Abstract
Background
Lay health advisor (LHA) programs are increasingly being implemented in the USA and globally in the context of health promotion and disease prevention. LHAs are effective in addressing health disparities when used to reach medically underserved populations, with strong evidence among African American and Hispanic women. Despite their success and the evidence supporting implementation of LHA programs in community settings, there are tremendous barriers to sustaining LHA programs and little is understood about their implementation and sustainability in “real-world” settings. The purpose of this study was to (1) propose a conceptual framework to investigate factors at individual, social, and organizational levels that impact LHA activity and retention; and (2) use prospective data to investigate the individual, social, and organizational factors that predict activity level and retention among a community-based sample of African American LHAs participating in an effective, evidence-based LHA program (National Witness Project; NWP).
Methods
Seventy-six LHAs were recruited from eight NWP sites across the USA. Baseline predictor data was collected from LHAs during a telephone questionnaire administered between 2010 and 2011. Outcome data on LHA participation and program activity levels were collected in the fall of 2012 from NWP program directors. Chi-square and ANOVA tests were used to identify differences between retained and completely inactive LHAs, and LHAs with high/moderate vs. low/no activity levels. Multivariable logistic regression models were conducted to identify variables that predicted LHA retention and activity levels.
Results
In multivariable models, LHAs based at sites with academic partnerships had increased odds of retention and high/moderate activity levels, even after adjusting for baseline LHA activity level. Higher religiosity among LHAs was associated with decreased odds of being highly/moderately active. LHA role clarity and self-efficacy were associated with retention and high/moderate activity in multivariable models unadjusted for baseline LHA activity level.
Conclusions
Organizational and role-related factors are critical in influencing the retention and activity levels of LHAs. Developing and fostering partnerships with academic institutions will be important strategies to promote successful implementation and sustainability of LHA programs. Clarifying role expectations and building self-efficacy during LHA recruitment and training should be further explored to promote LHA retention and participation.
Keywords: Lay health advisors, African Americans, Cancer screening, Sustainability, Implementation, Evidence-based programs
Background
Programs and policies that support the use of community-based lay health advisors (LHAs) hold tremendous promise for reducing cancer disparities. LHAs are trained peers or community members who share similar social, economic, cultural, and linguistic characteristics with the population of interest and typically deliver health education, navigation, and support in a range of community-based and clinical settings [1–3]. LHAs are often referred to as promotoras(es), peer educators, community health advisors, navigators, or peer outreach workers in the literature. Such programs are based on the premise that engaging community members contributes to community empowerment and capacity building, while also raising awareness of health and social justice issues, enhancing access to care, and improving health behaviors and outcomes [4]. LHA programs are increasingly being implemented in the USA and globally for a wide range of health issues [2-5]. Research suggests that LHA programs are effective in improving behavior change in several areas, including cancer screening [1, 6–13], with the strongest evidence among racial/ethnic minority women [6, 11, 14–20] who experience greater structural barriers to healthcare [21].
Eliminating racial and ethnic cancer disparities will require the successful dissemination, implementation, and sustainability of culturally appropriate evidence-based programs. Breast cancer in particular is responsible for a large proportion of cancer-related morbidity and mortality among African American women [22].The National Witness Project (NWP) is one example of an evidence-based LHA program; a national replication trial found that NWP was highly effective in increasing breast and cervical cancer screening among African American women [23, 24]. NWP uses a robust theory-based, culturally appropriate model [25] that is comparable to many other community-based LHA programs; during 60–90 min group-based “sessions” in community settings, a minimum of three to four trained African American LHAs provide resources, support, navigation, and education to African American women [20, 26]. Overall, half of the LHAs are African American breast and cervical cancer survivors who deliver empowering testimonials and narratives and serve as “role models” [26–30]; faith-based elements are often included (e.g., hymns, prayers), reflecting the common value of spirituality among African Americans [31–33]. While LHAs are often volunteers, some sites provide LHAs with stipends. LHAs work together with project directors from their site to organize and lead sessions and recruit participants, while project directors help identify host institutions, ensure a network with screening resources, secure funding and partnerships, and recruit LHAs. Project directors may be paid staff or volunteers, depending on program funding. Since 1990, NWP has been replicated and implemented in over 40 sites nationally (in both urban and rural settings), with over 400 volunteers, reaching more than 15,000 women annually. NWP has also been identified as one of the National Cancer Institute’s “Research Tested Intervention Programs” [25].
There are tremendous barriers to sustained implementation of LHA programs in practice, and little is understood about their sustainability. Sustainability has been defined as the continued use of program components and activities for the continued achievement of desirable program and population outcomes [34]. Documented barriers to sustainability of LHA programs include lack of funding and/or limited funding sources, lack of national standards and policies to guide program implementation, difficulty conducting ongoing program evaluation to support program continuation [35–37], and numerous costs to implementing programs (e.g., time and resources related to training, materials, supervision, space, evaluation) [35].
Another challenge to sustaining programs relates to the recruitment and retention of LHAs, as LHAs are often volunteers that receive no financial benefits or receive small stipends [35–38]. There can be high turnover and low activity levels and retention among LHAs, with global attrition rates (i.e., loss of trained eligible pool of LHAs) ranging from 3.2 to 77 % [39, 40]. There are several potential explanations for such variability in participation, including a range of support and incentive structures provided. Attrition rates are particularly high among volunteer LHAs [39–41]. Consistent with the broader literature on the sustainability of evidence-based programs [42], the dropout and low participation of LHAs hampers the impact and sustainability of LHA programs [40, 43, 44].
Studies in this area have been primarily conducted among low- and middle-income countries globally (e.g., [45, 46]). Qualitative and quantitative research suggests that social prestige, financial incentives, community and family approval, and sense of social responsibility and values are key motivating factors that affect LHA performance, activity level, and retention [39, 41, 45–48]. Aspects of the work environment, including clarity of job expectations and organizational processes and practices (incentives, supervision, support, training, etc.) [47, 49, 50], are also likely to influence LHA participation.
The factors influencing the activity level and retention of LHAs likely differ across diverse settings (e.g., US context vs. low- and middle-income countries). No studies, to our knowledge, have examined these factors among African American LHA programs in the USA, and few studies have empirically investigated a range of factors across individual, social, and organizational levels to understand LHA participation. This study seeks to address that gap by investigating individual, social, and organizational factors that predict activity level and retention among a community-based sample of African American LHAs. This research can inform strategies to successfully recruit, train, support, and sustain LHAs in community-based settings, with the ultimate goal of improving the implementation and sustainability of effective LHA programs.
Conceptual framework
Our conceptual framework (see Fig. 1) for examining factors that predict LHA activity level and retention was informed by prior research and conceptual models that have examined factors associated with retention among LHAs (predominately in global settings) [39, 41, 46, 47, 49, 51], as well as conceptual frameworks that focus on the sustainability of evidence-based interventions [34, 42, 52, 53].
Fig. 1.
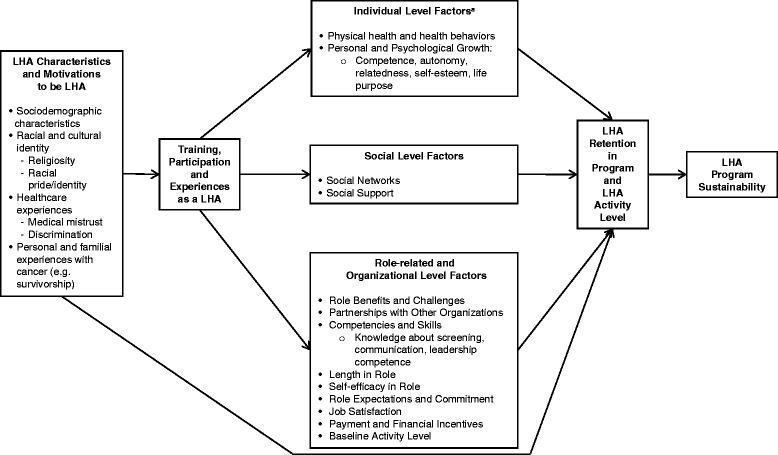
A conceptual framework of factors that impact lay health advisor retention and program activity level. aIndividual Level Factors that influence LHA retention and activity level also include LHA Characteristics and Motivations to be LHA
Individual level
We examined sociodemographic characteristics that theoretically could impact retention and activity level, including paid employment, age, education, marital status, and general health. We also examined aspects of personal and psychological growth (i.e., competence, autonomy, relatedness, self-esteem, life purpose) that LHAs could experience through the program and might impact their participation. These factors may be particularly important in the context of community-based programs that provide little economic compensation. Though not previously explored, pride in one’s racial identity (the extent to which being a member of a specific racial/ethnic group is a significant aspect of one’s identity) [54], perceptions of discrimination in healthcare settings and medical mistrust [55], and other prior personal experiences or beliefs (e.g., experiences as a cancer survivor, religiosity) may also provide initial and ongoing motivation to be a LHA in the African American community.
