Abstract
Objective:
People consume alcohol at problematic levels for many reasons. These different motivational pathways may have different biological underpinnings. Valid, brief measures that discriminate individuals’ reasons for drinking could facilitate inquiry into whether varied drinking motivations account for differential response to pharmacotherapies for alcohol use disorders. The current study evaluated the factor structure and predictive validity of a brief measure of alcohol use motivations developed for use in randomized clinical trials, the Reasons for Heavy Drinking Questionnaire (RHDQ).
Method:
The RHDQ was administered before treatment to 265 participants (70% male) with alcohol dependence according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, in three pharmacotherapy randomized clinical trials. Principal components analysis was used in half the sample to determine the RHDQ factor structure. This structure was verified with confirmatory factor analysis in the second half of the sample. The factors derived from this analysis were evaluated with respect to alcohol dependence severity indices.
Results:
A two-factor solution was identified. Factors were interpreted as Reinforcement and Normalizing. Reinforcement scores were weakly to moderately associated with severity, whereas normalizing scores were moderately to strongly associated with severity. In all cases in which significant associations between RHDQ scores and severity indices were observed, the relationship was significantly stronger for normalizing than for reinforcing.
Conclusions:
The RHDQ is a promising brief assessment of motivations for heavy alcohol use, particularly in the context of randomized clinical trials. Additional research should address factor structure stability in non–treatment-seeking individuals and the RHDQ’s utility in detecting and accounting for changes in drinking behavior, including in response to intervention.
The motives people endorse for drinking contribute to the development and maintenance of problematic alcohol use. Theoretical models posit that people drink for positive-rewarding-reinforcement benefit (Kuntsche et al., 2006), to relieve stress (i.e., negative reinforcement; DeMartini & Carey, 2011), to satisfy cravings (Anton et al., 1996), to restore suppressed allostatic balance (Koob, 2003), or out of habit (Vollstädt-Klein et al., 2010). These motives are all related to heavy, problematic drinking. Strong positive reinforcement or enhancement motives are related to higher alcohol quantity consumed (Cooper, 1994; Kuntsche et al., 2006). Strong endorsement of coping motives (drinking alcohol to alleviate acute distress) (Cooper et al., 1995; Thomas et al., 2003) is linked to greater alcohol problems, including dependence (Carpenter & Hasin, 1999; Merrill & Read, 2010). Higher severity of withdrawal-like symptoms has been linked to greater craving among alcohol-dependent adults, supporting a connection between withdrawal-relief motives and heavy drinking (Heinz et al., 2003; Malcolm et al., 2000). Although habit-based reasons for drinking have not been studied systematically, habitual or “compulsive” drinking has been linked to problematic drinking (Anton et al., 1996; Roberts et al., 1999). Measurement of individuals’ reasons for drinking could allow prediction of future problems and development of tailored treatments.
In clinical and research settings, there is value in understanding the relationships between treatment or experimental manipulations and individuals’ reasons for heavy drinking, particularly when investigating an intervention’s mechanism of action. Although various existing drinking motives scales have been validated in adults ranging from undergraduates to individuals with alcohol dependence (e.g., Kristjansson et al., 2011; Kuntsche et al., 2006; Mezquita et al., 2011), most were not developed for use in the context of treatment planning or monitoring with treatment-seeking populations, limiting their clinical utility.
Extant measures focus on motives (e.g., social facilitation, conformity) that are widely endorsed among young people and community samples of adults but may be less germane to treatment-seeking alcohol-dependent individuals (Kuntsche et al., 2006). For instance, commonly used measures do not evaluate the avoidance or “normalization” of withdrawal symptoms as a reason for drinking. Such reasons may be salient to individuals with physiological dependence who drink to avoid withdrawal and restore allostatic balance (Koob, 2003). In addition, most measures are too long (Kuntsche et al., 2005) for use in clinical research trials, which often entail extensive assessment batteries administered repeatedly. Thus, brief, psychometrically sound measures of reasons for drinking that could be administered in clinical trials with treatment-seeking individuals are needed.
We evaluated the utility of the Reasons for Heavy Drinking Questionnaire (RHDQ) in a large group of alcohol-dependent individuals seeking treatment in outpatient clinical trials. This initial validation study focused on the structure and psychometric properties of the RHDQ. Other validated scales capturing various aspects of drinking amount, craving, and severity were used to evaluate concurrent validity and conceptual convergence of the RHDQ.
Method
Participants
Data were obtained in three separate double-blind, randomized clinical trials of medications for alcohol dependence (N = 265). Studies were approved by the institutional review board. Participants were recruited via media advertisements, provided written informed consent, and did not participate in more than one study. Participants completed the RHDQ during a baseline visit before medication randomization. Study 1 evaluated the effects of naltrexone alone and in combination with gabapentin (Anton et al., 2011). Study 2 evaluated the effects of naltrexone alone and in combination with aripiprazole. Study 3 evaluated whether a genetic polymorphism moderates naltrexone response.
Participants (Table 1) met criteria for alcohol dependence according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; American Psychiatric Association, 1994), assessed via the Structured Clinical Interview for DSM-IV (First et al., 2002). Exclusion criteria were diagnosis of current/past dependence on any other substance except nicotine; current primary Axis I disorder; past-month use of any other substance except nicotine or marijuana (except Study 3; see below), indicated by urine drug screen and self-report; current suicidal/homicidal ideation; current psychotropic medication use (except Study 3; see below); serious alcohol-related medical illness; liver enzyme (alanine aminotransferase and aspartate aminotransferase) levels more than three times normal; and pending legal charges (i.e., none court referred).
