Introduction
First reported in 1928, Buschke-Ollendorff syndrome (BOS) is an autosomal dominant genodermatosis with high penetrance and variable expressivity. It is characterized by skin-colored or yellow smooth papules, plaques, and nodules up to 2 cm consisting of elastomas or collagenomas, known as dermatofibrosis lenticularis disseminata.1 This syndrome also has nearly pathognomonic radiographic findings of 1- to 10-mm spherical, radiopaque osteosclerotic foci with uneven contours at the epiphysis and metaphysis of the long bones, pelvis, carpi, and tarsi, with rare inclusion of the spine. These foci are known as osteopoikilosis or osteopathia condensans.2
This syndrome may have cutaneous manifestations during early childhood, with most findings developing by puberty. Radiographically, it generally manifests during adolescence and appears most commonly in the phalanges, carpi, and metacarpi but may appear as early as age 2.3 BOS is present equally in males and females, with an estimated prevalence of 1:20,000 in the general population.4 Patients may only have bone or dermatologic findings, but dermatologic manifestations are more commonly present and may include variations of grouped papules and nodules.3, 5 Debilitating symptoms are rare, but radiographic findings may be confused for primary osteoblastic or metastatic disease.6 We present a case of BOS incidentally diagnosed in a 20-year-old white man, with both radiologic and cutaneous findings discovered after complaints of a painful enlarging nodule on the right lower extremity.
Case report
A 20-year-old healthy, active-duty US Army, white male presented to his primary care physician complaining of a painful lump on his right leg for 2 months. The lesion had doubled in size over the 2-month period. His baseline pain was 2 of 10, which was exacerbated with his daily physical training. A radiograph of his leg, obtained by his physician's assistant for a concern of shin splints showed osteosclerotic foci present on the metaphyses of the tibia and fibula. The radiology finding was suggestive of BOS, and the patient was referred to the dermatology department for evaluation, diagnosis, and appropriate disposition of the soldier's future in the Army.
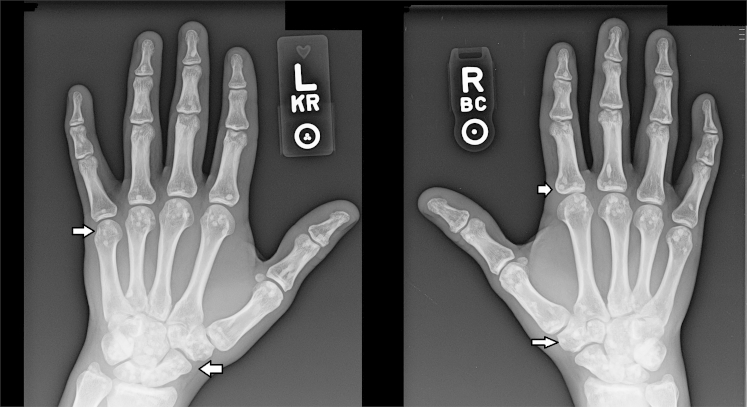
On presentation to the dermatology department, a raised, 3-cm, slightly erythematous, immobile nodule was observed on the right distal lateral lower extremity where the lump was described. In addition, a 5-cm confluent plaque of yellow 1- to 2-mm papules was present on his right lumbar region (Fig 1). Punch biopsies of the lumbar region and the leg nodule were completed. Findings on hematoxylin and eosin staining of the tissue were unremarkable. A Verhoeff–Van Gieson stain of the lumbar region plaque showed conspicuous accumulations of broad, branching, and interlacing elastic fibers in the mid to reticular dermis, with clumped fibers, consistent with an elastoma (Fig 2). Trichrome staining of the leg nodule showed thickening of collagen bundles expanding from the dermis into subcutaneous tissue, suggestive of an evolving collagenoma. In addition, bilateral radiographs of hands and wrists were taken, which found multiple well-demarcated sclerotic foci distributed throughout consistent with osteopoikilosis (Fig 3, Fig 4). The clinical, histopathologic, and radiographic findings supported a diagnosis of BOS.
Fig 1.

Clustered 1- to 2-mm yellow papules present on lower right lumbar area.
Fig 2.

Right lower lumbar punch biopsy site shows broad, branching, clumped, and interlacing elastic fibers in the mid to reticular dermis, consistent with elastoma compared with uninvolved areas of the dermis (Verhoeff–Van Gieson stain; original magnification: ×4).
Fig 3.

