Abstract
Background
Clinical training in most medical schools, including the Catholic University of Health and Allied Sciences (CUHAS), is offered in the form of junior and senior rotations. During these clinical rotations, students are expected to acquire and master the basic procedural skills. However, students’ learning process should be evaluated for quality improvement.
Objectives
This study was conducted to identify the basic medical procedural skills that third-year medical students should acquire and master and determine the level of students’ exposure on these procedures at the end of junior rotation in internal medicine. Identification of the gap between clinicians’ opinions, skills practiced by students, and third-year students’ curriculum in the medical department at CUHAS was also done.
Methods
The descriptive cross-sectional study was used to collect data through a self-administered, structured questionnaire from clinicians in medicine. A review of logbooks was considered to determine level of students’ exposure, and a document analysis was done using existing medical curriculum.
Results
The response of 71% (n=22) was obtained. Clinicians agreed on basic procedures that students should perform independently (ie, Foley catheter insertion, venipuncture, and intravenous drip insertion). Clinicians thought that lumbar punctures, abdominal paracentesis, and nasogastric tube insertion should be done under minimal supervision. A considerable number of students (25%, n=75) did not practice any procedure throughout their rotation. The majority of the students performed venipuncture independently (82.14%, n=56) and lumbar punctures (73.21%, n=56) under supervision. Less than 25% (n=56) of the students met the required number of exposures on the basic procedures. The procedures to be performed and the level of competency in the procedures are not specified in the current curriculum.
Conclusion
The study identified the procedures that should be taught and practiced by students. It also highlighted the discrepancies in the existing curriculum and the need to monitor and supervise students’ practice.
Keywords: basic procedures, internal medicine rotation, Tanzania, medical education, logbooks, procedural skills, clinical clerkship
Introduction
Qualified junior doctors are often required to work in resource-constrained settings because of severe shortages of doctors on the African continent. Junior doctors in such settings are expected to perform a range of medical procedures.1 The expectation for junior doctors to work competently and confidently is, however, not always achieved.2–6 In developing countries, medical students learn most of the required clinical skills while directly in contact with patients during clinical rotations. Studies have indicated great inconsistencies in the competencies of medical students, residents, and internists.2–6 Engum7 listed factors such as the lack of human and physical resources (including skills laboratories), limited clinical exposure, and the use of traditional curricula as factors that may compromise the quality of medical training. A further concern for medical educators is the finding that suggests that a considerable number of students may complete clinical rotations and medical training without adequate clinical exposure and therefore are deficient in basic clinical skills.1,2,7
Medical training in Tanzania is a 5-year program. It is structured in modules that are offered per semester. The first 2 years focus on biomedical science subjects, and the final 3 years cover clinical rotations. Clinical training in most medical schools, including the Catholic University of Health and Allied Sciences (CUHAS), is structured into junior and senior clerkships in four major clinical departments. These departments are internal medicine, surgery, obstetrics and gynecology, and pediatric and child health. Junior rotations commence in the second half of the third year that involve student placements for 10 weeks in each of the four departments. During the rotation, students keep a logbook record of at least five sessions in which they had performed and/or assisted in any of the listed medical procedures. The list of medical procedures was subsequently developed by experts from each department based on their experiences. It is reflected in the current logbook, and students are expected to perform or assist with the procedures prior to the start of their senior rotations. The average numbers of procedures performed per month in the medical department differ considerably. Venipuncture, intravenous (IV) drip insertion, and peripheral venous insertion are commonly performed procedures, while throat swabbing, arterial puncture, and central venous catheterization are rarely performed procedures.
In the absence of a standardized exit examination to attest junior doctors’ exit level competencies, there is a concern regarding their competence at the end of medical training. The aim of this study was, therefore, to identify a set of basic medical procedural skills that third-year medical students should acquire and master at the end of junior rotation. Secondly, the logbook review was done to determine students’ level of exposures on the identified procedures. Finally, a document analysis was undertaken to identify gaps between the procedures practiced by the students and learning objectives outlined in the existing third-year students’ curriculum in the medical department at CUHAS.
Methods
Study setting
This study was conducted at Bugando Medical Center (BMC), which is the referral and teaching hospital for CUHAS in northwest Tanzania.
Study design
This descriptive cross-sectional study was conducted to identify the basic procedural skills that students should acquire and master by the end of junior rotation in internal medicine. An analytical review of the logbook was done to examine students’ exposure to the skills, while a comparative document analysis provided insight on existing discrepancies between the skills practiced by the students and learning objectives outlined in third-year medical curriculum.
