Abstract
Background
Medication nonadherence is an important obstacle to cardiovascular disease management.
Objective
To improve adherence through real-time feedback based on theories of how social forces influence behavior.
Design
Two randomized controlled pilot trials called PROMOTE and SUPPORT. Participants stored statin medication in wireless-enabled pill bottles that transmitted adherence data to researchers.
Participants
Adults with diabetes and a history of low statin adherence based on pharmacy refills (i.e., Medication Possession Ratio [MPR] <80 % in the pre-randomization screening period).
Intervention
In PROMOTE, each participant was randomized to 1) weekly messages in which that participant’s statin adherence was compared to that of other participants (comparison), 2) weekly summaries of that participant’s statin adherence (summary), or 3) control. In SUPPORT, each participant identified another person (the Medication Adherence Partner [MAP]) to receive reports about that participant’s adherence, and was randomized to 1) daily reports to MAP, 2) weekly reports to MAP, 3) reports to MAP only if dose was missed, or 4) control.
Main Outcomes Measure
Adherence measured by pill bottle.
Key Results
Among 45,000 health plan members contacted by mail, <1 % joined the trial. Participants had low baseline MPRs (median = 60 %, IQR 41–72 %) but high pill-bottle adherence (90 % in PROMOTE, 92 % in SUPPORT) during the trial. In PROMOTE (n = 201) and SUPPORT (n = 200), no intervention demonstrated significantly better adherence vs. control. In a subgroup of PROMOTE participants with the lowest pre-study MPR, pill-bottle-measured adherence in the comparison arm (89 %) was higher than the control (86 %) and summary (76 %) arms, but differences were non-significant (p = 0.10).
Conclusions
Interventions based on social forces did not improve medication adherence vs. control over a 3-month period. Given the low percentage of invited individuals who enrolled, the studies may have attracted participants who required little encouragement to improve adherence other than study participation.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-015-3540-y) contains supplementary material, which is available to authorized users.
KEY WORDS: medication adherence, statins, social support, social force, interventions
BACKGROUND
There is growing evidence of strong associations between a patient’s social environment and health behavior.1 However, existing knowledge of how social forces can be used to promote better health behaviors is limited. Harnessing social forces could be an effective approach for promoting health behaviors, because patients typically only engage with their physicians and nurses during occasional health system visits a few hours a year, but they interact with their social networks much more frequently. Furthermore, social forces may be particularly effective at building enduring habits for healthy behavior and might be cost-effective to implement.
Social pressure—i.e., encouragement or discouragement from others to take a particular action—is a powerful social force that can influence individual behavior.2–4 An individual can experience social pressure when another person in his or her social network directly encourages an action or when the individual is aware that another person is observing, or will observe, that individual’s action.5 Within the context of medication adherence, if a patient’s adherence will be reported to another person (a Medication Adherence Partner, or MAP, a term created for this study), the patient may become more likely to adhere because the MAP explicitly encourages him to take his medication or because the patient anticipates that the MAP will chastise or encourage him upon learning of poor adherence. However, the optimal strategy for involving a MAP or providing feedback to a MAP is unknown. It is plausible that daily feedback about adherence would be most effective, since it provides information at the highest frequency.6 On the other hand, frequent feedback might also lead to “alert fatigue” and cause the MAP to neglect messages.7
Providing individuals with information about what others are doing can be an effective motivator, particularly for poor performers who learn that they are below average on a desired action such as taking one’s medication.8–11 An individual may feel compelled to improve medication adherence or other health behaviors when compared to the performance of “peers.”12 However, that feedback about relative performance could also discourage individuals who do not feel capable of improving their behavior. Additionally, there are minimal data about how this kind of feedback might affect health behaviors specifically.
Cardiovascular disease (CVD) is the leading cause of death in the United States. CVD risk can be significantly reduced by treating dyslipidemia. HMG-CoA reductase inhibitors, also known as statins, have reduced cholesterol levels and lowered mortality from CVD in multiple clinical trials.13,14 The majority of patients with CVD or diseases with equivalent cardiovascular risk, such as diabetes, require a statin to achieve the cholesterol targets in clinical practice guidelines.15 Despite the substantial benefits and reasonable risks associated with statins,16 adherence is strikingly poor.17–19 For example, one year after hospitalization for an acute coronary syndrome, nearly half of patients prescribed statins stop taking them.20 Reducing CVD-related morbidity, mortality, and healthcare costs will depend to a great degree on effective strategies to help patients improve medication adherence and other health behaviors.21
We conducted two pilot trials in a population at high risk for CVD. These trials aimed to improve pill-bottle-measured adherence through real-time feedback based on theories of how social forces influence behavior. For the promoting health through comparison (PROMOTE) study, the primary aim was to determine the efficacy of adherence feedback to the participant, in which the participant’s adherence was compared to that participants. For the social support (SUPPORT) study, the primary aim was to compare the efficacy of adherence feedback provided to a MAP at different frequencies.
METHODS
Overview
This study comprised two randomized controlled pilot trials in which participants were recruited from a population of patients enrolled in healthcare plans administered by Humana, a large US provider of health insurance and health services. After informed consent, participants were provided with a wireless electronic pill bottle (Vitality GlowCap; manufactured by Vitality Inc., Los Angeles, CA) that monitored their adherence to their statin medication.
