Health Organization (WHO) described obesity as a global epidemic [1]. In Australia, 35% of adults are overweight and 28% are obese [2]. Similarly high rates are found throughout the developed world [3, 4] increasing people’s risk of type 2 diabetes, cardiovascular disease and some cancers [5]. Excess body weight occurs due to an energy imbalance influenced by modifiable lifestyle factors of increased activity and reduced dietary intake [6]. The WHO identified mass media as effective for disseminating messages about obesity prevention to populations [1]. A substantial science base concerning principles of effective media campaigns may be applied to obesity prevention [7].
Previous weight and lifestyle campaigns
Evidence indicates mass media campaigns can positively influence health behaviours [7–9], including physical activity [10–12] and diet [13, 14]. Previous Australian state and national public health campaigns addressed these antecedents of overweight [13, 15–19]. More recently, public health campaigns in Australia [20–24] and elsewhere [25–28] have explicitly addressed overweight. There has also been considerable programming about overweight in mainstream media [29, 30]. The first such published evaluation used Body Mass Index (BMI) as the primary response indicator and no evidence of impact was found [31]. The BBC’s (United Kingdom) ‘Fighting Fit, Fighting Fat’ obesity reduction campaign recorded population recall of around one-in-five and behaviour change of 1% [25]. Other campaigns in the Netherlands [26, 28] and United Kingdom [27] successfully increased population awareness, with no marked improvements in behaviour. Australian campaigns [21, 23, 24] achieved unprompted or semi-prompted recall of 16–38%. The first public health campaign to associate abdominal adiposity with cancer risk [22] achieved increased public awareness of this link. Together these results indicate that in the early stages of implementation, obesity prevention mass media campaigns have yielded more impact on proximal variables such as message awareness and understanding than on intermediate impacts such as belief, attitudes and intentions, or on distal impacts such as behaviour or weight change.
Although mass media campaigns have traditionally been designed to change population health behaviours, they may actually exert the greatest, direct influence on crucial preceding attitudinal variables [10, 32] and indirectly influence behaviour by setting the agenda for discussion by the public and policy makers [33]. Health behaviour [34–36], communication theories [37] and prior research [7] indicate levering changes in cognitions and/or emotions offers a route to effecting improvements in health protective behaviours. Considering such processes in planning and evaluating weight and lifestyle campaigns should optimize their persuasive potential.
Previous obesity prevention campaigns have tended to emphasize messages about ‘how’ to achieve healthy weight through increased activity and healthy eating. Some campaigns have included messages on weight-related chronic disease—typically through voice overs, ‘skin deep’ representations of people affected by overweight or cartoon-like animations of internal disease processes [38]. Theory suggests designing obesity prevention campaigns to simultaneously ‘motivate’, ‘reinforce’ and ‘enable’ people to achieve change will optimize the chances of impact [39]. Such an approach entails communicating both ‘why’ and ‘how’ to change. Evidence from anti-smoking campaigns suggests messages oriented towards providing viewers with information on ‘why’ they should make health-related behaviour changes are associated with greater recall, perceived effectiveness, attitude, intention and behaviour change [33, 40–44]. Recent evidence also suggests messages about the health consequences of excess body weight accompanied by graphic imagery represent the most persuasive mass media approach to obesity prevention [45].
The ‘LiveLighter’ campaign
The ‘LiveLighter’ (LL) campaign is unique for explicitly presenting graphic anatomical images of visceral fat to illustrate negative health effects of overweight, [46–48] alongside recommending alternatives to obesogenic behaviours [49]. Development of LL was informed by a review [50] of best practice approaches to mass media and social marketing campaigns on physical activity, healthy eating and healthy weight [e.g. 1, 9, 37, 51, 52]. Campaign development and evaluation were guided by an applied analysis of behaviours the campaign intended to influence, in light of well-established principles of behaviour change [34–36], synthesized in Rogers [53] and Hill and Dixon [39]. Being a pragmatic campaign, LL drew on theory, but did not set out to comprehensively test a single theoretical model [54]. The campaign rationale contended at-risk individuals will act to reduce body weight and maintain that reduction to the extent they are: ‘motivated’—determined by the personal perceived and ‘felt’ threat of disease and the extent to which the benefits of weight reduction are seen to outweigh the costs [36], ‘enabled’—belief one has the skills and ability necessary for behaviour change [34, 35] and ‘reinforced’—characterized by the extent to which results are observable [53].
This paper reports evaluation of the first year of the LL campaign. The primary aim was to estimate the population-impact of LL on proximal outcomes (campaign recall and appraisal) and determine whether there were differences in these measures based on orientation of the message. Secondary aims were to estimate LL’s population-level impact on intermediate indicators (attitudes, beliefs and intentions) and more distal outcomes (behaviour changes).
Materials and methods
Intervention
The principal (30 s) LL campaign ad graphically depicted extensive visceral ‘toxic fat’ around an overweight person’s organs. To provide ‘motivation’ for change, the ad aimed to increase awareness and create new understanding of health consequences of overweight, together with exposure to physiological realities of overweight. This ad provided the ‘why’ change campaign message and was executed to engender interest, surprise and self-referent feelings such as alarm by convincing people they may be personally susceptible to the threat. Four supporting ads reminded viewers of this visceral imagery and provided ‘how’ to change messages, illustrating small achievable changes in activity and diet that can be made in the immediate-term to successfully avert the threat [55] (i.e. ‘enablement’). Highlighting opportunities for immediate action was central to the campaign rationale, to provide positive ‘self-reinforcement’ to help relieve any alarm felt in response to the ad and condition weight control behaviours [53]. Campaigns that seek to reframe an issue as a public health problem and provide suggestions for resolution are less likely to prompt defensive responses than health threats alone [55]. LL advertisements were extensively pre-tested with formative, qualitative research among overweight and healthy weight adults [56].
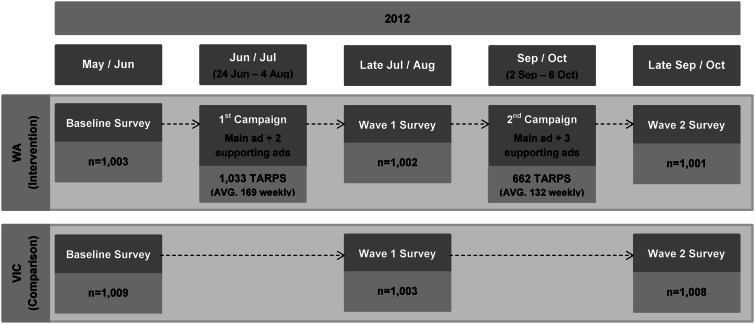
LL was launched in Western Australia (WA) (population 2.5 million) [57] on 24 June 2012. Because of greater likelihood of weight gain between ages 25 and 64 [2] the campaign primarily targeted this age group. Figure 1 shows campaign dates, evaluation design and Target Audience Rating Points (TARPs), a media exposure measure indicating reach and frequency of campaign waves [58]. The principal ad was broadcast during both media waves, complemented by two different supporting ads (15 s) on diet and activity. An additional supporting ad at the second media wave depicted the campaign Website (www.livelighter.com.au), where the ads and supporting information could be accessed. Paid television advertising was complemented by paid cinema, radio, print and online advertising. The campaign budget was comparable with those of commercial media campaigns. The advertising was part of a broader strategy aimed to generate community, media and political support, through media advocacy and stakeholder engagement, for policy and environmental changes supportive of healthy eating and physical activity.
