Abstract
Background
Driving time to a percutaneous coronary intervention (PCI)–capable hospital is important in timely treatment of acute myocardial infarction (AMI). Our objective was to determine whether driving time from one's residence to a PCI‐capable hospital contributes to AMI deaths. We conducted a cross‐sectional study of age‐ and sex‐adjusted mortality in census block groups to evaluate this question.
Methods and Results
We studied all (14 027) AMI deaths that occurred during 2008–2012 in Arkansas to assess the relationship between driving time from the population center of a block group (neighborhood) to the nearest PCI‐capable hospital. We estimated standardized mortality ratios in block groups that were adjusted for education (population over 25 years of age who did not graduate from high school), poverty (population living below federal poverty level), population density (population per square mile), mobility (population residing at the same address as 1 year ago), black (population that is black), rurality (rural households), geodesic distance, and driving time. The median geodesic distance and driving time were 12.8 miles (interquartile range 3.6–30.1) and 28.3 minutes (interquartile range 9.6–58.7), respectively. Risks in neighborhoods with long driving times (90th percentile) were 26% greater than risks in neighborhoods with short driving times (10th percentile), even after adjusting for education, poverty, population density, rurality, and black race (P<0.0001).
Conclusions
AMI mortality increases with increasing driving time to the nearest PCI‐capable hospital. Improving the healthcare system by reducing time to arrive at a PCI‐capable hospital could reduce AMI deaths.
Keywords: census block groups, driving time, health services, mortality/survival, myocardial infarction, percutaneous coronary intervention, risk factors
Subject Categories: Myocardial Infarction, Risk Factors, Mortality/Survival
Introduction
Acute myocardial infarction (AMI) is a leading cause of morbidity and mortality.1 In 2012, ≈118 000 deaths were reported due to AMI in the United States (http://wonder.cdc.gov/ucd-icd10.html). Primary percutaneous coronary intervention (PCI) is the preferred treatment for patients with an ST‐elevation myocardial infarction (STEMI),2, 3 a type of AMI that has high morbidity and mortality.1 Timely response and early PCI during the “golden hour” (60 minutes) has been shown to decrease morbidity and mortality associated with AMI.4, 5, 6 Driving time to a PCI‐capable hospital is an important factor in the timely response to this life‐saving intervention.5, 7 A study by Nallamothu and colleagues found that nearly 80% of the US population lived within 60 minutes to a PCI‐capable hospital with a median driving time of 11.3 minutes.8 However, there was a wide variation within the regions of the United States, with 7.6 minutes in the US Pacific region to 21.4 minutes in the US East South Central region.8 Similar geographical variation was observed in Canadian provinces as well.9 Studies have shown that the number of deaths from AMI increases by 6.5% for an increase in every mile from a PCI hospital, and driving time to the hospital is an important predictor of AMI mortality.10, 11 While these studies have looked at the driving time and distance from a patient's residence to a PCI‐capable hospital and its implications,8, 9, 10, 11 none of them evaluated driving time to a PCI‐capable hospital as a predictor of mortality in patients with AMI at a census block group (neighborhood) level.
We designed this study to examine the relationship of mortality from AMI with different measures, especially the driving time to the nearest PCI‐capable hospital. We hypothesize that increasing driving time to PCI‐capable hospitals is associated with higher AMI deaths. This relationship was assessed at the smallest geographical unit possible—census block groups (BGs). The results of this study are particularly relevant to rural communities that face additional challenges due to limited access to healthcare facilities.12
Methods
Death certificates from 2008 to 2012 for the state of Arkansas that coded AMI as an underlying cause of death with International Classification of Diseases, Tenth Revision codes I21 and I22 were obtained. Data on age and sex were obtained directly from death certificates. The residential address of each case was assigned a latitude and longitude using several geocoding procedures at the Arkansas Department of Health. The Science Advisory Committee of the Arkansas Department of Health, which serves as the Institutional Review Committee for the agency, approved the data use and the project. Only de‐identified data were obtained for analysis and reporting; hence, the need for informed consent was waived by the Science Advisory Committee.
AMI Deaths Assigned to BGs
Census BGs were used as proxies for neighborhoods, which are the units of analysis. AMI deaths were tabulated by age, sex, and the BG (neighborhood) where the deceased resided. Most addresses (93.1%) geocode directly to the latitude and longitude of a residence. The remaining addresses (6.9%) did not resolve to a residence (eg, post office box). These cases were presumed to reside in the Zip Code Tabulation Area (ZCTA) associated with the Zip Code on the death certificate, and they were apportioned to the BGs comprising the ZCTA.
