Abstract
Background
China is experiencing a marked increase in ST‐segment elevation myocardial infarction hospitalizations, with 30% occurring among women and higher risk of in‐hospital death in relatively younger age groups (<70). Yet, little is known about sex differences in ST‐segment elevation myocardial infarction presentation and management.
Methods and Results
In a nationally representative sample of patients with ST‐segment elevation myocardial infarction admitted to 162 Chinese hospitals in 2001, 2006, and 2011, we examined sex differences in hospitalization rates, clinical profiles, and quality of care. Among 11 986 patients, the proportion of women was unchanged between 2001 and 2011. The estimated national rates of hospital admission per 100 000 people increased from 4.6 in 2001 to 18.0 in 2011 among men (3.9‐fold increase) and from 1.9 to 8.0 among women (4.2‐fold increase) (P trend<0.0001). The median age of women increased from 68 years in 2001 to 72 years in 2011 (P trend<0.001); however, there was no age change in men (63 years in 2011) (P trend=0.48). After accounting for age, women had a higher frequency of comorbidities. Although there were significant sex differences in the time interval of >12 hours between symptom onset and admission time in 2001, since 2006 delays in presentation were comparable between women and men. Fewer women without contraindications received evidence‐based therapies than men, including reperfusion (57.5% versus 44.2%), early aspirin (88.8% versus 85.9%), and clopidogrel (56.9% versus 52.5%, P<0.001 for all) and the differences were largely unchanged over time.
Conclusions
Women experienced a higher increase in hospitalization rates for ST‐segment elevation myocardial infarction in China between 2001 and 2011 and were less likely to receive evidence‐based therapies, especially reperfusion. In addition to efforts to improve quality of care generally, understanding the reasons for this sex disparity and addressing these differences in care should be a priority.
Clinical Trial Registration
URL: https://www.clinicaltrials.gov. Unique identifier: NCT01624883.
Keywords: acute myocardial infarction, epidemiology, health policy, quality of care, sex
Subject Categories: Quality and Outcomes, Revascularization, Epidemiology, Myocardial Infarction
Introduction
As part of China's epidemiologic transition to higher rates of noncommunicable diseases, women, like men, are experiencing a rapid increase in the incidence of acute myocardial infarction (AMI) and AMI‐related mortality,1 as seen in other low‐ and middle‐income countries.2 In addition, the China Patient‐centered Evaluative Assessment of Cardiac Events (PEACE) study demonstrated sex differences in mortality with women at higher risk of death in younger age groups.3 Yet, much less is known about whether sex differences in clinical profiles and care quality differ between men and women and, if so, whether these differences are explained by age, and how they change over time.
Understanding sex differences in the clinical presentation and quality of care for high‐impact conditions like AMI is instrumental to the prioritization of resources for quality improvement programs. A recognition of sex differences in the treatment of myocardial infarction in the late 1990s and early 2000s4, 5, 6 in the United States led to national campaigns7 and female‐specific guidelines.8, 9, 10 Subsequently, sex gaps in care have narrowed over time.5, 11 Previous studies in China demonstrate similar sex differences in treatment of comorbidities and outcomes.3, 12, 13, 14 However, these studies were generally limited to single sites or centers located predominantly in urban areas and examined single points in time, warranting a national perspective on sex differences in clinical presentation and quality of care in China.12, 13 Moreover, given that women are older than men at the time of an AMI,3, 15 it remains unknown whether these differences could be explained by age or how sex‐based differences have changed over the last decade during improved access and healthcare quality in China.16
To provide insights into differences in patient characteristics and quality of care over time between men and women, we analyzed data from the China PEACE Retrospective AMI Study,17 which included a random nationally representative sample of patients with AMI from 63 urban and 99 rural hospitals across China in 2001, 2006, and 2011. We have previously shown women in the younger age group had higher in‐hospital mortality. In this study, our primary aim is to investigate sex differences in the presenting characteristics and quality of care of patients with ST‐segment elevation myocardial infarction (STEMI), whether these differences could be accounted for by age, and to examine temporal trends.
Methods
Study Design
The objectives, scope, and purpose of the China PEACE Retrospective AMI Study have been described previously.17 In brief, using 2‐stage random sampling, a nationally representative sample of patients admitted with AMI in 2001, 2006, and 2011 was obtained. We stratified the hospitals into 5 economic–geographical regions (eastern rural, central rural, western rural, eastern urban, and central–western urban) since hospital volumes and clinical capacities differ between urban and rural areas and between the 3 official economic–geographical regions (eastern, central, and western) of China. We used systematic random sampling procedures to select patients with AMI from the local hospital database of each sampled hospital in each study year. We used version 9 (410.xx) and version 10 (I21.xx; when available) ICD codes to screen for possible cases of AMI. These cases were then further confirmed by clinical record assessment. Detailed clinical data were then collected by data abstraction to identify those cases that represented initial AMI episodes according to the definition in the 2010 China National Guideline for STEMI.18 The central ethics committee at the National Center for Cardiovascular Diseases approved the study. All collaborating hospitals either accepted central ethics approval or obtained local approval by internal ethics committees. Because of the nature of the retrospective study, the requirement of informed consent was waived.