Fig. 1.
LL campaign timeline and evaluation design. Note: TARPs are a product of the percentage of the target audience exposed to an advertisement (reach) and the average number of times a target audience member would be exposed (frequency) [37]. Hence, 200 TARPs might represent 100% of the target audience receiving the message an average of two times over a specified period or 50% reached four times.
Evaluation design and sample
To assess campaign impact, a pre-campaign cross-sectional survey was undertaken and repeated following each media wave in WA (intervention state) and Victoria (comparison state) (see Fig. 1). A random sample of 2012 (intervention N = 1003; comparison N = 1009) adults aged 25–49 were surveyed at baseline, and 2005 at wave 1 (W1) (intervention N = 1002; comparison N = 1003) and wave 2 (W2) (intervention N = 1001; comparison N = 1008). The sample sizes yielded a sub-sample of overweight adults {based on BMI [weight (kg)/height (m)2] = 25+, using self-reported height and weight} [59] and parents (of at least one child under 18 years who resides with them) for analysis (largest 95% CI around an estimate of 50% is ±4.3%).
The evaluation was approved by Cancer Council Victoria’s Human Research Ethics Committee. Random digit dialling drew from a sample frame of private household telephone landline numbers. The person who identified as the youngest male aged 25–49 (or youngest female if no males) in the household was selected for interview. At each survey, quotas of 45/55% for sex (male/female), 35/65% for age-group (25–34/35–49) and 70/30% for region (metropolitan/rural) were achieved in both states. Response rates were 35%, 40% and 44% across the respective surveys.
Measures
Given practical and financial constraints on survey length, the survey instrument was designed to parsimoniously assess those indicators predicted to be influenced by the LL campaign, rather than to test a complete theoretical model.
Intervention sample
Campaign recall
Measured by asking respondents to describe any television advertisements about being overweight they had seen in the past month and coding mentions of LL ads.
Recognition
Measured by prompting respondents with a brief description (principal ad: ‘an overweight man eating pizza from the fridge’). Recall or recognition was summed to provide total awareness.
Perceived message effectiveness
Ratings of the campaign advertising were obtained in the post-campaign surveys (see Table II for wording), as such measures can predict health-related behaviour change [40–42, 60–65].
Table II.
Perceived effectiveness of LL in the intervention state
| Overall |
BMI |
||
|---|---|---|---|
| BMI < 25 | BMI 25+ | ||
| (N = 685) | (N = 287) | (N = 383) | |
| Principal ada | |||
| Was believable | 95.5 | 95.6 | 95.2 |
| Was relevant to me | 55.7 | 36.6b | 69.9** |
| Taught me something new | 52.3* | 49.7 | 55.3 |
| Made me stop and think | 75.8* | 70.7b | 78.9** |
| Made a strong argument for reducing weight | 87.7* | 88.6 | 86.8 |
| Made me motivated to take action to reach or stay a healthy weight | 65.3* | 63.1 | 66.0 |
| Made me feel uncomfortable | 35.6* | 33.9 | 37.2 |
| Prompted me to discuss the ad | 30.3* | 30.3 | 31.0 |
| Supporting ad(s)c | (N = 484) | (N = 197) | (N = 277) |
| Was believable | 94.8 | 94.7 | 94.7 |
| Was relevant to me | 56.3 | 46.7b | 62.6** |
| Taught me something new | 36.2b | 34.9 | 37.9 |
| Made me stop and think | 66.1b | 56.9b | 70.6** |
| Made a strong argument for reducing weight | 80.3b | 78.2 | 81.8 |
| Made me motivated to take action to reach or stay a healthy weight | 55.2b | 56.5 | 54.2 |
| Made me feel uncomfortable | 17.1b | 13.8 | 19.4 |
| Prompted me to discuss the ad | 18.8b | 13.8 | 22.7 |
aPooled responses to the principal ad in the first (Jun/Jul) and second media waves (Sept/Oct).
bReference category.
cPooled responses to the supporting ads shown in the first (Jun/Jul) and second media waves (Sept/Oct).
*Significant difference by ad type at P < 0.05 and
**BMI at P < 0.05.
All respondents
Self-referent thoughts about weight and health
Respondents were asked how often they thought about the health-related harms of overweight (i.e. perceived susceptibility defined by the Health Belief Model [36]) and what they thought the impact of weight loss would be on their health.
Attitudes
Given attitudes and beliefs form the basis on which decisions to act are made [36], overweight respondents (BMI = 25+) were asked to rate the personal perceived urgency of weight loss on a 10-point Likert scale (0 = ‘not at all’, 5 = ‘fairly’, 10 = ‘extremely’). Owing to positive skewness in the distribution, responses were dichotomized at the median (0–6 or 7–10) for analysis. Overweight respondents were also asked whether they thought the benefits of weight loss would outweigh the costs using a forced-choice categorical response scale.
Self-efficacy
Given belief that one has the skills and ability necessary for behaviour influences its occurrence, [34, 35] weight loss self-efficacy was rated by overweight respondents (BMI = 25+) on a 10-point Likert scale and dichotomized at the median as described above.
Intentions and behaviour
Intentions are thought to precede behaviour change [34]. Respondents were asked whether it was likely they would make specific dietary changes over the next 7 days. A composite scale combined ratings of ‘slightly’ or ‘very’ likely they would do two of the following in the next 7 days: (i) cut down the amount of high calorie foods you eat, (ii) drink fewer sugar-sweetened drinks, (iii) eat smaller portion sizes and (iv) eat more fruit and vegetables. Respondents were also asked the likelihood they would meet recommended physical activity levels in the following week; their current plans concerning weight loss; and whether they had taken any steps to try to lose weight in the last 7 days. Steps to weight loss include participants who reported at least one behaviour in the question: ‘In the past 7 days, what steps, if any, have you taken to try to lose weight?’
Overweight stereotypes
To check for potential unintended effects of the campaign on weight-based stereotypes, respondents were asked whether they agreed or disagreed that overweight (cf. ‘healthy’ weight) people are more likely to (i) be happier, (ii) lack willpower, (iii) have fewer friends, (iv) be more outgoing and (v) have less energy. A composite scale combined ratings of ‘agreed’ for two or more of these stereotypes. They were also asked whether they agreed with two broader societal stereotypes. (See Table III for details of survey wording.)
Table III.
