Abstract
Background
Primary dystonia is a chronic neurological movement disorder that causes abnormal muscle movements. Pain and emotional distress may accompany these physical symptoms. Behavioural interventions are used to help people with long term conditions improve their quality of life. Little is known about behavioural interventions applied to Dystonia. We report a systematic review of studies reporting current evidence of behavioural interventions for people with primary dystonia.
Methods
We did systematic searches of Medline, PsycINFO, AHMED and CINAHL. We assessed the methodological quality of included studies using a risk of bias tool. Any disagreements were resolved by liaising with an independent rater. Physiological outcomes such as dystonia severity and psychological outcomes such as sleep and depression were selected on the basis that primary dystonia causes motor and non-motor symptoms. No time limit was placed on the searches. A narrative synthesis of the results is presented.
Results
Of 1798 titles and abstracts screened, 14 full articles were retrieved and inclusion and exclusion criteria applied. Of these a final nine were eligible for the review (N = 73). Only two were Randomised Controlled Trials (RCTs). Using the Movement Disorders Society (MDS) dystonia classification, that was published after this work started, all of the included studies were of idiopathic adult onset focal dystonia without associated features. These included: blepharospasm (eye dystonia) (N = 1), cervical dystonia (neck dystonia) (N = 2), writer’s cramp (hand dystonia) (N = 3) and the yips (N = 3). No studies reported on dystonia that affects two or more body regions. Studies reported good adherence and response rates to treatment. Physiological and psychological improvements were noted in all studies at weekly, monthly and yearly follow-ups. Caution should be taken when interpreting the results because of the scarcity of RCTs identified, use of small sample sizes, and inappropriate statistical methods.
Conclusion
We identified few studies; mainly of poor methodological quality that all studied a focal dystonia. It is not possible to draw firm conclusions. Nevertheless, the data suggests that a combined behavioural therapy approach including relaxation practice for people with idiopathic adult onset focal dystonia merits further investigation.
Keywords: Idiopathic adult onset dystonia, Behavioural interventions, Self-management, Quality of life
Background
Dystonia is a neurological condition that can cause abnormal and repetitive muscle contractions and spasms [1]. It is the third most commonly diagnosed movement disorder after Parkinson’s disease and essential tremor [2] with a prevalence variously estimated to be in range of 30–7320 per million [2]. The wide variations on prevalence estimates reflect the different approaches and definitions used by different authors.
Idiopathic adult onset dystonias affecting one body part such as the hand (writer’s cramp) or eyes (blepharospasm) are known as focal dystonia and usually affect adults [1]. In contrast, generalised dystonia typically occurs during childhood and causes spasms and cramping in two or more affected body regions [1]. There may be genetic associations with some idiopathic adult onset dystonias; however, in a majority of cases the cause of disease is unknown [1].
Treatments for generalised and focal dystonia, including pharmaceutical or surgical options, focus predominately on the motor symptoms of the condition. Conservative therapies that have been suggested for helping people with idiopathic adult onset dystonia include: acupuncture, biofeedback, chiropractic manipulation, osteopathy, physiotherapy, speech therapy and transcutaneous electrical nerve stimulation (TENS) [3–6].
However People living with idiopathic adult onset dystonia can experience low self-efficacy, social withdrawal, a negative self-concept and subsequently, poor health outcomes and quality of life [7–10].
More specifically non-motor symptoms of dystonia can include impact on mood (low mood including depression) and emotions, cognitive functioning (such as memory) and impaired sleep [11] Similarly as with other conditions such as Parkinson’s disease, the non-motor symptoms dominate clinical impact and can lead to severe disability and an impaired quality of life [12].
A systematic review investigating the relationship between mental health and ‘primary and other genetic forms of dystonia’ found a relationship between dystonia and emotional disturbance, dystonia and psychiatric disorders and dystonia and cognitive difficulties [11].
People with cervical dystonia for example have a 91.4 % chance of meeting the criteria for a psychiatric illness compared to 35 % in the general population [13]. Other psychiatric illnesses include; major depression, social phobia, panic disorder and for these with focal dystonia a higher risk of obsessive compulsive disorder and anxiety disorder [14]. There is some evidence that cognitive behavioural therapy is effective in the use of the management of anxious thoughts and mood related to muscle tension which could lead to better patient outcomes, however the evidence is limited [15].
We report a systematic review of the evidence for all behavioural interventions for adults living with idiopathic adult onset dystonia.
Methods
The focus of this review is adults living with primary dystonia (idiopathic adult onset dystonia). We excluded studies of people with acquired dystonia to ensure we were reporting dystonia specific effects rather than the combined symptoms from any acquired disorder (e.g., psychiatric, infectious, toxic or neoplastic) [1].
When we developed the protocol for this review we used the terms then current and set our parameter for study entry to be a primary dystonia; this was the terminology used in our PRoSEPRO registration. Since then the Movement Disorder Society‘s new classification has been published. We did not exclude any studies on the basis of clinical features; axis one of the Movement Disorder Society (MDS) classification. In axis two of the MDS classification our entry criteria map onto the idiopathic domain which includes both sporadic and familial cases. We excluded studies of people with known nervous system pathology, known degenerate causes, and those with acquired causes from axis 2 of the MDS classification.
We have post-hoc classified the included studies according to the new MDS criteria. We have, however, kept our original terminology elsewhere in the paper.
Nearly all of the studies we identified had substantial methodological limitations including poor study designs, small samples, and inappropriate statistical tests. Therefore, we were unable to conduct a rigorous meta-analysis.
Search strategy
Between December 2014 and January 2015 we searched: Medline, PsycINFO, AHMED and CINAHL. No date restrictions were applied. Primary dystonia is a broad category encapsulating several different types of medical conditions but studies on dystonia are inconsistently coded in publication databases. For this review, we constructed a broad (sensitive) search strategy to identify relevant studies (please refer to Fig. 1).
Fig. 1.