ZCTAs usually overlap several BGs, and we included any BG that was at least partially within the ZCTA boundary. This criterion generated a list of eligible BGs from a ZIP Code. The American Community Survey estimated the number of persons of the same 5‐year age range and sex as the deceased in each of the eligible BGs. We apportioned the deceased to each eligible BG based on these population estimates; a portion of the case was assigned to each BG corresponding to the proportion of the “eligible” population in the BG. For example, suppose there were 2 BGs in the ZCTA, one containing 40 people of the appropriate age–sex and the other containing 60 people. The algorithm assigned 40/100 of the case to the first BG and 60/100 of the case to the second BG.
Latitude and longitude were assigned to a BG or ZCTA using functions in MATLAB's Mapping Toolbox (The Mathworks, Inc, Natick, MA), which locate points (residence of the deceased) within BG boundaries defined in shapefiles of 2010 census BGs (TIGER: www.census.gov). We also used MATLAB's Mapping Toolbox to generate maps.
Driving Time to the PCI‐Capable Hospital
We used the Network Analyst extension of ESRI ArcGIS 10.0 (ESRI Inc, Redlands, CA) to calculate the driving time by ground from Arkansas BGs to the nearest PCI‐capable hospitals in Arkansas and in bordering states (Louisiana, Mississippi, Missouri, Oklahoma, Tennessee, and Texas). We used a nationwide network data set (StreetMap North America) that holds detailed information regarding road network features such as speed limits and direction of travel along each road segment. An origin–destination cost matrix was generated with the population center of a BG as origin and PCI‐capable hospitals as destination. This BG‐specific covariate is referred to as “driving time.”
BG Covariates
BG‐level tabulations of surveys conducted by the American Community Survey were downloaded for the period 2008–2012. The following variables were selected for our analysis: number of persons by 5‐year age and sex categories, number of persons living in a household where the previous year's income was below the federal poverty level, number of persons over 25 years of age who did not complete high school, number of persons who were black, number of rural households in a BG, and number of persons living in the same residence as 1 year ago. The land area of the BG was obtained from the 2010 US Census summary file and the population density of the BG was computed.
The population counts were transformed before use as a covariate. The count in a BG, (rb), was converted to a proportion of the BG population, rb/nb. Shrinkage is a statistical procedure used to moderate extreme observed proportions (ie, when none [rb/nb=0] or all [rb/nb=1] observations have the attribute). It also adjusts for attenuation in relative risk estimates expected from measurement errors in the observed BG covariates. The median value of rb/nb over BG, m, was used to construct a shrinkage estimate of the proportion, pb=(rb+5 m)/(nb+5). The shrinkage estimate was probit‐transformed to create a BG‐level covariate that was used in analyses (ie, xb=probit[pb]). The covariates x_edu (did not graduate HS), x_pov (living below poverty level), x_home (same residence for past year), and x_black (black proportion) were computed this way. The covariate, x_den, was the logarithm (base 10) of the population density (persons per square mile).
We also determined the geodesic distance (miles) from the population center of the BG to the nearest PCI‐capable hospital (covariate: distance). PCI‐capable hospitals in or bordering Arkansas were obtained from the American Heart Association website (http://maps.heart.org/ml/#;) and the latitude–longitude of each was geocoded. Population center (downloaded from the US Census Bureau: http://www.census.gov/geo/reference/centersofpop.html) of a BG was used as a proxy for an individual's neighborhood of residence.
Statistical Analysis
Age‐ and sex‐specific AMI mortality rates were estimated in Arkansas’ BGs. Standardized mortality ratios, represented as where the subscript denotes BG‐specific values, were smoothed by regressing against BG covariates, xb. Expected cases, eb, were computed by applying age‐ and sex‐specific mortality rates from Arkansas (Figure 1) to the corresponding BG populations. We fit generalized additive Poisson regression models13 of the form, where ob denotes observed deaths and lneb is entered as an offset. A scatterplot smooth, S(xb), was fit using R software, mgvc‐package (mixed generalized additive model computation vehicle).14 The regression adjusts the expected number of cases in the BG, , and the ratio relative to eb provides an estimate of the relative risk . A significant smooth, S(xb), implies heterogeneity in AMI mortality rates among BGs that is associated with the covariate.