Social level
LHA programs rely on a strategy that builds upon and expands existing social networks. LHAs are often trained with other LHAs and work as a team to conduct educational sessions. Further, for many LHA programs, part of their role is to educate and provide support to people within their social networks. Thus, participation in LHA programs may increase the size and composition of one’s social network and enhance levels of perceived support. Providing support has health-related benefits and is a strong predictor of self-reported health [56, 57]. This is consistent with Riessman’s Helper Therapy Principle (the personal growth and benefits that nonprofessional helpers may experience through their training and service to others) [58] and supports the notion that LHAs may receive social and psychological benefits from their work that motivate them to participate and remain in such programs.
Role-related factors and organizational level
Role-related benefits experienced (e.g., social recognition, professional development) [49, 59], possible role challenges experienced (e.g., burnout, emotional stress, family conflict), and conditions of the work environment (e.g., insufficient training, supervision and leadership, organizational support, resources) could impact retention [49, 60, 61]. LHAs at sites with partnerships with other organizations that facilitate access to organizational resources pertinent to screening (e.g., academic institutions, medical centers, hospitals, cancer centers) may also impact participation. LHAs may develop new capacities and transferable competencies and skills (e.g., knowledge of screening, communication, leadership competence), factors that may influence their effectiveness, and potentially retention. Length in role, self-efficacy in role, role clarity and commitment, and job-satisfaction are other job-related factors that have not been well examined in this literature but are likely important in understanding retention [38, 62, 63]. Finally, payment or financial incentives have consistently been found to be strongly associated with activity level and retention in global settings [40, 47, 49].
Methods
Recruitment
We contacted eight NWP sites in the northeast, south, and mid-west regions of the USA. Sites were selected from a total of 20 sites that had attended the most recent NWP Annual Meeting for Education and Networking (AMEN) in 2010. The NWP local project director and the study principal investigator (RS) informed LHAs about the study through a mailed letter, telephone, and presentations at scheduled meetings and trainings. LHAs interested in participating provided written permission to be contacted by the study team. LHAs who expressed interest in participation were contacted by telephone to complete the informed consent process and to schedule the telephone-based study assessment. Institutional Review Board approval was awarded through Columbia University’s Mailman School of Public Health. A total of 84 eligible LHAs provided their contact information (representing the entire pool of eligible LHAs at those sites), and of those, a total of 76 women completed the consent process and participated in the study (response rate = 91 %).
Eligibility and data collection
Eligible participants had to be self-identified as African American or black, female, a LHA from the NWP (currently or within the past 2 years), over the age of 18, and English-speaking. Predictor variable data were collected during baseline interviewer-administered telephone surveys that took place between 2010 and 2011. Follow-up outcome data on LHA participation and activity levels were collected from project directors in late fall of 2012 and assessed LHA participation for the prior year. All study participants received a $25 gift card for their participation for each interview.
Predictors
Individual-level factors
Sociodemographic information collected from participants included age, income, education, insurance, healthcare provider, and employment. Autonomy, competence, and relatedness were measured using the 20-item Basic Psychological Needs Scale [64] (α = .61). Life engagement was measured with a six-item scale [65], for which participants rated how much they agreed with each item using a 5-point Likert scale (α = .51). Self-esteem was measured using the six-item Rosenberg self-esteem scale [66] (α = .70). General self-rated health was measured with a one-item validated measure [67]. Breast and cervical cancer survivorship was determined based on their NWP role (women who have a history of breast or cervical cancer act as both LHAs and “role models” and provide testimonials). Racial pride was evaluated using a seven-item scale developed for African Americans [31] (α = .80). Medical mistrust was measured using a sub-scale on disparities from the Group-Based Medical Mistrust Scale [68] (α = .89). Discrimination in healthcare was measured with one question from The Experiences of Discrimination Measure [55]. Participants were given a score of 0–3 based on their responses (response options: never, one to two times, three to four times, or five or more times). Religiosity was measured using a nine-item scale validated for African Americans [31] (α = .86).
Social factors
Social networks were measured using Cohen’s Social Network Index [69]. This index asked participants about 12 different types of social relationships and the quantity of social ties. For each type of relationship where the participant indicates that they speak to someone (in person or over the telephone) at least once every 2 weeks, that network was assigned 1 point (maximum score = 12). The total number of members in each network was summed to include the number of people they speak to at least once every 2 weeks. Social support was measured using the Social Provisions Scale, a validated ten-item scale [56]; respondents rated each item on a scale of 1 to 4 (α = .85).
Role-related and organizational factors
Knowledge of breast and cervical cancer and screening was measured using a 13-item scale developed by the NWP, with a score based on the percentage of correct answers (α = .62). Self-efficacy was measured using a 21-item scale validated among black LHAs [18] for measuring overall role self-efficacy and the sub-scales of growth self-efficacy, collective self-efficacy, and skills self-efficacy (response options, 1 (not at all confident) to 4 (very confident)) (α = .69–.85). Leadership competence was measured using the Sociopolitical Control Scale [70], with responses averaged to determine an overall score (α = .73). The 25-item Helper’s Perception Measure [59] measured mean perceptions of role-related benefits and challenges of being a LHA on a scale of 1 to 5 (1 = strongly disagree and 5 = strongly agree). LHA role expectations (commitment and clarity) were measured using nine items adapted for this study; participants indicated how much they agreed or disagreed with items using a 5-point scale (α = .86). Job satisfaction as a LHA was measured using a six-item adapted version of the validated Job Satisfaction Index [71] (α = .60). LHAs were asked if their current position with NWP was paid (yes; no). LHAs self-reported their baseline activity level in NWP as currently “active,” “inactive,” or “inactive but hope to become more active”. At the organizational level, we categorized LHAs as belonging to a site that was at an academic institution or had a partnership or affiliation with an academic institution (yes; no). Based on communication with the national and site leadership, this was defined as a NWP site that was housed within an academic institution or had a strong formal partnership with such an institution (e.g., schools of public health or medicine, academic hospitals, and cancer centers).
Outcomes
Data on LHA-continued participation was collected about 18–24 months after the LHA baseline survey from project directors of sites where LHA participants were associated. Consistent with other studies [39, 41, 72], we examined levels of participation. We defined “activity level” based on whether LHAs had conducted two or more educational sessions over the past year (high/moderate activity) versus fewer than two sessions in the prior year (low/no activity). Two sessions were determined to be a meaningful level of participation based on the data distribution (the median number of programs per year was 2) and conversations with NWP project directors. We also examined LHA “retention” based on this same data; retention was defined as whether a trained volunteer LHA had conducted any sessions in the community in the previous year. Participants were categorized as “completely inactive” (0 sessions in the past year) or “retained” (at least one session in the past year).
Statistical methods
Data were summarized using percentages, means, standard deviations, and ranges. To compare differences between LHAs who were retained (vs. completely inactive) and LHAs with high/moderate activity levels (vs. low/no activity levels), Fisher’s exact test or a chi-square test was used for categorical variables and analysis of variance (ANOVA) was used for continuous measures. To determine which variables remained independent predictors of activity level and retention status, multivariable logistic regression was used. All variables that were significant at the p ≤ 0.15 level in bivariate analysis were considered for inclusion in full multivariable logistic regression models. Models were then adjusted, using a stepwise selection approach, whereby only those variables that were significant at p < 0.05 were permitted to remain in the models; finally, reduced models are presented in Table 3. Results are organized according to the levels presented in our conceptual framework. We present models and tables in two separate ways (i.e., models that include and do not include baseline self-reported LHA activity) because of (1) concerns about the potential reliability of this self-report measure and (2) concerns about our ability to adequately explore other theoretically informed variables when baseline activity level is included in the model given the strength of this association and our sample size. Missing data was minimal. All analyses were performed using SAS 9.3 (SAS Institute, Cary, NC).
Table 3.