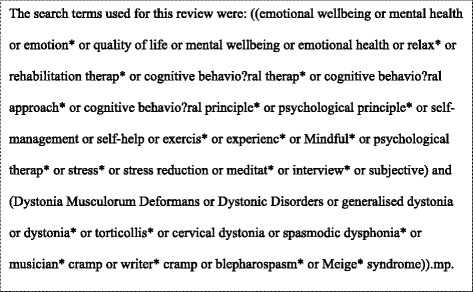
List of review search terms
Selection criteria
Relevant outcome measures included in this review are: wellbeing and/or quality of life and/or psychological functioning and/or sleep and/or other clinical measures such as dystonia severity and/or pain. We included studies of adults (≥18) reporting on individuals living with primary dystonia that examined the effect of behavioural interventions on relevant outcomes. Behavioural interventions are defined as interventions where patient behaviour is the key and the main aim to change that behaviour and can be applied at an individual level, community level or international level [16] (and can include highlighting thoughts processes, beliefs and appraisals and learning to challenge and modify these to improve and change behaviour [15].
We included studies published in English, French, German, Italian and Punjabi. Studies were excluded if they conducted research with individuals under the age of 18 years, animals and secondary types of dystonia or dystonia with another primary condition. Studies of non-behavioural - interventions e.g., medical treatments and psychodynamic therapy were excluded.
We included all primary research reporting quantitative outcome; irrespective of study design. Non-primary articles including secondary analyses, review papers, guidelines, statements, meeting summaries or comments were excluded.
Two independent reviewers (DE and CB) screened the studies’ titles and abstracts for eligibility. For potentially eligible studies’, full-texts were then screened by the rest of the team with the exception of MU who acted as an independent adjudicator, making a final decision on any disputed texts.
Assessing methodological quality
Assessments on all identified studies were performed using a risk of bias rating table that was adapted from a recent systematic review on sleep in primary dystonia [17]. The criteria of risk were based on: diagnosis process, sample size, use of a control group, relevant and valid outcome measures, sufficient description of the intervention, medication and statistics. Risk of bias for each study was rated according to a ‘low’, ‘moderate’, ‘high’ or ‘unclear’ score.
Data extraction
Socio-demographic and clinical details of study participants were extracted by CB and reviewed by the rest of the team for accuracy. Information about the studies’ research question(s), setting(s), behavioural intervention(s), method(s) and outcome measure(s) were also recorded using a pro-forma. The results of the studies were extracted to evaluate psychological (e.g., quality of life, well-being, sleep) and clinical (e.g., pain, dystonia severity, functioning) outcome measures in relation to the reported behavioural intervention(s). A narrative synthesis of the results is reported.
Results
The searches retrieved from the databases yielded 2133 hits. Two studies from one included article’s [18] reference list were identified and the abstracts reviewed; one was potentially eligible but the authors were unable to locate the full-text article and so it has been excluded [19]. We examined 14 full papers and included nine: (Fig. 2 [20]).
Fig. 2.
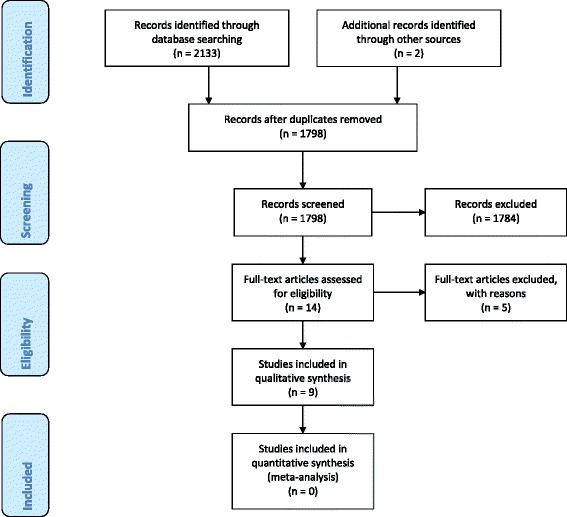
Flow diagram of screening and identification process [20]
We found limited evidence of the following behavioural interventions for different idiopathic adult-onset focal dystonia types: Solution-Focused Guided Imagery (SFGI) for the yips [18, 21, 22], exercise and relaxation practice [23] and Cognitive Behavioural Therapy (CBT) [24] for cervical dystonia, relaxation, systematic desensitisation (SD), assertiveness training and/or Electromyography (EMG) feedback [25], habit reversal with in vivo exposure, awareness training and re-education [26] and relaxation or habit reversal therapy [27] for writer’s cramp and conditioning therapy and relaxation practice for blepharospasm [28]. No studies reported on generalised dystonia. Of the nine studies we identified, two were Randomised Controlled Trials (RCTs) [23, 27] utilising small sample sizes. One RCT found a significant finding for improvement in handwriting quality in both the intervention and control groups at follow-up (week 20) [27]. While all studies reported improvements in dystonia severity and/or emotional distress at weekly, monthly and yearly follow-ups, the poor methodological quality of the data means that firm conclusions cannot be drawn about the effectiveness of behavioural therapies for people living with idiopathic adult onset dystonia.
Quality assessment
Table 1 provides an overview of the findings. Please see web Appendix for the criteria by which the studies were judged (adapted from Hertenstein et al. [17]).
Table 1.
Quality assessment summary
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| Bell and Thompson [18] | Moderate | High | High | Moderate | Moderate | Unclear | Low |
| Bell et al. 21] | Moderate | High | High | Moderate | Moderate | Unclear | High |
| Bell et al. [22] | Low | High | High | Moderate | Low | Unclear | High |
| Boyce et al. [23] | High | High | Moderate | Low | Moderate | Moderate | High |
| Cottraux et al. [25] | High | High | High | High | High | Unclear | Low |
| Faircloth and Reid [24] | Unclear | High | High | Moderate | Moderate | Unclear | Low |
| Greenberg [26] | Unclear | High | High | Moderate | Moderate | Unclear | Low |
| Sharpe [28] | Unclear | High | High | Unclear | High | Moderate | Unclear |
| Wieck et al. [27] | High | Moderate | Moderate | Moderate | Moderate | Unclear | Moderate |
1. Diagnostic process-How well was the diagnostic process described?
2. Sample size-Is this defined?
3. Control group-Is a control group included and if so how well is it defined?
4. Physiological/psychological measure-To what extent are validated outcome measures described/used?
5. Description of intervention-How clear is the description of the intervention?
6. Medication-How well are the medications described?
7. Statistics-How appropriate is the statistical approach?
Low low risk of bias; moderate moderate risk of bias, high high risk of bias, unclear unclear risk of bias
We found two RCTs (N = 20) [23] and (N = 23) [27], two are described as using multiple baseline across subjects design (N = 4) (which is when the same treatment is staggered across participants and multiple data points are obtained from the baseline, intervention and follow-up phases) [21, 22], and two case studies (N = 1) [24, 28]. The remaining three were described as being: a case study using a multiple baseline across situations design (N = 1) [18] (which includes studying the same behaviour across different circumstances, with an aim to test the relationship between treatment and behavioural change in a single subject), an uncontrolled multimodal study (drawing on different modalities including relaxation, systematic desensitization and assertiveness training and biofeedback which was tailored to participants), (N = 15) [25], and a clinical study (reporting the clinical treatment of four cases, delivered by a trained therapist) (N = 4) [26] (Table 2).
