Abstract
♦ Background:
A functioning catheter is vital to the success of peritoneal dialysis (PD). Catheter complications related to the insertion procedure remain a major hindrance to PD utilization. Most catheters are placed by surgeons. Suboptimal catheter outcomes appear to be related to inadequate training and experience during surgical residency and the absence of educational opportunities to remedy this deficit once the surgeon is in practice.
♦ Objective:
The aim of this report is to describe a 1-day comprehensive surgeon training program in PD access surgery and to convey the results of the first 7 courses.
♦ Methods:
Needs assessment data served as the foundation for formulating course objectives and content. A disease-based approach to PD was taken to provide both didactic instruction and laboratory exercises. Surgical simulators permitted skills development for each key task in catheter placement. Educational outcomes were measured with pre- and post-tests, course evaluation, and follow-up survey.
♦ Results:
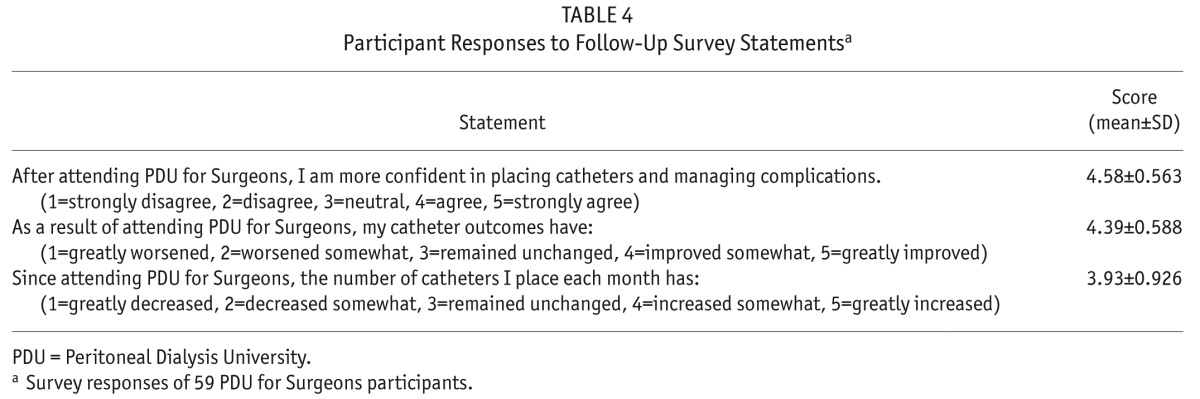
Seven courses were attended by 134 surgeons with an average faculty to participant ratio of 1:4 during hands-on laboratory sessions. Pre- and post-testing demonstrated a class-average normalized educational gain of 50%. On a 5-point Likert scale, the course was scored highly on 14 areas of evaluation with average responses ranging from 4.4 to 4.9. A follow-up survey conducted a mean of 28 months after the programs revealed significantly increased utilization of all 10 course-targeted PD access skills. Participants gave mean scores of 4.6 for improved confidence in case management and 4.4 for better catheter outcomes.
♦ Conclusions:
A comprehensive 1-day peritoneal access training course can produce long-term self-assessed improvement in surgical management and PD catheter outcomes.
Keywords: Surgical education, surgical skills course, simulation training, learning gain, peritoneal catheter placement, peritoneal dialysis
The success of peritoneal dialysis (PD) as renal replacement therapy depends upon a functional peritoneal catheter. After infectious complications, catheter mechanical problems are the most common reasons for PD failure, accounting for approximately 20% of patient transfers to hemodialysis during the first year (1–3). Most catheter malfunctions can be attributed to procedural errors and/or omission of recognized best practices and proactive techniques during catheter implantation (4,5). The incidence of catheter failure is probably much higher than reported since patients who never start therapy because of catheter dysfunction from the outset are not included in dialysis service databases (1,2). In addition, it is unknown what proportion of catheters removed for infectious complications is due to poor technique in subcutaneous tunnel construction and unfavorable exit-site location. Undoubtedly, lack of familiarity with appropriate catheter rescue and salvage procedures for mechanical and infectious complications further contributes to the catheter loss rate.