Study Sample
Only patients with a definite discharge diagnosis of STEMI (with or without prior cardiovascular disease) were eligible for inclusion in this study. The diagnosis of STEMI was determined by the combination of clinical discharge diagnosis terms and ECG results. The type of AMI was validated by review of ECG from randomly selected records by a cardiologist not involved in data abstraction, and there was a 94.7% concordance in the selected cases (Table S1). We excluded all patients whose STEMI occurred during the course of the hospitalization and those who were transferred in, transferred out, and were discharged alive in the first 24 hours of admission (Figure S1).
Data Collection and Measures
We collected data by central abstraction of medical charts with use of standardized data definitions, including patient characteristics (age, cardiovascular risk factors, clinical characteristics on presentation, and treatments) and hospital‐level characteristics (acuity level, teaching status, percutaneous coronary intervention [PCI] capability). We compared time from symptom onset to admission between men and women, which included both prehospital delay and time from arrival to admission. Admission was used to track the time of presentation because we lacked information about time to presentation at the hospital. We evaluated the use of treatments recommended by the 2010 National Guideline for STEMI,18 which are consistent with 2007 U.S. guidelines.19 Rates of utilization were assessed only in patients considered to be ideal for the treatment, defined as patients without accepted contraindications. Criteria identifying ideal candidates for guideline‐concordant therapies are detailed in Data S1. For the calculation of rates of diagnostic catheterization and PCI, we restricted our study group to patients admitted to facilities capable of performing PCI.
Statistical Analysis
To estimate nationally representative rates of hospitals admission in men and women for each study year, we applied weights proportional to the inverse sampling fraction of hospitals within each stratum and the sampling fraction of patients within each hospital, to account for differences in the sampling fraction for each period. Patient characteristics and treatments were compared between women and men, both overall and across the 3 study years (2001, 2006, and 2011). Categorical and continuous variables were summarized by percentages and medians (interquartile range), respectively, and compared using the χ2 tests and Student t tests, respectively. To examine trends across the different study periods for each sex, we used the Mann–Kendall test for continuous variables and the Cochran–Armitage test for categorical variables. We investigated the association between sex and the prevalence of cardiovascular risk factors, adjusted for age in logistic regression models. To examine the association between sex and treatment received, we also adjusted for age and other baseline characteristics as listed in Table 1 using multivariable logistic models. We included the 2‐way interaction term sex×year in the regression model to assess whether sex differences in presenting characteristics and treatment varied by study year. All statistical analyses were performed using SAS software (version 9.2, SAS Institute, Cary, NC).
Table 1.
Patient Characteristics According to Sex and Study Year
| Characteristic | Men, %a | P for Trends | Women, %a | P for Trends | ||||
|---|---|---|---|---|---|---|---|---|
| 2001 (n=1364) | 2006 (n=2541) | 2011 (n=4507) | 2001 (n=569) | 2006 (n=1040) | 2011 (n=1965) | |||
| Demographic | ||||||||
| Age, yb | 63 (53, 70) | 64 (54, 73) | 63 (53, 73) | 0.476 | 68 (62, 74) | 71 (65, 76) | 72 (64, 78) | <0.0001 |
| Cardiovascular risk factors | ||||||||
| Hypertension | 38.8 | 45.9 | 47.3 | <0.0001 | 47.8 | 53.4 | 60.6 | <0.0001 |
| Diabetes | 11 | 15.4 | 18.3 | <0.0001 | 21.1 | 25.8 | 26.9 | 0.010 |
| Current smoker | 38.7 | 41.3 | 48 | <0.0001 | 6 | 9 | 11.9 | <0.0001 |
| Medical history | ||||||||
| Coronary heart disease | 22.6 | 19.1 | 20.5 | 0.355 | 26.2 | 22.2 | 21.8 | 0.054 |
| Myocardial infarction | 10.3 | 9.7 | 11.6 | 0.058 | 9.5 | 8.8 | 9.3 | 0.970 |
