Abstract
Background and Purpose:
Medicine hospitalist programs have effectively incorporated hospitalist-run discharge clinics into clinical practice to help bridge the vulnerable transition periods after hospital discharge. A neurohospitalist discharge clinic would similarly allow continuity with the inpatient provider while addressing challenges in the coordination of neurologic care. We anticipated that this would afford a greater total number of patients to be seen and at a shorter interval.
Methods:
The number of posthospital discharge patients who were seen in general continuity per month in the 6 months prior to establishment of neurohospitalist discharge clinic and those seen over 1 full calendar year 6 months after clinic began was compared by reviewing medical records. Average length of time between discharge from hospital and first clinic visit was compared between patients seen in general neurology continuity clinic and those seen in discharge clinic.
Results:
There was a significant increase in the average number of postdischarge visits per month after initiation of neurohospitalist discharge clinic compared to prior (16.1 visits vs 10.5 visits, P = .001). Patients were seen significantly sooner after hospitalization in discharge clinic (35.9 ± 4.3 days) compared to those seen in general continuity clinic during the same time epoch (57.6 ± 4.1 days; p < 0.001).
Conclusions:
Creation of a neurohospitalist discharge clinic was effective in increasing posthospital discharge follow-up frequency and shortening duration of time to follow-up.
Keywords: neurohospitalist, outcomes, quality, safety
Introduction
The transition period between inpatient hospitalization and outpatient clinic follow-up is considered a particularly vulnerable time for patients due to the risk of adverse events and readmissions. In a review of Medicare beneficiaries who were discharged from 2003 to 2004, about 20% of patients were readmitted to the hospital within 30 days, and of those, there was no bill for an outpatient visit in 50% of cases prior to rehospitalization.1 A prospective study found that discharged medical patients who did not have timely primary care provider follow-up (within 4 weeks) were 10 times more likely to be readmitted at 30 days compared to patients who had timely follow-up.2 In patients discharged from a large academic medical center who were seen by their primary care physicians within 2 months, at least 1 medical error (eg, lack of follow-up or completion of planned postdischarge or pending diagnostic testing or medication reconciliation errors) was detected in 49% of reviewed records.3
These issues are of particular concern within a hospitalist model of care. An inherent discontinuity of care—as a patient’s inpatient and outpatient provider are unlikely to be the same person or even within the same practice group—holds the potential for a “voltage drop” while moving between settings.4 While patients may receive more cost-effective, high-quality care during their hospitalization, lack of continuity and appropriate sign-out during this vulnerable period may lead to patient harm.5,6
Our neurohospitalist program at University of California San Francisco (UCSF) Medical Center5 faced similar challenges and concerns when coordinating postdischarge neurology follow-up and continuity of care. Initially, postdischarge options included: (1) follow-up in a general neurology continuity clinic, which was staffed by neurology residents and rotating outpatient-based neurology faculty attendings, typically with one of the residents who cared for patient in the hospital, (2) referral to a subspecialty clinic, or (3) return to previously established outpatient neurology care in the community. Several obstacles to effective and expedited coordination of care included a limited number of clinic spots in general continuity clinic due to restrictions associated with need for resident supervision; prolonged wait times for evaluation in subspecialty clinics and inability to directly communicate with an outpatient provider as a specific physician in subspecialty group was not known at time of discharge; and challenges in providing exact clinic follow-up time and date for patients evaluated and discharged from the emergency department or nonneurology services especially during evening and night-time hours.
To try and address these barriers to care, we created a neurohospitalist-staffed discharge clinic in the 2012 to 2013 academic year to increase the number of patients who could be seen, to decrease the amount of time between discharge and outpatient follow-up, and to ensure continuation of the inpatient management and treatment plan by having the clinic staffed by the inpatient neurohospitalist group. Physician control over filling clinic appointment slots was also expected to help to create clear appointment dates prior to discharge and thus increase rates of follow-up.
Methods
Design
We introduced a neurohospitalist-staffed discharge clinic at a single academic, tertiary care center on July 1, 2012. For this study, we completed a retrospective electronic medical review of all patients seen in general neurology continuity and the discharge clinic in the 6 months prior to (January 1 through June 30, 2012) and in the full calendar year following (January 1 through December 31, 2013) creation of discharge clinic. Outcomes of interest were compared between patients seen in general continuity clinic versus those seen in hospital discharge clinic. We elected to review clinic visits 6 months after introduction of the discharge clinic to allow time for full integration of this follow-up option into inpatient discharge planning and management. The start date for chart review (January 1, 2012) was chosen based on the availability of chart data following transition to a new electronic medical record; because of this change in record system, only these 6 months of patient data were available.