The majority of PD catheters are placed by surgeons, amounting to almost 80% of catheter insertion procedures performed in the United States (6). Disappointing outcomes are thought to be due to inadequate training and experience in catheter insertion methods. In a national survey of US surgery training programs, Wong et al. found that 82% of programs reported training residents in PD catheter placement (7). During their surgical residency, 23% of trainees placed ≤ 2 catheters and 61% placed ≤ 5 catheters. Only 13% of residents placed > 10 catheters. Low PD utilization by nephrologists seemed to be a major driving factor for insufficient PD access experience because of low procedure volumes. It is likely, however, that frequent catheter complications resulting from inadequate surgical instruction discouraged nephrologists from making PD referrals. Fewer referrals prevent surgical trainees from ever gaining sufficient experience in catheter placement, perpetuating a vicious cycle of unacceptable outcomes, dissatisfaction with PD, and low PD utilization.
After surgical residency, practicing surgeons tend to perform procedures the way they were trained and are cautious about adopting a new technique that departs significantly from their previous practice or skill level without seeking some form of additional training. For practical reasons, they cannot afford to return to an apprenticeship environment to learn a new procedure and ethical concerns make it objectionable to use the operating room as a venue for acquisition of new technical skills. Therefore, there is a definite need for an educational program beyond the period of residency training to assist practicing surgeons to overcome the deficits in their peritoneal access surgery instruction. A complete educational experience would necessarily include both cognitive and skills development, recognizing that a hands-on opportunity is crucial for surgeons to learn new techniques (8).
The purpose of this report is to describe a 1-day comprehensive surgeon training program in PD access surgery comprised of both didactic sessions and a hands-on laboratory and to communicate the results of the first 7 courses.
Materials and Methods
Wake Forest University School of Medicine and the International Society for Peritoneal Dialysis (ISPD) jointly sponsored the development of a 1-day training course entitled Peritoneal Dialysis University for Surgeons (PDUS). The course planning committee identified educational needs that underlie professional practice gaps through study of ISPD guidelines and literature review. This needs assessment data served as the foundation for formulating the course objectives listed in Table 1. Creation of course content was in compliance with the Accreditation Council for Continuing Medical Education Standards for Commercial Support: Standards to Ensure Independence in Continuing Medical Education (CME) Activities (9).
TABLE 1.
Course Objectives
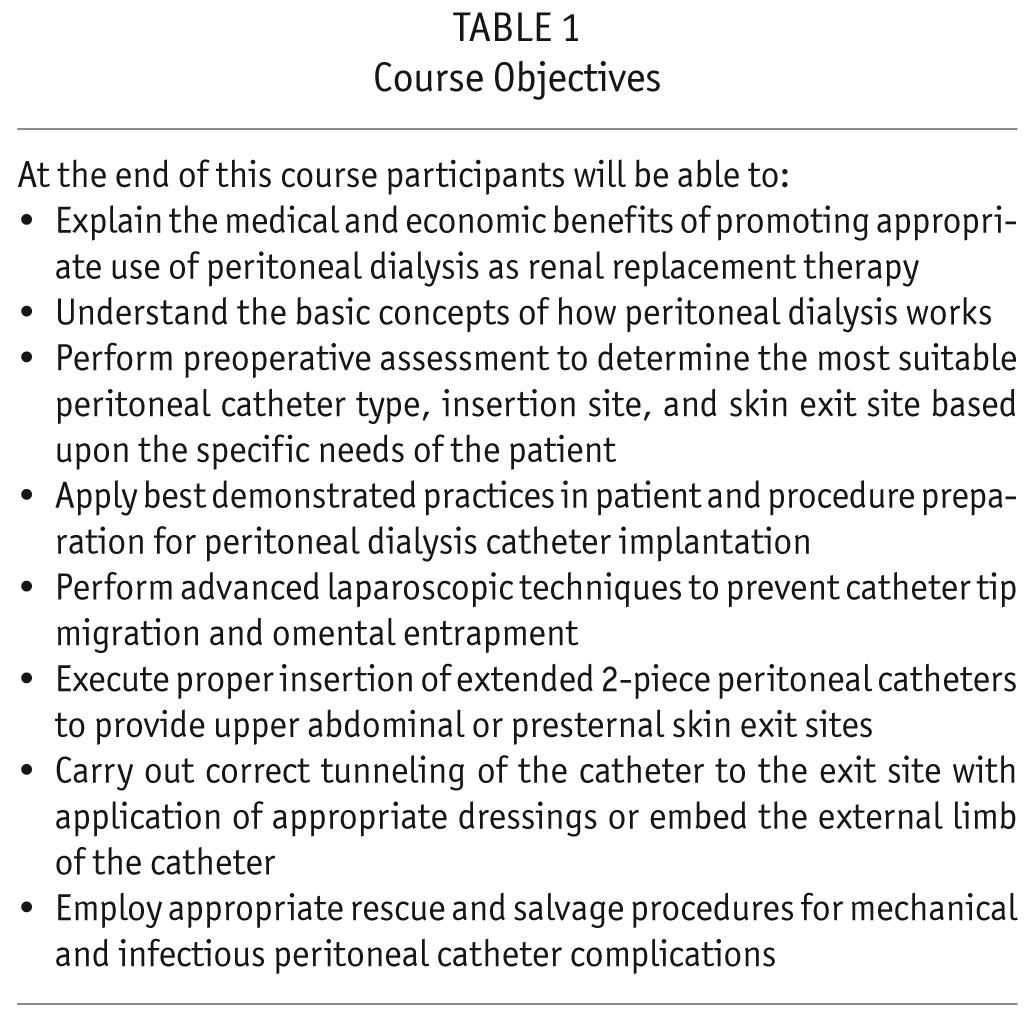