| PCI | 0.4 | 0.9 | 2.7 | <0.0001 | 0.9 | 0.9 | 1.5 | 0.138 |
| Stroke | 9.2 | 10.3 | 11.5 | 0.010 | 10 | 11.7 | 13.9 | 0.070 |
| Symptom onset to admission, hour | ||||||||
| <6 | 42.2 | 40.9 | 41.3 | 0.467 | 30.9 | 34.1 | 36.9 | 0.003 |
| 6 to 12 hours | 8.9 | 9.6 | 10.5 | 0.027 | 10.7 | 12.5 | 11.3 | 0.921 |
| >12 hours | 48.9 | 49.5 | 48.1 | 0.430 | 58.3 | 53.4 | 51.7 | 0.008 |
| Clinical characteristics | ||||||||
| Chest discomfort | 93.1 | 93.2 | 93.4 | 0.652 | 91.2 | 89.7 | 89.3 | 0.219 |
| Cardiogenic shock | 3.4 | 5.5 | 6 | 0.0005 | 6.2 | 7.6 | 7.9 | 0.205 |
| Cardiac arrest | 0.9 | 1.3 | 1.5 | 0.078 | 0.7 | 0.8 | 1.1 | 0.335 |
| Acute stroke | 0.7 | 1.5 | 1 | 0.930 | 1.1 | 2.6 | 1.1 | 0.318 |
| Heart rate ≥100 bpmb | 15.7 | 14.8 | 11.6 | <0.0001 | 20.2 | 22.0 | 18.4 | 0.098 |
| SBP ≥140 mm Hgb | 31.3 | 31.4 | 32.6 | 0.256 | 37.3 | 39.3 | 39.7 | 0.326 |
| LDL‐C level | ||||||||
| <130 | 35.2 | 55.8 | 67.6 | <0.0001 | 25.8 | 50.1 | 59.3 | <0.0001 |
| ≥130 | 11.7 | 15.4 | 18.2 | <0.0001 | 12.8 | 18.5 | 22.4 | <0.0001 |
| Unrecorded | 53.2 | 28.7 | 14.2 | <0.0001 | 61.3 | 31.4 | 18.3 | <0.0001 |
| eGFR, mL/min per 1.73 m2 b | 75.5 (60.0, 94.6) | 77.9 (61.7, 97.9) | 88.1 (68.9, 109.8) | <0.0001 | 63.7 (49.1, 81.9) | 66.4 (48.2, 84.2) | 76.1 (55.7, 100.1) | <0.0001 |
| Hospital characteristics | ||||||||
| Teaching hospital | 85 | 80.6 | 80.1 | 0.0001 | 83.5 | 79.7 | 77.8 | 0.003 |
| PCI‐capable hospital | 32.8 | 55.1 | 72.9 | <0.0001 | 34.3 | 52.6 | 69 | <0.0001 |
| Hospital with CCU | 81.1 | 76.3 | 79.4 | 0.952 | 78.6 | 77.4 | 78.6 | 0.791 |
| Economic–geographic region | ||||||||
| Central | 19.5 | 21 | 23.2 | <0.0001 | 16.9 | 17.9 | 22 | <0.0001 |
| Eastern | 65.7 | 58.4 | 54.7 | <0.0001 | 71.5 | 63.3 | 59.3 | <0.0001 |
| Western | 14.8 | 20.6 | 22.1 | <0.0001 | 11.6 | 18.8 | 18.7 | <0.0001 |
| Urban/rural | ||||||||
| Urban | 63.9 | 60.6 | 63.4 | 0.586 | 64 | 60.9 | 57.9 | 0.006 |
| Rural | 36.1 | 39.4 | 36.6 | 36 | 39.1 | 42.1 | ||
CCU indicates cardiac care unit; eGFR, estimated glomerular filtration rate; LDL‐C, low‐density lipoprotein cholesterol; PCI, percutaneous coronary intervention; SBP, systolic blood pressure.
Unless otherwise indicated.
Continuous variables displayed as median values with interquartile range.
Results
Study Sample
We sampled 18 631 cases, from which 18 110 (97.2%) had available records. We excluded 6645 cases that did not meet inclusion criteria, resulting in a study sample of 11, 986 patients with STEMI (Figure S1). There were 1364, 2541, and 4507 men (representing 29 094, 65 370, and 120 991 male patients nationally in weighted estimates) and 569, 1040, and 1965 women (representing 12 134, 27 098, and 53 585 female patients nationally in weighted estimates) in 2001, 2006, and 2011, respectively. Hospital admissions for STEMI per 100 000 people increased 4.2‐fold in men (4.6 in 2001, 10.0 in 2006, and 18.0 in 2011) and 3.9‐fold in women (1.9 in 2001, 4.1 in 2006, and 8.0 in 2011).
Patients Characteristics
From 2001 to 2011, the median age of patients increased from 68 to 72 years in women (P trend<0.001) but remained stable in men (63 years in 2011) (P trend=0.48). The proportions of men and women aged ≥80 years old significantly increased over time (Figure 1). The prevalence of cardiovascular risk factors increased over time for both women and men. Women had a higher prevalence of hypertension, diabetes mellitus, and coronary heart disease in each time period (P<0.001 for all comparisons) (Table 1). Similar findings were also found in the age‐adjusted results (Figure 2). In addition, sex differences in the prevalence of hypertension increased from 2001 to 2011, with women having a higher prevalence. However, sex differences in the prevalence of diabetes remained stable. Although there was no significant sex difference in those with a low‐density lipoprotein cholesterol >130 mg/dL in 2001, this risk factor was more prevalent in women in later time periods (Figure 2). Women were hospitalized less often in tertiary care hospitals and hospitals with the capacity to perform PCI.
Figure 1.
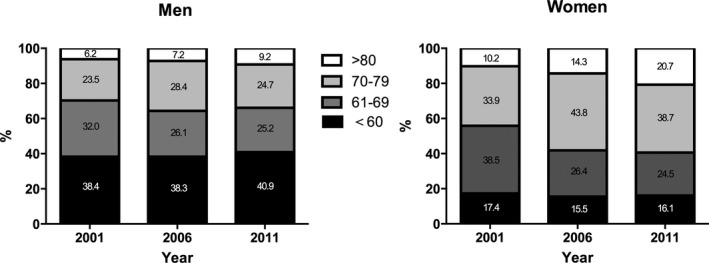
Age distribution of the study sample according to sex and year.