Radiograph of lower extremity with radiopaque round to oblong foci at epiphyses and metaphyses.
Fig 4.
Radiograph of left and right hands shows multiple ovoid osteosclerotic trabeculae at epiphyses of radius, ulna, carpal, metacarpal, and phalangeal joints.
Discussion
Although BOS may have genetically heterogeneous origins, it has been associated with a loss-of-function nonsense or frameshift mutation in the 78-kilobase pair LEMD3 gene on the long arm of chromosome 12. This gene is responsible for appropriate skeletal bone formation and downstream regulation of skin collagen and elastin production.6 The mutation leads to a decrease in the inhibition of transforming growth factor β and bone morphogenetic protein via the LEMD inner nuclear membrane protein interactions.6 This loss of function is phenotypically expressed with overproduction of collagen, elastin, and cancellous bone tissue, resulting in osteopoikilosis and elastomas.6, 7
Elastic tissue overproduction can be seen as small, uniform, symmetric papules known as dermatofibrosis lenticularis disseminata, or asymmetric nodules in large groups, resembling pseudoxanthomatous growths.4 Histologic examination finds overproduction of elastic tissue in an interlaced or fragmented pattern. Collagen fibrils can be present in a thick, clumped, or normal distribution in the reticular dermis with loss of rete ridges.4 These findings are best seen through collagen and elastin stains, such as Movat's pentachrome, Trichrome, Orcein, or Verhoeff-van Gieson stains.4 Cutaneous findings generally manifest during adolescence; a recent review article of connective tissue nevi reported that all cutaneous manifestations were complete at the latest by age 15.8
Osteopoikilosis is caused by an abnormality in the endochondral bone maturation process; radiographs of the hands, wrists, feet, ankles, knees, and pelvis can be taken for confirmation. However, the sclerotic foci can be mistaken for neoplastic processes, which may result in additional clinical evaluations for malignancy. Osseous metastases have been known to mimic osteopoikilosis but more typically present in the diaphysis of bones. If still in doubt, alkaline phosphatase level, scintigraphy, or bone biopsy should be done for further confirmation. Osteopoikilosis will not show increased alkaline phosphatase, radiotracer uptake, or positive tumor markers such as CD117 in mastocytosis associated malignancies or CA 15-3 in breast cancer.9
The increase in bone and dermal tissue does not lead to increased risk in morbidity; however, a unique aspect of this case is that the typically asymptomatic nodule was painful because of his daily physical training regimen. This pain could be caused by periostitis from repetitive trauma to the area, compression of regional neurovascular bundles around the increased collagen tissue formation, or increased intraosseous pressure inducing venous stasis, limited to the distal lateral area of osteosclerotic foci.2 Currently, what ultimately caused the pain is unknown, but the physical regimen required of military members acted as a catalyst.
Although BOS is generally benign, it has been associated with glucose intolerance, craniosynostosis, otosclerosis, cataracts, spinal stenosis, and muscle contractures, but to date few reports link BOS to pain worsened with exercise.2 Given subtle findings, radiographic images may not be obtained, thus leading to a missed diagnosis. Therefore, this condition should be in the differential of a painful nodule or biopsy-proven collagenoma.
From a military perspective, a diagnosis of BOS should not disqualify a person from accessioning into the military if previously asymptomatic. Given this patient's history and mild symptoms and his ability to complete prescribed training and military duty, it was determined that observation and education were sufficient, with documentation of findings to prevent unnecessary future work-up in the health care system.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
Disclaimer: The views expressed in this manuscript are those of the authors and do not reflect the official policy or position of the Department of the Army, Department of Defense, or the US Government.
References
- 1.Buschke A., Ollendorff H. Ein Fall von Dermatofibrosis Lenticularis Disseminata und Osteopathia Condensans Disseminata. Derm Wochenschr. 1928;86:257–262. [Google Scholar]
- 2.Paraskevas G., Raikos A., Stavrakas M., Spanidou S., Papaziogas B. Osteopoikilosis: a case report of a symptomatic patient. J Radiol Case Rep. 2009;3(12):38–43. doi: 10.3941/jrcr.v3i12.260. Published online December 1, 2009. Accessed September 26, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Szabo A.D. Osteopoikilosis in a twin. Clin Orthop and Related Research. 1971;79:156. doi: 10.1097/00003086-197109000-00023. [DOI] [PubMed] [Google Scholar]
- 4.Lazar A., Wang W. Diseases of collagen and elastic tissue. In: Lazar A., Brenn T., Calonje E., editors. McKee's Pathology of the Skin. Fourth Edition. Elsevier; © 2012. pp. 935–966. [Google Scholar]
- 5.Morrison J.G., Jones E.W., MacDonald D.M. Juvenile elastoma and osteopoikilosis (the Buschke–Ollendorff syndrome) Br J Dermatol. 1977;97(4):417–422. doi: 10.1111/j.1365-2133.1977.tb14251.x. [DOI] [PubMed] [Google Scholar]
- 6.Yadegari M., Whyte M.P., Mumm S. Buschke-Ollendorff syndrome: Absence of LEMD3 mutation in an affected family. Arch Dermatol. 2010;146(1):63–68. doi: 10.1001/archdermatol.2009.320. [DOI] [PubMed] [Google Scholar]
- 7.Dawson A.L., Schulman J.M., Jordan R.C., North J.P. Ossifying fibroma in Buschke–Ollendorff syndrome. J Cutan Pathol. 2014;41(9):740–744. doi: 10.1111/cup.12365. [DOI] [PubMed] [Google Scholar]
- 8.McCuaig C.C., Vera C., Kokta V. Connective tissue nevi in children: Institutional experience and review. J Am Acad Dermatol. 2012;67(5):890–897. doi: 10.1016/j.jaad.2012.01.036. [DOI] [PubMed] [Google Scholar]
- 9.Kennedy J.G., Donahue J.R., Aydin H., Hoang B.H., Huvos A., Morris C. Metastatic breast carcinoma to bone disguised by osteopoikilosis. Skeletal Radiol. 2003;32:240–243. doi: 10.1007/s00256-002-0605-x. [DOI] [PubMed] [Google Scholar]