Abstract
Objective:
The purpose of this study was to examine the associations between the number of substance use disorder (SUD) criteria as listed in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, and other- and self-directed forms of violence among youth ages 12–17 in the general population.
Method:
Data were obtained from the National Survey on Drug Use and Health pooled across survey years 2008–2013, with a combined sample of 108,560 respondents ages 12–17. Violence categories defined by suicide attempt (self-directed) and attacking someone with the intent for serious injury (other-directed) were categorized as follows: none, self-directed only, other-directed only, and combined self-/other-directed. Multinomial logistic regression estimated odds ratios of the increased number of criteria for alcohol, marijuana, and other illicit drug use, and nicotine dependence for each violence category, by controlling for sociodemographics and criminal justice involvement.
Results:
The multivariable model indicates that increased number of SUD criteria confers significantly higher odds for each violence category versus no violence. For combined violence versus self-directed violence, male gender, non-Hispanic Black and mixed race (with non-Hispanic White as referent), nicotine dependence, increased number of alcohol use disorder criteria, and other drug use disorder criteria have significantly higher odds, whereas Native Hawaiian/Pacific Islander and age have significantly lower odds. For combined violence versus other-directed violence, non-Hispanic mixed race and the increased number of other drug use disorder criteria have significantly higher odds, whereas male gender, non-Hispanic Black and Native Hawaiian/Pacific Islander, and Hispanic have significantly lower odds.
Conclusions:
The identification of the combined self-/other-directed violence in the general population provides additional support for clinical studies that established associations between self- and other-directed violent behaviors. Prevention and treatment programs need to address both instances of violence and suicidality.
Same-sex peer violence, dating violence, and suicidality among young people are significant public health problems in the United States, with serious consequences in the educational and corrective sectors. Both these other- and self-directed forms of violence have the potential to inflict great losses in productivity and lives, given the fact that suicide and homicide were the second and third leading causes of death among youth ages 12–17 between 1999 and 2013 (Centers for Disease Control and Prevention, 2015).
The relationship between suicidal behavior and interpersonal violence has been a focus of psychiatric studies on clinical populations for many years (Apter et al., 1993; Links et al., 2003; Pfeffer et al., 1989; Plutchik et al., 1989). In a review of this literature, Plutchik (1995) has noted that a number of risk factors (e.g., schizophrenia, substance use disorders [SUDs], history of psychiatric hospitalization, poor impulse control) and protective factors (e.g., large social network, social supports, religiosity) are common for suicide and violence against others and has attempted to relate suicide to violence in a systematic way based on a Two-Stage Model of Countervailing Forces that can amplify or attenuate aggressive impulse and increase or decrease the probability of action toward suicide and violence risk.
In addition, a growing body of research particularly on adolescents in the general population has compared associations between suicidality and violence against others with a particular focus on the joint presence of these behaviors (Bossarte et al., 2008; Cleary, 2000; Harford et al., 2012; Swahn et al., 2013). Cleary (2000) examined the association between victimization (i.e., being threatened with a weapon, property damaged, felt unsafe at school) and suicidal and/or violent behaviors among 1,569 high schools students in New York State, excluding New York City. Victimized students were at greater risk for suicidality, violence, and both suicidality and violence than students who reported no victimization, and the relative risk was 2.6 times as high for reporting both suicidality and violence.
Bossarte et al. (2008) developed a behavioral typology for multiple types of dating/peer violence among perpetrators and victims based on self-reports of physical violence, psychological abuse, and suicidality in a school sample of dating adolescents. The typology yielded five clusters: low violence, 21%; same-sex peer violence, 24%; dating violence, 17%; psychological abuse, 27%; and high violence, 11%. The high-violence cluster had the highest levels of both dating physical violence and psychological abuse and had the highest levels of both same-sex peer physical violence and psychological abuse as both victims and perpetrators. The high-violence cluster also had the highest level of suicidal behavior.
In a national study based on the National Youth Risk Behavior Survey, high school students behaving with combined violence, when compared with students in the other-directed or self-directed violence categories, were more likely to be younger and depressed and to engage in heavy episodic drinking (HED) (i.e., having five or more drinks of alcohol) in the past 30 days and illicit substance use (Harford et al., 2012). Using a similar typology, Swahn et al. (2013) found significant associations between combined violence (physical fighting and suicide attempt) and early drinking onset, heavy drinking, and feelings of sadness. Drinking onset before age 13 versus nondrinkers was significantly related to violence but not significantly different among different patterns of violence. The odds of HED, weapon possession in the past year, and depressed feelings (i.e., feeling sad or hopeless every day for 2 weeks) were significantly higher for the combined versus no violence than for physical fighting versus no violence. The existence of adolescents with a history of both suicidal behavior and violence toward others appears to be a meaningful and reliable phenomenon in need of replication in other independent national samples.
Previously, using data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), we have derived four broad categories of violence: other-directed violence, self-directed violence, combined other-/self-directed violence, and no or minimal violence among adults (Harford et al., 2013). Notably, the group with combined self- and other-directed violence, compared with these two separate forms of violence, was more strongly associated with SUDs (90%), mood disorders (66%), and personality disorders (79%). The identification of a small category with combined forms of violence in our earlier study has established associations between self- and other-directed violent behaviors in adults.
The present study was set to further replicate the combined form of self- and other-directed violence in youth and examine whether it was distinct from separate forms of violence. However, instead of using the dichotomous measures SUD criteria according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; American Psychiatric Association, 1994), we incorporated ordered categorization of an increasing number of DSM-IV alcohol use disorder (AUD) criteria (except the criterion of legal problems) to be consistent with more recent formulations of these criteria (American Psychiatric Association, 1994, 2013). Specifically, the objective is to expand the current literature related to substance use and violence by establishing increased number of SUD criteria as a risk factor for different patterns of violence in a national sample of youth ages 12–17. Based on current literature, it is hypothesized that increased number of SUD criteria will be associated with self-directed and other-directed violence and will show evidence of stronger associations with combined violence than either other-directed or self-directed violence.
Concerns with interpretation of DSM-IV/DSM-5 symptom criteria, especially among adolescents, have raised questions regarding their utility (Rehm et al., 2013; Saunders, 2013). Because heavy alcohol use over time had been shown to be a major risk factor for both morbidity (e.g., injury, violence perpetration) and mortality (e.g., highway fatality, cirrhosis), Rehm et al. (2013) proposed heavy use over time as an alternative to DSM-5 as a measure of SUDs to avoid misinterpretation of DSM-5 criteria and stigmatization. Therefore, in a related objective, this study assesses associations between HED and the increased number of AUD criteria and patterns of violence.
Method
Study design
The study sample is drawn from the National Survey on Drug Use and Health (NSDUH), annual surveys of the civilian noninstitutionalized U.S. population ages 12 years and older. The NSDUH is sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA) and is conducted annually under contract with RTI International (Research Triangle Park, NC; SAMHSA, 2014). The survey collects information on demographics, substance use, and mental health using a combination of computer-assisted, face-to-face interviews and audio computer-assisted, self-administered interviews.
Participants are selected by an independent multistage area probability sample design for each of the 50 states and the District of Columbia. Youths and young adults are over-sampled with approximately equal samples sizes among three age groups: 12–17 years, 18–25 years, and 26 years or older. Nearly 70,000 respondents are interviewed in each survey year, with the weighted interview response rate exceeding 70%. The present study was based on reports of adolescent respondents from public use data, which did not include all of the original respondents due to a subsampling step used in the disclosure protection procedures. In view of the relatively small samples for critical variables (e.g., suicide attempt, illicit SUD, minorities), we pooled data from several consecutive national surveys from 2008 to 2013 to augment our study sample, which comprised 108,560 respondents ages 12–17.
Measures
Dependent variables.
A violence typology was constructed from a cross-tabulation of other-directed violence and self-directed violence, with the following four violence categories: none, self-directed only, other-directed only, and combined self-/other-directed. For other-directed violence, respondents were asked, “During the past 12 months, how many times have you attacked someone with the intent to seriously hurt them?” This single item alone measured other-directed violence in a dichotomous category (one or more times = 1 and none = 0). Although NSDUH includes two additional measures (based on self-reports of having been arrested or booked for murder, homicide, or nonnegligent manslaughter, and other assault or battery) for aggravated assault that may qualify as a more serious measure of other-directed violence, there were too few cases for inclusion in the violence typology.