Figure 1.
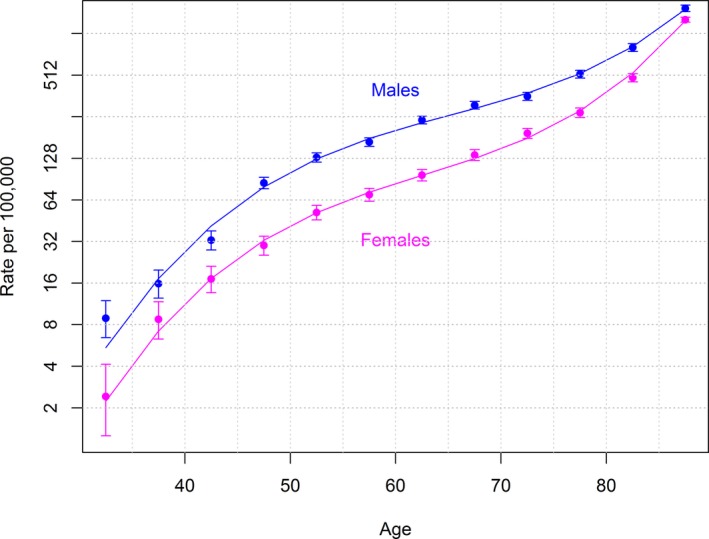
Age‐ and sex‐specific acute myocardial infarction mortality rates during 2008–2012 in the combined non‐Hispanic white and non‐Hispanic black populations of Arkansas.
The estimated relative risk derived from regressions on BG covariates show spatial variation because of the spatial distribution of the BG covariates. However, because of effects from risk factors that are not in the regression model, these covariates may not adequately reflect the underlying variation in AMI mortality rates. Geographically weighted regression15 was used to further adjust relative risk estimates in BGs for such unexplained geospatial variation in AMI mortality rates.
We conducted 2 sensitivity analyses. We used the centroid of a census BG to calculate the distance to the nearest PCI hospital instead of the population center. We also calculated the maximum distance of an individual living within a BG to the population center.
Results
From 2008 to 2012, there were 14 079 AMI deaths in Arkansas. Of these deaths, 11 726 (83.3%) were white, 1817 (12.9%) were black, and the remaining (3.8%) were races other than white or black, or the race was unknown. Over 99% were non‐Hispanic. Figure 1 shows the age‐ and sex‐specific mortality rates for AMI mortality in the combined non‐Hispanic white and non‐Hispanic black population. These rates were the reference rates for computing relative risks in BGs. Figure 2A maps estimates of BG relative risks after covariate adjustments for education, poverty, population density, rurality, black race, and geospatial variation (geographically weighted regression). It shows BG‐specific relative risk estimates of AMI mortality in Arkansas for the years 2008 through 2012. The 2147 BGs were divided into 6 relative risk categories with cut points at the 10th, 25th, 50th, 75th, and 90th percentiles. There were greater than 3‐fold differences in relative risk of AMI mortality across the state, even among adjacent BGs. Most of the BGs with the high relative risk were located in the eastern part of the state in the Mississippi Delta region.
Figure 2.
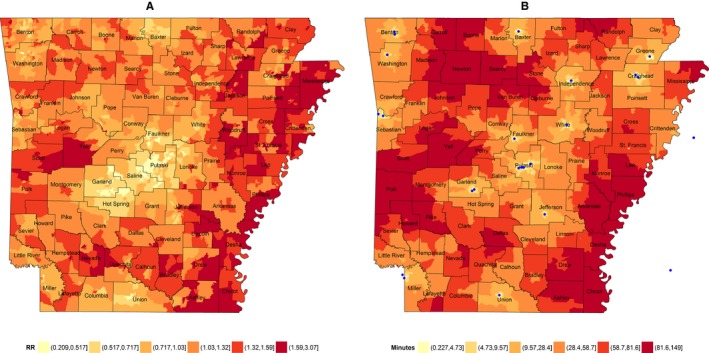
A, Block group (BG)–specific estimates of the relative risk for acute myocardial infarction mortality among Arkansans, ages 30+, during 2008–2012. (B) Driving time from population center of BG to the nearest percutaneous coronary intervention–capable hospital (blue dots). Estimates (RR) are based on trends in the standardized mortality ratio with BG measures of education, poverty, population density, percent rural, black race, and geographical location (spatial trends). The 10th, 25th, 50th, 75th, and 90th percentiles among BGs determine the boundaries of color interval.