Standard Protocol Approvals, Registrations, and Patient Consents
The study was approved by the UCSF Committee on Human Research. A waiver of informed consent was granted.
Intervention
The clinic was to be staffed by neurohospitalist attendings and neurohospitalist fellows (who had attending supervision), with an average of four half days of clinic per month. The schedule was created early to allow for flexibility around physician administrative, teaching, and vacation time.
Prior to creation of the discharge clinic, patients evaluated by the general neurology teams who needed nonsubspecialty, posthospitalization follow-up were scheduled in general neurology continuity clinic, typically with the one of the residents on the inpatient team and an outpatient rotating neurology attending. Appointments were made based on next available clinic time and often an exact time and date were not known at time of discharge, so follow-up was coordinated via phone call or letter from clinic staff. After the follow-up visit, patients either returned for follow-up in general continuity clinic, were referred to subspecialty clinic as needed, or were asked to return on an as needed basis.
Patients were scheduled in general neurology continuity clinic or the discharge clinic at the discretion of the inpatient team and attending. Typically, patients who needed to be seen quickly in order to follow-up pending tests, assess treatment response, or who were anticipated to only need a single outpatient follow-up visit based on their diagnosis (eg, Bell’s palsy after emergency department neurology consult evaluation) were preferentially scheduled in the discharge clinic, although factors such as availability of continuity clinic appointment times also determined where patients were ultimately scheduled. Follow-up, then, was not randomized, with the parameters above dictating physician decision regarding clinic assignment. Attendings and residents on service were usually able to make appointments in the discharge clinic in real time given prescheduled clinic dates and times, such that most patients left the hospital with an appointment listed on their discharge paperwork. After clinic follow-up, patients were either transitioned to general neurology continuity clinic, were referred to subspecialty clinic, continued follow-up with a neurohospitalist attending or fellow, or were asked to return on an as needed basis. Inpatient neurohospitalist attendings or fellows were expected to discuss and sign-out patients from the discharge clinic with their outpatient provider who would be assuming care.
Subjects
All patients seen in general neurology continuity clinic in the 6 months prior to establishment of neurohospitalist discharge clinic during the prespecified study periods were included in initial chart review, except for patients who were scheduled for lumbar puncture only in clinic. Patients were identified from the outpatient clinic’s administrative billing database and by searching for patients seen in either of 2 clinics based on known provider schedules. Clinic visits were considered “posthospital discharge” if the clinic visit was the first neurology appointment following emergency department visit or inpatient hospitalization at UCSF, and follow-up after hospitalization at other hospitals were excluded from this category. The patient had to have been evaluated by or cared for by one of the neurology inpatient services during hospitalization.
Data collected from electronic medical records included age and gender of patients, date of clinic visit and date of prior hospital discharge, location/nature of neurologic evaluation (emergency department consult, inpatient consult, or primary neurology service patent), and principal diagnosis. Principal diagnoses were categorized into groups of neurologic disease based on pathophysiology or localization. We also calculated the distance in miles between clinic and patient’s listed home address (when available) using Google Maps7 to allow for comparison between clinic populations.
Outcomes
The primary outcomes of interest examined were total number of patients seen posthospital discharge per month and length of time in days between hospital discharge and clinic visit. Average number of patients seen in continuity clinic per month in the 6 months prior to establishment of the discharge clinic was compared with the average number of patients seen posthospitalization in discharge and continuity clinics per month during the full year following creation.
Statistical Analysis
Comparison of average length of time from discharge to clinic visit was done between patients seen in general continuity clinic in the 6 months prior to establishment of the discharge clinic and those seen in the discharge clinic during 2013 using 2-sample t test assuming unequal variances. A similar test was done to compare average length of time for patients seen during 2013 in general continuity clinic with those seen in the discharge clinic during the same period. The average number of patients seen postdischarge per month was compared over 2 time epochs: from January 1 to June 30, 2012 and from January 1 to December 31, 2013. Secondary analyses of gender and location/nature of inpatient encounter frequency distributions were done using Pearson χ2 test for independence and average age of patients and mean distance in miles from clinic via single factor analysis of variance test. An exploratory analysis comparing the overall readmission rates during the 2 time epochs of the study from the inpatient neurology and neurovascular ward services was also done. Statistical significance for all outcomes was set at α < .05.