Figure 2.
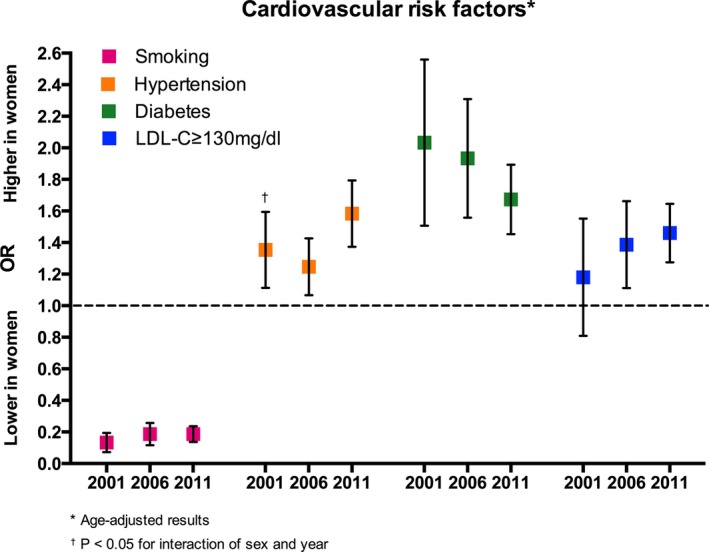
Temporal trends of age‐adjusted results in sex differences in cardiovascular risk factors. LDL‐C indicates low‐density lipoprotein cholesterol; OR, odds ratio.
Women were consistently were more likely to have systolic blood pressure over 140 mm Hg and heart rate over 100 bpm. Comparing 2001, 2006, and 2011, sex differences in heart rate >100 bpm increased, yet differences in the presence of systolic blood pressure measurements did not change. Although there were significant sex differences in the time interval of >12 hours between symptom onset and admission time in 2001, since 2006 delays in presentation were comparable between women and men (Figure 3). The age‐adjusted results showed that there was no sex difference in chest discomfort in 2001 and 2006, but not 2011.
Figure 3.
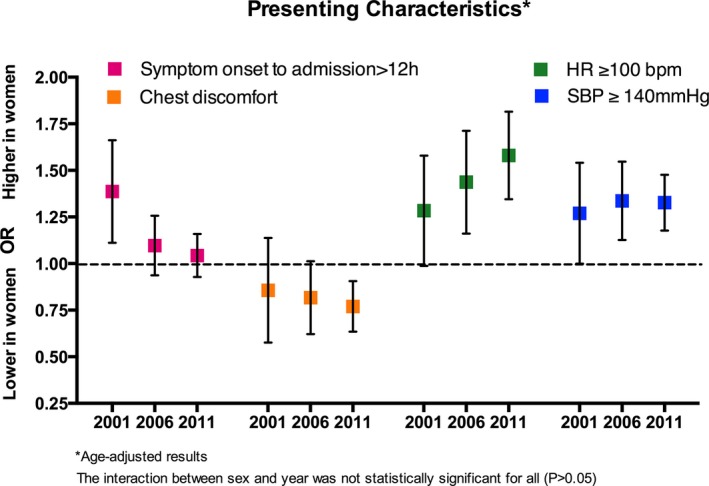
Temporal trends of age‐adjusted results in sex differences in presenting characteristics. HR indicates heart rate; OR, odds ratio; SBP, systolic blood pressure.
Treatment Among Ideal Candidates
The proportion of ideal patients for aspirin, clopidogrel, β‐blocker, angiotensin‐converting enzyme inhibitor/angiotensin II receptor blocker, and statin treatments remained unchanged over time in both sex groups (Table S2). Although the proportion of women ideal for reperfusion therapy increased significantly over the last decade (from 35.7% in 2001 to 43.0% in 2011, P trend=0.001), they remained less likely than men (48.2%) to be ideal patients for reperfusion therapy in 2011.
Overall, differences in treatment were consistently observed over the study period. The absolute differences between men and women receiving fibrinolytic therapy, primary PCI, or any reperfusion therapy were 6.7%, 5.5%, and 13.2% in 2011, respectively. In addition, any coronary angiography and nonprimary PCI were performed less commonly during initial AMI hospitalization in women in all time periods. Fewer women received aspirin or clopidogrel within 24 hours of admission (Table 2). After adjusting for age and other baseline characteristics, women without contraindications to treatment were significantly less likely to receive reperfusion therapy, coronary angiography, and nonprimary PCI in all time periods (Table S3). No significant sex differences were observed in the administration of other examined medications, including β‐blocker, angiotensin‐converting enzyme inhibitor/ angiotensin II receptor blocker, and statin. Between 2001 and 2011, sex differences in treatment persisted, and in some cases widened. In particular, sex differences in the utilization of primary PCI increased (Figure 4).
