Abstract
Background
Atrial fibrillation (AF) is a common cardiac arrhythmia and increases risk of ischemic stroke. Data on the prevalence of AF in Thailand is lacking especially in patients with hypertension. The objectives of this study were to determine prevalence of AF in patients with hypertension and to determine factors that are associated with increased prevalence of AF in a multicenter nationwide study.
Methods
A cross-sectional survey for the national outcome evaluation among hypertensive patients visiting 831 public hospitals in Thailand was conducted between 2011 and 2012 to evaluate status of standard care in hypertensive patients visiting public Thailand Ministry of Public Health (MoPH) hospitals. Inclusion criteria were hypertensive patients aged at least 20 years who had received medical care in the targeted hospital for at least 12 months. The main outcome measurement was AF rhythm, and was measured along with potential risk factors age, gender and cardiovascular risk factors.
Results
There were 13207 hypertensive patients who had ECG data recorded during the survey. AF was detected in 457 patients (3.46 %). Prevalence of AF increased with increasing age, was more common in males and in patients with chronic kidney disease (CKD). Multivariable modelling was conducted to assess which factors were most associated with increased prevalence of AF, and the results showed older age followed by male gender, low LDL-cholesterol and increased uric acid levels were the most important risk factors for AF in this population.
Conclusions
Prevalence of AF in hypertensive patients was 3.46 %. Factors associated with increased risk of AF are old age, male gender, low LDL-cholesterol and elevated uric acid level.
Keywords: Atrial fibrillation, Prevalence, Hypertension
Background
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia [1, 2]. The prevalence and incidence increases with age and is more prevalent in men than women [2]. It is estimated that the prevalence of AF is approximately 1–2 % [3]. Prevalence of AF in Asian countries has been reported to be slightly lower than in western populations [4–6]. However, due to the much larger population size of Asia, the burden of AF has been estimated to be much larger in the Asian population compared to western countries. It is estimated that approximately 49 million men and 23 million women in Asia will suffer from AF in 2050 [7]. This number is roughly 12 times more than current estimates in United States [8]. AF may be classified as valvular and non-valvular in origin. Majority of AF are non-valvular etiology [3]. Prevalence of AF increases in patients with certain risk factors such as hypertension [9, 10]. Hypertension increases risk of AF by approximately 1.5 fold in both men and women and is likely to be the most important risk factor for developing AF [11].
Non-valvular AF is an important cause of ischemic stroke both in western and Asian population [5, 12]. The annual incidence of ischemic stroke in patients with non-valvular AF has been reported to be around 5 % [5, 12]. There are many risk factors for ischemic stroke in patients with non-valvular AF such as diabetes mellitus, systemic hypertension, old age, heart failure or left ventricular dysfunction, along with a history of ischemic stroke or transient ischemic attack (TIA) [6, 9, 10].
Prevalence of AF in Asian population has been reported from many countries such as China [5, 13], Japan [14], Korea [15], Taiwan [5], and Singapore [16]. There are limited data for the prevalence of AF in Thailand, both in the general population and in patients with risk factors such as hypertension. We sought to determine the prevalence of AF in patients with hypertension among a large nationwide cross-sectional study in patients with hypertension. Secondary objectives of this study were 1) to determine the prevalence of AF in patients with hypertension stratified by age and gender and 2) to determine factors associated with AF.
Methods
Study population
A cross-sectional survey for the national outcome evaluation among hypertensive patients visiting public hospitals in Thailand was conducted between 2011 and 2012 to evaluate status of standard care in hypertensive patients visiting public Thailand Ministry of Public Health (MoPH) hospitals in Thailand including private clinics in the Thailand National Health Security Office (NHSO)’s program in Bangkok. Inclusion criteria for the present study were hypertensive patients aged at least 20 years old who received medical care in the participating hospital for the previous 12 months. Patients participating in clinical trials were excluded.
