Abstract
Objective:
Use of marijuana before or while driving significantly contributes to driving impairment and elevated risk of motor vehicle accidents; however, this risk behavior is common among users. Little is known about the etiology of driving while under the influence of marijuana.
Method:
Guided by social learning theory, this study examined marijuana outcome expectancies and other driving-related cognitions as predictors of the frequency of driving after smoking marijuana (DASM) and smoking marijuana while driving (SMWD). A community sample of 151 (64% male) non–treatment-seeking frequent marijuana users completed questionnaires on variables of interest.
Results:
Perceived driving-related peer norms (i.e., perception that fewer friends disapprove of DASM and SMWD and of riding with a driver under the influence of marijuana) were associated with lower frequency of both DASM and SMWD. Perceived dangerousness of DASM was also associated with decreased frequency of DASM.
Conclusions:
Our findings suggest a range of potentially important targets for interventions intended to reduce the likelihood and frequency of driving while under the influence of marijuana.
Marijuana is the most commonly used drug other than alcohol in the United States (Substance Abuse and Mental Health Services Administration, 2013). Since 1996, 23 states and Washington, DC, have legalized and enacted comprehensive public medical marijuana programs. Both Washington and Colorado passed legislation to allow use of marijuana for recreational purposes (Office of National Drug Control Policy, 2013), and Oregon and Alaska have passed similar legislation (Ferner, 2014a, 2014b). As states continue to adopt legislation to decriminalize and to medically and recreationally legalize marijuana, its availability and the prevalence of use is likely to increase considerably. Widespread use, along with legislative changes in marijuana drug policy, is of substantial public health concern, particularly with respect to the potential for increasing incidence of marijuana-related risk behaviors.
Driving under the influence of marijuana
One particularly concerning risk behavior is driving while under the influence of marijuana, which may include driving after smoking marijuana (DASM) or smoking marijuana while driving (SMWD). Despite past controversy about marijuana’s impact on driving (Smiley, 1998), research suggests that marijuana significantly impairs judgment, motor coordination, and reaction time, and studies have found a direct association between blood Δ9-ntetrahydrocannabinol (THC) concentration and impaired driving ability (Hartman & Huestis, 2013; Lenné et al., 2010). Specifically, individuals who drive after use of marijuana display increased psychomotor impairment and delayed reaction to obstacles in the road (Liguori et al., 1998; Ramaekers et al., 2004). Marijuana use is associated with significantly increased risk of involvement in a motor vehicle accident (Li et al., 2012) and elevated risk of fatal accidents (Asbridge et al., 2012). Crash risk increases progressively with the dose and frequency of marijuana use (Li et al., 2012), with the risk of being involved in an accident virtually doubling after marijuana use (Ramaekers et al., 2004). This dose-dependent association is particularly alarming because of the increasing potency of marijuana (Mehmedic et al., 2010; Vindenes et al., 2013) and the increased prevalence of marijuana-involved driving in recent years (Johnson et al., 2012). Furthermore, acute marijuana use has been associated with reported reduction in driving speed; however, such conscious efforts to compensate for potential impairment may be misleading as they are largely unsuccessful and likely contribute to a false perception of safer driving (Bates & Blakely, 1999).
Despite the clear risks, rates of driving under the influence of marijuana are high. Of current marijuana users in college, 44% of men and 9% of women reported driving after using marijuana in the past 28 days, and 51% of men and 35% of women reported riding with a driver who had recently used marijuana (Whitehill et al., 2014). In another college student sample, driving after marijuana use was as common as driving following alcohol consumption and was perceived to be more normative with fewer adverse consequences (McCarthy et al., 2007). Recent research in Colorado found that the proportion of drivers in fatal motor vehicle crashes who were marijuana-positive was decreasing before marijuana legalization but has increased after legalization and is higher relative to other states (Salomonsen-Sautel et al., 2014). There was also a significant increase in marijuana-positive driving among fatally injured drivers in California (Pollini et al., 2015). Although driving while under the influence of marijuana is common, not all marijuana users engage in this behavior, and it is unclear what differentiates between those who do and do not. As described below, potential individual differences in marijuana-related cognitions that may provide key insights into this growing public health problem include expectancies, normative perceptions, perceived dangerousness, and perceived negative consequences.
Marijuana-related cognitions
Social learning theory (SLT; Bandura, 1969; Bandura & Cervone, 1986) provides a unifying framework for examining the comparative roles that marijuana-related cognitions play in decisions to drive while under the influence of marijuana. According to SLT (Bandura & Cervone, 1986), outcome expectancies, defined as cognitive representations of learning processes reflecting positively and negatively valenced effects of drug consumption, are key determinants of behavior, conceptualized as mediators through which learning and biology influence decisions. While marijuana outcome expectancies are established as predictors of marijuana use patterns (Aarons et al., 2001; Schafer & Brown, 1991; Vangsness et al., 2005), more research is needed to determine their influence on driving while under the influence of marijuana. Only one study to date, conducted among college students, has focused on this question, and found that more salient negative marijuana expectancies were associated with lower likelihood of driving while under the influence of marijuana (Arterberry et al., 2013).
SLT also highlights the role of learning from the social environment, which may be apparent in one’s perceptions regarding the incidence (i.e., descriptive norms) and/or acceptability (i.e., injunctive norms) of a given behavior. Research suggests that perceived norms are important factors in understanding marijuana use and related risk behaviors (Kilmer et al., 2006; LaBrie et al., 2010; Neighbors et al., 2008). Perceived peer disapproval of driving following marijuana use or riding with a driver under the influence of marijuana may be protective against engaging in such behaviors (Arterberry et al., 2013; McCarthy et al., 2007). Consequently, perception of these behaviors as normative may be a crucial predictor of driving while under the influence of marijuana.
Two additional cognitive predictors of driving under the influence of marijuana include perceived dangerousness of driving after marijuana use and perceived negative consequences of driving under the influence of marijuana. In line with these perceptions, marijuana users often erroneously believe that marijuana does not impair driving performance or increase accident risk (Swift et al., 2010). Among college students, the perception that driving following smoking marijuana is less dangerous—reflected by lower scores on a measure of perceived dangerousness of driving under the influence of marijuana—was associated with a higher likelihood of and frequency of driving following marijuana use (Arterberry et al., 2013; McCarthy et al., 2007). Students who scored lower on a measure of the perception of negative consequences of driving under the influence of marijuana—reflecting the perception that negative consequences are less probable—reported increased frequency of driving following use in one college sample (McCarthy et al., 2007) but not in another (Arterberry et al., 2013).