Table 2.
In‐Hospital Treatments Among Ideal Patients According to Sex and Year
| Characteristic | Overall, N (%) | P Value | Men, % | P for Trends | Women, % | P for Trends | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | 2001 | 2006 | 2011 | 2001 | 2006 | 2011 | ||||
| Acute medication | |||||||||||
| Aspirin ≤24 hoursa | 7023 (88.8) | 2765 (85.9) | <0.0001 | 81.1 | 87.7 | 91.8 | <0.0001 | 78.0 | 85.0 | 88.8 | <0.0001 |
| Clopidogrel ≤24 hoursa | 4454 (56.9) | 1679 (52.5) | <0.0001 | 1.4 | 44.3 | 80 | <0.0001 | 0.8 | 36.5 | 75.5 | <0.0001 |
| β‐Blockers ≤24 hoursa | 2371 (56.8) | 770 (52.6) | 0.005 | 47.8 | 62.7 | 56.1 | 0.095 | 46.4 | 54.8 | 53.1 | 0.202 |
| ACE‐inhibitor/ARBa , b | 5073 (65.8) | 1994 (63.8) | 0.044 | 60.8 | 69.6 | 65.2 | 0.214 | 59.2 | 66.7 | 63.6 | 0.332 |
| Statina , b | 6180 (76.5) | 2476 (75.1) | 0.117 | 30.3 | 75.0 | 91.5 | <0.0001 | 27.8 | 72.6 | 90.4 | <0.0001 |
| Reperfusion therapyb | |||||||||||
| With reperfusion | 2289 (57.5) | 646 (44.2) | <0.0001 | 56.3 | 58.0 | 57.6 | 0.702 | 47.3 | 42.2 | 44.4 | 0.758 |
| Primary PCI | 757 (19.0) | 203 (13.9) | <0.0001 | 8.7 | 15.1 | 24.2 | <0.0001 | 8.4 | 8.9 | 17.7 | <0.0001 |
| Fibrinolytic therapy | 1535 (38.6) | 443 (30.3) | <0.0001 | 47.7 | 43.0 | 33.5 | <0.0001 | 38.9 | 33.3 | 26.8 | 0.0002 |
| Procedurec | |||||||||||
| Nonprimary PCI | 1117 (21.8) | 299 (14.3) | <0.0001 | 9.6 | 19.4 | 24.4 | <0.0001 | 5.6 | 10.2 | 17.1 | <0.0001 |
| Cardiac catheterization | 2414 (47.0) | 669 (31.9) | <0.0001 | 34.2 | 41.7 | 51.1 | <0.0001 | 26.2 | 25.0 | 35.5 | <0.0001 |
ACE, angiotensin‐converting enzyme; ARB, angiotensin II receptor blocker; PCI, percutaneous coronary intervention.
Only among patients without contraindications for the treatment.
During hospitalization.
Only among patients admitted into a hospital capable of PCI.
Figure 4.
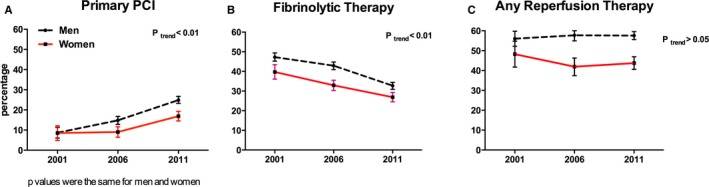
Temporal trends of sex differences in reperfusion therapy among ideal candidates. A, Primary PCI. B, Fibrinolytic therapy. C, Any reperfusion. PCI indicates percutaneous coronary intervention.
Discussion
In this large, national study in China of hospitalization for STEMI, we found marked sex differences in clinical profiles and quality of care. Women, who experienced a slightly higher increase (4.2‐fold versus 3.9‐fold) in STEMI over the study period, were older, had greater comorbidities, and were less likely to be ideal patients for many evidence‐based therapies. Among ideal patients, women were significantly less likely to receive a revascularization strategy (including fibrinolysis or cardiac catheterization with or without PCI), even after accounting for differences in clinical profiles. These sex‐based differences in patient characteristics and hospital care did not change significantly over the past decade, underscoring the need to specifically address these findings with quality improvement efforts.
We had previously shown in the China PEACE study that the risk of mortality was age dependent and most pronounced among younger women (<70 years of age) with STEMI, even after accounting for differences in clinical presentation and treatments.3 However, we had not investigated temporal trends in sex differences as they relate to patient characteristics and receipt of evidence‐based therapies in STEMI. We found that even after adjusting for age, with the exception of smoking, a predominantly male activity in China,20 risk factors including greater age, diabetes, hypertension, and dyslipidemia were more common in women presenting with STEMI. These are consistent with prior national and international studies.21, 22
The clinical presentation of women differed from men. Indeed, half of the women in our study presented outside the time window for reperfusion therapy, which is consistent over the last decade. However, we did observe a decrease in the delay to admission among women, and sex differences in the time interval of >12 hours between symptom onset and admission time disappeared since 2006, which might partly be due to improved healthcare accessibility for women in China.23
While the quality of care improved for both men and women, significant sex gaps exist and have not improved over time. Significantly fewer women received a reperfusion strategy, even when they presented promptly for treatment. Additionally, among patients deemed to be ideal candidates, women were less likely than men to receive aspirin and clopidogrel. Sex differences in treatment response have not been supported by the literature; rather, prior studies indicate that both women and men derive similar reductions in morbidity and mortality with the prescriptions of aspirin, clopidogrel, and with invasive cardiac procedures,4 and guidelines do not recommend differential use of these therapies based upon sex. The disparities in care identified in this study require full‐scale investigation into clinical decision‐making and targeted efforts to diminish such disparities.