Results
In the 6 months prior to initiation of the neurohospitalist discharge clinic, there were a total of 316 visits in the general neurology continuity clinic. Of these, 63 (19.9%) visits involved posthospital discharge. During the 2012 to 2013 calendar year, 6 months after starting discharge clinic, there were 565 visits in general neurology continuity clinic, of which 115 (20.4%) visits were posthospital discharge. In addition, there were a total of 162 visits in the neurohospitalist discharge clinic over this same time period, of which 78 (48.1%) visits were posthospital discharge appointments. Overall, there was a significant increase in the average number of total postdischarge visits from 10.5 visits per month in the 6 months prior to initiation of the discharge clinic to 16.1 visits per month during the 2013 calendar year (t = 3.9, P = .001; see Figure 1).
Figure 1.
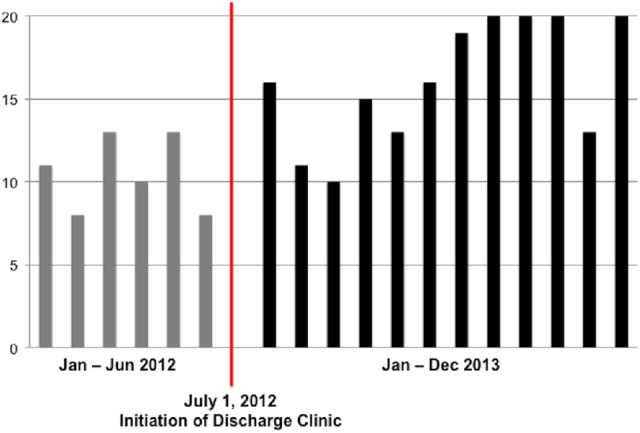
Total number of posthospitalization discharge patient clinic visits per month.
Clinical characteristics of patients seen posthospital discharge are shown in Table 1. There was no difference in the average age across 3 groups (F = 0.098, P = .91) or gender distribution (χ2 = 0.66, P = .72). There was no significant difference in the distribution of initial patient encounter setting (emergency department consult vs inpatient consult vs primary neurology service) across the 3 groups of patients seen in clinic (χ2 = 2.19, P = .70). In addition, there was no significant difference in the distance patients had to travel to clinic after hospital discharge (F = 1.21, P = .30).
Table 1.
Clinical Characteristics of Posthospitalization Patients Seen in General Continuity and Neurohospitalist Discharge Clinic.
| Continuity Clinic, January-June, 2012 (n = 63) | Continuity Clinic, in 2013 (n = 115) | Neurohospitalist Clinic, in 2013 (n = 78) | |
|---|---|---|---|
| Age, mean ± standard error | 53.0 ± 2.5 years | 52.2 ± 1.6 years | 53.4 ± 2.1 years |
| Male, n (%) | 28 (44%) | 54 (47%) | 32 (41%) |
| Time from discharge to visit, mean ± standard error | 67.5 ± 6.3 days | 57.6 ± 4.1 days | 35.9 ± 4.3 days |
| Distance from clinic, mean ± standard error | 60.0 ± 9.7 miles | 42.1 ± 5.1 miles | 50.1 ± 10.6 miles |
| Neuro encounter type, n (%) | |||
| ED consult | 12 (19%) | 30 (22%) | 15 (19%) |
| Inpatient consult | 21 (33%) | 39 (34%) | 26 (33%) |
| Inpatient wards | 30 (48%) | 46 (40%) | 37 (47%) |
| Principal diagnosis, n (%) | |||
| Demyelinating disease | 3 (5%) | 7 (6%) | 6 (8%) |
| Neuromuscular disease | 11 (17%) | 12 (10%) | 15 (19%) |
| Seizure | 13 (21%) | 18 (16%) | 13 (17%) |
| CNS infection | 5 (8%) | 10 (9%) | 12 (15%) |
| Cerebrovascular disease | 5 (8%) | 14 (12%) | 9 (12%) |
| Dementia/delirium | 6 (10%) | 16 (14%) | 7 (9%) |
| Headache | 8 (13%) | 21 (18%) | 7 (9%) |
| Spinal cord disease | 5 (8%) | 7 (6%) | 3 (4%) |
| Dizziness/vertigo | 2 (3%) | 5 (4%) | 4 (5%) |
| Other | 5 (8%) | 5 (4%) | 2 (2%) |
Abbreviations: ED, emergency department; CNS, central nervous system.