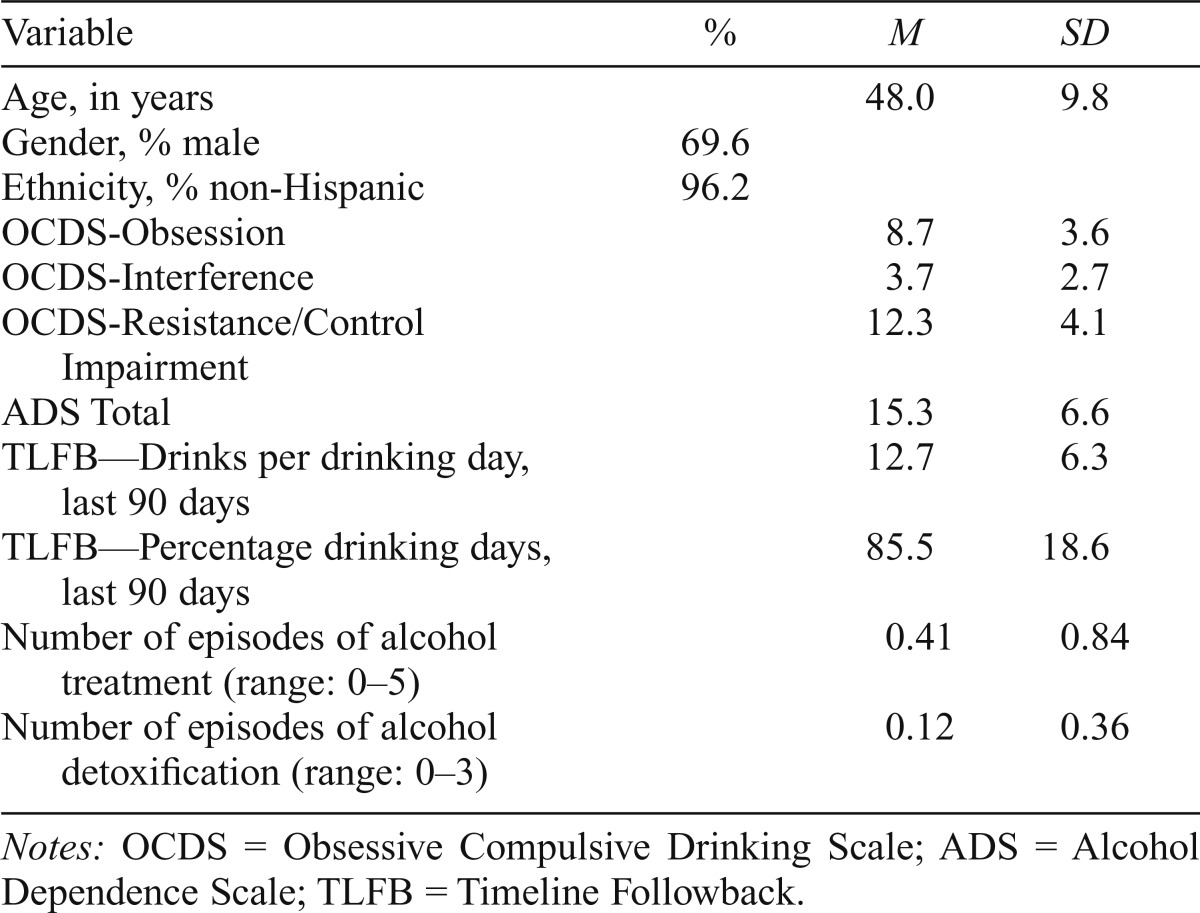
Table 1.
Sample characteristics of treatment-seeking alcohol-dependent individuals participating in three pharmacotherapy trials (N = 265)
| Variable | % | M | SD |
| Age, in years | 48.0 | 9.8 | |
| Gender, % male | 69.6 | ||
| Ethnicity, % non-Hispanic | 96.2 | ||
| OCDS-Obsession | 8.7 | 3.6 | |
| OCDS-Interference | 3.7 | 2.7 | |
| OCDS-Resistance/Control Impairment | 12.3 | 4.1 | |
| ADS Total | 15.3 | 6.6 | |
| TLFB—Drinks per drinking day, last 90 days | 12.7 | 6.3 | |
| TLFB—Percentage drinking days, last 90 days | 85.5 | 18.6 | |
| Number of episodes of alcohol treatment (range: 0–5) | 0.41 | 0.84 | |
| Number of episodes of alcohol detoxification (range: 0–3) | 0.12 | 0.36 |
Notes: OCDS = Obsessive Compulsive Drinking Scale; ADS = Alcohol Dependence Scale; TLFB = Timeline Followback.
Participants were required to be 21–65 years of age (M = 48.0, SD = 9.8) and able to maintain 4-day sobriety before randomization. For Study 1, participants were required to have a history of no more than one inpatient alcohol detoxification admission; for Study 2, participants were required to drink 10 or more drinks per day; and for Study 3, current antidepressant use and past-month cocaine use were permitted (a negative urine drug screen for cocaine was required before participating).
Measures
Reasons for Heavy Drinking Questionnaire.
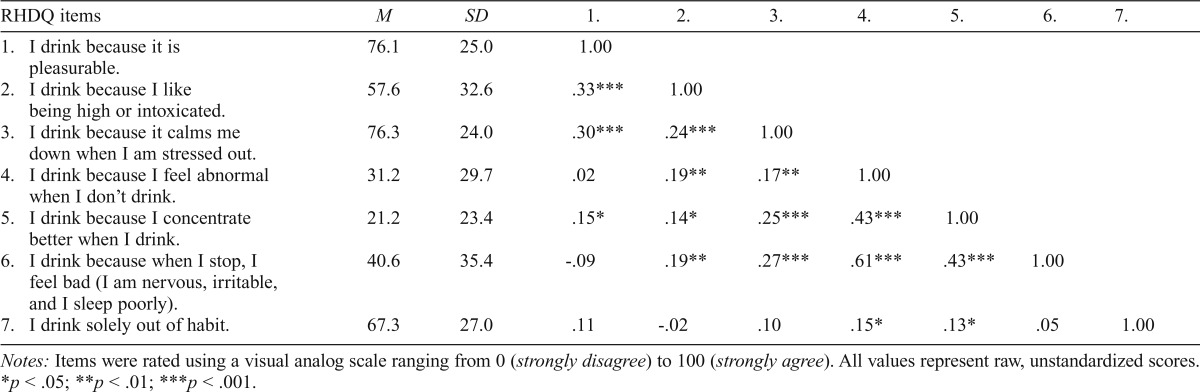
The RHDQ included seven items and was constructed by one of the authors (R.F.A.) after interviews with hundreds of individuals participating in pharmacotherapy trials over many years, as a brief self-report tool to capture domains relevant to reasons people may drink to excess. Participants rated each item by marking a position on a visual analog scale ranging from 0 (strongly disagree) to 100 (strongly agree) presented as a line on a tablet computer; scores were computed by the software based on the relative position marked on each line. Items, means, and standard deviations are presented in Table 2.