For self-directed violence, respondents were queried in the adolescent depression module about depressive symptoms that lasted most of the day or almost every day for 2 weeks or longer and whether they made a suicide attempt (n = 2,550) during the period of time or most recent period of time when they were depressed. Elsewhere in the mental health treatment module, they were asked if they ever received treatment or counseling because they thought/tried to kill themselves in the past 12 months (n = 3,536). Based on these two questions about suicide attempt, a positive response to either question was used as the measure of self-directed violence (n = 4,919).
Independent variables.
Past-year DSM-IV SUD criteria (except the criterion of legal problems) for alcohol, marijuana, cocaine, hallucinogens, heroin, inhalants, pain relievers, sedatives, stimulants, and tranquilizers were counted and categorized as follows: 0–1 criteria (referent), 2–3 criteria, or 4 or more criteria. Considering the relatively small number of cases that met the SUD criteria for cocaine, hallucinogens, heroin, inhalants, pain relievers, sedatives, stimulants, and tranquilizers, these drugs were combined as all other illicit drugs. Of note, the NSDUH assessment of nicotine dependence was based on the Nicotine Dependence Syndrome Scale (Heatherton et al., 1991) and the Fagerström Test of Nicotine Dependence (Fagerström, 1978) for respondents who reported smoking cigarettes in the past month.
HED, defined as drinking five or more drinks on the same occasion on at least 1 day in the past 30 days, was assessed as a dichotomous variable and combined with an increased number of AUD criteria (≥2 vs. 0–1) to create the following categorical variable (both ≥2 AUD criteria and HED; ≥2 AUD criteria only; HED only; 0–1 AUD criteria and no HED as referent).
Criminal justice involvement was a covariate measured by self-reports of having been arrested or booked in the past year for crimes (i.e., theft, larceny, burglary, robbery, arson, driving while intoxicated, drunkenness, possession/manufacture/sale of drugs, fraud, possessing stolen goods, or vandalism) other than aggravated assault.
Sociodemographic variables included gender (male, with female as referent), age in years, race/ethnicity (non-Hispanic Black, Native American/Alaskan Native, Hawaiian/Pacific Islander, Asian, mixed race [more than one race], Hispanic, with non-Hispanic White as referent), and family income (<$10,000, $10,000–29,999, $30,000–74,999, with ≥$75,000 as referent).
Analytic plan
As a preliminary step, frequency distributions of each study variable and the violence typology were examined separately for each survey year before the data were pooled. Frequency distributions of study variables were also compared between the two measures of self-directed violence (i.e., suicide attempt in the depressive episode and treatment because of suicidal behavior). Sensitivity analysis for each of the two measures of self-directed violence was assessed in separate logistic regression models. Logistic regression first assessed the differences between HED and the increased number of AUD criteria with respect to the association with violence typology. Separate multinomial logistic regression models of violence typology were subsequently conducted for the increased number of criteria for each SUD and criminal justice involvement, adjusting for sociodemographic factors. The final model included increased number of criteria for all substance use, criminal justice involvement, and sociodemographic factors; therefore, the odds ratios were mutually adjusted.
In addition, logistic regression controlling for the same sociodemographic factors was used to examine the odds of aggravated assault for combined versus other-directed violence categories as well as the odds of past-year major depressive episode (MDE) for combined versus self-directed violence categories. Because self-directed violence was measured by one of the items from the MDE category, the diagnosis of MDE in this study excluded the suicidal behavior criterion. Because aggravated assault and MDE could be indicators of other- and self-directed violence, respectively, we did not include these two risk factors along with increased number of SUD criteria in the overall analysis.
Analyses were conducted using the statistical modeling program Mplus Version 7 (Muthén & Muthén, 1998–2012). Mplus allows the specification of complex survey design in the models for stratification, clustering, and sampling weights that reflect unequal probabilities of selection. These three sampling features were taken into account for parameter estimation as well as standard error and model fit calculations.
Results
Preliminary analyses (available on request) found that the distributions of study variables and the violence typology were comparable across survey years. The distributions of study variables also were comparable between the two self-directed violence measures despite slightly higher prevalence of non-Hispanic Asian (4.6% vs. 2.2%) and Hispanic (20.9% vs. 17.0%), and lower prevalence of non-Hispanic White (57.1% vs. 63.4%), and older age (15.2 vs. 14.9 years) among adolescents who attempted suicide during depression episodes than those who received treatment because of suicide thought/attempt. Sensitivity analysis suggested that the final model shown in Table 4 would not be greatly affected by using only one of these two measures to define self-directed violence.
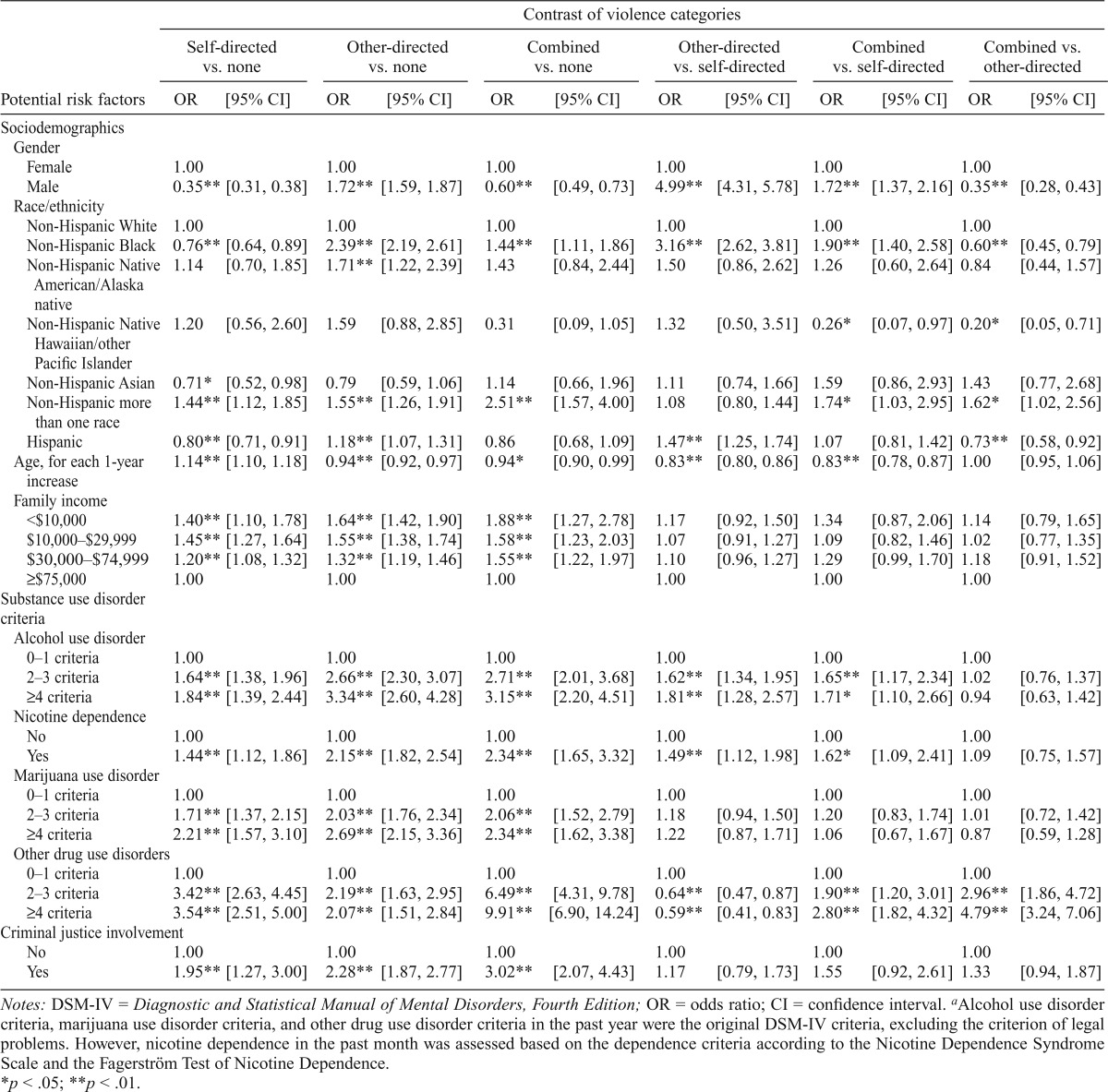
Table 4.