Patients were seen significantly sooner in the discharge clinic in 2013 after hospital discharge (35.9 ± 4.3 days) compared to those seen in continuity clinic in the 6 months prior to initiation of discharge clinic from January to June 2012 (67.5 ± 6.3 days; t test = 4.12, P = .00007). Patients were also seen significantly sooner in the discharge clinic compared to those seen in continuity clinic in 2013 (57.6 ± 4.1 days; t test = 3.62, P = .0003).
From January to June 2012, there were a total of 565 inpatient admissions to the inpatient neurology and neurovascular services, of which 32 (5.7%) were readmissions. From January to December 2013, there were a total of 838 admissions to the inpatient services, of which 43 (5.1%) were readmissions. This difference was not statistically significant (P = .33).
Discussion
We successfully incorporated a neurohospitalist-staffed discharge clinic into the routine follow-up of patients evaluated in the emergency department and inpatient settings by our general neurology inpatient services at an academic, tertiary care medical center. Establishment of the clinic was associated with an increased total number of posthospitalization clinic visits per month. In addition, patients seen in the discharge clinic were seen at a significantly sooner interval after hospital discharge, which was not unexpected given nonrandomized selection of patients with need for expedited follow-up.
During this study period, we found from our anecdotal experience that the discharge clinic was also able to address other obstacles to effective follow-up including facile communication regarding patients between inpatient and outpatient providers—as they were all members of a single neurohospitalist group or, often, the same provider—and providing patients and their families with appointment information prior to discharge from the hospital. By allowing inpatient providers to control and create clinic schedules months in advance and by empowering providers to allot patients into clinic appointments in real-time, we found that it was much easier to coordinate disposition planning and follow-up of diagnostic testing. Patients and their families also expressed appreciation about having clear follow-up established prior to discharge, and this helped ease concerns about being lost to follow-up or not knowing how to contact providers after hospital discharge. Among our group of neurohospitalists, we also found that initiation of the discharge clinic led to an increased emphasis on active discharge follow-up planning as a fundamental aspect of effective and efficient patient care. As such, we found that creation of a neurohospitalist discharge clinic led to a culture change in terms of active discharge planning and greater awareness across providers and trainees of the importance of coordinated follow-up once the patient left the hospital.
As part of an academic center, a concern regarding the creation of a neurohospitalist-staffed discharge clinic was the potential loss of educational opportunities for trainees. Based on the number of postdischarge visits increasing overall, patients were not simply shifted from continuity clinic to discharge clinic; the overall percentage of postdischarge visits in continuity clinic was not changed by introduction of discharge clinic. In addition, the discharge clinic was meant to be a bridge to continued neurologic care (when needed) and often included transitioning patients to regular follow-up in continuity clinic with inpatient resident providers after being seen once in the discharge clinic to ensure effective coordination of immediate postdischarge planning and testing. A discharge clinic itself also affords teaching and mentorship opportunities for faculty when working with fellows. Ensuring effective transition of neurologic care from the inpatient to outpatient setting is an important part of the job of a neurohospitalist and should be emphasized during training. As critical thinking and evaluation of the quality and efficiency of medical care has also been highlighted as a core competency in recent updates of neurology residency training milestones, we also hope to include resident trainees in discharge clinic as distinct experience from general continuity clinic.
Some might argue that such a clinic should be staffed by general outpatient or rotating subspecialty neurology faculty, as opposed to neurohospitalists. The former would allow for perhaps more direct transition to continued outpatient care and undoubtedly would also allow for an increased number of patients to be seen at shorter interval after discharge; however, neurohospitalists are specialists in acute neurologic disorders and hospital systems of care, and so may be ideally positioned to help identify and address issues that may lead to hospital readmission and in decisions regarding adjustment of the continuation of treatment plan started during inpatient hospitalization. In addition, not every patient will need continued outpatient follow-up, and so neurohospitalists can provide closure and answer questions for patients and families who do not need continued specific neurologic care, serving as effective gatekeepers in deciding which patients need to be referred to subspecialists within neurology for longitudinal care. As described by medicine hospitalist groups’ experience,8 we also hope that regular involvement in neurology discharge clinic will provide feedback for neurohospitalist providers regarding management decisions and outcomes and additional obstacles to coordinated care and to use that information to improve inpatient care for future patients.