Gaps in the literature
Limited empirical evidence suggests that marijuana outcome expectancies, perceived norms regarding marijuana use and driving, and other driving-related marijuana cognitions may play important roles in the decision to drive while under the influence of marijuana. However, additional research with regular marijuana users in community samples is needed to better understand the propensity to drive while under the influence of marijuana.
The goal of this research was to assess risk factors for DASM in a community sample of frequent marijuana users. We advance prior research via analysis of risk factors for SMWD, a distinction that may pose even greater risk than DASM. As compared to DASM, SMWD may increase risk for driving during peak marijuana-related behavioral impairment and may increase the risk of arrest for both driving while in possession of marijuana and driving under the influence of marijuana. The psychoactive effect of marijuana is experienced almost immediately after smoking, peaking after approximately 30 minutes and lasting 1–3 hours (Grotenhermen, 2003). Consequently, marijuana intoxication would likely coincide with driving if someone is smoking in a vehicle but may or may not be at peak levels if it is smoked at some point before driving. Despite challenges with roadside testing for marijuana intoxication (Looby et al., 2007), evidence of SMWD carries stronger implications for the criminal offense of driving under the influence of marijuana, again distinguishing this as a potentially more risky behavior. Furthermore, much like smoking tobacco cigarettes while driving (Stevens & Minton, 2001), handling marijuana materials while driving detracts from attention to the road and surroundings. Coupled with established impairments in attention and concentration during marijuana intoxication (Crane et al., 2013; Ramaekers et al., 2009), SMWD ultimately places the driver, passengers, and others at risk.
Present study
Guided by SLT and prior research, we hypothesized that the following risk factors would be associated with greater levels of driving while under the influence of marijuana (DASM and SMWD): stronger positive marijuana outcome expectancies, weaker negative marijuana outcome expectancies, lower perceived dangerousness, lower perceived likelihood of negative consequences of driving while under the influence of marijuana, and less salient perceived driving-related peer norms measured by perceived peer disapproval of driving during/after smoking and perceived refusal to ride with a driver who had smoked or was smoking marijuana.
Method
Sample description
This study uses data obtained from participants (N = 151) who completed the baseline assessments of an experimental study of marijuana’s acute effects on impulsivity (Metrik et al., 2012). This Brown University Institutional Review Board–approved study recruited non–treatment-seeking frequent marijuana users from the community who met the following inclusion criteria: native English speakers, 18–30 years of age, marijuana use at least once per week in the past month and at least 10 times in the past 6 months, and self-reported ability to abstain from marijuana for 24 hours without withdrawal (due to the marijuana administration component of the parent study). Exclusion criteria were the following: history of substance use treatment or intent to quit or receive treatment for marijuana use; past-month affective disorder or history of panic attacks, psychotic state, or suicidal state; alcohol dependence determined with the Structured Clinical Interview for DSM-IV Non-Patient Edition (SCID; First et al., 2002); and smoking 20 or more tobacco cigarettes per day (see Metrik et al., 2012, for more details).
Measures
The reliable and valid calendar-assisted, clinician-administered Timeline Followback interview (Dennis et al., 2004) was used to assess past-60-day use of marijuana, alcohol, and tobacco. Minor and serious marijuana-related problems during the past 90 days were assessed with the 22-item Marijuana Problems Scale (Stephens et al., 2000).
Driving while under the influence of marijuana.
Lifetime frequency of DASM was assessed with a single question asking how many times a participant had driven after smoking marijuana during his or her lifetime. Participants selected one of the following seven responses: never, 1–2 times, 3–5 times, 6–10 times, 11–50 times, 51–100 times, or over 100 times. SMWD was assessed with a single dichotomous (yes/no) question asking whether participants had ever smoked marijuana in the car while driving.
Marijuana-related cognitions.
Marijuana outcome expectancies were assessed with the 48-item Marijuana Effect Expectancy Questionnaire (MEEQ; Schafer & Brown, 1991). The MEEQ measures positive marijuana outcome expectancies across three domains (relaxation and tension reduction, social and sexual facilitation, perceptual and cognitive enhancement) and negative marijuana outcome expectancies across three domains (cognitive and behavioral impairment, global negative effects, and craving and physical effects). Items are rated on 5-point Likert scales from 1 (disagree strongly) to 5 (agree strongly). Mean composite scores were used for positive and negative subscales. In the current sample, internal consistency (Cronbach’s α) for each of these two subscales was .81.
Three domains of driving-related cognitions pertaining to driving while under the influence of marijuana were assessed including perceived driving-related peer norms, perceived dangerousness, and perceived negative consequences (Arterberry et al., 2013; McCarthy et al., 2007). Perceived driving-related peer norms were assessed with two items (r = .83) asking participants to indicate how many (0–3) of their three closest friends disapprove of DASM/SMWD and how many would refuse to ride with a friend who was DASM/SMWD. Responses to these two questions were summed for a total normative belief score. Perceived dangerousness of driving while under the influence of marijuana was assessed with a single item asking how dangerous it is to drive within 2 hours after smoking marijuana on a 4-point Likert scale (not at all dangerous to very dangerous). Perceived negative consequences of DASM/SMWD were assessed via four questions whereby participants rated the likelihood a driver their age would experience certain consequences from driving during/after smoking marijuana, comprising being stopped by police, being drug tested, being arrested, and having an accident. Responses were made on a 4-point Likert scale (not very likely to very likely). A mean composite was used. Cronbach’s α was .78.
Data analytic plan
Descriptive statistics and regression analyses were executed in SPSS Version 22 (IBM Corp., Armonk, NY). Initial bivariate correlations examined the relationships among measures of driving outcomes, expectancies, and driving cognitions. Multiple regression was used to examine predictors of lifetime frequency of DASM in one model. Logistic regression was used to examine predictors of whether participants reported ever SMWD in another model. In both models, predictors included positive and negative marijuana expectancies and driving-related cognitions (perceived dangerousness, perceived negative consequences, and perceived norms for driving). Gender was included as a covariate in all models because of gender differences commonly reported in the literature regarding driving under the influence of marijuana (Richer & Bergeron, 2009; Whitehill et al., 2014). Age was also included as a covariate because older age would present more opportunity to engage in SMWD or DASM.