Participants
All 22 clinicians from the department of internal medicine and all third-year students who completed their junior rotation in internal medicine during the study period (September 2012 to March 2013) were invited to participate in the study.
Permission was sought and obtained from joint BMC hospital and CUHAS ethical committee. Participation in the study was completely voluntary, and participants were informed of their rights to anonymity and withdrawal prior to giving consent.
Sample size, sampling procedures, and data collection plan
All 22 clinicians and 75 of 151 registered third year students of 2012/2013 who completed the internal medicine rotation during the study period were eligible for this study; hence, a convenient sample of students was selected.
A list of basic procedures included in the questionnaire was obtained from the Medical School Objectives Project, Report 1 from Association of American Medical Colleges, and Sanders et al’s study findings2,8 and were combined with those listed in the students’ logbooks. This was done due to the fact that even though the Tanzania Commission for Universities advocates for competency-based curricula for medical schools, CUHAS still uses a content-based curriculum, and therefore competences often demanded are not defined in the current curriculum. A self-administered, structured questionnaire was circulated to the participating clinicians for their input. The questionnaire asked clinicians to indicate their degree of agreement that the listed procedural skill should have been taught by the end of the third-year rotation. For each of the listed skills, clinicians had to respond by selecting either agree, neutral, or disagree. The generated list of skills contained IV drip insertion, venipuncture, Foley catheterization, lumbar puncture, arterial puncture, nasogastric tube insertion, abdominal paracentesis, thoracentesis, throat swabbing, peripheral venous line insertion, and central venous catheterization. The second question inquired about the level of competency that students needed to demonstrate at the end of the rotation on each of the listed skills. Respondents were given three options as to whether students should perform the procedure 1) independently, 2) with supervision, or 3) should only have observed the procedure. The level of exposure suggested by the clinicians on the basic procedures (five times) was checked against the completed logbooks of the third-year medical students.
The logbooks of 75 students who completed the junior rotation in medical department were reviewed, while document analysis existing medical curriculum was conducted. Themes outlining the learning objectives related to medical procedures during junior rotation in internal medicine were generated and interpreted.
Statistical analysis
The descriptive statistics were performed on the quantitative data. Frequency tables were used to illustrate the percentage of agreement on the identified basic medical procedural skills, and bar charts were used to display students’ exposure as recorded in their logbooks. A basic medical procedure was included upon a majority agreement (more than 75%) by the clinician respondents. Document analysis on medical curriculum was done to identify the gaps in the third-year medical curriculum regarding basic medical skills competency. Themes were manually generated and coded with respect to basic procedures to be acquired in the third year.
Results
The response rate was 71%; 15 of 22 clinicians responded to the questionnaire. Seven clinicians who did not respond were junior doctors. The teaching experiences among respondents varied from 2 years for junior clinicians to 10 years for senior clinicians. Although all respondents had been involved in teaching activities, only eight (53%) reported ever having read the existing medical curriculum. Five of the eight clinicians (62%) reported that their day-to-day teaching had been aligned with the curriculum. Nineteen of the 75 logbooks that had been reviewed for analysis were empty, hence excluded from further analysis after performing sensitivity analysis that showed no significant difference on the conclusion of the study findings.
Clinicians’ opinions on basic medical procedures
From the circulated list, respondents identified six basic procedures as indicated in Table 1 for medical students to have acquired by the end of the junior rotation. The majority of the clinicians strongly agreed on the six procedures to be included, namely intravenous drip insertion, venipuncture, nasogastric tube insertion, Foley catheterization, lumbar puncture, and abdominal paracentesis. Central venous catheterization was the only procedure in which clinicians did not strongly agree on its inclusion as a basic procedure. Of the six identified procedures; Foley catheterization was the only skill that was not listed in the students’ logbooks, indicating a lack of information of practice on this procedure.
Table 1.