Adjusted odds ratios from multinomial logistic regression of violence categories on sociodemographic status, past-year DSM-IV substance use disorder criteria,a and criminal justice involvement, among youth ages 12–17
| Potential risk factors | Contrast of violence categories |
|||||||||||
| Self-directed vs. none |
Other-directed vs. none |
Combined vs. none |
Other-directed vs. self-directed |
Combined vs. self-directed |
Combined vs. other-directed |
|||||||
| OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | |
| Sociodemographics | ||||||||||||
| Gender | ||||||||||||
| Female | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Male | 0.35** | [0.31, 0.38] | 1.72** | [1.59, 1.87] | 0.60** | [0.49, 0.73] | 4.99** | [4.31, 5.78] | 1.72** | [1.37, 2.16] | 0.35** | [0.28, 0.43] |
| Race/ethnicity | ||||||||||||
| Non-Hispanic White | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Non-Hispanic Black | 0.76** | [0.64, 0.89] | 2.39** | [2.19, 2.61] | 1.44** | [1.11, 1.86] | 3.16** | [2.62, 3.81] | 1.90** | [1.40, 2.58] | 0.60** | [0.45, 0.79] |
| Non-Hispanic Native American/Alaska native | 1.14 | [0.70, 1.85] | 1 71** | [1.22, 2.39] | 1.43 | [0.84, 2.44] | 1.50 | [0.86, 2.62] | 1.26 | [0.60, 2.64] | 0.84 | [0.44, 1.57] |
| Non-Hispanic Native | 1.20 | [0.56, 2.60] | 1.59 | [0.88, 2.85] | 0.31 | [0.09, 1.05] | 1.32 | [0.50, 3.51] | 0.26* | [0.07, 0.97] | 0.20* | [0.05, 0.71] |
| Hawaiian/other Pacific Islander | ||||||||||||
| Non-Hispanic Asian | 0.71* | [0.52, 0.98] | 0.79 | [0.59, 1.06] | 1.14 | [0.66, 1.96] | 1.11 | [0.74, 1.66] | 1.59 | [0.86, 2.93] | 1.43 | [0.77, 2.68] |
| Non-Hispanic more than one race | 1.44** | [1.12, 1.85] | 1.55** | [1.26, 1.91] | 2.51** | [1.57, 4.00] | 1.08 | [0.80, 1.44] | 1.74* | [1.03, 2.95] | 1.62* | [1.02, 2.56] |
| Hispanic | 0.80** | [0.71, 0.91] | 1.18** | [1.07, 1.31] | 0.86 | [0.68, 1.09] | 1.47** | [1.25, 1.74] | 1.07 | [0.81, 1.42] | 0.73** | [0.58, 0.92] |
| Age, for each 1-year increase | 1.14** | [1.10, 1.18] | 0.94** | [0.92, 0.97] | 0.94* | [0.90, 0.99] | 0.83** | [0.80, 0.86] | 0.83** | [0.78, 0.87] | 1.00 | [0.95, 1.06] |
| Family income | ||||||||||||
| <$10,000 | 1.40** | [1.10, 1.78] | 1.64** | [1.42, 1.90] | 1.88** | [1.27, 2.78] | 1.17 | [0.92, 1.50] | 1.34 | [0.87, 2.06] | 1.14 | [0.79, 1.65] |
| $10,000–$29,999 | 1.45** | [1.27, 1.64] | 1.55** | [1.38, 1.74] | 1.58** | [1.23, 2.03] | 1.07 | [0.91, 1.27] | 1.09 | [0.82, 1.46] | 1.02 | [0.77, 1.35] |
| $30,000–$74,999 | 1.20** | [1.08, 1.32] | 1.32** | [1.19, 1.46] | 1.55** | [1.22, 1.97] | 1.10 | [0.96, 1.27] | 1.29 | [0.99, 1.70] | 1.18 | [0.91, 1.52] |
| ≥$75,000 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Substance use disorder criteria Alcohol use disorder | ||||||||||||
| 0–1 criteria | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 2–3 criteria | 1.64** | [1.38, 1.96] | 2.66** | [2.30, 3.07] | 2.71** | [2.01, 3.68] | 1.62** | [1.34, 1.95] | 1.65** | [1.17, 2.34] | 1.02 | [0.76, 1.37] |
| ≥4 criteria | ||||||||||||
| Nicotine dependence | 1.84** | [1.39, 2.44] | 3.34** | [2.60, 4.28] | 3.15** | [2.20, 4.51] | 1.81** | [1.28, 2.57] | 1.71* | [1.10, 2.66] | 0.94 | [0.63, 1.42] |
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Yes | ||||||||||||
| Marijuana use disorder | 1.44** | [1.12, 1.86] | 2.15** | [1.82, 2.54] | 2.34** | [1.65, 3.32] | 1.49** | [1.12, 1.98] | 1.62* | [1.09, 2.41] | 1.09 | [0.75, 1.57] |
| 0–1 criteria | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 2–3 criteria | 1.71** | [1.37, 2.15] | 2.03** | [1.76, 2.34] | 2.06** | [1.52, 2.79] | 1.18 | [0.94, 1.50] | 1.20 | [0.83, 1.74] | 1.01 | [0.72, 1.42] |
| ≥4 criteria | 2.21** | [1.57, 3.10] | 2.69** | [2.15, 3.36] | 2.34** | [1.62, 3.38] | 1.22 | [0.87, 1.71] | 1.06 | [0.67, 1.67] | 0.87 | [0.59, 1.28] |
| Other drug use disorders | ||||||||||||
| 0–1 criteria | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 2–3 criteria | 3.42** | [2.63, 4.45] | 2.19** | [1.63, 2.95] | 6.49** | [4.31, 9.78] | 0.64** | [0.47, 0.87] | 1.90** | [1.20, 3.01] | 2.96** | [1.86, 4.72] |
| ≥4 criteria | 3.54** | [2.51, 5.00] | 2.07** | [1.51, 2.84] | 9.91** | [6.90, 14.24] | 0.59** | [0.41, 0.83] | 2.80** | [1.82, 4.32] | 4.79** | [3.24, 7.06] |
| Criminal justice involvement | ||||||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Yes | 1.95** | [1.27, 3.00] | 2.28** | [1.87, 2.77] | 3.02** | [2.07, 4.43] | 1.17 | [0.79, 1.73] | 1.55 | [0.92, 2.61] | 1.33 | [0.94, 1.87] |
Notes: DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; OR = odds ratio; CI = confidence interval.
Alcohol use disorder criteria, marijuana use disorder criteria, and other drug use disorder criteria in the past year were the original DSM-IV criteria, excluding the criterion of legal problems. However, nicotine dependence in the past month was assessed based on the dependence criteria according to the Nicotine Dependence Syndrome Scale and the Fagerström Test of Nicotine Dependence.
p < .05;
p < .01.