Results
Marijuana use and driving descriptives
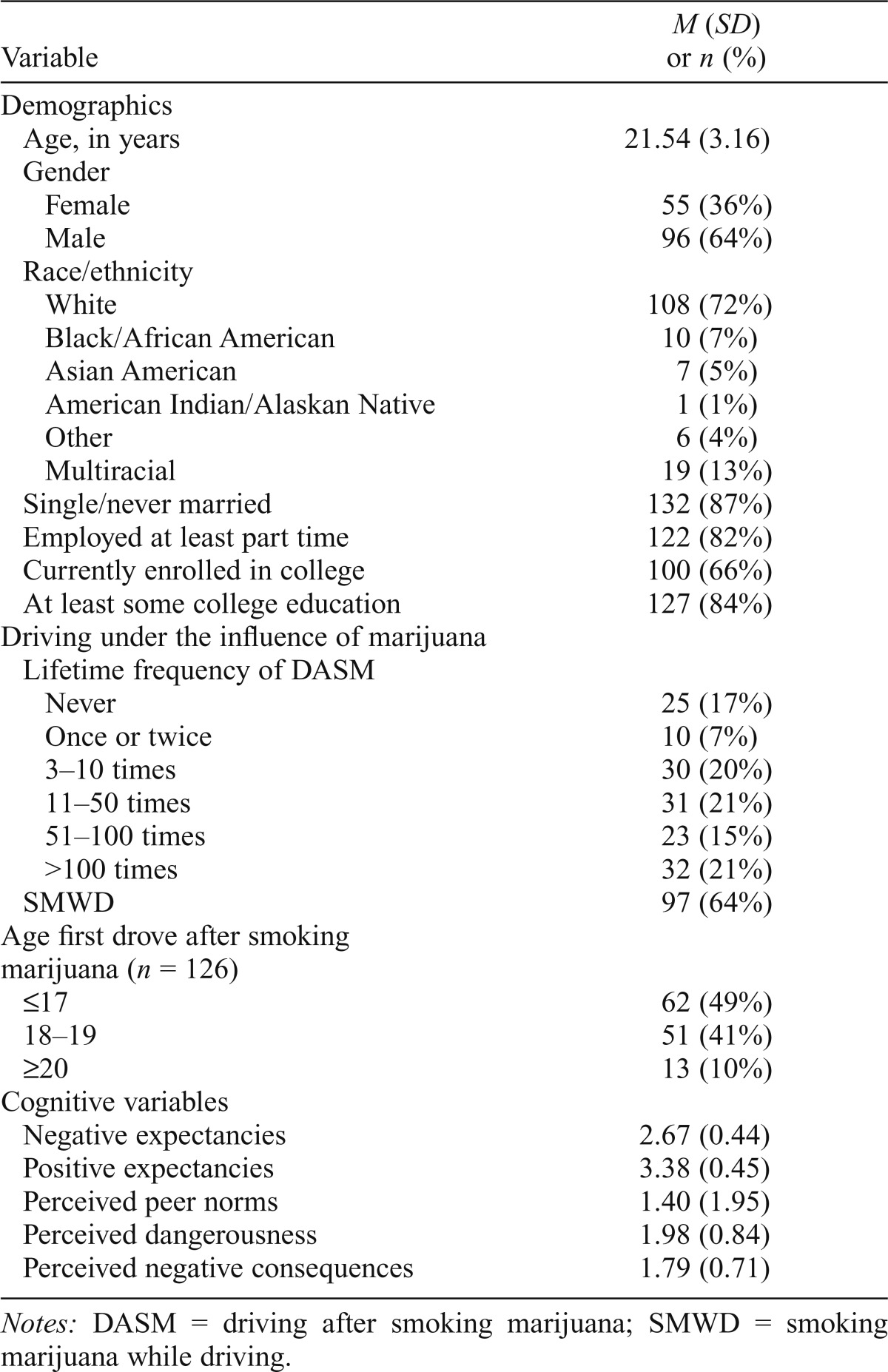
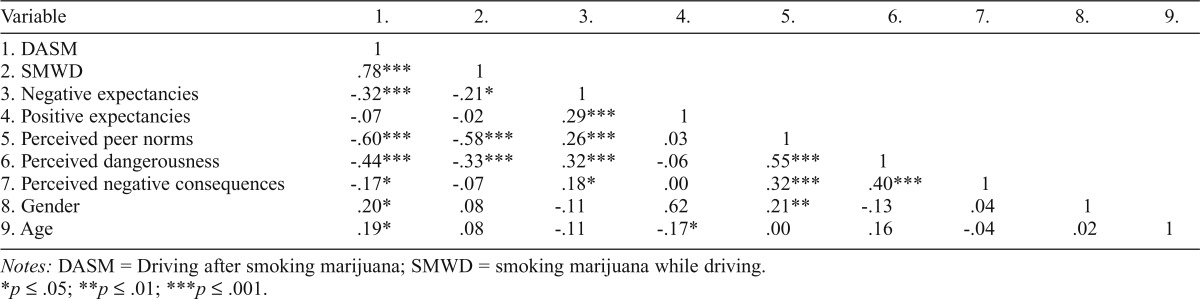
Sample descriptive and substance use characteristics are presented in Tables 1 and 2. With respect to driving under the influence of marijuana, 83% of the sample reported DASM and 64% of the sample reported SMWD during their lifetime. Model variable intercorrelations are presented in Table 3. DASM was positively correlated with SMWD, gender, and age, and negatively correlated with negative expectancies, perceived peer norms, perceived dangerousness, and perceived negative consequences (ps < .05). SMWD was negatively correlated with negative expectancies, perceived peer norms, and perceived dangerousness (ps < .05).
Table 1.
Sample descriptives
| Variable | M (SD) or n (%) |
| Demographics | |
| Age, in years | 21.54 (3.16) |
| Gender | |
| Female | 55 (36%) |
| Male | 96 (64%) |
| Race/ethnicity | |
| White | 108 (72%) |
| Black/African American | 10 (7%) |
| Asian American | 7 (5%) |
| American Indian/Alaskan Native | 1 (1%) |
| Other | 6 (4%) |
| Multiracial | 19 (13%) |
| Single/never married | 132 (87%) |
| Employed at least part time | 122 (82%) |
| Currently enrolled in college | 100 (66%) |
| At least some college education | 127 (84%) |
| Driving under the influence of marijuana | |
| Lifetime frequency of DASM | |
| Never | 25 (17%) |
| Once or twice | 10 (7%) |
| 3–10 times | 30 (20%) |
| 11–50 times | 31 (21%) |
| 51–100 times | 23 (15%) |
| >100 times | 32 (21%) |
| SMWD | 97 (64%) |
| Age first drove after smoking marijuana (n = 126) | |
| ≤17 | 62 (49%) |
| 18–19 | 51 (41%) |
| ≥20 | 13 (10%) |
| Cognitive variables | |
| Negative expectancies | 2.67 (0.44) |
| Positive expectancies | 3.38 (0.45) |
| Perceived peer norms | 1.40 (1.95) |
| Perceived dangerousness | 1.98 (0.84) |
| Perceived negative consequences | 1.79 (0.71) |
Notes: DASM = driving after smoking marijuana; SMWD = smoking marijuana while driving.