Table 2.
Means, standard deviations, and correlations among Reasons for Heavy Drinking Questionnaire (RHDQ) items (N = 265)
| RHDQ items | M | SD | 1. | 2. | 3. | 4. | 5. | 6. | 7. |
| 1. I drink because it is pleasurable. | 76.1 | 25.0 | 1.00 | ||||||
| 2. I drink because I like being high or intoxicated. | 57.6 | 32.6 | .33*** | 1.00 | |||||
| 3. I drink because it calms me down when I am stressed out. | 76.3 | 24.0 | .30*** | .24*** | 1.00 | ||||
| 4. I drink because I feel abnormal when I don’t drink. | 31.2 | 29.7 | .02 | .19** | .17** | 1.00 | |||
| 5. I drink because I concentrate better when I drink. | 21.2 | 23.4 | .15* | .14* | .25*** | .43*** | 1.00 | ||
| 6. I drink because when I stop, I feel bad (I am nervous, irritable, and I sleep poorly). | 40.6 | 35.4 | -.09 | .19** | .27*** | .61*** | .43*** | 1.00 | |
| 7. I drink solely out of habit. | 67.3 | 27.0 | .11 | -.02 | .10 | .15* | .13* | .05 | 1.00 |
Notes: Items were rated using a visual analog scale ranging from 0 (strongly disagree) to 100 (strongly agree). All values represent raw, unstandardized scores.
p < .05;
p < .01;
p < .001.
Obsessive Compulsive Drinking Scale (OCDS).
The OCDS (Anton et al., 1996; Kranzler et al., 1999) assessed obsessive thoughts about alcohol use and compulsive drinking behaviors in three domains (Roberts et al., 1999): Obsession (frequency and impact of drinking-related thoughts and drives); Interference (degree to which drinking-related thoughts interfere with adaptive functioning); and Resistance/Control Impairment (inability to resist/control drinking-related thoughts) (Cronbach’s α = .78–.82).
Alcohol Dependence Scale (ADS).
The ADS assessed alcohol dependence symptoms (Skinner & Allen, 1982). Previous studies have demonstrated strong psychometric properties in clinical samples (e.g., Allen et al., 1994; Kahler et al., 2003; Skinner & Allen, 1982). A total severity score was computed (α = .85).
Inventory of Drinking Situations-42 (IDS-42).
The IDS-42 (Annis et al., 1987) was developed in adults with alcohol dependence histories to identify circumstances leading to relapse or excessive drinking. Participants rated their frequency of heavy drinking in each situation (1 = never to 4 = always). Scales were computed per Stewart et al. (2000): Positively Reinforcing, Negatively Reinforcing, and Temptation. Only Study 3 participants (n = 93) completed the IDS-42 (α’s: Positively Reinforcing = .91, Negatively Reinforcing = .95, Temptation = .83).
Timeline Followback (TLFB).
The TLFB (Sobell & Sobell, 1996) assessed alcohol use volume (drinks per drinking day, M = 12.71, SD = 6.26) and frequency (percentage of drinking days, M = 85.49, SD = 18.57) over 90 days before study enrollment.
Alcohol treatment history.
The Addiction Severity Index (McLellan et al., 1992) assessed the number of previous episodes of alcohol treatment (range: 0–5) and alcohol detoxification (range: 0–3).
Data analysis
Latent structure analyses.
A combination of principal components analysis (PCA), confirmatory factor analysis (CFA), and internal consistency analysis (Cronbach’s α, average inter-item correlation) was used to evaluate the RHDQ latent structure. First, PCA was performed in a randomly selected sample of half the participants (n = 132) to identify an initial RHDQ factor structure, determined by a variety of indices including Cattell’s scree test (Cattell, 1966), the “eigenvalues greater than 1” rule (Kaiser, 1960), model fit indices, solution interpretability, number of items per factor, and consistency with theoretical predictions. Initial models were subjected to oblique (promax) rotation. Next, a CFA was performed in MPlus. Models were tested in the half of the sample (n = 133) that was not used for the PCA. The two random samples did not differ significantly on any key variables (ps > .05).
Scale assignment, interpretation, and scoring.
Each item was assigned to its primary factor based on its maximum structure coefficient. As a check on the robustness of factor assignments, the process was repeated using the maximum pattern coefficients from the oblique and orthogonal rotation solutions. The content of items assigned to a given factor was used to conceptually define and label the factor. Subscale scores were developed by computing a mean value across all items assigned to a factor.
Associations with alcohol use variables.
Correlations were computed between RHDQ scale scores and other alcohol-related measures to examine concurrent validity and provide preliminary evidence of utility of the newly developed scale. To test whether the strength of correlations with alcohol-related measures significantly differed by RHDQ subscale, Steiger’s z test for overlapping dependent correlations (Hoerger, 2013; Steiger, 1980) was used. This approach accounted for the correlation between the Reinforcement and Normalizing drinking scales (r = .24, p < .001) and is less susceptible than Hotelling’s t test to type I error.
The utility of the RHDQ in accounting for alcohol use patterns was tested against the IDS-42 in the subset of participants from Study 3 (n = 93). Correlations were computed between RHDQ and IDS-42 scales, and a series of hierarchical regressions was performed wherein the RHDQ and IDS-42 scales were entered into separate steps to predict TLFB baseline drinks per drinking day. This analysis addressed whether the IDS-42 scales accounted for a significant increment in the variance of each alcohol use variable after accounting for RHDQ responses in step 1, and vice versa.
Results
Descriptive statistics
Item means, standard deviations, and inter-item correlations were calculated (Table 2). Mean scores ranged from 21.22 (Item 5) to 76.33 (Item 3). Scores for Item 7 were not significantly related to scores for Items 1, 2, 3, or 6 and were modestly correlated with Items 4 and 5.
