Abstract
Rationale: Asthma has been reported to be more prevalent among Hispanics of Puerto Rican heritage than among other Hispanics and among Hispanics born in the United States or who immigrated as children than among those who came as adults; however, direct comparisons across Hispanic groups are lacking.
Objectives: To test whether asthma is more prevalent among Hispanics of Puerto Rican heritage than among other Hispanic groups, whether asthma is associated with age of immigration, and whether chronic obstructive pulmonary disease varies by heritage in a large, population-based cohort of Hispanics in the United States.
Methods: The Hispanic Community Health Study/Study of Latinos researchers recruited a population-based probability sample of 16,415 Hispanics/Latinos, 18–74 years of age, in New York City, Chicago, Miami, and San Diego. Participants self-reported Puerto Rican, Cuban, Dominican, Mexican, Central American, or South American heritage; birthplace; and, if relevant, age at immigration. A respiratory questionnaire and standardized spirometry were performed with post-bronchodilator measures for those with airflow limitation.
Measurements and Main Results: The prevalence of physician-diagnosed asthma among Puerto Ricans (36.5%; 95% confidence interval, 33.6–39.5%) was higher than among other Hispanics (odds ratio, 3.9; 95% confidence interval, 3.3–4.6). Hispanics who were born in the mainland United States or had immigrated as children had a higher asthma prevalence than those who had immigrated as adults (19.6, 19.4, and 14.1%, respectively; P < 0.001). Current asthma, bronchodilator responsiveness, and wheeze followed similar patterns. Chronic obstructive pulmonary disease prevalence was higher among Puerto Ricans (14.1%) and Cubans (9.8%) than among other Hispanics (<6.0%), but it did not vary across Hispanic heritages after adjustment for smoking and prior asthma (P = 0.22), by country of birth, or by age at immigration.
Conclusions: Asthma was more prevalent among Puerto Ricans, other Hispanics born in the United States, and those who had immigrated as children than among other Hispanics. In contrast, the higher prevalence of chronic obstructive pulmonary disease among Puerto Ricans and Cubans was largely reflective of differential smoking patterns and asthma.
Keywords: asthma, chronic obstructive pulmonary disease, race/ethnicity, social determinants of health
At a Glance Commentary
Scientific Knowledge on the Subject
Asthma has been reported to be more prevalent among Hispanics of Puerto Rican heritage and Hispanics born in the United States, and some studies have suggested that Hispanics of Mexican heritage may have a lower risk of chronic obstructive pulmonary disease (COPD); however, direct comparisons across Hispanic groups are lacking.
What This Study Adds to the Field
Asthma was up to three times more common among Hispanics of Puerto Rican heritage than among other Hispanics. Hispanics who were born in the mainland United States or immigrated to the United States as children had a higher asthma prevalence than those who immigrated as adults. In contrast, the prevalence of COPD did not differ by Hispanic heritage after accounting for smoking patterns and asthma earlier in life (onset before age 45 yr). These findings suggest that exposure to a more Americanized environment or lifestyle at a young age may contribute to asthma in Hispanics and suggest that differences in COPD prevalence across Hispanic groups is due mostly to variation in the prevalence of cigarette smoking and asthma earlier in life.
Hispanics are the largest and fastest-growing minority population in the United States, accounting for 17% of the U.S. population currently and projected to represent an estimated 30% of the U.S. population by 2050 (1). Over one-third of U.S. Hispanics were born outside the United States, and approximately one-half of immigrants to the United States are Hispanic (2, 3).
Asthma is the leading cause of hospitalization among young adults in the United States of Hispanic and non-Hispanic ethnicity (4, 5). Several studies suggest that persons in and from Puerto Rico, an unincorporated territory of the United States, have a particularly high prevalence of asthma (4, 6–10). However, direct comparisons between Hispanics of different heritages are not available, except in smaller studies that do not allow confident conclusions to be drawn about possible differences in respiratory disease across Hispanic groups.
Puerto Ricans move to the mainland United States at a younger age, on average, than other Hispanics, potentially resulting in earlier exposures and acculturation in the United States, and they may be subject to more Americanized exposures in Puerto Rico than Hispanics who emigrate from other countries. Early life exposures have been implicated in the pathogenesis of asthma due to effects on innate and adaptive immunity (11). Given that immigration to the United States implies a change in environmental and allergen exposures, birth in the United States and immigration to the United States at an early age may affect asthma risk. Indeed, some U.S. studies suggest a higher risk of asthma among Hispanics born in the United States than in those who immigrated to the United States (6, 12–15); however, these studies have generally been small or have focused on Hispanics of one heritage.
Chronic obstructive pulmonary disease (COPD) is the third leading cause of death in the United States. COPD mortality is lower among Hispanics than among non-Hispanics (16), in part due to lower prevalence of cigarette smoking in some Hispanic groups (17). Some studies have suggested that some Hispanics may be at reduced risk of COPD (18, 19), whereas others found no difference by ancestry (20) and after adjustment for smoking (21). The prevalence of spirometry defined COPD across the major Hispanic groups, particularly in relation to smoking and asthma, has not been described.
We therefore examined the prevalence of asthma and COPD in the HCHS/SOL (Hispanic Community Health Study/Study of Latinos), hypothesizing that asthma would be more prevalent among Puerto Ricans than among Hispanics of other heritages and among other Hispanics who were born in or had immigrated to the United States as children than among those who had immigrated as adults. Some of the results we report were previously presented in abstract form (22).
Methods
The HCHS/SOL is a community-based probability sample cohort study designed to examine risk factors of chronic disease among Hispanics of Mexican, Puerto Rican, Cuban, Dominican, Central American, and South American heritages living in the United States (23, 24). The HCHS/SOL researchers recruited and evaluated 16,415 self-identified Hispanics/Latinos ages 18–74 years between 2008 and 2011 in four U.S. communities (Bronx, NY; Chicago, IL; Miami, FL; and San Diego, CA). Households were selected using a stratified, two-stage area probability sample design with oversampling to increase the likelihood that a selected address would yield a Hispanic/Latino household (23). Of 39,384 individuals who were screened and selected and who met the eligibility criteria, 16,415 Hispanics (41.7%) from 9,872 households were enrolled. The study oversampled those ages 45–74 years to facilitate examination of target outcomes.
As HCHS/SOL recruited only Hispanics, we compared prevalence estimates in the MESA (Multi-Ethnic Study of Atherosclerosis), in which investigators recruited a multiethnic sample ages 45–84 years without clinical cardiovascular disease between 2000 and 2002 (25). MESA conducted examinations between 2010 and 2012 with pulmonary measures identical to those used in HCHS/SOL. The studies were approved by the institutional review boards at each participating institution, and written informed consent was obtained from all participants.
Self-reported Diagnoses and Symptoms
A standard respiratory questionnaire (26) was used to ascertain respiratory diagnoses and symptoms. Physician-diagnosed asthma was defined by affirmative responses to the items “Have you ever had asthma?” and “Was it diagnosed by a doctor or other healthcare professional?” Current asthma was defined as physician-diagnosed asthma with the use of an asthma treatment within the previous 12 months.