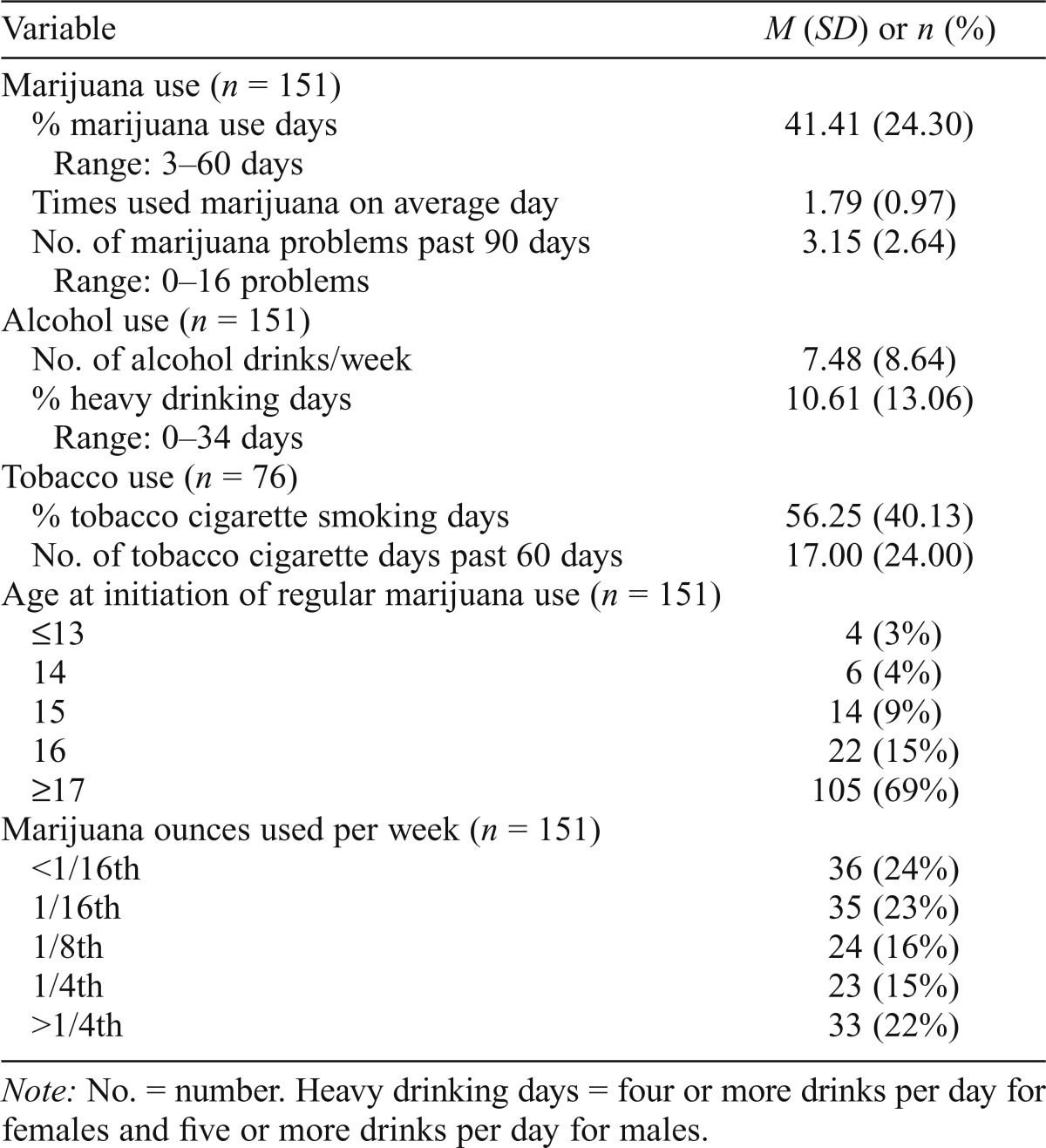
Table 2.
Substance use characteristics
| Variable | M (SD) or n (%) |
| Marijuana use (n = 151) | 41.41 (24.30) |
| % marijuana use days | |
| Range: 3–60 days | |
| Times used marijuana on average day | 1.79 (0.97) |
| No. of marijuana problems past 90 days | 3.15 (2.64) |
| Range: 0–16 problems | |
| Alcohol use (n = 151) | |
| No. of alcohol drinks/week | 7.48 (8.64) |
| % heavy drinking days | 10.61 (13.06) |
| Range: 0–34 days | |
| Tobacco use (n = 76) | |
| % tobacco cigarette smoking days | 56.25 (40.13) |
| No. of tobacco cigarette days past 60 days | 17.00 (24.00) |
| Age at initiation of regular marijuana use (n = 151) | |
| ≤13 | 4 (3%) |
| 14 | 6 (4%) |
| 15 | 14 (9%) |
| 16 | 22 (15%) |
| ≥17 | 105 (69%) |
| Marijuana ounces used per week (n = 151) | |
| ˂1/16th | 36 (24%) |
| 1/16th | 35 (23%) |
| 1/8th | 24 (16%) |
| 1/4th | 23 (15%) |
| >1/4th | 33 (22%) |
Note: No. = number. Heavy drinking days = four or more drinks per day for females and five or more drinks per day for males.
Table 3.