The median geodesic distance (shortest path) and driving time from the population center of a BG (neighborhood) to the nearest PCI‐capable hospital were 12.8 miles (interquartile range [IQR] 3.6–30.1) and 28.3 minutes (IQR 9.6–58.7), respectively. Figure 2B shows the location of 26 PCI‐capable hospitals (blue dots) and BGs with population centers within specified driving times. Driving times for the 10th, 25th, 50th, 75th, and 90th percentiles were 4.7, 9.6, 28.3, 58.7, and 81.6 minutes, respectively. In 509 BGs, driving time to the nearest PCI‐capable hospital exceeds 60 minutes. Twenty‐one percent of the state's population 35 years of age and older reside in these BGs (over 362 000 people). Of note, the neighborhoods (BGs) that have the longest driving time to a nearest PCI‐capable hospital (90th percentile colored dark red in Figure 2B) correspond with areas having higher relative risk of AMI mortality (90th percentile colored dark red in Figure 2A). These neighborhoods in the western part of the state are mountainous (Ozark and Ouachita mountains), and those in the eastern part of the state are bisected by 4 large rivers (Arkansas, Mississippi, White River, and St. Francis). These natural barriers contribute to long driving times.
Table shows regression estimates and 95% CIs for the relative risk at selected percentiles (10th, 25th, 50th, 75th, and 90th) of the BG covariates: poverty, education, population density, rurality, black race, mobility, geodesic distance, and the driving time to the nearest PCI‐capable hospital. Each univariate model estimated a significant trend in AMI mortality relative to Arkansas age‐ and sex‐specific mortality rates. AMI mortality rates increase with increasing proportions for those who did not graduate from high school (education), who are living below poverty level (poverty), BGs with higher proportion of rural households, who are black, as well as with distance and driving time from a PCI‐capable hospital. AMI mortality rates decrease with increasing population density and proportion living in the same residence as the previous year (mobility). Education is the strongest predictor (explained deviance of 13.5%), with AMI mortality increasing more than 2‐fold (from 0.7 to 1.3) when the relative risk in 10% of BG with the highest percent not completing high school is compared to the relative risk in the lowest 10% of BG. Increasing mortality trends were also associated with distance (explained deviance of 11.2%) and driving time (explained deviance of 9.9%). Mortality trends with distance or driving time from the population center to the nearest PCI‐capable hospital were comparable to trends with the socioeconomic covariates, education and poverty, and substantially stronger than trends with urbanization (population density) and black race.
Table 1.
Regression Estimates of the Relative Risk (RR) of Acute Myocardial Infarction (AMI) Mortality in Arkansas at Ages 30+, 2008–2012, at Selected Percentiles of Block Group (BG) Covariates
| Covariate/Regression Model | RR at Covariate Percentilea 10th, 25th, 50th, 75th, 90th | Percent Explained Deviance | P Value |
|---|---|---|---|
| Univariateb | |||
| Education | 0.66, 0.86, 1.07, 1.22, 1.31 | 13.5 | <0.0001 |
| LCB | 0.62, 0.83, 1.03, 1.18, 1.26 | ||
| UCB | 0.71, 0.90, 1.10, 1.27, 1.38 | ||
| Poverty | 0.75, 0.88, 1.02, 1.19, 1.33 | 9.0 | <0.0001 |
| LCB | 0.71, 0.84, 0.98, 1.14, 1.26 | ||
| UCB | 0.80, 0.91, 1.05, 1.24, 1.40 | ||
| Population density | 1.21, 1.12, 0.97, 0.86, 0.82 | 4.0 | <0.0001 |
| LCB | 1.16, 1.08, 0.95, 0.83, 0.78 | ||
| UCB | 1.27, 1.16, 1.00, 0.90, 0.87 | ||
| Rurality | 0.88, 0.88, 1.12, 1.10, 1.10 | 2.2 | <0.0001 |