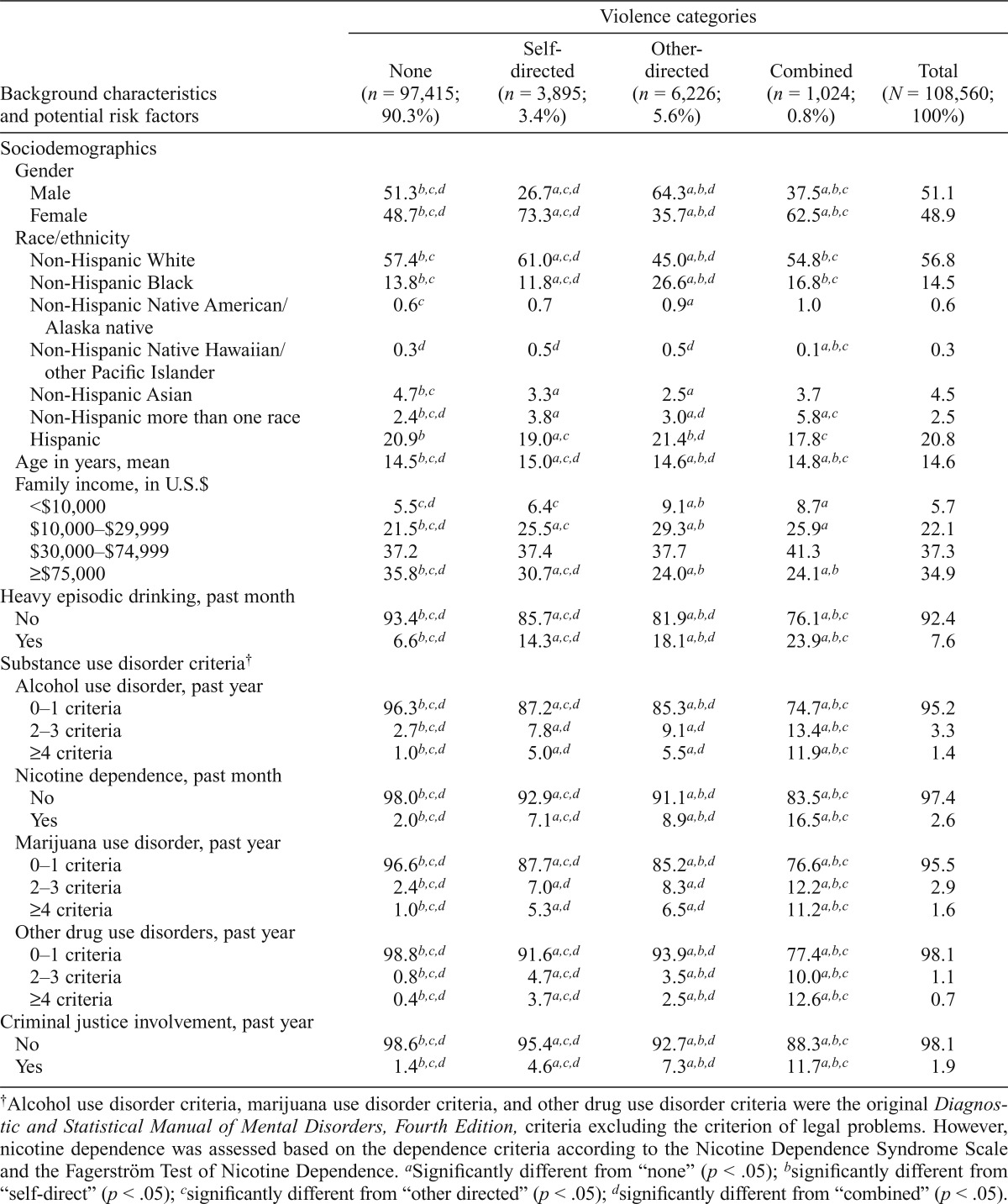
In the NSDUH for the combined years from 2008 to 2013, violent behaviors in 12- to 17-year-olds were distributed as follows: none, 90.3% (95% CI [90.0%, 90.5%]); self-directed only, 3.4% (95% CI [3.2%, 3.5%]); other-directed only, 5.6% (95% CI [5.4%, 5.8%]); and combined self-/other-directed, 0.8% (95% CI [0.7%, 0.9%]). Distributions of demographics and other background characteristics for each violence category are shown in Table 1. Other-directed violence, compared with other violence categories, is notable for higher prevalence of male gender, non-Hispanic blacks, and Hispanics. Combined violence, compared with other violence categories, shows a higher prevalence of non-Hispanic mixed race, HED, an increased number of criteria for each SUD, and criminal justice involvement. Note that the prevalence of two or more AUD criteria slightly surpasses the prevalence of HED in the combined violence category, even though it is considerably lower in other violence categories (Table 1).
Table 1.
Weighted distribution (%) of background characteristics by violence category among youth ages 12–17
| Background characteristics and potential risk factors | Violence categories |
||||
| None (n = 97,415; 90.3%) | Self-directed (n = 3,895; 3.4%) | Other-directed (n = 6,226; 5.6%) | Combined (n = 1,024; 0.8%) | Total (N = 108,560; 100%) | |
| Sociodemographics | |||||
| Gender | |||||
| Male | 51.3b,c,d | 26.7a,c,d | 64.3a,b,d | 37.5a,b,c | 51.1 |
| Female | 48.7b,c,d | 73.3a,c,d | 35.7a,b,d | 62.5a,b,c | 48.9 |
| Race/ethnicity | |||||
| Non-Hispanic White | 57.4b,c | 61.0a,c,d | 45.0a,b,d | 54.8b,c | 56.8 |
| Non-Hispanic Black | 13.8b,c | 11.8a,c,d | 26.6a,b,d | 16.8b,c | 14.5 |
| Non-Hispanic Native American/Alaska native | 0.6c | 0.7 | 0.9a | 1.0 | 0.6 |
| Non-Hispanic Native Hawaiian/other Pacific Islander | 0.3d | 0.5d | 0.5d | 0.1a,b,c | 0.3 |
| Non-Hispanic Asian | 47b,c | 3.3a | 2.5a | 3.7 | 4.5 |
| Non-Hispanic more than one race | 2 4b,c,d | 3.8a | 3.0a,d | 5.8a,c | 2.5 |
| Hispanic | 20.9b | 19.0a,c | 21.4b,d | 17.8c | 20.8 |
| Age in years, mean | 14.5b,c,d | 15.0a,c,d | 14.6a,b,d | 14.8a,b,c | 14.6 |
| Family income, in U.S.$ | |||||
| <$10,000 | 5.5c,d | 6.4c | 9.1a,b | 8.7a | 5.7 |
| $10,000–$29,999 | 21.5b,c,d | 25.5a,c | 29.3a,b | 25.9a | 22.1 |
| $30,000–$74,999 | 37.2 | 37.4 | 37.7 | 41.3 | 37.3 |
| ≥$75,000 | 35.8b,c,d | 30.7a,c,d | 24.0a,b | 24.1a,b | 34.9 |
| Heavy episodic drinking, past month | |||||
| No | 93.4b,c,d | 85.7a,c,d | 81.9a,b,d | 76.1a,b,c | 92.4 |
| Yes | 6.6b,c,d | 14.3a,c,d | 18.1a,b,d | 23.9a,b,c | 7.6 |
| Substance use disorder criteria† | |||||
| Alcohol use disorder, past year | |||||
| 0–1 criteria | 96.3b,c,d | 87.2a,c,d | 85.3a,b,d | 74.7a,b,c | 95.2 |
| 2–3 criteria | 2.7b,c,d | 7.8a,d | 9.1a,d | 13.4a,b,c | 3.3 |
| ≥4 criteria | 1.0b,c,d | 5.0a,d | 5.5a,d | 11.9a,b,c | 1.4 |
| Nicotine dependence, past month | |||||
| No | 98.0b,c,d | 92.9a,c,d | 91.1a,b,d | 83.5a,b,c | 97.4 |
| Yes | 2.0b,c,d | 7.1a,c,d | 8.9a,b,d | 16.5a,b,c | 2.6 |
| Marijuana use disorder, past year | |||||
| 0–1 criteria | 96.6b,c,d | 87.7a,c,d | 85.2a,b,d | 76.6a,b,c | 95.5 |
| 2–3 criteria | 2.4b,c,d | 7.0a,d | 8.3a,d | 12.2a,b,c | 2.9 |
| ≥4 criteria | 1.0b,c,d | 5.3a,d | 6.5a,d | 11.2a,b,c | 1.6 |
| Other drug use disorders, past year | |||||
| 0–1 criteria | 98.8b,c,d | 91.6a,c,d | 93.9a,b,d | 77.4a,b,c | 98.1 |
| 2–3 criteria | 0.8b,c,d | 4.7a,c,d | 3.5a,b,d | 10.0a,b,c | 1.1 |
| ≥4 criteria | 0.4b,c,d | 3.7a,c,d | 2.5a,b,d | 12.6a,b,c | 0.7 |
| Criminal justice involvement, past year | |||||
| No | 98.6b,c,d | 95.4a,c,d | 92.7a,b,d | 88.3a,b,c | 98.1 |
| Yes | 1.4b,c,d | 4.6a,c,d | 7.3a,b,d | 11.7a,b,c | 1.9 |
Alcohol use disorder criteria, marijuana use disorder criteria, and other drug use disorder criteria were the original Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, criteria excluding the criterion of legal problems. However, nicotine dependence was assessed based on the dependence criteria according to the Nicotine Dependence Syndrome Scale and the Fagerström Test of Nicotine Dependence.
Significantly different from “none” (p < .05);
significantly different from “self-direct” (p < .05);
significantly different from “other directed” (p < .05);
significantly different from “combined” (p < .05).
