Abstract
Objective:
Previous meta-analyses of cohort studies indicate a J-shaped relationship between alcohol consumption and all-cause mortality, with reduced risk for low-volume drinkers. However, low-volume drinkers may appear healthy only because the “abstainers” with whom they are compared are biased toward ill health. The purpose of this study was to determine whether misclassifying former and occasional drinkers as abstainers and other potentially confounding study characteristics underlie observed positive health outcomes for low-volume drinkers in prospective studies of all-cause mortality.
Method:
A systematic review and meta-regression analysis of studies investigating alcohol use and mortality risk after controlling for quality-related study characteristics was conducted in a population of 3,998,626 individuals, among whom 367,103 deaths were recorded.
Results:
Without adjustment, meta-analysis of all 87 included studies replicated the classic J-shaped curve, with low-volume drinkers (1.3–24.9 g ethanol per day) having reduced mortality risk (RR = 0.86, 95% CI [0.83, 0.90]). Occasional drinkers (<1.3 g per day) had similar mortality risk (RR = 0.84, 95% CI [0.79, 0.89]), and former drinkers had elevated risk (RR = 1.22, 95% CI [1.14, 1.31]). After adjustment for abstainer biases and quality-related study characteristics, no significant reduction in mortality risk was observed for low-volume drinkers (RR = 0.97, 95% CI [0.88, 1.07]). Analyses of higher-quality bias-free studies also failed to find reduced mortality risk for low-volume alcohol drinkers. Risk estimates for occasional drinkers were similar to those for low- and medium-volume drinkers.
Conclusions:
Estimates of mortality risk from alcohol are significantly altered by study design and characteristics. Meta-analyses adjusting for these factors find that low-volume alcohol consumption has no net mortality benefit compared with lifetime abstention or occasional drinking. These findings have implications for public policy, the formulation of low-risk drinking guidelines, and future research on alcohol and health.
There has been increasing discussion within the field of alcohol epidemiology regarding the scientific status of claimed health benefits from the consumption of alcohol in relatively low doses (Chikritzhs et al., 2015; Holmes et al., 2014). The status of the hypothesis that alcohol in moderation confers health benefits has implications for estimations of the global burden of disease from alcohol (Lim et al., 2012) and the development of public health policies to reduce alcohol’s harm (Babor et al., 2010) and national guidelines for low-risk alcohol use (Stockwell & Room, 2012).
It has been suggested that the epidemiological (Ronksley et al., 2011) and physiological evidence (Brien et al., 2011) for both an association and a causal mechanism is sufficiently compelling to recommend consideration of advising abstainers to drink. However, an increasing number of questions have been raised about the quality of the studies contained in these meta-analyses. We first summarize some reasons for skepticism and then present new meta-analyses that explore the extent to which alternative study designs enhance or minimize associations indicative of health benefits.
Theoretical and empirical background
Evidence of health benefits from alcohol use has been reported for implausible types and numbers of health conditions in observational longitudinal studies. Fekjaer (2013) identified a long list of such conditions (including deafness, hip fractures, the common cold, cancers, birth complications, dementia, and liver cirrhosis) in which the classic J-shape curve was observed, with lower risk for low-volume drinkers compared with abstainers. In some cases—notably a reduced likelihood of alcoholic liver cirrhosis among low-volume drinkers (Rehm et al., 2010) and of developmental disorders of infants born of low-volume drinking mothers (Kelly et al., 2009)—a causal basis for such associations is highly unlikely. These findings raise the question as to whether a range of lifestyle and/or genetic confounding factors that favor “moderate drinkers” over abstainers are responsible.
Naimi et al. (2005) reported that 27 (90%) of 30 potential adverse confounders for coronary heart disease were more prevalent among abstainers than among moderate drinkers. Fillmore et al. (2006) classified prospective studies on alcohol and health according to their definition of “an abstainer” (i.e., the reference group that all classes of drinker are typically compared with in these studies). They reported that when studies explicitly excluded former and occasional drinkers from the abstainer reference group, there was limited evidence of protection from moderate alcohol consumption. The underlying theory was that as people age and become unwell, they are more likely to quit or substantially reduce their alcohol consumption, leading to an exaggeration of the already poor health profiles of abstainers (Kerr et al., 2002; Shaper et al., 1988).
Consistent with this view, Mäkelä et al. (2005) showed that reclassifying former drinkers as abstainers, thereby placing them in the reference group, markedly lowered the relative risk (RR) estimates for all active drinkers. Taking a more rigorous approach to the role of potential bias caused by former drinkers, Liang and Chikritzhs (2013) argued that former drinkers should be combined with current drinkers when drinking groups are compared with lifelong abstainers and that bias is not eliminated by merely separating former drinkers from abstainers.
A recent investigation of a large cohort from the European Prospective Investigation into Cancer (EPIC; Bergmann et al., 2013) used an analysis that took into account mortality risks from multiple and competing causes at multiple points over the life course. A reduced risk of death from heart disease was associated with alcohol consumption, but only when study participants with a history of ill health were excluded from analysis. Such exclusions are often conducted to mitigate confounding but may also be a source of selection bias. The authors concluded: “The apparent health benefit of low to moderate alcohol-use found in observational studies could therefore in large part be due to various selection biases and competing risks, which are related to both lifetime alcohol use and risk of disease, usually occurring later in life” (Bergmann et al., p. 1789).
Competing risks are also an issue for studies of all-cause mortality because the comparative risk of different diseases varies across the life course (e.g., coronary disease usually occurs later in life than does injury, cancer, or liver disease). This in turn creates selection bias in the sampling of individuals available to participate in cohort studies, especially in older cohorts (Stockwell & Chikritzhs, 2013).
The kinds of methodological problems identified above are quite common in this literature, in particular the practice of misclassifying former and occasional drinkers as abstainers (Stockwell et al., 2012).
Objective and overall analytic strategy
The purpose of the current study was to investigate the extent to which abstainer reference group bias (e.g., mixing former and occasional drinkers with abstainers) and other potential study-level confounders influence the risk relationship between alcohol use and mortality. Changes in RR estimates will also be examined after progressively excluding studies from meta-analyses based on theory-driven methodological design problems outlined in previous critiques (Stockwell & Chikritzhs, 2013; Stockwell et al., 2012). Consistency of results across these different analyses will be assessed to address the question as to whether low-dose alcohol consumption provides net protection in relation to all-cause mortality.
Method
Overall approach
We performed a systematic review following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (Moher et al., 2009) on original prospective studies concerning the association between alcohol consumption and all-cause mortality. The study protocol was first approved as an R01 grant application to the U.S. National Institutes of Health (Award # 1RO1AAO19939–02) and is presented as online Appendix A. (See “Supplementary Materials” available with this article online.) The codebook is also available from the authors on request.
Inclusion criteria
Included studies were original English-language research articles published in the peer-reviewed literature that quantified the relationship between all-cause mortality and alcohol consumption among human populations in cohort studies. All genders, age groups, and subjects from any racial, ethnic, cultural, or religious groups were eligible for inclusion, regardless of geographic region. Studies were excluded if all-cause mortality outcomes could not be separated from morbidity outcomes. Studies were also excluded if the sample was defined in terms of pre-existing illness or poor health status. When more than one publication of the same study was available, the most recent or comprehensive in its treatment of potential bias and confounding was selected.
Data sources
We identified all potentially relevant English-language articles published up to December 31, 2014, by searching PubMed (last searched February 25, 2015) and the Web of Science and through reference list cross-checking of previous meta-analyses.
Search strategy
We used the following key words and subject headings to identify relevant articles in electronic databases: [mortality OR death OR coronary heart disease OR coronary artery disease OR ischemic heart disease OR atherosclerotic heart disease] AND [alcohol OR consumption OR ethanol OR alcohol drinking] AND [cohort OR prospective OR longitudinal].
Study selection
Two trained reviewers read the titles of all the citations retrieved from the electronic database searches and removed those clearly unrelated to the relationship between mortality and alcohol consumption. At the next stage of study selection, abstracts were reviewed to further exclude studies that clearly did not meet inclusion criteria. At the third stage, the full articles were checked for eligibility with cross-checking by senior investigators. Reasons for exclusion were documented at each stage. The reference lists from two previous meta-analyses—Fillmore et al. (2006) and Ronksley et al. (2011)—also were searched for additional eligible studies that would not otherwise have been included.
Data extraction
Two reviewers extracted and coded data from all studies fulfilling the inclusion criteria, and any disagreements were resolved by discussion with the investigators. The original Fillmore et al. (2006) codebook was refined to provide more detailed classifications of the type of reference groups used and methods of quantifying alcohol consumption and study characteristics. The coding of all variables in the analysis presented here was double-checked by the first two authors (T.S. and J.Z.).
Data items
Summary measures of outcome.
The outcome of interest was defined as all-cause mortality. Hazard ratios and rate ratio estimates of mortality in individual studies were used as the RR estimates. Where studies only reported mortality rates, these were converted to RR estimates (Woodward, 2000). When occasional drinkers were the reference category and risk for abstainers was independently assessed, risk values were recalculated with abstainers as the reference group (Fillmore et al., 2006).
Measures of alcohol consumption.
The primary exposure variable of interest was mean daily alcohol consumption in grams of ethanol assessed at baseline. When studies did not define the grams of alcohol per unit or drink, we used published sources for country-specific estimates of typical drink size varying from 8 g in the United Kingdom to 19.75 g in Japan (see Appendix A) (International Center for Alcohol Policies, 2010; Turner, 1990).
