Abstract
Hemophilia A is an inherited, X-linked, recessive disorder caused by deficiency of clotting factor VIII. Intracranial hemorrhage is the leading cause of morbidity and mortality in these patients. Use of factor replacement products and medications had improved outcome in these patients. But in developing countries many such patients are not able to afford factor replacement products. We report a case of traumatic intracerebellar hemorrage in a hemophilia child. This child presented to us as a case of sub-acute intracerebellar hemorrage, he was managed conservatively with six units of fresh frozen plasma transfusion. He improved clinically and on follow-up investigation hematoma was found to have dissolved spontaneously. Through this report we want to emphasize that those cases of hemophilia presenting with acute or sub-acute intracranial bleed, conservative approach through procoagulant transfusion and intravenous fibrinolysis inhibitors should be tried as first line of management. Before daring for surgery sufficient amount of factor replacement should be kept available.
Keywords: Conservative approach, Hemophilia, intracerebellar bleed
Introduction
Hemophilia is one of the oldest described genetic diseases. It is the most common X-linked genetic disease and the second most common factor deficiency after von Willebrand disease.[1] It has been further classified into A, B and C depending upon deficient clotting factor (VIII, IX and XI), respectively. Hemophilia A makes up approximately 80% of all hemophilia cases. The worldwide incidence of hemophilia A is approximately 1 case per 5000 male individuals. Because hemophilia is an X-linked recessive condition, it occurs predominantly in males. Females usually are asymptomatic carriers.
Case Report
A 12-year-old boy from rural area sustained head injury due to fall from height of 2 m while playing, 2 months back. He had history of transient loss of consciousness and vomiting, without history of convulsion or ear nose and throat bleeding. Computed tomography (CT) scan was done after 24 h of trauma. It revealed a well circumscribed, midline placed, hyperdense lesion in posterior fossa, without hydrocephalous [Figure 1]. All features were suggestive of acute intracerebellar bleeding. He was advised to consult a neurosurgeon. Because of his stable condition, parents differed. One and half month after this incidence, he again developed insidious onset of occipital headache and nuchal stiffness, followed by intermittent vomiting and unsteadiness of gait. He had history of bleeding disorder in his family. One of his brothers had already expired in early childhood, because of excessive bleeding from an external wound. On examination, we found bilateral papilloedema, truncal ataxia ansd nuchal stiffness. Magnetic resonance imaging of brain revealed mid-posterior cerebellar, sub-acute, intracerebellar bleed, extending down towards foramen of Magnum. There was associated mass effect, compressing the 4th ventricle and causing tri ventricular dilatation [Figures 2–5]. His coagulation profile was suggestive of moderately severe hemophilia (Raised Activated Partial Thromboplastin Time and factor VIII assay – 3% of normal factor). He was managed conservatively with six units of fresh frozen plasma transfusion and intravenous tranexamic acid. He improved clinically, and was discharged with oral tranexamic acid preparation, 3 times daily for next 10 days. Parents and the child were explained the reason for the disease and the child was advised to avoid outdoor and sports activities, where there is risk of accidental injury. On follow-up after 1 and ½ month, the child was fine and attending school regularly. Hematoma had spontaneously resolved as seen in the repeat CT scan [Figure 6].
Figure 1.
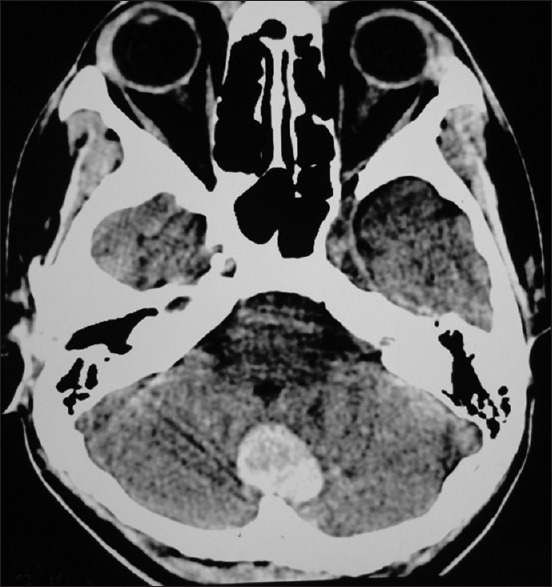
Plain computed tomography scan of brain, axial view showing well circumscribed, midline placed, hyperdense lesion in posterior fossa, without hydrocephalous
Figure 2.
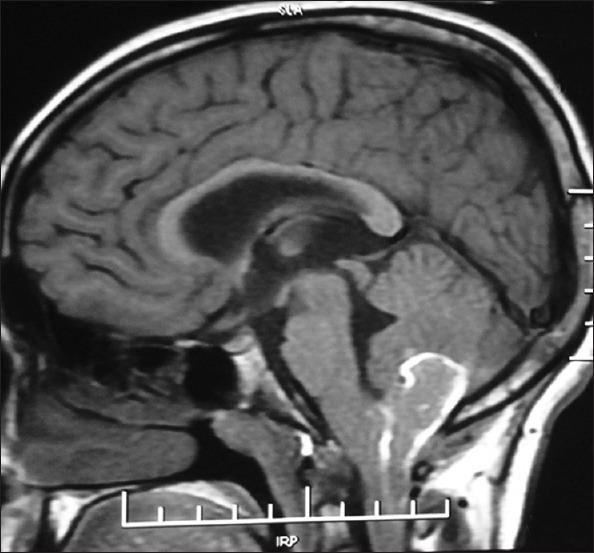
Plain magnetic resonance imaging of brain, T1Wi showing mid posterior cerebellar, sub-acute, intracerebellar bleed with extension down towards foramen of Magnum. Peripheral hyperintensity in plain T1Wi image is due to peripheral meth haemoglobin component
Figure 5.