Principal components analysis results
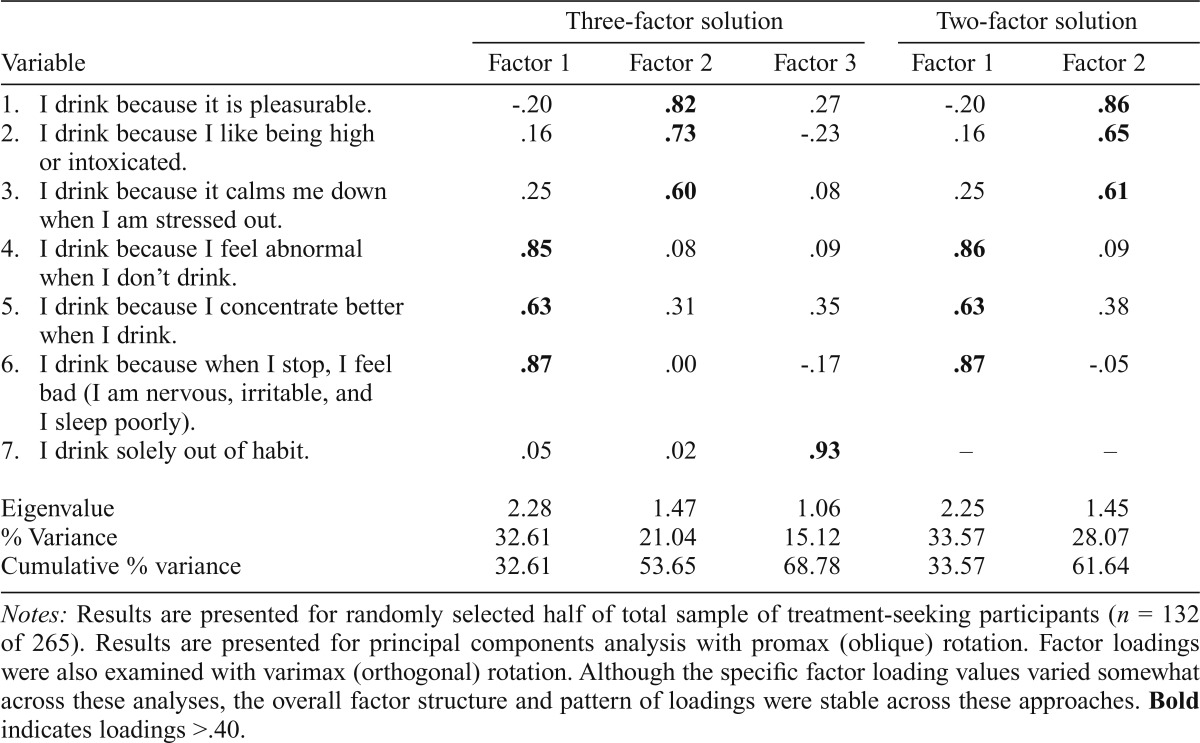
In initial PCA models using promax (oblique) rotation and in which the number of factors was determined by eigenvalues greater than 1, a three-factor solution emerged. Each item was assigned to a primary factor based on the maximum pattern coefficient obtained from the factor solution (Table 3). Based on the content of items loading on each factor, factors were tentatively labeled as (1) Normalizing Drinking, (2) Reinforcement Drinking, and (3) Habitual Drinking. Factor loadings for the rotated solution are presented in Table 3. No items had cross loadings for which factor loadings exceeded a magnitude of .40. The three factors collectively accounted for 68.78% of the overall variance in scores.
Table 3.
Principal components analysis: Factor loadings, Eigenvalues, and explained variance of the Reasons for Heavy Drinking Questionnaire in treatment-seeking alcohol-dependent adults, three- and two-factor models (n = 132)
| Three-factor solution |
Two-factor solution |
||||
| Variable | Factor 1 | Factor 2 | Factor 3 | Factor 1 | Factor 2 |
| 1. I drink because it is pleasurable. | -.20 | .82 | .27 | -.20 | .86 |
| 2. I drink because I like being high or intoxicated. | .16 | .73 | -.23 | .16 | .65 |
| 3. I drink because it calms me down when I am stressed out. | .25 | .60 | .08 | .25 | .61 |
| 4. I drink because I feel abnormal when I don’t drink. | .85 | .08 | .09 | .86 | .09 |
| 5. I drink because I concentrate better when I drink. | .63 | .31 | .35 | .63 | .38 |
| 6. I drink because when I stop, I feel bad (I am nervous, irritable, and I sleep poorly). | .87 | .00 | -.17 | .87 | -.05 |
| 7. I drink solely out of habit. | .05 | .02 | .93 | – | – |
| Eigenvalue | 2.28 | 1.47 | 1.06 | 2.25 | 1.45 |
| % Variance | 32.61 | 21.04 | 15.12 | 33.57 | 28.07 |
| Cumulative % variance | 32.61 | 53.65 | 68.78 | 33.57 | 61.64 |
Notes: Results are presented for randomly selected half of total sample of treatment-seeking participants (n = 132 of 265). Results are presented for principal components analysis with promax (oblique) rotation. Factor loadings were also examined with varimax (orthogonal) rotation. Although the specific factor loading values varied somewhat across these analyses, the overall factor structure and pattern of loadings were stable across these approaches. Bold indicates loadings >.40.
Two-factor models were also tested in which Item 7 was either included or omitted, given its loading on a single-item factor in the PCA. When Item 7 was included, Items 1 through 6 demonstrated comparable loadings to the baseline model, and Item 7 demonstrated weak loadings on both F1 and F2 (factor loadings, F1 = .23, F2 = .29). When Item 7 was removed, the solution (F1: Items 4, 5, 6; F2: Items 1, 2, 3) accounted for a cumulative 61.64% of variance in scores.
Confirmatory factor analysis results
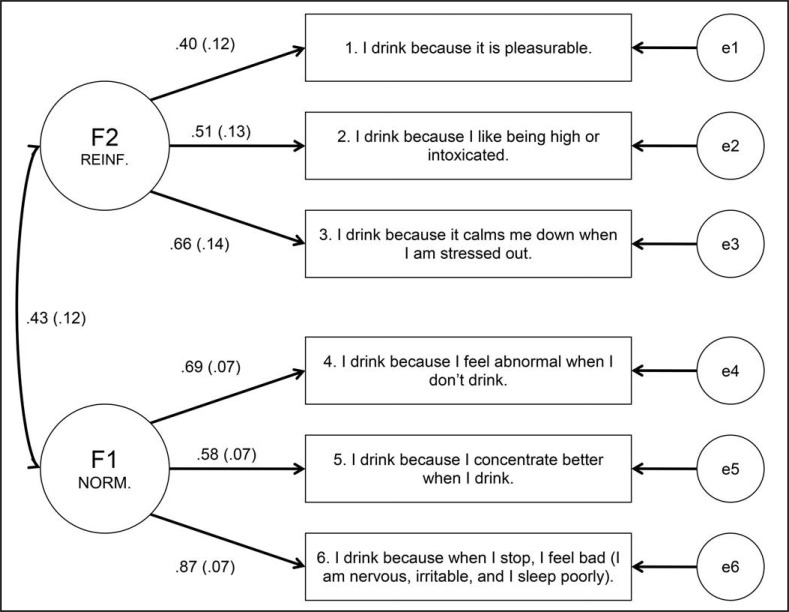
Per the PCA results, a three-factor baseline CFA model (F1: Items 4, 5, 6; F2: Items 1, 2, 3; F3: Item 7) was specified, where the single-item F3 loading was constrained to 1 and the variance to 0. Next, a two-factor model where Item 7 was omitted (F1: Items 4, 5, 6; F2: Items 1, 2, 3) was evaluated. Inclusion of Item 7 did not significantly improve model fit in any configuration. The six-item two-factor solution provided the best balance of fit and parsimony (Figure 1).