Participants
All participants were Humana members with diabetes of any type, on a once-a-day statin regimen, and with poor statin adherence based on pharmacy refill claims data (i.e. Medication Possession Ratio [MPR] <80 % in the recent 12-month pre-randomization screening period). Eligible individuals were ≥18 years of age at enrollment, spoke English, reported no major statin side effects, and did not have liver disease. Participants needed regular access to a computer to receive study communications via email; this access could be through a friend or library. For the SUPPORT study, each participant also had to identify a MAP who would receive their adherence information via email during the intervention period. Prior to enrollment, the MAP had to agree to receive study related communications.
Design
Potentially eligible participants were identified by Humana through review of the pharmacy claim database, and were then mailed one study invitation letter directly from Humana. Invitation letters described the study, including compensation for participation, and directed potential participants to the study’s website. The two trials were conducted simultaneously; each potentially eligible participant was invited to join either SUPPORT or PROMOTE. No participant received an invitation to join both studies or to choose between studies. The studies were conducted by the same investigators and staff.
The study website was hosted on Way to Health, an internet research platform based at the University of Pennsylvania that uses online tools, wireless technologies, and other applications to allow investigators to test ways of improving health. On the platform (see Online Appendices 1–3), individuals created a personal account (for study communications), completed further eligibility screening, and provided informed consent. Contact information for the study coordinator was provided. Eligible participants were mailed a GlowCap pill bottle with instructions. Upon successfully activating the pill bottle and a data feed to Way to Health, participants underwent random assignment to study arms.
Electronic Pill Bottle
The GlowCap device resembles a standard pill bottle. The GlowCap was sent as a kit with two parts: 1) a pill bottle with a top capable of sending a wireless timestamp whenever it is removed, and 2) a plug-in gateway that transmits this information via a cellular network to the GlowCap’s manufacturer and ultimately to the Way to Health platform. An Internet connection is not necessary. No cost is passed to the participant. Participants were instructed to pour their statin pills into the GlowCap bottle. The cap cannot be used with other pill bottles.
Interventions
PROMOTE participants were randomized to one of three arms. Each Arm 1 (comparison) participant received weekly email messages comparing the individual’s statin adherence to that of other participants and specifying whether adherence was above or below the average, along with a message of encouragement tailored to his or her ranking (Online Appendix 1). Each Arm 2 (summary) participant received an email summary of his or her adherence from the previous week. Arm 3 (control) participants did not receive emails about adherence.
For the SUPPORT study, participants were randomized to one of four arms. In Arm 1 (daily), each MAP received a daily email specifying whether the participant had taken the statin. In Arm 2 (weekly), each MAP received a weekly email summary of the participant’s adherence the previous week. In Arm 3 (missed dose), each MAP received an email notification only if the participant’s dose on the previous day was missed. In Arm 4 (control), the MAP received no adherence emails. Online Appendix 2 shows these messages.
All participants could view their pill-bottle adherence in a color-coded calendar displayed on their Way to Health account (Online Appendix 3).
Outcomes and Measurement
The primary outcome was adherence measured by the wireless pill bottle, calculated as the percentage of days with a bottle opening. A secondary outcome was self-reported adherence measured using the Morisky Medication Adherence Scale (MMAS), a validated 8-item self-reported adherence questionnaire.22–24 The MMAS was administered at enrollment and end of study. At enrollment, participants also completed the Zimet Multidimensional Scale of Perceived Social Support.25,26 Participants also recorded age, sex, race, Hispanic ethnicity, education level, and body mass index. We obtained the number of medications from pharmacy claims. Participants in the SUPPORT trial specified their relationship with the MAPs from a list, collapsed to four categories (Intimate Partners, Children, Other Relatives, and Friends).
Statistical Analyses
We estimated power using preliminary adherence data from studies in other population groups by conducting simulations (using Stata software) that assumed normally distributed adherence rates and assessing pairwise comparison across arms with Bonferroni correction. Based on these estimates, the trials were designed with > 80 % power to detect a 10-percentage-point difference in adherence between any two study arms in each study, using a Bonferroni-adjusted two-sided type 1 error rate to adjust for the main hypothesis tests comparing each intervention arm to control. We inflated the sample size by 20 % to account for potential participant drop-out.
We conducted analyses using SAS (version 9.3, 2011) with a two-sided p value <0.05 as the criterion for statistical significance. Medians are reported with the (25th, 75th) percentiles (interquartile range, IQR). We used the Kruskal–Wallis test to compare continuous variables and chi-square tests to compare categorical variables across intervention arms.
We estimated daily odds of GlowCap adherence using generalized estimation equation (GEE) models that produced robust standard errors by assuming a correlation structure for repeated measurement (per patient), while adjusting for time (weeks) and study arm as fixed effects. Using calculated Morisky scores from baseline survey data, we grouped study participants into high, medium, and low levels of baseline medication adherence, and tested whether intervention effects on average daily adherence differed for patients with different levels of baseline adherence, by adding interaction terms between arm and baseline adherence levels, and alternatively, by conducting subgroup analysis for patients with low, medium, or high adherence.