Variable intercorrelations
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. |
| 1. DASM | 1 | ||||||||
| 2. SMWD | .78*** | 1 | |||||||
| 3. Negative expectancies | -.32*** | -.21* | 1 | ||||||
| 4. Positive expectancies | -.07 | -.02 | .29*** | 1 | |||||
| 5. Perceived peer norms | -.60*** | -.58*** | .26*** | .03 | 1 | ||||
| 6. Perceived dangerousness | -.44*** | -.33*** | .32*** | -.06 | .55*** | 1 | |||
| 7. Perceived negative consequences | -.17* | -.07 | .18* | .00 | .32*** | .40*** | 1 | ||
| 8. Gender | .20* | .08 | -.11 | .62 | .21** | -.13 | .04 | 1 | |
| 9. Age | .19* | .08 | -.11 | -.17* | .00 | .16 | -.04 | .02 | 1 |
Notes: DASM = Driving after smoking marijuana; SMWD = smoking marijuana while driving.
p ≤ .05;
p ≤ .01;
p ≤ .001.
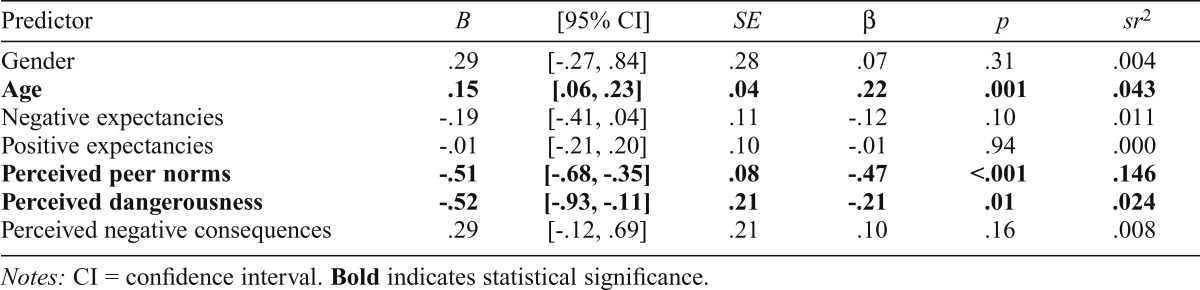
Predicting frequency of driving after smoking marijuana
Table 4 presents the multiple regression model results for predicting frequency of DASM. As hypothesized, less salient perceived driving-related peer norms (i.e., perception that fewer friends disapprove of driving during/after smoking and of riding with a driver under the influence of marijuana) were associated with increased frequency of DASM. Perceptions that driving while under the influence of marijuana is less dangerous—reflected by lower scores on a measure of perceived dangerousness of driving under the influence of marijuana—were associated with increased frequency of DASM. Negative and positive marijuana expectancies and perceived negative consequences were not significantly associated with DASM.
Table 4.
Multiple regression model predicting frequency of driving after smoking marijuana (n = 151)
| Predictor | B | [95% CI] | SE | β | p | sr2 |
| Gender | .29 | [-.27, .84] | .28 | .07 | .31 | .004 |
| Age | .15 | [.06, .23] | .04 | .22 | .001 | .043 |
| Negative expectancies | -.19 | [-.41, .04] | .11 | -.12 | .10 | .011 |
| Positive expectancies | -.01 | [-.21, .20] | .10 | -.01 | .94 | .000 |
| Perceived peer norms | -.51 | [-.68, -.35] | .08 | -.47 | <.001 | .146 |
| Perceived dangerousness | -.52 | [-.93, -.11] | .21 | -.21 | .01 | .024 |
| Perceived negative consequences | .29 | [-.12, .69] | .21 | .10 | .16 | .008 |
Notes: CI = confidence interval. Bold indicates statistical significance.
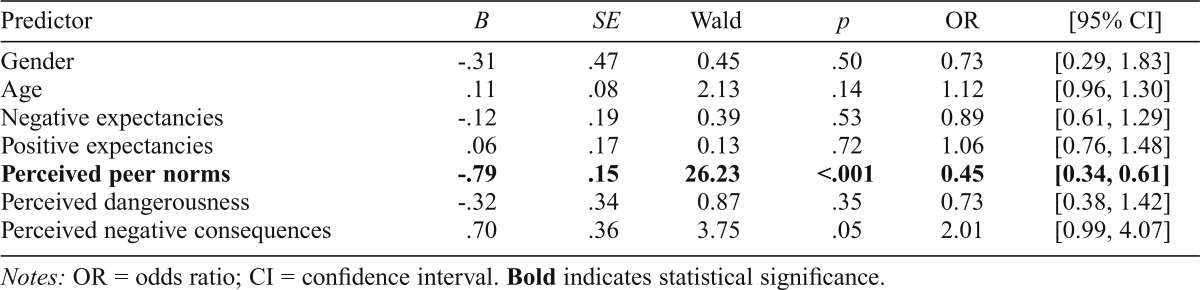
Predicting smoking marijuana while driving
Table 5 presents the logistic regression model results for predicting SMWD. Two participants had missing data on this outcome; thus, models were run using an n of 149. As hypothesized, higher levels of the perceived norms variable (i.e., peer disapproval) were associated with decreased likelihood of SMWD. However, both negative and positive marijuana expectancies, perceived dangerousness, and perceived negative consequences were not significantly associated with SMWD.
Table 5.
Logistic regression model predicting smoking marijuana while driving (n = 149)
| Predictor | B | SE | Wald | p | OR | [95% CI] |
| Gender | -.31 | .47 | 0.45 | .50 | 0.73 | [0.29, 1.83] |
| Age | .11 | .08 | 2.13 | .14 | 1.12 | [0.96, 1.30] |
| Negative expectancies | -.12 | .19 | 0.39 | .53 | 0.89 | [0.61, 1.29] |
| Positive expectancies | .06 | .17 | 0.13 | .72 | 1.06 | [0.76, 1.48] |
| Perceived peer norms | -.79 | .15 | 26.23 | <.001 | 0.45 | [0.34, 0.61] |
| Perceived dangerousness | -.32 | .34 | 0.87 | .35 | 0.73 | [0.38, 1.42] |
| Perceived negative consequences | .70 | .36 | 3.75 | .05 | 2.01 | [0.99, 4.07] |
Notes: OR = odds ratio; CI = confidence interval. Bold indicates statistical significance.