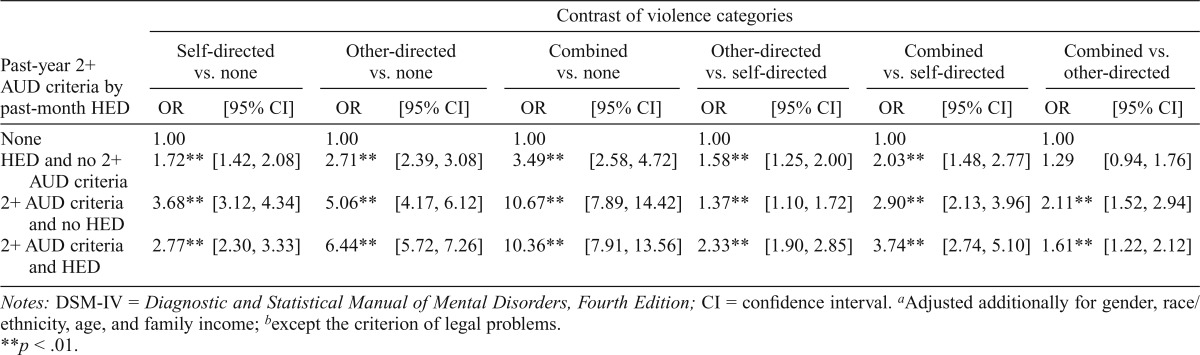
The multinomial logistic regression, including the dummy variables of two or more AUD criteria and HED as predictors, is shown in Table 2. Each dummy variable shows significantly higher odds for each violence category versus no violence, but the dummy variables for two or more AUD criteria, with and without HED, show significantly higher odds for each violence category than HED alone. Each variable also confers significantly higher odds for other-directed and combined violence versus self-directed violence. Having two or more AUD criteria, with and without HED, confers significantly higher odds for combined violence versus either self-directed or other-directed violence. Therefore, we chose an increased number of AUD criteria rather than HED for the following analyses.
Table 2.
Adjusted odds ratios (ORs)a from multinomial logistic regression of violence categories on past-year 2+ DSM-IV alcohol use disorder (AUD) criteriab and past-month heavy episodic drinking (HED), among youth ages 12–17
| Past-year 2+ AUD criteria by past-month HED | Contrast of violence categories |
|||||||||||
| Self-directed vs. none |
Other-directed vs. none |
Combined vs. none |
Other-directed vs. self-directed |
Combined vs. self-directed |
Combined vs. other-directed |
|||||||
| OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | |
| None | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| HED and no 2+ AUD criteria | 1.72** | [1.42, 2.08] | 2.71** | [2.39, 3.08] | 3.49** | [2.58, 4.72] | 1.58** | [1.25, 2.00] | 2.03** | [1.48, 2.77] | 1.29 | [0.94, 1.76] |
| 2+ AUD criteria and no HED | 3.68** | [3.12, 4.34] | 5.06** | [4.17, 6.12] | 10.67** | [7.89, 14.42] | 1.37** | [1.10, 1.72] | 2.90** | [2.13, 3.96] | 2.11** | [1.52, 2.94] |
| 2+ AUD criteria and HED | 2.77** | [2.30, 3.33] | 6.44** | [5.72, 7.26] | 10.36** | [7.91, 13.56] | 2.33** | [1.90, 2.85] | 3.74** | [2.74, 5.10] | 1.61** | [1.22, 2.12] |
Notes: DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; CI = confidence interval.
Adjusted additionally for gender, race/ethnicity, age, and family income;
except the criterion of legal problems.
p < .01.
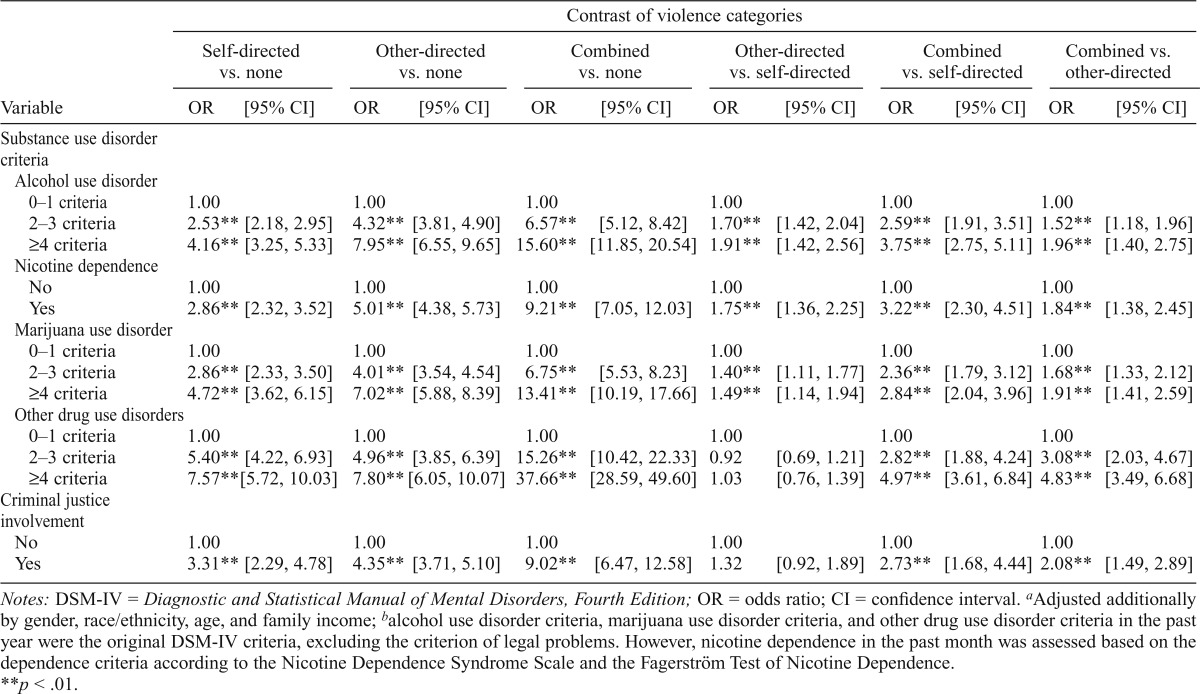
Table 3 shows the odds ratios, adjusted for sociodemographics, from multinomial logistic regression models with an increased number of criteria of SUD and criminal justice involvement separately as the independent variable. Each predictor is a risk factor with significantly higher odds for each violence category versus no violence. The increased number of AUD criteria and marijuana use disorder criteria and nicotine dependence confer significantly higher odds for other-directed versus self-directed violence. Each predictor has higher odds for combined violence versus other- and self-directed violence.
Table 3.
Adjusted odds ratiosa from multinomial logistic regression of violence categories on each covariate from past-year DSM-IV substance use disorder criteriab and criminal justice involvement separately, among youth ages 12–17
| Variable | Contrast of violence categories |
|||||||||||
| Self-directed vs. none |
Other-directed vs. none |
Combined vs. none |
Other-directed vs.self-directed |
Combined vs. self-directed |
Combined vs. other-directed |
|||||||
| OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | |
| Substance use disorder criteria | ||||||||||||
| Alcohol use disorder | ||||||||||||
| 0–1 criteria | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 2–3 criteria | 2.53** | [2.18, 2.95] | 4.32** | [3.81, 4.90] | 6.57** | [5.12, 8.42] | 1.70** | [1.42, 2.04] | 2.59** | [1.91,3.51] | 1.52** | [1.18, 1.96] |
| ≥4 criteria | 4.16** | [3.25, 5.33] | 7.95** | [6.55, 9.65] | 15.60** | [11.85, 20.54] | 1.91** | [1.42, 2.56] | 3.75** | [2.75,5.11] | 1.96** | [1.40, 2.75] |
| Nicotine dependence | ||||||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Yes | 2.86** | [2.32, 3.52] | 5.01** | [4.38, 5.73] | 9.21** | [7.05, 12.03] | 1.75** | [1.36, 2.25] | 3.22** | [2.30,4.51] | 1.84** | [1.38, 2.45] |
| Marijuana use disorder | ||||||||||||
| 0–1 criteria | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 2–3 criteria | 2.86** | [2.33, 3.50] | 4.01** | [3.54, 4.54] | 6.75** | [5.53, 8.23] | 1.40** | [1.11, 1.77] | 2.36** | [1.79,3.12] | 1.68** | [1.33, 2.12] |
| ≥4 criteria | 4.72** | [3.62, 6.15] | 7.02** | [5.88, 8.39] | 13.41** | [10.19, 17.66] | 1.49** | [1.14, 1.94] | 2.84** | [2.04,3.96] | 1.91** | [1.41, 2.59] |
| Other drug use disorders | ||||||||||||
| 0–1 criteria | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 2–3 criteria | 5.40** | [4.22, 6.93] | 4.96** | [3.85, 6.39] | 15.26** | [10.42, 22.33] | 0.92 | [0.69, 1.21] | 2.82** | [1.88,4.24] | 3.08** | [2.03, 4.67] |
| ≥4 criteria | 7.57** | [5.72, 10.03] | 7.80** | [6.05, 10.07] | 37.66** | [28.59, 49.60] | 1.03 | [0.76, 1.39] | 4.97** | [3.61,6.84] | 4.83** | [3.49, 6.68] |
| Criminal justice involvement | ||||||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Yes | 3.31** | [2.29, 4.78] | 4.35** | [3.71, 5.10] | 9.02** | [6.47, 12.58] | 1.32 | [0.92, 1.89] | 2.73** | [1.68,4.44] | 2.08** | [1.49, 2.89] |
Notes: DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; OR = odds ratio; CI = confidence interval.