We also fit generalized linear models to test whether changes in Morisky scores from baseline to end of intervention varied by arm.
RESULTS
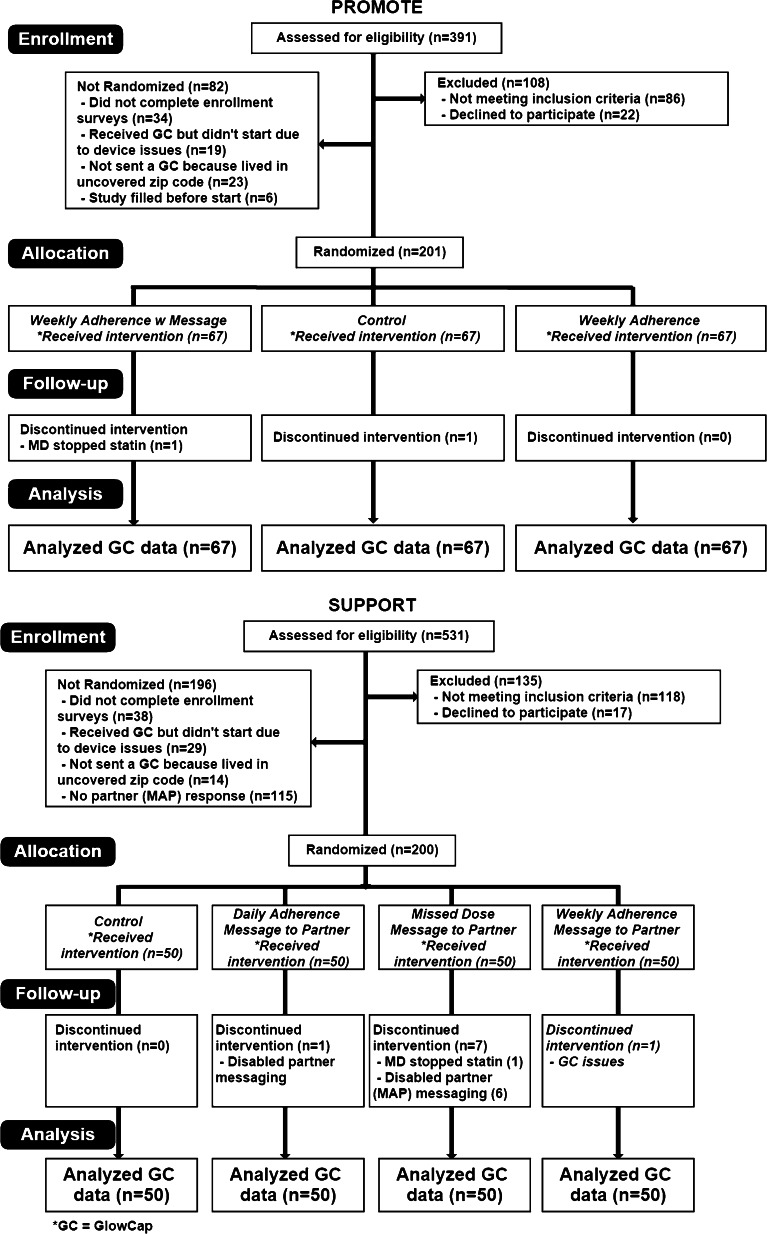
A total of 45,000 Humana members identified as eligible for the study received invitation letters (n = 17,500 to PROMOTE and n = 27,500 to SUPPORT). A total of 201 enrolled in the PROMOTE trial and 200 enrolled in the SUPPORT trial (Fig. 1). Median MPR for statin use for the 401 participants during the screening pre-enrollment period was 60 % (IQR 41–72 %; mean 58 %, SD 25 %).
Fig. 1.
Consort diagrams, by study.
Operations
No adverse events were reported. The median number of times that participants accessed their Way to Health accounts was 5 (IQR 3, 10). In the SUPPORT trial, seven (5 %) participants experienced GlowCap malfunctions, which led to incorrect messages to the MAPs that specified missed doses of statins. MAP messaging was disabled at the request of these participants.
Baseline Characteristics
The two studies had similar demographics. In the PROMOTE study (Table 1), the median age was 70 years, 57 % were men, 86 % were white, and 80 % had Medicare. About 30 % had a high school degree or less. In the SUPPORT study (Table 2), the median age was 68 years, 50 % were men, 87 % were white, and 78 % had Medicare. In the SUPPORT study, 61 % of MAPs were intimate partners of participants, while 24 % were children (adults over 18 years), 7 % were other relatives, and 8 % were friends (Table 3).
Table 1.