The rising burden of modifiable cardiovascular risk factors among women will require local and national efforts to advance primary and secondary prevention strategies; such efforts may need to directly target women at high risk of heart attack. The marked underutilization of coronary catheterization and reperfusion therapy should prompt quality improvement efforts to ensure that the evidence‐based management of STEMI is rigorously applied in patients of both sexes.24 In the interim, large‐scale educational initiatives targeting women should be implemented in both pre‐hospital and in‐hospital settings to increase women's and their health providers’ awareness of cardiovascular disease and recognition of symptoms of AMI,25which has been proven to be effective in the Go Red for Women campaign, which was initiated in the United States.25 Ultimately, dispelling myths (or old assumptions) and improving awareness is difficult and will require innovative, multipronged efforts.
Limitations
The results of our study should be interpreted with consideration of several limitations. First, residual confounding of measured or unmeasured variables might affect the observed results. However, we accounted for traditional clinical factors common among risk models predicting early mortality. Second, given that relatively few patients underwent a cardiac catheterization, we were not able to adjust our analysis to account for the severity and extent of coronary artery diseases that might contribute to the sex differences in mortality.26 However, these data are not typically included in risk‐adjusted models, and it is not clear that anatomy would affect in‐hospital mortality differently in men and women.
Conclusions
In a large, nationally representative observational study in China, women hospitalized with STEMI were older, had greater delays in care seeking, more comorbidities, and worse disease severity than men. Moreover, women were less likely to be candidates for, and less likely to receive, evidence‐based therapies as compared with men. These disparities have changed little over the past decade despite large‐scale efforts to increase access and quality. These findings underscore the need for improved systems to ensure the prompt diagnosis and use of evidence‐based treatments for women with STEMI, particularly with respect to reperfusion therapies.
Sources of Funding
This project was partly supported by the Research Special Fund for Public Welfare Industry of Health (201202025) from National Health and Family Planning Commission of China, and the National Key Technology R&D Program (2013BAI09B01) from the Ministry of Science and Technology of China. Xue Du is funded by China Scholarship Council (2014). Dr Krumholz is supported by grant U01 HL105270‐03 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute. The sponsors had no role in the conduct of the study; in the collection, management, analysis, and interpretation of the data; or in the preparation or approval of the manuscript.
Disclosures
Dr Krumholz reports being the recipient of research grants from Medtronic and Johnson & Johnson, through Yale University, to develop methods of clinical trial data sharing. Dr Krumholz reports that he is the chair of a cardiac scientific advisory board for United Health. Dr Masoudi receives salary support from the American College of Cardiology for his role as the Senior Medical Officer of the National Cardiovascular Data Registries. The authors declare no other relevant conflicts of interest.
Supporting information
Appendix S1. China PEACE‐Retrospective AMI Study Site Investigators by Hospital China PEACE Study Consultants
Table S1. Validation of Acute Myocardial Infarction (AMI) Type (ST‐Segment Elevation Myocardial Infarction or Non ST‐Segment Elevation Myocardial Infarction)
Figure S1. Study cohort.
Data S1. Definitions for ideal candidates for the treatments.
Table S2. Proportions of Patients Ideal for Treatments by Sex and Year
Table S3. Age and Fully Adjusted Odds Ratios (Women Compared With Men) of Treatments During Hospitalization
Acknowledgments
We appreciate the multiple contributions made by study teams at the China Oxford Centre for International Health Research and the Yale‐New Haven Hospital Center for Outcomes Research and Evaluation in the realms of study design and operations, particularly the data collection by Yi Pi, Jiamin Liu, Wuhanbilige Hundei, Haibo Zhang, Lijuan Zhan, Lihua Zhang, and Wenchi Guan. We appreciate the advice by Yongfei Wang, Zhenqiu Lin, Shuxia Li, and Haiqun Lin.