We converted alcohol intake into grams per day using the midpoints of reported categories. For open-ended top categories (e.g., ≥6 drinks/day) we followed other meta-analysts by adding three quarters of the range of the next lowest category to the lower bound (e.g., if 3–5 drinks, this would be 6+((5–3) × 0.75) = 7.5) (Roerecke & Rehm, 2012). It was necessary to make some assumption or estimate of mean consumption for these upper unbounded categories.
We used a predetermined definition of “low-volume” drinking (up to 20 g of ethanol per day for both men and women) against which to test the health benefits hypothesis based on Australian National Health and Medical Research Council low-risk drinking guidelines (National Health and Medical Research Council of Australia, 2009). This was operationalized as up to 24 g per day given that respondents in the studies reported whole drinks rather than grams: 24 g per day is closer to two than three 10-g standard drinks per day. We used the broad definition of “occasional drinking” as less than one drink per week, because few studies reported outcomes for drinking less than monthly.
Quality assessment
To identify potential study-level covariates to be controlled in multivariable meta-regression analyses (Greenland, 1998; Normand, 1999), each study was coded for publication year, sample size, population characteristics (age, gender, country), and whether covariates (e.g., smoking status, previous illness) were controlled for in individual studies. Covariates available for all selected studies were median age of study participants at first assessment, sex, country in which a study was conducted, date a study was conducted, number of years of follow-up, whether persons with previous illnesses were excluded, and quality of the measure used for typical daily alcohol intake.
On theoretical grounds, it was expected that a long follow-up period, inclusion of individuals with previous illnesses, and an earlier age at intake would be study characteristics that reduce selection biases (Bergmann et al., 2013; Stockwell & Chikritzhs, 2013). Studies were classified according to the presence or absence of two key types of potential bias: (a) including former drinkers and/or (b) including occasional drinkers in the abstainer reference category.
Following Fillmore et al. (2006), lifetime abstention was strictly defined as zero consumption and did not include studies with any level of occasional lifetime or past-year drinking (e.g., less than 12 drinks or “rarely” or “hardly ever” drinking). Such self-reported infrequent drinkers have been shown to greatly underreport their personal consumption (Stockwell et al., 2014; Ye et al., 2013). When studies assessed usual or typical drinking patterns over a month or a week, it was assumed that individuals classified as abstainers by this method would include occasional drinkers (e.g., abstaining in a typical week is still consistent with drinking less than once a week). We coded a drinking measure as “adequate” for the purpose of estimating average daily alcohol intake if both quantity and frequency of drinking were assessed for a period of at least 1 week. Given that simple quantity–frequency measures of drinking typically result in substantial underreporting (e.g., Stockwell et al., 2014), we recognize these are minimal criteria for adequacy of measurement, necessitated by the poor overall quality of drinking measures in this literature.
Analyses
Visual inspection of the data suggested the presence of extreme outliers among estimates of the risk of all-cause mortality from drinking. Estimates of RR were classified as “extreme” when they were outside of the interval of the sample mean of natural log RR ± 2 times the standard deviation of estimates within each drinking category (Acuna & Rodrigues, 2014; Pagano & Gauvreau, 2000; Woodward, 2000). This procedure identified 11 risk estimates significantly below the mean (RR range: 0.1–0.46) and 18 risk estimates markedly higher (OR range: 1.89–4.57). Compared with other available methods (Cook & Weisberg, 1982; Viechtbauer & Cheung, 2010), this is a conservative approach excluding relatively few risk estimates. Removal of outliers made no substantive difference to the results; therefore, models are presented without any outlier estimates excluded.
Publication bias was assessed first through visual inspection of the funnel plot of log-RR of all-cause mortality due to alcohol consumption against the inverse standard error of log-RR (see Figure C1 in Appendix C) (Woodward, 2000), and also by Egger’s linear regression method (Egger et al., 1997). We also assessed between-study heterogeneity of RRs using Cochran’s Q (Cochran, 1954) and the I2 statistic (Higgins & Thompson, 2002). When significant heterogeneity was detected, mixed-effects models were used to obtain the summarized RR estimates.
Mixed regression analyses were performed in which drinking groups and control variables were treated as fixed effects with a random-intercept study effect (Normand, 1999). The dependent variable was the natural log of the RR estimated using the rate ratio or hazard ratio of each drinking group in relation to the abstainer category. Analyses were weighted by the inverse of the estimated variance of the natural log RR. Variance was estimated from reported standard errors or confidence intervals (CIs). The weights for each individual study were created using the inverse variance weight method used in mixed regression analysis in order to get maximum precision for the main results of the meta-analysis (Woodward, 2000). Studies with large or small estimates and/or variance can be highly influential. Sensitivity analyses also were run after excluding such studies to detect influential cases (Woodward, 2000).
Drinking levels were examined in terms of predefined specific consumption levels. Drinking categories were defined as (a) lifetime abstainers; (b) former drinkers now completely abstaining; (c) current occasional drinkers, up to one drink per week (<1.30 g per day); (d) low-volume drinkers, up to two drinks or 1.30–24.9 g per day; (e) medium-volume drinkers, up to four drinks or 25–44.9 g per day; (f) high-volume drinkers, up to six drinks or 45–64.9 g per day; and (g) higher volume drinkers, more than six drinks or 65 g per day. The adequacy of methods used by studies also was assessed against minimal quality criteria as discussed above.
Median cohort age, sex, country, quality of drinking measure, and abstainer bias variables were included as covariates in adjusted models. The country in which a study was conducted was dichotomized into those with mainly Caucasian populations versus without variable to reflect evidence that health protection from moderate drinking was more likely to be observed among Caucasians (Kerr et al., 2011).
Other covariates were selected for inclusion on empirical grounds based on p values of bivariable tests of the natural log-RR and each covariate, and significant correlations with other variables. Based on bivariable analysis of the data set, any variable producing a bivariable test result with p < .20 was considered a candidate for the multivariable regression analyses of the natural log-RR of all-cause mortality and alcohol consumption (Hosmer & Lemeshow, 2000). Independent variables with particularly high intercorrelations (>.30) were identified, less precise measures were excluded (Stokes et al., 2000), and the variable pool was reduced to avoid synonymous variables and collinearity (Pagano & Gauvreau, 2000).
Median age of a study cohort was treated as a continuous variable, whereas other variables with fixed multiple response options were all reduced to two or three category variables (see Table 1 and Table D1 in online Appendix D) to remove options with few or no values and to make the models more efficient. Median age of the study population at intake, gender, or being a mainly Caucasian versus non-Caucasian population were tested as possible effect modifiers of the relationship between alcohol consumption and mortality. No significant interactions were observed; therefore, pooled meta-analyses of all studies are presented.
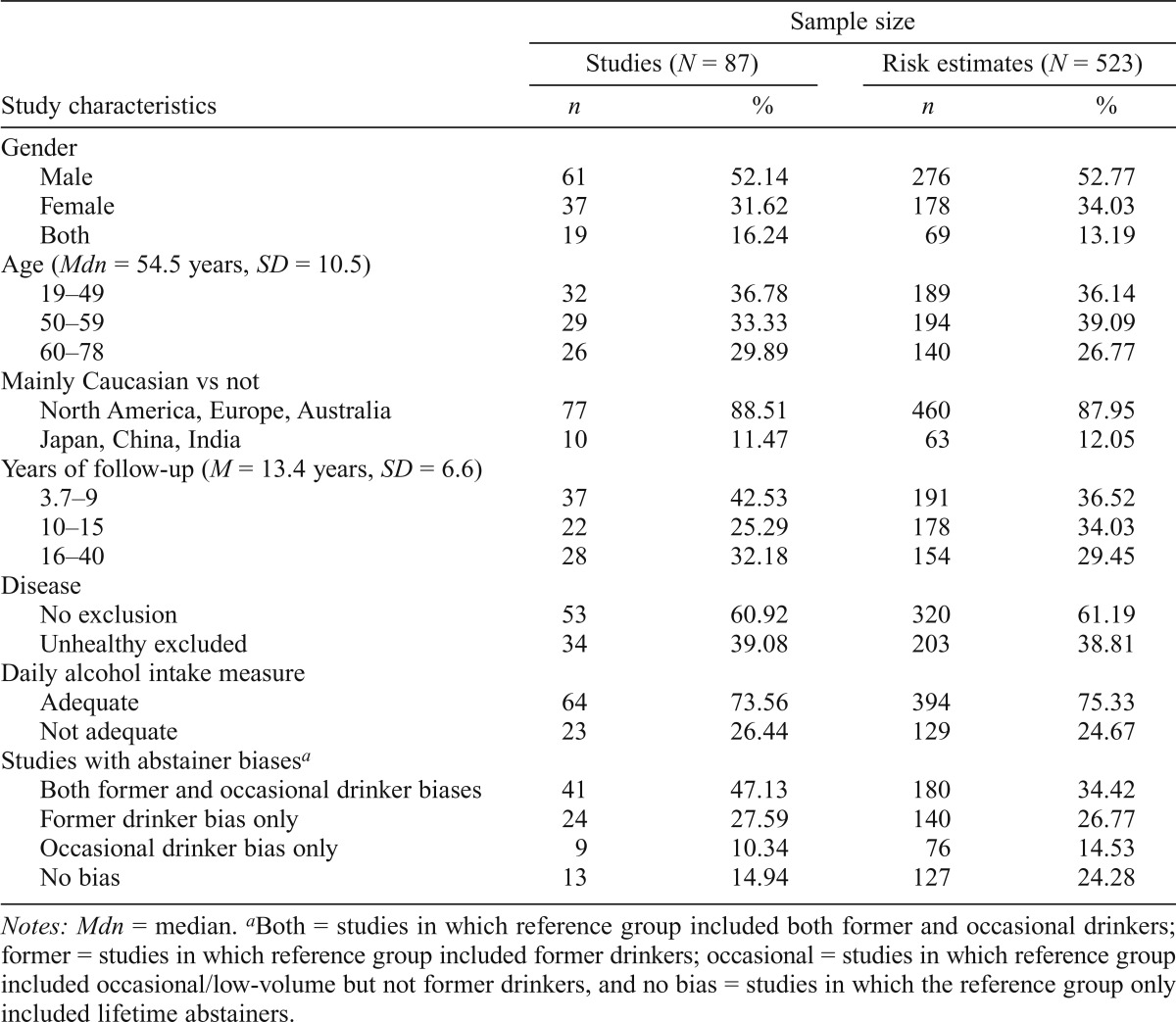
Table 1.