Adjusted additionally by gender, race/ethnicity, age, and family income;
alcohol use disorder criteria, marijuana use disorder criteria, and other drug use disorder criteria in the past year were the original DSM-IV criteria, excluding the criterion of legal problems. However, nicotine dependence in the past month was assessed based on the dependence criteria according to the Nicotine Dependence Syndrome Scale and the Fagerström Test of Nicotine Dependence.
p < .01.
Table 4 shows the odds ratios from multinomial logistic regression including all other variables of interest in addition to sociodemographic factors. With no violence as the reference for comparison, males have higher odds for other-directed violence and lower odds for self-directed and combined violence than females. Compared with non-Hispanic Whites, non-Hispanic Blacks have lower odds for self-directed violence and higher odds for other-directed and combined violence, non-Hispanic Native Americans have higher odds for other-directed violence, non-Hispanic Asians have lower odds for self-directed violence, non-Hispanics with multiple races have higher odds for each violence category, and Hispanics have lower odds for self-directed violence and higher odds for other-directed violence. Increased age indicates higher odds for self-directed violence and lower odds for other-directed violence. Family income less than $75,000 indicates higher odds for each violence class versus no violence.
For other-directed versus self-directed violence, male gender, non-Hispanic Black and Hispanic (compared with non-Hispanic White), and younger age indicate higher odds. For combined versus self-directed violence, male gender and non-Hispanic Black and mixed race indicate higher odds, but non-Hispanic Native Hawaiian/other Pacific Islander and older age indicate lower odds. For combined versus other-directed violence, non-Hispanic mixed race indicates higher odds, but male gender, non-Hispanic Black, non-Hispanic Native Hawaiian/other Pacific Islander, and Hispanic indicate lower odds.
The increased number of criteria for each substance use and criminal justice involvement confer significantly higher odds for each violence category versus no violence. For other-directed versus self-directed violence, the increased number of AUD criteria and nicotine dependence confer high odds and the increased number of other drug use disorder (DUD) criteria confers lower odds. For combined versus self-directed violence, nicotine dependence, and the increased number of AUD criteria and other DUD criteria confer higher odds. For combined versus other-directed violence, the increased number of other DUD criteria confers higher odds.
Although MDE and aggregate assault were not part of the violence typology for self-directed and other-directed violence, respectively, they were found to be significant predictors in two separate models adjusting for the same background variables as in other models presented in Table 3. MDE in the past year confers higher odds for combined violence versus self-directed violence (OR = 1.32, 95% CI [1.08, 1.61], p = .008). Aggravated assault in the past year confers significantly higher odds for combined violence versus other-directed violence (OR = 1.66, 95% CI [1.12, 2.45], p = .012).
Discussion
Ancillary to the research on SUDs, this study explored the predictive associations of two or more DSM-IV AUD criteria (except the criterion of legal problems) and HED with violence. Findings from the study indicate that the measure of two or more AUD criteria by itself without HED is more strongly associated with violence than HED by itself without two or more AUD criteria. Adolescents diagnosed with two or more AUD criteria, whether they engaged in HED or not, tend to have significantly higher odds for reporting violence in each category than those who engaged in HED but had 0–1 AUD criteria. Although the presence of HED in the past 30 days hardly constitutes an adequate measure of heavy alcohol use over time, adolescents who engage in HED are unquestionably at risk for violence. The endorsement of DSM-IV symptom criteria, whether or not it indicates greater severity, would appear to indicate greater problematic and persistent substance involvement than HED, at least with respect to violence behavior in the NSDUH sample of 12- to 17-year-olds.
Although SUD criteria are a risk factor for violence, the risk of self-directed, other-directed, and combined violence varies by different substances. Findings from the present study indicate that alcohol, marijuana, and other DUD criteria and nicotine dependence are significantly related to violence toward others and self. They are consistent with the findings from general population studies of violence toward others (Coid et al., 2006; Corrigan & Watson, 2005; Pulay et al., 2008) and toward self (Borowsky et al., 2001; Harris & Barraclough, 1997; Roy et al., 1990) and, more importantly, expand on the findings from prior studies for combined violence (Bossarte et al., 2008; Cleary, 2000; Harford et al., 2012; Swahn et al., 2013).
Nevertheless, comparisons between the violence categories show that the increased number of marijuana use disorder criteria was no longer a significant predictor to discriminate one form of violence from another. Neither did the increased number of AUD criteria or nicotine dependence significantly discriminate between combined and other-directed violence. When compared with self-directed violence, the odds for other-directed violence were raised by the increased number of AUD criteria and nicotine dependence but lowered by the increased number of other DUD criteria, whereas the odds for combined violence were raised by the increased number of other DUD criteria. Further, the increased number of other DUD criteria was the only one among SUD criteria to distinguish between combined and other-directed violence.
Moss et al. (2014) note that early polysubstance use of alcohol, cigarettes, and marijuana (notably alcohol and marijuana, and alcohol, cigarettes, and marijuana) is strongly related to DSM-IV SUDs in young adulthood and the use of other illicit drugs. This is frequently identified as the “gateway” hypothesis in the classic studies by Kandel (1975) and Kandel and Faust (1975), which posit that the major substances of use accompany other illicit drug involvement and potentially serve as a gateway to deeper drug involvement. Our findings further indicate that those arrested for aggravated assault were at significantly higher risk for the combined violence relative to other-directed violence, as were those with MDE for combined violence relative to self-directed violence. Overall, these findings indicate that the combined violence group represents a high-risk subpopulation of adolescents.
Consistent with the literature, female gender and older age were related to self-directed violence, whereas male gender and younger age were related to violence toward others. Lower family income was related to all forms of violence (McLaughlin et al., 2011), although family income did not differentiate between different forms of violence. This risk profile of race-ethnicity is comparable to the reports of previous studies (Harford et al., 2012; Wu et al., 2011) and indicates higher violence toward others among non-Hispanic Black, Native American, and mixed race, and Hispanic youth and lower violence toward self among non-Hispanic Black and Asian and Hispanic youth when compared with non-Hispanic White youth. Studies of multiracial youth indicate heavy involvement in substance use and violence (Chen et al., 2012; Choi et al., 2006; Wu et al., 2011).
In a previous NSDUH study, Chen et al. (2012) found that HED and illicit drug use among mixed-race adolescents were associated with delinquent behaviors, affiliations with delinquent peers, and lower parental perceptions of drug use as harmful. Although marginalization among minorities inhibits ties to conventional institutions (e.g., family and school), perceived racial discrimination and poor ethnic identity are important risk factors for mixed-race youth (Choi et al., 2006). In the present study, non-Hispanic mixed race is the only racial/ethnic group that consistently exhibits significantly higher risk than non-Hispanic White for self-directed, other-directed, and combined violence among youth.