The need for a neurology discharge clinic may be unique to academic or large practice settings, where there is a clear distinction (eg, different practitioners) between neurohospitalists and primary outpatient neurology providers. In practices where inpatient duties are shared on a rotating basis among a group of neurologists who otherwise work in a shared outpatient setting, obstacles to transition of neurologic care are likely decreased. In practices where typical outpatient follow-up may be delayed due to long wait times, incorporation of a similarly structured clinic whose emphasis is posthospital discharge and is staffed by provider who was recently working on the inpatient side is likely to be associated with similar positive outcomes.
Our study has some limitations. Many of the benefits of a neurohospitalist-staffed discharge clinic that we report upon are qualitative in nature and based on our anecdotal experience and are not directly captured by our defined outcomes. In addition, by looking retrospectively only at patients seen in continuity clinic and discharge clinic, information regarding frequency and expediency of follow-up in neurology subspecialty clinics or with previously established outpatient neurology care was not captured in our review. We also only reviewed the charts of patients who were seen in clinic and do not have information regarding patients who did not return for scheduled follow-up. These are important populations for us to consider, as the overall goal of creating discharge clinic is to reduce potential barriers and discontinuities in care.
What also remains to be seen, of course, is whether quicker post-discharge follow-up in neurology will similarly be directly associated with improvement in important metrics such as hospital readmission rates, reduction of medical errors, and patient satisfaction as described by medicine hospitalist practices.9,10 At our center, there was no significant difference in the overall rate of readmissions to the inpatient services between the time epochs of interest, but further studies are needed to see if these rates may be lower in those patients seen in clinic posthospital discharge and also to incorporate patients who were seen initially by the consult service and in the emergency department (and then in clinic) to assess the potential impact of reduction in subsequent hospital visits. The ideal timeframe for the first clinic visit in order to maximize reduction of risk of medical errors or readmissions (typically defined as 2 to 4 weeks in medicine hospitalist literature8–10) is likely to be different in neurology and may also be disease specific. Additional analyses of these important metrics may help achieve the goal of providing care to patients with a wide array of neurologic disorders and continue to strengthen and buttress the bridge between inpatient and outpatient neurologic care.
Depiction of total number of postdischarge clinic visits per month in both general continuity clinic and neurohospitalist discharge clinic, shown in the sixth month prior to initiation of discharge clinic and in the full calendar year afterward.
Footnotes
Declaration of Conflicting Interests: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr Shah reports no disclosures. Dr Douglas receives personal compensation in his role as editor in chief of The Neurohospitalist journal. Dr Scott reports no disclosures. Dr Josephson receives personal compensation in his roles as editor in chief of Journal Watch Neurology and in an editorial capacity for Continuum Audio.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the medicare fee-for-service program. N Engl J Med. 2009;360(3):1418–1428. [DOI] [PubMed] [Google Scholar]
- 2. Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5(7):392–397. [DOI] [PubMed] [Google Scholar]
- 3. Moore C, Wisnivesky J, Williams S, McGinn T. Medical errors related to discontinuity of care from an inpatient to outpatient setting. J Gen Intern Med. 2003;18(8):646–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wachter RM, Pantilat SZ. The “continuity visit” and the hospitalist model of care. Am J Med. 2001;111(9b):40s–42s. [DOI] [PubMed] [Google Scholar]
- 5. Douglas VC, Scott BJ, Berg G, Freeman WD, Josephson SA. Effect of a neurohospitalist service on outcomes at an academic medical center. Neurology. 2012;79(10):988–994. [DOI] [PubMed] [Google Scholar]
- 6. Josephson SA, Engstrom JW, Wachter RM. Neurohospitalists: an emerging model for inpatient neurological care. Ann Neurology. 2008;63(2):135–140. [DOI] [PubMed] [Google Scholar]
- 7. Google Maps. Website http://www.google.com/maps. Accessed July 15 2015.
- 8. Doctoroff L. Interval Examination: establishment of a hospitalist-staffed discharge clinic. J Gen Intern Med. 2012;27(10):1377–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Doctoroff L, Nijhawan A, McNally D, Vanka A, Yu R, Mukamal KJ. The characteristics and impact of a hospitalist- staffed post-discharge clinic. Am J Med. 2013;126(11):1016e 9–1016 e15. [DOI] [PubMed] [Google Scholar]
- 10. Shu C-C, Hsu N-C, Lin Y-F, Wang J-Y, Lin J-W, Ko W-J. Integrated postdischarge transitional care in a hospitalist system to improve discharge outcome: an experimental study. BMC Med. 2011;9:96–103. [DOI] [PMC free article] [PubMed] [Google Scholar]