PROMOTE Participant Characteristics, Overall and by Study (N = 201)
| Arms | |||||
|---|---|---|---|---|---|
| Variables | Total (N = 201) | Comparison (n = 67) | Summary (n = 67) | Control (n = 67) | P value* |
| Median Age (IQR) | 70 (62, 73) | 70 (61, 75) | 70 (63, 73) | 69 (61, 73) | 0.71 (K) |
| Mean Age (SD) | 67 (10) | 68 (10) | 67 (11) | 67 (10) | |
| Male (%) | 114 (57) | 42 (63) | 33 (49) | 39 (58) | 0.28 (P) |
| Median BMI (IQR) | 30 (27, 36) | 31 (29, 36) | 30 (26, 35) | 31 (27, 36) | 0.14 (K) |
| Race (%) | 0.35 (P) | ||||
| American Indian | 1 (1) | 1 (1) | 0 | 0 | |
| Asian | 5 (2) | 1 (1) | 3 (4) | 1 (1) | |
| Black | 18 (9) | 8 (12) | 8 (12) | 2 (3) | |
| Hawaiian or Other Pacific Islander | 0 | 0 | 0 | 0 | |
| White | 173 (86) | 56 (84) | 54 (81) | 63 (94) | |
| Other/Multiracial | 4 (2) | 1 (1) | 2 (3) | 1 (1) | |
| Hispanic ethnicity | 8 (4) | 4 (6) | 2 (3) | 2 (3) | 0.59 (P) |
| Insurance type ** | 0.05 (P) | ||||
| Private | 34 (17) | 4 (6) | 16 (24) | 14 (21) | |
| Medicare | 161 (80) | 59 (88) | 50 (75) | 52 (78) | |
| Medicaid | 4 (2) | 3 (4) | 0 | 1 (1) | |
| Self-Insured | 1 (1) | 0 | 1 (1) | 0 | |
| Uninsured | 1 (1) | 1 (1) | 0 | 0 | |
| Frequently fill statin medication without using Humana | 33 (16) | 13 (19) | 12 (18) | 8 (12) | 0.47 (P) |
| Diabetes type | 0.53 (P) | ||||
| Type 1 | 12 (6) | 4 (6) | 4 (6) | 4 (6) | |
| Type 2 | 182 (91) | 62 (93) | 62 (93) | 58 (88) | |
| Other/Unknown | 6 (3) | 1(1) | 1(1) | 4 (6) | |
| Missing | 1 | 0 | 0 | 1 | |
| Highest level of education | 0.984 (P) | ||||
| Less than High School | 10 (5) | 3 (4) | 3 (5) | 4 (6) | |
| GED | 9 (4) | 4 (6) | 3 (4) | 2 (3) | |
| High School Degree | 41 (20) | 13 (19) | 13 (19) | 15 (22) | |
| Some College | 61 (30) | 18 (27) | 24 (36) | 19 (28) | |
| Collage Degree | 47 (23) | 18 (27) | 13 (19) | 16 (24) | |
| Graduate Degree | 33 (16) | 11 (16) | 11 (16) | 11 (16) | |
| Median Morisky Score (IQR) | 6 (4.75, 7) | 6 (5, 7) | 6 (4.75, 7) | 5.5 (4.75, 7) | 0.097 (K) |
| Categorical Morisky Score | 0.06 (P) | ||||
| High Adherence | 3 (2) | 1 (2) | 1 (2) | 1 (1) | |
| Medium Adherence | 100 (50) | 36 (55) | 40 (61) | 24 (36) | |
| Low Adherence | 96 (48) | 29 (44) | 25 (38) | 42 (63) | |
| Missing | 2 | 1 | 1 | 0 | |
| Median Baseline MPR (IQR) | 0.58 (0.49, 0.74) | 0.66 (0.49, 0.74) | 0.49 (0.33, 0.74) | 0.58 (0.49, 0.74) | 0.33 (K) |
| Median Number of Meds (IQR) | 10 (6, 13) | 9 (7, 12) | 10 (6, 13) | 10 (6, 15.5) | 0.89 (K) |
* K = Kruskal–Wallis test, P = Pearson's Chi-Square Test
** This category indicates the primary payer, although all participants had their health benefits provided through Humana. For example, Medicare beneficiaries in the study had Medicare Advantage plans that were provided through Humana. As a second example, some patients had Medicaid which had contracted with Humana to provide insurance benefits
Table 2.