Discussion
The present study examined predictors of the frequency of DASM and likelihood of SMWD in a community sample of regular marijuana users. Our results revealed one risk factor that was relevant for both greater frequency of DASM and higher likelihood that an individual reported SMWD: perceived peer norms (i.e., belief that fewer friends would disapprove of driving while under the influence of marijuana and would ride with a driver under the influence of marijuana). We also found evidence of a unique predictor of DASM: perception that driving while under the influence of marijuana was less dangerous—reflected by lower scores on a measure of perceived dangerousness of driving under the influence of marijuana—was associated with greater frequency of DASM. This finding replicates outcomes from previous research indicating that perceived dangerousness was linked with driving while under the influence of marijuana (Arterberry et al., 2013). Together, these results suggest that perceived normative beliefs and perceived dangerousness regarding driving while under the influence of marijuana may both be key components contributing to the decision to DASM or SMWD. Targeting perceptions regarding driving under the influence of marijuana as a normative behavior, and one that is not dangerous, may serve to decrease this risk behavior.
Although one would expect an association between negative marijuana expectancies and DASM or SMWD more so than with positive expectancies, neither variable was significantly predictive of either outcome variable in the present study. Arterberry and colleagues (2013) found that negative expectancies were an important predictor of driving while under the influence of marijuana, and further, SLT implicates expectancies regarding the outcomes of a behavior as important predictors of whether one engages in that behavior. In the current study, there was a bivariate association between negative expectancies and both outcome variables. Despite this, there was a lack of association in the multivariate models once the other variables were included, and this is likely a reflection of restriction of range in marijuana experience within the current sample. Arterberry and colleagues (2013) included individuals who reported ever using marijuana during their lifetime in their sample, resulting in a broad range of marijuana use patterns. The current sample, however, comprised frequent marijuana users who reported current marijuana use at least weekly, resulting in a truncated range and a reduction of correlation values with this variable. Consequently, frequent marijuana users in the current study have fewer negative expectancies regarding marijuana use and actually report more salient positive as compared with negative marijuana expectancies. However, positive marijuana expectancies failed to predict marijuana-related driving outcomes in this study and in the study conducted by Arterberry and colleagues (2013). The lack of a relationship between positive expectancies and driving while under the influence of marijuana may be related to the content of the positive marijuana expectancy subscales in the MEEQ measure. Subscales that comprise positive expectancies (i.e., relaxation and tension reduction, social and sexual facilitation, and perceptual and cognitive enhancement) appear to be less relevant to driving-related outcomes as compared with subscales that comprise negative expectancies (i.e., cognitive and behavioral impairment and global negative effects).
The perception of negative consequences specifically associated with DASM or SMWD was not linked with either outcome. This also aligns with previous research whereby perception of negative consequences was not predictive of driving while under the influence of marijuana or likelihood of riding with a driver under the influence of marijuana (Arterberry et al., 2013). Although we did not collect data on driving offenses and legal consequences in this study, it is possible that the participants experienced minimal negative consequences associated with driving while under the influence of marijuana and thus learned that negative consequences associated with this behavior tend to be negligible. Investigation of driving-related offenses and consequences of driving while under the influence of marijuana is a crucial future direction in this line of research. It is also conceivable that recent marijuana-related legislation, such as decriminalization, legal medical marijuana usage, and legal recreational marijuana usage, has contributed to the rise in driving following marijuana use via perpetuation of misperception regarding marijuana being a safe and minimally impairing substance. Unlike blood alcohol concentration testing that is commonly used on the road and linked with driving skill impairment, reliable roadside THC detection testing is still under development. This lack of a universal roadside standard may perpetuate misleading beliefs regarding the safety of driving under the influence of marijuana and contribute to maintenance of this behavior among regular marijuana users. An accurate, reliable, and portable device for roadside testing of marijuana intoxication and impairment is essential and of immediate relevance for public safety. Such roadside testing devices will aid in challenging perception of negligible consequences related to DASM or SMWD and will facilitate prevention efforts to reduce such risky marijuana-related driving behaviors.
Although this research makes valuable contributions to the marijuana-related driving literature, this study is a first step in a line of research pertaining to predictors of driving under the influence of marijuana among regular marijuana users. As such, there are several limitations to this initial investigation. The current study did not collect data on driving offenses or assess whether participants drove on a regular basis; future studies should collect information on driving offenses and typical driving patterns to provide better sample characterization. In addition, the present study relied on retrospective reports of DASM and SMWD, and the question pertaining to DASM did not clearly define the post-smoking period. As such, it is not possible to know exactly when driving following use of marijuana occurred. Furthermore, the two questions regarding perceived peer norms were summed for a total normative belief score consistent with previous research (Arterberry et al., 2013; McCarthy et al., 2007), but future work should tease apart the unique influence of injunctive versus descriptive norms on this behavior. To do so, more comprehensive measures of these constructs, with good psychometric properties, need to be developed. In addition, our measure of DASM used “over 100 times” as the highest response category. Although there is likely variability among those who reported this category (21% of the sample), it is unclear whether individuals who have engaged in this behavior 101 versus 200 times, for example, would be qualitatively different from one another. Moreover, the cross-sectional nature of the study precludes us from ascertaining the direction of the effect of cognitions on driving behavior. Learning that occurs due to increased experience with driving under the influence of marijuana may also result in subsequent alterations regarding the perceived dangerousness, likelihood of negative consequences, or acceptability of such behavior among peers. Finally, marijuana is currently used in many forms and via a multitude of administration modes (i.e., smoked marijuana, portable vaporization devices, and edibles). The measures used in the current study and in previous research included questions specifically pertaining to smoking marijuana. Subsequent research should expand these questions to encompass the many available forms of marijuana and modes of administration, as other forms and modes are likely to make use during driving less difficult, more concealable, and thus more problematic as a public health issue.
An interesting future direction would involve the use of ecological momentary assessment to better ascertain immediate predictors of DASM or SMWD and could facilitate provision of more accurate estimates regarding amount smoked before or during driving, how long before driving marijuana use occurred, or one’s real-time perception of how driving behavior will be affected. Furthermore, perception of driving-related risk may differ as a function of marijuana use pattern and history. Regular marijuana users may perceive reduced risk from DASM or SMWD compared with infrequent users because their experience of driving under the influence without direct negative consequences (e.g., arrest) supports this conviction.
There are several clinical implications of the present research. Findings from the current study suggest that perceived normative beliefs regarding driving while under the influence of marijuana play a crucial role in the decision to DASM or SMWD. Such normative beliefs develop over time following exposure to peer behavior and media portrayal of decisions to drive following substance use. In this regard, although risks regarding driving following consumption of alcohol have been a focus of public service messages for some time, similar campaigns have not yet been launched for marijuana. The absence of such messages and campaigns may lead to increased propensity to engage in this hazardous behavior and perceptions of negligible risk (McCarthy et al., 2007). Shaping public health programs and messages to alter normative perceptions of driving while under the influence of marijuana to capitalize on strengthening negative marijuana outcome expectancies and reducing positive marijuana outcome expectancies will likely have a powerful effect on decreasing instances of DASM or SMWD in this population.