A two-stage stratified cluster, proportional to the size sampling technique was used to select a nationally and provincially representative sample of hypertensive patients in Thailand. For every province outside Bangkok, the targeted hospital included all hospitals that were public hospitals under the MoPH. For Bangkok, the targeted hospital included all hospitals and clinics participating in the Thailand NHSO’s program. The first stage of sampling was at the province level representing 77 strata, and the second stage of sampling was the level of hospital in each province in Thailand. Hospitals in each province were stratified into 5 strata by their sizes i.e., regional center hospital (>500 beds), provincial general hospital (200 – 500 beds), large community hospital (90 – 120 beds), medium community hospital (60 beds), and small community hospital (10 – 30 beds). All university hospitals were excluded from our study.
The study was approved by the Ethical Review Committee for Research in Human Subjects, Thailand Ministry of Public Health, and the Royal Thai Army Medical Department Ethical Review Board as well as local institutional review boards of the participating hospitals. Written informed consent was obtained prior to participation.
Data collection
There were a total of 831 hospitals under the Thai universal coverage scheme: 25 regional hospitals, 70 general hospitals and 736 community hospitals. All regional and general hospitals were selected as well as 70 % of small community hospital, 20 % of medium size community hospital and 10 % of large community hospital. This faction was based on the proportion of patient care undertaken at the various levels of hospitals. Patients with diagnosis of hypertension were randomly selected according to the proportion of patients registered at each hospital. Sample size of study population was calculated from the proportion to size model for each province.
Data were retrieved from patients’ medical records and included baseline information, status of hypertensive complication, and results of laboratory tests.
Measurements
Collected variables were demographic data, weight, height, body mass index (BMI), systolic blood pressure (SBP), diastolic blood pressure (DBP), cardiovascular risk factors, blood chemistry data including fasting plasma glucose (FPG), serum creatinine, uric acid, lipid profiles, available ECG data and results, and complication related to hypertension including stroke. Glomerular filtration rate (GFR) was calculated from epidemiology collaboration formula (EPI). Stroke was classified as ischemic stroke, TIA, unspecified stroke, hemorrhagic stroke.
Data management team sent query to study site to verify data if needed. Data and site monitoring was performed in 10 % of study site or approximately 60 hospitals by a random selection process.
ECG is not a prerequisite for the main study. It was noted in the case record form (CRF) whether there were ECG data in the medical record. For those who had ECG, results of the ECG interpretation were recorded. Cardiac rhythm was noted for the presence or absence of AF.
Main outcome measurements include AF rhythm and factors that might be related to AF such as age, gender, cardiovascular risk factors.
Statistical analysis
Continuous data were presented as mean and standard deviation while categorical variables were presented as number and percentages. Prevalence data was reported as percentage and 95 % confidence interval. Comparisons of continuous data were made by an independent sample t-test. For categorical variables, comparisons were made by the chi-square test. Continuous data were grouped for the analysis of Odds ratio as follows; age ≥ 65 years, SBP ≥ 140 mmHg, DBP ≥ 90 mmHg, TC ≥ 200 mg/dl, TG ≥ 200 mg/dl, HDL < 40 mg/dl, LDL ≥ 100 mg/dl, BMI ≥ 25 kg/m2, GFR < 60 ml/min, uric acid ≥ 7 mg/dl in male and ≥ 6 mg/dl in female. Odds ratio and 95 % confidence interval (CI) for univariate analysis were made by the Likelihood ratio test. Multivariate logistic regression analysis (with forward LR) was performed to determine the independent factors associated with increased risk of AF using complete-cases analysis and imputation method for the missing data. Missing values were imputed based on the means of complete cases with noise added based on the t-distribution. A p-value less than 0.05 was considered significant. Statistical analysis was performed with SPSS version 20.