| LCB | 0.84, 0.84, 1.04, 1.05, 1.05 | ||
| UCB | 0.93, 0.93, 1.22, 1.15, 1.15 | ||
| Black | 0.98, 0.95, 0.95, 1.04, 1.17 | 1.9 | <0.0001 |
| LCB | 0.93, 0.91, 0.91, 0.99, 1.10 | ||
| UCB | 1.04, 0.99, 0.99, 1.09, 1.25 | ||
| Mobility | 1.07, 1.02, 0.99, 0.97, 0.97 | 0.5 | 0.0097 |
| LCB | 1.02, 0.98, 0.95, 0.94, 0.92 | ||
| UCB | 1.13, 1.06, 1.02, 1.01, 1.02 | ||
| Distance | 0.75, 0.78, 0.93, 1.21, 1.35 | 11.2 | <0.0001 |
| LCB | 0.71, 0.74, 0.89, 1.16, 1.28 | ||
| UCB | 0.79, 0.81, 0.97, 1.26, 1.42 | ||
| Driving time | 0.75, 0.79, 0.94, 1.19, 1.33 | 9.9 | <0.0001 |
| LCB | 0.71, 0.75, 0.91, 1.15, 1.26 | ||
| UCB | 0.79, 0.82, 0.98, 1.25, 1.40 | ||
| Multivariatec | |||
| Education | |||
| Poverty | 0.90, 0.95, 1.00, 1.06, 1.11 | 15.4 | <0.0001 |
| LCB | 0.86, 0.92, 0.97, 1.03, 1.06 | ||
| UCB | 0.94, 0.98, 1.03, 1.10, 1.17 | ||
| Population density | 1.10. 1.04, 1.03, 0.92. 0.84 | 17.6 | <0.0001 |
| LCB | 1.04, 0.99, 0.99, 0.88, 0.79 | ||
| UCB | 1.15, 1.09, 1.08, 0.96, 0.90 | ||
| Rurality | 1.04, 1.04, 1.02, 0.96, 0.96 | 18.7 | <0.0001 |
| LCB | 1.00, 1.00, 0.99, 0.92, 0.92 | ||
| UCB | 1.09, 1.09, 1.05, 1.00, 1.00 | ||
| Black | 0.99, 0.99, 1.00, 1.01, 1.02 | 18.7 | 0.467 |
| LCB | 0.94, 0.96, 0.97, 0.97, 0.97 | ||
| UCB | 1.03, 1.02, 1.03, 1.04, 1.07 | ||
| Driving time | 0.88, 0.90, 0.98, 1.07, 1.11 | 21.5 | <0.0001 |
| LCB | 0.84, 0.86, 0.94, 1.03, 1.06 | ||
| UCB | 0.93, 0.94, 1.01, 1.11, 1.16 | ||
RR estimates evaluated at the specified percentiles of the BG covariate.
Univariate models estimate the BG AMI mortality risk associated with the covariate relative to Arkansas age‐ and sex‐specific rates. LCB/UCB: lower and upper 95% confidence bounds.
Multivariate model estimates the BG AMI mortality risk associated with the covariate after adjusting for the covariates that precede it in the table.
The results of multivariate analyses are also shown in Table. The multivariate analysis shows an incremental increase in percent deviance when sequentially adding BG covariates to a regression model beginning with education, then adding poverty, population density, rurality, black race, and the driving time to the nearest PCI‐capable hospital. Mobility was dropped from the multivariate model because it was not significant when other variables were included. Distance variable was dropped from the multivariate model as it was highly correlated with the driving time. The multivariate model shown in Table explains 21.5% of the deviance in AMI mortality among neighborhoods (BGs). It shows that 2.6% of the deviance in AMI mortality is explained by the driving time to the nearest PCI‐capable hospital after adjusting for the effects of education, poverty, population density, rurality, and black race. This increase in risk of death is statistically significant (P<0.0001). Figure 2A is a composite of the relative risks in BG that was estimated by the multivariate model in Table, and a spatial adjustment of the residuals from the multivariate model. The residuals from the multivariate model exhibit strong spatial patterns indicating that there are other unobserved factors that are differentially distributed across regions of the state, and are also associated with mortality.
Figure 3 shows the trend in the relative risk of AMI mortality with the increasing driving time to the nearest PCI‐capable hospital. The relative risk ranges from at most 0.88 in the 10% of BGs with the shortest driving times to 1.11 in the 10% of BGs with the longest driving times. This indicates a 26% excess risk of AMI mortality attributable to the driving time to the nearest PCI‐capable hospital after adjusting for education, poverty, population density, rurality, and black race.
Figure 3.