Adjusted proportions and state by study phase interactions for attitudinal and behavioural measures
|
Overall sample |
BMI 25+ |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adjusted proportions |
Adjusted proportions |
|||||||||||||
| WA |
VIC |
F (df) | WA |
VIC |
F (df) | |||||||||
| B | W1 | W2 | B | W1 | W2 | B | W1 | W2 | B | W1 | W2 | |||
| N | 973 | 968 | 981 | 986 | 975 | 966 | N | 540 | 509 | 524 | 539 | 519 | 523 | |
| Awareness of the effect of weight status on health | ||||||||||||||
| In the last 7 days, how often, if at all, did you think about the harms to your health of being or becoming overweight? | 50.7 | 57.6 | 58.8 | 48.0 | 46.9 | 52.3 | B cf. W1: F(1, 3854) = 4.05*; B cf. W2: F(1, 3841) = 2.20 | 62.5 | 71.0 | 71.3 | 61.8 | 61.8 | 59.4 | B cf. W1: F(1, 4949) = 3.30; B cf. W2: F(1, 4960) = 5.30* |
| If you lost weight, do you think your health would: improve (a little or a lot)? | 70.7 | 72.5 | 74.3 | 69.6 | 71.4 | 71.8 | B cf. W1: F(1, 3838) = 0.21; B cf. W2: F(1, 3827) = 0.67 | 87.1 | 84.8 | 87.4 | 87.1 | 87.3 | 87.6 | B cf. W1: F(1, 4946) = 0.33; B cf. W2: F(1, 4958) = 0.01 |
| Weight loss attitudesa | ||||||||||||||
| Thinking about the things you’d need to do to lose weight, do you think: the sacrifices would outweigh the benefits? | 64.1 | 68.4 | 72.2 | 65.7 | 66.9 | 66.8 | B cf. W1: F(1, 2078) = 0.27; B cf. W2: F(1, 2091) = 1.81 | |||||||
| How confident are you that you could lose enough weight to achieve a healthy weight? (7–10) | 60.5 | 64.2 | 66.9 | 60.9 | 61.4 | 63.1 | B cf. W1: F(1, 2041) = 0.46; B cf. W2: F(1, 2061) = 0.44 | |||||||
| How would you rate the urgency of your losing weight? (7–10) | 30.1 | 30.9 | 31.0 | 30.1 | 30.3 | 31.9 | B cf. W1: F(1, 2065) = 0.02; B cf. W2: F(1, 2075) = 0.01 | |||||||
| Weight loss intentions & behaviours | ||||||||||||||
| Intend to make dietary changes in the next 7 daysb | 59.6 | 60.2 | 66.9 | 52.7 | 60.4 | 65.0 | B cf. W1: F(1, 3859) = 2.28; B cf. W2: F(1, 3848) = 0.95 | 66.5 | 63.6 | 69.2 | 61.4 | 62.7 | 68.4 | B cf. W1: F(1, 4950) = 0.50; B cf. W2: F(1, 4963) = 0.38 |
| Intend to do 30 min of moderate physical activity in the next 7 days | 73.6 | 76.9 | 84.0 | 75.6 | 72.4 | 78.1 | B cf. W1: F(1, 3852) = 3.65; B cf. W2: F(1, 3843) = 3.91* | 74.0 | 77.1 | 84.0 | 75.3 | 73.9 | 78.4 | B cf. W1: F(1, 4946) = 0.75; B cf. W2: F(1, 4960) = 1.85 |
| Plan to lose weight within the next month | 41.7 | 36.6 | 44.6 | 35.1 | 36.9 | 42.2 | B cf. W1: F(1, 2605) = 2.18; B cf. W2: F(1, 2660) = 1.05 | 46.3 | 42.3 | 50.4 | 42.5 | 41.7 | 48.1 | B cf. W1: F(1, 4490) = 0.31; B cf. W2: F(1, 4530) = 0.09 |
| Taken steps to lose weight in the last 7 daysc | 54.5 | 50.8 | 51.4 | 42.7 | 45.0 | 46.8 | B cf. W1: F(1, 3196) = 1.78; B cf. W2: F(1, 3221) = 1.85 | 66.0 | 61.4 | 59.8 | 51.5 | 56.5 | 53.8 | B cf. W1: F(1, 4725) = 2.67; B cf. W2: F(1, 4754) = 2.15 |
| Overweight stereotypes | ||||||||||||||
| Individual stereotypesd | 76.0 | 73.4 | 72.9 | 70.8 | 73.2 | 72.6 | B cf. W1: F(1, 3859) = 2.05; B cf. W2: F(1, 3848) = 2.39 | 75.5 | 71.1 | 72.1 | 72.7 | 73.3 | 74.0 | B cf. W1: F(1, 4950) = 1.22; B cf. W2: F(1, 4963) = 1.36 |
| Nowadays an overweight person is more likely to be blamed for their health problems | 87.2 | 85.6 | 87.1 | 86.3 | 84.5 | 83.8 | B cf. W1: F(1, 3823) = 0.03; B cf. W2: F(1, 3815) = 1.04 | 86.9 | 86.4 | 87.6 | 89.7 | 86.4 | 83.1 | B cf. W1: F(1, 4929) = 0.84; B cf. W2: F(1, 4945) = 3.44 |
| Health authorities exaggerate the harmful effects of being overweight | 18.2 | 18.0 | 13.2 | 19.6 | 16.4 | 16.5 | B cf. W1: F(1, 3831) = 0.49; B cf. W2: F(1, 3819) = 1.12 | 21.2 | 19.7 | 13.1 | 21.0 | 16.1 | 18.2 | B cf. W1: F(1, 4937) = 0.51; B cf. W2: F(1, 4944) = 2.06 |
B, Baseline Survey; W1, Survey wave 1; W2, Survey wave 2.
aOnly asked of BMI 25+.
bIncludes participants who reported it is ‘slightly’ or ‘very’ likely they would do two of the following in the next 7 days: (i) cut down the amount of high calorie foods you eat, (ii) drink fewer sugar-sweetened drinks, (iii) eat smaller portion sizes and (iv) eat more fruit and vegetables.
cIncludes participants who reported at least one behaviour in response to: ‘In the past 7 days, what steps, if any, have you taken to try to lose weight?’.
dIncludes participants who ‘agree’ with two or more stereotypes: compared with healthy weight people, overweight people are more likely to (i) be happier, (ii) lack willpower, (iii) have fewer friends, (iv) be more outgoing, and (v) have less energy.
*Significant difference at P < 0.05.
Statistical analysis
Data were analysed using Stata SE 11.1 (StataCorp, Texas) during 2013 and weighted to the population on sex, age, place of residence [66] and educational attainment [67]. Chi-square analysis assessed whether demographic characteristics differed between states at each survey. Logistic regression analysis tested interactions by state (WA versus Victoria) and subsequent surveys (baseline versus W1; baseline versus W2) controlling for socio-economic status (SES) and BMI. Interactions were tested for the full sample and the sub-sample of overweight/obese respondents. Overweight/obese and healthy weight/underweight categories were combined and are referred to as ‘overweight’ and ‘not overweight’, respectively. Logistic regression was undertaken to determine whether campaign recall differed according to sex, age, BMI, parental status, place of residence and SES when controlling for all other factors and time spent viewing commercial television. Differences in ratings of perceived effectiveness by ad type (principal versus supplementary) were tested using logistic regression controlling for individual-level clustering and the above demographics.