The list of medical procedures that 15 clinicians agreed on
| Medical procedure | Level of agreement to be a basic procedure
|
||
|---|---|---|---|
| Strongly agree, n (%) | Neutral, n (%) | Strongly disagree, n (%) | |
| IV drip insertion | 15 (100) | 0 | 0 |
| Venipuncture | 15 (100) | 0 | 0 |
| Nasogastric tube | 15 (100) | 0 | 0 |
| Foley catheterization | 14 (93.3) | 1 (6.7) | 0 |
| Lumbar puncture | 13 (86.7) | 2 (13.3) | 0 |
| Abdominal paracentesis | 13 (86.7) | 2 (13.3) | 0 |
| Peripheral venous insertion | 8 (53.3) | 3 (20.0) | 4 (26.7) |
| Throat swabbing | 7 (46.7) | 7 (46.7) | 1 (6.6) |
| Arterial puncture | 7 (46.7) | 6 (40.0) | 2 (13.3) |
| ECGa reading | 2 (13.3) | 9 (60.0) | 4 (26.7) |
| Central venous catheterization | 0 | 5 (33.3) | 10 (66.7) |
Notes:
ECG is also referred to as EKG.
Abbreviations: IV, intravenous; ECG, electrocardiogram.
Clinicians’ opinions on level of competence on identified basic medical procedures
Although participants identified six basic procedures for medical students to acquire during junior rotation, the level of competence required of students differed among clinicians (Tables 1 and 2). Venipuncture, IV drip insertion, and Foley catheterization were identified as basic procedures that students should perform independently at the end of rotation. More than 50% of respondents agreed that performing lumbar puncture and abdominal paracentesis should be included as basic procedures for students to perform under necessary supervision. Inserting nasogastric tube was mentioned as a basic procedure, although its competence was not agreed upon.
Table 2.
Identified level of competency on basic procedures by the end of rotation
| Medical procedure | Level of competence student should perform by the end of internal medicine junior rotation (n=15)
|
||
|---|---|---|---|
| Independently, n (%) | Supervised, n (%) | Observe only, n (%) | |
| Venipuncture | 13 (86.7) | 2 (13.3) | 0 |
| IV drip insertion | 10 (66.7) | 4 (26.7) | 1 (0.07) |
| Foley catheterization | 8 (53.3) | 6 (40.0) | 1 (0.07) |
| Nasogastric tube | 7 (46.7) | 7 (46.7) | 1 (0.07) |
| Lumbar puncture | 3 (20.0) | 10 (66.7) | 2 (13.3) |
| Abdominal paracentesis | 3 (20.0) | 10 (66.7) | 2 (13.3) |
| Throat swabbing | 3 (20.0) | 8 (53.3) | 4 (26.7) |
| Peripheral venous insertion | 3 (20.0) | 7 (46.7) | 5 (33.3) |
| ECGa reading | 2 (13.3) | 7 (46.7) | 6 (40.0) |
| Arterial puncture | 0 | 8 (53.3) | 7 (46.7) |
| Central venous catheterization | 0 | 3 (20.0) | 12 (80.0) |
Note:
ECG is also referred to as EKG.
Abbreviations: IV, intravenous; ECG, electrocardiogram.
Students’ exposure on identified basic procedures
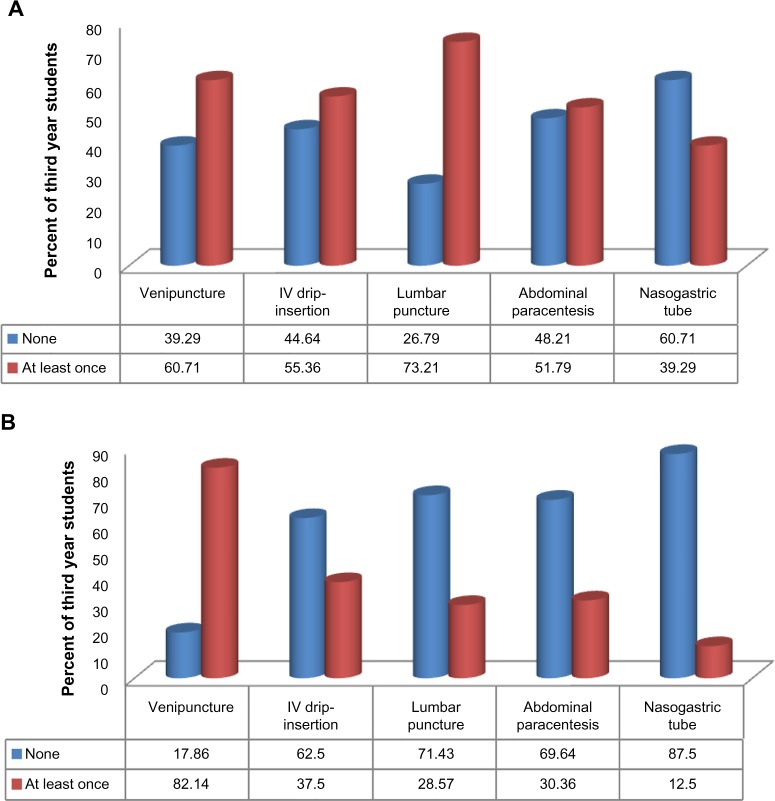
Over the period of junior and senior clinical rotations, students keep a logbook record of the number of procedures that they assist and perform, and this logbook is monitored by residents and faculty. The logbook contains specific procedures namely venipuncture, IV drip insertion, cutdown, lumbar puncture, abdominal paracentesis, throat swabbing, and inserting nasogastric tube. A comparison between the logbook list and the clinician-identified list reveals the absence of Foley catheterization. There is thus no information available on students’ exposure level on this procedure. About 25% (19/75) of the students did not perform any procedures during their rotation. Based on 56 logbooks, the students’ exposure to the procedures differed considerably, with the majority of them neither assisting nor performing nasogastric tube and abdominal paracentesis procedures (Figures 1A and B).