Table 2.
Included studies basic characteristics and sample
| Citation | Setting (Country and location) | Design | Sample size (N=) | Mean age (Years) | Gender (m) (f) | Ethnicity | AAOa (Years) | MDb (Years) | PM/Tc |
|---|---|---|---|---|---|---|---|---|---|
| Bell and Thompson [18] | Golf course | CS | 1 (case study) | 40y | 1 m | Caucasian/“White” | NR | 3y | NR |
| Bell et al. [21] | USA, golf courses | CS | N = 3 | 51y | 3 m | Caucasian | NR | NR | NR |
| Bell et al. [22] | USA, golf courses | CS | N = 4 | 51y | 4 m | Caucasian | NR | NR | NR |
| Boyce et al. [23] | Australia, Physiotherapy out-patients clinic & and at home. | pRCT | N = 20 intervention group N = 9; control group N = 11 | 57.8y | 70 % f; 30 % m | NR | NR | 10.2y | Botulinum toxin therapy injections |
| Cottraux et al. [25] | unspecified, | pRCT | N = 15 Multimodal treatment N = 9; (EMG) feedback N = 4 | 36y | 27 % f, 73 % m | NR | NR | 3.6y | psychotherapy |
| Faircloth and Reid [24] | England, unspecified | CS | 1 | 36y | 1 m | NR | 26y | 10y | Botulinum Toxin therapy injections |
| Greenberg [26] | England, London, participants’ homes | CLs | 4 | 52y | 25 % f; 75 % m | NR (1 said to be West Indian) | 49y | 3.5y | NR |
| Sharpe [28] | Unspecified, hospital | CS | 1 | 51y | 1 m | NR | 50/51y | Around 11 months | ‘tetrabenazine and imipramine’ |
| Wieck et al. [27] | London, England, Neurology clinic, participants’ homes | RCT | N = 23 Intervention group N = 11; Control group N- = 12 | intervention group: 52y control group: 49y | 35 % f; 65 % m | NR | NR | Intervention 10y; control 13y | Psychotherapy, biofeedback and drugs. |
CS case studies, pRCT pilot randomised controlled trial, CLs clinical study, NR not reported, EMG electromyography
aAverage age of onset in years. bMean duration of condition, cPrevious medications/treatments
The studies originated from Australia [17], England [24, 26, 27] and the United States of America (USA) [21, 22]; Bell and Thompson [18], Cottraux et al. [25] and Sharpe [28] do not specify the country where their studies were conducted (Table 2).
Boyce et al. [23], Greenberg [26], Sharpe [28] and Wieck et al. [27], conducted the research in hospitals. Bell and Thompson [18] and Bell et al. [21, 22] observed putting on golf courses. Cottraux et al. [25] described their research setting as a clinical study using participants who were referred to their department. Faircloth and Reid [24] did not provide definite details of where their research was conducted (Table 2).
Idiopathic adult onset focal dystonia
We found one study examining blepharospasm [28], two studies that investigated cervical dystonia [23, 24], three studies that conducted research with patients living with writer’s cramp [25–27] and three studies that tested an intervention for the yips [18, 21, 22] which is a type of dystonia that causes ‘jerks, tremors and spasms [and] predominately affects the distal upper extremity’ (p.424) [29]. We found the yips to occur in golfers [18, 21, 22]. Consequently, none of the identified studies included patients with generalised dystonia and therefore, the findings of this review can only report on the effectiveness of behavioural therapies for focal dystonia (Table 3).
Table 3.
Included studies interventions
| Citation and conditiona | Intervention and control | Length of each treatment session (mins) | Frequency | Duration |
|---|---|---|---|---|
| Bell and Thompson [18] Golfing Yips | Intervention: SFGI protocol Control: None |
20–30 | 2x weekly | Unclear duration noted as a number of rounds of golf with follow-up |
| Bell et al. [21] Golfing Yips | Intervention: SFGI protocol Control: None |
20 | 2x weekly | Unclear duration noted as a number of rounds of golf with follow-up |
| Bell et al. [22] Golfing Yips | Intervention: SFGI protocol Control: None |
15 | 2x weekly (unclear) | Unclear duration noted as a number of rounds of golf with follow-up |
| Boyce et al. [23] Cervical dystonia (neck dystonia) | Intervention: Exercise plus relaxation Control: Relaxation only | 30 (approx.) | 4x weekly for the first 4 weeks and then 8x ‘fortnightly for the following eight weeks’ | 8 sessions over 12 weeks |
| Cottraux et al. [25] Writer’s cramp (hand dystonia) | Intervention: Multimodal behaviour therapy package with or without EMG feedback Control: None |
20 (EMG feedback) | 2x daily (without EMG feedback), Unspecified for EMG feedback |
Average total = 14.7 sessions (time period unspecified) |
| Faircloth and Reid [24] Cervical dystonia (neck dystonia) | Intervention: Cognitive Behavioural Therapy (CBT) approach adapting negative thoughts and beliefs into more productive thinking styles Control: None |
Unspecified | Unspecified | ‘9 sessions lasting 10.5 h’ |
| Greenberg [26] Writer’s cramp (hand dystonia) | Intervention: Habit reversal with awareness training, re-education and in vivo exposure. (included encouragement from family to practice) Control: None |
Unclear (for one participant 1 h is reported) | Unspecified | Average total = 4 sessions over 5.5 h |
| Sharpe [28] Blepharospasm (eye dystonia) | Intervention: ‘Flexible behavioural therapy approach Control: None |
60 | Unspecified | Approx. 17 h over 14 weeks (1 week included in-patient treatment) |
| Wieck et al. [27] Writer’s cramp (hand dystonia) | Intervention: Habit reversal (plus homework practice) Control: Relaxation |
90 | 5x monthly | 1 month |
EMG electromyography, SFGI solution focused guided imagery
a The identified studies examined different forms of the MDS idiopathic adult onset focal dystonia category
Three studies provided a full report of participants’ ethnicity [18, 21, 22]. Greenberg [26] described the ethnicity of one out of his four participants. The mean age taken across the entire sample (N = 73) was 47 years (range 36–57.8 years) although it is unclear whether Wieck et al. [27] included the ages of three participants who withdrew (Table 2).