Results
Respondent characteristics
Table I shows the samples surveyed in each state and study phase comprised similar distributions for all demographic characteristics except a greater proportion of WA than Victorian respondents were of high SES at baseline (P < 0.05) and at W2 (P < 0.05). Consequently all multivariate analyses controlled for SES.
Table I.
Demographic characteristics, by state and study phase
|
Western Australia |
Victoria |
|||||
|---|---|---|---|---|---|---|
| Baseline (June) (%) (N = 1003) | W1 (August) (%) (N = 1002) | W2 (October) (%) (N = 1001) | Baseline (June) (%) (N = 1009) | W1 (August) (%) (N = 1003) | W2 (October) (%) (N = 1008) | |
| Sex | ||||||
| Male | 45.1 | 44.8 | 45.0 | 45.3 | 44.9 | 44.6 |
| Female | 54.9 | 55.2 | 55.0 | 54.7 | 55.1 | 55.4 |
| Age (years) | ||||||
| 25–34 | 34.9 | 34.8 | 34.7 | 35.1 | 35.0 | 35.7 |
| 35–44 | 40.4 | 41.1 | 38.1 | 38.9 | 40.6 | 36.3 |
| 45–49 | 24.7 | 24.1 | 27.3 | 26.1 | 24.4 | 28.0 |
| Parent (child under 18) | 57.5 | 60.1 | 53.5 | 60.8 | 58.2 | 52.3 |
| BMIa | ||||||
| Underweight | 2.7 | 1.8 | 1.8 | 2.2 | 2.7 | 1.6 |
| Healthy weight | 41.8 | 45.7 | 44.8 | 43.1 | 44.1 | 44.3 |
| Overweight | 35.8 | 35.7 | 35.5 | 37.8 | 34.9 | 37.6 |
| Obese | 19.7 | 16.8 | 17.9 | 16.8 | 18.4 | 16.6 |
| Place of residence | ||||||
| Metropolitan | 70.0 | 70.0 | 70.0 | 70.0 | 69.8 | 69.4 |
| Rural | 30.0 | 30.0 | 30.0 | 30.0 | 30.2 | 30.6 |
| SESb | ||||||
| Low SES | 27.9 | 30.2 | 28.1 | 33.2 | 32.9 | 33.1 |
| Mid SES | 39.4 | 38.1 | 38.5 | 40.1 | 40.4 | 40.8 |
| High SES | 32.7* | 31.7 | 33.4* | 26.7* | 26.6 | 26.1* |
| Completed secondary school | 69.6 | 68.5 | 70.2 | 70.4 | 68.9 | 68.3 |
| Aboriginal and/or Torres Strait Islander (ATSI) | 1.6 | 0.9 | 0.8 | 0.8 | 0.4 | 1.3 |
Unweighted percentages. Percentages are rounded so may not sum to 100%.
aWeight status based on BMI [weight (kg)/height (m)2] using self-reported height and weight classified into weight categories according to internationally recognized cutoffs [59].
bSES was determined according to the Index of Relative Socio-Economic Disadvantage (IRSD) rankings for Western Australia and Victoria as described by the Australian Bureau of Statistics [68, 69] based on respondent’s home postcode. Low IRSD indicates greater disadvantage, high IRSD indicated least disadvantage. At baseline, no IRSD value was available for 21 respondents, 24 at W1 and 38 at W2.
*Significant difference at P < 0.05.
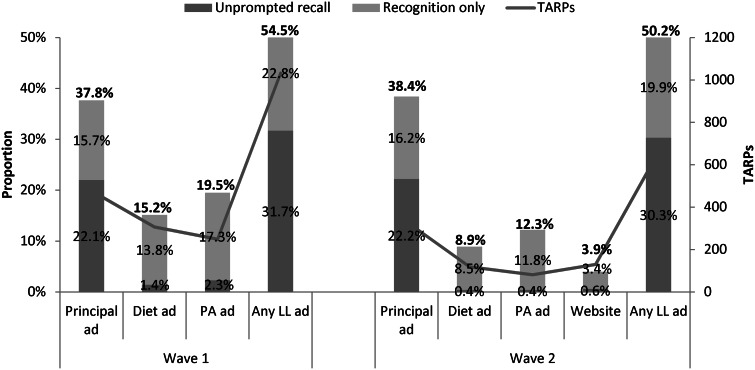
Recall and total awareness of the LL campaign
Time-by-state comparisons indicated a strong effect of the campaign on unprompted recall of weight-related advertising [W1: F(1, 3917) = 20.54, P < 0.001; W2: F(1, 3920) = 15.17, P < 0.001]. In WA there was a significant increase from 36% to 55% and 48%, respectively, in the post-campaign surveys [W1: odds ratio (OR), 2.22, 1.77–2.79, P < 0.001; W2: OR = 1.69, 1.35–2.12, P < 0.001], whereas in Victoria the proportions remained stable across surveys at 29%, 29% and 26% (W1: OR = 1.02, 0.80–1.31, P = 0.85; W2: OR = 0.86, 0.67–1.11, P = 0.25). Around one-in-three adults recalled any LL ad and total campaign awareness was 54% at W1 and 50% at W2 (Fig. 2). Among overweight respondents total awareness was 58% at W1 and 53% at W2 (not shown in Fig. 2).
Fig. 2.
Awareness of LL in the intervention state by TARPs. Note: Any LL ad includes general mentions of toxic fat and figures are greater than the sum of the individual ads as more than one ad could be counted for a given respondent.
At W1, campaign recall was significantly greater among overweight adults (35% cf. 27%; OR = 1.48, 1.03–2.14, P = 0.03). At W2, parents were more likely to recall LL (35% cf. 26%; OR = 1.59, 1.09–2.32, P = 0.02). Campaign recall did not significantly differ by sex or SES.
Perceived effectiveness of the LL campaign
Respondents who recognized at least one campaign ad (48% W1 and 43% W2) were asked to appraise it. Campaign ads were perceived by almost all adults who saw them as ‘believable’ and to have ‘made a strong argument for reducing weight’, with approximately half recognizing them as ‘relevant to me’ (see Table II). Respondents who saw the principal ad showed a higher likelihood of saying the ad ‘made me stop and think’ (OR = 1.65, 1.20–2.27, P = 0.01), ‘taught me something new’ (OR = 1.98, 1.48–2.65, P < 0.001), ‘made a strong argument for reducing weight’ (OR = 1.55, 1.01–2.37, P = 0.04), ‘motivated me to take action to reach or stay a healthy weight’ (OR = 1.49, 1.11–2.01, P = 0.01), ‘made me feel uncomfortable’ (OR = 2.63, 1.87–3.69, P < 0.001) and prompted discussion (OR = 1.72, 1.23–2.41, P = 0.01), compared with respondents who saw the supporting ads. Overweight adults were more likely to agree the principal and supporting ads were ‘relevant to me’ (OR = 4.23, 2.77–6.44, P < 0.001; OR = 1.92, 1.18–3.13, P = 0.01) and ‘made me stop and think’ (OR = 1.69, 1.06–2.68, P = 0.03; OR = 1.79, 1.08–2.98, P = 0.02).