Footnotes
This research was supported by National Institute on Drug Abuse (NIDA) Grant R01DA021403 (to Jane Metrik). Manuscript preparation and data analysis were supported by National Institute on Alcohol Abuse and Alcoholism Grants 2T32AA007459 (to Elizabeth R. Aston and Jennifer E. Merrill), K01AA022938 (to Jennifer E. Merrill), and R01AA019546 (to Denis M. McCarthy), and NIDA Grant K01DA039311 (to Elizabeth R. Aston).
References
- Aarons G. A., Brown S. A., Stice E., Coe M. T. Psychometric evaluation of the marijuana and stimulant effect expectancy questionnaires for adolescents. Addictive Behaviors. 2001;26:219–236. doi: 10.1016/s0306-4603(00)00103-9. doi:10.1016/S0306-4603(00)00103-9. [DOI] [PubMed] [Google Scholar]
- Arterberry B. J., Treloar H. R., Smith A. E., Martens M. P., Pedersen S. L., McCarthy D. M. Marijuana use, driving, and related cognitions. Psychology of Addictive Behaviors. 2013;27:854–860. doi: 10.1037/a0030877. doi:10.1037/a0030877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asbridge M., Hayden J. A., Cartwright J. L. Acute cannabis consumption and motor vehicle collision risk: Systematic review of observational studies and meta-analysis. BMJ. 2012;344:e536. doi: 10.1136/bmj.e536. doi:10.1136/bmj.e536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Social-learning theory of identificatory processes. In: Goslin D. A., editor. Handbook of socialization theory and research. Chicago, IL: Rand McNally; 1969. pp. 213–262. [Google Scholar]
- Bandura A., Cervone D. Differential engagement of self-reactive influences in cognitive motivation. Organizational Behavior and Human Decision Processes. 1986;38:92–113. doi:10.1016/0749-5978(86)90028-2. [Google Scholar]
- Bates M. N., Blakely T. A. Role of cannabis in motor vehicle crashes. Epidemiologic Reviews. 1999;21:222–232. doi: 10.1093/oxfordjournals.epirev.a017998. doi:10.1093/oxfordjournals.epirev.a017998. [DOI] [PubMed] [Google Scholar]
- Crane N. A., Schuster R. M., Fusar-Poli P., Gonzalez R. Effects of cannabis on neurocognitive functioning: Recent advances, neurodevelopmental influences, and sex differences. Neuropsychology Review. 2013;23:117–137. doi: 10.1007/s11065-012-9222-1. doi:10.1007/s11065-012-9222-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M. L., Funk R., Godley S. H., Godley M. D., Waldron H. Cross-validation of the alcohol and cannabis use measures in the Global Appraisal of Individual Needs (GAIN) and Timeline Followback (TLFB; Form 90) among adolescents in substance abuse treatment. Addiction. 2004;99(Supplement 2):120–128. doi: 10.1111/j.1360-0443.2004.00859.x. doi:10.1111/j.1360-0443.2004.00859.x. [DOI] [PubMed] [Google Scholar]
- Ferner M. Oregon becomes third state to legalize recreational marijuana. Huffington Post. 2014a, November 4 Retrieved from http://www.huffingtonpost.com/2014/11/04/oregon-legalizes-marijuana-measure-91_n_5947344.html. [Google Scholar]
- Ferner M. Alaska becomes fourth state to legalize recreational marijuana. Huffington Post. 2014b, November 5 Retrieved from http://www.huffingtonpost.com/2014/11/05/alaska-marijuana-legalization_n_5947516.html. [Google Scholar]
- First M., Spitzer R., Gibbon M., Williams J. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-Patient Edition (SCID-I/NP) New York, NY: Biometrics Research; 2002. [Google Scholar]
- Grotenhermen F. Pharmacokinetics and pharmacodynamics of cannabinoids. Clinical Pharmacokinetics. 2003;42:327–360. doi: 10.2165/00003088-200342040-00003. doi:10.2165/00003088-200342040-00003. [DOI] [PubMed] [Google Scholar]
- Hartman R. L., Huestis M. A. Cannabis effects on driving skills. Clinical Chemistry. 2013;59:478–492. doi: 10.1373/clinchem.2012.194381. doi:10.1373/clinchem.2012.194381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson M. B., Kelley-Baker T., Voas R. B., Lacey J. H. The prevalence of cannabis-involved driving in California. Drug andAlcohol Dependence. 2012;123:105–109. doi: 10.1016/j.drugalcdep.2011.10.023. doi:10.1016/j.drugalcdep.2011.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilmer J. R., Walker D. D., Lee C. M., Palmer R. S., Mallett K. A., Fabiano P., Larimer M. E. Misperceptions of college student marijuana use: Implications for prevention. Journal of Studies on Alcohol. 2006;67:277–281. doi: 10.15288/jsa.2006.67.277. doi:10.15288/jsa.2006.67.277. [DOI] [PubMed] [Google Scholar]
- LaBrie J. W., Hummer J. F., Lac A., Lee C. M. Direct and indirect effects of injunctive norms on marijuana use: The role of reference groups. Journal of Studies on Alcohol and Drugs. 2010;71:904–908. doi: 10.15288/jsad.2010.71.904. doi:10.15288/jsad.2010.71.904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenne M. G., Dietze P. M., Triggs T. J., Walmsley S., Murphy B., Redman J. R. The effects of cannabis and alcohol on simulated arterial driving: Influences of driving experience and task demand. Accident Analysis and Prevention. 2010;42:859–866. doi: 10.1016/j.aap.2009.04.021. doi:10.1016/j.aap.2009.04.021. [DOI] [PubMed] [Google Scholar]
- Li M.-C., Brady J. E., DiMaggio C. J., Lusardi A. R., Tzong K. Y., Li G. Marijuana use and motor vehicle crashes. Epidemiologic Reviews. 2012;34:65–72. doi: 10.1093/epirev/mxr017. doi:10.1093/epirev/mxr017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liguori A., Gatto C. P., Robinson J. H. Effects of marijuana on equilibrium, psychomotor performance, and simulated driving. Behavioural Pharmacology. 1998;9:599–609. doi: 10.1097/00008877-199811000-00015. doi:10.1097/00008877-199811000-00015. [DOI] [PubMed] [Google Scholar]
