Introduction
Metallosis is a complication occurring in the joint space as a result of corrosion of metallic prostheses. The corrosion of metallic prostheses leads to deposition of metallic debris and inflammation in the joint space. Metallosis has been reported with stainless steel, titanium, and cobalt chromium alloy femoral prostheses articulating either with a similar metal or a polymer component. Commonly, metallosis is associated with pain and eventually requires replacement of the prosthesis. Cutaneous metallosis is characterized by dyspigmentation of the skin overlying the joint space affected by metallosis. The blue-black skin dyspigmentation, which may occur secondary to joint space metallosis, may be misdiagnosed as an acquired dermal melanocytosis. We report a case of initially asymptomatic joint space and cutaneous metallosis in a patient with a cobalt-chromium molybdenum alloy and titanium-aluminum-vanadium alloy knee prosthesis.
Case report
A 71-year-old African-American woman presented with blue-black dermal pigmentation on her right anterior leg just below the knee (Fig 1). She reported noticing the oddly pigmented area approximately 1 year before her visit. Upon examination, the blue-black pigmented areas were nonerythematous but had hypertrichosis (Fig 2). The patient denied having pain and had experienced no recent trauma. She reported having undergone arthroplasty of her right knee 8 years prior for rheumatoid arthritis. Punch biopsy (3 mm) was performed.
Fig 1.
Blue-black pigmented lesions on upper anterior and lower anteromedial aspects of right leg.
Fig 2.
Hypertrichosis overlying blue-black pigmented lesion on upper anterior aspect of right leg.
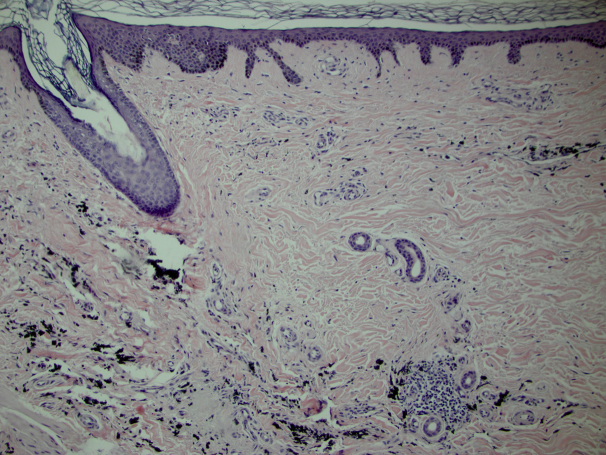
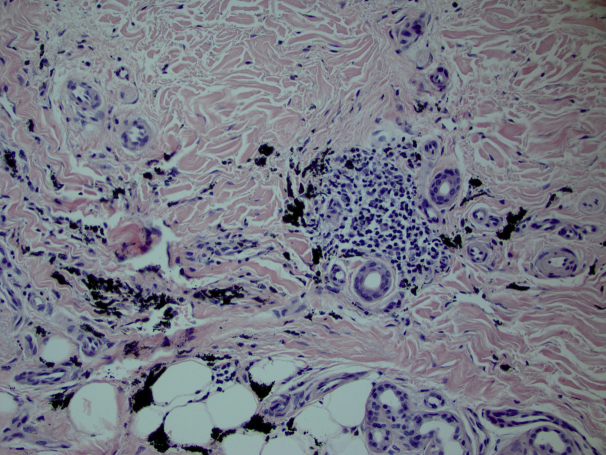
Histopathologic examination of the skin found no epidermal changes. A remarkable interstitial and adnexal accumulation of coarse black granular pigment particles with minimal inflammatory infiltrate was noted (Fig 3). The black particulate matter was seen both within histiocytes and dispersed extracellularly within the dermis with extension to the subcutis. There was no vasculitis (Fig 4). The clinicopathologic correlation favored a diagnosis of cutaneous metallosis secondary to knee prosthesis failure. The patient's orthopedic surgeon recommended replacement of the knee prosthesis. During a conference with the patient's orthopedic surgeon after prosthesis replacement, it was established that the patient had metallosis caused by a corroded knee prosthesis. The metal constituents of the knee prosthesis included a femoral component composed of cobalt-chromium- molybdenum alloy and a tibial component composed of titanium-aluminum-vanadium alloy. The blue-black pigmentation on the patient's right anterior leg was determined to be the cutaneous manifestation of this metallosis; however, the mechanism of the associated hypertrichosis is unknown.