Reduced multivariable models predicting lay health advisors’ retention in the program and high/moderate activity levels
| Model A: model predicting retentiona | |||
| Odds ratio | 95 % confidence interval | p value | |
| A1. Without baseline LHA activity | |||
| Type of institution | |||
| Academic | Reference | – | 0.003 |
| Non-academic | 0.16 | (0.05, 0.55) | |
| Length in program | 0.99 | (0.98, 0.99) | 0.03 |
| Role expectations (clarity and commitment) | 5.73 | (1.43, 22.9) | 0.01 |
| A2. Adjusting for baseline LHA activity | |||
| Type of institution | |||
| Academic | Reference | – | 0.0005 |
| Non-academic | 0.022 | (0.002, 0.19) | |
| Baseline activity level | |||
| Active | 62.7 | (6.29, 579) | 0.0003 |
| Inactive | Reference | – | |
| Model B: model predicting high/moderate activity levelsb | |||
| Odds ratio | 95 % confidence interval | p value | |
| B1. Without baseline LHA activity | |||
| Type of Institution | |||
| Academic | Reference | – | 0.009 |
| Non-academic | 0.21 | (0.06, 0.67) | |
| Self efficacy (overall) | 12.7 | (1.31, 123) | 0.03 |
| Religiosity | 0.8 | (0.64, 0.99) | 0.05 |
| B2. Adjusting for baseline LHA activity | |||
| Type of Institution | |||
| Academic | Reference | – | 0.0002 |
| Non-academic | 0.05 | (0.01, 0.24) | |
| Religiosity | 0.70 | (0.52, 0.95) | 0.02 |
| Baseline activity level | |||
| Active | 59.2 | (9.56, 367) | <0.0001 |
| Inactive | Reference | – | |
a Retention in program status was defined by whether an LHA conducted at least one educational sessions in the year. Retained LHAs conducted at least one educational session in the past year
bProgram activity level was defined by the average number of educational sessions completed by LHAs in the year. LHAs considered to be moderately/highly active completed two or more educational sessions in the past year
Results
LHA and position characteristics
Seventy-six (76) LHAs participated in this study; half of these women (50 %) (n = 38) were breast or cervical cancer survivors. LHAs were involved in the program for a mean of 65.8 months (approximately 5 1/2 years), ranging from 0 months (for newly trained LHAs) to 16 years. Ninety-two percent (92 %) of LHAs were in voluntary NWP positions (i.e., were reported not being paid a salary for being a LHA by NWP or the organization where NWP is based) and 51 % of the sample was not currently employed outside of the NWP (predominately due to retirement). Participating LHAs represented a diversity of geographic sites: 14 (18 %) were from Harlem, NY; 10 (13 %) were from Syracuse, NY; 17 (22 %) were from Little Rock, AR; 5 (7 %) were from Long Island, NY; 6 (8 %) were from Tampa, FL; 4 (5 %) were from Chicago, IL; 17 (22 %) were from Buffalo, NY; and 3 (4 %) were from Wichita, KS. Additional characteristics of LHAs, organized by activity level (high/moderate vs. low/no), are reported in Tables 1 and 2. Overall, 71 % of sites were affiliated with or had partnerships with academic institutions.
Table 1.
Sociodemographic and health-related characteristics of lay health advisors (n = 76) by activity level
| All LHAs (n = 76) | Low/no activity (n = 28) | Highly/moderately active (n = 48) | p value | ||||
|---|---|---|---|---|---|---|---|
| n or mean (SD) | % or [range] | n or mean (SD) | % or [range] | n or mean (SD) | % or [range] | ||
| Length of activity in program (months) | 65.8 (53.0) | [0–192] | 70.6 (55.5) | [3–192] | 63.0 (51.9) | [0–180] | 0.48 |
| Level of activity at baseline | |||||||
| Active | 59 | 78 | 15 | 54 | 44 | 92 | 0.0005 |
| Inactive | 2 | 3 | 2 | 7 | 0 | 0 | |
| Inactive, but hope to become more active | 15 | 20 | 11 | 39 | 4 | 8 | |
| Breast/cervical cancer survivorship | 0.15 | ||||||
| Cancer survivor | 38 | 50 | 11 | 39 | 27 | 56 | |
| No history of cancer | 38 | 50 | 17 | 61 | 21 | 44 | |
| Employed | 0.15 | ||||||
| Employed by the NWP | 6 | 8 | 0 | 0 | 6 | 13 | |
| Employed outside of the NWP | 24 | 32 | 10 | 36 | 21 | 44 | |
| Not employed/retired | 29 | 51 | 18 | 64 | 21 | 44 | |
| Position | 0.08 | ||||||
| Paid | 6 | 8 | 0 | 0 | 6 | 13 | |
| Voluntary | 70 | 92 | 28 | 100 | 42 | 88 | |
| Age | 54.9 (13.5) | [21–78] | 57.1 (12.9) | [22–78] | 53.5 (13.9) | [21–76] | 0.27 |
| Education | 0.31 | ||||||
| ≤Some college | 30 | 39 | 13 | 46 | 17 | 35 | |
| Associate’s or Bachelor’s degree | 33 | 43 | 9 | 32 | 24 | 50 | |
| Graduate or professional degree | 13 | 17 | 6 | 21 | 7 | 15 | |
| Income | 0.45 | ||||||
| <$10,000–$24,999 | 16 | 21 | 6 | 21 | 10 | 21 | |
| $25,000–$49,999 | 22 | 29 | 7 | 25 | 15 | 31 | |
| >$50,000 | 32 | 42 | 11 | 39 | 21 | 44 | |
| Refused | 6 | 8 | 4 | 14 | 2 | 4 | |
| Marital status | 0.45 | ||||||
| Married | 32 | 42 | 11 | 39 | 21 | 44 | |
| Never married | 23 | 30 | 10 | 36 | 13 | 27 | |
| Separated/divorced/widowed | 20 | 26 | 6 | 21 | 14 | 29 | |
| Did not respond | 1 | 1 | 1 | 4 | 0 | 0 | |
| Have primary care provider | 69 | 91 | 23 | 82 | 46 | 96 | 0.09 |
| Primary insurance | 0.45 | ||||||
| Medicaid or Medicare | 31 | 41 | 14 | 50 | 17 | 35 | |
| Employer-provided insurance | 33 | 43 | 10 | 36 | 23 | 48 | |
| None/other | 12 | 16 | 4 | 14 | 8 | 17 | |
| Self-rated health | 0.32 | ||||||
| Excellent/very good | 24 | 32 | 6 | 21 | 18 | 38 | |
| Good | 37 | 49 | 15 | 54 | 22 | 46 | |
| Fair/poor | 15 | 19 | 7 | 25 | 8 | 17 | |
| Current smoker | 6 | 8 | 3 | 11 | 3 | 6 | 0.66 |
| Servings fruits and vegetables per day | 3.1 (1.5) | [1–10] | 2.8 (1.3) | [1–5] | 3.2 (1.6) | [1–10] | 0.29 |
| Days per week of exercise | 2.8 (2.2) | [0–7] | 3.0 (2.6) | [0–7] | 2.7 (2.0) | [0–7] | 0.66 |
Program activity level was defined by the average number of educational sessions completed by LHAs per year. LHAs with low/no activity completed an average of less than two educational sessions per year and LHAs who were moderately/highly active completed two or more educational sessions per year.
Table 2.