Results
There were a total of 71440 with hypertension enrolled in the main study during 2011–2012. ECG was performed in 13207 patients (18.5 %). Average age was 63.6 ± 11.1 years, 4711 (35.7 %) were male. Baseline variables between patients with and without ECG were numerically similar for SBP (130.8 ± 16.3 vs 129.9 ± 16.0 mmHg), DBP (75.0 ± 10.8 vs 75.4 ± 10.5 mmHg), FPG (116.2 ± 40.4 vs 120.3 ± 43.1 mg/dl), serum creatinine (1.17 ± 0.87 vs 1.17 ± 1.10 mg/dl), total cholesterol (190.7 ± 44.1 vs 192.5 ± 44.2 mg/dl), triglyceride (158.2 ± 92.8 vs 163.7 ± 100.4 mg/dl), HDL-cholesterol (47.8 ± 13.7 vs 48.0 ± 14.3 mg/dl) and LDL-cholesterol (113.5 ± 37.4 vs 114.2 ± 37.3 mg/dl) with a slightly older age for patients who had ECG (63.6 ± 11.1 vs 61.1 ± 11.2 years) and greater proportion of male (35.7 vs 33.7 %).
Among 13207 patients with available ECG, AF was detected in 457 patients (3.46 %, 95 % CI 3.16-3.79). Baseline characteristics between patients with and without AF are shown in Table 1. Prevalence of AF increased with increasing age, more common in male and in patients with chronic kidney disease (CKD). Figure 1 showed the bar graph of prevalence of AF for every 10-year of age and separate between men and women. Since the increased prevalence of AF in males was evident only until the 7th decade of life and the prevalence in individuals ≥ 70 years was roughly the same in men and women, we performed additional analysis for interaction between age and gender on the prevalence of AF. The results showed that there was a significant interaction (p for interaction test <0.001) between age and gender on the association of AF.
Table 1.
Baseline characteristics of patients (total number of subjects = 13207)
| Baseline variables | n | Mean ± SD or number (%) |
|---|---|---|
| Age | 13207 | 63.6 ± 11.1 |
| Gender | 13207 | |
| Male | 4711 (35.7) | |
| Female | 8796 (64.3) | |
| Current smoker | 13207 | |
| yes | 750 (5.7) | |
| no | 12457 (94.3) | |
| Type of hospital | 12800 | |
| Urban | 5258 (41.1) | |
| Community | 7542 (58.9) | |
| DM | 13207 | |
| yes | 3653 (27.7) | |
| no | 9554 (72.3) | |
| SBP | 13197 | 130.8 ± 16.3 |
| DBP | 13186 | 75.0 ± 10.8 |
| TC | 11635 | 190.7 ± 44.1 |
| TG | 11882 | 158.2 ± 92.8 |
| HDL | 11268 | 47.8 ± 13.7 |
| LDL | 11536 | 113.5 ± 37.4 |
| BMI | 11865 | 25.2 ± 4.49 |
| GFR_EPI | 12248 | 66.7 ± 23.9 |
| Uric acid | 5392 | 6.15 ± 1.95 |
SD standard deviation, DM diabetes mellitus, SBP systolic blood pressure, DBP diastolic blood pressure, TC total cholesterol, TG triglyceride, HDL high density lipoprotein cholesterol, LDL low density lipoprotein cholesterol, BMI body mass index, GFR_EPI glomerular filtration rate by epidemiology collaboration formula
Fig. 1.
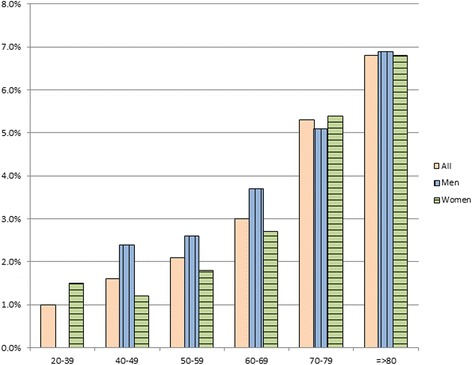
Prevalence of AF in men and women at different age groups
We did not collect the data on antihypertensive medications except for angiotensin converting enzyme inhibitor (ACEI) or angiotensin receptor blocker (ARB) due to the special interest on the use of this drug group in Asian population. ACEI or ARB was prescribed in 2838 patients (21.5 %). There was no significant association between ACEI or ARB and AF (prevalence of AF was 3.0 % in patients with ACEI or ARB and 3.6 % in those without, p = 0.157).