Fig 3.
Low-power view. Interstitial and adnexal accumulation of coarse black granular pigment particles with minimal inflammatory infiltrate.
Fig 4.
High-power view. Interstitial and adnexal accumulation of coarse black granular pigment particles with minimal inflammatory infiltrate.
Discussion
Metallosis is a well-recognized phenomenon, and the mechanism is well documented in the orthopedic literature.1, 2, 3 Metallosis is usually defined as aseptic fibrosis, local necrosis, or loosening of prosthesis secondary to metallic corrosion and release of metallic wear debris into the tissues of the affected joint. Metallosis may be accompanied by gray discoloration of the tissues of the joint, pain, an effusion, and elevated serum metal levels. Metallosis has been documented with stainless steel, titanium, and cobalt-chromium alloy femoral prostheses articulating either with a similar metal or less commonly with a polymer component. Cutaneous metallosis, as seen in our patient, is seldom reported in the literature. Cutaneous deposits of metal after knee arthroplasty generally occur when metal particles generated by wear and corrosion of the metal prosthesis induce an inflammatory response and deposit in the surrounding tissues. Cutaneous metallosis has been described after failure of various joint arthroplasties,2, 4 but, to the best of our knowledge, this has only been described once in total knee arthroplasty.5
Our patient's lesions were noted to be migratory as the lesion started proximally and progressed distally on the right leg. It is remarkable that the patient initially presented with no pain or swelling in the affected joint and exhibited hypertrichosis overlying the blue-black pigmented areas (Figs 1 and 2). Cutaneous metallosis has been associated previously with swelling, pain, and grayish-black discoloration of the affected tissue. Our patient's presentation with associated hypertrichosis is novel. This case is of interest because the cutaneous presentation of metallosis is seldom described and may potentially be misdiagnosed as another acquired dermal melanocytosis, including blue nevi, malignant melanoma, nevi of Ito, or other dermal dyspigmentation including drug-induced pigmentation (eg, minocycline).6 Clinicians should heighten their suspicion for cutaneous metallosis secondary to hardware failure when encountering patients with skin discoloration in the setting of a previous joint arthroplasty.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Crites B.M., Berend M.E., Ritter M.A. Metal-backed patellar components: a brief report on 10-year survival. Clin Orthop. 2001;388:103–104. [PubMed] [Google Scholar]
- 2.Sporer S.M., Chalmers P.N. Cutaneous manifestation of metallosis in a metal-on-metal total hip arthroplasty after acetabular liner dissociation. J Arthroplasty. 2012;27(8):1580.e13–1580.e16. doi: 10.1016/j.arth.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 3.Pritchett J.W. Adverse reaction to metal debris: metallosis of the resurfaced hip. Curr Orthop Pract. 2012;23(1):50–58. [Google Scholar]
- 4.Asahina A., Fujita H., Fukuda S. Extensive skin pigmentation caused by deposits of metallic particles following total elbow arthroplasty: metallosis or not. Br J Dermatol. 2007;157(5):1074–1076. doi: 10.1111/j.1365-2133.2007.08161.x. [DOI] [PubMed] [Google Scholar]
- 5.Park J.Y., Shin D.H., Choi J.S., Kim K.H. Metallic discoloration on the right shin caused by titanium alloy prostheses in a patient with right total knee replacement. Ann Dermatol. 2013;25(3):356–359. doi: 10.5021/ad.2013.25.3.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akimoto M., Hara H., Suzuki H. Metallosis of the skin mimicking malignant skin tumour. Br J Dermatol. 2003;149:653. doi: 10.1046/j.1365-2133.2003.05387.x. [DOI] [PubMed] [Google Scholar]