Individual, social, and role-related/organizational characteristics of lay health advisors (n = 76) by activity level
| All LHAs (n = 76) | Low/no activity (n = 28) | High/moderate activity (n = 48) | p value | ||||
|---|---|---|---|---|---|---|---|
| Measure [possible range] | Mean score (SD) | Range | Mean score (SD) | Range | Mean score (SD) | Range | |
| Individual level factors | |||||||
| Religiosity [9–36] | 33.7 (3.2) | 18–36 | 34.4 (2.3) | 28–36 | 33.3 (3.6) | 18–36 | 0.12 |
| Racial pride [7–28] | 24.2 (3.0) | 10.0–28.0 | 24.1 (3.6) | 10.0–28.0 | 24.2 (2.6) | 18.0–28.0 | 0.92 |
| Medical mistrust [1–5] | 2.2 (0.8) | 1.0–4.0 | 2.2 (0.9) | 1.0–4.0 | 2.1 (0.8) | 1.0–3.7 | 0.87 |
| Discrimination in healthcare settings [0–3] | 1.0 (1.2) | 0–3 | 0.9 (1.3) | 0–3 | 1.0 (1.2) | 0–3 | 0.70 |
| Basic psychological needs scale | |||||||
| Autonomy [1–7] | 6.1 (0.6) | 4.0–7.0 | 6.0 (0.5) | 4.6–6.9 | 6.1 (0.7) | 4.0–7.0 | 0.64 |
| Competence [1–7] | 6.3 (0.8) | 2.6–7.0 | 6.2 (1.0) | 2.6–7.0 | 6.4 (0.7) | 4.6–7.2 | 0.19 |
| Relatedness [1–7] | 6.4 (0.6) | 4.4–7.0 | 6.3 (0.5) | 5.1–7.0 | 6.2 (0.7) | 4.4–7.0 | 0.82 |
| Life engagement test [6–30] | 28.8 (1.4) | 24–30 | 28.8 (1.4) | 24–30 | 28.9 (1.5) | 24–30 | 0.76 |
| Rosenberg self-esteem scale [6–24] | 22.9 (1.5) | 18–24 | 22.8 (1.5) | 18–24 | 23.0 (1.5) | 19–24 | 0.57 |
| Social level factors | |||||||
| Number of Social networks [0–12] | 7.4 (1.7) | 3–10 | 7.3 (1.6) | 5–10 | 7.5 (1.7) | 3–10 | 0.55 |
| Total number of people in network [0—infinity] | 50.5 (46.8) | 13–272 | 44.0 (31.9) | 14–146 | 54.2 (53.4) | 13–272 | 0.37 |
| Social provisions scale | |||||||
| Overall [10–40] | 37.5 (3.3) | 26–40 | 37.5 (2.4) | 32–40 | 37.5 (3.8) | 26–40 | 0.99 |
| Guidance [2–8] | 7.7 (0.8) | 4–8 | 7.7 (0.7) | 5–8 | 7.7 (0.9) | 4–8 | 1.00 |
| Worth [2–8] | 7.4 (0.9) | 5–8 | 7.4 (0.8) | 6–8 | 7.4 (1.0) | 5–8 | 0.94 |
| Integration [2–8] | 7.4 (0.8) | 5–8 | 7.2 (0.8) | 5–8 | 7.5 (0.8) | 5–8 | 0.23 |
| Attachment [2–8] | 7.5 (0.9) | 4–8 | 7.6 (0.6) | 6–8 | 7.4 (1.0) | 4–8 | 0.46 |
| Alliance [2–8] | 7.6 (0.7) | 5–8 | 7.7 (0.6) | 6–8 | 7.6 (0.8) | 5–8 | 0.71 |
| Role-related and organizational factors | |||||||
| Partnerships with other organizations | 0.02 | ||||||
| Academic | 54 | 71 | 15 | 54 | 39 | 81 | |
| Non-academic | 22 | 29 | 13 | 46 | 9 | 19 | |
| Breast cancer knowledge Mean score (% correct) [0–100] |
84 (14) | 46–100 | 79 (17) | 46–100 | 88 (11) | 54–100 | 0.008 |
| Self-efficacy | |||||||
| Overall [1–4] | 3.7 (0.3) | 2.8–4.0 | 3.6 (0.3) | 2.8–4.0 | 3.8 (0.2) | 3.1–4.0 | 0.04 |
| Skills [1–4] | 3.7 (0.3) | 2.9–4.0 | 3.6 (0.3) | 2.9–4.0 | 3.7 (0.3) | 2.9–4.0 | 0.06 |
| Growth [1–4] | 3.7 (0.3) | 2.9–4.0 | 3.6 (0.3) | 2.8–4.0 | 3.8 (0.3) | 2.9–4.0 | 0.06 |
| Collective [1–4] | 3.9 (0.3) | 2.7–4.0 | 3.8 (0.4) | 2.7–4.0 | 3.9 (0.3) | 3.0–4.0 | 0.36 |
| Leadership competence [1–5] | 4.1 (0.5) | 2.8–5.0 | 4.0 (0.5) | 2.9–5.0 | 4.1 (0.5) | 2.8–4.9 | 0.48 |
| Helper’s perception | |||||||
| Role benefits [1–5] | 4.5 (0.4) | 3.4–5.0 | 4.5 (0.4) | 3.4–5 | 4.5 (0.4) | 3.6–5.0 | 0.81 |
| Role stressors [1–5] | 1.6 (0.5) | 1.0–3.0 | 1.7 (0.5) | 1.0–2.6 | 1.6 (0.5) | 1.0–3.0 | 0.55 |
| Role expectations (clarity and commitment) [1–5] | 4.6 (0.4) | 3.2– 5.0 | 4.5 (0.5) | 3.2–5.0 | 4.6 (0.4) | 3.7–5.0 | 0.20 |
| Job satisfaction index [1–5] | 4.4 (0.5) | 3.4–5.0 | 4.4 (0.5) | 3.4–5.0 | 4.4 (0.5) | 3.4–5.0 | 0.92 |
Program activity level was defined by the average number of educational sessions completed by LHAs per year. LHAs with low/no activity completed an average of less than two educational sessions per year and LHAs who were moderately/highly active completed two or more educational sessions per year
Retention in the program and activity level
As reported by project directors, LHA retention in this sample was 68 %; 32 % (n = 24) of LHAs were completely inactive at follow-up (defined as conducting 0 sessions in the prior year). Of the 68 % who were still active at follow-up, 46 (88.5 %) reported being active at baseline, while the remaining 6 (11.5 %) reported that they were inactive but hoped to become more active. We found that 37 % (n = 28) of participants had low activity levels (defined as conducting fewer than two educational sessions in the past year) at follow-up. The number of sessions conducted per year by LHAs ranged from 0 to 32 (mean = 3.8; median = 2).
Models predicting complete inactivity vs. retention in the program
Comparisons between LHAs who were completely inactive vs. retained (retention status at follow-up) showed possible relationships in bivariate models (at p ≤ 0.15) for variables at the individual and role-related/organizational levels. At the individual level, age (p = 0.06) and self-reported health (p = 0.12) were significant, with younger women and those reporting good to excellent health more likely to be retained. At the role-related and organizational level, a number of factors were significant: partnership with academic site (p = 0.002; academic sites had better retention); length in program (p = 0.13; less time in program for those who were retained, mean of 59.6 months vs. 79.4 months); breast cancer knowledge (p = 0.01; higher knowledge among retained); overall self-efficacy (p = 0.07) and growth self-efficacy (p = 0.08) (with higher self-efficacy for those retained); role clarity and commitment (p = 0.05) (with higher scores for those retained); and self-reported baseline LHA activity (p = 0.0005) (LHAs active at baseline were more likely to be retained).
Final models A1 and A2
Results from the final models (displayed in Table 3, models A1 and A2) showed that LHA retention was only significantly associated with variables from the role-related and organizational level. In model A1, LHAs based at non-academic sites had significantly decreased odds of being retained at follow-up than LHAs from academic sites (p = 0.003; odds ratio (OR), 0.16; confidence interval (CI), 0.05, 0.55). LHAs who had been in the program longer had decreased odds of being retained (p = 0.03; OR, 0.99; CI, 0.98, 0.99) than LHAs who were newer to the program. Finally, LHAs who reported greater role clarity and commitment had 5.7 times increased odds of being retained at follow-up than LHAs who had lower expectations or commitment (p = 0.01; OR, 5.73; CI, 1.43, 22.9). After adjustment for self-reported baseline LHA activity status (model A2), affiliation with a non-academic site remained significantly associated with decreased odds of LHA retention.
Models predicting high/moderate activity vs. low/no activity in the program
In bivariate models comparing LHAs who were highly/moderately active to those who were less/not at all active, possible differences (at p ≤ 0.15) were observed for variables under domains of individual level factors and role-related and organizational factors. Differences were observed for individual level factors: survivorship status (p = 0.15, active members more likely to be survivors), employment status (p = 0.15; active members more likely to be employed), having primary healthcare provider (p = 0.09, active members more likely to have PCP), and religiosity (p = 0.12, active members having lower scores). At the role-related and organizational level, the following were significant: partnership with academic site (p = 0.02, active members coming from academic sites), position payment (p = 0.08; active members more likely to be paid), breast cancer knowledge (p = 0.008; active members having higher scores), overall self-efficacy (p = 0.04), skill self-efficacy (p = 0.06), and growth self-efficacy (p = 0.06, active members having higher scores). Self-reported baseline activity status was also significantly associated with activity level, with LHAs active at baseline more likely to be active at follow-up (p = .0005).
Final models B1 and B2
In the final models for activity level (displayed in Table 3, models B1 and B2), LHA activity level was associated with variables at the individual and role-related/organizational levels. As seen in model B1, LHAs based at non-academic sites had decreased odds of being highly/moderately active compared to LHAs from academic sites (p = 0.009; OR, 0.21; CI, 0.06, 0.67), after controlling for self-efficacy and religiosity. In addition, higher overall self-efficacy scores were associated with increased odds of being highly/moderately active (p = 0.03; OR, 12.7; CI, 1.31, 123.00). Higher religiosity scores were associated with decreased odds of being highly/moderately active at follow-up (p = 0.05; OR, 0.80; CI, 0.64, 0.99). After adjustment for baseline activity status (model B2), affiliation with a non-academic site and religiosity remained associated with decreased odds of high/moderate activity level.