Impact of the LL campaign on attitudes and behaviour
Table III shows adjusted proportions and Wald tests of interactions by state and study phase for baseline, W1 and W2 outcome measures. Significant results are described in-text. Compared with baseline, a greater proportion of WA adults reported thinking about the harms to their health of being or becoming overweight at W1 (OR = 1.32, 1.06–1.65, P = 0.01), whereas this difference was not seen in Victoria (OR = 0.95, 0.76–1.19, P = 0.68). The same pattern of results was found among overweight adults at W2 (WA: OR = 1.49, 1.07–2.07, P = 0.02; Victoria: OR = 0.90, 0.66–1.24, P = 0.53). The proportion of WA adults who reported they would likely meet physical activity recommendations in the immediate term increased significantly from baseline to W2 (OR = 1.89, 1.44–2.47, P < 0.001), whereas such an increase was not seen in Victoria (OR = 1.15, 0.88–1.50, P = 0.30). Interactions tested by state and study phase for weight loss attitudes and overweight stereotypes were not significant.
Discussion
LL campaign advertising in WA achieved strong penetration in a media environment containing much editorial, advertising and entertainment content on overweight. Gaining ‘cut-through’ is a necessary prerequisite for effective mass media communication of health messages [70] and is a particular challenge for obesity prevention messages given the cluttered media environment. Campaign awareness was fairly stable across the two waves (54% and 50%) despite a reduction in total TARPs at W2 (1033 cf. 662). This population reach is comparable with that reported for other obesity prevention campaigns locally (49%) [16] and internationally (56%) [28].
That overweight adults were significantly more likely to recognize the self-relevance of the principal ad provides evidence LL reached and resonated with the target audience. This specificity distinguishes LL from other obesity prevention campaigns which found no difference in campaign awareness or self-relevance by BMI [22, 25, 71]. That parents were more likely to recall the campaign at W2 is encouraging as the association between parents’ and children’s body weight [72–74] is at least partly attributable to parental modelling and supervision [75, 76]. Some obesity prevention campaigns have been recalled more by women and higher SES respondents [16, 23, 24]. Notably, recall of LL was similar by gender and across SES.
The principal ad was more commonly recalled after each media wave than supporting ads and the difference was disproportionate to the level of TARPs. This suggests the ‘why’ message was more likely to reach respondents than the ‘how’ messages; a finding consistent with anti-smoking campaigns where use of graphic imagery to illustrate negative health effects of smoking (‘why’ messages) have been associated with higher recall and changes in attitudes, intentions and behaviours than ‘how’ messages [33, 43, 44]. As with anti-smoking advertisements, the LL campaign ‘why’ ad was perceived to have a more effective message than the ‘how’ ads. Such perceptions have been shown to predict subsequent quit intentions and positive changes in smoking behaviours in response to anti-smoking advertising [40–42]. A recent quantitative study comparing viewer’s short-term reactions to various adult-targeted obesity prevention campaign ads found the principal LL ad outperformed others on message acceptance, argument strength, negative emotional impact and personalized perceived effectiveness [45]. These findings contrast with other research [77] which found consumers would prefer messages focussed only on lifestyle change without mentioning body weight. LL took an unequivocal focus on overweight and obesity, backing this up with lifestyle recommendations.
The message of the LL campaign ‘why’ ad aimed to increase awareness of health consequences of overweight to ‘motivate’ lifestyle change [36]. Accordingly, in the intervention state following LL, thoughts about the harms to health of being overweight increased and overweight adults more commonly considered the threat of weight-related disease. The ‘how’ messages of the supporting ads aimed to ‘enable’ viewers to modify their lifestyle [34, 35] by demonstrating immediate and achievable changes that provide positive ‘self-reinforcement’ [53]. The importance of accompanying ‘why’ messages with ‘how’ messages to empower people to avert health threats has been illustrated [55]. Evidence LL enabled viewers to act is found in increased intentions to meet activity guidelines in the immediate term, which is encouraging given such intentions have been associated with weight loss and improved health in the longer-term [78]. LL’s physical activity supporting ad was better recalled and recognized than the dietary supporting ad, despite marginally fewer TARPs for the former—consistent with activity intentions showing more evidence of movement than intentions to change dietary behaviour. Greater recall of physical activity messages than dietary change messages has been reported previously [79]. That an increase in intentions was not evident until W2, despite fewer TARPs for the preceding media wave, suggests the importance of continued reinforcement of the campaign messages over time and with continued investment, further change can be achieved.
As might be expected in the initial phases of a mass media campaign on obesity prevention, LL was not associated with any other changes in weight loss intentions or behaviour. It might be premature to conclude a campaign such as this is inherently incapable of causing behaviour change because a more likely explanation is measurement took place too early for behaviour change to register. LL is a relatively ‘immature’ campaign [70]. To be successful population campaigns require regular media activity over an extended period of time [7, 80, 81] in order to attempt to counter the significant environmental drivers precipitating and maintaining weight gain [82]. Campaigns addressing the complex behaviours antecedent to overweight reduction have commonly not shown direct and immediate impacts on behaviour at the population-level [10, 32, 83, 84] and behavioural effects are more likely to be reported in the longer-term [85]. The present findings would argue for continuing greater emphasis on the ‘why’ message to motivate change, ahead of the ‘how’ message that is useful to people who have become motivated to change. Overall, given awareness (health consequences) increased at W1 and increased intentions (physical activity) emerged at W2, findings support the underpinning of obesity prevention campaigns with a theoretical orientation that recognizes changes in attitudes and beliefs are necessary precursors to volitional behaviour change [34]. Findings also add to the existing body of literature which suggests sustained campaign activity is required to promote measurable behavioural impact [7, 33, 80, 81].
Some have suggested campaigns such as LL could unintentionally stigmatize overweight people [77, 86]. Pleasingly, endorsement of stereotypes of overweight individuals, a measure of the social component of stigma, did not increase after LL aired. Although overweight respondents were significantly more likely than healthy weight respondents to recognize the self-relevance of LL ads, this evaluation found they were no more likely to experience a negative emotional response to the ads. However, in a comparative ad rating study testing short-term reactions to ads, overweight adults did show stronger negative emotional reactions to the principal LL ad than healthy weight participants, as well as stronger perceptions of perceived effectiveness such as confidence and motivation in response to the ad [45]. Future longitudinal research should examine the extent to which negative emotional responses to obesity prevention advertising are tied with perceptions of advertising effectiveness and adaptive behavioural responses. The campaign did not affect perceptions that health authorities exaggerate health effects of overweight, implying acceptance of the campaign message that overweight is associated with serious health issues, which could provide motivation for weight reduction.