Figure 2 showed bivariate analysis of demographic data, and cardiovascular risk factors in relation to the prevalence of AF including Odds ratio and 95 % CI. Factors that were associated with increased risk of AF at the p value < 0.10 from univariate analysis were old age, male gender, high diastolic blood pressure, low total cholesterol or LDL-cholesterol, normal BMI, impaired renal function, and high uric acid levels. Multivariate analysis of factors that were associated with increased prevalence of AF was performed and the results revealed that the strongest association was old age followed by male gender, low LDL-cholesterol and increased uric acid levels (Table 2).
Fig. 2.
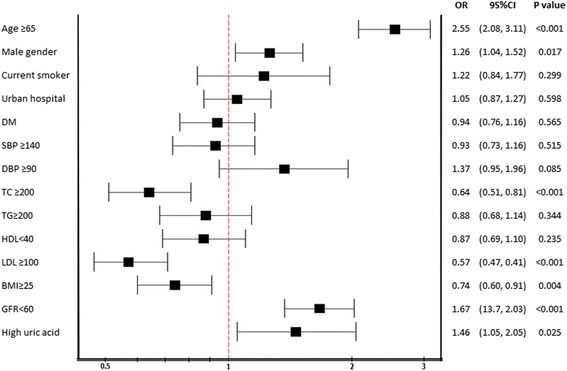
Bivariate analysis factors affecting AF
Table 2.
Multivariate analysis of factors that had independent association with AF along with the prevalence of AF for complete cases
| Factors | %AF | ORcrude | ORadj | 95 % CI | OR(IMP) | 95%CI |
|---|---|---|---|---|---|---|
| Age ≥65 years | 4.1 | 2.55*** | 2.86*** | 1.89–4.33 | 2.44*** | 1.99–2.98 |
| Male gender | 3.6 | 1.26* | 1.98** | 1.35–2.91 | 0.86 | 0.71–1.04 |
| LDL <100 mg/dl | 4.0 | 1.74*** | 1.87** | 1.28–2.73 | 1.62*** | 1.32–1.96 |
| High uric acid level | 3.2 | 1.46* | 1.48* | 1.02–2.17 | 1.26* | 1.04–1.51 |
*p < 0.05, **p < 0.01, ***p < 0.001
OR adj odds ratio after adjusting for potential confounders, OR(IMP) odds ratio after imputating missing data, CI confidence interval, LDL low density lipoprotein cholesterol
Since a number of patients had missing values for uric acid. This may have decreased the statistical power of the complete-cases analysis. We subsequently applied imputations to handle the missing value and the results of the multivariate analysis after imputation showed that three of the four original independent associations with AF remained significant (Table 2).
Table 3 showed the relationship between number of these 4 factors and the Odds and 95 % CI of AF. The Odds of AF increased from 1.64 in patients with only 1 association factor to 8.99 for those with all 4 factors compared to those without any of these 4 factors.
Table 3.
Relationship between numbers of independent factors associated with atrial fibrillation and Odds of having atrial fibrillation. Patient without any of these 4 factors were treated as the reference group
| Number of factors associated with AF | OR | 95 % CI | P value |
|---|---|---|---|
| 0 | reference | ||
| 1 | 1.64 | 1.07–2.51 | 0.022 |
| 2 | 2.46 | 1.66–3.63 | <0.001 |
| 3 | 4.30 | 2.90–6.38 | <0.001 |
| 4 | 8.99 | 5.02–16.07 | <0.001 |
AF atrial fibrillation, OR Odds ratio, CI confidence interval
We also collected the data on the history of ischemic stroke. The prevalence of previous ischemic stroke in this study was 3.8 %. AF was a significant and independent factor associated with ischemic stroke with the OR and 95 % CI of 2.32 (1.64–3.29).