Characteristics of all studies included in meta-analyses on alcohol use and all-cause mortality
| Sample size |
||||
| Studies (N = 87) |
Risk estimates (N = 523) |
|||
| Study characteristics | n | % | n | % |
| Gender | ||||
| Male | 61 | 52.14 | 276 | 52.77 |
| Female | 37 | 31.62 | 178 | 34.03 |
| Both | 19 | 16.24 | 69 | 13.19 |
| Age (Mdn = 54.5 years, SD = 10.5) | ||||
| 19–49 | 32 | 36.78 | 189 | 36.14 |
| 50–59 | 29 | 33.33 | 194 | 39.09 |
| 60–78 | 26 | 29.89 | 140 | 26.77 |
| Mainly Caucasian vs not | ||||
| North America, Europe, Australia | 77 | 88.51 | 460 | 87.95 |
| Japan, China, India | 10 | 11.47 | 63 | 12.05 |
| Years of follow-up (M = 13.4 years, SD = 6.6) | ||||
| 3.7–9 | 37 | 42.53 | 191 | 36.52 |
| 10–15 | 22 | 25.29 | 178 | 34.03 |
| 16–40 | 28 | 32.18 | 154 | 29.45 |
| Disease | ||||
| No exclusion | 53 | 60.92 | 320 | 61.19 |
| Unhealthy excluded | 34 | 39.08 | 203 | 38.81 |
| Daily alcohol intake measure | ||||
| Adequate | 64 | 73.56 | 394 | 75.33 |
| Not adequate | 23 | 26.44 | 129 | 24.67 |
| Studies with abstainer biasesa | ||||
| Both former and occasional drinker biases | 41 | 47.13 | 180 | 34.42 |
| Former drinker bias only | 24 | 27.59 | 140 | 26.77 |
| Occasional drinker bias only | 9 | 10.34 | 76 | 14.53 |
| No bias | 13 | 14.94 | 127 | 24.28 |
Notes: Mdn = median.
Both = studies in which reference group included both former and occasional drinkers; former = studies in which reference group included former drinkers; occasional = studies in which reference group included occasional/low-volume but not former drinkers, and no bias = studies in which the reference group only included lifetime abstainers.
All significance tests assumed two-tailed p values or 95% CIs. All statistical analyses were performed using SAS Version 9.3 (SAS Institute Inc., Cary, NC), and the SAS PROC MIXED procedure was used to model the log-transformed RR.
Synthesis of results
We used three separate meta-analytical approaches to explore the role of abstainer biases caused by drinker misclassification errors and other predetermined study quality variables. For the first approach (Table 3), analyses were conducted on all 87 studies with the effects of various abstainer biases controlled for by inclusion of covariates in all models. Second, stratified meta-analyses were performed on four distinct subsets of studies grouped according to the number and type of abstainer biases present (Table 4). A third approach (Table 5) modeled only studies that met stricter quality criteria; that is, the analysis included studies in which only strictly defined lifetime abstainers were included in the reference group, there was an adequate measure of mean daily alcohol volume, smoking status was controlled for, and median age of the study population was less than 60 years at intake (to minimize lifetime selection biases at enrollment) and at least 55 years at follow-up (i.e., an age at which coronary heart disease and hence potential health protection may occur). Sensitivity analyses were conducted in which studies were excluded one at a time to determine if they were influential in the significance of observed estimates. Synthesis of results essentially involved examining the consistency of results across these three analytic strategies.
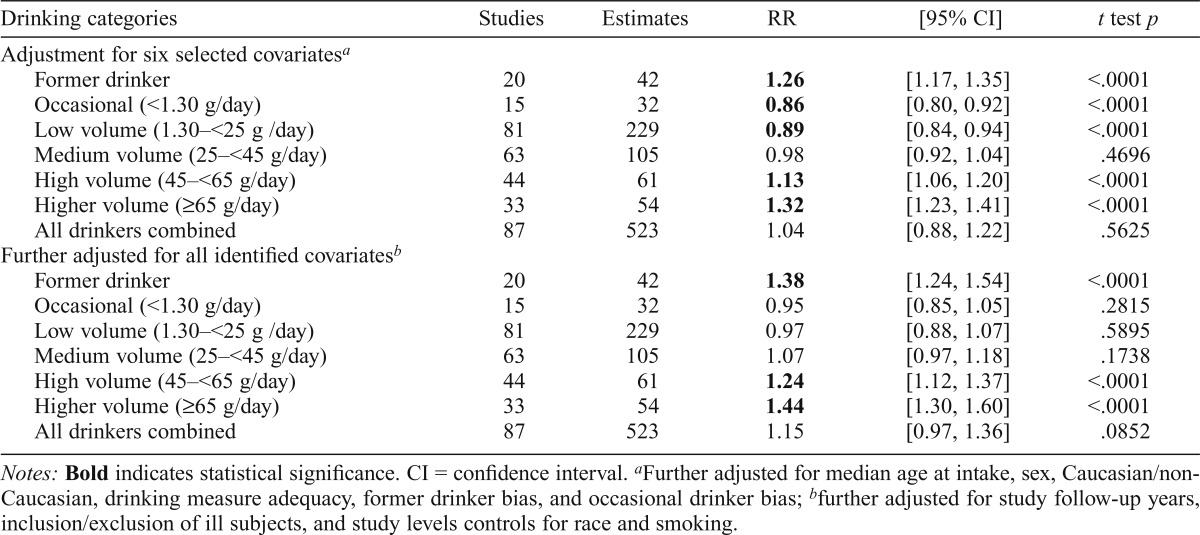
Table 3.
All-cause mortality relative risk (RR) estimates for different categories of drinker compared with abstainers, weighted and adjusted for between-study variation and study-level covariates, with adjustment for abstainer biases and study quality-related characteristics (N = 523 estimates from 87 studies)
| Drinking categories | Studies | Estimates | RR | [95% CI] | t test p |
| Adjustment for six selected covariatesa | |||||
| Former drinker | 20 | 42 | 1.26 | [1.17, 1.35] | <.0001 |
| Occasional (<1.30 g/day) | 15 | 32 | 0.86 | [0.80, 0.92] | <.0001 |
| Low volume (1.30–<25 g /day) | 81 | 229 | 0.89 | [0.84, 0.94] | <.0001 |
| Medium volume (25–<45 g/day) | 63 | 105 | 0.98 | [0.92, 1.04] | .4696 |
| High volume (45–<65 g/day) | 44 | 61 | 1.13 | [1.06, 1.20] | <.0001 |
| Higher volume (≥65 g/day) | 33 | 54 | 1.32 | [1.23, 1.41] | <.0001 |
| All drinkers combined | 87 | 523 | 1.04 | [0.88, 1.22] | .5625 |
| Further adjusted for all identified covariatesb | |||||
| Former drinker | 20 | 42 | 1.38 | [1.24, 1.54] | <.0001 |
| Occasional (<1.30 g/day) | 15 | 32 | 0.95 | [0.85, 1.05] | .2815 |
| Low volume (1.30–<25 g /day) | 81 | 229 | 0.97 | [0.88, 1.07] | .5895 |
| Medium volume (25–<45 g/day) | 63 | 105 | 1.07 | [0.97, 1.18] | .1738 |
| High volume (45–<65 g/day) | 44 | 61 | 1.24 | [1.12, 1.37] | <.0001 |
| Higher volume (≥65 g/day) | 33 | 54 | 1.44 | [1.30, 1.60] | <.0001 |
| All drinkers combined | 87 | 523 | 1.15 | [0.97, 1.36] | .0852 |
Notes: Bold indicates statistical significance. CI = confidence interval.
Further adjusted for median age at intake, sex, Caucasian/non-Caucasian, drinking measure adequacy, former drinker bias, and occasional drinker bias;
further adjusted for study follow-up years, inclusion/exclusion of ill subjects, and study levels controls for race and smoking.