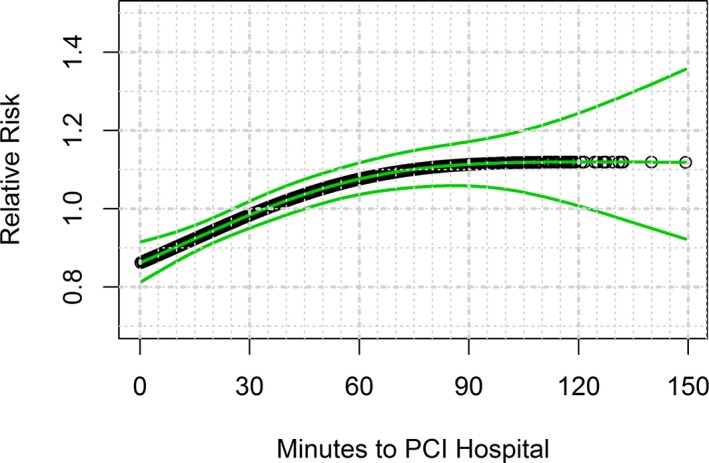
Adjusted relative risk of acute myocardial infarction mortality with 95% confidence bounds (green) as a function of driving time from the population center of the block group to the nearest percutaneous coronary intervention (PCI)–capable hospital.
The results from our sensitivity analysis using centroid of a census BG to calculate the distance to the nearest PCI‐capable hospital yielded similar results. The median distance to a PCI hospital from the centroid of a census BG was 13.0 miles (IQR 3.7–30.2). In another analysis, we found that in 75% of BGs, all the residents were within 5 miles of the population center and in slightly more than 95% of BGs, all residents were within 10 miles of the population center.
Discussion
To our knowledge, this is the first study to assess driving time to the nearest PCI‐capable hospital as a predictor of AMI mortality at the neighborhood (census BG) level. We found a 26% increase in relative risk of AMI mortality as the driving time to nearest PCI‐capable hospital increases after adjusting for education, poverty, population density, rurality, and black race. The median distance to a PCI hospital in the state of Arkansas is 12.8 miles (IQR 3.6–30.1). This is much higher than the US median distance of 7.9 miles (IQR 3.5–22.4).8 The median driving time to the nearest PCI‐capable hospital is 28.3 minutes (IQR 9.6–58.7) in the state of Arkansas. This is over 2.5 times higher than the US median driving time of 11.3 minutes (IQR 5.7–28.5).9 Furthermore, 21% of the state's population 35 years of age and older resides in BGs (over 362 000 people) where driving time exceeds 60 minutes. We calculated the driving time from the population center of the decedent's census BG of residence to the nearest PCI‐capable hospital. This calculation of driving time estimates the average time of all residents in a given census BG. This, along with low educational attainment and poverty, may have contributed to the high age‐adjusted mortality from AMI in Arkansas (85.5 per 100 000 population) compared to the national average (36.9 per 100 000 population).16 The role of education and poverty in AMI mortality cannot be understated. However, adjusting for these predictors does not completely explain the association of driving time with AMI mortality.
AMI mortality rates were not uniform across Arkansas’ neighborhoods (BGs), and this heterogeneity could be explained in part by differences in the incidence of AMI among neighborhoods (BGs). Driving time presumably affects death rates following AMI and not the incidence of AMI. More proximal individual‐level risk factors such as diet, physical inactivity, smoking, obesity, and comorbidities such as hypertension correlate with the neighborhood (BG) covariates we used such as education, poverty, and race. It is our view that these covariates indirectly account for some of the underlying differences. These covariates accounted for 17.8% of the deviance in AMI mortality rates among neighborhoods (BGs), and they reduce the contribution of driving time from 9.9% of the deviance to 2.6% (Table). However, the unmeasured confounding due to not accounting for individual‐level risk factors and their regional distribution cannot be completely eliminated in the study.