Discussion
Our study showed that prevalence of AF in Thai population with hypertension was 3.46 %. The prevalence increased in male, elderly, low LDL-cholesterol and high uric acid levels. This is the first report of prevalence of AF in Thai population based on a nationally representative sample. Our study was systematically conducted and employed stratified cluster sampling based on population and hospital size.
AF represents a large burden to the population mainly due to the embolic complication [17]. Ischemic stroke related to AF has been reported to be more disabling than stroke not related to AF [18]. It is one of the most common sustained arrhythmias and more common in the elderly population [1, 2]. Stroke prophylaxis strategies have been shown to be very cost effective [19] although the treatment might cause major bleeding and intracranial bleeding. Anticoagulation is recommended in patients with AF and at least one risk factor [3].
Previous reports indicate that prevalence of AF in western populations is generally greater than Asian populations [4, 6]. There was no clear explanation for this but it could be related to genetic predisposition reported by previous studies on specific polymorphisms that related to AF [20, 21]. We aimed to study prevalence of AF in the Thai hypertensive population since hypertension is a common cardiovascular risk factor and predisposes individuals to AF [11]. Anticoagulant to prevent stroke is recommended in AF patients in the setting of hypertension [3, 18]. Therefore, prevalence of AF in our study may represent an over-estimate in general population, but is likely to be a valid estimate for the Thai hypertensive population. Prevalence of AF in our study was 3.46 % which is greater than 1.21 % and 1.3 % prevalence of AF in general population in Thailand [22, 23], 0.65 % for China [24], 0.56 % for Japan [25] and 0.95 % and 1.2 % prevalence of AF in the United States and United Kingdom [8, 26]. However, our results are comparable with those from a study conducted by Davies and colleagues which reported the prevalence of 5.1 % in male and 2.6 % in female [27].
Univariate analysis of our study showed that factors associated with AF were old age, male gender, low total cholesterol or LDL-cholesterol, normal BMI, impaired renal function, and high uric acid levels. However, after adjusting for confounding, only old age, male gender, low LDL-cholesterol and high uric acid levels remained significantly associated with AF, with elderly as the important factor. Prevalence of AF increases with age due to degenerative process of the atrial muscle and conducting cells [2, 28]. The results of our study are similar with those conducted on both western and other Asian populations [6]. The finding on more predominance in males is also consistent with previous reports [8, 29]. We noticed a significant interaction of age and gender on the prevalence of AF. Male gender was more likely to have AF compared to female in the age group less than 70 years but no such association after the age of 70. This finding was not found in previous reports from Europe [29] and United States [8]. However, similar interaction has been reported from Taiwan [5]. Therefore, the effect of male gender on the increased prevalence of AF in Asian population may disappear after the age of 70 years. Renal impairment has been reported as a risk factor in some previous studies [14, 30]. From our study, however, although renal impairment was associated with AF at the crude level, it did not remain significant when adjusting for other covariates.
We do not have a clear explanation why AF was related to low LDL-cholesterol in our study. Studies about the impact of Hyperlipidemia on AF show mixed results. Indeed, some reports indicate that hyperlipidemic patients have a lower risk of AF [14, 31], as in our study. However, another study showed that hyperlipidemia had a higher risk of AF [24]. The relationship between AF and low LDL-cholesterol in our study should be interpreted with caution due to the cross-sectional nature of our study. It is possible that patients with AF may have dyslipidemia, and treatment with statins was not recorded in our dataset.
For the association we identified between AF and hyperuricemia, there have been few studies to support our findings. Although, some previous studies showed that hyperuricemia is an independent risk factor for AF [32, 33]. It is postulated that hyperuricemia can have effect on the inflammatory and fibrotic process [34] leading to an increased atrial size and eventually AF [32] which may occur with or without a preceding inflammatory process. Some studies showed that treatment of hyperuricemia can prevent inflammatory and fibrosis formation in certain disease such as pericarditis [35, 36].