(J Am Heart Assoc. 2016;5:e002157 doi: 10.1161/JAHA.115.002157)
Accompanying Appendix S1, which lists the members of the China PEACE‐Retrospective AMI Study Site Investigators by Hospital and China PEACE Study Consultants, Tables S1 through S3, Figure S1, and Data S1 are available at http://jaha.ahajournals.org/content/5/2/e003012/suppl/DC1
References
- 1. Yang G, Wang Y, Zeng Y, Gao GF, Liang X, Zhou M, Wan X, Yu S, Jiang Y, Naghavi M, Vos T, Wang H, Lopez AD, Murray CJ. Rapid health transition in China, 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet. 2013;381:1987–2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yusuf S, Rangarajan S, Teo K, Islam S, Li W, Liu L, Bo J, Lou Q, Lu F, Liu T, Yu L, Zhang S, Mony P, Swaminathan S, Mohan V, Gupta R, Kumar R, Vijayakumar K, Lear S, Anand S, Wielgosz A, Diaz R, Avezum A, Lopez‐Jaramillo P, Lanas F, Yusoff K, Ismail N, Iqbal R, Rahman O, Rosengren A, Yusufali A, Kelishadi R, Kruger A, Puoane T, Szuba A, Chifamba J, Oguz A, McQueen M, McKee M, Dagenais G; Investigators P . Cardiovascular risk and events in 17 low‐, middle‐, and high‐income countries. N Engl J Med. 2014;371:818–827. [DOI] [PubMed] [Google Scholar]
- 3. Zheng X, Dreyer RP, Hu S, Spatz ES, Masoudi FA, Spertus JA, Nasir K, Li X, Li J, Wang S, Krumholz HM, Jiang L; for the China PCG . Age‐specific gender differences in early mortality following ST‐segment elevation myocardial infarction in China. Heart. 2015;101:349–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gan SC, Beaver SK, Houck PM, MacLehose RF, Lawson HW, Chan L. Treatment of acute myocardial infarction and 30‐day mortality among women and men. N Engl J Med. 2000;343:8–15. [DOI] [PubMed] [Google Scholar]
- 5. Vaccarino V, Parsons L, Peterson ED, Rogers WJ, Kiefe CI, Canto J. Sex differences in mortality after acute myocardial infarction: changes from 1994 to 2006. Arch Intern Med. 2009;169:1767–1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gupta A, Wang Y, Spertus JA, Geda M, Lorenze N, Nkonde‐Price C, D'Onofrio G, Lichtman JH, Krumholz HM. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol. 2014;64:337–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. The Go Red for Women Campaign. Available at: http://www.goredforwomen.org. Accessed February 10, 2016.
- 8. Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, Lloyd‐Jones DM, Newby LK, Pina IL, Roger VL, Shaw LJ, Zhao D, Beckie TM, Bushnell C, D'Armiento J, Kris‐Etherton PM, Fang J, Ganiats TG, Gomes AS, Gracia CR, Haan CK, Jackson EA, Judelson DR, Kelepouris E, Lavie CJ, Moore A, Nussmeier NA, Ofili E, Oparil S, Ouyang P, Pinn VW, Sherif K, Smith SC Jr, Sopko G, Chandra‐Strobos N, Urbina EM, Vaccarino V, Wenger NK. Effectiveness‐based guidelines for the prevention of cardiovascular disease in women–2011 update: a guideline from the American Heart Association. Circulation. 2011;123:1243–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mosca L, Banka CL, Benjamin EJ, Berra K, Bushnell C, Dolor RJ, Ganiats TG, Gomes AS, Gornik HL, Gracia C, Gulati M, Haan CK, Judelson DR, Keenan N, Kelepouris E, Michos ED, Newby LK, Oparil S, Ouyang P, Oz MC, Petitti D, Pinn VW, Redberg RF, Scott R, Sherif K, Smith SC Jr, Sopko G, Steinhorn RH, Stone NJ, Taubert KA, Todd BA, Urbina E, Wenger NK; Expert Panel/Writing G, American Heart A, American Academy of Family P, American College of O, Gynecologists, American College of Cardiology F, Society of Thoracic S, American Medical Women's A, Centers for Disease C, Prevention, Office of Research on Women's H, Association of Black C, American College of P, World Heart F, National Heart L, Blood I and American College of Nurse P . Evidence‐based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation. 2007;115:1481–1501.17309915 [Google Scholar]
- 10. Mosca L, Appel LJ, Benjamin EJ, Berra K, Chandra‐Strobos N, Fabunmi RP, Grady D, Haan CK, Hayes SN, Judelson DR, Keenan NL, McBride P, Oparil S, Ouyang P, Oz MC, Mendelsohn ME, Pasternak RC, Pinn VW, Robertson RM, Schenck‐Gustafsson K, Sila CA, Smith SC Jr, Sopko G, Taylor AL, Walsh BW, Wenger NK, Williams CL; American Heart A . Evidence‐based guidelines for cardiovascular disease prevention in women. Circulation. 2004;109:672–693. [DOI] [PubMed] [Google Scholar]