Figure 1.
Confirmatory factor analysis final model: Two-factor structure of the Reasons for Heavy Drinking Questionnaire for second half of sample (n = 133) (i.e., participants not selected for principal components analysis). REINF. = reinforcement; NORM. = normalizing. Standardized coefficients are shown with standard errors in parentheses. All values are significant at p < .05. Model fit indices: χ2(14) = 26.51, p = .022; root mean square error of approximation = .082, 90% CI [.03, .13], p = .02; comparative fit index = .926; standardized root mean square residual = .064.
Scale computation
Estimated scale scores were computed by averaging scores for items assigned to each scale (i.e., Reinforcement = 1, 2, 3; Normalizing = 4, 5, 6). Mean scores were 70.01 (SD = 19.95) for Reinforcement and 30.98 (SD = 24.18) for Normalizing. Cronbach’s α was .54 for Reinforcement and .74 for Normalizing. Average inter-item correlations were .29 for Reinforcement and .49 for Normalizing.
Associations with alcohol-related outcomes
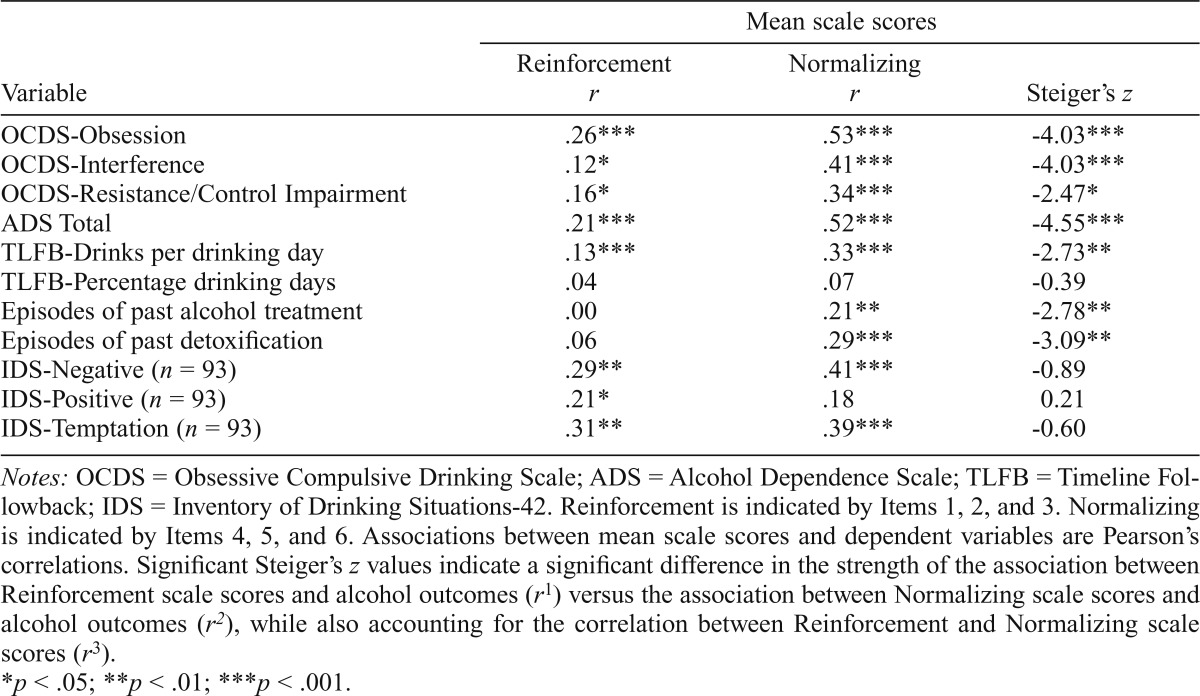
Correlations between RHDQ factors/scales and drinking-related outcomes are summarized in Table 4. Reinforcement scores demonstrated weak to moderate associations with OCDS scores, whereas Normalizing scores demonstrated moderate to strong associations. A similar pattern was observed for ADS scores. Neither scale was significantly correlated with TLFB percentage drinking days. Both scales were positively associated with TLFB drinks per drinking day. Normalizing—but not Reinforcement—was significantly related to history of alcohol treatment, including past detoxifications. For all significant correlations, Steiger’s z tests revealed that Normalizing scores were more strongly correlated with other alcohol-related variables than Reinforcement scores. Responses to Item 7 from the original item pool were weakly and positively correlated with OCDS-Obsession (r = .13, p < .05) and OCDS-Resistance/Control Impairment (r = .16, p < .05) scores but not with any other drinking-related outcome variables measured here.
Table 4.