Results of our study have some clinical implications. Our main objective was to get an accurate estimate of prevalence of AF in hypertensive population. Our prevalence estimate 3.46 % AF in the hypertensive population is high considering the malignant course of this disease that might cause a serious thromboembolic stroke. We demonstrate that there are other factors that could even further increase the prevalence of AF with odds ratio as high as 20 for certain combinations of the associated factors. For example, males older than 65 years of age with an LDL less than 100 mg/dl and elevated uric acid have a very high risk of AF. Regular monitoring with ECG or teaching patients to feel the regularity of their pulse should be considered in practice guideline [3]. Such an approach may help reduce the number of serious strokes related to AF by giving stroke prophylaxis treatment.
There were some limitations of our study. First, this study did not initially plan to study ECG finding, and collection of ECG data was incidental (if it was contained in a patient’s medical record) and only 18.5 % of patients had ECG data. Due to a slightly higher proportion of males and a marginally older sample patient with ECG, compared with those without ECG, the prevalence of AF of 3.46 % may represent an overestimate of prevalence in the Thai hypertensive population. If we adjust for the small difference in age and gender between patients with and without ECG, the prevalence of AF for the whole population (with and without ECG) would be 3.3 % if adjusting for gender, 3.28 % if adjusting for age, and 3.15 % if adjusting for both factors. Secondly, this study did not have data on medications such as antihypertensive medications, antithrombotic medication and statins. Lastly, this study is a cross-sectional study, not a cohort study, so factors associated with AF cannot be concluded to represent risk factors, only factors associated with AF. However, the main strength of this study is that this is s nationwide study and probable one of the first in Southeast Asia region.
Conclusions
In conclusion, prevalence of AF in hypertensive population in our study was 3.46 % which is higher than prevalence of AF in the general community setting considered in most previous reports. The results from our study are useful for future study of the management of AF.
Availability of data and materials
The dataset supporting the conclusions of this article is available in http://www.damus.in.th.
Abbreviations
- AF
atrial fibrillation
- BMI
body mass index
- CI
confidence interval
- CKD
chronic kidney disease
- CRF
case record form
- DBP
diastolic blood pressure
- ECG
electrocardiogram
- EPI
epidemiology collaboration formula
- FPG
fasting plasma glucose
- GFR
glomerular filtration rate
- HDL
high density lipoprotein
- LDL
low density lipoprotein
- MoPH
ministry of public health
- NHSO
national health security office
- SBP
systolic blood pressure
- TIA
transient ischemic attack
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
RK, RR and SR participated in conception and design, BT, NS, CH and AY performed statistical analysis, RK and CH drafted the manuscript. All authors read and approved the final manuscript.
References
- 1.Nguyen TN, Hilmer SN, Cumming RG. Review of epidemiology and management of atrial fibrillation in developing countries. Int J Cardiol. 2013;167:2412–20. doi: 10.1016/j.ijcard.2013.01.184. [DOI] [PubMed] [Google Scholar]
- 2.Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna WP, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006;114:119–25. doi: 10.1161/CIRCULATIONAHA.105.595140. [DOI] [PubMed] [Google Scholar]
- 3.Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012;33:2719–47. doi: 10.1093/eurheartj/ehs253. [DOI] [PubMed] [Google Scholar]
- 4.Chiang CE, Zhang S, Tse HF, Teo WS, Omar R, Sriratanasathavorn C. Atrial fibrillation management in Asia: from the Asian expert forum on atrial fibrillation. Int J Cardiol. 2013;164:21–32. doi: 10.1016/j.ijcard.2011.12.033. [DOI] [PubMed] [Google Scholar]
- 5.Chien KL, Su TC, Hsu HC, Chang WT, Chen PC, Chen MF, et al. Atrial fibrillation prevalence, incidence and risk of stroke and all-cause death among Chinese. Int J Cardiol. 2010;139:173–80. doi: 10.1016/j.ijcard.2008.10.045. [DOI] [PubMed] [Google Scholar]
- 6.Tse HF, Wang YJ, Ahmed Ai-Abdullah M, Pizarro-Borromeo AB, Chiang CE, Krittayaphong R, et al. Stroke prevention in atrial fibrillation--an Asian stroke perspective. Heart Rhythm. 2013;10:1082–8. doi: 10.1016/j.hrthm.2013.03.017. [DOI] [PubMed] [Google Scholar]
- 7.United Nations Department of Economic and Social Affairs PD. World Population Prospects. New York; 2011 [05.01.12]; Available from: http://esa.un.org/unpd/wpp/unpp/panel_population.htm.
