Abstract
Oxidative stress is thought to be one of the main mediators of neuronal damage in human neurodegenerative disease. Still, the dissection of causal relationships has turned out to be remarkably difficult. Here, we have analyzed global protein oxidation in terms of carbonylation of membrane proteins and cytoplasmic proteins in three different mammalian species: aged human cortex and cerebellum from patients with or without Alzheimer's disease, mouse cortex and cerebellum from young and old animals, and adult rat hippocampus and cortex subjected or not subjected to cerebral ischemia. Most tissues showed relatively similar levels of protein oxidation. However, human cortex was affected by severe membrane protein oxidation, while exhibiting lower than average cytoplasmic protein oxidation. In contrast, ex vivo autooxidation of murine cortical tissue primarily induced aqueous protein oxidation, while in vivo biological aging or cerebral ischemia had no major effect on brain protein oxidation. The unusually high levels of membrane protein oxidation in the human cortex were also not predicted by lipid peroxidation, as the levels of isoprostane immunoreactivity in human samples were considerably lower than in rodent tissues. Our results indicate that the aged human cortex is under steady pressure from specific and potentially detrimental membrane protein oxidation. The pronounced difference between humans, mice and rats regarding the primary site of cortical oxidation might have contributed to the unresolved difficulties in translating into therapies the wealth of data describing successful antioxidant neuroprotection in rodents.
Keywords: Aging, Alzheimer's disease, Animal models, Neurodegeneration, Oxidative stress, Protein oxidation
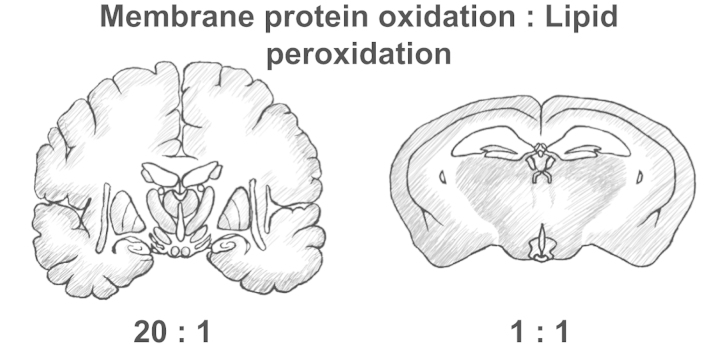
Graphical abstract
Highlights
-
•
Membrane proteins from the human cerebral cortex show specific and severe oxidation.
-
•
This contrasts to human cerebellum and to mouse cortex and cerebellum of any age.
-
•
It also contrasts to adult rat cortex and hippocampus with or without ischemia.
-
•
Lipid peroxidation is not a predictor of membrane protein oxidation.
-
•
Membrane protein oxidation might be related to impending neurodegeneration.
Introduction
Oxidative stress and redox dysregulation are biochemical characteristics of aging and many neurodegenerative disorders [1], [2], [3], [4]. For instance, increased steady-state levels of oxidative end products have been reported for the majority of neurodegenerative diseases. However, only few of the clinical studies pursuing antioxidant regimens have ended with a positive outcome, and the benefit was usually modest [2], [5]. Thus, it is possible that some of the functionally relevant targets of oxidation in these diseases are still to be discovered.
The potential biochemical victims of redox failure in the aged or injured human brain are diverse. Results from post-mortem studies have indicated that in Alzheimer's disease, above-normal levels of oxidation in proteins can occur on soluble proteins as well as protein filaments and aggregates [6]. Various side chains as well as the protein backbone may be affected. Specifically, protein tyrosine nitration [7], dityrosine formation [7], glycoxidation [8] and protein carbonyl accumulation [9], [10] have been described. Moreover, significant damage to nucleic acids has been demonstrated [10], [11], [12]. Notably though, effect sizes in many of these investigations have been relatively small [9], [10].
Integral membrane proteins have rarely been studied as separate entity in brain protein oxidation studies, despite the fact that various observations indicate a special role for these proteins as targets of oxidation. For instance, membrane proteins of the inner mitochondrial membrane massively accumulate the antioxidant amino acid methionine as a means of autoprotection [13], whereas other redox-active amino acids are avoided in an oxygen usage-dependent manner [14], [15]. In senescence accelerated-prone mice, spin labeling studies have indicated a selective, oxidative stress-induced alteration of synaptosomal membrane protein structure [16]. Moreover, model studies in vitro [17] and in cultivated cells [18], [19] have suggested the occurrence and relevance of one-electron transfer reactions from within the lipid bilayer onto the lateral surfaces of the embedded membrane proteins. After all, the fact that only lipophilic antioxidants show relevant neuroprotective capacity in cell culture [19], [20], [21] might not only be due to their selective prevention of lipid peroxidation, but also due to their selective prevention of integral membrane protein oxidation. Hence, we have investigated the extent of membrane protein oxidation in neural tissues from mice, rats, and humans, in order to achieve a basic characterization of its occurrence in the central nervous system.