Improving the readiness of healthcare systems and response to care for people with AMI can prevent deaths and long‐term healthcare costs. A system of care where there is a coordinated response involving individuals, emergency medical services, and hospitals through integration, collaboration, and networking has been shown to avert deaths due to AMI.17, 18, 19 There are different systems of care utilized by various entities (ie, regional, statewide, healthcare system, and hospitals) for AMI care. Some of the examples of systems of care for heart attack are the Mission: Lifeline STEMI system of care promulgated by the American Heart Association (http://maps.heart.org/ml/#;); and the RACE (Regional Approach to Cardiovascular Emergencies (https://racecars.dcri.duke.edu/) project utilized by the Carolinas Healthcare System. Additionally, a recent report from the National Cardiovascular Data Registry showed that the median interhospital driving time was 57 minutes (IQR 36–88 minutes) in the United States.20 The interhospital driving times suggest that fibrinolytic therapy should be considered for some of these patients, as supported by the Mission: Lifeline and RACE protocols. This analysis might help organize a statewide system of care for STEMI, as was done in North Carolina. The American College of Cardiology (ACC) and the AHA endorsed such approaches as a new Class I recommendation that each community should develop a STEMI system of care.21
There are limitations to our study. First, driving time to the nearest PCI‐capable hospital does not include the time for the EMS to arrive at the scene, and the time spent by EMS at the scene; hence, our driving time estimates are more conservative than what happens in reality. Second, the driving time does not include interhospital transfer time, which also impacts mortality.22 Third, the time from when an individual develops symptoms and then decides to seek care at any healthcare facility can be highly variable. This “Act in Time” response time was not measured. Fourth, we calculated the driving time from the population center of a BG rather than from an individual's residence. Fifth, we did not account for other unmeasured variables such weather factors, which can impact driving time. Lastly, we were unable to parse out the deaths specifically due to STEMI from the death certificates that listed cause of death as AMI. Some of these deaths may have been due to non‐STEMI. Also, accuracy in coding for AMI deaths could lead to differential misclassification by place of death (at home versus en‐route or in‐hospital), and distance to care centers.23 Nonetheless, the pathophysiologic basis of both STEMI and non‐STEMI is the same (ie, luminal obstruction by a thrombus in the narrowed atherosclerotic coronary artery), and the preferred therapy for both types of AMI remains early revascularization.
Conclusions
This study shows that AMI mortality increases with increasing driving time to the nearest PCI‐capable hospital. Improving the healthcare system by reducing time to arrive at a PCI‐capable hospital could reduce AMI deaths.
Acknowledgment
The authors are thankful to Dr John Morgan for his assistance in geocoding the addresses of the deceased to census block groups.
(J Am Heart Assoc. 2016;5:e002378 doi: 10.1161/JAHA.115.002378)
The views expressed in this article are those of the authors and do not necessarily reflect that of the Arkansas Department of Health.
References
- 1. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER III, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB; American Heart Association Statistics C, Stroke Statistics S . Executive summary: Heart Disease and Stroke Statistics–2014 update: a report from the American Heart Association. Circulation. 2014;129:399–410. [DOI] [PubMed] [Google Scholar]
- 2. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13–20. [DOI] [PubMed] [Google Scholar]
- 3. Weaver WD, Simes RJ, Betriu A, Grines CL, Zijlstra F, Garcia E, Grinfeld L, Gibbons RJ, Ribeiro EE, DeWood MA, Ribichini F. Comparison of primary coronary angioplasty and intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review. JAMA. 1997;278:2093–2098. [PubMed] [Google Scholar]
- 4. Boersma E, Maas AC, Deckers JW, Simoons ML. Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet. 1996;348:771–775. [DOI] [PubMed] [Google Scholar]
- 5. De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109:1223–1225. [DOI] [PubMed] [Google Scholar]