Of the 73 participants 27 (37 %) were female. For five studies 100 % of the sample were male [18, 21, 22, 24, 28] (Table 2). Adherence rates for all of the identified studies were at above 50 % although sample sizes for each study were very low (see Table 4). Two RCTs looking at cervical dystonia and writer’s cramp reported slightly higher levels of adherence among the control groups (91 % for Boyce et al. [23] and 92 % for Wieck et al. [27]) compared with the intervention groups (78 % for Boyce et al. [23] and 82 % for Wieck et al. [27]). Cottraux et al. [25] described an adherence rate of 60 % among people with writer’s cramp with two participants refusing treatment and four participants withdrawing during the intervention phase. Interestingly, Cottraux et al. [25] found that three participants, who had received treatment, later withdrew from the study despite reporting handwriting improvements.
Table 4.
summary of outcome measures and findings for each identified study
| Citation and condition | Outcome measure(s) and timings | Procedure | Facilitator and evidence of facilitator training | Results & Adherence | Comments |
|---|---|---|---|---|---|
| Bell and Thompson [18] Golfing Yips | Yip frequency, baseline, during 5 rounds of golf and at a 60-day follow-up Physiological – observed yip frequency & Putting percentages. |
Researcher read aloud the SGFI protocol to the participant prior to them putting. | Researcher (also, participant and playing partner recorded yip frequency and putting percentage) Training not reported |
Exposure to the SFGI reduced yip frequency from an average of 9.2 yips per round to 0.2 yips per round. Only 1 yip occurrence was recorded during the intervention phase. At baseline, the participant averaged 77 % putts within four feet compared with 97 % during the intervention phase. The participant averaged 81 % of putts within four feet or less at the 60-day follow-up. While the participant said that they felt more confident to putt after being exposed to SFGI, they were unsure why it had helped and were worried that their yips would reoccur. 100 % adherence |
There was no control group to compare the findings, although the authors note that ‘each participant serves as their own control as participants’ performance is compared across baseline and intervention phases’ The study recruited only one participant and so no statistical power, generalisability or reliability. Results open to reporter bias. Yip type was unspecified. |
| Bell et al. [21] Golfing Yips | Yip occurrences were observed at baseline, during at least 5 treatment sessions of golf and at a 3-week follow-up golfing session after the last SFGI round. Physiological – yip occurrences and percentage of putting with the yips. |
1-2 independent observers were stationed at each site. The primary researcher read aloud the SFGI protocol to participants prior to them putting. | Primary researcher (also, 3 trained observers recorded putting behaviour and yip frequency) | Participant 1, BL yips 4, Reduced to 1.4, FU NR Effect size, moderate (0.65). Participant 2, BL yips 3, Reduced to 1.3 FU NR Effect size, moderate (0.55). Participant 3, BL yips 3.6, Reduced to 0.8 FU NR Effect size, moderate (0.73). (1 participant withdrew after completing four rounds of golf at baseline) |
It is unclear whether the primary researcher was 1 of the 3 trained observers. Training provision was specified for the 3 observers but not for the primary researcher. The study is underpowered because it reports on only 3 participants. No control group to compare. No reported p values. The author’s note that no attempt was made to exclude Type I or Type II yips and so some or all of the participants may have been living with secondary yip dystonia. |
| Bell et al. [22] Golfing Yips | Yip frequency was measured at baseline, immediately after treatment and at follow-up (12–14 weeks post-treatment). Physiological – symptom severity, looking at the frequency of yip occurrences. Observations of the golfers putting were video-recorded. |
Individual/1 facilitator read aloud the SGFI protocol to each participant and then recorded the participant’s answers 15 min prior to them putting. | Trained facilitators (individual/1 facilitator per participant). | 100 % of participants showed a decrease in the frequency of yip behaviour: At baseline (average Mean of yip frequency): 2.86 Treatment stage (average Mean of yip frequency): 0.68 Maintenance - at least 12 weeks from treatment stage (average Mean of yip frequency): 0.08. Effect sizes reported as either ‘large’ or ‘medium’ for baseline and treatment and baseline and maintenance. 100 % Adherence |
The study is underpowered because it reports on only 4 participants. No control group to compare. No reported p values. |
| Boyce et al. [23] Cervical dystonia (neck dystonia) | Baseline (week 0), during treatment (week 6), post-treatment (week 12) and at a 4-week follow-up (week 16). Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS) Participants video-recorded and 2 neurologists masked to treatment allocation evaluated symptom severity (primary outcome). Self-rated pain and disability. Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS) (secondary outcomes). depression and quality of life The Beck Depression Inventory Craniocervical Dystonia Questionnaire 24 (secondary outcomes). Cervical range of motion was recorded using a Cervical Range of Motion device (secondary outcome). Attendance at the physiotherapy sessions, adverse effects and muscle soreness were also documented. Participants completed diaries |
Intervention: ‘Active neck exercises plus [whole body] relaxation’ Control: Whole body relaxation programme |
Physiotherapist (individual/supervised physiotherapy sessions) Participants were also encouraged to practise exercises at home No mention of training |
No adverse effects reported. Mild muscle soreness was reported in 66 % of the sample. No significant differences between intervention and control group at treatment and follow-up phases. The intervention group showed an (non-significant) improvement in depression scores compared to the control group in week 12 and ‘a greater (non-significant) improvement in TWSTRS’ in weeks 12 and 16 (p. 6). Effect size: −1.9 (reported difference between the intervention and control groups on TWSTRS). The physiotherapy and home exercise sessions were ‘well-adhered to by both groups’ Adherence 78 % intervention 91 % control |
Small sample and effect size. Confounding variable: N = 7 received Botulinum Toxin therapy injections which may have reduced the effect size. No results were found to be significant. The authors note that the Cervical Range of Motion instrument has unknown reliability for people with cervical dystonia and head tremor/jerks. |
| Cottraux et al. [25] Writer’s cramp (hand dystonia) | Writing quality was observed at baseline (pre)-intervention), post-intervention (last session) and follow-up (at varying weeks between 1 to 9 months). Participants copied a standardised piece of text in the clinic and recorded the amount of cramps they experienced. An independent evaluator also rated participants’ frequency of spasms, writing improvement and writing quality using 3 separate scales across baseline, treatment and follow up phases. |