- 8.Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285:2370–5. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 9.Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285:2864–70. doi: 10.1001/jama.285.22.2864. [DOI] [PubMed] [Google Scholar]
- 10.Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137:263–72. doi: 10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- 11.Benjamin EJ, Levy D, Vaziri SM, D'Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994;271:840–4. doi: 10.1001/jama.1994.03510350050036. [DOI] [PubMed] [Google Scholar]
- 12.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983–8. doi: 10.1161/01.STR.22.8.983. [DOI] [PubMed] [Google Scholar]
- 13.Long MJ, Jiang CQ, Lam TH, Xu L, Zhang WS, Lin JM, et al. Atrial fibrillation and obesity among older Chinese: the Guangzhou Biobank Cohort Study. Int J Cardiol. 2011;148:48–52. doi: 10.1016/j.ijcard.2009.10.022. [DOI] [PubMed] [Google Scholar]
- 14.Iguchi Y, Kimura K, Shibazaki K, Aoki J, Kobayashi K, Sakai K, et al. Annual incidence of atrial fibrillation and related factors in adults. Am J Cardiol. 2010;106:1129–33. doi: 10.1016/j.amjcard.2010.06.030. [DOI] [PubMed] [Google Scholar]
- 15.Jeong JH. Prevalence of and risk factors for atrial fibrillation in Korean adults older than 40 years. J Korean Med Sci. 2005;20:26–30. doi: 10.3346/jkms.2005.20.1.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yap KB, Ng TP, Ong HY. Low prevalence of atrial fibrillation in community-dwelling Chinese aged 55 years or older in Singapore: a population-based study. J Electrocardiol. 2008;41:94–8. doi: 10.1016/j.jelectrocard.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 17.Ghatnekar O, Glader EL. The effect of atrial fibrillation on stroke-related inpatient costs in Sweden: a 3-year analysis of registry incidence data from 2001. Value Health. 2008;11:862–8. doi: 10.1111/j.1524-4733.2008.00359.x. [DOI] [PubMed] [Google Scholar]
- 18.Marini C, De Santis F, Sacco S, Russo T, Olivieri L, Totaro R, et al. Contribution of atrial fibrillation to incidence and outcome of ischemic stroke: results from a population-based study. Stroke. 2005;36:1115–9. doi: 10.1161/01.STR.0000166053.83476.4a. [DOI] [PubMed] [Google Scholar]
- 19.Vestergaard AS, Ehlers LH. A Health Economic Evaluation of Stroke Prevention in Atrial Fibrillation: Guideline Adherence Versus the Observed Treatment Strategy Prior to 2012 in Denmark. Pharmacoeconomics. 2015. [DOI] [PubMed]
- 20.Smith JG, Newton-Cheh C, Almgren P, Melander O, Platonov PG. Genetic polymorphisms for estimating risk of atrial fibrillation in the general population: a prospective study. Arch Intern Med. 2012;172:742–4. doi: 10.1001/archinternmed.2012.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Everett BM, Cook NR, Conen D, Chasman DI, Ridker PM, Albert CM. Novel genetic markers improve measures of atrial fibrillation risk prediction. Eur Heart J. 2013;34:2243–51. doi: 10.1093/eurheartj/eht033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kiatchoosakun S, Pachirat O, Chirawatkul A, Choprapawan C, Tatsanavivat P. Prevalence of cardiac arrhythmias in Thai community. J Med Assoc Thai. 1999;82:727–33. [PubMed] [Google Scholar]
- 23.Assantachai P, Panchavinnin P, Pisalsarakij D. An electrocardiographic survey of elderly Thai people in the rural community. J Med Assoc Thai. 2002;85:1273–9. [PubMed] [Google Scholar]