Figure 1.
Medical procedures that the 56 students (A) assisted in and (B) performed.
Abbreviation: IV, intravenous.
Majority of the students assisted in venipuncture, IV drip insertion, lumbar puncture, and abdominal paracentesis at least once during their rotation (Figure 1A). With reference to the independent performance of procedures, we found that venipuncture (82%) was the most performed procedure (Figure 1B). Although the majority (73%) of the third-year medical students assisted with the lumbar puncture procedure, tentatively few (~29%) performed it independently (Figures 1A and B).
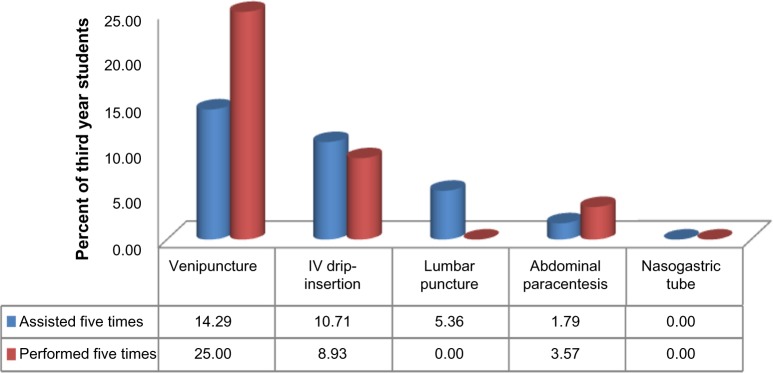
Based on departmental requirement of performing and assisting procedures five times, it appears that only a few students met the department stipulation in terms of the number of exposures, and these were mainly in venipuncture and IV drip insertion (Figure 2). Venipuncture was still the only procedure that a higher proportion of third-year students performed independently than those who assisted with the procedure (25% vs 14%). None of the students assisted or performed nasogastric tube insertion as per departmental requirement.
Figure 2.
Medical procedures that 56 students performed/assisted as per departmental requirement.
Abbreviation: IV, intravenous.
Discrepancies on current medical curriculum
A document analysis was undertaken to provide insight on the discrepancies between the procedures outlined in the current curriculum and the procedures practiced by the students. The current content-based curriculum at CUHAS does not clearly specify a list of medical procedures. It is structured in modules and delivered in a semesterized system and is heavily content-orientated. The medical students cover biomedical science subjects including anatomy, biochemistry, basic and clinical physiology, behavioral sciences, developmental studies, microbiology/immunology, parasitology/entomology, introduction to clinical methods, pathology, and epidemiology and research methods in the first 2 years. They learn clinical pharmacology, management of diseases, and medical ethics in their third year. The management of diseases is supposed to fit in the respective departments, but the program does not outline how students should acquire the basic procedure. There is also no guidance on the level at which to expect competent performance from students.