‘Relaxation, and/or systematic desensitisation (SD), and/or assertiveness training through role playing were combined with Electromyography (EMG) feedback’ (2 participants were not given EMG feedback) (P. 182) | Unspecified but participants were referred to authors’ department No mention of training |
69 % of the sample (N = 9) showed improvements in writing at follow-up (time at follow-up varied between participants, ranging from 1 to 9 months) Of the 4 participants who withdrew during the treatment phase, 3 showed an improvement in handwriting. Adherence 60 % (2 participants refused treatment and 4 withdrew during the treatment phase) |
Small sample size. Limited results and follow-up data to draw meaningful conclusions. 7 participants were reported as presenting with severe mental health problems prior to data collection. 2 participants felt depressed or worried despite showing an improvement on the handwriting scale. 1 participant was described as having ‘’normal handwriting’ out of the 69 % who reported an improvement |
| Faircloth and Reid [24] Cervical dystonia (neck dystonia) | Measures were conducted at baseline (pre-treatment), post-treatment and at one, three and six month follow-ups. The participant was asked to record, using visual analogue scales, how many times they spent worrying about the physical and emotional aspects of their dystonia. The Beck Depression Inventory and the Beck Anxiety Inventory measured the participant’s overall psychological health. |
Enabling self-focus, generating adaptive beliefs and challenging negative thinking. | Unspecified | Improvements were noted in psychological well-being (i.e., anxiety and depression). Pain and discomfort in the participant’s neck was reported as less severe. All of the participant’s 6 months follow-up scores were lower than at baseline. | Small study (N = 1) and so not statistically generalisable. Only subjective (validated and unvalidated) self-report measures were used. |
| Greenberg [26] Writer’s cramp (hand dystonia) | Measures were conducted at baseline (pre-treatment), 1 month, 6 months and various time periods between 2 and 6 years. Patient and therapist independently rated how severely the patient’s problem affected their everyday life and how it impacted on their ability to achieve their targets. Patients were observed during the clinic to assess their writing rate. The patient measured their writing abilities outside of the clinical hospital and where possible a friend or relative confirmed the findings. Fear and anxiety were also rated using general, validated measures. |
A combination of ‘habit reversal, in vivo exposure and re-education’ [apart from 1 participant] Awareness training, encouragement from relatives and homework practice were also given. | Nurse therapists, family and friends supervised homework practice and offered encouragement the nurse therapists received 1–2 sessions of teaching in habit reversal therapy |
The treatment showed an improvement in writing skills at least until the 6-months follow-up phase (p. 297). All 4 participants responded to the treatment. 1 participant relapsed after stopping habit reversal practice. 100 % Adherence |
Small sample size. Not all of the measures were observed. An independent assessor did not assess tidiness. Therapists only observed handwriting in artificial settings. ‘The habit reversal adopted in this trial – extension of the wrist, fingers, and thumb – inevitably means that the pen is released for 5 s. The spasm could thus be said to be rewarded by avoidance’ 1 participant was reported as experiencing high levels of anxiety. |
| Sharpe [28] Blepharospasm (eye dystonia) | Unspecified, baseline, treatment and 9 months follow-up | Relaxation (exercise) training for the eyelids, learning not to force the eyelids open and seeking rewarding reinforcements for keeping the eyelids open | Unspecified | Outcomes included reduction of eyelid spasm and ache as well as relaxation of the eyelids. Participant was able to control spasms and resume daily social and business activities. No deterioration was reported at the 9-months follow-up. 100 % Adherence |
Small study (N = 1) and so not statistically generalisable. Minimal description of follow-up procedures or outcome measures. |
| Wieck et al. [27] Writer’s cramp (hand dystonia) | Outcome measures were recorded at baseline (pre-treatment, weeks 0 and 4), post-treatment (week 8) and at a 3 months follow-up (week 20). ‘Observation of writing within the session, assessment of writing tasks completed at home, and blind ratings by an independent assessor’ |
Patients were educated to know when their symptoms were triggered and to immediately respond (e.g., by putting down the pen) until their cramp stopped. Severer participants were asked to draw lines proceeding to more complex shapes and finally, words. Control group trained to practice ‘progressive relaxation technique’ (p. 113). |
2 therapists No mention of training |
No significant differences were reported between the intervention and control groups on 89 % of the measures. There was an increase in the frequency of words written at home among the relaxation group than with the habit reversal group (where there was a slight decrease). Both groups improved significantly ‘in legibility, number of interruptions, and the ratings for problem severity, pain and difficultly’ (p. 114). However, this was only slightly and participants ‘remained substantially handicapped’ with regards to writing speed (p. 114). The authors conclude that they found no evidence to suggest that habit reversal treatment is more effective than general relaxation. Adherence 82 % intervention 92 % control |
Small sample size. N = 1 experienced anxiety and avoidance behaviour and N = 3 experienced generalised anxiety |
Three studies looking at writer’s cramp reported participants were living with various emotional disturbances [25–27]. Of these three studies, two [25, 27] examined patients’ physical and mental health. However, Cottraux et al. [25] only screened 10 patients (out of the 15 originally recruited into the study) using Multiple Personality Inventory (MMPI) referred to as MimiMult. While participants who were screened with MMPI were not reported as presenting with a consistent pathological pattern, Cottraux et al. [25] noted that seven individuals reported chronic emotional or sexual disturbances. Furthermore, all participants had previously used various treatments including tranquillizers, bromocriptine and psychotherapy [25]. Greenberg [26] reported that one participant out of four displayed general anxiety symptoms. Wieck et al. [27] described one participant in their study as anxious and displaying avoidance behaviour and two patients were reported with living with generalised anxiety.