SUPPORT Participant Characteristics, Overall and by Arm (N = 200)
| Arms | ||||||
|---|---|---|---|---|---|---|
| Variables | Total (N = 200) | Daily Message (n = 50) | Weekly Message (n = 50) | Missed Dose Message (n = 50) | Control (n = 50) | P value* |
| Median Age (IQR) | 68 (60, 72) | 68.5 (59, 74) | 67 (57, 72) | 67 (60, 72) | 70 (63, 72) | 0.58 (K) |
| Mean Age | 66 (10) | 67 (10) | 66 (10) | 65 (9) | 67 (10) | |
| Male (%) | 100 (50) | 20 (40) | 25 (50) | 28 (56) | 27 (54) | 0.39 (P) |
| Median BMI (IQR) | 31 (27, 36) | 32 (28, 36) | 30 (27, 36) | 30 (27, 35) | 31 (28, 37) | 0.66 (K) |
| Race (%) | 0.13 (P) | |||||
| American Indian | 1 (1) | 0 | 0 | 1 (2) | 0 | |
| Asian | 5 (3) | 0 | 1 (2) | 2 (4) | 2 (4) | |
| Black | 10 (5) | 0 | 3 (6) | 4 (8) | 3 (6) | |
| Hawaiian or Other Pacific Islander | 1 (1) | 0 | 1 (2) | 0 | 0 | |
| White | 174 (87) | 45 (90) | 41 (82) | 43 (86) | 45 (90) | |
| Other/Multiracial | 9 (5) | 5 (10) | 4 (8) | 0 | 0 | |
| Hispanic ethnicity | 12 (6) | 4 (8) | 5 (10) | 2 (4) | 1 (2) | 0.32 (P) |
| Insurance type | 0.65 (P) | |||||
| Private | 40 (20) | 10 (20) | 11 (22) | 10 (20) | 9 (18) | |
| Medicare | 155 (78) | 40 (80) | 38 (76) | 37 (74) | 40 (80) | |
| Medicaid | 5 (3) | 0 | 1 (2) | 3 (6) | 1 (2) | |
| Self-Insured | 0 | 0 | 0 | 0 | 0 | |
| Uninsured | 0 | 0 | 0 | 0 | 0 | |
| Frequently fill statin medication without using Humana | 30 (15) | 9 (18) | 9 (18) | 9 (18) | 3 (6) | 0.24 (P) |
| Diabetes type | 0.52 (P) | |||||
| Type 1 | 8 (4) | 3 (6) | 3 (6) | 1 (2) | 1 (2) | |
| Type 2 | 177 (89) | 42 (86) | 42 (84) | 45 (92) | 48 (96) | |
| Other/Unknown | 13 (7) | 4 (8) | 5 (10) | 3 (6) | 1 (2) | |
| Missing | 2 | 1 | 0 | 1 | 0 | |
| Highest level of education | 0.75 (P) | |||||
| Less than High School | 10 (5) | 5 (10) | 1 (2) | 3 (6) | 1 (2) | |
| GED | 6 (3) | 1 (2) | 3 (6) | 1 (2) | 1 (2) | |
| High School Degree | 35 (18) | 12 (24) | 10 (20) | 5 (10) | 8 (16) | |
| Some College | 68 (34) | 14 (28) | 17 (34) | 18 (36) | 19 (38) | |
| College Degree | 49 (25) | 11 (22) | 11 (22) | 14 (28) | 13 (26) | |
| Graduate Degree | 32 (16) | 7 (14) | 8 (16) | 9 (18) | 8 (16) | |
| Median Morisky Score (IQR) | 5.75 (4.75, 7) | 5.38 (4, 6.75) | 6 (4.75, 7) | 5.75 (4.75, 7) | 5.75 (4.75, 7) | 0.45 (K) |
| Categorical Morisky Score | 0.64 (P) | |||||
| High Adherence | 3 (2) | 1(2) | 2 (4) | 0 | 0 | |
| Medium Adherence | 90 (45) | 21 (42) | 24 (48) | 23 (46) | 22 (44) | |
| Low Adherence | 107 (54) | 28 (56) | 24 (48) | 27 (54) | 28 (56) | |
| Median Baseline MPR (IQR) | 0.58 (0.49, 0.74) | 0.58 (0.49, 0.74) | 0.58 (0.49, 0.74) | 0.58 (0.49, 0.74) | 0.68 (0.49, 0.74) | 0.70 (K) |
| Median Number of Meds (IQR) | 11 (7, 15) | 12 (9, 16) | 10 (7, 14) | 11 (7, 15) | 9.5 (6.50, 14) | 0.47 (K) |
* K = Kruskal–Wallis test, P = Pearson's Chi-Square Test
Table 3.
SUPPORT Descriptive Statistics of Contact with Partner (MAP), Overall and by Arm
| Overall (N = 187) | Daily Message (n = 47) | Weekly Message (n = 49) | Missed Dose Message (n = 45) | Control (n = 46) | P value | |
|---|---|---|---|---|---|---|
| MAP Relationship (%) | 0.31 | |||||
| Intimate partners | 114 (61) | 24 (51) | 30 (61) | 31 (69) | 29 (63) | |
| Children | 45 (24) | 16 (34) | 11 (22) | 9 (20) | 9 (20) | |
| Other relatives | 13 (7) | 6 (13) | 3 (6) | 1 (2) | 3 (7) | |
| Friends | 15 (8) | 1 (2) | 5 (10) | 4 (9) | 5 (11) | |
| Frequency of Any Type of Contact | 0.70 | |||||
| Missing | 1 | 0 | 1 | 0 | 0 | |
| Less than once a month | 21 (11) | 5 (11) | 5 (10) | 6 (13) | 5 (11) | |
| Less than once a week | 12 (6) | 2 (4) | 5 (10) | 4 (9) | 1 (2) | |
| Once a week or more | 153 (82) | 40 (85) | 38 (79) | 35 (78) | 40 (87) | |
| Frequency of Adherence Discussions | 0.39 | |||||
| Missing | 1 | 0 | 1 | 0 | 0 | |
| Less than once a month | 61 (33) | 9 (19) | 18 (38) | 15 (33) | 19 (41) | |
| Less than once a week | 56 (30) | 18 (38) | 14 (29) | 13 (29) | 11 (24) | |
| Once a week or more | 69 (37) | 20 (43) | 16 (33) | 17 (38) | 16 (35) | |
| Methods of Communication | 0.83 | |||||
| Missing | 2 | 0 | 2 | 0 | 0 | |
| Face to face | 141 (76) | 38 (81) | 36 (77) | 33 (73) | 34 (74) | |
| Other means | 44 (24) | 9 (19) | 11 (23) | 12 (27) | 12 (26) | |
At baseline, some participants acknowledged that they sometimes obtained their statins using a method other than their Humana pharmacy benefits (15 % in PROMOTE; 16 % in SUPPORT).