Discussion
This study sought to address a notable gap in the literature by examining individual, social, and organizational/role-related factors that predict retention and activity level among a sample of 76 LHAs from eight urban and rural NWP sites. We found that 32 % of trained LHAs were completely inactive at follow-up, consistent with other studies that have been conducted in predominately low- and middle-income countries [39, 41, 48]. This study helps to quantify concerns about LHA retention and participation that have been reported elsewhere [35–38] and suggests that retention factors likely impact the sustainability of LHA programs. On the other hand, given that many of the LHAs were voluntary and not paid for participation in the program, the rates of retention and activity level are impressive and indicate strong commitment to the program among LHAs.
A notable finding from this study is that role-related and organizational factors were consistently associated with LHA retention and activity level. LHAs located at sites that were affiliated with or had strong partnerships with academic institutions were consistently more likely to be retained and to have high/moderate activity levels, even after adjustment for self-reported baseline LHA activity level. LHAs from non-academic sites had about an 80 % decrease in odds of being active, compared to those from academic sites (in models not adjusting for baseline LHA activity level). Though we are not aware of prior research that has empirically tested whether partnerships with academic institutions predict retention of LHAs, there is literature that suggests that such partnerships are integral to the sustainability of community-based programs, including LHA programs [34, 73, 74]. Based on this finding, we collected post hoc data from the project directors on differences between sites with and without academic partnerships that could contribute to these findings. Specifically, sites with academic partnerships were more likely to provide stipends to their LHAs, hold regular trainings, have a steering committee in place, and have physical space dedicated to the program (data not shown).
In addition, it is possible that sites with strong connections to academic institutions are more likely to have other sources of funding to support LHAs and LHA programs when there are interruptions in funding streams. This corresponds to findings from our earlier replication research [24] that demonstrated the crucial nature of having both “Administrative” and “Community Champions” for successful replication. The administrative champion would often be a key resource for securing support, grants and resources. It may be that the academic partners are more likely to have individuals serving as an administrative champion who are vested in shared outcomes with the LHAs, providing key organizational structure, resources and support to sustain such programs. Research is needed to understand this finding and to identify actionable processes in place at sites with academic partnerships to inform strategies that can be used to support and retain LHAs.
Other factors that impacted participation of LHAs in the program included length of time in NWP, suggesting that LHAs who have been in NWP longer may need extra support to prevent dropout or burn-out. Factors leading to and the impact of burn-out on LHAs and other volunteers are not well understood and warrant further research. Alternatively, as has been suggested in prior research in the context of Latina promotora programs [36, 37], LHA dropout may reflect the social mobility of LHAs who have gained new skills, competencies, and expertise and who are now are able to make advances in their careers. These explanations should be further explored in longitudinal research and qualitative or ethnographic research among LHAs. Additionally, in our research, LHAs who reported having clear role expectations were more than five times more likely to be retained (vs. completely inactive) at follow-up, suggesting that this is an important factor that impacts retention. This is consistent with other research that highlights the importance of role clarity, commitment, and expectations in influencing worker motivation and retention [39, 41, 49, 61]. This finding also suggests that clarifying role expectations when enrolling new LHAs is a critical part of the recruitment and training process that should be addressed on an ongoing basis.
In predicting activity level (high/moderate vs. low/no), we found that role self-efficacy was associated with greater activity level and that religiosity was associated with lower activity level in this sample. Consistent with prior research in global settings [46], this finding indicates that strategies to increase LHA self-efficacy through training and feedback may be important in increasing participation among LHAs. Furthermore, LHAs with high levels of religiosity may need additional support to be active in the program, potentially due to additional religious commitments affiliated with their faith and/or church duties or due to related volunteer responsibilities that may compete with their time. These factors should be further explored in larger studies, given that our observed association between self-efficacy and activity level had very wide confidence intervals, which, coupled with our sample size, suggests some instability in model estimates. Furthermore, our findings related to religiosity may be more specific to the NWP and other faith-based LHA programs, given that the program often includes faith-based elements and can be implemented in faith-based settings. Of note, role clarity and overall role self-efficacy were no longer associated with retention and activity level (respectively) after controlling for self-reported baseline LHA activity level. It is possible that self-efficacy is a marker of previous activity that in turn predicts subsequent activity, and this should be explored in future studies with larger sample sizes.
In contrast to the literature in global settings (e.g., [39, 41, 46, 48, 75]), we did not find that family approval/conflict, social prestige, and payment/economic incentives were critical factors impacting LHA participation. This suggests that it is important to consider differences in factors shaping LHA retention across different contexts. For example, economic and financial factors and family approval may be less important in the US context where LHAs may take on these roles in addition to other forms of paid employment and where women may have more economic and social independence from their families and partners [76]. These findings should also be interpreted in the context of our study, in which there was low variability in terms of payment because the overwhelming majority (92 %) of LHAs were unpaid volunteers. There is currently much debate about the payment of LHAs [77, 78] and the strengths and limitations of formalizing these roles. In addition, we had low variability on the items related to family conflict and social prestige (women reported low family conflict and high social prestige); these items were included as part of a larger scale that measured role challenges and benefits, respectively, and thus may contribute to differences across studies.
There are several limitations that should be recognized. While this is one of the largest studies to date of African American LHAs in the USA, it would be ideal to have a larger sample size for conducting quantitative analyses and multivariable models. As a result, our confidence intervals are wide for some analyses (e.g., self-efficacy), suggesting that the magnitude of the effect is difficult to determine given our sample size. Our findings are also primarily generalizable to LHA programs in community-based settings among racial/ethnic minority populations, including programs that involve cancer survivors as LHAs. While the characteristics of our sample are very similar to characteristics of other US-based community health workers (CHWs) [79], it is important to note distinctions between LHAs and CHWs. Despite similarities in characteristics and frequent overlap in qualifications and roles (e.g., provide culturally and linguistically appropriate health education, advocate for community and individual care), CHWs are typically paid and can have additional roles (e.g., proactively identifying and enrolling eligible individuals in health or social service programs, coordinating care for community residents) that may distinguish them from LHAs [80]. CHWs, but not LHAs, have been explicitly recognized under the Affordable Care Act as a part of the interdisciplinary training to support care through area health education centers and patient-centered medical homes [81, 82].
It is also possible that we underestimated LHA dropout, given that LHAs who participated in the study at follow-up may have already been more motivated and involved than those who did not participate. Ideally, we would have been able to conduct analyses based on scaling approaches (e.g., ordinal categories for activity level). Our sample size and the distribution of data prevented us from using this modeling approach; however, exploratory bivariate analyses using ordinal categories suggested that findings were consistent with those presented here. Unfortunately, we were not able to assess the performance or effectiveness of LHAs as part of our outcome, nor do we have information about the kind of payment that LHAs received (e.g., wage, stipend, etc.). In addition, due to limited sample size and the fact that there were eight sites, we did not have the statistical power to control for site in multivariable models. Since academic affiliation is significant and included in all models, this could control for some of the clustering of site. Finally, we recognize that sustainability and retention are likely affected by national, state, and local policies, including funding or financial resources of the sites, although these factors were beyond the scope of this study. Future research should examine broader policy factors that affect the sustainability of LHA programs.
Strengths of the study should be recognized. We conducted data collection from eight urban and rural sites in the USA and had a high response rate among LHAs. We conducted research among African American LHAs in the US context, a population and setting that has been highly underrepresented in this literature. Our results also contribute to limited research on the implementation and sustainability of evidence-based programs. Unlike many studies in this area, our study was longitudinal and the outcome was measured using an objective, non-self-reported measure (activity reported by project directors) with an excellent retention rate of participants. Finally, our conceptual framework was theory-based, comprehensive, and multi-level.
Very little research has tested strategies and interventions to promote involvement and activity levels among LHAs or the sustainability of LHA programs. The limited research that has been conducted suggests that a multi-level, localized, or context-specific approach may be important [38, 83]. Expanding incentive systems to include both financial and non-financial incentives may be important to motivate and retain LHAs [39, 41, 84, 85]. Stipends, gas cards, transportation, childcare, and meals have been suggested as strategies to increase participation and commitment among LHAs [35, 51]. Non-financial recognition (e.g., social and community recognition) may also be important in influencing participation [35–37, 39, 41, 60, 78], as are opportunities for career building and advancement (e.g., training, ongoing skill development) [5, 86].
We have additional recommendations, based on our findings. Clear communication about role expectations during recruitment and ongoing training to build and maintain self-efficacy may be important strategies to promote LHA retention, consistent with prior research [36, 37, 39, 41, 60, 86, 87]. Supportive feedback and supervision have been found to be important [5, 47, 60]. Forming partnerships and locating program champions (community members and professionals who take responsibility for identifying potential funding sources and network with other community partners and leaders to lobby for space, funding, and other resources) [36, 37] may also be critical for LHA program sustainability, as suggested by our research here and in our earlier work [24]. Building the capacity of promotoras and community participants to apply for funding [38] and building leadership capacity [88] are other strategies that have not been well-explored, but warrant further research. Given limited knowledge in this area, developing and testing evidence-based strategies and policies that promote sustainability of LHA programs should be a priority area for future research [38].