A number of study limitations need to be highlighted. First, although the surveys provide extensive data on SUDs, psychiatric history was excluded in the NSDUH youth sample. Second, the measurement and categorization of violent behavior in the present study are based on retrospective reports and are restricted to a limited number of question items. Third, the assessment of suicide attempt includes two separate measurement contexts—periods of depression and treatment—either of which may introduce variations in lethality, ideation, seriousness in intent to die, impulsivity, or more extensive psychiatric complications. Although more detailed assessment of suicide attempt is beyond the scope and measurement in the present study, separate analysis for the two assessments yielded comparable findings related to the SUD criteria and other study covariates. Fourth, the measurement of criminal justice involvement excludes individuals who avoid arrest or engage in other social transgressions.
Fifth, other-directed violence does not discriminate between the roles of instigator and victim, multiparty instigation, or incident severity. Sixth, many persons who engage in violence may be incarcerated or homeless and thus are not included in the survey sample analyzed in this study; the estimates of the prevalence of violence categories are conservative. Seventh, the study is limited to cross-sectional data, which impede the assessment of directionality between important covariates (i.e., SUDs, arrest, and MDE) and the co-occurrence of attack and suicide attempt. Eighth, in NSDUH, the measure of HED was based on the past 30 days and the measure of DSM-IV AUD was based on the past year; therefore, the comparison of violence risk between HED and two or more DSM-IV criteria could be affected by the different reference periods. Finally, our focus on ordered categorization of SUD severity in terms of the increased number of SUD criteria is not consistent with the DSM-IV SUD diagnosis typically found in the literature.
However, deviation from the norm is justifiable in the transition to DSM-5. For example, in the case of AUD, studies indicate that DSM-IV AUD criteria do not provide support for the distinction between alcohol abuse and dependence (Langenbucher et al., 2004; Martin et al., 1996) and that DSM-IV AUD criteria are indicators of a unidimensional latent trait (Gelhorn et al., 2007; Harford et al., 2009; Kirisci et al., 2006; Saha et al., 2006). Interpretation of DSM-IV AUD is further complicated by both conceptual and measurement issues (Gelhorn et al., 2008; Harford et al., 2010; Hasin & Paykin, 1998, 1999; Schuckit et al., 2008).
DSM-IV excludes individuals who report one or two alcohol-dependence criteria (i.e., diagnostic orphans), and these individuals are actually at a higher risk for subsequent AUDs compared with those without any dependence criteria (Harford et al., 2010). Because the DSM-IV diagnosis of alcohol abuse may include diagnostic orphans who met one or two dependence criteria, comparisons between abuse and dependence are confounded. Gelhorn and colleagues (2008) noted that DSM-IV diagnosis of alcohol abuse may include some individuals who meet all four abuse criteria as well as two dependence criteria.
Coupled with the NESARC study of adult violence (Harford et al., 2013), the present study provides further support that combined violence is a meaningful and reliable categorization of violence in both adult and youth populations. Because this study concerns nonfatal violence only, mortality studies are needed to determine the extent to which combined violence can be a useful category of violent behavior for our understanding of murder–suicide cases. Many mental health disorders include aggressive behaviors toward others and self (i.e., schizophrenia, bipolar mood disorders, personality disorder) and may pose a major risk factor for these rare events. Measures of aggressive impulsivity need to be incorporated into longitudinal studies to examine the long-range outcomes related to this population.
In conclusion, HED, increased severity of AUD, and polysubstance use disorders are risk factors for violence and should be the focus of school-based prevention programs. Findings from the present study underscore the need for comprehensive prevention programs with targeted interventions to prevent or reduce self-directed and other-directed forms of violent behaviors. Prevention and treatment programs particularly need to address combined violence. Although the percentage of combined violence in this general population of 12- to 17-year-olds is small (0.8%), this group was associated with higher internalizing and externalizing disorders, which could pose problems for intervention designed to target only one side of the symptoms. Future studies on the correlates of combined violence are thus recommended. More generally, it is essential to emphasize approaches that combine and/or coordinate adolescent health care and criminal justice.
Footnotes
This article is based on a study conducted for the Alcohol Epidemiologic Data System project funded by the National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health through Contract No. HH-SN275201300016C to CSR, Incorporated. The views and opinions expressed in this article are those of the authors and should not be construed to represent the views of the sponsoring agency or the federal government.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: Author; 2013. [Google Scholar]
- Apter A., Plutchik R., van Praag H. M. Anxiety, impulsivity and depressed mood in relation to suicidal and violent behavior. Acta Psychiatrica Scandinavica. 1993;87:1–5. doi: 10.1111/j.1600-0447.1993.tb03321.x. doi:10.1111/j.1600-0447.1993.tb03321.x. [DOI] [PubMed] [Google Scholar]
- Borowsky I. W., Ireland M., Resnick M. D. Adolescent suicide attempts: Risks and protectors. Pediatrics. 2001;107:485–493. doi: 10.1542/peds.107.3.485. doi:10.1542/peds.107.3.485. [DOI] [PubMed] [Google Scholar]
- Bossarte R. M., Simon T. R., Swahn M. H. Clustering of adolescent dating violence, peer violence, and suicidal behavior. Journal of Interpersonal Violence. 2008;23:815–833. doi: 10.1177/0886260507313950. doi:10.1177/0886260507313950. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. WISQARS. 2015 [Web-based injury statistics query and reporting system]. Retrieved from http://webappa.cdc.gov/sasweb/ncipc/leadcaus10_us.html. [Google Scholar]
- Chen H. J., Balan S., Price R. K. Association of contextual factors with drug use and binge drinking among White, Native American, and mixed-race adolescents in the general population. Journal of Youth and Adolescence. 2012;41:1426–1441. doi: 10.1007/s10964-012-9789-0. doi:10.1007/s10964-012-9789-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi Y., Harachi T. W., Gillmore M. R., Catalano R. F. Are multiracial adolescents at greater risk? Comparisons of rates, patterns, and correlates of substance use and violence between monoracial and multiracial adolescents. American Journal of Orthopsychiatry. 2006;76:86–97. doi: 10.1037/0002-9432.76.1.86. doi:10.1037/0002-9432.76.1.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleary S. D. Adolescent victimization and associated suicidal and violent behaviors. Adolescence. 2000;35:671–682. [PubMed] [Google Scholar]
- Coid J., Yang M., Roberts A., Ullrich S., Moran P., Bebbington P., Singleton N. Violence and psychiatric morbidity in a national household population—A report from the British Household Survey. American Journal of Epidemiology. 2006;164:1199–1208. doi: 10.1093/aje/kwj339. doi:10.1093/aje/kwj339. [DOI] [PubMed] [Google Scholar]
- Corrigan P. W., Watson A. C. Findings from the National Comorbidity Survey on the frequency of violent behavior in individuals with psychiatric disorders. Psychiatry Research. 2005;136:153–162. doi: 10.1016/j.psychres.2005.06.005. doi:10.1016/j.psychres.2005.06.005. [DOI] [PubMed] [Google Scholar]
- Fagerström K. O. Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addictive Behaviors. 1978;3:235–241. doi: 10.1016/0306-4603(78)90024-2. doi:10.1016/0306-4603(78)90024-2. [DOI] [PubMed] [Google Scholar]