The curriculum was devised to provide both didactic instruction and laboratory exercises. Lecture topics were selected to give participants an in-depth background in medical and economic aspects of PD as renal replacement therapy and surgical fundamentals for providing and maintaining peritoneal access. A hands-on laboratory experience was developed to teach specific skills in performing access procedures. High-fidelity human torso simulators were constructed for this purpose so that attendees could learn and practice critical tasks in catheter placement. To assure sufficient hands-on exposure in the laboratory, 20 registrants were considered optimal course size to permit a group of 4 individuals to rotate through each of 5 faculty-supervised surgical skill stations. Course materials produced for distribution to the attendees included a syllabus with a printout of lecture slides, a laboratory guide, a surgeon's guidebook to PD access procedures, and a digital video disc demonstrating implantation techniques for PD catheters. Wake Forest University School of Medicine, the accrediting CME provider, designated this educational activity for a maximum of 8.25 American Medical Association Physician's Recognition Award Category 1 Credits. Courses were funded by participants' registration fees and unrestricted educational grants from industry and the ISPD.
A written test comprised of 20 questions was created to measure knowledge level before and upon completion of the course. An evaluation form was prepared to appraise the participants' perception of the effectiveness of the curriculum content and their overall satisfaction with how the course was conducted. The course evaluation employed a 5-point Likert scale with 1 being very low and 5 representing very high. A follow-up survey was designed to assess changes in the participants' surgical practices as a result of attending the course. All previous course participants received an invitation to participate in the online survey. The survey plan included 3 reminder invitations at 2-week intervals to non-responders.
Effectiveness of the educational experience as a whole was determined using pre-test and post-test scores to calculate class-average normalized educational gain (g). This metric is the ratio of the whole group's performance to the maximum achievable improvement and is expressed mathematically as:
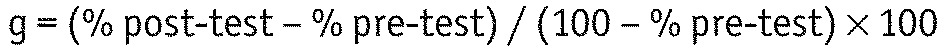 |
A value of g ≥ 30% was accepted as indicating an effective educational intervention (10–12).
Contingency table analyses were performed with chi-squared test for unpaired data and McNemar's test for paired data. Analyses were performed with GraphPad Prism version 6.02 and GraphPad QuickCalcs (GraphPad Software, San Diego, CA, USA). All results were considered significant at p < 0.05.
Results
Seven PDUS courses were conducted at major cities across the United States from November 2010 through June 2014. A total of 134 surgeons from private and academic practices attended the course, averaging 19.1 surgeons per event. The course pre-test was completed by 131 participants (97.8%) with a mean of 48.4% correct responses to test questions. The post-test was completed by 117 participants (87.3%) with a mean of 74.2% correct responses, representing a statistically significant improvement in test scores (p < 0.0001). Class-average normalized educational gain was 50%.