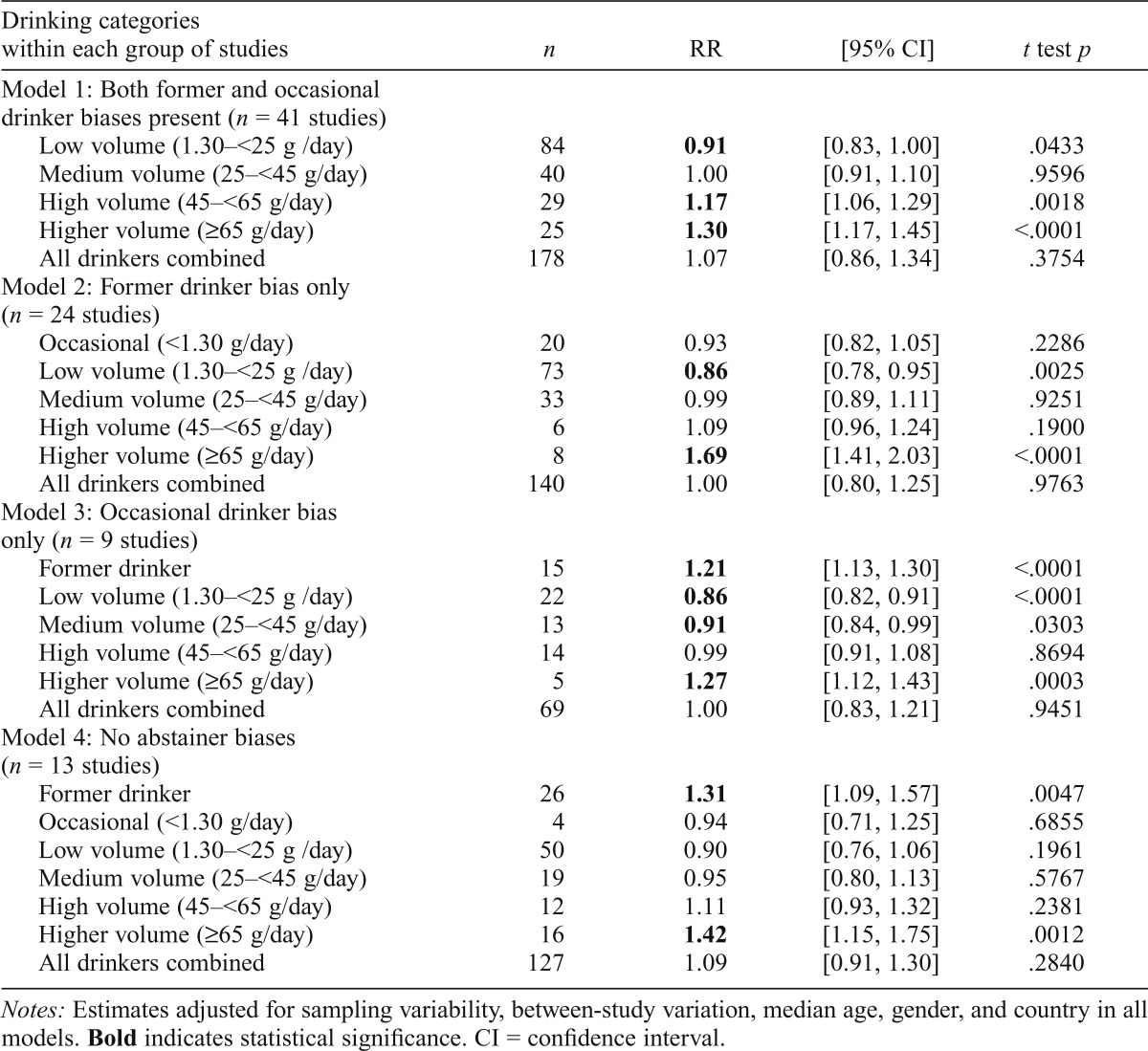
Table 4.
All-cause mortality relative risk (RR) estimates for different drinkers compared with abstainers, weighted and adjusted for between-study variation and covariates (N = 523 estimates from 87 studies) in models stratified by type of abstainer bias present
| Drinking categories within each group of studies | n | RR | [95% CI] | t test p |
| Model 1: Both former and occasional drinker biases present (n = 41 studies) | ||||
| Low volume (1.30–<25 g /day) | 84 | 0.91 | [0.83, 1.00] | .0433 |
| Medium volume (25–<45 g/day) | 40 | 1.00 | [0.91, 1.10] | .9596 |
| High volume (45–<65 g/day) | 29 | 1.17 | [1.06, 1.29] | .0018 |
| Higher volume (≥65 g/day) | 25 | 1.30 | [1.17, 1.45] | <.0001 |
| All drinkers combined | 178 | 1.07 | [0.86, 1.34] | .3754 |
| Model 2: Former drinker bias only (n = 24 studies) | ||||
| Occasional (<1.30 g/day) | 20 | 0.93 | [0.82, 1.05] | .2286 |
| Low volume (1.30–<25 g /day) | 73 | 0.86 | [0.78, 0.95] | .0025 |
| Medium volume (25–<45 g/day) | 33 | 0.99 | [0.89, 1.11] | .9251 |
| High volume (45–<65 g/day) | 6 | 1.09 | [0.96, 1.24] | .1900 |
| Higher volume (≥65 g/day) | 8 | 1.69 | [1.41, 2.03] | <.0001 |
| All drinkers combined | 140 | 1.00 | [0.80, 1.25] | .9763 |
| Model 3: Occasional drinker bias only (n = 9 studies) | ||||
| Former drinker | 15 | 1.21 | [1.13, 1.30] | <.0001 |
| Low volume (1.30–<25 g /day) | 22 | 0.86 | [0.82, 0.91] | <.0001 |
| Medium volume (25–<45 g/day) | 13 | 0.91 | [0.84, 0.99] | .0303 |
| High volume (45–<65 g/day) | 14 | 0.99 | [0.91, 1.08] | .8694 |
| Higher volume (≥65 g/day) | 5 | 1.27 | [1.12, 1.43] | .0003 |
| All drinkers combined | 69 | 1.00 | [0.83, 1.21] | .9451 |
| Model 4: No abstainer biases (n = 13 studies) | ||||
| Former drinker | 26 | 1.31 | [1.09, 1.57] | .0047 |
| Occasional (<1.30 g/day) | 4 | 0.94 | [0.71, 1.25] | .6855 |
| Low volume (1.30–<25 g /day) | 50 | 0.90 | [0.76, 1.06] | .1961 |
| Medium volume (25–<45 g/day) | 19 | 0.95 | [0.80, 1.13] | .5767 |
| High volume (45–<65 g/day) | 12 | 1.11 | [0.93, 1.32] | .2381 |
| Higher volume (≥65 g/day) | 16 | 1.42 | [1.15, 1.75] | .0012 |
| All drinkers combined | 127 | 1.09 | [0.91, 1.30] | .2840 |
Notes: Estimates adjusted for sampling variability, between-study variation, median age, gender, and country in all models. Bold indicates statistical significance. CI = confidence interval.
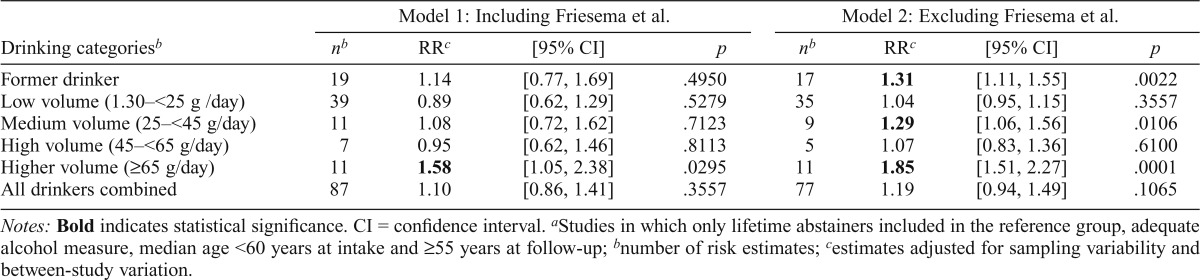
Table 5.
Adjusted relative risks (RRs) of all-cause mortality for different levels of alcohol consumption compared with lifetime abstainers estimated from higher quality studiesa with and without one influential study (Friesema et al., 2007)
| Model 1: Including Friesema et al. |
Model 2: Excluding Friesema et al. |
|||||||
| Drinking categoriesb | nb | RRc | [95% CI] | p | nb | RRc | [95% CI] | p |
| Former drinker | 19 | 1.14 | [0.77, 1.69] | .4950 | 17 | 1.31 | [1.11, 1.55] | .0022 |
| Low volume (1.30–<25 g /day) | 39 | 0.89 | [0.62, 1.29] | .5279 | 35 | 1.04 | [0.95, 1.15] | .3557 |
| Medium volume (25–<45 g/day) | 11 | 1.08 | [0.72, 1.62] | .7123 | 9 | 1.29 | [1.06, 1.56] | .0106 |
| High volume (45–<65 g/day) | 7 | 0.95 | [0.62, 1.46] | .8113 | 5 | 1.07 | [0.83, 1.36] | .6100 |
| Higher volume (≥65 g/day) | 11 | 1.58 | [1.05, 2.38] | .0295 | 11 | 1.85 | [1.51, 2.27] | .0001 |
| All drinkers combined | 87 | 1.10 | [0.86, 1.41] | .3557 | 77 | 1.19 | [0.94, 1.49] | .1065 |
Notes: Bold indicates statistical significance. CI = confidence interval.
Studies in which only lifetime abstainers included in the reference group, adequate alcohol measure, median age <60 years at intake and ≥55 years at follow-up;
number of risk estimates;
estimates adjusted for sampling variability and between-study variation.