Outcomes
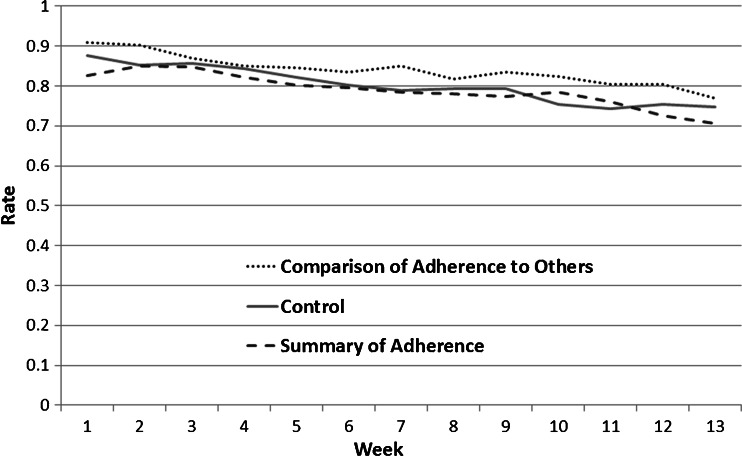
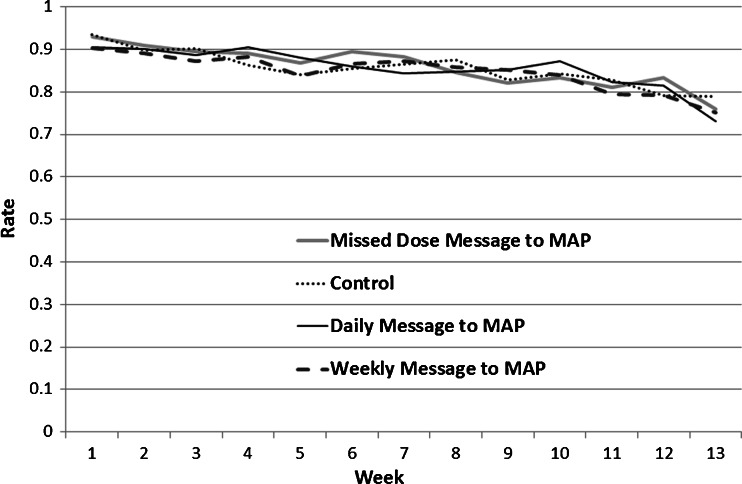
When assessed in the total populations of the PROMOTE and SUPPORT studies, median adherence during the intervention period was 90 % or higher (Median 90 % in PROMOTE, 92 % in SUPPORT; mean adherence in PROMOTE was 81 % [SD 24 %] and in SUPPORT was 85 % [SD 0.17]). Visual inspection of the adherence plots in Figures 2 and 3 demonstrates that bottle-measured adherence declined over time in all arms of both studies.
Fig. 2.
PROMOTE overall mean weekly adherence, by Arm.
Fig. 3.
SUPPORT overall mean weekly adherence, by Arm.
In PROMOTE, neither intervention demonstrated significantly better adherence than the control arm. Among participants with below median adherence pre-intervention, adherence during the intervention in the comparison arm was higher than in the control and no-comparison arms, but these differences were not statistically significant (median 89 % vs. 86 % and 76 %, p = 0.10).
For the SUPPORT study, none of the interventions demonstrated significantly better adherence than the control arm (Fig. 3). Overall, there were no statistically significant differences in frequency of reported contact between MAPs and participants. Eighty-two percent of participants stated that any such contact took place once a week or more. Thirty-seven percent of SUPPORT participants reported speaking to their MAPs specifically about adherence once a week or more frequently.
In SUPPORT and PROMOTE, interaction terms between study arms and the baseline Morisky adherence category were non-significant.
Finally, there were also no significant differences in either study between arms in the secondary outcome of change in Morisky self-reported adherence score.
DISCUSSION
This pair of pilot randomized trials demonstrated the feasibility of implementing adherence interventions based on social forces, but the social forces and social comparison interventions did not improve adherence compared to control over the 3-month intervention period. In a PROMOTE trial subgroup analysis of participants with low baseline adherence (defined as MPR < median), the comparison intervention had higher adherence when compared to the other two arms, but this comparison was not statistically significant. Despite limiting enrollment to individuals with a MPR <80 % based on claims data, we found that the median adherence rate in the pooled populations of the two studies was higher than 90 % (as measured by electronic pill bottles) during the intervention.