- Looby A., Earleywine M., Gieringer D. Roadside sobriety tests and attitudes toward a regulated cannabis market. Harm Reduction Journal. 2007;4:4. doi: 10.1186/1477-7517-4-4. doi:10.1186/1477-7517-4-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy D. M., Lynch A. M., Pederson S. L. Driving afteruse of alcohol and marijuana in college students. Psychology of Addictive Behaviors. 2007;21:425–430. doi: 10.1037/0893-164X.21.3.425. doi:10.1037/0893-164X.21.3.425. [DOI] [PubMed] [Google Scholar]
- Mehmedic Z., Chandra S., Slade D., Denham H., Foster S., Patel A. S., ElSohly M. A. Potency trends of Δ9-THC and other cannabinoids in confiscated cannabis preparations from 1993 to 2008. Journal of Forensic Sciences. 2010;55:1209–1217. doi: 10.1111/j.1556-4029.2010.01441.x. doi:10.1111/j.1556-4029.2010.01441.x. [DOI] [PubMed] [Google Scholar]
- Metrik J., Kahler C. W., Reynolds B., McGeary J. E., Monti P. M., Haney M., Rohsenow D. J. Balanced placebo design with marijuana: Pharmacological and expectancy effects on impulsivity and risk taking. Psychopharmacology. 2012;223:489–499. doi: 10.1007/s00213-012-2740-y. doi:10.1007/s00213-012-2740-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neighbors C., Geisner I. M., Lee C. M. Perceived marijuana norms and social expectancies among entering college student marijuana users. Psychology of Addictive Behaviors. 2008;22:433–438. doi: 10.1037/0893-164X.22.3.433. doi:10.1037/0893-164X.22.3.433. [DOI] [PubMed] [Google Scholar]
- Office of National Drug Control Policy. Marijuana Resource Center: State Laws Related to Marijuana. 2013. Retrieved from https://www.whitehouse.gov/ondcp/state-laws-related-to-marijuana. [Google Scholar]
- Pollini R. A., Romano E., Johnson M. B., Lacey J. H. The impact of marijuana decriminalization on California drivers. Drug and Alcohol Dependence. 2015;150:135–140. doi: 10.1016/j.drugalcdep.2015.02.024. doi:10.1016/j.drugalcdep.2015.02.024. [DOI] [PubMed] [Google Scholar]
- Ramaekers J. G., Berghaus G., van Laar M., Drummer O. H. Dose related risk of motor vehicle crashes after cannabis use. Drug and Alcohol Dependence. 2004;73:109–119. doi: 10.1016/j.drugalcdep.2003.10.008. doi:10.1016/j.drugalcdep.2003.10.008. [DOI] [PubMed] [Google Scholar]
- Ramaekers J. G., Kauert G., Theunissen E. L., Toennes S. W., Moeller M. R. Neurocognitive performance during acute THC intoxication in heavy and occasional cannabis users. Journal of Psychopharmacology. 2009;23:266–277. doi: 10.1177/0269881108092393. doi:10.1177/0269881108092393. [DOI] [PubMed] [Google Scholar]
- Richer I., Bergeron J. Driving under the influence of cannabis: Links with dangerous driving, psychological predictors, and accident involvement. Accident Analysis and Prevention. 2009;41:299–307. doi: 10.1016/j.aap.2008.12.004. doi:10.1016/j.aap.2008.12.004. [DOI] [PubMed] [Google Scholar]
- Salomonsen-Sautel S., Min S.-J., Sakai J. T., Thurstone C., Hopfer C. Trends in fatal motor vehicle crashes before and after marijuana commercialization in Colorado. Drug and Alcohol Dependence. 2014;140:137–144. doi: 10.1016/j.drugalcdep.2014.04.008. doi:10.1016/j.drugalcdep.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer J., Brown S. A. Marijuana and cocaine effect expectancies and drug use patterns. Journal of Consulting and Clinical Psychology. 1991;59:558–565. doi: 10.1037//0022-006x.59.4.558. doi:10.1037/0022-006X.59.4.558. [DOI] [PubMed] [Google Scholar]
- Smiley A. Marijuana: On-road and driving simulator studies. In: Kalant H., editor. The health effects of cannabis. Toronto, Ontario: Centre for Addiction and Mental Health; 1998. [Google Scholar]
- Stephens R. S., Roffman R. A., Curtin L. Comparison of extended versus brief treatments for marijuana use. Journal of Consulting and Clinical Psychology. 2000;68:898–908. doi:10.1037/0022-006X.68.5.898. [PubMed] [Google Scholar]
- Stevens A., Minton R. In-vehicle distraction and fatal accidents in England and Wales. Accident Analysis and Prevention. 2001;33:539–545. doi: 10.1016/s0001-4575(00)00068-3. doi:10.1016/S0001-4575(00)00068-3. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. 2013. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings (HHS Publication No. (SMA) 13–4795). Rockville, MD: Author. [Google Scholar]
- Swift W., Jones C., Donnelly N. Cannabis use while driving: A descriptive study of Australian cannabis users. Drugs: Education, Prevention and Policy. 2010;17:573–586. doi:10.3109/09687630903264286. [Google Scholar]
- Vangsness L., Bry B. H., LaBouvie E. W. Impulsivity, negative expectancies, and marijuana use: A test of the acquired preparedness model. Addictive Behaviors. 2005;30:1071–1076. doi: 10.1016/j.addbeh.2004.11.003. doi:10.1016/j.addbeh.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Vindenes V, Strand D. H., Kristoffersen L., Boix F, Mørland J. Has the intake of THC by cannabis users changed over the last decade? Evidence of increased exposure by analysis of blood THC concentrations in impaired drivers. Forensic Science International. 2013;226:197–201. doi: 10.1016/j.forsciint.2013.01.017. doi:10.1016/j.forsciint.2013.01.017. [DOI] [PubMed] [Google Scholar]
- Whitehill J. M., Rivara F. P., Moreno M. A. Marijuana-using drivers, alcohol-using drivers, and their passengers: Prevalence and risk factors among underage college students. JAMA Pediatrics. 2014;168:618–624. doi: 10.1001/jamapediatrics.2013.5300. doi:10.1001/jamapediatrics.2013.5300. [DOI] [PMC free article] [PubMed] [Google Scholar]