Wheeze was defined as ever having had “an attack of wheezing or whistling in your chest that made you feel short of breath,” and dyspnea was defined by a positive response to the item “Are you troubled by shortness of breath when hurrying on level ground or walking up a slight hill?”
Items were translated into Spanish and confirmed with focus groups.
Place of Birth and Age of Immigration
Heritage was identified by asking, “Which best describes your Hispanic/Latino heritage?” Participants were asked, “In what country or territory were you born?” Separate codes were recorded for “United States,” “Puerto Rico,” and “other countries.” The age at immigration into the mainland United States was defined as current age minus the number of years living in the United States, assessed by the item “From the time that you FIRST moved to the United States to today, about how many years have you lived in the mainland United States (50 states + DC)?” The mainland United States was defined as the 50 U.S. states and Washington, DC. Childhood versus adult immigration was dichotomized at 16 years of age.
Spirometry
Spirometry was conducted in accordance with American Thoracic Society/European Respiratory Society guidelines (27) using a dry rolling sealed spirometer with automated quality checks (Occupational Marketing, Houston, TX) according to the MESA-Lung study protocol (28) with overreading by one investigator. All participants, except those with recent cardiovascular events or surgery, were asked to perform prebronchodilator spirometry. Participants with prebronchodilator FEV1/FVC ratios less than 0.70 or less than the lower limit of normal (29) met the criteria to perform post-bronchodilator spirometry.
COPD was defined by a post-bronchodilator FEV1/FVC ratio less than 0.70 (30). A positive bronchodilator response was defined as an increase in the FEV1 of 200 milliliters or greater and an increase in FEV1% predicted of 12% or greater.
Covariates
Information on demographics, education, income, health insurance, and smoking was obtained by questionnaire. Never smoking was defined as smoking fewer than 100 cigarettes ever, and current smoking was defined as self-reported smoking of a cigarette in the previous 30 days. Height and weight were measured following a standardized protocol. Acculturation was assessed on the basis of two factors from the Short Acculturation Scale for Hispanics (31)—one on language preference and the other on social relationships—and an item on Hispanic compared with American food preference, as previously described (32).
Statistical Analysis
Prevalence estimates were calculated and weighted to adjust for disproportionate selection probabilities and to adjust for bias due to differential nonresponse at the household and person levels (23, 24). All analyses accounted for cluster sampling and the use of stratification in sample selection. Estimates are applicable to the study target population, defined as Hispanics/Latinos ages 18–74 years living in the four study communities.
Prevalence estimates were stratified by Hispanic heritage using survey logistic regression–predicted marginals, which adjusted each subgroup to the target population distribution of age, sex, education, health insurance, years in the United States, smoking status, and body mass index. As certain Hispanic/Latino heritages tended to be concentrated in specific geographic areas, not all heritages were present in each study site, creating the possibility of confounding between heritage and site. We therefore examined for possible site effects by fitting additional survey logistic regression models, adjusting for a 17-level heritage-by-site interaction term in place of heritage.
Prevalence estimates of COPD were restricted to participants age 45 years and older. Prevalence estimates of bronchodilator responsiveness were restricted to participants with airflow limitation. Missing assessments of COPD and bronchodilator responsiveness were accounted for using a three-step process. Missing data for prebronchodilator spirometry were accounted for by inverse probability weighting. Weights were developed using a logistic regression model from a set of baseline covariates. COPD and bronchodilator responsiveness for participants with missing post-bronchodilator spirometry data along with sporadic missing data for covariates were then estimated with multiple imputation using inverse probability weighting. See Table E1 in the online supplement for details. Analyses in MESA proceeded in a similar fashion but were unweighted.
All analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC) and SUDAAN release 11.0.0 (RTI International, Research Triangle Park, NC) software.
Results
The HCHS/SOL research team recruited 16,415 participants, of whom 98.2% completed the respiratory questionnaire (Figure E1). Hispanics of Mexican heritage were recruited predominantly in San Diego and Chicago, Puerto Ricans in New York City and Chicago, Cubans in Miami, Dominicans in New York City, and Central and South Americans in Miami and Chicago (Table E2).
Prebronchodilator spirometry was completed by 94.1% of participants, and post-bronchodilator spirometry by 1,073 (76% of those selected). Participants with spirometry measures were modestly younger, better educated, and more likely to be male and uninsured compared with those who did not complete spirometry (Table E3).
The estimated Hispanic heritage in the four communities was 38% Mexican, 16% Puerto Rican, 20% Cuban, 7% Central American, 10% Dominican, 5% South American, and 4% other or mixed. Forty-eight percent were male, and 50% were older than 45 years of age. Twenty-one percent currently smoked cigarettes, and 17% had previously smoked cigarettes. Twenty-three percent were born in the mainland United States, 15% had moved to the United States as children, and 63% had moved to the United States as adults.
Table 1 shows participant characteristics stratified by Hispanic heritage. Cubans were older than the overall average, and a higher proportion of Dominicans were women. Education varied modestly, and health insurance varied appreciably, across heritages. Approximately half of Puerto Ricans and those of other or mixed heritages had been born in the continental United States, a much greater proportion than others, and more Puerto Ricans and Dominicans had moved to the mainland United States as children. Smoking was most common among Puerto Ricans, followed by Cubans and other or mixed heritages.
Table 1.