Associations between Reasons for Heavy Drinking Questionnaire scales and measures of craving, alcohol dependence severity, and drinking behavior (N = 265)
| Variable | Mean scale scores |
||
| Reinforcement r | Normalizing r | Steiger’s z | |
| OCDS-Obsession | .26*** | .53*** | -4.03*** |
| OCDS-Interference | .12* | .41*** | -4.03*** |
| OCDS-Resistance/Control Impairment | .16* | .34*** | -2.47* |
| ADS Total | .21*** | .52*** | -4.55*** |
| TLFB-Drinks per drinking day | .13*** | .33*** | -2.73** |
| TLFB-Percentage drinking days | .04 | .07 | -0.39 |
| Episodes of past alcohol treatment | .00 | .21** | -2.78** |
| Episodes of past detoxification | .06 | .29*** | -3.09** |
| IDS-Negative (n = 93) | .29** | .41*** | -0.89 |
| IDS-Positive (n = 93) | .21* | .18 | 0.21 |
| IDS-Temptation (n = 93) | .31** | .39*** | -0.60 |
Notes: OCDS = Obsessive Compulsive Drinking Scale; ADS = Alcohol Dependence Scale; TLFB = Timeline Followback; IDS = Inventory of Drinking Situations-42. Reinforcement is indicated by Items 1, 2, and 3. Normalizing is indicated by Items 4, 5, and 6. Associations between mean scale scores and dependent variables are Pearson’s correlations. Significant Steiger’s z values indicate a significant difference in the strength of the association between Reinforcement scale scores and alcohol outcomes (r1) versus the association between Normalizing scale scores and alcohol outcomes (r2), while also accounting for the correlation between Reinforcement and Normalizing scale scores (r3).
p < .05;
p < .01;
p < .001.
The utility of the RHDQ versus the IDS-42 in accounting for drinking outcomes was examined. There was no significant difference in the relation between RHDQ and IDS-42 scores for any combination of scales, per Steiger’s z tests. RHDQ-Reinforcement—but not RHDQ-Normalizing—was significantly related to IDS-Positive Reinforcement (r = .21, p < .05). Both RHDQ scales were positively and significantly related to IDS-Negatively Reinforcing and IDS-Temptation (Table 4). In accounting for drinking outcomes, hierarchical regressions revealed that, when the RHDQ was entered in the first step of the model, the IDS-42 did not account for a significant increase in variance in TLFB drinks per drinking day (Step 1 R2 = .26; R2 change = .04, p = .17) beyond the RHDQ. When the order was reversed and IDS scores were entered in the first step, RHDQ scores accounted for a significant increase in variance in TLFB drinks per drinking day (Step 1 R2 = .18; R2 change = .12, p < .001) beyond the IDS.
Discussion
This study reported the latent structure and preliminary validity of a brief, novel self-report measure of reasons for drinking alcohol to excess in treatment-seeking, alcohol-dependent adults. Results generally supported two RHDQ factors. High scores on the Reinforcement factor indicated a tendency to endorse both hedonic (positive reinforcement) and stress relief (negative reinforcement) heavy drinking motives. High scores on the Normalizing factor reflected a predisposition toward consuming alcohol to “feel normal,” or to avoid negative physiological consequences associated with alcohol dependence and withdrawal and to reinstate homeostasis. This structure parallels prominent conceptualizations of motivational pathways underpinning problematic alcohol use (Wise & Koob, 2014). A third potential factor (habit) appeared conceptually orthogonal to the other two factors. One-item factors are prone to instability and the phrasing (i.e., use of the qualifier “solely”) may have affected endorsement and covariance patterns, but the nature and utility of measuring “habitual drinking” need further exploration.
The two RHDQ factors also correspond to factors and scales identified in prior literature. Mo et al. (2013) described development and validation of a brief, six-item version of the Desires for Alcohol Questionnaire (DAQ-6), which assesses alcohol craving. A two-factor structure (1: negative reinforcement expectancies, 2: strong desires and intentions) was observed among adults participating in residential treatment. Although RHDQ item content differed somewhat from DAQ-6, both measures include one scale that includes reasons for drinking commonly endorsed in the general population that can lead to problematic use (i.e., RHDQ-Reinforcement and DAQ-6 Coping) and a scale on which high scores likely reflect more pathological reasons for drinking (i.e., RHDQ-Normalizing and DAQ-6 Urges). Because the RHDQ and DAQ-6 were initially validated in clinical samples of alcohol-dependent adults and appear promising for use in clinical research contexts, future studies should compare their utility in longitudinal trials.
Supporting the concurrent validity of the RHDQ, scores on both RHDQ scales were positively correlated with most other measures of alcohol-related cognitions, alcohol dependence, intensity of alcohol use, and past alcohol treatment. Compared with Reinforcement scores, Normalizing scores consistently demonstrated stronger correlations with more severe or chronic alcohol use indices. Because the Normalizing scale items were created to reflect dysregulated physiology associated with chronic alcohol use, this finding is not surprising. This result is consistent with the allostatic model (Koob, 2003), although the strong endorsement of Reinforcement items also implies that, as a group, moderately severe, treatment-seeking people retain hedonic reasons for drinking despite their need to normalize certain phenomena by drinking. These findings suggest that the allostatic model may exist along a continuum.
The lack of significant correlation between RHDQ scales and baseline alcohol use frequency may have been attributable to a restricted (high) range in alcohol use frequency. Participants were seeking treatment and met criteria for alcohol dependence. In the 90 days before their study participation, nearly 60% of participants reported consuming alcohol on at least 90% of days, and over 90% of participants reported consuming alcohol on more than 50% of days. An association between RHDQ scales and drinking frequency may be observable later in treatment (i.e., when some participants reduce alcohol use frequency, increasing the range), or among non–treatment-seeking individuals with less heavy drinking.
The multidimensional nature of the measure reflects putative neurobiological pathways to alcohol use disorder. The identified factors and corresponding scales may be useful in assessing the efficacy of pharmacological interventions designed to target these distinct pathways. For instance, the opioid antagonist naltrexone diminishes the hedonic or reinforcing value of alcohol (O’Malley et al., 2002), likely via dopamine and opioid mechanisms (Anton, 2008). The RHDQ-Reinforcement scale may be most sensitive to the effects of naltrexone and similar drugs. Alternatively, gabapentin and topiramate are believed to regulate gamma–aminobutyric acid/glutamate imbalances often associated with alcohol withdrawal and reinstate allostasis, among other effects (Johnson, 2004; Roberto et al., 2008). The RHDQ-Normalizing scale may be particularly sensitive to these medications but not to medications that target alcohol’s reinforcing effects. The RHDQ could thus be useful in detecting the therapeutic effects of specific pharmacological and behavioral interventions tailored to individuals who drink for particular reasons.
Although the primary contribution of the RHDQ is its coverage of new content compared with other motives questionnaires, its brevity confers low burden and heightened utility in clinical and longitudinal research. When pitted against the IDS-42, the RHDQ accounted for a significant increment in variance in drinks per drinking day. Thus, despite being brief, the RHDQ may perform at least as well as some longer scales in accounting for patterns of alcohol use.