- 11. Radovanovic D, Nallamothu BK, Seifert B, Bertel O, Eberli F, Urban P, Pedrazzini G, Rickli H, Stauffer JC, Windecker S, Erne P; Investigators AP . Temporal trends in treatment of ST‐elevation myocardial infarction among men and women in Switzerland between 1997 and 2011. Eur Heart J Acute Cardiovasc Care. 2012;1:183–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chen Y, Jiang L, Smith M, Pan H, Collins R, Peto R, Chen Z; Group ftCC‐c . Sex differences in hospital mortality following acute myocardial infarction in China: findings from a study of 45 852 patients in the COMMIT/CCS‐2 study. Heart Asia. 2011;3:104–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhang B, Zhang W, Huang RC, Zhang Y, Liu J, Zheng ZG, Jiang DM, Sun YJ, Ren LN, Zhou XC, Qi GX. Gender disparity in early death after ST‐elevation myocardial infarction. Chin Med J (Engl). 2013;126:3481–3485. [PubMed] [Google Scholar]
- 14. Song XT, Chen YD, Pan WQ, Lu SZ. Gender based differences in patients with acute coronary syndrome: findings from Chinese Registry of Acute Coronary Events (CRACE). Chin Med J (Engl). 2007;120:1063–1067. [PubMed] [Google Scholar]
- 15. Nauta ST, Deckers JW, van Domburg RT, Akkerhuis KM. Sex‐related trends in mortality in hospitalized men and women after myocardial infarction between 1985 and 2008: equal benefit for women and men. Circulation. 2012;126:2184–2189. [DOI] [PubMed] [Google Scholar]
- 16. Hu S, Tang S, Liu Y, Zhao Y, Escobar ML, de Ferranti D. Reform of how health care is paid for in China: challenges and opportunities. Lancet. 2008;372:1846–1853. [DOI] [PubMed] [Google Scholar]
- 17. Dharmarajan K, Li J, Li X, Lin Z, Krumholz HM, Jiang L. The China Patient‐Centered Evaluative Assessment of Cardiac Events (China PEACE) retrospective study of acute myocardial infarction: study design. Circ Cardiovasc Qual Outcomes. 2013;6:732–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. China Society of Cardiology of Chinese Medical Association Editorial Board of Chinese Journal of Cardiology . Guideline for diagnosis and treatment of patients with ST‐elevation myocardial infarction. Zhonghua Xin Xue Guan Bing Za Zhi. 2010;38:675–690. [PubMed] [Google Scholar]
- 19. Antman EM, Hand M, Armstrong PW, Bates ER, Green LA, Halasyamani LK, Hochman JS, Krumholz HM, Lamas GA, Mullany CJ, Pearle DL, Sloan MA, Smith SC Jr, Anbe DT, Kushner FG, Ornato JP, Jacobs AK, Adams CD, Anderson JL, Buller CE, Creager MA, Ettinger SM, Halperin JL, Hunt SA, Lytle BW, Nishimura R, Page RL, Riegel B, Tarkington LG, Yancy CW. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST‐Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee. Circulation. 2008;117:296–329. [DOI] [PubMed] [Google Scholar]
- 20. Liu L. Cardiovascular diseases in China. Biochem Cell Biol. 2007;85:157–163. [DOI] [PubMed] [Google Scholar]
- 21. Berger JS, Elliott L, Gallup D, Roe M, Granger CB, Armstrong PW, Simes RJ, White HD, Van de Werf F, Topol EJ, Hochman JS, Newby LK, Harrington RA, Califf RM, Becker RC, Douglas PS. Sex differences in mortality following acute coronary syndromes. JAMA. 2009;302:874–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Heer T, Gitt AK, Juenger C, Schiele R, Wienbergen H, Towae F, Gottwitz M, Zahn R, Zeymer U, Senges J. Gender differences in acute non‐ST‐segment elevation myocardial infarction. Am J Cardiol. 2006;98:160–166. [DOI] [PubMed] [Google Scholar]
- 23. Tang S, Meng Q, Chen L, Bekedam H, Evans T, Whitehead M. Tackling the challenges to health equity in China. Lancet. 2008;372:1493–1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Canto JG, Rogers WJ, Goldberg RJ, Peterson ED, Wenger NK, Vaccarino V, Kiefe CI, Frederick PD, Sopko G, Zheng ZJ. Association of age and sex with myocardial infarction symptom presentation and in‐hospital mortality. JAMA. 2012;307:813–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mosca L, Mochari H, Christian A, Berra K, Taubert K, Mills T, Burdick KA, Simpson SL. National study of women's awareness, preventive action, and barriers to cardiovascular health. Circulation. 2006;113:525–534. [DOI] [PubMed] [Google Scholar]
- 26. Duvernoy CS, Smith DE, Manohar P, Schaefer A, Kline‐Rogers E, Share D, McNamara R, Gurm HS, Moscucci M. Gender differences in adverse outcomes after contemporary percutaneous coronary intervention: an analysis from the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2) percutaneous coronary intervention registry. Am Heart J. 2010;159:677–683.e1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. China PEACE‐Retrospective AMI Study Site Investigators by Hospital China PEACE Study Consultants
Table S1. Validation of Acute Myocardial Infarction (AMI) Type (ST‐Segment Elevation Myocardial Infarction or Non ST‐Segment Elevation Myocardial Infarction)
Figure S1. Study cohort.
Data S1. Definitions for ideal candidates for the treatments.
Table S2. Proportions of Patients Ideal for Treatments by Sex and Year
Table S3. Age and Fully Adjusted Odds Ratios (Women Compared With Men) of Treatments During Hospitalization