Estimated Population Characteristics in the Hispanic Community Health Study/Study of Latinos
| Mexican |
Puerto Rican |
Cuban |
Central American |
Dominican |
South American |
Other or Mixed |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | |
| Sample size* | 6,438 |
2,659 |
2,324 |
1,712 |
1,426 |
1,059 |
511 |
|||||||
| Age, yr, mean | 38.6 | 0.37 | 42.9 | 0.50 | 46.6 | 0.53 | 39.8 | 0.49 | 39.1 | 0.67 | 42.4 | 0.76 | 35.3 | 0.80 |
| Sex, % female | 53.3 | 0.97 | 49.5 | 1.45 | 47.7 | 1.04 | 52.8 | 1.67 | 60.2 | 1.93 | 54.7 | 2.00 | 50.4 | 3.54 |
| Educational attainment, % | ||||||||||||||
| Less than high school | 36.0 | 1.34 | 36.7 | 1.63 | 22.1 | 1.06 | 38.6 | 1.67 | 37.2 | 1.80 | 21.8 | 1.92 | 20.3 | 2.95 |
| High school | 29.8 | 1.00 | 27.4 | 1.22 | 29.9 | 1.35 | 26.1 | 1.43 | 23.3 | 1.82 | 27.5 | 1.82 | 22.9 | 3.53 |
| Beyond high school | 34.2 | 1.58 | 35.9 | 1.61 | 48.0 | 1.46 | 35.4 | 1.63 | 39.5 | 1.75 | 50.7 | 2.13 | 56.8 | 3.72 |
| Yearly household income, % | ||||||||||||||
| ≤$10,000 | 10.0 | 0.73 | 18.2 | 1.28 | 15.8 | 1.04 | 13.9 | 1.24 | 15.4 | 1.36 | 9.7 | 1.12 | 8.7 | 1.44 |
| >$10,000–$20,000 | 26.9 | 1.32 | 27.5 | 1.37 | 30.0 | 1.18 | 33.3 | 1.78 | 33.9 | 2.23 | 30.3 | 1.85 | 20.9 | 2.48 |
| >$20,000–$40,000 | 34.7 | 1.10 | 24.5 | 1.52 | 25.9 | 1.23 | 29.2 | 1.68 | 29.0 | 1.77 | 34.5 | 1.94 | 32.3 | 3.30 |
| >$40,000–$75,000 | 16.3 | 0.98 | 14.8 | 1.08 | 8.5 | 0.77 | 9.7 | 1.18 | 9.2 | 0.99 | 12.9 | 1.43 | 19.7 | 2.69 |
| >$75,000 | 6.9 | 1.16 | 6.3 | 0.74 | 3.9 | 0.68 | 2.1 | 0.49 | 2.1 | 0.57 | 4.5 | 0.94 | 9.6 | 2.16 |
| Refused/missing | 5.3 | 0.38 | 8.8 | 0.72 | 15.8 | 1.07 | 11.8 | 1.03 | 10.6 | 1.04 | 8.1 | 1.16 | 8.8 | 1.65 |
| Health insurance, % | 42.4 | 1.42 | 78.3 | 1.37 | 41.7 | 1.65 | 31.3 | 2.09 | 70.7 | 1.98 | 41.5 | 2.21 | 56.1 | 3.64 |
| Age at immigration, % | ||||||||||||||
| Born in United States | 23.8 | 1.04 | 47.7 | 1.56 | 7.1 | 0.92 | 7.0 | 1.13 | 16.0 | 1.99 | 5.7 | 0.95 | 56.0 | 3.57 |
| 0–15 yr | 14.1 | 0.74 | 23.5 | 1.41 | 9.5 | 0.69 | 11.3 | 1.16 | 17.7 | 1.46 | 12.1 | 1.65 | 12.4 | 3.11 |
| >15 yr | 62.2 | 1.16 | 28.8 | 1.56 | 83.4 | 1.20 | 81.6 | 1.55 | 66.3 | 2.36 | 82.3 | 1.94 | 31.7 | 2.86 |
| 10 or more yr in United States†, % | 76.1 | 1.18 | 93.4 | 0.87 | 50.7 | 1.87 | 62.9 | 2.11 | 75.0 | 1.97 | 59.0 | 2.39 | 86.5 | 2.30 |
| Body mass index, kg/m2, mean | 29.2 | 0.15 | 30.7 | 0.23 | 29.0 | 0.16 | 29.1 | 0.18 | 29.5 | 0.32 | 28.0 | 0.25 | 29.5 | 0.36 |
| Smoking status, % | ||||||||||||||
| Never smoker | 64.1 | 1.06 | 49.5 | 1.55 | 54.4 | 1.53 | 70.7 | 1.63 | 77.1 | 1.69 | 65.3 | 2.18 | 56.5 | 3.54 |
| Former smoker | 18.4 | 0.82 | 16.8 | 1.17 | 19.1 | 0.94 | 14.8 | 1.17 | 11.1 | 1.10 | 21.6 | 1.60 | 17.7 | 2.44 |
| Current smoker | 17.6 | 0.90 | 33.8 | 1.39 | 26.6 | 1.32 | 14.5 | 1.20 | 11.8 | 1.53 | 13.1 | 1.48 | 25.8 | 3.18 |
| >10 pack-years‡, % | 8.1 | 0.53 | 25.3 | 1.45 | 29.9 | 1.38 | 9.3 | 0.89 | 8.4 | 0.84 | 10.6 | 1.17 | 13.6 | 2.05 |
Sample size completing the respiratory questionnaire from which the population estimates are derived. All estimates account for sampling weight and study design.
Among those who immigrated to the United States.
Among ever smokers.
Prevalence of Asthma by Hispanic Heritage
The prevalence of physician-diagnosed lifetime asthma among Hispanics was 16.4% (95% confidence interval [CI], 15.4–17.4), and the prevalence of current asthma was 7.4% (95% CI, 6.8–8.1). The prevalence of asthma varied by Hispanic heritage (P < 0.001) and was highest among Puerto Ricans; intermediate among Cubans, Dominicans, and other or mixed heritage groups; and lowest among Mexicans (Table 2). The age- and sex-adjusted odds ratio for asthma among Puerto Ricans compared with Hispanics of other heritages was 3.9 (95% CI, 3.3–4.6). These differences changed little in the fully adjusted analysis (Table 2). Additional adjustment for three measures of acculturation made no material differences to the results; for example, the acculturation-adjusted prevalence of asthma was 31.0% among Puerto Ricans and 7.7% among Mexicans. Similar differences across Hispanic heritages were observed for current asthma, symptoms of wheezing that resulted in shortness of breath, wheeze in the previous 12 months, dyspnea, and bronchodilator responsiveness, although the last item did not attain statistical significance (Table 2; Table E4). The findings for asthma and bronchodilator responsiveness were little changed among never smokers (Table E5).
Table 2.