Conclusions
This research highlights some of the key role-related and organizational factors that influence LHA program participation and retention, critical indicators of the sustainability of evidence-based LHA programs. This information can be used to inform implementation and sustainability of LHA programs for underserved populations in community settings and can help advance the development of conceptual frameworks related to overall sustainability of evidence-based programs. This study addresses an important gap, as there have been very few empirical studies that have provided insight into the sustainability of LHA programs in the US context. We suggest future directions for informing potential strategies to support LHAs (e.g., emphasis on role expectations and building self-efficacy at trainings) and for informing strategies to promote successful program implementation and sustainability (e.g., identifying program champions and developing partnerships with academic institutions). Given that LHA programs are increasingly being used globally and nationally to effectively improve health and address health disparities and that there are growing opportunities for the integration of LHAs in prevention and healthcare delivery, it is critical that more research focus on program implementation and sustainability to maximize their reach and impact.
Acknowledgements
We are grateful to the NWP National Steering Committee, project directors, coordinators, LHAs, and role models from the National Witness Project who contributed their time to this study. In particular, we would like to thank and acknowledge Detric “Dee” Johnson and Mattye Willis for all of their efforts and support. This research was funded by a grant from the National Cancer Institute (5R03CA150543-03, “Serving as a Lay Health Advisor: The Impact on Self and Community).
Abbreviations
- AMEN
Annual Meeting for Education and Networking
- CHW
community health worker
- CI
confidence interval
- LHA
lay health advisor
- NWP
The National Witness Project
- OR
odds ratio
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
RCS conceived of the study and participated in the data collection and analysis for the study and drafted the manuscript. SKD participated in the data collection and coordination for the study and assisted in drafting the manuscript. NL participated in the data analysis and interpretation of the results. LJ assisted with the original study conception and contributed to the drafting of the manuscript. HST assisted with original study conception and contributed to drafting the manuscript. DMC was involved in drafting the manuscript, interpreting the results, and revising the manuscript critically. DOE assisted with original study conception and contributed to drafting the manuscript. All authors read and approved the final manuscript.
Contributor Information
Rachel C. Shelton, Phone: 212-342-3919, Email: rs3108@cumc.columbia.edu
Sheba King Dunston, Email: drshebaking@gmail.com.
Nicole Leoce, Email: nil2103@columbia.edu.
Lina Jandorf, Email: Lina.Jandorf@mssm.edu.
Hayley S. Thompson, Email: thompsoh@karmanos.org
Danielle M. Crookes, Email: Dac2179@cumc.columbia.edu
Deborah O. Erwin, Email: Deborah.Erwin@RoswellPark.org
References
- 1.Brownstein JN, Hirsch GR, Rosenthal EL, Rush CH. Community health workers “101” for primary care providers and other stakeholders in health care systems. J Ambul Care Manage. 2011;34(3):210–20. doi: 10.1097/JAC.0b013e31821c645d. [DOI] [PubMed] [Google Scholar]
- 2.Earp JAL, Viadro CI, Vincus AA, Altpeter M, Flax V, Mayne L, Eng E. Lay health advisors: a strategy for getting the word out about breast cancer. Health Educ Behav. 1997;24(4):432–51. doi: 10.1177/109019819702400404. [DOI] [PubMed] [Google Scholar]
- 3.Eng E, Parker E, Harlan C. Lay health advisor intervention strategies: a continuum from natural helping. Health Educ Behav. 1997;24(4):413–7. doi: 10.1177/109019819702400402. [DOI] [PubMed] [Google Scholar]
- 4.Eng E, Young R. Lay health advisors as community change agents. Fam Community Health. 1992;15(1):24–40. doi: 10.1097/00003727-199204000-00005. [DOI] [Google Scholar]
- 5.Herman AA. Community health workers and integrated primary health care teams in the 21st century. J Ambul Care Manage. 2011;34(4):354–61. doi: 10.1097/JAC.0b013e31822cbcd0. [DOI] [PubMed] [Google Scholar]
- 6.Earp JA, Eng E, O'Malley MS, Altpeter M, Rauscher G, Mayne L, Mathews HF, Lynch KS, Qaqish B. Increasing use of mammography among older, rural African American women: results from a community trial. Am J Public Health. 2002;92(4):646–54. doi: 10.2105/AJPH.92.4.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kratzke C, Garzon L, Lombard J, Karlowicz K. Training community health workers: factors that influence mammography use. J Community Health. 2010;35(6):683–8. doi: 10.1007/s10900-010-9272-3. [DOI] [PubMed] [Google Scholar]
- 8.Legler J, Meissner HI, Coyne C, Breen N, Chollette V, Rimer BK. The effectiveness of interventions to promote mammography among women with historically lower rates of screening. Cancer Epidemiol Biomark Prev. 2002;11(1):59–71. [PubMed] [Google Scholar]
- 9.Paskett E, Tatum C, Rushing J, Michielutte R, Bell R, Foley KL, Bittoni M, Dickinson SL, McAlearney AS, Reeves K. Randomized trial of an intervention to improve mammography utilization among a triracial rural population of women. J Natl Cancer Inst. 2006;98(17):1226–37. doi: 10.1093/jnci/djj333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wadler BM, Judge CM, Prout M, Allen JD, Geller AC. Improving breast cancer control via the use of community health workers in South Africa: a critical review. J. Oncol. 2011; doi:10.1155/2011/150423. [DOI] [PMC free article] [PubMed]
- 11.Viswanathan M, Kraschnewski J, Nishikawa B, Morgan LC, Thieda P, Honeycutt A, Lohr KN, Jonas D. Outcomes of community health worker interventions. In. Rockville, MD: Agency for Healthcare Research and Quality; 2009. [PMC free article] [PubMed] [Google Scholar]
- 12.Margolis KL, Lurie N, McGovern PG, Tyrrell M, Slater JS. Increasing breast and cervical cancer screening in low-income women. J Gen Intern Med. 1998;13(8):515–21. doi: 10.1046/j.1525-1497.1998.00161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perry HB, Zulliger R, Rogers MM. Community health workers in low-, middle-, and high-income countries: an overview of their history, recent evolution, and current effectiveness. Annu Rev Public Health. 2014;35:399–421. doi: 10.1146/annurev-publhealth-032013-182354. [DOI] [PubMed] [Google Scholar]
- 14.Gibbons MC, Tyus NC. Systematic review of US-based randomized controlled trials using community health workers. Progress in community health partnerships: research, education, and action. 2007;1(4):371–81. doi: 10.1353/cpr.2007.0035. [DOI] [PubMed] [Google Scholar]
- 15.Swider SM. Outcome effectiveness of community health workers: an integrative literature review. Public Health Nurs. 2002;19(1):11–20. doi: 10.1046/j.1525-1446.2002.19003.x. [DOI] [PubMed] [Google Scholar]
- 16.Wells KJ, Luque JS, Miladinovic B, Vargas N, Asvat Y, Roetzheim RG, Kumar A. Do community health worker interventions improve rates of screening mammography in the United States? A systematic review. Cancer Epidemiol. Biomarkers Prev. 2011;20(8):1580–98. doi: 10.1158/1055-9965.EPI-11-0276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O’Brien MJ, Halbert CH, Bixby R, Pimentel S, Shea JA. Community health worker intervention to decrease cervical cancer disparities in Hispanic women. J Gen Intern Med. 2010;25(11):1186–92. doi: 10.1007/s11606-010-1434-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Russell KM, Champion VL, Monahan PO, Millon-Underwood S, Zhao Q, Spacey N, Rush NL, Paskett ED. Randomized trial of a lay health advisor and computer intervention to increase mammography screening in African American women. Cancer Epidemiol Biomark Prev. 2010;19(1):201–10. doi: 10.1158/1055-9965.EPI-09-0569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kiger H. Outreach to multiethnic, multicultural, and multilingual women for breast cancer and cervical cancer education and screening: a model using professional and volunteer staffing. Fam Community Health. 2003;26(4):307–18. doi: 10.1097/00003727-200310000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Erwin DO, Spatz TS, Stotts RC, Hollenberg JA. Increasing mammography practice by African American women. Cancer Pract. 1999;7(2):78–85. doi: 10.1046/j.1523-5394.1999.07204.x. [DOI] [PubMed] [Google Scholar]
- 21.Shelton RC, Goldman RE, Emmons KM, Sorensen G, Allen JD. An investigation into the social context of low-income, urban black and Latina women implications for adherence to recommended health behaviors. Health Educ Behav. 2011;38(5):471–81. doi: 10.1177/1090198110382502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American Cancer Society. Cancer facts and figures for African Americans. 2013-2014. Atlanta: American Cancer Society; 2013.