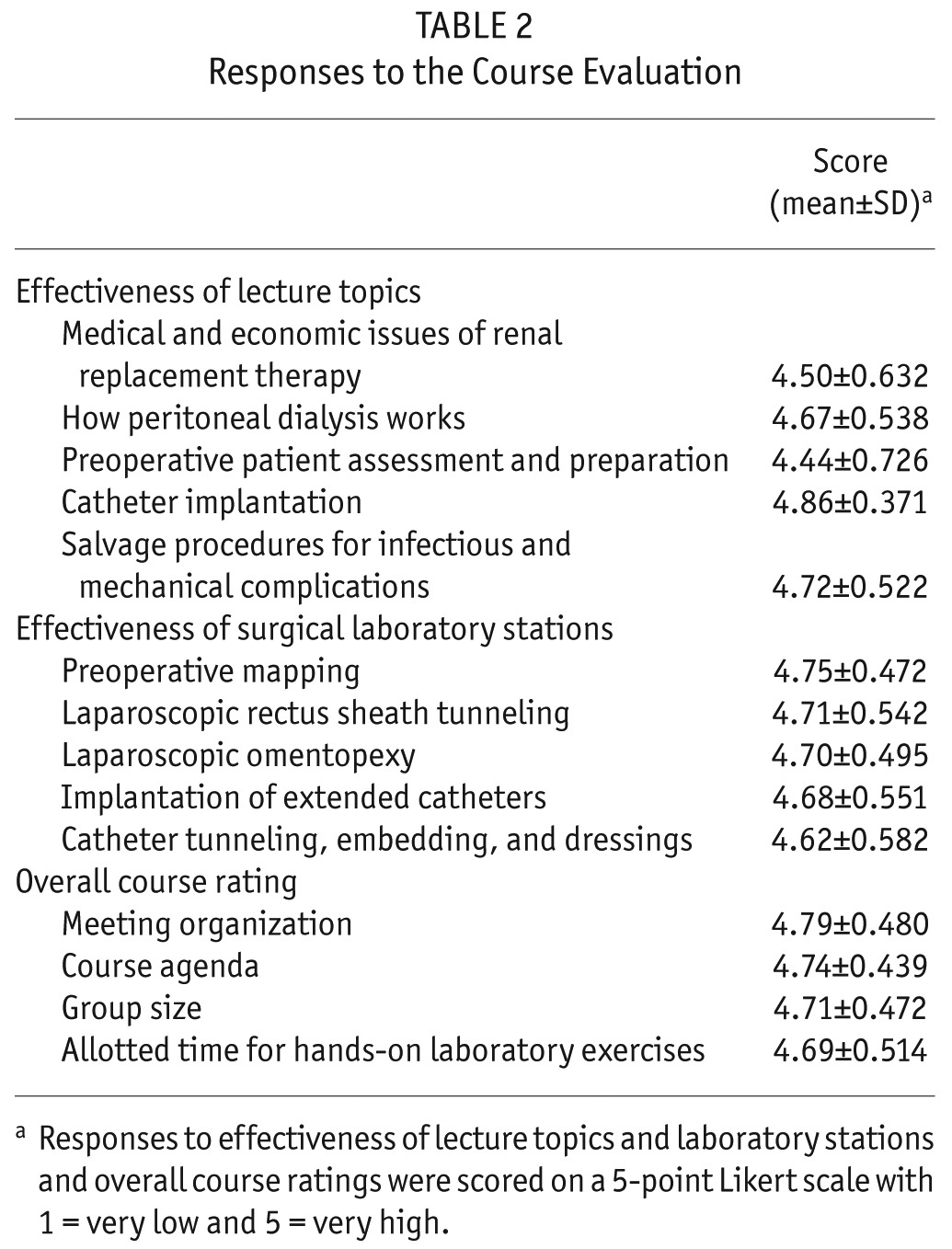
The course evaluation form was modified between the third and fourth sessions of the course; however, 14 questions remained common during the 2 time periods. The results of the course evaluations completed by 128 participants (95.5%) are summarized in Table 2. The course was scored highly in the 14 areas of the evaluation with average responses ranging from 4.44 to 4.86.
TABLE 2.
Responses to the Course Evaluation
Fifty-nine (44%) of the course participants responded to the online follow-up survey conducted a mean of 27.5 ± 13.8 months (interval: 5.6 – 49.2) after the PDUS programs. There was significantly increased utilization of all 10 course-targeted PD access skills (Table 3). After attending the PDUS, the participants felt more confident in their ability to place catheters and manage complications, their catheter outcomes were improved, and the volume of catheter placement procedures increased (Table 4).
TABLE 3.