Prevalence Estimates of Physician-diagnosed Asthma and Bronchodilator Responsiveness from the Hispanic Community Health Study/Study of Latinos
| Mexican | Puerto Rican | Cuban | Central American | Dominican | South American | Other or Mixed | P Value | |
|---|---|---|---|---|---|---|---|---|
| Sample size | 6,438 | 2,659 | 2,324 | 1,712 | 1,426 | 1,059 | 511 | |
| Physician-diagnosed asthma, ever | ||||||||
| Age and sex adjusted | 7.5 (6.6–8.6) | 36.5 (33.6–39.5) | 21.8 (19.9–23.9) | 11.2 (9.4–13.3) | 15.4 (13.1–18.1) | 9.1 (7.0–11.8) | 17.7 (13.5–22.9) | <0.001 |
| Multivariate analysis | 7.8 (6.8–8.9) | 30.9 (27.8–34.2) | 23.3 (21.1–25.7) | 12.8 (10.7–15.2) | 15.7 (13.0–18.7) | 10.4 (7.9–13.5) | 16.5 (12.5–21.4) | <0.001 |
| Physician-diagnosed asthma, current | ||||||||
| Age and sex adjusted | 3.1 (2.5–3.8) | 21.9 (19.5–24.6) | 7.2 (6.0–8.7) | 3.5 (2.6–4.6) | 6.7 (5.3–8.4) | 3.2 (2.1–4.7) | 7.8 (5.5–10.9) | <0.001 |
| Multivariate analysis | 3.4 (2.7–4.1) | 15.3 (13.2–17.6) | 8.6 (7.1–10.4) | 4.5 (3.4–6.0) | 6.7 (5.3–8.5) | 4.3 (2.9–6.2) | 6.9 (4.8–9.8) | <0.001 |
| Bronchodilator responsiveness | ||||||||
| Sample size | 354 | 224 | 231 | 74 | 89 | 61 | 37 | |
| Age and sex adjusted | 11.5 (7.1–17.9) | 24.2 (9.2–49.0) | 10.2 (5.0–19.1) | 8.0 (3.5–17.0) | 15.5 (8. 2–27.1) | 10.7 (4.2–24.4) | 15.5 (0.3–83.3) | 0.465 |
| Multivariate analysis | 11.0 (6.5–17.9) | 21.2 (7.5–45.6) | 12.1 (6.3–21.6) | 9.6 (4.1–20.6) | 16.0 (8.4–28.1) | 12.3 (5.0–27.0) | 14.7 (0.2–85.2) | 0.799 |
| Second multivariate analysis | 12.8 (7.7–20.5) | 18.0 (7.1–37.4) | 12.5 (6.7–22.0) | 10.3 (4.5–21.8) | 14.2 (7.5–25.0) | 13.7 (6.0–28.4) | 15.8 (0.3–31.2) | 0.935 |
Ninety-five percent confidence intervals are shown in parentheses. Sample size represents number completing the respiratory questionnaire (or post-bronchodilator spirometry) from which the population estimates are derived. All estimates account for sampling weight and study design. P values comparing backgrounds are derived from a survey logistic regression Wald F test with 6 numerator degrees of freedom. Multivariate model adjusted for age, sex, educational attainment, age at immigration, 10 or more years in the United States, smoking status, body mass index, and health insurance. Second model for bronchodilator responsiveness was not adjusted for health insurance but was additionally adjusted for current pulmonary medication use and prebronchodilator FEV1.
The prevalence of asthma varied by site and was particularly high in New York City (Figure E2). Most Puerto Ricans were recruited in New York City, which might have accounted for the difference by Hispanic heritage. However, the prevalence of asthma among Puerto Ricans in New York City was higher than that among Dominicans and others also recruited in New York City, and the prevalence of asthma was much higher in Puerto Ricans in Chicago than among all other Hispanics in Chicago (Figure E2).
Age at Immigration and Asthma
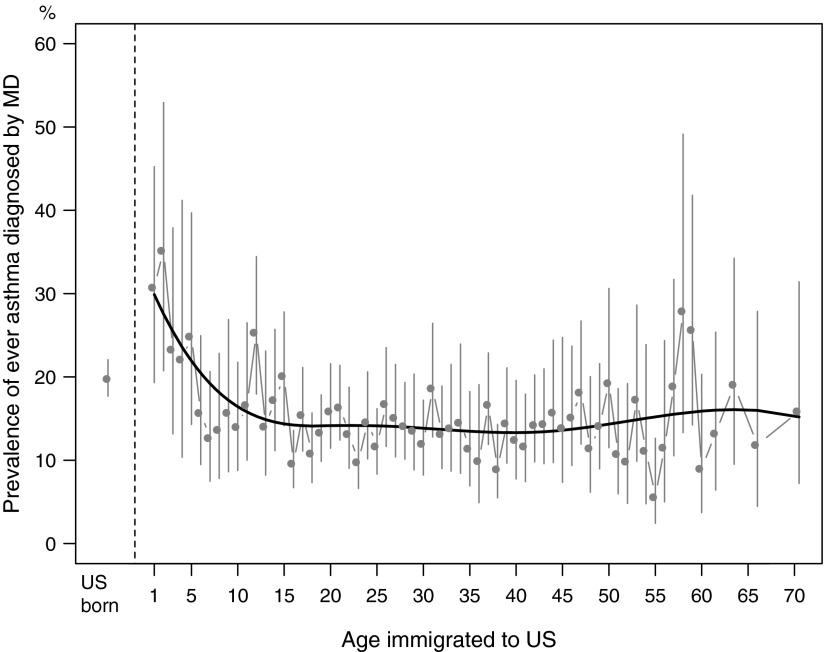
The adjusted prevalence of asthma among Hispanics who had immigrated to the United States as adults was 14.1% compared with 19.4% among those who had immigrated as children and 19.6% among those who were born in the United States (Table 3). These differences were independent of age, sex, educational attainment, smoking status, body mass index, and health insurance, which differed across these groups (Table E6), and persisted among never smokers (P = 0.001). Among Hispanics who immigrated to the United States, the prevalence of asthma was highest among those who immigrated in early childhood compared with those who had immigrated as adults, with an inflection point between ages 5 and 15 years (Figure 1).
Table 3.
Prevalence Estimates of Physician-diagnosed Asthma and Bronchodilator Responsiveness from the Hispanic Community Health Study/Study of Latinos by Age at Immigration to the United States
| Born in United States | Immigrated at Age 0–15 Yr | Immigrated at Age >15 Yr | P Value | |
|---|---|---|---|---|
| Sample size | 2,083 | 2,035 | 11,271 | |
| Physician-diagnosed asthma, ever | ||||
| Multivariate analysis | 19.6 (17.3–22.0) | 19.4 (16.9–22.2) | 14.1 (13.0–15.3) | <0.001 |
| Physician-diagnosed asthma, current | ||||
| Multivariate analysis | 9.5 (8.0–11.3) | 8.5 (6.9–10.5) | 6.0 (5.3–6.7) | <0.001 |
| Bronchodilator responsiveness | ||||
| Sample size | 215 | 120 | 735 | |
| Multivariate analysis | 24.5 (13.5–39.8) | 13.2 (2.7–42.1) | 10.7 (5.7–18.8) | 0.269 |
| Second multivariate analysis | 26.0 (15.0–41.0) | 11.8 (2.6–36.9) | 10.7(5.7–18.9) | 0.239 |
Ninety-five percent confidence intervals are shown in parentheses. Sample size represents number completing the respiratory questionnaire (or post-bronchodilator spirometry) from which the population estimates are derived. All estimates account for sampling weight and study design. P values comparing age of immigration categories are derived from a survey logistic regression Wald F test with 2 numerator degrees of freedom. Multivariate model adjusted for age, sex, educational attainment, age at immigration, 10 or more years in the United States, smoking status, body mass index, and health insurance. Second model for bronchodilator responsiveness was not adjusted for health insurance but was additionally adjusted for current pulmonary medication use and prebronchodilator FEV1.
Figure 1.
Estimated prevalence of asthma by age at immigration to the continental United States. The gray vertical lines represent 95% confidence intervals around the point estimates of asthma prevalence at each year of age of immigration adjusted for age, sex, and Hispanic heritage. The black line is the cubic smooth spline curve fitted across the point estimates.
Current asthma and bronchodilator responsiveness were also higher among participants who had immigrated as children and those who were born in the United States than in the other groups (Table 3), although the differences were not statistically significant for bronchodilator responsiveness.