- Gelhorn H., Hartman C., Sakai J., Stallings M., Young S., Rhee S. H., Crowley T. Toward DSM-V: An item response theory analysis of the diagnostic process for DSM-IV alcohol abuse and dependence in adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:1329–1339. doi: 10.1097/CHI.0b013e318184ff2e. doi:10.1097/CHI.0b013e318184ff2e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelhorn H. L., Sakai J. T., Price R. K., Crowley T. J. DSM-IV conduct disorder criteria as predictors of antisocial personality disorder. Comprehensive Psychiatry. 2007;48:529–538. doi: 10.1016/j.comppsych.2007.04.009. doi:10.1016/j.comppsych.2007.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harford T. C., Yi H.-Y., Faden V. B., Chen C. M. The dimensionality of DSM-IV alcohol use disorders among adolescent and adult drinkers and symptom patterns by age, gender, and race/ethnicity. Alcoholism: Clinical and Experimental Research. 2009;33:868–878. doi: 10.1111/j.1530-0277.2009.00910.x. doi:10.1111/j.1530-0277.2009.00910.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harford T. C., Yi H.-Y., Freeman R. C. A typology of violence against self and others and its associations with drinking and other drug use among high school students in a U.S. general population survey. Journal of Child & Adolescent Substance Abuse. 2012;21:349–366. doi: 10.1080/1067828X.2012.710028. doi:10.1080/1067828X.2012.710028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harford T. C., Yi H.-Y., Grant B. F. The five-year diagnostic utility of “diagnostic orphans” for alcohol use disorders in a national sample of young adults. Journal of Studies on Alcohol and Drugs. 2010;71:410–417. doi: 10.15288/jsad.2010.71.410. doi:10.15288/jsad.2010.71.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harford T. C., Yi H.-Y., Grant B. F. Other- and self-directed forms of violence and their relationships to DSM-IV substance use and other psychiatric disorders in a national survey of adults. Comprehensive Psychiatry. 2013;54:731–739. doi: 10.1016/j.comppsych.2013.02.003. doi:10.1016/j.comppsych.2013.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris E. C., Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. British Journal of Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. doi:10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- Hasin D., Paykin A. Dependence symptoms but no diagnosis: Diagnostic ‘orphans’ in a community sample. Drug and Alcohol Dependence. 1998;50:19–26. doi: 10.1016/s0376-8716(98)00007-6. doi:10.1016/S0376-8716(98)00007-6. [DOI] [PubMed] [Google Scholar]
- Hasin D., Paykin A. Dependence symptoms but no diagnosis: Diagnostic ‘orphans’ in a 1992 national sample. Drug and Alcohol Dependence. 1999;53:215–222. doi: 10.1016/s0376-8716(98)00133-1. doi:10.1016/S0376-8716(98)00133-1. [DOI] [PubMed] [Google Scholar]
- Heatherton T. F., Kozlowski L. T., Frecker R. C., Fagerström K. O. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. doi:10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Kandel D. Stages in adolescent involvement in drug use. Science. 1975;190:912–914. doi: 10.1126/science.1188374. doi:10.1126/science.1188374. [DOI] [PubMed] [Google Scholar]
- Kandel D., Faust R. Sequence and stages in patterns of adolescent drug use. Archives of General Psychiatry. 1975;32:923–932. doi: 10.1001/archpsyc.1975.01760250115013. doi:10.1001/archpsyc.1975.01760250115013. [DOI] [PubMed] [Google Scholar]
- Kirisci L., Tarter R. E., Vanyukov M., Martin C., Mezzich A., Brown S. Application of item response theory to quantify substance use disorder severity. Addictive Behaviors. 2006;31:1035–1049. doi: 10.1016/j.addbeh.2006.03.033. doi:10.1016/j.addbeh.2006.03.033. [DOI] [PubMed] [Google Scholar]
- Langenbucher J. W., Labouvie E., Martin C. S., Sanjuan P. M., Bavly L., Kirisci L., Chung T. An application of item response theory analysis to alcohol, cannabis, and cocaine criteria in DSM-IV. Journal of Abnormal Psychology. 2004;113:72–80. doi: 10.1037/0021-843X.113.1.72. doi:10.1037/0021-843X.113.1.72. [DOI] [PubMed] [Google Scholar]
- Links P. S., Gould B., Ratnayake R. Assessing suicidal youth with antisocial, borderline, or narcissistic personality disorder. Canadian Journal of Psychiatry. 2003;48:301–310. doi: 10.1177/070674370304800505. [DOI] [PubMed] [Google Scholar]
- Martin C. S., Langenbucher J. W., Kaczynski N. A., Chung T. Staging in the onset of DSM-IV alcohol symptoms in adolescents: Survival/hazard analyses. Journal of Studies on Alcohol. 1996;57:549–558. doi: 10.15288/jsa.1996.57.549. doi:10.15288/jsa.1996.57.549. [DOI] [PubMed] [Google Scholar]
- McLaughlin K. A., Breslau J., Green J. G., Lakoma M. D., Sampson N. A., Zaslavsky A. M., Kessler R. C. Childhood socioeconomic status and the onset, persistence, and severity of DSM-IV mental disorders in a US national sample. Social Science & Medicine. 2011;73:1088–1096. doi: 10.1016/j.socscimed.2011.06.011. doi:10.1016/j.socscimed.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss H. B., Chen C. M., Yi H.-Y. Early adolescent patterns of alcohol, cigarettes, and marijuana polysubstance use and young adult substance use outcomes in a nationally representative sample. Drug and Alcohol Dependence. 2014;136:51–62. doi: 10.1016/j.drugalcdep.2013.12.011. doi:10.1016/j.drugalcdep.2013.12.011. [DOI] [PubMed] [Google Scholar]
- Muthén L. K., Muthén B. O.1998. –2012Mplus user’s guide 7th ed.Los Angeles, CA: Authors [Google Scholar]
- Pfeffer C. R., Newcorn J., Kaplan G., Mizruchi M. S., Plutchik R. Subtypes of suicidal and assaultive behaviors in adolescent psychiatric inpatients: A research note. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 1989;30:151–163. doi: 10.1111/j.1469-7610.1989.tb00774.x. doi:10.1111/j.1469-7610.1989.tb00774.x. [DOI] [PubMed] [Google Scholar]
- Plutchik R. Outward and inward directed aggressiveness: The interaction between violence and suicidality. Pharmacopsychiatry. 1995;28(Supplement 2):47–57. doi: 10.1055/s-2007-979620. doi:10.1055/s-2007-979620. [DOI] [PubMed] [Google Scholar]
- Plutchik R., van Praag H. M., Conte H. R. Correlates of suicide and violence risk: III. A two-stage model of countervailing forces. Psychiatry Research. 1989;28:215–225. doi: 10.1016/0165-1781(89)90048-6. doi:10.1016/0165-1781(89)90048-6. [DOI] [PubMed] [Google Scholar]
- Pulay A. J., Dawson D. A., Hasin D. S., Goldstein R. B., Ruan W. J., Pickering R. P., Grant B. F. Violent behavior and DSM-IV psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2008;69:12–22. doi: 10.4088/jcp.v69n0103. doi:10.4088/JCP.v69n0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J., Marmet S., Anderson P., Gual A., Kraus L., Nutt D. J., Gmel G. Defining substance use disorders: Do we really need more than heavy use? Alcohol and Alcoholism. 2013;48:633–640. doi: 10.1093/alcalc/agt127. doi:10.1093/alcalc/agt127. [DOI] [PubMed] [Google Scholar]
- Roy A., Lamparski D., DeJong J., Moore V., Linnoila M. Characteristics of alcoholics who attempt suicide. American Journal of Psychiatry. 1990;147:761–765. doi: 10.1176/ajp.147.6.761. doi:10.1176/ajp.147.6.761. [DOI] [PubMed] [Google Scholar]
- Saha T. D., Chou S. P., Grant B. F. Toward an alcohol use disorder continuum using item response theory: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine. 2006;36:931–941. doi: 10.1017/S003329170600746X. doi:10.1017/S003329170600746X. [DOI] [PubMed] [Google Scholar]
- Saunders J. B. The concept of substance use disorders. A commentary on ‘Defining substance use disorders: Do we really need more than heavy use’ by Rehm et al. Alcohol and Alcoholism. 2013;48:644–645. doi: 10.1093/alcalc/agt146. doi:10.1093/alcalc/agt146. [DOI] [PubMed] [Google Scholar]
- Schuckit M. A., Danko G. P., Smith T. L., Bierut L. J., Bucholz K. K., Edenberg H. J., Hinga B. The prognostic implications of DSM-IV abuse criteria in drinking adolescents. Drug and Alcohol Dependence. 2008;97:94–104. doi: 10.1016/j.drugalcdep.2008.03.020. doi:10.1016/j.drugalcdep.2008.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. 2013 National Survey on Drug Use and Health Public Use File Codebook. Rockville, MD: Author; 2014. [Google Scholar]
- Swahn M. H., Bossarte R. M., Palmier J. B., Yao H. Co-occurring physical fighting and suicide attempts among U.S. high school students: Examining patterns of early alcohol use initiation and current binge drinking. Western Journal of Emergency Medicine. 2013;14:341–346. doi: 10.5811/westjem.2013.3.15705. doi:10.5811/westjem.2013.3.15705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L. T., Woody G. E., Yang C., Pan J. J., Blazer D. G. Racial/ethnic variations in substance-related disorders among adolescents in the United States. Archives of General Psychiatry. 2011;68:1176–1185. doi: 10.1001/archgenpsychiatry.2011.120. doi:10.1001/archgenpsychiatry.2011.120. [DOI] [PMC free article] [PubMed] [Google Scholar]