Use of a pre–post-test comparison group evaluation design significantly enhances the strength of the evidence of campaign effects by allowing comparisons longitudinally in outcomes of interest in exposed and unexposed populations, controlling for most threats to internal validity [70, 79, 87]. Limitations include difference in history of exposure to nutrition, activity and obesity prevention campaigns in the two states [7, 13, 16, 19]. For example, this could have led to a greater effect of the campaign given the audience was primed to think about the issues addressed, or to the campaign having a lesser impact than a new message might for an audience not previously primed to think about their weight, diet or activity. It was not possible to control for potential confounders unrelated to the campaign that were unique to WA and may have affected weight-related intentions and behaviours. Reliance on self-report and risk of socially desirable responses are possible sources of bias, although seemingly unlikely to apply differentially to the intervention and comparison states.
Conclusions
LL achieved significant ‘cut-through’ amidst the cluttered field of mass media messages about overweight. Population awareness, which compares favourably with other obesity prevention campaigns, was maintained after W2 despite a reduced media buy. LL was more likely to be recalled by overweight adults who were consistently more likely to perceive the campaign was relevant to them, suggesting LL reached and resonated with the target audience. That the principal campaign ad was more likely than supporting ads to reach viewers and be rated favourably on measures of perceived message effectiveness, suggests the importance of inclusion of the ‘why’ change message alongside the ‘how’ to change message. Despite significant countervailing environmental forces, LL was associated with some population-level improvements in proximal and intermediate markers of campaign impact, and was not associated with an increase in negative stereotypes about overweight individuals. The sequence of these improvements supports the influence of mass media campaigns on crucial preceding attitudinal variables and the need for sustained media activity over time. Findings provide evidence to help inform planning and development of future public health campaigns addressing overweight.
Acknowledgements
The authors gratefully acknowledge the work of the Survey Research Centre at Edith Cowan University, Western Australia in undertaking the data collection for this study.
Funding
This study was funded by the National Heart Foundation of Australia (Western Australian Division), which is contracted by the Department of Health Western Australia to conduct the ‘LiveLighter’ campaign in partnership with the Cancer Council Western Australia.
Conflict of interest statement
Five of the authors (Swanson, Szybiak, Shilton, Pratt & Slevin) are employees of the Heart Foundation (Western Australia) or Cancer Council Western Australia who were involved in the development and/or implementation of the ‘LiveLighter’ campaign.
References
- 1.WHO. Obesity: preventing and managing the global epidemic. Geneva: WHO, 1998. [PubMed] [Google Scholar]
- 2.Australian Bureau of Statistics. Australian Health Survey: Updated Results, 2011-12. Catalogue No. 4364.0.55.003, Canberra: Australian Bureau of Statistics, 2013. [Google Scholar]
- 3.Flegal KM, Carroll MD, Kit BK. et al. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 2012; 307: 491–7. [DOI] [PubMed] [Google Scholar]
- 4.Stevens GA, Singh GM, Lu Y. et al. National, regional, and global trends in adult overweight and obesity prevalences. Popul Health Metr 2012; 10: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO. Diet, nutrition and the prevention of chronic disease: Report of a Joint WHO/FAO Expert Consultation. WHO Technical Report Series No. 916. Geneva: WHO, 2003. [Google Scholar]
- 6.International Agency for Research on Cancer. Weight control and physical activity. Lyon: World Health Organization, 2002. [Google Scholar]
- 7.Wakefield MA, Loken B, Hornik RC. Use of mass media campaigns to change health behaviour. Lancet 2010; 376: 1261–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Snyder LB, Hamilton MA. A meta-analysis of U.S. health campaign effects on behaviour: emphasize enforcement, exposure, and new information, and beware the secular trend In Hornik R.C. (ed). Public health communication: Evidence for behaviour change ). Mahway, NJ: Lawrence Erlbaum; 2002, 357–84. [Google Scholar]
- 9.Stead M, Gordon R, Angus K. et al. A systematic review of social marketing effectiveness. Health Educ 2007; 107: 126–91. [Google Scholar]
- 10.Cavill N, Bauman A. Changing the way people think about health-enhancing physical activity: do mass media campaigns have a role? J Sports Sci 2004; 22: 771–90. [DOI] [PubMed] [Google Scholar]
- 11.Huhman ME, Potter LD, Duke JC. et al. Evaluation of a national physical activity intervention for children. VERB campaign, 2002-2004. Am J Prev Med 2007; 32: 38–43. [DOI] [PubMed] [Google Scholar]
- 12.Leavy JE, Bull FC, Rosenberg M. et al. Physical activity mass media campaigns and their evaluation: a systematic review of the literature 2003-2010. Health Educ Res 2011; 26: 1060–85. [DOI] [PubMed] [Google Scholar]
- 13.Pollard CM, Miller MR, Daly AM. et al. Increasing fruit and vegetable consumption: success of the Western Australian go for 2&5? Campaign. Public Health Nutr 2008; 11: 314–20. [DOI] [PubMed] [Google Scholar]
- 14.Pomerleau J, Lock K, Knai C. et al. Interventions designed to increase adult fruit and vegetable intake can be effective: a systematic review of the literature. J Nutr 2005; 1486–95. [DOI] [PubMed] [Google Scholar]
- 15.Bauman A, Bellew B, Owen N. et al. Impact of an Australian mass media campaign targeting physical activity in 1998. Am J Prev Med 2001; 21: 41–7. [DOI] [PubMed] [Google Scholar]
- 16.Leavy JE, Rosenberg M, Bauman AE. et al. Effects of find thirty every day®: cross-sectional findings from a Western Australian population-wide mass media campaign, 2008-2010. Health Educ Behav 2013; 40: 480–92. [DOI] [PubMed] [Google Scholar]
- 17.Rosenberg M, Ferguson Evaluation of the Unplug and Play media campaign, 2011. Perth: University of Western Australia, Health Promotion Evaluation Unit, 2011. [Google Scholar]
- 18.Carins JE, Rundle-Thiele SR. Eating for the better: a social marketing review (2000-2012). Public Health Nutr 2013; 28: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dixon H, Borland R, Segan C. et al. Public reaction to Victoria's “2 Fruit 'n' 5 Veg Every Day” campaign and reported consumption of fruit and vegetables. Prev Med 1998; 27: 572–82. [DOI] [PubMed] [Google Scholar]
- 20.Department of Health and Ageing. Evaluation of the Australian Better Health Initiative Measure Up social marketing campaign: Phase 1 Melbourne: The Social Research Centre (SRC), 2010.