The association of age of immigration with current asthma was modified by Hispanic heritage (P = 0.004 for interaction). Figure E3 shows large, monotonic differences in current asthma prevalence by age at immigration among Central Americans and Mexicans (both P < 0.05); consistent but nonsignificant associations among Cubans, Dominicans, and other or mixed heritages; and no evidence for association among Puerto Ricans and South Americans. The findings were similar for ever having had asthma (Figure E4). There was little or no evidence for effect modification by site (P-interaction = 0.87 and P = 0.06, respectively), with similar findings across all sites (Figure E5).
Wheeze that contributed to shortness of breath was also lower among Hispanics who had immigrated to the United States at age 16 years or older (12.5%) than in those who had immigrated before age 16 years (15.9%) or among those who were born in the United States (17.6%; P < 0.001). The findings were similar for current wheeze and, with more variation, dyspnea (Table E7).
COPD
The prevalence of COPD among participants older than 45 years of age was 8.2% (95% CI, 7.1–9.5). The age- and sex-adjusted prevalence of COPD differed by Hispanic heritage (P < 0.001) and was higher among Puerto Ricans and Cubans and compared with others (Table 4). However, differences were attenuated by adjustment for smoking history and asthma with onset before age 45 years resulting in no differences in COPD prevalence by Hispanic heritage in the fully adjusted model (Table 4). These findings were similar in analyses restricted to participants with 10 or more pack-years of smoking (Table E8).
Table 4.
Prevalence Estimates of Chronic Obstructive Pulmonary Disease for Participants Ages 45 Years and Older from the Hispanic Community Health Study/Study of Latinos
| Mexican | Puerto Rican | Cuban | Central American | Dominican | South American | Other or Mixed | P Value | |
|---|---|---|---|---|---|---|---|---|
| Sample size | 3,383 | 1,547 | 1,454 | 873 | 760 | 604 | 195 | |
| Age and sex adjusted | 4.6 (3.6–6.0) | 14.1 (9.9–19.6) | 9.8 (8.3–11.6) | 5.2 (3.6–7.3) | 5.6 (3.6–8.4) | 5.9 (3.7–9.5) | 5.1 (2.0–12.0) | < 0.001 |
| Multivariate analysis | 5.5 (4.3–7.1) | 12.6 (9.3–16.8) | 8.4 (6.8–10.2) | 6.2 (4.3–8.9) | 7.1 (4.6–10.8) | 6.8 (4.4–10.4) | 5.5 (2.2–12.7) | 0.002 |
| Second multivariate analysis | 6.5 (5.1–8.2) | 11.1 (7.9–15.3) | 8.0 (6.6–9.7) | 6.6 (4.6–9.3) | 7.5 (5.0–11.1) | 7.2 (4.8–10.8) | 5.8 (2.3–13.4) | 0.223 |
Ninety-five percent confidence intervals are shown in parentheses. Sample size represents participants age 45 years and older completing prebronchodilator spirometry and post-bronchodilator spirometry, when indicated, from which the population estimates are derived. P value comparing backgrounds is from a survey logistic regression Wald F test with 6 numerator degrees of freedom. Multivariate analysis is adjusted for age, sex, educational attainment, age at immigration, 10 or more years in the United States, smoking status, pack-years of smoking, and health insurance. Second multivariate model is adjusted for all items in the multivariate analysis except health insurance plus asthma onset before age 45 years.
There was no evidence that age at immigration was associated with COPD. The adjusted prevalence of COPD was 7.8% (95% CI, 6.9–8.8%) among Hispanics who had immigrated to the United States as adults, 11.1% (95% CI, 6.4–18.7%) among those who had immigrated as children, and 8.1% (95% CI, 5.1–12.5%) among those who were born in the mainland United States (P = 0.46 for trend).
Comparisons in MESA
The prevalence of asthma among Hispanics of Mexican heritage in MESA was 8.8%, similar to that in HCHS/SOL. The prevalence of asthma was somewhat higher in non-Hispanic whites and non-Hispanic African Americans than Hispanics of Mexican heritage in MESA (Table E9), but it was not nearly as high as that among Puerto Ricans, Cubans, and Dominicans in HCHS/SOL. A similar but less marked pattern was present for the prevalence of wheezing in the previous 12 months. The prevalence of COPD among Hispanics in HCHS/SOL was not dissimilar from that among non-Hispanics in MESA.
Discussion
In this large, population-based U.S. study, Puerto Ricans had a threefold higher prevalence of asthma compared with Hispanics of other heritages. Among non–Puerto Rican Hispanics, those who were born in United States or who had immigrated to the United States as children had a higher prevalence of asthma than those who immigrated as adults. The findings were similar for bronchodilator responsiveness and wheeze. In contrast, there was no evidence that prevalence of COPD differed by Hispanic heritage or varied by age at immigration after accounting for differences in smoking and asthma history.
The present study is by far the largest on this topic to report on Hispanics of multiple heritages. The noted high prevalence of asthma among Puerto Ricans is consistent with prior smaller studies that showed a prevalence of 12–26% in Puerto Ricans compared with the U.S. national prevalence of approximately 8% (4, 5, 7, 8) and in a large, nationally representative sample (15). Unlike prior studies on this topic, the present findings were not potentially due to selection bias, differences by site, or diagnostic bias, as noted by the consistent findings for bronchodilator responsiveness and symptoms of wheezing. The low prevalence among those from Mexico, Central America, and South America is consistent with evidence that asthma is less common among Mexican Americans than among non-Hispanic whites (6, 12), similar to the comparisons with MESA reported here and a prior study including Central Americans and South Americans (33).
Asthma prevalence was high among Puerto Ricans who were born in the mainland United States and Puerto Rico, regardless of age at migration. In contrast, other Hispanics who were born in the United States or who had immigrated to the United States as children had a higher prevalence of asthma than those who had immigrated to the United States as adults. Prior studies have found similar associations in Mexican Americans (12–15, 34) and, recently, in non-Hispanic whites and African Americans (15). Similar findings have been reported for immigrants to Great Britain, Sweden, and, more variably, Israel (35–37).
In contrast, there was no suggestion that COPD prevalence was related to either Hispanic heritage or age at immigration after accounting for history of smoking and a prior history of asthma. In studies from the United States, Central America, and South America, researchers have found a lower prevalence of COPD among Mexican Americans compared with non-Hispanic Americans (16, 38, 39) and among Mexicans compared with South Americans (40), although much of these differences was attributable to smoking patterns. In the present study, the largest on the topic to date, the higher prevalence of COPD among Puerto Ricans and Cubans was largely explained by differences in smoking patterns and asthma earlier in life. Mexican Americans had the lowest prevalence of all groups; however, the multivariate 95% CI for Mexican Americans included the prevalence estimates of all other groups except Puerto Ricans, and there was no evidence for differential COPD prevalence in the multivariate results.