Limitations and future directions
The use of cross-sectional data from baseline assessments obviates conclusions regarding stability, sensitivity to change over time, or prediction of intervention response. Future studies should use prospective longitudinal designs with repeated administration of the RHDQ. A different strategy of scale construction may have resulted in different items and performance characteristics, including greater stability for the Reinforcement scale. The sample included only treatment-seeking adults enrolled in clinical trials of pharmacotherapies for alcohol dependence, and the different studies from which the current sample was drawn had slightly different inclusion/exclusion criteria. Therefore, the factor structure, validity, and utility of the RHDQ in different settings or populations—including people with a fuller range of drinking profiles or comorbidities or at different stages in the development of alcohol use disorder—are unknown. Despite these limitations, the RHDQ is a promising tool for briefly measuring important reasons for heavy alcohol use, particularly in clinical trials.
Acknowledgments
Drs. Pat Latham, Konstantin Voronin, and Alicia Baros coordinated data collection and assisted in subject assessment and data management. The RHDQ content is copyright protected, and permission for use should be sought from the corresponding author or his designate.
Footnotes
This research was supported by National Institute on Alcohol Abuse and Alcoholism Grants K05 AA017435, R01 AA017633, R01 AA009568, and R21 AA017525 (to Raymond F. Anton, principal investigator); P50 AA010761-16 (to Howard C. Becker, principal investigator); K99AA021419 (to Joseph P. Schacht, principal investigator); National Institute of Mental Health Grant T32 MH18869-26 (to Dean G. Kilpatrick & Carla Kmett Danielson, principal investigators); and National Institute on Drug Abuse Grant K23 DA038257 (to Zachary W. Adams, principal investigator). Raymond F. Anton, M.D., holds a copyright on the content of the Reasons for Heavy Drinking Questionnaire.
References
- Allen J. P., Fertig J. B., Towle L. H., Altshuler V. B., Vrublevsky A. G., Valentik Y. V., Zanis D. A. Psychometric analyses of the Alcohol Dependence Scale among United States and Russian clinical samples. International Journal of the Addictions. 1994;29:71–87. doi: 10.3109/10826089409047369. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Annis H., Davis C. S., Graham J. M. Inventory of Drinking Situations (IDS) user’s guide. Toronto, Ontario: Addiction Research Foundation of Ontario; 1987. [Google Scholar]
- Anton R. F. Naltrexone for the management of alcohol dependence. The New England Journal of Medicine. 2008;359:715–721. doi: 10.1056/NEJMct0801733. doi:10.1056/NEJMct0801733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anton R. F., Moak D. H., Latham P. K. The obsessive compulsive drinking scale: A new method of assessing outcome in alcoholism treatment studies. Archives of General Psychiatry. 1996;53:225–231. doi: 10.1001/archpsyc.1996.01830030047008. doi:10.1001/archpsyc.1996.01830030047008. [DOI] [PubMed] [Google Scholar]
- Anton R. F., Myrick H., Wright T. M., Latham P. K., Baros A. M., Waid L. R., Randall P. K. Gabapentin combined with naltrexone for the treatment of alcohol dependence. American Journal of Psychiatry. 2011;168:709–717. doi: 10.1176/appi.ajp.2011.10101436. doi:10.1176/aapi.ajp.2011.10101436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter K. M., Hasin D. S. Drinking to cope with negative affect and DSM-IV alcohol use disorders: A test of three alternative explanations. Journal of Studies on Alcohol. 1999;60:694–704. doi: 10.15288/jsa.1999.60.694. doi:10.15288/jsa.1999.60.694. [DOI] [PubMed] [Google Scholar]
- Cattell R. B. The scree test for the number of factors. Multivariate Behavioral Research. 1966;1:245–276. doi: 10.1207/s15327906mbr0102_10. doi:10.1207/s15327906mbr0102_10. [DOI] [PubMed] [Google Scholar]
- Cooper M. L. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment. 1994;6:117–128. doi:10.1037/1040-3590.6.2.117. [Google Scholar]
- Cooper M. L., Frone M. R., Russell M., Mudar P. Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology. 1995;69:990–1005. doi: 10.1037//0022-3514.69.5.990. doi:10.1037/0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- DeMartini K. S., Carey K. B. The role of anxiety sensitivity and drinking motives in predicting alcohol use: A critical review. Clinical Psychology Review. 2011;31:169–177. doi: 10.1016/j.cpr.2010.10.001. doi:10.1016/j.cpr.2010.10.001. [DOI] [PubMed] [Google Scholar]
- First M. B., Gibbon M., Spitzer R. L., Williams J. B. W. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version. New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Heinz A., Löber S., Georgi A., Wrase J., Hermann D., Rey E.-R., Mann K. Reward craving and withdrawal relief craving: Assessment of different motivational pathways to alcohol intake. Alcohol and Alcoholism. 2003;38:35–39. doi: 10.1093/alcalc/agg005. doi:10.1093/alcalc/agg005. [DOI] [PubMed] [Google Scholar]
- Hoerger M. ZH: An updated version of Steiger’s Z and web-based calculator for testing the statistical significance of the difference between dependent correlations. 2013 Retrieved from www.psychmike.com/dependent_correlations.php.