- 21.French S, Wood L, Rosenberg M. et al. Healthy Weight, Draw the Line campaign evaluation. Evaluation report 1, baseline and post media wave one data. Perth: University of Western Australia, 2009. [Google Scholar]
- 22.Morley B, Wakefield M, Dunlop S. et al. Impact of a mass media campaign linking abdominal obesity and cancer: a natural exposure evaluation. Health Educ Res 2009; 24: 1069–79. [DOI] [PubMed] [Google Scholar]
- 23.King EL, Grunseit AC, O’Hara BJ. et al. Evaluating the effectiveness of an Australian obesity mass-media campaign: how did the ‘Measure-Up’ campaign measure up in New South Wales? Health Educ Res 2013; 28: 1029–39. [DOI] [PubMed] [Google Scholar]
- 24.Myers P. ANPHA, Evaluation of the ‘Swap it, Don’t Stop it’ social marketing campaign, (wave 6). Melbourne: The Social Research Centre (SRC), 2012. [Google Scholar]
- 25.Wardle J, Rapoport L, Miles A. et al. Mass education for obesity prevention: the penetration of the BBC’s ‘Fighting Fat, Fighting Fit’ campaign. Health Educ Res 2001; 16: 343–55. [DOI] [PubMed] [Google Scholar]
- 26.Wammes B, Oenema A, Brug J. The evaluation of a mass media campaign aimed at weight gain prevention among young Dutch adults. Obesity 2007; 15: 2780–9. [DOI] [PubMed] [Google Scholar]
- 27.Croker H, Lucas R, Wardle J. Cluster-randomised trial to evaluate the ‘Change for Life’ mass media/social marketing campaign in the UK. BMC Public Health 2012; 12: 404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Wechem SN, van Assema P, Brug J. et al. Results of a community-based campaign to reduce fat intake. Nutr Health 1997; 11: 207–18. [DOI] [PubMed] [Google Scholar]
- 29.Bonfiglioli CM, Smith BJ, King LA. et al. Choice and voice: obesity debates in television news. Med J Aust 2007; 187: 442–5. [DOI] [PubMed] [Google Scholar]
- 30.Domoff SE, Hinman NG, Koball AM. et al. The effects of reality television on weight bias: an examination of the biggest loser. Obesity 2012; 20: 993–8. [DOI] [PubMed] [Google Scholar]
- 31.Jeffery RW, Gray CW, French SA. et al. “Evaluation of weight reduction in a community intervention for cardiovascular disease risk: changes in body mass index in the Minnesota Heart Health Program.”. Int J Obes Relat Metab Disord 1995; 19: 30–9. [PubMed] [Google Scholar]
- 32.Beaudoin CE, Fernandez C, Wall JL. et al. Promoting healthy eating and physical activity: short-term effects of a mass media campaign. Am J Prev Med 2007; 32: 217–23. [DOI] [PubMed] [Google Scholar]
- 33.Durkin S, Brennan E, Wakefield M. Mass media campaigns to promote smoking cessation among adults: an integrative review. Tob Control 2012; 21: 127–38. [DOI] [PubMed] [Google Scholar]
- 34.Ajzen I, Fishbein M. Understanding attitudes and predicting social behaviour. NJ: Prentice Hall, 1980. [Google Scholar]
- 35.Bandura A. Health promotion by social cognitive means. Health Educ Behav 2004; 31: 143–64. [DOI] [PubMed] [Google Scholar]
- 36.Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q 1984; 11: 1–47. [DOI] [PubMed] [Google Scholar]
- 37.McGuire WJ. Public communication as a strategy for inducing health promoting behavioural change. Prev Med 1984; 13: 299–319. [DOI] [PubMed] [Google Scholar]
- 38.Dixon H, Scully M, Cotter T. et al. Healthy weight and lifestyle advertisements: an assessment of their persuasive potential. Health Educ Res 2015; 30: 569–79. [DOI] [PubMed] [Google Scholar]
- 39.Hill D, Dixon H. Achieving behavioural changes in individuals and populations In: Elwood JM, Sutcliffe SB. (eds). Cancer Control. New York: Oxford University Press, 2010. [Google Scholar]
- 40.Brennan E, Durkin SJ, Wakefield M. et al. Assessing the effectiveness of antismoking television advertisements: do audience ratings of perceived effectiveness predict changes in quitting intentions and smoking behaviours? Tob Control 2013; 0: 1–7. [DOI] [PubMed] [Google Scholar]
- 41.Davis KC, Nonnemaker J, Duke J. et al. Perceived effectiveness of cessation advertisements: the importance of audience reactions and practical implications for media campaign planning. Health Commun 2013; 28: 461–72. [DOI] [PubMed] [Google Scholar]
- 42.Davis KC, Nonnemaker JM, Farrelly MC. et al. Exploring differences in smokers’ perceptions of the effectiveness of cessation media messages. Tob Control 2011; 20: 26–33. [DOI] [PubMed] [Google Scholar]
- 43.Duke JC, Nonnemaker JM, Davis KC. et al. The impact of cessation media messages on cessation-related outcomes: results from a national experiment of smokers. Am J Health Promot 2014; 28: 242–50. [DOI] [PubMed] [Google Scholar]
- 44.Biener L, Wakefield M, Shiner CM. et al. How broadcast volume and emotional content affect youth recall of anti-tobacco advertising. Am J Prev Med 2008; 35: 14–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dixon H, Scully M, Durkin S. et al. Finding the keys to successful adult-targeted advertisements on obesity prevention: an experimental audience testing study. BMC Public Health 2015. Available at: http://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-015-2159-6 Accessed: 7 December 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Britton KA, Massaro JM, Murabito JM. et al. Body fat distribution, incident cardiovascular disease, cancer, and all-cause mortality. J Am Coll Cardiol 2013; 62: 921–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Despres JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature 2006; 444: 881–7. [DOI] [PubMed] [Google Scholar]
- 48.WHO. Fact sheet No.311.Available at: http://www.who.int/mediacentre/factsheets/fs311/en/index.html. Accessed: 15 July 2014.
- 49.Flay BR, DiTecco D, Schlegal RP. Mass media in health promotion: an analysis using an extended information-processing model. Health Educ Q 1980; 7: 127–47. [DOI] [PubMed] [Google Scholar]
- 50.Bauman A, Bellew B. Healthy Lifestyle Promotion Programs in Western Australia: a review of evaluation and market research into mass media and social marketing campaigns focussed on healthy eating, physical activity and healthy weight. Final Report. Prepared for the National Heart Foundation of Australia, 2011. [WA Division] Available at: https://livelighter.com.au/Assets/resource/researchevidence/Social-Marketing-Review-Bauman-Bellew-Heart-Foundation-WA.pdf. Accessed: 22 October 2015.
- 51.Randolph W, Viswanath K. Lessons learned from public health mass media campaigns: marketing health in a crowded media world. Annu Rev Public Health 2004; 25: 419–37. [DOI] [PubMed] [Google Scholar]
- 52.Rogers EM, Storey JD. (1987). Communication campaigns In Berger C. R., Chafee S. H. (eds). Handbook of Communication Science. London: Sage, 1987, 817–46. [Google Scholar]
- 53.Rogers EM. Diffusion of innovations, 5th edn. New York: Free Press, 2003. [Google Scholar]
- 54.Noar SM. A 10-year retrospective of research in health mass media campaigns: where do we go from here? J Health Commun 2006; 11: 21–42. [DOI] [PubMed] [Google Scholar]
- 55.Ruiter RAC, Kessels LTE, Peters GJY et al. Sixty years of fear appeal research: current state of the evidence. Int J Psychol 2014; 49: 63–70. [DOI] [PubMed] [Google Scholar]
- 56.Murphy M. Heart Foundation (WA) & Cancer Council (Vic), Healthy Lifestyle Promotion Program: report of research to evaluate social marketing advertising concepts, 2012.