The high pill-bottle adherence rates—found even in the control arms—were unexpected. This finding may be related to the low enrollment rate among individuals invited to join the trials. Less than 1 % of health plan members who received letters participated in the trial, suggesting that the participants who enrolled were a highly select subsample of the entire eligible population. It is possible that participants were individuals with existing interest in improving their medication adherence and that trial enrollment and pill bottle usage, even for control arm participants, provided sufficient encouragement to make this improvement. The improvement in medication adherence across all arms might be explained by a “Hawthorne effect,” the phenomenon that behavior under observation often changes substantially. Alternatively, it is possible that participants had higher adherence than their MPR calculated from claims data suggested. For example, a statin MPR could underestimate true adherence if an individual obtains a supply of statins without using the pharmacy insurance benefit that generates the claims used to calculate MPRs. Notably, 15 % of participants in PROMOTE and 16 % in SUPPORT acknowledged receiving statins without submitting pharmacy benefit claims. As a second example, in situations where the physician reduces the statin dose, the patient may cut pills and use up the current supply, which would also underestimate adherence. Notably, almost a third of participants had high self-rated adherence on the baseline MMAS, providing some evidence that the MPR-based approach to identifying eligible individuals may have included adults with high statin adherence.
The trial’s high baseline adherence rates may have limited the ability to detect differences between intervention arms (i.e., a “ceiling effect”). Although not statistically significant, Figure 2 reveals that the comparison arm of the PROMOTE trial had higher adherence for most of the study. On the other hand, Figure 3 shows that in the SUPPORT trial, adherence rates were extremely similar across all four arms. We also acknowledge the possibility that social forces or the mode of message delivery were simply not an effective intervention. Although it did not test the impact of social forces, a pilot trial by Gatwood et al. using tailored messages did not detect improvements in adherence rates (measured through pharmacy claims) vs. standard care among patients with diabetes.27
The study had several limitations. The interventions lasted only 3 months; differences in adherence might emerge over a longer period of time. The two studies required all individuals to use electronic pill bottles, which may have increased adherence, as participants knew their actions were being recorded. The primary outcome of pill-bottle-measured adherence has limitations, including bottle malfunction. The study did not have additional objective measures of intervention effects, such as serum cholesterol. We also did not provide training or incentives to MAPs or collect information about their interactions with participants, limiting our ability to draw inferences about communication between pairs.
We also acknowledge limitations of generalizability. The generalizability of the SUPPORT study was limited in that enrollment was restricted to individuals who could identify a MAP who was willing to receive adherence messages. Future studies of social support to improve health behaviors such as adherence could consider either assigning a member of the study staff to act as a MAP or a peer mentor identified by the study. Participants in both trials were older and had a higher level of education than most US residents.28 Interventions based on social forces that were implemented among less advantaged or younger patients might be more efficacious.12 Enrollment also required computer use, which might limit dissemination of similar interventions in the future. On the other hand, due to the randomized controlled design, these trials should have high internal validity.
CONCLUSIONS
Two pilot trials revealed that interventions based on social support and social comparison were feasible to implement and well tolerated by participants. Median adherence rates in the trials were over 90 %, and the interventions did not lead to significant differences in medication adherence. The trials were limited by short duration, and the results may apply primarily to individuals who seek support for their medication adherence. Investigators designing future trials that use MPR screening criteria may consider restricting the population to individuals using one pharmacy service and/or supplemental inclusion criteria such as self-reported adherence to increase the probability that participants truly have low adherence.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(DOCX 112 kb)
Acknowledgments
The authors acknowledge the advice of Mr. Jeff Spurlock at Humana regarding recruitment processes and analysis of claims data.
Compliance with Ethical Standards
Financial Support
Funding for this study was provided by Merck, Sharpe, and Dohme Corp. The investigators had complete control over the recruitment procedures, data collection, data analysis, and presentation. Humana Inc. also provided support for the study by identifying potentially eligible members and mailing letters to those individuals.
Conflict of Interest
Kevin Volpp is a principal at the behavioral economics consulting firm VAL Health and has received consulting income and research support from CVS Health as well as research support from Humana, Weight Watchers, and the Vitality Institute (not related to Vitality, Inc., the manufacturer of the GlowCap pill bottle). Andrea Troxel has received consulting income from VAL Health and research support from the Vitality Institute and Weight Watchers. Jalpa Doshi has served as an advisory board member for Merck & Co., Inc., and has received research support from Humana, Pfizer, and Amgen. Peter Reese has received research support from CVS for studies of medication adherence. The other authors of this manuscript have no conflicts of interest to disclose.