- Johnson B. A. Progress in the development of topiramate for treating alcohol dependence: From a hypothesis to a proof-of-concept study. Alcoholism: Clinical and Experimental Research. 2004;28:1137–1144. doi: 10.1097/01.alc.0000134533.96915.08. doi:10.1097/01.ALC.0000134533.96915.08. [DOI] [PubMed] [Google Scholar]
- Kahler C. W., Strong D. R., Hayaki J., Ramsey S. E., Brown R. A. An item response analysis of the Alcohol Dependence Scale in treatment-seeking alcoholics. Journal of Studies on Alcohol. 2003;64:127–136. doi: 10.15288/jsa.2003.64.127. doi:10.15288/jsa.2003.64.127. [DOI] [PubMed] [Google Scholar]
- Kaiser H. F. The application of electronic computers to factor analysis. Educational and Psychological Measurement. 1960;20:141–151. doi:10.1177/001316446002000116. [Google Scholar]
- Koob G. F. Alcoholism: Allostasis and beyond. Alcoholism: Clinical and Experimental Research. 2003;27:232–243. doi: 10.1097/01.ALC.0000057122.36127.C2. doi:10.1097/01.ALC.0000057122.36127.C2. [DOI] [PubMed] [Google Scholar]
- Kranzler H. R., Mulgrew C. L., Modesto-Lowe V., Burleson J. A. Validity of the Obsessive Compulsive Drinking Scale (OCDS): Does craving predict drinking behavior? Alcoholism: Clinical and Experimental Research. 1999;23:108–114. doi:10.1111/j.1530-0277.1999.tb04030.x. [PubMed] [Google Scholar]
- Kristjansson S. D., Agrawal A., Littlefield A. K., Pergadia M. L., Lessov-Schlaggar C. N., Sartor C. E., Heath A. C. Drinking motives in female smokers: Factor structure, alcohol dependence, and genetic influences. Alcoholism: Clinical and Experimental Research. 2011;35:345–354. doi: 10.1111/j.1530-0277.2010.01350.x. doi:10.1111/j.1530-0277.2010.01350.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuntsche E., Knibbe R., Gmel G., Engels R. Who drinks and why? A review of socio-demographic, personality, and contextual issues behind the drinking motives in young people. Addictive Behaviors. 2006;31:1844–1857. doi: 10.1016/j.addbeh.2005.12.028. doi:10.1016/j.addbeh.2005.12.028. [DOI] [PubMed] [Google Scholar]
- Malcolm R., Herron J. E., Anton R. F., Roberts J., Moore J. Recurrent detoxification may elevate alcohol craving as measured by the Obsessive Compulsive Drinking scale. Alcohol. 2000;20:181–185. doi: 10.1016/s0741-8329(99)00073-7. doi:10.1016/S0741-8329(99)00073-7. [DOI] [PubMed] [Google Scholar]
- McLellan A. T., Kushner H., Metzger D., Peters R., Smith I., Grissom G., Argeriou M. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. doi:10.1016/0740-5472(92)90062-S. [DOI] [PubMed] [Google Scholar]
- Merrill J. E., Read J. P. Motivational pathways to unique types of alcohol consequences. Psychology of Addictive Behaviors. 2010;24:705–711. doi: 10.1037/a0020135. doi:10.1037/a0020135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezquita L., Stewart S. H., Ibanez M. I., Ruiperez M. A., Villa H., Moya J., Ortet G. Drinking motives in clinical and general populations. European Addiction Research. 2011;17:250–261. doi: 10.1159/000328510. doi:10.1159/000328510. [DOI] [PubMed] [Google Scholar]
- Mo C., Deane F. P., Lyons G. C. B., Kelly P. J. Factor analysis and validity of a short six-item version of the Desires for Alcohol Questionnaire. Journal of Substance Abuse Treatment. 2013;44:557–564. doi: 10.1016/j.jsat.2012.12.002. doi:10.1016/j.jsat.2012.12.002. [DOI] [PubMed] [Google Scholar]
- O’Malley S. S., Krishnan-Sarin S., Farren C., Sinha R., Kreek M. J. Naltrexone decreases craving and alcohol self-administration in alcohol-dependent subjects and activates the hypothalamo-pituitaryadrenocortical axis. Psychopharmacology. 2002;160:19–29. doi: 10.1007/s002130100919. doi:10.1007/s002130100919. [DOI] [PubMed] [Google Scholar]
- Roberto M., Gilpin N. W., O’Dell L. E., Cruz M. T., Morse A. C., Siggins G. R., Koob G. F. Cellular and behavioral interactions of gabapentin with alcohol dependence. Journal of Neuroscience. 2008;28:5762–5771. doi: 10.1523/JNEUROSCI.0575-08.2008. doi:10.1523/JNEUROSCI.0575-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts J. S., Anton R. F., Latham P. K., Moak D. H. Factor structure and predictive validity of the Obsessive Compulsive Drinking Scale. Alcoholism: Clinical and Experimental Research. 1999;23:1484–1491. doi:10.1111/j.1530-0277.1999.tb04671.x. [PubMed] [Google Scholar]
- Skinner H. A., Allen B. A. Alcohol dependence syndrome: Measurement and validation. Journal of Abnormal Psychology. 1982;91:199–209. doi: 10.1037//0021-843x.91.3.199. doi:10.1037/0021-843X.91.3.199. [DOI] [PubMed] [Google Scholar]
- Sobell L. C., Sobell M. B. Timeline followback user’s guide: A calendar method for assessing alcohol and drug use. Toronto, Ontario: Addiction Research Foundation; 1996. [Google Scholar]
- Steiger J. H. Tests for comparing elements of a correlation matrix. Psychological Bulletin. 1980;87:245–251. doi:10.1037/0033-2909.87.2.245. [Google Scholar]
- Stewart S. H., Samoluk S. B., Conrod P. J., Pihl R. O., Dongier M. Psychometric evaluation of the short form inventory of drinking situations (IDS-42) in a community-recruited sample of substanceabusing women. Journal of Substance Abuse. 2000;11:305–321. doi: 10.1016/s0899-3289(00)00029-8. doi:10.1016/S0899-3289(00)00029-8. [DOI] [PubMed] [Google Scholar]
- Thomas S. E., Randall C. L., Carrigan M. H. Drinking to cope in socially anxious individuals: A controlled study. Alcoholism: Clinical and Experimental Research. 2003;27:1937–1943. doi: 10.1097/01.ALC.0000100942.30743.8C. doi:10.1097/01.ALC.0000100942.30743.8C. [DOI] [PubMed] [Google Scholar]
- Vollstädt-Klein S., Wichert S., Rabinstein J., Bühler M., Klein O., Ende G., Mann K. Initial, habitual and compulsive alcohol use is characterized by a shift of cue processing from ventral to dorsal striatum. Addiction. 2010;105:1741–1749. doi: 10.1111/j.1360-0443.2010.03022.x. doi:10.1111/j.1360-0443.2010.03022.x. [DOI] [PubMed] [Google Scholar]
- Wise R. A., Koob G. F. The development and maintenance of drug addiction. Neuropsychopharmacology. 2014;39:254–262. doi: 10.1038/npp.2013.261. doi:10.1038/npp.2013.261. [DOI] [PMC free article] [PubMed] [Google Scholar]