The mechanisms behind the higher prevalence of asthma among Puerto Ricans and other Hispanics of Caribbean origin were not examined in detail in the present study but may include greater exposure to active and passive tobacco smoke (41); a greater predisposition to allergic disease, including rhinitis, eczema (42), and atopy (43, 44); environmental exposures (43, 45); premature birth (46); other socioeconomic factors (47); and genetic (18, 48) and epigenetic (49) factors. Early life exposures may also be implicated (41), which is supported by our findings of the markedly elevated risk of asthma among Hispanics who had immigrated to the United States before age 6 years. Early-life exposures encountered in predominantly urban U.S. environments may include increased dust, cockroach- and mold-borne allergens, and air pollution exposures (45), which may increase the risk of developing asthma via eosinophilic and noneosinophilic mechanisms (50). Acculturation has also been suggested to play a role in asthma development (15). However, in the present study, measures of acculturation based upon language, social factors, and food preferences had little impact on the results, possibly because they were collinear with items already in the model, such as years in the mainland United States.
Evidence for contributions of both genetic and nongenetic factors to asthma is suggested by its higher prevalence among Puerto Ricans than in Dominicans and other Hispanics in the Bronx and also than Mexicans and other Hispanics in Chicago in addition to its considerably higher prevalence among Puerto Ricans in the Bronx compared with Chicago.
Although the present study is the largest population-based study of Hispanics in the United States, particularly one that includes post-bronchodilator spirometry measures, it has a number of limitations. First, the sample was drawn predominantly from urban settings, and hence the results may not fully capture respiratory disease related to nonurban exposures. Whereas asthma prevalence may be lower in rural than in urban settings, COPD might be higher (51). Furthermore, residents of Puerto Rico and Hispanics in the U.S. Southwest were not included in the HCHS/SOL. The response rate to the study was modest, and not all participants completed spirometry. However, we used two-stage weighted and multiple imputation to account for missing data; therefore, the estimates are likely to be reasonably accurate. A control group of non-Hispanics was not included in the original design; however, we included results for Hispanics and non-Hispanics in MESA, in which researchers ascertained respiratory disease in an identical manner in the same time period in two of the same cities as HCHS/SOL, although the strategy and years of cohort recruitment differed. Hispanic heritage was based upon self-report, which has limitations but is a reasonable standard; subsequent work will evaluate heritage including ancestral markers. Asthma was also defined by self-report of a physician’s diagnosis, which may be subject to bias, and there is some degree of misclassification with COPD. However, the results for asthma restricted to never smokers and COPD restricted to participants with 10 or more pack-years yielded findings that were highly consistent with those from the overall cohort.
In conclusion, asthma prevalence was high in Puerto Ricans, regardless of place of birth and age at immigration. Among other Hispanics, birth in the United States, and particularly immigration to the United States as a child, was associated with elevated asthma risk. Consistent associations were observed for symptoms of wheeze and bronchodilator responsiveness, and there was no relationship between age at immigration and COPD after adjustment for smoking, demonstrating a specific association likely not due to diagnostic bias. In contrast, differences in COPD prevalence across Hispanic heritages in this study were fully explained by smoking patterns and asthma earlier in life. These findings suggest that exposure to the U.S. environment or lifestyle at a young age may contribute to asthma and that differences in smoking and asthma drive much of the variation in COPD prevalence across different Hispanic groups.
Acknowledgments
Acknowledgment
The authors thank the staff and participants of HCHS/SOL for their important contributions. A complete list of staff and investigators has been published previously (23) and is also available on the study website (http://www.cscc.unc.edu/hchs/). The authors also thank the other investigators, the staff, and the participants in the MESA study. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org/. Statistical analyses for HCHS/SOL were performed at the University of North Carolina; those for MESA were performed at Columbia University.
Footnotes
The HCHS/SOL (Hispanic Community Health Study/Study of Latinos) was performed as a collaborative study supported by contracts from the NHLBI to the University of North Carolina (N01-HC65233), the University of Miami (N01-HC65234), the Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following institutes, centers, or offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: the National Center on Minority Health and Health Disparities, the National Institute on Deafness and Other Communication Disorders, the National Institute of Dental and Craniofacial Research, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Neurological Disorders and Stroke, and the Office of Dietary Supplements. MESA (Multi-Ethnic Study of Atherosclerosis) and the MESA Lung Study were supported by NHLBI grants R01-HL077612, RC1-HL100543, and R01-HL083091 and contracts N01-HC-95159, N01-HC-95160, N01-HC-95161, N01-HC-95162, N01-HC-95163, N01-HC-95164, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168, and N01-HC-95169. They were also supported by National Center for Research Resources grants UL1-TR-000040 and UL1-TR-001079. The funding agency had a role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; and in the review and approval of the manuscript.
Author Contributions: R.G.B.: drafted the manuscript, obtained funding, participated in data collection, oversaw the statistical analysis for MESA, and provided critical revisions; L.L., A.G.H., L.A.-S., R.C.K., T.K.A., K.L., L.J.S., E.S.M., M.S., A.R., and J.S.L.: obtained funding, participated in data collection, and provided critical revisions; and S.M.D., A.N., and F.G.: performed the statistical analysis for HCHS/SOL and provided critical revisions.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1164/rccm.201506-1211OC on October 12, 2015
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.U.S. Census Bureau. 2012 national population projections [accessed 2015 Oct 23]. Available from: https://www.census.gov/population/projections/data/national/2012.html.
- 2.Brown A, Patten E Pew Research Center. Table 3. Statistical portrait of the foreign-born population in the United States, 2012 [accessed 2015 Oct 23]. Available from: http://www.pewhispanic.org/2014/04/29/statistical-portrait-of-the-foreign-born-population-in-the-united-states-2012/#foreign-born-by-region-of-birth-2000-and-2012.