Bell et al. [21, 22] did not specify how long their participants had been living with dystonia. Sharpe [28] was the only author who reported that the participant had been living with dystonia for under a year (10 months), stating that the participant had also experienced dystonia symptoms for four weeks 11 months earlier. The average duration of dystonia in the remaining six studies was seven years.
Interventions
All of the identified studies examined various behavioural therapies. These include SFGI protocol to individuals experiencing yips [18, 21, 22], which typically causes spasms in the upper limb(s) and can occur in various sports including golf [29], combined behavioural and physical practice including relaxation for patients with cervical dystonia [23], SD, assertiveness training and/or EMG feedback on patients with writer’s cramp [25] and CBT for cervical dystonia [24]. Greenberg [26] investigated the effectiveness of habit reversal therapy (which aims to reduce spasm and involuntary movements by delivering fine motor techniques that are opposite to the involuntary contraction) with awareness training, re-education, and ‘in vivo exposure in which a hierarchy of situations was constructed in which cramp was increasingly likely to occur.’(p.234) Sharpe [28] examined the effects of relaxation with conditioning therapy for one patient with blepharospasm. Finally, Wieck et al. [27] investigated writer’s cramp and assigned the control group individually tailored sessions of relaxation and the intervention group, habit reversal therapy. While the studies’ interventions were fairly diverse, they all focused on examining the effectiveness of enabling participants to self-manage their disability outside of the clinical setting [18, 21–28].
Outcome measures
Eight studies reported outcome measures utilising independently assessed and/or facilitator-led ratings and/or self-report un-validated and/or validated measures to evaluate physiological and/or psychological improvement [18, 21–27].
Two studies used the Beck Depression Inventory to assess depression scores [23, 24]. Faircloth and Reid [24] also used un-validated self-report measures to evaluate psychological wellbeing and an un-validated measure to investigate physical functioning. The authors did not objectively measure any clinical outcomes [24].
The studies examining writer’s cramp observed writing frequency among participants in and outside of the clinic [25–27]. However, Greenberg [26] was the only author examining writer’s cramp to not use an independent assessor to verify handwriting improvements. Instead, only patients and therapists involved in treatment delivery rated handwriting quality [26]. Cottraux et al. [25] utilised an independent evaluator to rate spasm frequency, handwriting quality and handwriting improvement on three separate scales that were combined to obtain the overall mean value of each participant’s handwriting improvement score. Since these data were only obtained in the clinic participants were also asked to self-evaluate their handwriting in a non-clinical setting [25]. However, data obtained from participants outside of the clinic were not systematically scored [25].
Having applied the SFGI protocol, Bell and Thompson [18] requested that the participant and a playing partner record yip behaviour during putting. Similarly, Bell et al. [21] used trained observers to watch putting behaviour among the participants. Video observations of putting behaviour were used by Bell et al. [22] to increase inter-reliability. Bell and Thompson [18] and Bell et al. [21, 22] also used the SFGI protocol to ask participants questions about the severity of their dystonia.
Sharpe [28] did not report using any outcome measures. The authors of this review were unable to contact Sharpe [28] given how long ago the study was published. Nonetheless, Sharpe [28] provides details about outcomes post-treatment and at the 9-month follow-up.
Discussion
We found very limited evidence for behavioural interventions in the treatment and management of idiopathic adult onset dystonia. All of the studies we identified were for the MDS idiopathic adult onset focal dystonias group. The findings therefore only apply to this group. There were some promising results from the RCTs and uncontrolled studies that behavioural therapies can improve peoples’ physical and emotional well-being. Some of the underlying mechanisms mapped onto the behavioural interventions specifically included action planning and problem solving to improve productivity and overall management, education and behavioural experiments to empower and help control symptoms and education and distraction to manage anxiety through cognitive restricting to lessen anxiety and also the severity of dystonia. However all of the identified studies used small samples and nearly all had substantial methodological weaknesses which precluded a rigorous meta-analysis. Therefore, none of the findings can be generalised beyond the study setting. The available evidence applies only to focal dystonias and we cannot make any comment based on possible effectiveness from empirical data for dystonias affecting more than one body segment. Nevertheless, the theoretical justification for behavioural interventions is equally applicable to more than just focal dystonias. This means that the very limited empirical data might be applicable to a wider population of those affected by dystonia. A possible reason for why there have been very few research studies examining the effectiveness of behavioural therapies for people with dystonia could be because idiopathic adult onset dystonia is often misdiagnosed as an emotional illness limiting acceptance of behavioural interventions [9].
There have however been other studies which have also shown that CBT could be beneficial with other movement disorders. For example in a pilot study, tailored CBT for this with depression and Parkinson disease showed a reduction in negative cognitions, reduced depressive symptoms and an increase in the sense of social support [30].
Strengths and limitations of the review
The authors of this review employed a rigorous search and screening strategy to identify and evaluate the relevant studies. It has highlighted an important gap in the literature and is one of the first reviews too examine behavioural interventions for the management of dystonia.
Since Sharpe’s [28] study was conducted some time ago the review authors were unable to obtain information about what outcome measures he utilised. Furthermore, the review found no studies examining the effects of behavioural therapies in people with generalised dystonia. Consequently, this review is limited in not being able to comment whether behavioural treatments would be effective for this patient group. Conducting a meta-analysis was not possible because of study heterogeneity.
Future research and practice
Future research is necessary to establish the effects, if any, of behavioural interventions in patients living with idiopathic adult onset dystonia. Consequently, researchers should consider RCTs with powered sample size, clearly specifying the diagnostic process involved and using physiological and psychological validated outcome measures to capture changes. Detailing the severity of patients’ dystonia could also be useful for comparing treatment effectiveness across different levels of dystonia.
Future research should also examine generalised dystonia in relation to behavioural therapies to address the current gap in the medical and psychology literature.