- 24.Zhou Z, Hu D. An epidemiological study on the prevalence of atrial fibrillation in the Chinese population of mainland China. J Epidemiol. 2008;18:209–16. doi: 10.2188/jea.JE2008021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Inoue H, Fujiki A, Origasa H, Ogawa S, Okumura K, Kubota I, et al. Prevalence of atrial fibrillation in the general population of Japan: an analysis based on periodic health examination. Int J Cardiol. 2009;137:102–7. doi: 10.1016/j.ijcard.2008.06.029. [DOI] [PubMed] [Google Scholar]
- 26.Majeed A, Moser K, Carroll K. Trends in the prevalence and management of atrial fibrillation in general practice in England and Wales, 1994–1998: analysis of data from the general practice research database. Heart. 2001;86:284–8. doi: 10.1136/heart.86.3.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Davis RC, Hobbs FD, Kenkre JE, Roalfe AK, Iles R, Lip GY, et al. Prevalence of atrial fibrillation in the general population and in high-risk groups: the ECHOES study. Europace. 2012;14:1553–9. doi: 10.1093/europace/eus087. [DOI] [PubMed] [Google Scholar]
- 28.Burstein B, Nattel S. Atrial fibrosis: mechanisms and clinical relevance in atrial fibrillation. J Am Coll Cardiol. 2008;51:802–9. doi: 10.1016/j.jacc.2007.09.064. [DOI] [PubMed] [Google Scholar]
- 29.Heeringa J, van der Kuip DA, Hofman A, Kors JA, van Herpen G, Stricker BH, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J. 2006;27:949–53. doi: 10.1093/eurheartj/ehi825. [DOI] [PubMed] [Google Scholar]
- 30.Alonso A, Lopez FL, Matsushita K, Loehr LR, Agarwal SK, Chen LY, et al. Chronic kidney disease is associated with the incidence of atrial fibrillation: the Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2011;123:2946–53. doi: 10.1161/CIRCULATIONAHA.111.020982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang S. Atrial fibrillation in mainland China: epidemiology and current management. Heart. 2009;95:1052–5. doi: 10.1136/hrt.2008.146589. [DOI] [PubMed] [Google Scholar]
- 32.Chao TF, Hung CL, Chen SJ, Wang KL, Chen TJ, Lin YJ, et al. The association between hyperuricemia, left atrial size and new-onset atrial fibrillation. Int J Cardiol. 2013;168:4027–32. doi: 10.1016/j.ijcard.2013.06.067. [DOI] [PubMed] [Google Scholar]
- 33.Valbusa F, Bertolini L, Bonapace S, Zenari L, Zoppini G, Arcaro G, et al. Relation of elevated serum uric acid levels to incidence of atrial fibrillation in patients with type 2 diabetes mellitus. Am J Cardiol. 2013;112:499–504. doi: 10.1016/j.amjcard.2013.04.012. [DOI] [PubMed] [Google Scholar]
- 34.Bergamini C, Cicoira M, Rossi A, Vassanelli C. Oxidative stress and hyperuricaemia: pathophysiology, clinical relevance, and therapeutic implications in chronic heart failure. Eur J Heart Fail. 2009;11:444–52. doi: 10.1093/eurjhf/hfp042. [DOI] [PubMed] [Google Scholar]
- 35.Imazio M, Brucato A, Cemin R, Ferrua S, Maggiolini S, Beqaraj F, et al. A randomized trial of colchicine for acute pericarditis. N Engl J Med. 2013;369:1522–8. doi: 10.1056/NEJMoa1208536. [DOI] [PubMed] [Google Scholar]
- 36.Imazio M, Bobbio M, Cecchi E, Demarie D, Demichelis B, Pomari F, et al. Colchicine in addition to conventional therapy for acute pericarditis: results of the COlchicine for acute PEricarditis (COPE) trial. Circulation. 2005;112:2012–6. doi: 10.1161/CIRCULATIONAHA.105.542738. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting the conclusions of this article is available in http://www.damus.in.th.