- 57.Australian Bureau of Statistics. Australian Demographic Statistics., 2014, Catalogue No. 3101.0, Canberra: Australian Bureau of Statistics, 2013. [Google Scholar]
- 58.Dunlop S, Cotter T, Perez D. et al. Televised antismoking advertising: effects of level and duration of exposure. Am J Public Health 2013; 103: e66–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.WHO. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. 1995, WHO technical report Series 854. Geneva: WHO. [PubMed] [Google Scholar]
- 60.Biener L, McCallum-Keeler G, Nyman AL. Adults’ response to Massachusetts anti-tobacco television advertisements: impact of viewer and advertisement characteristics. Tob Control 2000; 9: 401–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dunlop SM, Cotter T, Perez D. When your smoking is not just about you: anti-smoking advertising, interpersonal pressure and quitting outcomes. J Health Commun 2014; 19: 41–56. [DOI] [PubMed] [Google Scholar]
- 62.Dunlop SM, Wakefield M, Kashima Y. The contribution of antismoking advertising to quitting: intra- and interpersonal processes. J Health Commun 2008; 13: 250–66. [DOI] [PubMed] [Google Scholar]
- 63.Durkin S, Biener L, Wakefield MA. Effects of different types of antismoking ads on reducing disparities in smoking cessation among socioeconomic subgroups. Am J Public Health 2009; 99: 2217–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Farrelly MC, Duke JC, Davis KC. et al. Promotion of smoking cessation with emotional and/or graphic antismoking advertising. Am J Prev Med 2012; 43: 475–82. [DOI] [PubMed] [Google Scholar]
- 65.van den Putte B, Yzer M, Southwell BG. et al. Interpersonal communication as an indirect pathway for the effect of antismoking media content on smoking cessation. J Health Commun 2011; 16: 470–85. [DOI] [PubMed] [Google Scholar]
- 66.Australian Bureau of Statistics. Census of Population and Housing 2011. Catalogue No. 2005.0, Canberra: Australian Bureau of Statistics, 2012. [Google Scholar]
- 67.Australian Bureau of Statistics. 2006 Census of Population and Housing. Catalogue No. 2914.0. Canberra: Australian Bureau of Statistics, 2007. [Google Scholar]
- 68.Australian Bureau of Statistics. Information paper: an introduction to Socio-Economic Indexes for Areas (SEIFA) 2006. Catalogue No. 2039.0, Canberra: Australian Bureau of Statistics, 2008. [Google Scholar]
- 69.Australian Bureau of Statistics. Census of population and housing: Socio-Economic Indexes for Areas (SEIFA) Australian – Data only, 2006. Catalogue No. 2033.0.55.001, Canberra: Australian Bureau of Statistics, 2008. [Google Scholar]
- 70.Hornik RC. Public health communication: evidence for behaviour change. New Jersey: Lawrence Erlbaum Associates, 2002. [Google Scholar]
- 71.Wammes B, Breedveld B, Looman C. et al. The impact of a national mass media campaign in The Netherlands on the prevention of weight gain. Public Health Nutr 2005; 8: 1250–7. [DOI] [PubMed] [Google Scholar]
- 72.Burke V, Beilin LJ, Dunbar D. Family lifestyle and parental body mass index as predictors of body mass index in Australian children: a longitudinal study. Int J Obes Relat Metab Disord 2001; 25: 147–57. [DOI] [PubMed] [Google Scholar]
- 73.Cooper R, Hypponen E, Berry D. et al. Associations between parental and offspring adiposity up to midlife: the contribution of adult lifestyle factors in the 1958 British Birth Cohort Study. Am J Clin Nutr 2010; 92: 946–53. [DOI] [PubMed] [Google Scholar]
- 74.Jaaskelainen A, Pussinen J, Nuutinen O. et al. Intergenerational transmission of overweight among Finnish adolescents and their parents: a 16-year follow-up study. Int J Obes 2011; 35: 1289–94. [DOI] [PubMed] [Google Scholar]
- 75.Moore LL, Lombardi DA, White MJ. et al. Influence of parents’ activity levels on activity of young children. J Pediatr 1991; 118: 215–9. [DOI] [PubMed] [Google Scholar]
- 76.Oliveria SA, Ellison RC, Moore LL. et al. Parent-child relationships in nutrient intake: the Framingham children's study. Am J Clin Nutr 1992; 56: 593–8. [DOI] [PubMed] [Google Scholar]
- 77.Puhl R, Peterson JL, Luedicke J. Fighting obesity or obese persons? Public perceptions of obesity-related health messages. Int J Obes 2013; 37: 774–82. [DOI] [PubMed] [Google Scholar]
- 78.United States Department of Health and Human Services. Physical activity and health: a report of the surgeon general. Washington, DC: US Government Printing Office, 1996. DHHS publication S/N 017-023-00196-5. Available at: www.cdc.gov/nccdphp/sgr/sgr.htm. Accessed: 4 September 2014. [Google Scholar]
- 79.James N, Shilton T, Maitland C. et al. Encouraging Australians to draw the line on gaining weight. J Sci Med Sport 2011; 14: e24 [Google Scholar]
- 80.Hill D, Wakefield M. Designing and evaluating population-wide campaigns In: Stewart BW, Wild CP. (eds). World Cancer Report, 2014. Lyon: International Agency for Research on Cancer, 2014. [Google Scholar]
- 81.Durkin S, Wakefield M. Commentary on Sims et al. (2014) and Langley et al. (2014): mass media campaigns require adequate and sustained funding to change population health behaviours. Addiction 2014; 109: 1003–4. [DOI] [PubMed] [Google Scholar]
- 82.Swinburn B, Sacks G, Hall KD. et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet 2011; 378: 804–14. [DOI] [PubMed] [Google Scholar]
- 83.Bauman A, McLean G, Hurdle D. et al. Evaluation of the national ‘Push Play’ campaign in New Zealand—creating population awareness of physical activity. N Z Med J 2003; 116: U535. [PubMed] [Google Scholar]
- 84.Wimbush E, Macgregor A, Fraser E. Impacts of a national mass media campaign on walking in Scotland. Health Promot Int 1998; 13: 45–53. [Google Scholar]
- 85.Huhman M, Potter LD, Wong FL. et al. Effects of a mass media campaign to increase physical activity among children: year-1 results of the VERB campaign. Pediatrics 2005; 116: e277–84. [DOI] [PubMed] [Google Scholar]
- 86.MacLean L, Edwards N, Garrard M. et al. Obesity, stigma and public health planning. Health Promot Int 2009; 24: 88–93. [DOI] [PubMed] [Google Scholar]
- 87.Flay BR, Cook TD. Three models for summative evaluation of prevention campaigns with a mass media component In: Rice R, Atkin C. (eds). Public Communication Campaigns, 2nd edn. Newbury Park, CA: Sage, 1989. [Google Scholar]