Results
Study selection
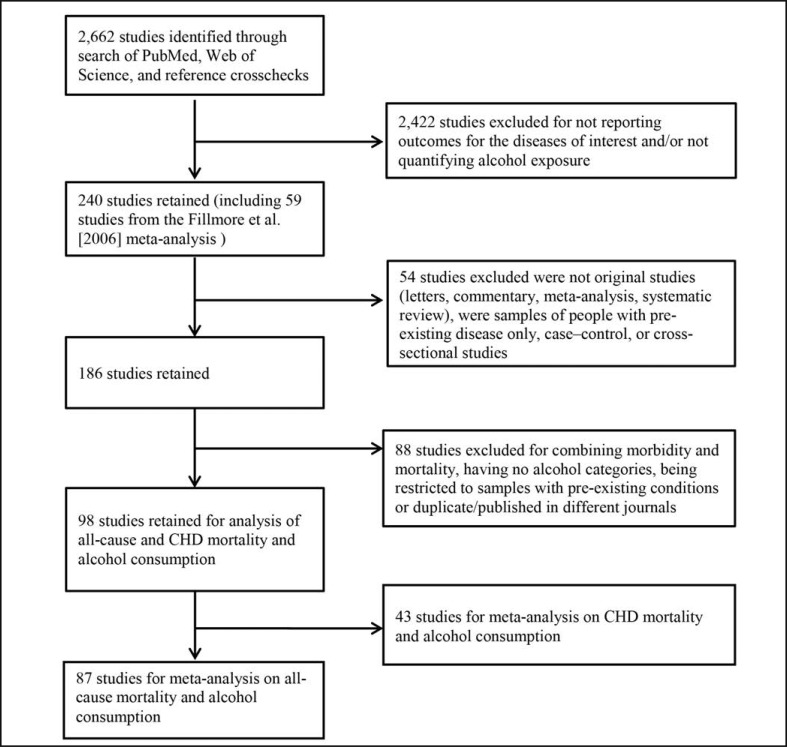
Of the 2,662 studies initially identified, 87 satisfied the criteria for meta-analysis on all-cause mortality outcomes after further removing studies for reasons identified in Figure 1. Citations and details of all included studies can be found in Tables B1–4 in online Appendix B.
Figure 1.
Flow chart of systematic search process for studies of alcohol consumption and risk of all-cause mortality. CHD = coronary heart disease.
Study characteristics including controls for potential bias
The 87 selected studies included a total of 523 estimates of the risk relationships between levels of alcohol consumption and all-cause mortality. Among these, 30 studies reported separate estimates for men and women, 31 for men only, 7 for women only, and 19 for both combined. Only 13 of these studies (127 risk estimates) were coded as free of abstainer biases because they strictly defined lifetime abstainers as the reference group. Table 1 summarizes these and other study characteristics. A summary of potentially confounding variables controlled for or not in each study is provided in online Appendix D (Table D1).
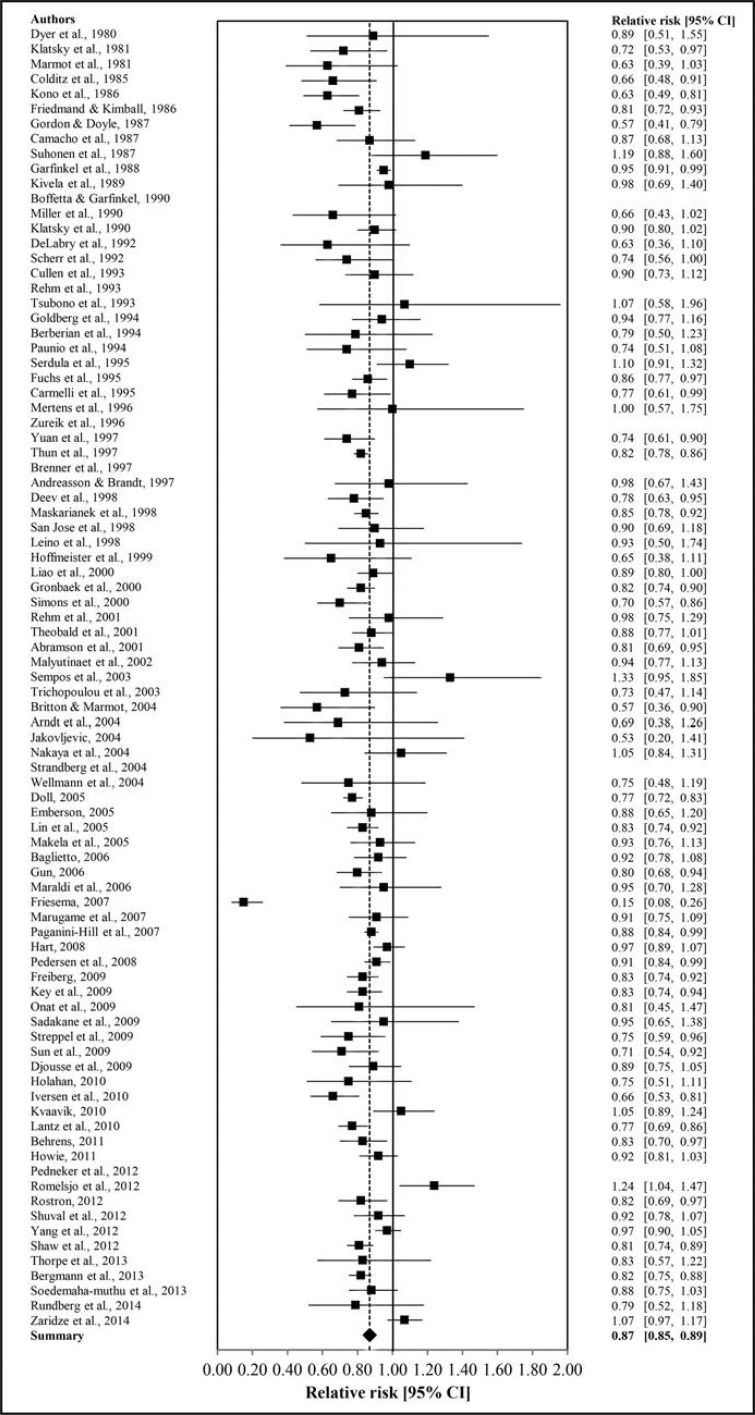
Results of individual studies
Two forest plots illustrate the range of RR estimates for (a) any level of drinking (Figure C2 in online Appendix C) and (b) low-volume drinking (Figure 2) across individual studies (Woodward, 2000). Consistent with most previous meta-analyses, these indicate (a) a wide range of estimates across different studies and (b) mean estimates for low-volume drinking significantly below unity, indicating health protection in comparison with abstainers. When all drinking outcomes are considered collectively in each study and compared against those for abstainers, no significant overall difference is observed, although again there is great variation across studies (see also Figure C2 in online Appendix C).
Figure 2.
Estimates of the relative risk of all-cause mortality associated with low-volume drinking in 81 studies. CI = confidence interval.
Synthesis of results
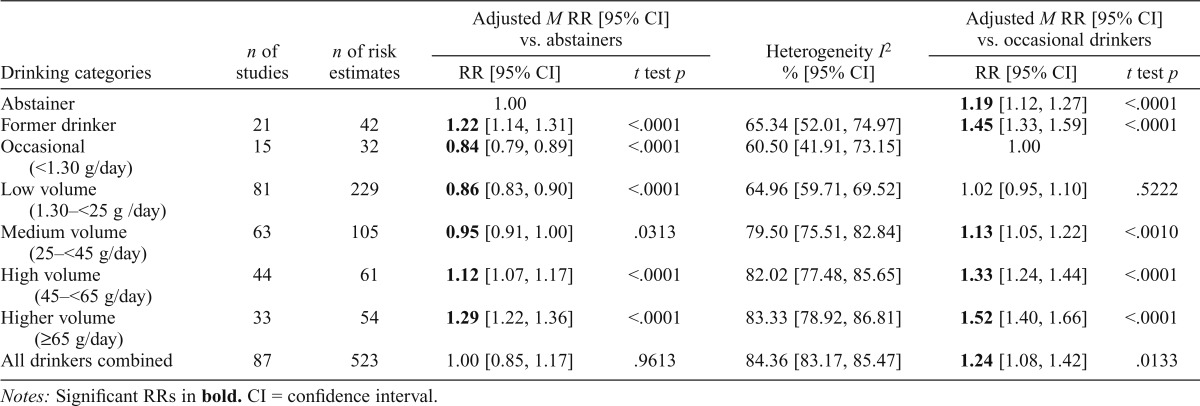
Pooled estimates of all-cause mortality with limited adjustment.
Table 2 presents mean estimates of all-cause mortality risk by level of alcohol intake with standard adjustments only for both precision and between-study variation in estimates. Analyses of simple RR means indicated a significant protective effect for both low-volume (RR = 0.86, 95% CI [0.83, 0.90], p < .0001) and occasional drinkers (RR = 0.84, 95% CI [0.79, 0.89], p < .0001). Significantly increased risk was evident for former (RR = 1.22, 95% CI [1.14, 1.31], p < .0001), high-volume (RR = 1.12, 95% CI [1.07, 1.17], p < .0001), and higher volume drinkers (RR = 1.29, 95% CI [1.22, 1.36], p < .0001). There was significant heterogeneity across studies (p < .001) for all drinking categories using the Q statistic and with I2 estimates also all significant and above 50%. No significant publication bias was detected using Egger’s linear regression tests at the .05 significance level for individual drinking categories or all drinkers combined.
Table 2.
Weighted mean relative risk (RR) estimates of all-cause mortality adjusted for between-study variation for different categories of drinkers compared with abstainers (N = 87 studies and 523 risk estimates) with tests of publication bias and heterogeneity, but not adjusted for study characteristics
| Adjusted M RR [95% CI] vs. abstainers |
Adjusted M RR [95% CI] vs. occasional drinkers |
||||||
| Drinking categories | n of studies | n of estimates | RR [95% CI] | t test p | Heterogeneity I2 % [95% CI] | RR [95% CI] | t test p |
| Abstainer | 1.00 | 1.19 [1.12, 1.27] | <.0001 | ||||
| Former drinker | 21 | 42 | 1.22 [1.14, 1.31] | <.0001 | 65.34 [52.01, 74.97] | 1.45 [1.33, 1.59] | <.0001 |
| Occasional (<1.30 g/day) | 15 | 32 | 0.84 [0.79, 0.89] | <.0001 | 60.50 [41.91, 73.15] | 1.00 | |
| Low volume (1.30–<25 g/day) | 81 | 229 | 0.86 [0.83, 0.90] | <.0001 | 64.96 [59.71, 69.52] | 1.02 [0.95, 1.10] | .5222 |
| Medium volume (25–<45 g/day) | 63 | 105 | 0.95 [0.91, 1.00] | .0313 | 79.50 [75.51, 82.84] | 1.13 [1.05, 1.22] | <.0010 |
| High volume (45–<65 g/day) | 44 | 61 | 1.12 [1.07, 1.17] | <.0001 | 82.02 [77.48, 85.65] | 1.33 [1.24, 1.44] | <.0001 |
| Higher volume (≥65 g/day) | 33 | 54 | 1.29 [1.22, 1.36] | <.0001 | 83.33 [78.92, 86.81] | 1.52 [1.40, 1.66] | <.0001 |
| All drinkers combined | 87 | 523 | 1.00 [0.85, 1.17] | .9613 | 84.36 [83.17, 85.47] | 1.24 [1.08, 1.42] | .0133 |
Notes: Significant RRs in bold. CI = confidence interval.