Discussion
This study used the opinions of clinicians to identify the basic medical procedures and the level of competence required of medical students by the end of their junior rotation in the internal medicine department. The procedures identified for independent practice included venipuncture, IV drip insertion, and Foley catheterization. The procedures to be performed under supervision included lumbar puncture and abdominal paracentesis. Faculty thought that students should not attempt a central venous catheterization. The identified procedures, with the exception of the abdominal paracentesis procedures, had also been emphasized in other studies.2,7,8 Knowledge of basic procedures and competency-based frameworks for medical students is important as it provides a link between undergraduate and postgraduate training.9 A far greater concern is findings of studies showing that some students complete medical training without performing any procedures6,10 and/or without becoming competent in specified skills.6,11 Venipuncture and IV drip insertion are procedures that students should be able to perform with assistance and independently at the end of rotation. However, a considerable proportion of students did not perform these procedures despite the availability of adequate opportunities. Other studies revealed similar findings in which students had not been guided toward clinical practice of basic procedures despite there being opportunities to do so.1,5,7,12 However, venipuncture was the only procedure that students highly recorded as having practiced independently during rotations. This could be explained by the fact that venipuncture is the most common procedure performed in the wards, thus providing plenty of opportunities to students. In addition, venipuncture is a relatively easy procedure to perform compared to other procedures like lumbar puncture, nasogastric tube insertion, and abdominal paracentesis.
There were also some procedures namely arterial puncture, throat swabbing, and peripheral venous insertion in which the clinicians did not agree on the level of competency required of students. The implication of this disagreement may be reflected in inconsistent training, because the curriculum does not stipulate skills training as a basic requirement. The disagreement among clinicians on what students should be taught may have far-reaching effects on the ultimate competency and clinical skills acquisition of the students.
Most students did not perform lumbar puncture, nasogastric tube insertion, and abdominal paracentesis independently. However, based on clinicians’ expectation, this was not surprising since the procedures were deemed to be performed under supervision. A study by Coberly and Goldenhar5 identified lumbar puncture as one of six basic procedures for competence in fourth-year medical students. Although venipuncture was highly performed, students reportedly lacked competence in performing the procedure effectively.5 Similar findings were observed among students who showed high proficiency in venipuncture, IV placement, Foley catheter placement, and arterial puncture.2 It is also possible that students are not well prepared as had been reported in Moghadami’s et al’s13 study. Residents are expected to have competency in basic procedures such as lumbar puncture, insertion of a peripheral IV line, nasogastric tube, and a Foley catheter at entry.3 Insufficient skills to perform important clinical procedures were observed among medical students, interns, junior doctors, and residents.4,6,12 These deficiencies could be traced back to the junior rotation in which basic procedures should be practiced to gain competence.
In addition, this study revealed that only a few students performed the required number of departmental procedures. This could be attributed to the insufficient number of some procedures being conducted in the department. This finding led to clinical rotations have currently been extended to other district hospitals. Other studies have also found that reasons for poor performance and incompetence in some basic procedures may be attributed to the lack of a well-defined curriculum, which fails to emphasize the clinical components to be developed during medical training.2
With bedside teaching as the mode of clinical teaching, it is possible that the logbooks may not adequately reflect the overall competency of students but rather reflect exposure to procedures. The absence of clearly specified criteria in the curriculum to judge students’ competency may have added to the widening of the competency gap, as it would be difficult to reinforce any expectations from students without such curricular guidance.6,11,14 Although clerkship may not provide sufficient skill training to students,15 the overall completion of logbooks by only 75% of the students not only suggests a lack of commitment from the students but also the inadequacy of the supervisory process during the rotation. With the existing curriculum at CUHAS lacking in specific learning objectives for the junior rotation, clinicians may focus on opportunistic conditions that present in the wards and disregard some other required procedures.
Limitations of the study included the sample involving only half of the third-year cohort who completed internal medicine rotation during the study period and hence may suffer the effect of small sample size. Identifying the basic procedures was only done once from a single medical institution. The study could have been improved with use of Delphi model.
Conclusion and recommendations
This study has identified the basic procedures to be taught and mastered by third-year students in the department of medicine. The skills include Foley catheter insertion, venipuncture, IV drip insertion, lumbar puncture, paracentesis, and nasogastric tube insertion. Although some students performed the basic procedures with minimal supervision and independently, a considerable number of students completed their junior rotation without performing all the identified basic procedural skills. This finding has highlighted the need for an efficient monitoring system to assess students’ exposure and competency to basic procedures, which we believe will facilitate their transition from the junior to the senior clinical rotations and ultimately ensure their competent practice as professionals. The curriculum needs to be reviewed to improve the setting of clear and defined outcomes that lead to competency on the identified skills.
With the increasing number of students at medical schools, students’ exposure to patients may be limited, hence leading to inadequate exposure to basic procedural skills. In order to address this challenge, CUHAS is in the process of implementing several measures including changing the medical curriculum from the current content-based curriculum to competency-based curriculum. The use of simulation and clinical skills laboratories will be highly emphasized in order to provide a safe and protected environment in which students can practice clinical skills before using them in real clinical settings. Lastly, CUHAS is planning to include more hospitals that will be used as teaching sites to increase students’ exposure to clinical practice.