Follow-Up Survey of Peritoneal Dialysis Access Procedure Utilizationa
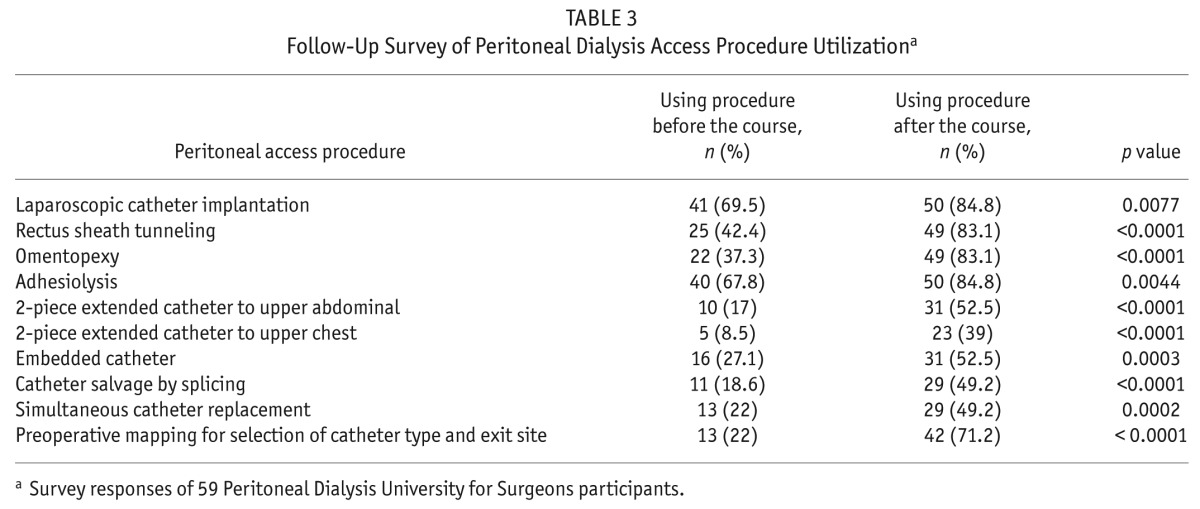
TABLE 4.
Participant Responses to Follow-Up Survey Statementsa
Discussion
A comprehensive 1-day training course in peritoneal access surgery fills a current educational deficit in surgical residency training and at the same time offers an effective learning program that minimizes the surgeon's time away from a busy practice. Peritoneal Dialysis University for Surgeons takes a disease-based approach to this educational experience by delivering in-depth knowledge about renal replacement therapy and provides a firm grasp of the cognitive elements related to PD access procedures. The course also recognizes the importance of providing the surgeon a hands-on opportunity to acquire new skills through the use of simulator-based training. The simulators permit guided learning, during which the participant acquires the skill to perform each step of the operative procedure under close supervision of an instructor.
Several metrics were used to gauge the success of the PDUS program, including pre- and post-tests, a course evaluation, and a follow-up survey. Pre- and post-tests were used to measure learning gain. While mean absolute learning gain (% post-test score – % pre-test score) was 25.8% and mean relative gain (% absolute gain / % pre-test score × 100) was 53.3%, we elected to use class-average normalized gain in order to diminish the confounding effects of pre-course knowledge and other potential baseline group characteristics. The normalized gain of 50% calculated for the PDUS program is well above the 30% threshold that is generally considered the minimum value at which educational interventions can be regarded as effective (10–12).
Course and follow-up survey evaluations using Likert scale analyses were employed to study the curricular effectiveness and perceived values of the PDUS educational experience. Participants uniformly gave high scores on all queried elements. The follow-up survey also indicated that there was a significant increase in utilization of surgical skills taught in the course. One of the limitations of evaluating the efficacy of the PDUS program is not being able to monitor clinical outcomes after surgeons start performing these acquired skills; however, there is strong research evidence that simulator-based training, when included as part of a structured program, results in effective skills transfer to the patient-based setting (13). Most medical educators would agree that knowledge and skill acquisition eventually leads to improved patient care (14).
The follow-up response rate of surveyed PDUS participants was 44%, not dissimilar to the 32 to 48% response rates of other physician surveys using comparable online or postal methodology (7,15–17). Low physician response rates have been attributed to survey fatigue, survey loss, time demands, and general indifference. Low response rates potentially introduce nonresponse bias. Therefore, the views of the fewer responders may not represent the views of the larger population being surveyed. However, nonresponse bias may be of less concern in physician surveys than in surveys of the general public (17).
The results of the first 7 PDUS programs is an encouraging start towards shaping a surgical workforce into capable PD access providers. With minimal modifications based upon specific geographic regional needs and/or resource limitations, the course structure can be adapted to create similar programs on an international level. An important spinoff of the PDUS has been the development of an interventionalist program for radiologists and nephrologists entitled Peritoneal Dialysis University for Interventionalists (PDUI). Scheduled in tandem with the PDUS courses, 2 PDUI programs have been conducted to date with the same favorable responses from the attendees. A common course objective now exists for both programs, namely, surgeons and interventionalists working collaboratively to develop common pathways and techniques to provide timely peritoneal access and to resolve PD complications. Dates and locations of future programs can be found under Events & Meetings on the ISPD website (www.ispd.org) or the individual websites for the PDUS (www.pdusurgeons.com) and PDUI (www.pduinir.com) programs.