- 23.Erwin DO, Spatz TS, Stotts RC, Hollenberg JA, Deloney LA. Increasing mammography and breast self‐examination in African American women using the witness project™ model. J Cancer Educ. 1996;11(4):210–5. doi: 10.1080/08858199609528430. [DOI] [PubMed] [Google Scholar]
- 24.Erwin DO, Ivory J, Stayton C, Willis M, Jandorf L, Thompson H, Womack S, Hurd TC. Replication and dissemination of a cancer education model for African American women. Cancer Control. 2003;10(5):Suppl:13–21. doi: 10.1177/107327480301005s03. [DOI] [PubMed] [Google Scholar]
- 25.National Cancer Institute: The Witness Project. Products. http://rtips.cancer.gov/rtips/productDownloads.do?programId=270521. Accessed 15 Sep 2015.
- 26.Erwin DO. The Witness Project: narratives that shape the cancer experience for African American women. In: McMullin J, Weiner D, editors. In confronting cancer: metaphors, advocacy, and anthropology. Sante Fe, CA: School for Advanced Research Seminar Series; 2009. pp. 125–46. [Google Scholar]
- 27.Kreuter MW, Green MC, Cappella JN, Slater MD, Wise ME, Storey D, Clark EM, O’Keefe DJ, Erwin DO, Holmes K. Narrative communication in cancer prevention and control: a framework to guide research and application. Ann Behav Med. 2007;33(3):221–35. doi: 10.1007/BF02879904. [DOI] [PubMed] [Google Scholar]
- 28.Erwin DO. Cancer education takes on a spiritual focus for the African American faith community. J Cancer Educ. 2002;17(1):46–9. doi: 10.1080/08858190209528792. [DOI] [PubMed] [Google Scholar]
- 29.Hurd TC, Muti P, Erwin DO, Womack S. An evaluation of the integration of non-traditional learning tools into a community based breast and cervical cancer education program: the Witness Project of Buffalo. BMC Cancer. 2003;3(1):18. doi: 10.1186/1471-2407-3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bailey EJ, Erwin DO, Belin P. Using cultural beliefs and patterns to improve mammography utilization among African-American women: the Witness Project. J Natl Med Assoc. 2000;92(3):136. [PMC free article] [PubMed] [Google Scholar]
- 31.Lukwago SN, Kreuter MW, Bucholtz DC, Holt CL, Clark EM. Development and validation of brief scales to measure collectivism, religiosity, racial pride, and time orientation in urban African American women. Fam Community Health. 2001;24(3):63–71. doi: 10.1097/00003727-200110000-00008. [DOI] [PubMed] [Google Scholar]
- 32.Erwin DO, Spatz TS, Turturro CL. Development of an African‐American role model intervention to increase breast self‐examination and mammography. J Cancer Educ. 1992;7(4):311–9. doi: 10.1080/08858199209528188. [DOI] [PubMed] [Google Scholar]
- 33.Taylor RJ, Mattis J, Chatters LM. Subjective religiosity among African Americans: a synthesis of findings from five national samples. Journal of black psychology. 1999;25(4):524–43. doi: 10.1177/0095798499025004004. [DOI] [Google Scholar]
- 34.Scheirer MA, Dearing JW. An agenda for research on the sustainability of public health programs. Am J Public Health. 2011;101(11):2059. doi: 10.2105/AJPH.2011.300193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Twombly EC, Holtz KD, Stringer K. Using Promotores programs to improve Latino health outcomes: Implementation challenges for community-based nonprofit organizations. J Soc Serv Res. 2012;38(3):305–12. doi: 10.1080/01488376.2011.633804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Koskan A, Friedman DB, Messias DKH, Brandt HM, Walsemann K. Sustainability of promotora initiatives: program planners’ perspectives. J Public Health Manag Pract. 2013;19(5):E1–9. doi: 10.1097/PHH.0b013e318280012a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Koskan AM, Hilfinger Messias DK, Friedman DB, Brandt HM, Walsemann KM. Program planners’ perspectives of promotora roles, recruitment, and selection. Ethn Health. 2013;18(3):262–79. doi: 10.1080/13557858.2012.730605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Strachan DL, Källander K, ten Asbroek AH, Kirkwood B, Meek SR, Benton L, Conteh L, Tibenderana J, Hill Z. Interventions to improve motivation and retention of community health workers delivering integrated community case management (iCCM): stakeholder perceptions and priorities. AmJTrop Med Hyg. 2012;87(5):Suppl:111–9. doi: 10.4269/ajtmh.2012.12-0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alam K, Tasneem S, Oliveras E. Retention of female volunteer community health workers in Dhaka urban slums: a case-control study. Health Policy Plan. 2012;27:477–86. doi: 10.1093/heapol/czr059. [DOI] [PubMed] [Google Scholar]
- 40.Bhattacharyya K, Winch P, LeBan K, Tien M. Community health worker incentives and disincentives: how they affect motivation, retention and sustainability. Arlington, Virginia: USAID-BASICS II; 2001. [Google Scholar]
- 41.Alam K, Tasneem S, Oliveras E. Performance of female volunteer community health workers in Dhaka’s urban slums. A case control study. Dhaka: ICDDR, B.; 2011. [Google Scholar]
- 42.Aarons GA, Hurlburt M, Horwitz SM. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm Policy Ment Health Ment Health Serv Res. 2011;38(1):4–23. doi: 10.1007/s10488-010-0327-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kabwa P, Isoke B, Nyakahuma G. International Conference on AIDS. 1996. Factors affecting dropout rate of community volunteer AIDS educators; p. 189. [Google Scholar]
- 44.Yiu C, Au WT, Tang CS. Burnout and duration of service among Chinese voluntary workers. Asian J Soc Psychol. 2001;4(2):103–11. doi: 10.1111/j.1467-839X.2001.00079.x. [DOI] [Google Scholar]
- 45.Kkmoe M, Kalofonos I. Becoming and remaining community health workers: perspectives from Ethiopia and Mozambique. Soc Sci Med. 2013;87:52–9. doi: 10.1016/j.socscimed.2013.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gopalan SS, Mohanty S, Das A. Assessing community health workers’ performance motivation: a mixed-methods approach on India's Accredited Social Health Activists (ASHA) programme. BMJ open. 2012;2(5) doi: 10.1136/bmjopen-2012-001557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rahman SM, Ali NA, Jennings L, Seraji MHR, Mannan I, Shah R, Al-Mahmud AB, Bari S, Hossain D, Das MK. Research Factors affecting recruitment and retention of community health workers in a newborn care intervention in Bangladesh. Human Resource for Health. 2010;8(12):2–14. doi: 10.1186/1478-4491-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Khan SH, Chowdhury A, Karim F, Barua MK. Training and retaining Shasthyo Shebika: reasons for turnover of community health workers in Bangladesh. Health Care Manag. 1998;17(1):37–47. [PubMed] [Google Scholar]
- 49.Henderson LN, Tulloch J. Incentives for retaining and motivating health workers in Pacific and Asian countries. Hum Resour Health. 2008;6(1):18. doi: 10.1186/1478-4491-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rowe AK, de Savigny D, Lanata CF, Victora CG. How can we achieve and maintain high-quality performance of health workers in low-resource settings? Lancet. 2005;366(9490):1026–35. doi: 10.1016/S0140-6736(05)67028-6. [DOI] [PubMed] [Google Scholar]
- 51.Greenspan JA, McMahon SA, Chebet JJ, Mpunga M, Urassa DP, Winch PJ. Sources of community health worker motivation: a qualitative study in Morogoro Region. Tanzania Hum Resour Health. 2013;11(1):1–12. doi: 10.1186/1478-4491-11-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Calhoun A, Mainor A, Moreland-Russell S, Maier RC, Brossart L, Luke DA. Using the Program Sustainability Assessment Tool to assess and plan for sustainability. Prev Chronic Dis. 2014;11:130185. doi:10.5888/pcd11.130185. [DOI] [PMC free article] [PubMed]
- 53.Stirman SW, Kimberly J, Cook N, Calloway A, Castro F, Charns M. The sustainability of new programs and innovations: a review of the empirical literature and recommendations for future research. Implement Sci. 2012;7(17):1–19. doi: 10.1186/1748-5908-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sellers RM, Smith MA, Shelton JN, Rowley SA, Chavous TM. Multidimensional model of racial identity: a reconceptualization of African American racial identity. Personal Soc Psychol Rev. 1998;2(1):18–39. doi: 10.1207/s15327957pspr0201_2. [DOI] [PubMed] [Google Scholar]
- 55.Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005;61(7):1576–96. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 56.Cutrona CE, Russell DW. The provisions of social relationships and adaptation to stress. Greenwich, Connecticut: JAI Press; 1987. [Google Scholar]
- 57.Brown SL, Nesse RM, Vinokur AD, Smith DM. Providing social support may be more beneficial than receiving it results from a prospective study of mortality. Psychol Sci. 2003;14(4):320–7. doi: 10.1111/1467-9280.14461. [DOI] [PubMed] [Google Scholar]
- 58.Riessman F. The" helper" therapy principle. Social work. 1965;10(2):27-32.