Acknowledgments
The authors extend their gratitude to Touch Foundation, CUHAS Management, and SAFRI fellows for their financial and moral support. Without the support of Dean of School of Medicine, this study would not have been done, thank you indeed. The authors would like to extend their gratitude to all participants.
Footnotes
Disclosure
The authors report no conflicts of interest in this work. The funders mentioned had no role in the design of the study, data collection and analysis, the decision to publish, or the preparation of the manuscript for publication.
References
- 1.Wu EH, Elnicki DM, Alper EJ, et al. Procedural and interpretive skills of medical students: experiences and attitudes of third-year students. Acad Med. 2006;81(10 Suppl):S48–S51. doi: 10.1097/00001888-200610001-00013. [DOI] [PubMed] [Google Scholar]
- 2.Sanders CW, Janine CE, Thomas KB. A survey of basic technical skills of medical students. Acad Med. 2004;79(9):873–875. doi: 10.1097/00001888-200409000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Langdale AL, Doug S, Joyce W, Susan Ml, Louis V, Craig SS. Preparing graduates for the first year of residency: are medical schools meeting the need? Acad Med. 2003;78(1):39–44. doi: 10.1097/00001888-200301000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Burch VC, Nash RG, Zabow T, et al. A structured assessment of newly qualified medical graduates. Med Educ. 2005;39:723–731. doi: 10.1111/j.1365-2929.2005.02192.x. [DOI] [PubMed] [Google Scholar]
- 5.Coberly L, Goldenhar LM. Ready or not, here they come: acting interns’ experience and perceived competency performing basic medical procedures. J Gen Intern Med. 2007:491–494. doi: 10.1007/s11606-007-0107-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Promes BS, Chudgar MS, Grochowski CO, et al. Gaps in procedural experience and competency in medical school graduates. Acad Emerg Med. 2009;16:S58–S62. doi: 10.1111/j.1553-2712.2009.00600.x. [DOI] [PubMed] [Google Scholar]
- 7.Engum SA. Do you know your students’ basic clinical skills exposure? Am J Surg. 2003;186(2):175–181. doi: 10.1016/s0002-9610(03)00182-x. [DOI] [PubMed] [Google Scholar]
- 8.Association of American Medical Colleges The Medical School Objectives Writing Group: learning objectives for medical school education-guidelines for medical schools. Report 1 of the Medical School Objectives Project. Acad Med. 1994;74:13–18. doi: 10.1097/00001888-199901000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Frank JR, Snell LS, Cate OT, et al. Competency-based medical education: theory to practice. Med Teach. 2010;32(8):638–645. doi: 10.3109/0142159X.2010.501190. [DOI] [PubMed] [Google Scholar]
- 10.Moercke A, Eika B. What are the clinical skills levels of newly graduated physicians? Self-assessment study of an intended curriculum identified by a Delphi process. Med Educ. 2002;36:472–478. doi: 10.1046/j.1365-2923.2002.01208.x. [DOI] [PubMed] [Google Scholar]
- 11.Charlotte R, Torben S, Jorgen H, et al. Medical students’ experience in practical skills is far from stakeholders’ expectations. Med Teach. 2001;23(4):412–416. doi: 10.1080/01421590120043017. [DOI] [PubMed] [Google Scholar]
- 12.Dehmer J, Amos K, Farrell T, Meyer A, Newton W, Meyers M. Competence and confidence with basic porcedural skills: the experience and opinions of fourth-year medical students at a single institution. Acad Med. 2013;88(5):682–687. doi: 10.1097/ACM.0b013e31828b0007. [DOI] [PubMed] [Google Scholar]
- 13.Moghadami M, Amini M, Mahbudi A, Raeeat D, Panahi B. Procedural skills training in medical undergraduate curriculum, a multi center study from 3 universities in southern Iran. J Med Educ. 2009;13(4):121–125. [Google Scholar]
- 14.Matheson C, Matheson D. How well prepared are medical students for their first year as doctors? The views of consultants and specialist registrars in two teaching hospitals. Postgrad Med J. 2009;85:582–589. doi: 10.1136/pgmj.2008.071639. [DOI] [PubMed] [Google Scholar]
- 15.Remmen R, Albert JS, Derese A, et al. Unsatisfactory basic skills performance by students in traditional medical curricula. Med Teach. 1998;20(6):579–582. [Google Scholar]