Table 2 also presents RR estimates using occasional drinkers instead of abstainers as the reference, as recommended by some prominent researchers (Rehm et al., 2008). The methodology for these estimates is detailed in Box 1, online Appendix A. Compared with occasional drinkers, in this model abstainers were at significantly higher risk (RR = 1.19, 95% CI [1.12, 1.27], p < .0001), low-volume drinkers were not at significantly different risk (RR = 1.02, 95% CI [0.95, 1.10]), and all drinkers combined were at significantly higher risk (RR = 1.24, 95% CI [1.08, 1.42], p = .0133).
Pooled estimates of all-cause mortality after adjustment.
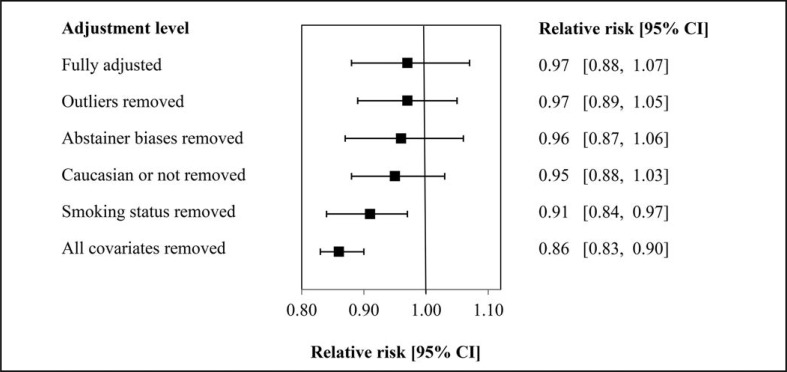
Table 3 illustrates two further mixed models with successive adjustments for (a) the precision of estimates and between-study variation and (b) the addition of key study characteristics treated as covariates. In fully adjusted models no significant protection was estimated for occasional (RR = 0.95, 95% CI [0.85, 1.05]), low-volume (RR = 0.97, 95% CI [0.88, 1.07]), or medium-volume drinkers (RR = 1.07, 95% CI [0.97, 1.18]). In each model, both former and high-volume drinkers showed a significantly elevated risk of all-cause mortality. The same pattern of results was obtained in sensitivity analyses after elimination of outliers (not reported).
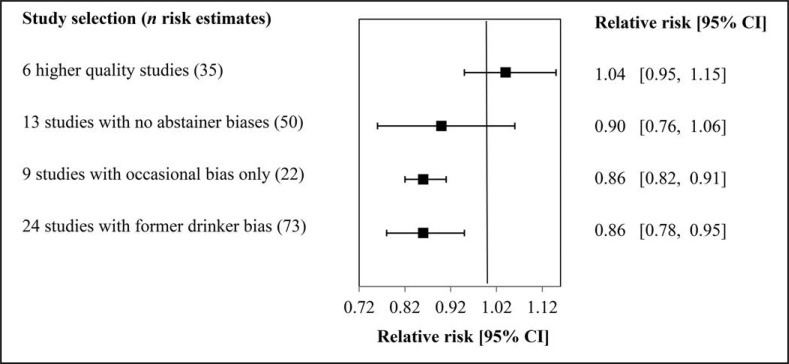
Figure 3 summarizes the changes in the all-cause mortality RR estimates for low-volume drinkers after successive inclusion of key covariates. As controls for abstainer biases and key covariates are removed, the RR estimate changes from 0.97 (95% CI [0.88, 1.07]) down to 0.86 (95% CI [0.83, 0.90]). Further details of the impact of removing individual covariates from the model are shown in online Appendix E, which confirms the importance of former drinker bias while suggesting that occasional drinker bias may be less influential.
Figure 3.
All-cause mortality relative-risk estimates for low-volume alcohol consumers versus lifetime abstainers with and without influential covariates (n = 81 studies, 229 risk estimates). CI = confidence interval.
Estimates of all-cause mortality risk among studies stratified by abstainer bias.
Although all models using studies with at least one abstainer bias showed evidence of health benefits, the risk of all-cause mortality for low-volume drinkers in bias-free studies (Model 4 in Table 4) was not significantly reduced, although the RR was below unity. By contrast, mortality risk was significantly elevated among higher volume drinkers as well as former drinkers in these models. The available estimates for occasional drinkers (only Model 2 and Model 4 in Table 4) found no significant reduction or elevation in risk of all-cause mortality. Similar results were obtained in sensitivity analyses excluding outliers.
Meta-analysis of higher quality studies.
As shown in Table 5, meta-analysis of seven higher quality studies free from abstainer bias indicated no significantly altered risk of all-cause mortality for any drinking group with the exception of a raised risk for higher volume drinkers (RR = 1.58, 95% CI [1.05, 2.38], p = .0295). Sensitivity analysis that each excluded just one study at a time identified Friesema et al. (2007) as being highly influential. The analysis of outliers in the pooled sample of 87 studies also identified 6 of the 8 estimates in this study as extreme outliers.
When this study was removed, all RR estimates increased with both former (RR = 1.31, 95% CI [1.11, 1.55], p = .0022) and medium-volume drinkers (RR = 1.29, 95% CI [1.06, 1.56], p = .0106) having significantly elevated all-cause mortality risk. The risk estimate for low-volume drinkers was close to unity (RR = 1.04, 95% CI [0.95, 1.15]). Results were otherwise stable after removal of each of the other six studies, and a similar pattern of results was obtained in sensitivity analyses after elimination of outliers. Examination of the heterogeneity of risk estimates across studies showed these to be significant but substantially reduced in the six higher quality studies without Friesema et al. included (see online Appendix F). I2 estimates were below 50% for former, low-, and medium-volume drinkers (i.e., of limited practical significance).
Figure 4 illustrates how the unadjusted estimate of RR for low-volume drinkers approaches unity as abstainer biases were successively eliminated and different subgroups of studies used.
Figure 4.
All-cause mortality relative risk for low-volume drinkers versus lifetime abstainers after controlling for design characteristics by study selection in adjusted models. CI = confidence interval.
Discussion
Summary of evidence
Three meta-analytic strategies were used to explore the role of abstainer reference group biases caused by drinker misclassification errors and several other study-level quality covariates in studies of the relationship between alcohol consumption and all-cause mortality. Drinker misclassification errors were common. Of 87 studies identified, 65 included former drinkers in the “abstainer” reference group, 50 included occasional drinkers, and only 13 were free from both these abstainer biases. However, even this last group contained other potentially serious methodological problems that could have biased results in either direction.
Using several analytic approaches, we found evidence that abstainer biases and other study characteristics influenced the shape of the risk relationship between mortality and rising alcohol consumption. In summary, analyses of groups of higher quality studies free from abstainer biases were less likely to find evidence of reduced risk of mortality (i.e., health benefits) at low levels of alcohol consumption. Rather, the pattern of results is more consistent with a linear dose response than a J-shaped curve describing the risk relationships between level of alcohol consumption and all-cause mortality.
Our first analytic strategy involved pooling all 87 studies and attempting to control for design characteristics and potential biases in a step-by-step fashion (Table 2 and Table 3). In each model, regardless of degree of adjustment for design characteristics and covariates, we consistently found that former drinkers had significantly elevated risk of all-cause mortality compared with abstainers. This confirms the well-accepted need to control for former-drinker bias and not include former drinkers in the abstainer reference group (Roerecke & Rehm, 2012; Ronksley et al., 2011).
We also replicated the J-shaped curve when only limited controls for study characteristics were used (i.e., showing low-volume drinkers with reduced mortality risk and high-volume drinkers with increased mortality risk). Significant heterogeneity was detected in these estimates. However, a J-shaped curve was not observed when abstainer biases and other study characteristics were controlled for (Table 3). In the fully adjusted model, mortality risk for former, high-volume, and higher volume drinkers was increased, whereas low- and medium-volume drinkers displayed nonsignificant RRs close to unity (RR = 0.97 and 1.07, respectively).
In each of these pooled models, regardless of level of control for study-level characteristics, RRs for occasional drinkers were similar to those for low-volume drinkers. Thus, if occasional drinkers were used as the reference group (as recommended by some epidemiologists, e.g., Rehm et al., 2008), low-volume drinkers would have RRs close to unity in each of these models (i.e., not be experiencing health protective effects). Evidence that lifetime abstainers have poorer health even before their peers begin drinking (Ng Fat & Shelton, 2012) also provides some support for choosing occasional drinkers as the reference group and is consistent with the observation of increased mortality risk for abstainers (RR = 1.19, 95% CI [1.12, 1.27]) versus occasional drinkers shown in Table 2.