- 59.Roman LA, Lindsay JK, Moore JS, Shoemaker AL. Community health workers: examining the helper therapy principle. Public Health Nurs. 1999;16(2):87–95. doi: 10.1046/j.1525-1446.1999.00087.x. [DOI] [PubMed] [Google Scholar]
- 60.Jaskiewicz W, Tulenko K. Increasing community health worker productivity and effectiveness: a review of the influence of the work environment. Hum Resour Health. 2012;10(1):38. doi: 10.1186/1478-4491-10-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Haines A, Sanders D, Lehmann U, Rowe AK, Lawn JE, Jan S, Walker DG, Bhutta Z. Achieving child survival goals: potential contribution of community health workers. Lancet. 2007;369(9579):2121–31. doi: 10.1016/S0140-6736(07)60325-0. [DOI] [PubMed] [Google Scholar]
- 62.Latham GP, Pinder CC. Work motivation theory and research at the dawn of the twenty-first century. Annu Rev Psychol. 2005;56:485–516. doi: 10.1146/annurev.psych.55.090902.142105. [DOI] [PubMed] [Google Scholar]
- 63.Mueller D, Kurowski C, Mills A. Managing health workforce performance. Component-literature review: determinants and levers of health worker motivation and satisfaction. London School of Hygiene and Tropical Medicine.: Health Economics and Financing Program London; 2005. [Google Scholar]
- 64.Deci EL, Ryan RM. The" what" and" why" of goal pursuits: human needs and the self-determination of behavior. Psychol Inq. 2000;11(4):227–68. doi: 10.1207/S15327965PLI1104_01. [DOI] [Google Scholar]
- 65.Scheier MF, Wrosch C, Baum A, Cohen S, Martire LM, Matthews KA, Schulz R, Zdaniuk B. The life engagement test: assessing purpose in life. J Behav Med. 2006;29(3):291–8. doi: 10.1007/s10865-005-9044-1. [DOI] [PubMed] [Google Scholar]
- 66.Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- 67.Idler EL, Angel RJ. Self-rated health and mortality in the NHANES-I Epidemiologic Follow-up Study. Am J Public Health. 1990;80(4):446–52. doi: 10.2105/AJPH.80.4.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Thompson HS, Valdimarsdottir HB, Winkel G, Jandorf L, Redd W. The Group-Based Medical Mistrust Scale: psychometric properties and association with breast cancer screening. Prev Med. 2004;38(2):209–18. doi: 10.1016/j.ypmed.2003.09.041. [DOI] [PubMed] [Google Scholar]
- 69.Cohen S, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM. Social ties and susceptibility to the common cold. JAMA. 1997;277(24):1940–4. doi: 10.1001/jama.1997.03540480040036. [DOI] [PubMed] [Google Scholar]
- 70.Zimmerman MA, Zahniser JH. Refinements of sphere-specific measures of perceived control: development of a sociopolitical control scale. J Community Psychol. 1991;19(2):189–204. doi: 10.1002/1520-6629(199104)19:2<189::AID-JCOP2290190210>3.0.CO;2-6. [DOI] [Google Scholar]
- 71.Schriesheim C, Tsui AS. Development and validation of a short satisfaction instrument for use in survey feedback interventions. In: Western Academy of Management Meeting: 1980; 1980;115-17
- 72.David F, Chin F. An analysis of the determinants of family planning volunteer workers performance in Iloilo City. Philippine population journal. 1993;9(1-4):12–25. [PubMed] [Google Scholar]
- 73.Smith SA, Blumenthal DS. Community health workers support community-based participatory research ethics: lessons learned along the research-to-practice-to-community continuum. J Health Care Poor Underserved. 2012;23(4):77. doi: 10.1353/hpu.2012.0156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Otiniano AD, Carroll-Scott A, Toy P, Wallace SP. Supporting Latino communities’ natural helpers: a case study of promotoras in a research capacity building course. J Immigr Minor Health. 2012;14(4):657–63. doi: 10.1007/s10903-011-9519-9. [DOI] [PubMed] [Google Scholar]
- 75.Rahman M, Tasneem S. Determinants of income of the Shasthya Shebikas: evidences from a pilot MNCH initiative in the Nilphamari district of Bangladesh: BRAC Research & Evaluation Division. 2008. [Google Scholar]
- 76.Erwin DO, Johnson VA, Trevino M, Duke K, Feliciano L, Jandorf L. A comparison of African American and Latina social networks as indicators for culturally tailoring a breast and cervical cancer education intervention. Cancer. 2007;109(S2):368–77. doi: 10.1002/cncr.22356. [DOI] [PubMed] [Google Scholar]
- 77.Maes KC, Kohrt BA, Closser S. Culture, status and context in community health worker pay: pitfalls and opportunities for policy research. A commentary on Glenton et al. (2010) Soc Sci Med. 2010;71(8):1375–8. doi: 10.1016/j.socscimed.2010.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cherrington A, Ayala GX, Elder JP, Arredondo EM, Fouad M, Scarinci I. Recognizing the diverse roles of community health workers in the elimination of health disparities: from paid staff to volunteers. Ethn Dis. 2010;20(2):189. [PMC free article] [PubMed] [Google Scholar]
- 79.Ingram M, Reinschmidt KM, Schachter KA, Davidson CL, Sabo SJ, De Zapien JG, Carvajal SC. Establishing a professional profile of community health workers: results from a national study of roles, activities and training. J Community Health. 2012;37(2):529–37. doi: 10.1007/s10900-011-9475-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.111th United States Congress. The Patient Protection and Affordable Care Act, Public Law 111-148. Washington, DC; 2010:516-18. https://www.gpo.gov/fdsys/pkg/PLAW-111publ148/html/PLAW-111publ148.htm.
- 81.Community Health Worker Opportunities and the Affordable Care Act (ACA). http://www.urban.org/sites/default/files/alfresco/publication-pdfs/413071-Opportunities-for-Community-Health-Workers-in-the-Era-of-Health-Reform.PDF.
- 82.Katzen A, Morgan M. Affordable Care Act Opportunities for Community Health Workers. In. Cambridge, MA: Center for Health Law & Policy Innovation, Harvard Law School; 2014. [Google Scholar]
- 83.Glenton C, Scheel IB, Pradhan S, Lewin S, Hodgins S, Shrestha V. The female community health volunteer programme in Nepal: decision makers’ perceptions of volunteerism, payment and other incentives. Soc Sci Med. 2010;70(12):1920–7. doi: 10.1016/j.socscimed.2010.02.034. [DOI] [PubMed] [Google Scholar]
- 84.Kironde S, Klaasen S. What motivates lay volunteers in high burden but resource-limited tuberculosis control programmes? Perceptions from the Northern Cape province, South Africa. Int J Tuberc Lung Dis. 2002;6(2):104–10. [PubMed] [Google Scholar]
- 85.Willis-Shattuck M, Bidwell P, Thomas S, Wyness L, Blaauw D, Ditlopo P. Motivation and retention of health workers in developing countries: a systematic review. BMC Health Serv Res. 2008;8(1):247. doi: 10.1186/1472-6963-8-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Carter-Pokras OD, Jaschek G, Martinez IL, Brown PB, Mora SE, Newton N, Luciani I. Perspectives on Latino lay health promoter programs: Maryland, 2009. Am J Public Health. 2011;101(12):2281–6. doi: 10.2105/AJPH.2011.300317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Guinan JJ, McCallum L, Painter L, Dykes J, Gold J. Stressors and rewards of being an AIDS emotional-support volunteer: a scale for use by care-givers for people with AIDS. AIDS Care. 1991;3(2):137–50. doi: 10.1080/09540129108253056. [DOI] [PubMed] [Google Scholar]
- 88.Goodman RM. A construct for building the capacity of community-based initiatives in racial and ethnic communities: a qualitative cross-case analysis. J Public Health Manag Pract. 2009;15(2):E1–8. doi: 10.1097/01.PHH.0000346019.12641.1f. [DOI] [PubMed] [Google Scholar]