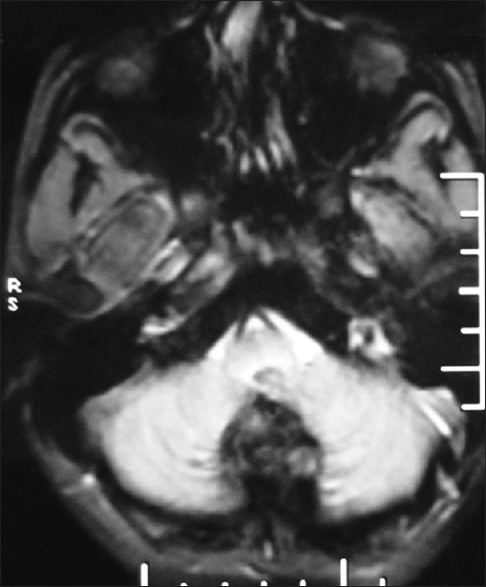
Gradient echo sequence showing hypo intense lesion in mid posterior cerebellar area
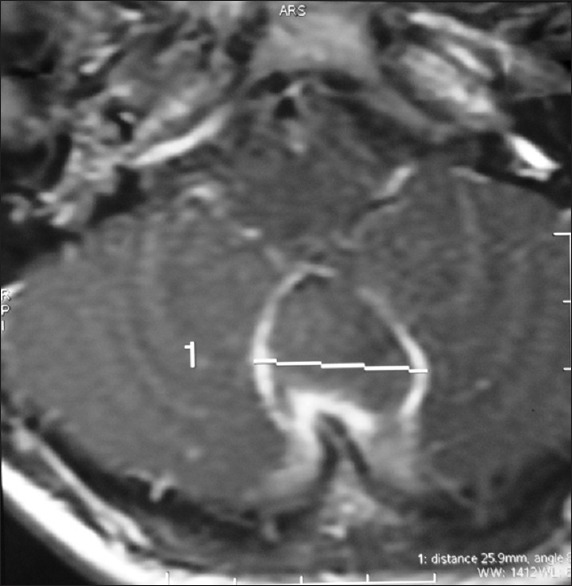
Figure 6.

After 1 and ½ month of conservative management, plain computed tomography scan axial view showing, resolved posterior fossa hematoma
Figure 3.

Contrast magnetic resonance imaging of brain showing peripheral rim enhancement of lesion, with compression of the 4th ventricle
Figure 4.
Contrast magnetic resonance imaging of brain, axial view showing peripheral rim enhancement of lesion
Discussion
The classification of the severity of hemophilia has been based on plasma procoagulant levels. Persons with less than 1% normal factor are considered to have severe hemophilia. Persons with 1-3% normal factor are considered to have moderately severe hemophilia and more than 3% but <30% normal factor are considered to have mild hemophilia.[2] Factor VIII supplementation is the cornerstone to arrest bleeding in hemophilia cases. Fresh frozen plasma, cryoprecipitate and factor VIII concentrates are rich in factor VIII.[2,3] Among the above products factor VIII concentrates are the best, as it rapidly corrects the levels. Fibrinolysis inhibitors like tranexamic acid and epsilon aminocaproic acid further enhance clot formation by inhibiting clot lysis. As these patients require frequent factor replacement, making them prone to AIDS and viral hepatitis. With improved screening of donors, new methods of factor concentrate purification, and recombinant concentrates, infectious complications had decreased significantly.
Intracranial hemorrhage and hemorrhages into the soft tissue around vital areas, such as the airway or internal organs, remain the most important life-threatening complications.[4] In children sports injury is the major cause of intracranial bleed. Early detection and prompt correction of factor level prevents devastating complications. There are few case reports of successful intracranial surgery in hemophilia patients available in literature.[4] This was possible because of the availability of clotting factor replacement therapy. The recommended factor level desired before proceeding for intracranial surgery is 80-100% and this level has to be maintained for 14 post-operative days. These clotting factor are expensive. In developing countries many such patients are not able to afford them. In developed countries much importance has been given to prophylactic recombinant product therapy. A cost-benefit analysis indicates that this approach reduces overall factor use and significantly reduces morbidity. Factor concentrates have made home-replacement therapy possible, improving patients’ quality of life.
Conclusion
With appropriate education and treatment, patients with hemophilia can live full and productive lives. Choosing safe sports is vital for children with hemophilia. In case of traumatic intracranial bleed, prompt diagnosis and conservative approach through procoagulant transfusion and intravenous fibrinolysis inhibitors should be tried as first line of management. Before daring for surgery sufficient amount of factor replacement should be kept available.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Miller CH. Genetics of hemophilia and von Willebrand's disease. In: Hilgartner MW, Pochedly C, editors. Hemophilia in the Child and Adult. 3rd ed. New York, NY, USA: Raven Press; 1989. pp. 297–345. [Google Scholar]
- 2.Kerr CB. Intracranial haemorrhage in haemophilia. J Neurol Neurosurg Psychiatry. 1964;27:166–73. doi: 10.1136/jnnp.27.2.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Silverstein A. Intracranial bleeding in hemophilia. Arch Neurol. 1960;3:141. doi: 10.1001/archneur.1960.00450020021005. [DOI] [PubMed] [Google Scholar]
- 4.Kwa SB. Surgery in haemophilia patients. Singapore Med J. 1968;9:7–11. [PubMed] [Google Scholar]