- 6. Rathore SS, Curtis JP, Chen J, Wang Y, Nallamothu BK, Epstein AJ, Krumholz HM; National Cardiovascular Data Registry . Association of door‐to‐balloon time and mortality in patients admitted to hospital with ST elevation myocardial infarction: national cohort study. BMJ. 2009;338:b1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cannon CP, Gibson CM, Lambrew CT, Shoultz DA, Levy D, French WJ, Gore JM, Weaver WD, Rogers WJ, Tiefenbrunn AJ. Relationship of symptom‐onset‐to‐balloon time and door‐to‐balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283:2941–2947. [DOI] [PubMed] [Google Scholar]
- 8. Nallamothu BK, Bates ER, Wang Y, Bradley EH, Krumholz HM. Driving times and distances to hospitals with percutaneous coronary intervention in the United States: implications for prehospital triage of patients with ST‐elevation myocardial infarction. Circulation. 2006;113:1189–1195. [DOI] [PubMed] [Google Scholar]
- 9. Patel AB, Tu JV, Waters NM, Ko DT, Eisenberg MJ, Huynh T, Rinfret S, Knudtson ML, Ghali WA. Access to primary percutaneous coronary intervention for ST‐segment elevation myocardial infarction in Canada: a geographic analysis. Open Med. 2010;4:e13–e21. [PMC free article] [PubMed] [Google Scholar]
- 10. Avdic D. A matter of life and death? Hospital distance and quality of care. Essen, Germany: CINCH—Health Economics Research Center; 2015:1. [Google Scholar]
- 11. Buchmueller TCJM, Wold C. How far to the hospital? The effect of hospital closures on access to care. J Health Econ. 2006;25:740–761. [DOI] [PubMed] [Google Scholar]
- 12. Ross JS, Normand SL, Wang Y, Nallamothu BK, Lichtman JH, Krumholz HM. Hospital remoteness and thirty‐day mortality from three serious conditions. Health Aff (Millwood). 2008;27:1707–1717. [DOI] [PubMed] [Google Scholar]
- 13. Hastie TJ, Tibshirani RJ. Generalized Additive Models. Boca Raton: Chapman & Hall/CRC; 1990. [Google Scholar]
- 14. R_Core_Team . R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2014. [Google Scholar]
- 15. Fotheringham AS, Brunsdon C, Charlton M. Geographically Weighted Regression. West Sussex, England: John Wiley & Sons, LTD; 2002. [Google Scholar]
- 16. Centers for Disease Control and Prevention, National Center for Health Statistics . Underlying cause of death 1999–2013 on CDC Wonder online database, released 2015. Data are from the multiple cause of death files, 1999–2013, as compiled from data provided by the 57 vital statistics jurisdictions through the vital statistics cooperative program. 2015.
- 17. Glickman SW, Granger CB, Ou FS, O'Brien S, Lytle BL, Cairns CB, Mears G, Hoekstra JW, Garvey JL, Peterson ED, Jollis JG. Impact of a statewide ST‐segment‐elevation myocardial infarction regionalization program on treatment times for women, minorities, and the elderly. Circ Cardiovasc Qual Outcomes. 2010;3:514–521. [DOI] [PubMed] [Google Scholar]
- 18. Jollis JG, Roettig ML, Aluko AO, Anstrom KJ, Applegate RJ, Babb JD, Berger PB, Bohle DJ, Fletcher SM, Garvey JL, Hathaway WR, Hoekstra JW, Kelly RV, Maddox WT Jr, Shiber JR, Valeri FS, Watling BA, Wilson BH, Granger CB. Implementation of a statewide system for coronary reperfusion for ST‐segment elevation myocardial infarction. JAMA. 2007;298:2371–2380. [DOI] [PubMed] [Google Scholar]
- 19. Parikh SV, Treichler DB, DePaola S, Sharpe J, Valdes M, Addo T, Das SR, McGuire DK, de Lemos JA, Keeley EC, Warner JJ, Holper EM. Systems‐based improvement in door‐to‐balloon times at a large urban teaching hospital: a follow‐up study from Parkland Health and Hospital System. Circ Cardiovasc Qual Outcomes. 2009;2:116–122. [DOI] [PubMed] [Google Scholar]
- 20. Vora AN, Holmes DN, Rokos I, Roe MT, Granger CB, French WJ, Antman E, Henry TD, Thomas L, Bates ER, Wang TY. Fibrinolysis use among patients requiring interhospital transfer for ST‐segment elevation myocardial infarction care: a report from the US National Cardiovascular Data Registry. JAMA Intern Med. 2015;175:207–215. [DOI] [PubMed] [Google Scholar]
- 21. Kushner FG, Hand M, Smith SC Jr, King SB III, Anderson JL, Antman EM, Bailey SR, Bates ER, Blankenship JC, Casey DE Jr, Green LA, Hochman JS, Jacobs AK, Krumholz HM, Morrison DA, Ornato JP, Pearle DL, Peterson ED, Sloan MA, Whitlow PL, Williams DO. 2009 Focused updates: ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2009;120:2271–2306. [DOI] [PubMed] [Google Scholar]
- 22. De Luca G, Ernst N, Suryapranata H, Ottervanger JP, Hoorntje JC, Gosselink AT, Dambrink JH, de Boer MJ, van ‘t Hof AW. Relation of interhospital delay and mortality in patients with ST‐segment elevation myocardial infarction transferred for primary coronary angioplasty. Am J Cardiol. 2005;95:1361–1363. [DOI] [PubMed] [Google Scholar]
- 23. Pagidipati NJ, Gaziano TA. Estimating deaths from cardiovascular disease: a review of global methodologies of mortality measurement. Circulation. 2013;127:749–756. [DOI] [PMC free article] [PubMed] [Google Scholar]