On one hand, it can be argued that occasional drinking in most developed countries is more normative than abstinence and also that consumption of less than one drink per week is unlikely to confer any biological health benefit. On the other hand, it can be argued that some low-volume drinkers are underestimating their consumption and are thus misclassified as occasional drinkers (Stockwell et al., 2014).
The second set of analyses stratified studies according to the presence or absence of different types of abstainer bias (Table 4). Here, groups of studies containing former and/or occasional drinker biases also replicated the J-shaped curve—that is, significant protection was observed for low-volume drinkers and elevated risk for higher volume drinkers. However, the model with 13 studies free from abstainer biases showed no significant protection for low-volume drinkers, although the RR estimate was below unity (RR = 0.90, 95% CI [0.76, 1.06]). Former and higher volume drinkers were consistently at increased risk for all-cause mortality in these models.
A third analysis (Table 5) was performed on higher quality studies that were free from abstainer biases, used an “adequate” measure of mean alcohol consumption, followed subjects up to an age at which cardiovascular disease becomes a greater risk (at least 55 years), and did not use an aged population at intake more likely to be subject to an array of lifetime selection biases (Bergmann et al., 2013). Once more, there was significantly increased risk of all-cause mortality for former and higher volume drinkers, whereas there was no significant protection for low-volume drinkers (RR = 1.04, 95% CI [0.95, 1.15]). Heterogeneity of these estimates across studies was still significant, but, for former, low-, and medium-volume drinkers, it was at a level considered to have no practical importance. Thus, for each of the three strategies, evidence for reduced mortality risk among low-volume drinkers largely disappeared once design and methodological issues were controlled for directly in the analysis or by study selection.
Although former drinkers had a 38% increased risk of mortality compared with lifetime abstainers in the pooled and fully adjusted model (Table 3), there was mixed evidence for the importance of controlling for occasional drinker bias. Only 17 studies reported separate estimates for occasional drinkers even with the broad definition of less than one drink per week. In both the pooled model using all 87 studies and the model with the 13 error-free studies, occasional drinkers had reduced mortality risk, although this was only significant in the pooled model (Table 2). In the model with 13 error-free studies, however, there were only three risk estimates available for occasional drinkers and none at all in the model using the 6 higher quality studies (i.e., occasional drinkers were misclassified as low-volume drinkers in these latter studies).
Uncertainty about the significance of occasional-drinker bias adds a note of caution when interpreting the results of our final model of higher quality studies. Nonetheless, it may be that occasional drinkers are a more appropriate reference group against which to compare low-volume drinkers in that (a) they may have more personal and lifestyle characteristics in common with low-volume drinkers that may otherwise confound observed risk relationships, and (b) it may be implausible to suggest a physiological basis for health benefits associated with occasional consumption (Knott et al., 2015).
Study characteristics other than drinker misclassification errors strongly influenced whether health protective effects were indicated in studies and may be at least as important. Controlling for some study-level variables (including length of follow-up, median age, smoking status, and ethnicity) in the models increased RR estimates for low-volume drinkers. This is consistent with evidence for systematic biases operating across the life course in prospective studies of alcohol and health that will be more pronounced among older populations (Bergmann et al., 2013; Stockwell & Chikritzhs, 2013). The results are also consistent with studies of other lifestyle factors associated with moderate drinking being responsible for the appearance of reduced mortality risk (Naimi et al., 2005) and the possible absence of protective effects in non-Caucasian populations (Kerr et al., 2011).
Limitations
A number of limitations and caveats around our findings need to be acknowledged. A major limitation involves imperfect measurement of alcohol consumption in most included studies. Self-reported alcohol consumption is mostly under-reported (Stockwell et al., 2014), and even the classification of drinkers as lifetime abstainers can be unreliable (Kerr et al., 2002). The number of available studies in some stratified analyses was small, and therefore there may be limited power to control for potential study-level confounders. However, the required number of estimates per variable for linear regression can be much smaller than in logistic regression, and a minimum of at least two estimates per variable is recommended for linear regression analysis (Austin & Steyerberg, 2015), suggesting that the sample sizes were adequate in all models presented.
It has been demonstrated that a pattern of heavy episodic (i.e., “binge”) drinking is not associated with the appearance of reduced health risks even when average daily volume is low (Roerecke & Rehm, 2010). Too few studies adequately controlled for this variable to investigate its effect on different outcomes across studies. Finally, our findings only apply to the net effect of alcohol at different doses on all-cause mortality, and different risk relationships likely apply for specific disease categories.
Conclusions
The hypothesis that abstainer biases crucially determine the shape of the risk relationship between alcohol consumption and mortality is partly supported by our findings. Specifically, the common practice of including former drinkers in the abstainer reference group will bias drinking risk estimates downward, thereby magnifying the appearance of health benefits from low-level drinking. RR estimates for former drinkers were consistently high, second only to the heaviest alcohol consumption category. This is likely because of individuals giving up drinking for health reasons, which bias toward shorter life expectancy, whether or not this is related to their drinking. Evidence for significant bias because of the inclusion of occasional drinkers with abstainers could not be confirmed and requires further investigation, as does the proposal that they replace lifelong abstainers as the most appropriate reference group for evaluating the risk of drinking in future studies.
It is also noteworthy that in all the pooled models presented, regardless of whether outliers were excluded or study-level characteristics were controlled for, occasional drinkers had very similar mortality risks to low-volume drinkers. This means that if occasional drinkers are considered to be a more appropriate reference group than lifetime abstainers, there would be no evidence of health protective effects for low-volume drinkers or any other category of drinker.
In summary, our study suggests that a skeptical position is warranted in relation to the evidence that low-volume consumption is associated with net health benefits. This conclusion is consistent with a recent Mendelian randomization study that found that a genetic variant associated with reduced drinking lowered rather than increased cardiovascular risk among low-volume drinkers (Holmes et al., 2014). We recommend that future prospective studies on alcohol and health minimize bias attributable to the misclassification of former and occasional drinkers by carefully excluding these from the abstainer reference group.
Our analyses also indicate that other study quality characteristics need to be addressed, such as the adequacy of measures of both average daily alcohol consumption and potentially confounding lifestyle variables. We also recommend that (a) outcomes for occasional drinkers should be estimated separately from those for low-volume drinkers, (b) consideration should be given to using occasional drinkers as the reference group in these prospective observational studies given evidence that lifetime abstainers have poorer health for reasons other than their drinking (Ng Fat & Shelton, 2012), (c) following Bergmann et al., drinking behavior needs to be assessed at multiple time points so that more stable drinking patterns can be identified and health risks/benefits more firmly identified, and (d) following Liang and Chikritzhs (2013), efforts should be made to estimate the volume and duration of drinking by former drinkers so they can be correctly classified along with current drinkers for less biased estimates of risk.
Acknowledgment
We acknowledge with deep gratitude the contributions of our late colleague and principal investigator Kaye Middleton Fillmore, Ph.D., to our thinking and the analyses reported in this article.
Footnotes
This study was funded by National Institutes of Health Award # 1RO1AAO19939-02. This grant was initially held by our late colleague and principal investigator Kaye Middleton Fillmore, Ph.D.