Disclosures
JHC has served as a consultant for MedComp, Inc. and Baxter Healthcare and as a speaker for Baxter Home Therapies Institute, DaVita Healthcare Partners, and Fresenius Medical Care. TP is a Baxter Healthcare consultant and a speaker for DaVita Healthcare Partners and Fresenius Medical Care. SWA is a consultant and speaker for Baxter Healthcare. JB serves as a consultant, medical advisory board, for NxStage Medical.
Acknowledgments
This study was supported by an unrestricted educational grant from the Society for Education & Research in Peritoneal Access Surgery.
REFERENCES
- 1. Guo A, Mujais S. Patient and technique survival on peritoneal dialysis in the United States: evaluation in large incident cohorts. Kidney Int 2003; 64:S3–12. [DOI] [PubMed] [Google Scholar]
- 2. Mujais S, Story K. Peritoneal dialysis in the US: evaluation of outcomes in contemporary cohorts. Kidney Int 2006; 70:S21–6. [DOI] [PubMed] [Google Scholar]
- 3. Crabtree JH. Who should place peritoneal dialysis catheters? Perit Dial Int 2010; 30:142–50. [DOI] [PubMed] [Google Scholar]
- 4. Wong LP, Yamamoto KT, Reddy V, Cobb D, Chamberlin A, Pham H, et al. Patient education and care for peritoneal dialysis catheter placement: a quality improvement study. Perit Dial Int 2014; 34:12–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Crabtree JH. Peritoneal dialysis catheter implantation: avoiding problems and optimizing outcomes. Semin Dial 2015; 28:12–5. [DOI] [PubMed] [Google Scholar]
- 6. Physician/Supplier Procedure Summary Master File, 2013. Baltimore, MD: Centers for Medicare & Medicaid Services, Department of Health & Human Services. [Google Scholar]
- 7. Wong LP, Liebman SE, Wakefield KA, Messing S. Training of surgeons in peritoneal dialysis catheter placement in the United States: a national survey. Clin J Am Soc Nephrol 2010; 5:1439–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sachdeva AK. Acquiring skills in new procedures and technology: the challenge and the opportunity. Arch Surg 2005; 140:387. [DOI] [PubMed] [Google Scholar]
- 9. Accreditation Council for Continuing Medical Education Standards for Commercial Support : Standards to Ensure Independence in CME Activities. [Available online at: http://www.accme.org/requirements/accreditation-requirements-cme-providers/standards-for-commercial-support; accessed 3 September 2015]
- 10. Hake RR. Interactive-engagement vs traditional methods: a six-thousand-student survey of mechanics test data for introductory physics courses. Am J Phys 1998; 66:64–74. [Google Scholar]
- 11. Colt HG, Davoudi M, Murgu S, Rohani NZ. Measuring learning gain during a one-day introductory bronchoscopy course. Surg Endosc 2011; 25:207–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ezeala CC, Ram AA, Vulakouvaki N. Learning gain of pharmacy students after introducing guided learning with computer simulation in a pharmacology class in Fiji. J Educ Eval Health Prof 2013; 10:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dawe SR, Pena GN, Windsor JA, Broeders JA, Cregan PC, Hewett PJ, et al. Systematic review of skills transfer after surgical simulation-based training. Br J Surg 2014; 101:1063–76. [DOI] [PubMed] [Google Scholar]
- 14. Norman G. The American College of Chest Physicians evidence-based educational guidelines for continuing medical education interventions: a critical review of evidence-based educational guidelines. Chest 2009; 135:834–7. [DOI] [PubMed] [Google Scholar]
- 15. Grava-Gubins I, Scott S. Effects of various methodologic strategies: survey response rates among Canadian physicians and physicians-in-training. Can Fam Physician 2008; 54:1424–30. [PMC free article] [PubMed] [Google Scholar]
- 16. Thorpe C, Ryan B, McLean SL, Burt A, Stewart M, Brown JB. How to obtain excellent response rates when surveying physicians. Fam Pract 2009; 26:65–8. [DOI] [PubMed] [Google Scholar]
- 17. Kellerman SE, Herold J. Physician response to surveys. A review of the literature. Am J Prev Med 2001; 20:61–7. [DOI] [PubMed] [Google Scholar]