- 3.Brown A, Patten E Pew Research Center. Statistical portrait of Hispanics in the United States, 2012 [accessed 2015 Oct 23]. Available from: http://www.pewhispanic.org/2014/04/29/statistical-portrait-of-hispanics-in-the-united-states-2012/
- 4.Moorman JE, Zahran H, Truman BI, Molla MT Centers for Disease Control and Prevention (CDC) Current asthma prevalence—United States, 2006–2008. MMWR Surveill Summ. 2011;60(Suppl.)(1):84–86. [PubMed] [Google Scholar]
- 5.Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, Liu X. Trends in asthma prevalence, health care use, and mortality in the United States, 2001-2010. NCHS Data Brief. 2012;(94):1–8. [PubMed] [Google Scholar]
- 6.Subramanian SV, Jun HJ, Kawachi I, Wright RJ. Contribution of race/ethnicity and country of origin to variations in lifetime reported asthma: evidence for a nativity advantage. Am J Public Health. 2009;99:690–697. doi: 10.2105/AJPH.2007.128843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lara M, Akinbami L, Flores G, Morgenstern H. Heterogeneity of childhood asthma among Hispanic children: Puerto Rican children bear a disproportionate burden. Pediatrics. 2006;117:43–53. doi: 10.1542/peds.2004-1714. [DOI] [PubMed] [Google Scholar]
- 8.Dumanovsky T, Matte TD. Variation in adult asthma prevalence in Hispanic subpopulations in New York City. J Asthma. 2007;44:297–303. doi: 10.1080/02770900701344140. [DOI] [PubMed] [Google Scholar]
- 9.Rose D, Mannino DM, Leaderer BP. Asthma prevalence among US adults, 1998–2000: role of Puerto Rican ethnicity and behavioral and geographic factors. Am J Public Health. 2006;96:880–888. doi: 10.2105/AJPH.2004.050039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koinis-Mitchell D, Sato AF, Kopel SJ, McQuaid EL, Seifer R, Klein R, Esteban C, Lobato D, Ortega AN, Canino G, et al. Immigration and acculturation-related factors and asthma morbidity in Latino children. J Pediatr Psychol. 2011;36:1130–1143. doi: 10.1093/jpepsy/jsr041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raedler D, Schaub B. Immune mechanisms and development of childhood asthma. Lancet Respir Med. 2014;2:647–656. doi: 10.1016/S2213-2600(14)70129-8. [DOI] [PubMed] [Google Scholar]
- 12.McHugh MK, Symanski E, Pompeii LA, Delclos GL. Prevalence of asthma among adult females and males in the United States: results from the National Health and Nutrition Examination Survey (NHANES), 2001-2004. J Asthma. 2009;46:759–766. doi: 10.1080/02770900903067895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Svendsen ER, Gonzales M, Ross M, Neas LM. Variability in childhood allergy and asthma across ethnicity, language, and residency duration in El Paso, Texas: a cross-sectional study. Environ Health. 2009;8:55. doi: 10.1186/1476-069X-8-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eldeirawi K, McConnell R, Furner S, Freels S, Stayner L, Hernandez E, Amoruso L, Torres S, Persky VW. Associations of doctor-diagnosed asthma with immigration status, age at immigration, and length of residence in the United States in a sample of Mexican American school children in Chicago. J Asthma. 2009;46:796–802. [PubMed] [Google Scholar]
- 15.Iqbal S, Oraka E, Chew GL, Flanders WD. Association between birthplace and current asthma: the role of environment and acculturation. Am J Public Health. 2014;104(Suppl. 1):S175–S182. doi: 10.2105/AJPH.2013.301509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ford ES, Croft JB, Mannino DM, Wheaton AG, Zhang X, Giles WH. COPD surveillance—United States, 1999-2011. Chest. 2013;144:284–305. doi: 10.1378/chest.13-0809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaplan RC, Bangdiwala SI, Barnhart JM, Castañeda SF, Gellman MD, Lee DJ, Pérez-Stable EJ, Talavera GA, Youngblood ME, Giachello AL. Smoking among U.S. Hispanic/Latino adults: the Hispanic community health study/study of Latinos. Am J Prev Med. 2014;46:496–506. doi: 10.1016/j.amepre.2014.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bruse S, Sood A, Petersen H, Liu Y, Leng S, Celedón JC, Gilliland F, Celli B, Belinsky SA, Tesfaigzi Y. New Mexican Hispanic smokers have lower odds of chronic obstructive pulmonary disease and less decline in lung function than non-Hispanic whites. Am J Respir Crit Care Med. 2011;184:1254–1260. doi: 10.1164/rccm.201103-0568OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Diaz AA, Come CE, Mannino DM, Pinto-Plata V, Divo MJ, Bigelow C, Celli B, Washko GR. Obstructive lung disease in Mexican Americans and non-Hispanic whites: an analysis of diagnosis and survival in the National Health and Nutritional Examination Survey III Follow-up Study. Chest. 2014;145:282–289. doi: 10.1378/chest.13-1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Powell R, Davidson D, Divers J, Manichaikul A, Carr JJ, Detrano R, Hoffman EA, Jiang R, Kronmal RA, Liu K, et al. Genetic ancestry and the relationship of cigarette smoking to lung function and per cent emphysema in four race/ethnic groups: a cross-sectional study. Thorax. 2013;68:634–642. doi: 10.1136/thoraxjnl-2012-202116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kinney GL, Thomas DSK, Cicutto L, Newman LS, Lutz S, Honkanson JE. The protective effect of Hispanic ethnicity on chronic obstructive pulmonary disease mortality is mitigated by smoking behavior. J Pulm Respir Med. 2014;4:220. doi: 10.4172/2161-105X.1000220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barr RG, LaVange L, Henderson A, Aviles-Santa L, Kaplan R, Aldrich T, Liu K, Smith LJ, Mendes ES, Salathe M, et al. Prevalence of Pulmonary symptoms and disease in Hispanic subgroups: results from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) [abstract] Am J Respir Crit Care Med. 2011;183:A1716. [Google Scholar]
- 23.LaVange LM, Kalsbeek WD, Sorlie PD, Avilés-Santa LM, Kaplan RC, Barnhart J, Liu K, Giachello A, Lee DJ, Ryan J, et al. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:642–649. doi: 10.1016/j.annepidem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sorlie PD, Avilés-Santa LM, Wassertheil-Smoller S, Kaplan RC, Daviglus ML, Giachello AL, Schneiderman N, Raij L, Talavera G, Allison M, et al. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:629–641. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR, Jr, Kronmal R, Liu K, et al. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 26.Ferris BG. Epidemiology Standardization Project (American Thoracic Society) Am Rev Respir Dis. 1978;118:1–120. [PubMed] [Google Scholar]
- 27.Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, Coates A, van der Grinten CP, Gustafsson P, Hankinson J, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26:948–968. doi: 10.1183/09031936.05.00035205. [DOI] [PubMed] [Google Scholar]
- 28.Hankinson JL, Kawut SM, Shahar E, Smith LJ, Stukovsky KH, Barr RG. Performance of American Thoracic Society-recommended spirometry reference values in a multiethnic sample of adults: the Multi-Ethnic Study of Atherosclerosis (MESA) lung study. Chest. 2010;137:138–145. doi: 10.1378/chest.09-0919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159:179–187. doi: 10.1164/ajrccm.159.1.9712108. [DOI] [PubMed] [Google Scholar]