It is only by addressing the many challenges in designing robust studies of behavioural interventions for the dystonias that we can find out if behavioural treatments can help these stigmatising and disabling chronic disorders.
Conclusion
In conclusion, this review identified nine studies all with low methodological quality, making it difficult to establish the effectiveness of behavioural interventions in patients living with idiopathic adult onset dystonia. The limited data indicates, however, that behavioural therapies could have a beneficial effect for enabling individuals to manage their dystonia, particularly when combined with relaxation practice [23, 25, 27, 28]. Further high-quality research is needed to fully assess the effectiveness of holistic behavioural therapies in patients with idiopathic adult onset dystonia.
Abbreviations
- CBT
cognitive behavioural therapy
- EMG
electromyography
- MDS
Movement Disorder Society
- MMPI
multiple personality inventory
- RCTs
randomised controlled trials
- SD
systematic desensitisation
- SFGI
solution-focused guided imagery
- TENS
transcutaneous electrical nerve stimulation
- TWSTRS
Toronto Western Spasmodic Torticollis Rating Scale
- USA
United States of America
Appendix
Table 5.
Criteria for quality assessment
| Risk of bias rating | ||||
|---|---|---|---|---|
| Low | Moderate | High | Unclear | |
| Diagnostic process | Diagnosis according to established, published criteria | Diagnostic process is described in sufficient detail, but no published criteria were used | Authors mention who performed the diagnosis (e.g., experienced movement specialists) but do not describe the diagnostic process itself | Diagnostic process not described |
| Sample size | ≥ 100 per group (sufficient to detect an effect of Cohen‘s d=0.35) | 21-99 per group | < 20 per group (not sufficient to detect a sample size of Cohen‘s d = 0.8) | Sample size not mentioned |
| Control group | Healthy controls matched for age and sex | Unmatched healthy controls, matched only for age or only for sex, historical control group, controls with another disorder but no healthy controls | No control group | Not mentioned whether control group was included |
| Physiological/ psychological measure | Valid physiological and/or psychological measures of subjective and objective measures (for example clinician ratings of dystonia severity according to validated scale and/or psychological wellbeing and one validated self-report questionnaire) | One adequate physiological and/or psychological measure (for example clinician ratings of dystonia severity according to validated scale and/or psychological wellbeing or one validated self-report questionnaire) | Unvalidated subjective and/or objective measures, questionnaire insensitive or otherwise inappropriate | Measures not sufficiently described |
| Description of intervention | An adequate, clear and comprehensive description of the intervention is provided, including the following: what is being tested, theoretical framework underlying the intervention, components of the intervention, how it was delivered and by whom, what research methods were employed, analytical techniques, when and where it was delivered, whether any materials were used and a description of any relevant facilitator/researcher training | Partially full descriptions of the intervention are provided (i.e. between 1-5 components of this criterion lack sufficient detail or are not provided but the remaining 6-11 components are described in detail) | Very few details are given about how the intervention was delivered (e.g. between 1-5 components of this criterion are adequately described but the remaining 6-11 are not described in detail and/or missing) or otherwise inappropriate or irrelevant descriptions are provided | None of the criterion’s components are described |
| Medication | Un-medicated sample | Medicated sample, medication reported in detail | Medicated sample, medication insufficiently described | Medication not described |
| Statistics | Analysis/statistical approach is adequate for design and sample size, conditions for use of statistical approach tested and described in sufficient detail | Minor shortcomings leading to imprecision, but not invalidation of the results, e.g. conditions for use of statistical approach not tested or not described | Major shortcomings, e.g. no significance testing, inappropriate statistical procedure | Statistical approach not sufficiently described |
Adapted from Hertenstein et al. [18]
Footnotes
Competing interests
HS has received a funding grant from The Dystonia Society to develop a behavioural intervention with Mindfulness practice for patients living with dystonia. The authors declare that they have no competing interests.
Authors’ contributions
This systematic review was conceived by CB, DE, GD, EH, NT, MU, HS. CB registered the review with PROSPERO and received support from DE. CB took the lead for writing this review. DE conducted database searches and CB, GD, EH, NT, HS screened the results. CB extracted the data. MU acted as an independent rater. CB authored the manuscript while the other authors read and commented on previous drafts. All authors read and approved the final manuscript.
Contributor Information
C. J. Bernstein, Email: C.J.Bernstein@warwick.ac.uk
D. R. Ellard, Email: D.R.Ellard@warwick.ac.uk
G. Davies, Email: gail@mind-lab.com
E. Hertenstein, Email: Elisabeth.hertenstein@uniklinik-freiburg.de
N. K. Y. Tang, Email: N.Tang@warwick.ac.uk
M. Underwood, Email: M.Underwood@warwick.ac.uk
H. Sandhu, Email: Harbinder.K.Sandhu@warwick.ac.uk
References
- 1.Albanese A, Bhatia K, Bressman SB, Delong MR, Fahn S, Fung VSC, et al. Phenomenology and classification of dystonia: a consensus update. Mov Disord. 2013;28(7):863–73. doi: 10.1002/mds.25475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Defazio G. The epidemiology of primary dystonia: current evidence and perspectives. Eur J Neurol. 2010;17(Suppl 1):9–14. doi: 10.1111/j.1468-1331.2010.03053.x. [DOI] [PubMed] [Google Scholar]