REFERENCES
- 1.Cialdini RB, Goldstein NJ. Social influence: compliance and conformity. Annu Rev Psychol. 2004;55:591–621. doi: 10.1146/annurev.psych.55.090902.142015. [DOI] [PubMed] [Google Scholar]
- 2.Mukherjee JS, Ivers L, Leandre F, Farmer P, Behforouz H. Antiretroviral therapy in resource-poor settings. Decreasing barriers to access and promoting adherence. J Acquir Immune Defic Syndr. 2006;43(Suppl 1):S123–S126. doi: 10.1097/01.qai.0000248348.25630.74. [DOI] [PubMed] [Google Scholar]
- 3.Franke MF, Kaigamba F, Socci AR, et al. Improved retention associated with community-based accompaniment for antiretroviral therapy delivery in rural rwanda. Clin Infect Dis Off Publ Infect Dis Soc Am. 2013;56:1319–26. doi: 10.1093/cid/cis1193. [DOI] [PubMed] [Google Scholar]
- 4.Koenig SP, Leandre F, Farmer PE. Scaling-up HIV treatment programmes in resource-limited settings: the rural Haiti experience. AIDS. 2004;18(Suppl 3):S21–S25. doi: 10.1097/00002030-200406003-00005. [DOI] [PubMed] [Google Scholar]
- 5.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357:370–9. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 6.Allcott H, Rogers T. The short-run and long-run effects of behavioral interventions: Experimental evidence from energy conservation. Natl Bur Econ Res. 2012.
- 7.Kesselheim AS, Cresswell K, Phansalkar S, Bates DW, Sheikh A. Clinical decision support systems could be modified to reduce 'alert fatigue' while still minimizing the risk of litigation. Health Aff. 2011;30:2310–7. doi: 10.1377/hlthaff.2010.1111. [DOI] [PubMed] [Google Scholar]
- 8.Allcott H. Social norms and energy conservation. J Public Econ. 2011;95:1082–95. doi: 10.1016/j.jpubeco.2011.03.003. [DOI] [Google Scholar]
- 9.Goldstein NJ, Cialdini RB, Griskevicius V. A room with a viewpoint: Using social norms to motivate environmental conservation in hotels. J Consum Res. 2008;35:472–82. doi: 10.1086/586910. [DOI] [Google Scholar]
- 10.Frey BS, Meier S. Social comparisons and pro-social behavior: Testing "conditional cooperation" in a field experiment. Am Econ Rev. 2004;94:1717–22. doi: 10.1257/0002828043052187. [DOI] [Google Scholar]
- 11.Coffman LC, Featherstone CR, Kessler JB. Can Social Information Affect What Job You Choose and Keep?.
- 12.Long JA, Jahnle EC, Richardson DM, Loewenstein G, Volpp KG. Peer mentoring and financial incentives to improve glucose control in African American veterans: a randomized trial. Ann Intern Med. 2012;156:416–24. doi: 10.7326/0003-4819-156-6-201203200-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994;344:1383-9. [PubMed]
- 14.Cannon CP, Braunwald E, McCabe CH, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004;350:1495–1504. doi: 10.1056/NEJMoa040583. [DOI] [PubMed] [Google Scholar]
- 15.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143-421. [PubMed]
- 16.Baigent C, Keech A, Kearney PM, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–78. doi: 10.1016/S0140-6736(05)67394-1. [DOI] [PubMed] [Google Scholar]
- 17.Shah ND, Dunlay SM, Ting HH, et al. Long-term medication adherence after myocardial infarction: experience of a community. Am J Med. 2009;122:961 e7–13. doi: 10.1016/j.amjmed.2008.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ho PM, Magid DJ, Shetterly SM, et al. Medication nonadherence is associated with a broad range of adverse outcomes in patients with coronary artery disease. Am Heart J. 2008;155:772–9. doi: 10.1016/j.ahj.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 19.Ho PM, Rumsfeld JS, Masoudi FA, et al. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166:1836–41. doi: 10.1001/archinte.166.17.1836. [DOI] [PubMed] [Google Scholar]
- 20.Jackevicius CA, Mamdani M, Tu JV. Adherence with statin therapy in elderly patients with and without acute coronary syndromes. JAMA. 2002;288:462–7. doi: 10.1001/jama.288.4.462. [DOI] [PubMed] [Google Scholar]
- 21.Loewenstein G, Brennan T, Volpp KG. Asymmetric paternalism to improve health behaviors. JAMA. 2007;298:2415–7. doi: 10.1001/jama.298.20.2415. [DOI] [PubMed] [Google Scholar]
- 22.Morisky DE, DiMatteo MR. Improving the measurement of self-reported medication nonadherence: response to authors. J Clin Epidemiol. 2011;64:255–7. doi: 10.1016/j.jclinepi.2010.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10:348–54. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 24.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. J Pers Assess. 1988;52:30–41. doi: 10.1207/s15327752jpa5201_2. [DOI] [Google Scholar]
- 26.Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J Pers Assess. 1990;55:610–7. doi: 10.1207/s15327752jpa5503&4_17. [DOI] [PubMed] [Google Scholar]
- 27.Gatwood J, Balkrishnan R, Erickson SR, An LC, Piette JD, Farris KB. The impact of tailored text messages on health beliefs and medication adherence in adults with diabetes: A randomized pilot study. Res Social Adm Pharm RSAP. 2015. [DOI] [PubMed]
- 28.Ryan CL, Siebens J. Educational Attainment in the United States: 2009. URL: http://www.census.gov/prod/2012pubs/p20-566.pdf United States Census Bureau. U.S. Department of Commerce. 2012. Accessed: 08/20/2015.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 112 kb)