References
- Acuna E., Rodrigues C. A meta-analysis study of outlier detection methods in classification. Mayaguez, Puerto Rico: University of Puerto Rico at Mayaguez; 2014. Retrieved from http://academic.uprm.edu/eacuna/paperout.pdf. [Google Scholar]
- Austin P. C., Steyerberg E. W. The number of subjects per variable required in linear regression analyses. Journal of Clinical Epidemiology. 2015;68:627–636. doi: 10.1016/j.jclinepi.2014.12.014. doi:10.1016/j.jclinepi.2014.12.014. [DOI] [PubMed] [Google Scholar]
- Babor T. F., Caetano R., Casswell S., Edwards G., Giesbrecht N., Graham K., Rossow I. Alcohol: No ordinary commodity: Research and public policy. 2nd ed. Oxford, England: Oxford University Press; 2010. doi:10.1093/acprof:oso/9780199551149.001.0001. [Google Scholar]
- Bergmann M. M., Rehm J., Klipstein-Grobusch K., Boeing H., Schütze M., Drogan D., Ferrari P. The association of pattern of lifetime alcohol use and cause of death in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. International Journal of Epidemiology. 2013;42:1772–1790. doi: 10.1093/ije/dyt154. doi:10.1093/ije/dyt154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brien S. E., Ronksley P. E., Turner B. J., Mukamal K. J., Ghali W. A. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: Systematic review and meta-analysis of interventional studies. BMJ. 2011;342:d636. doi: 10.1136/bmj.d636. doi:10.1136/bmj.d636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chikritzhs T., Stockwell T., Naimi T., Andreasson S., Dangardt F., Liang W. Has the leaning tower of presumed health benefits from ‘moderate’ alcohol use finally collapsed? Addiction. 2015;110:726–727. doi: 10.1111/add.12828. doi:10.1111/add.12828. [DOI] [PubMed] [Google Scholar]
- Cochran W. G. The combination of estimates from different experiments. Biometrics. 1954;10:101–129. doi:10.2307/3001666. [Google Scholar]
- Cook R. D., Weisberg S. Residuals and influence in regression. New York, NY: Chapman and Hall; 1982. [Google Scholar]
- Egger M., Smith G. D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. doi:10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fekjaer H. O. Alcohol—a universal preventive agent? A critical analysis. Addiction. 2013;108:2051–2057. doi: 10.1111/add.12104. doi:10.1111/add.12104. [DOI] [PubMed] [Google Scholar]
- Fillmore K. M., Kerr W. C., Stockwell T., Chikritzhs T., Bostrom A. Moderate alcohol use and reduced mortality risk: Systematic error in prospective studies. Addiction Research & Theory. 2006;14:101–132. doi: 10.1016/j.annepidem.2007.01.005. doi:10.1080/16066350500497983. [DOI] [PubMed] [Google Scholar]
- Friesema I. H. M., Zwietering P. J., Veenstra M. Y., Knottnerus J. A., Garretsen H. F. L., Lemmens P. H. H. M. Alcohol intake and cardiovascular disease and mortality: The role of pre-existing disease. Journal of Epidemiology and Community Health. 2007;61:441–446. doi: 10.1136/jech.2006.050419. doi:10.1136/jech.2006.050419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland S. Meta-analysis. In: Rothman K. J., Greenland S., editors. Modern epidemiology. Philadelphia, PA: Lippincott Williams & Wilkins; 1998. [Google Scholar]
- Higgins J. P. T., Thompson S. G. Quantifying heterogeneity in a meta-analysis. Statistics in Medicine. 2002;21:1539–1558. doi: 10.1002/sim.1186. doi:10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- Holmes M. V., Dale C. E., Zuccolo L., Silverwood R. J., Guo Y., Ye Z., Casas J. P. the InterAct Consortium. Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ. 2014;349:g4164. doi: 10.1136/bmj.g4164. doi:10.1136/bmj.g4164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosmer D. W., Lemeshow S. Applied logistic regression. New York, NY: Wiley; 2000. [Google Scholar]
- International Center for Alcohol Policies. International drinking guidelines. 2010. Retrieved from http://www.icap.org. [Google Scholar]
- Kelly Y., Sacker A., Gray R., Kelly J., Wolke D., Quigley M. A. Light drinking in pregnancy, a risk for behavioural problems and cognitive deficits at 3 years of age? International Journal of Epidemiology. 2009;38:129–140. doi: 10.1093/ije/dyn230. doi:10.1093/ije/dyn230. [DOI] [PubMed] [Google Scholar]
- Kerr W. C., Fillmore K. M., Bostrom A. Stability of alcohol consumption over time: Evidence from three longitudinal surveys from the United States. Journal of Studies on Alcohol. 2002;63:325–333. doi: 10.15288/jsa.2002.63.325. doi:10.15288/jsa.2002.63.325. [DOI] [PubMed] [Google Scholar]
- Kerr W. C., Greenfield T. K., Bond J., Ye Y., Rehm J. Racial and ethnic differences in all-cause mortality risk according to alcohol consumption patterns in the national alcohol surveys. American Journal of Epidemiology. 2011;174:769–778. doi: 10.1093/aje/kwr147. doi:10.1093/aje/kwr147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knott C. S., Coombs N., Stamatakis E., Biddulph J. P. All cause mortality and the case for age specific alcohol consumption guidelines: Pooled analyses of up to 10 population based cohorts. BMJ. 2015;350:h384. doi: 10.1136/bmj.h384. doi:10.1136/bmj.h384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang W., Chikritzhs T. The association between alcohol exposure and self-reported health status: The effect of separating former and current drinkers. PLoS One. 2013;8(2):e55881. doi: 10.1371/journal.pone.0055881. doi:10.1371/journal.pone.0055881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim S. S., Vos T., Flaxman A. D., Danaei G., Shibuya K., Adair-Rohani H., Baxter A. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. doi:10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mäkelä P., Paljärvi T., Poikolainen K. Heavy and nonheavy drinking occasions, all-cause and cardiovascular mortality and hospitalizations: A follow-up study in a population with a low consumption level. Journal of Studies on Alcohol. 2005;66:722–728. doi: 10.15288/jsa.2005.66.722. doi:10.15288/jsa.2005.66.722. [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G the PRISMA Group. Preferred reporting items for systematic reviews and metaanalyses: The PRISMA statement. PLoS Medicine. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. doi:10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naimi T. S., Brown D. W., Brewer R. D., Giles W. H., Mensah G., Serdula M. K., Stroup D. F. Cardiovascular risk factors and confounders among nondrinking and moderate-drinking U.S. adults. American Journal of Preventive Medicine. 2005;28:369–373. doi: 10.1016/j.amepre.2005.01.011. doi:10.1016/j.amepre.2005.01.011. [DOI] [PubMed] [Google Scholar]
- National Health and Medical Research Council of Australia. Australian guidelines to reduce health risk from drinking alcohol. Canberra, Australia: Attorney-General’s Department; 2009. [Google Scholar]
- Ng Fat L., Shelton N. Associations between self-reported illness and non-drinking in young adults. Addiction. 2012;107:1612–1620. doi: 10.1111/j.1360-0443.2012.03878.x. doi:10.1111/j.1360-0443.2012.03878.x. [DOI] [PubMed] [Google Scholar]
- Normand S.-L. T. Meta-analysis: Formulating, evaluating, combining, and reporting. Statistics in Medicine. 1999;18:321–359. doi: 10.1002/(sici)1097-0258(19990215)18:3<321::aid-sim28>3.0.co;2-p. doi:10.1002/(SICI)1097-0258(19990215)18:3<321::AID-SIM28>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- Pagano M., Gauvreau K. Principles of biostatistics. 2nd ed. Pacific Grove, CA: Duxbury; 2000. [Google Scholar]
- Rehm J., Irving H., Ye Y., Kerr W. C., Bond J., Greenfield T. K. Are lifetime abstainers the best control group in alcohol epidemiology? On the stability and validity of reported lifetime abstention. American Journal of Epidemiology. 2008;168:866–871. doi: 10.1093/aje/kwn093. doi:10.1093/aje/kwn093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J., Taylor B., Mohapatra S., Irving H., Baliunas D., Patra J., Roerecke M. Alcohol as a risk factor for liver cirrhosis: A systematic review and meta-analysis. Drug and Alcohol Review. 2010;29:437–445. doi: 10.1111/j.1465-3362.2009.00153.x. doi:10.1111/j.1465-3362.2009.00153.x. [DOI] [PubMed] [Google Scholar]
- Roerecke M., Rehm J. Irregular heavy drinking occasions and risk of ischemic heart disease: A systematic review and meta-analysis. American Journal of Epidemiology. 2010;171:633–644. doi: 10.1093/aje/kwp451. doi:10.1093/aje/kwp451. [DOI] [PubMed] [Google Scholar]
- Roerecke M., Rehm J. The cardioprotective association of average alcohol consumption and ischaemic heart disease: A systematic review and meta-analysis. Addiction. 2012;107:1246–1260. doi: 10.1111/j.1360-0443.2012.03780.x. doi:10.1111/j.1360-0443.2012.03780.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronksley P. E., Brien S. E., Turner B. J., Mukamal K. J., Ghali W. A. Association of alcohol consumption with selected cardiovascular disease outcomes: A systematic review and meta-analysis. BMJ. 2011;342:d671. doi: 10.1136/bmj.d671. doi:10.1136/bmj.d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaper A. G., Wannamethee G., Walker M. Alcohol and mortality in British men: Explaining the U-shaped curve. The Lancet. 1988;332:1267–1273. doi: 10.1016/s0140-6736(88)92890-5. doi:10.1016/S0140-6736(88)92890-5. [DOI] [PubMed] [Google Scholar]
- Stockwell T., Chikritzhs T. Commentary: Another serious challenge to the hypothesis that moderate drinking is good for health? International Journal of Epidemiology. 2013;42:1792–1794. doi: 10.1093/ije/dyt217. doi:10.1093/ije/dyt217. [DOI] [PubMed] [Google Scholar]
- Stockwell T., Greer A., Fillmore K., Chikritzhs T., Zeisser C. How good is the science? BMJ. 2012;344:e2276. doi: 10.1136/bmj.e2276. author reply e2294. doi:10.1136/bmj.e2276. [DOI] [PubMed] [Google Scholar]
- Stockwell T., Room R. Constructing and responding to low-risk drinking guidelines: Conceptualisation, evidence and reception. Drug and Alcohol Review. 2012;31:121–125. doi: 10.1111/j.1465-3362.2011.00416.x. doi:10.1111/j.1465-3362.2011.00416.x. [DOI] [PubMed] [Google Scholar]
- Stockwell T., Zhao J., Macdonald S. Who under-reports their alcohol consumption in telephone surveys and by how much? An application of the ‘yesterday method’ in a national Canadian substance use survey. Addiction. 2014;109:1657–1666. doi: 10.1111/add.12609. doi:10.1111/add.12609. [DOI] [PubMed] [Google Scholar]
- Stokes M. E., Davis C. S., Koch G. G. Categorical data analysis using the SAS system. 2nd ed. Cary, NC: SAS Institute; 2000. [Google Scholar]
- Turner C. How much alcohol is in a ‘standard drink’? An analysis of 125 studies. British Journal of Addiction. 1990;85:1171–1175. doi: 10.1111/j.1360-0443.1990.tb03442.x. [DOI] [PubMed] [Google Scholar]
- Viechtbauer W., Cheung M. W. Outlier and influence diagnostics for meta-analysis. Research Synthesis Methods. 2010;1:112–125. doi: 10.1002/jrsm.11. doi:10.1002/jrsm.11. [DOI] [PubMed] [Google Scholar]
- Woodward M. Epidemiology study design and data analysis. Boca Raton, FL: Chapman & Hall/CRC; 2000. [Google Scholar]
- Ye Y., Bond J., Cherpitel C. J., Stockwell T., Macdonald S., Rehm J. Risk of injury due to alcohol: Evaluating potential bias using the case-crossover usual-frequency method. Epidemiology. 2013;24:240–243. doi: 10.1097/EDE.0b013e3182801cb4. doi:10.1097/EDE.0b013e3182801cb4. [DOI] [PMC free article] [PubMed] [Google Scholar]