- 3.Albanese A, Asmus F, Bhatia KP, Elia AE, Elibol B, Filippini G, et al. EFNS guidelines on diagnosis and treatment of primary dystonias. Eur J Neurol. 2011;18(1):5–18. doi: 10.1111/j.1468-1331.2010.03042.x. [DOI] [PubMed] [Google Scholar]
- 4.De Pauw J, Van der Velden K, Meirte J, Van Daele U, Truijen S, Cras P, et al. The effectiveness of physiotherapy for cervical dystonia: a systematic literature review. J Neurol. 2014;261(10):1857–65. doi: 10.1007/s00415-013-7220-8. [DOI] [PubMed] [Google Scholar]
- 5.Delnooz CC, Horstink MW, Tijssen MA, van de Warrenburg BP. Paramedical treatment in primary dystonia: a systematic review. Mov Disord. 2009;24(15):2187–98. doi: 10.1002/mds.22608. [DOI] [PubMed] [Google Scholar]
- 6.Snaith A, Wade D. Dystonia. BMJ Clin Evid. 2011;2011:1211. [PMC free article] [PubMed] [Google Scholar]
- 7.Ben-Shlomo Y, Camfield L, Warner T. What are the determinants of quality of life in people with cervical dystonia? J Neurol Neurosurg Psychiatry. 2002;72(5):608–14. doi: 10.1136/jnnp.72.5.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jahanshahi M. Psychosocial factors and depression in torticollis. J Psychosom Res. 1991;35(4–5):493–507. doi: 10.1016/0022-3999(91)90044-O. [DOI] [PubMed] [Google Scholar]
- 9.Lim VK. Health related quality of life in patients with dystonia and their caregivers in New Zealand and Australia. Mov Disord. 2007;22(7):998–1003. doi: 10.1002/mds.21486. [DOI] [PubMed] [Google Scholar]
- 10.Zetterberg L, Lindmark B, Söderlund A, Åsenlöf P. Self-perceived non-motor aspects of cervical dystonia and their association with disability. J Rehabil Med. 2012;44(11):950–4. doi: 10.2340/16501977-1055. [DOI] [PubMed] [Google Scholar]
- 11.Kuyper DJ, Parra V, Aerts S, Okun MS, Kluger B. Nonmotor manifestations of dystonia: a systematic review. Mov Disord. 2011;26(7):1206–17. doi: 10.1002/mds.23709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chaudhuri KR, Healy DG, Schapira AH, National Institute for Clinical Excellence Non-motor symptoms of Parkinson’s disease: diagnosis and management. Lancet Neurol. 2006;5(3):235–45. doi: 10.1016/S1474-4422(06)70373-8. [DOI] [PubMed] [Google Scholar]
- 13.Gundel H, Wolf A, Xidara V, Busch R, Ceballos-Baumann AO. Social phobia in spasmodic torticollis. J Neurol Neurosurg Psychiatry. 2001;71(4):499–504. doi: 10.1136/jnnp.71.4.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zurowski M, McDonald WM, Fox S, Marsh L. Psychiatric comorbidities in dystonia: emerging concepts. Mov Disord. 2013;28(7):914–20. doi: 10.1002/mds.25501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berardelli I, Pasquini M, Roselli V, Biondi M, Berardelli A, Fabbrini G. Cognitive Behavioral Therapy in movement disorders: a review. Mov Disord Clin Prac. 2015;2(2):107–15. doi: 10.1002/mdc3.12160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cutler DM. Behavioral health interventions: what works and why? In: Anderson NB, Bulatao RA, Cohen B, editors. Critical perspectives on racial and ethnic differences in health in late life. Washington DC: The National Academies Press; 2004. pp. 643–74. [PubMed] [Google Scholar]
- 17.Hertenstein E, Tang NK, Bernstein CJ, Nissen C, Underwood MR, Sandhu HK. Sleep in patients with dystonia: a systematic review on the state of research and perspectives. Sleep Med Rev. 2015 doi: 10.1016/j.smrv.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 18.Bell RJ, Thompson CL. Solution-focused guided imagery for a golfer experiencing the yips: a case study. Athletic Insight. 2007;9(1):52–66. [Google Scholar]
- 19.Blundell N. A cure for the yips: a case study. Golf Victoria. 1990;31(5):11–23. [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009 [PMC free article] [PubMed] [Google Scholar]
- 21.Bell RJ, Skinner CH, Fisher L. Decreasing putting yips in accomplished golfers via solution-focused guided imagery: A single-subject research design. J Applied Sport Psych. 2009;21(1):1–14. doi: 10.1080/10413200802443776. [DOI] [Google Scholar]
- 22.Bell RJ, Skinner CH, Halbrook MK. Solution-focused guided imagery as an intervention for golfers with the yips. J Imagery Res Sport Physical Activity. 2011;6:1. doi: 10.2202/1932-0191.1059. [DOI] [Google Scholar]
- 23.Boyce MJ, Canning CG, Mahant N, Morris J, Latimer J, Fung VSC. Active exercise for individuals with cervical dystonia: a pilot randomized controlled trial. Clin Rehabil. 2012;27(3):226–35. doi: 10.1177/0269215512456221. [DOI] [PubMed] [Google Scholar]
- 24.Faircloth S, Reid S. A cognitive-behavioural approach to the management of idiopathic cervical dystonia. J Behav Ther Exp Psychiatry. 2006;37(3):239–46. doi: 10.1016/j.jbtep.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 25.Cottraux JA, Juenet C, Collet L. The treatment of writer’s cramp with multimodal behaviour therapy and biofeedback: a study of 15 cases. Br J Psychiatry. 1983;142:180–3. doi: 10.1192/bjp.142.2.180. [DOI] [PubMed] [Google Scholar]
- 26.Greenberg D. Writer’s cramp – a habit for reversal? J Behav Ther Exp Psychiatry. 1983;14(3):233–9. doi: 10.1016/0005-7916(83)90054-X. [DOI] [PubMed] [Google Scholar]
- 27.Wieck A, Harrington R, Marks I, Marsden C. Writer’s cramp: a controlled trial of habit reversal treatment. Br J Psychiatry. 1988;153:111–5. doi: 10.1192/bjp.153.1.111. [DOI] [PubMed] [Google Scholar]
- 28.Sharpe R. Behaviour therapy in a case of blepharospasm. Br J Psychiatry. 1974;124:603–4. doi: 10.1192/bjp.124.6.603. [DOI] [PubMed] [Google Scholar]
- 29.Smith AM, Malo SA, Laskowski ER, Sabick M, Cooney WP, Finnie SB, et al. A multidisciplinary study of the “yips” phenomenon in golf: an exploratory analysis. Sports Med. 2000;30(6):423–37. doi: 10.2165/00007256-200030060-00004. [DOI] [PubMed] [Google Scholar]
- 30.Dobkin RD, Allen LA, Menza M. Cognitive-behavioral therapy for depression in Parkinson's disease: a pilot study. Mov Disord. 2007;22(7):946–52. doi: 10.1002/mds.21455. [DOI] [PubMed] [Google Scholar]