- 30.Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, Barnes PJ, Fabbri LM, Martinez FJ, Nishimura M, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187:347–365. doi: 10.1164/rccm.201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 31.Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for Hispanics. Hisp J Behav Sci. 1987;9:183–205. [Google Scholar]
- 32.Isasi CR, Ayala GX, Sotres-Alvarez D, Madanat H, Penedo F, Loria CM, Elder JP, Daviglus ML, Barnhart J, Siega-Riz AM. Is acculturation related to obesity in Hispanic/Latino adults? Results from the Hispanic Community Health Study/Study of Latinos. J Obes. 2015;2015:186276. doi: 10.1155/2015/186276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Menezes AM, Montes de Oca M, Pérez-Padilla R, Nadeau G, Wehrmeister FC, Lopez-Varela MV, Muiño A, Jardim JR, Valdivia G, Tálamo C PLATINO Team. Increased risk of exacerbation and hospitalization in subjects with an overlap phenotype: COPD-asthma. Chest. 2014;145:297–304. doi: 10.1378/chest.13-0622. [DOI] [PubMed] [Google Scholar]
- 34.Eldeirawi KM, Persky VW. Associations of acculturation and country of birth with asthma and wheezing in Mexican American youths. J Asthma. 2006;43:279–286. doi: 10.1080/0277090060022869. [DOI] [PubMed] [Google Scholar]
- 35.Bråbäck L, Vogt H, Hjern A. Migration and asthma medication in international adoptees and immigrant families in Sweden. Clin Exp Allergy. 2011;41:1108–1115. doi: 10.1111/j.1365-2222.2011.03744.x. [DOI] [PubMed] [Google Scholar]
- 36.Pereg D, Tirosh A, Lishner M, Goldberg A, Shochat T, Confino-Cohen R. Prevalence of asthma in a large group of Israeli adolescents: influence of country of birth and age at migration. Allergy. 2008;63:1040–1045. doi: 10.1111/j.1398-9995.2008.01661.x. [DOI] [PubMed] [Google Scholar]
- 37.Netuveli G, Hurwitz B, Sheikh A. Ethnic variations in incidence of asthma episodes in England & Wales: national study of 502,482 patients in primary care. Respir Res. 2005;6:120. doi: 10.1186/1465-9921-6-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tilert T, Dillon C, Paulose-Ram R, Hnizdo E, Doney B. Estimating the U.S. prevalence of chronic obstructive pulmonary disease using pre- and post-bronchodilator spirometry: the National Health and Nutrition Examination Survey (NHANES) 2007-2010. Respir Res. 2013;14:103. doi: 10.1186/1465-9921-14-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ford ES, Mannino DM, Wheaton AG, Giles WH, Presley-Cantrell L, Croft JB. Trends in the prevalence of obstructive and restrictive lung function among adults in the United States: findings from the National Health and Nutrition Examination surveys from 1988-1994 to 2007-2010. Chest. 2013;143:1395–1406. doi: 10.1378/chest.12-1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Menezes AMB, Perez-Padilla R, Jardim JR, Muiño A, Lopez MV, Valdivia G, Montes de Oca M, Talamo C, Hallal PC, Victora CG PLATINO Team. Chronic obstructive pulmonary disease in five Latin American cities (the PLATINO study): a prevalence study. Lancet. 2005;366:1875–1881. doi: 10.1016/S0140-6736(05)67632-5. [DOI] [PubMed] [Google Scholar]
- 41.Bunyavanich S, Silberg JL, Lasky-Su J, Gillespie NA, Lange NE, Canino G, Celedón JC. A twin study of early-childhood asthma in Puerto Ricans. PLoS One. 2013;8:e68473. doi: 10.1371/journal.pone.0068473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Silverberg JI, Hanifin JM. Adult eczema prevalence and associations with asthma and other health and demographic factors: a US population-based study. J Allergy Clin Immunol. 2013;132:1132–1138. doi: 10.1016/j.jaci.2013.08.031. [DOI] [PubMed] [Google Scholar]
- 43.Forno E, Cloutier MM, Datta S, Paul K, Sylvia J, Calvert D, Thornton-Thompson S, Wakefield DB, Brehm J, Hamilton RG, et al. Mouse allergen, lung function, and atopy in Puerto Rican children. PLoS One. 2012;7:e40383. doi: 10.1371/journal.pone.0040383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kumar R, Nguyen EA, Roth LA, Oh SS, Gignoux CR, Huntsman S, Eng C, Moreno-Estrada A, Sandoval K, Peñaloza-Espinosa RI, et al. Factors associated with degree of atopy in Latino children in a nationwide pediatric sample: the Genes-environments and Admixture in Latino Asthmatics (GALA II) study. J Allergy Clin Immunol. 2013;132:896–905.e1. doi: 10.1016/j.jaci.2013.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nishimura KK, Galanter JM, Roth LA, Oh SS, Thakur N, Nguyen EA, Thyne S, Farber HJ, Serebrisky D, Kumar R, et al. Early-life air pollution and asthma risk in minority children: the GALA II and SAGE II studies. Am J Respir Crit Care Med. 2013;188:309–318. doi: 10.1164/rccm.201302-0264OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rosas-Salazar C, Ramratnam SK, Brehm JM, Han YY, Boutaoui N, Forno E, Acosta-Pérez E, Alvarez M, Colón-Semidey A, Canino G, et al. Prematurity, atopy, and childhood asthma in Puerto Ricans. J Allergy Clin Immunol. 2014;133:357–362. doi: 10.1016/j.jaci.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thakur N, Oh SS, Nguyen EA, Martin M, Roth LA, Galanter J, Gignoux CR, Eng C, Davis A, Meade K, et al. Socioeconomic status and childhood asthma in urban minority youths: the GALA II and SAGE II studies. Am J Respir Crit Care Med. 2013;188:1202–1209. doi: 10.1164/rccm.201306-1016OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Torgerson DG, Ampleford EJ, Chiu GY, Gauderman WJ, Gignoux CR, Graves PE, Himes BE, Levin AM, Mathias RA, Hancock DB, et al. Mexico City Childhood Asthma Study (MCAAS); Children’s Health Study (CHS) and HARBORS study; Genetics of Asthma in Latino Americans (GALA) Study, Study of Genes-Environment and Admixture in Latino Americans (GALA2) and Study of African Americans, Asthma, Genes & Environments (SAGE); Childhood Asthma Research and Education (CARE) Network; Childhood Asthma Management Program (CAMP); Study of Asthma Phenotypes and Pharmacogenomic Interactions by Race-Ethnicity (SAPPHIRE); Genetic Research on Asthma in African Diaspora (GRAAD) Study. Meta-analysis of genome-wide association studies of asthma in ethnically diverse North American populations. Nat Genet. 2011;43:887–892. doi: 10.1038/ng.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen W, Boutaoui N, Brehm JM, Han YY, Schmitz C, Cressley A, Acosta-Pérez E, Alvarez M, Colón-Semidey A, Baccarelli AA, et al. ADCYAP1R1 and asthma in Puerto Rican children. Am J Respir Crit Care Med. 2013;187:584–588. doi: 10.1164/rccm.201210-1789OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gibson PG, Henry RL, Shah S, Powell H, Wang H. Migration to a western country increases asthma symptoms but not eosinophilic airway inflammation. Pediatr Pulmonol. 2003;36:209–215. doi: 10.1002/ppul.10323. [DOI] [PubMed] [Google Scholar]
- 51.Abrams TE, Vaughan-Sarrazin M, Fan VS, Kaboli PJ. Geographic isolation and the risk for chronic obstructive pulmonary disease-related mortality: a cohort study. Ann Intern Med. 2011;155:80–86. doi: 10.7326/0003-4819-155-2-201107190-00003. [DOI] [PubMed] [Google Scholar]