Materials and methods
Human Alzheimer's disease tissue
Post-mortem tissue samples from neocortex and cerebellum of three non-demented individuals (Hu1–Hu3) and three Alzheimer׳s disease patients (Hu4–Hu6) were obtained from the Brain Bank of the Paul Flechsig Institute for Brain Research at the University of Leipzig. The diagnosis of definite Alzheimer's disease was based on the presence of neurofibrillary tangles and neuritic plaques in hippocampus and neocortex and met the criteria of the National Institute on Aging (NIA) and the Consortium to Establish a Registry for Alzheimer's Disease (CERAD) [22]. All cortical tissues were from Brodman area 22 of the temporal lobe. Alzheimer's disease cases were Braak stage V/VI, controls were either free of discernible neuropathological changes or possessed only a few isolated neurofibrillary tangles [23]. Terminal cause of death was bronchopneumonia in all cases. Further diagnoses and post mortem intervals (PMI) were: Hu1: age 78 y, male, PMI 24 h; nicotine abuse, arteriosclerosis. Hu2: age 84 y, female, PMI 36 h; chronic alcoholism. Hu3: age 82 y, male, PMI 46 h; arteriosclerosis. Hu4: age 69 y, male, PMI 40 h. Hu5: age 64 y, female, PMI 32 h. Hu6: age 88 y, female, PMI 48 h. Regarding the potential influence of the additional diagnoses in the non-demented individuals on brain protein oxidation, no data from human samples seem to exist. Consideration of plasma markers indicates that chronic alcohol abuse might be associated with elevated protein oxidation, whereas smoking appears to have a minor effect at most [24]. In rodent models, all conditions have been linked with variable manifestations of oxidative stress in the periphery. However, major effects on the brain have not been reported.
Mouse aging cohort
A cohort of C57BL/6J mice was established and aged under standard animal care conditions. After weaning, male and female animals were caged separately in groups of maximum 5 littermates per cage, with free access to food and water, residing in temperature-, humidity-, and light-controlled rooms (12 h light/dark cycle). Young (Ms1–Ms3) and old (Ms4–Ms9) mice were caged individually 1 week before sacrifice by cervical dislocation. The removed brains were flash-frozen in isopentane/dry ice, wrapped in parafilm, individually placed in small plastic boxes and thereupon stored at −80 °C. To match the human tissues analyzed, cortex and cerebellum were chosen for the determination of membrane protein oxidation. Animal parameters were: Ms1: age 152 d, male, weight 27 g. Ms2: age 150 d, male, weight 30 g. Ms3: age 150 d, female, weight 27 g. Ms4: age 651 d, male, weight 34 g. Ms5: age 642 d, female, weight 26 g. Ms6: age 808 d, female, weight 28 g. Ms7: age 794 d, male, weight 34 g. Ms8: age 651 d, female, weight 27 g. Ms9: age 651 d, male, weight 34 g.
Bilateral carotid artery occlusion (BCAO) in rats
BCAO with hemorrhagic hypotension was applied to male, 10–12 week old Sprague–Dawley rats as described [25]. After 2 h, the animals were sacrificed, and the anatomical regions of interest were dissected and frozen at −80 °C. As only the hippocampus is selectively affected by cell loss in this model of cerebral ischemia, cortex and hippocampus (in lieu of cerebellum) were further processed for biochemical analysis. Non-ischemic, naive rats (R1–R3) of the same cohort were used as controls for the cerebral ischemia rats (R4–R7).
Membrane protein preparation
Human, mouse and rat brain samples were fractionated by differential centrifugation. Samples of ~100–200 mg were homogenized on ice with a Potter-Elvehjem apparatus in 6 volumes of buffer A, containing 5 mM TRIS pH 7.4, 1 mM EDTA, 1 mM DTT, 10 µM phenothiazine, and 1× protease inhibitor cocktail (Sigma-Aldrich). Following 60 passages through a 25-gauge needle and brief sonication (3×5 s), the homogenate was mildly centrifuged (800g for 10 min at 4 °C) to remove any protein aggregates and insoluble material. The supernatant was then ultracentrifuged (100,000g for 90 min at 4 °C) to generate membrane (pellet) and cytoplasmic (supernatant) fractions, which were quality controlled by Western blotting against the marker proteins Na+/K+-ATPase (ATP1A1) and superoxide dismutase (SOD1) using monoclonal antibodies (anti-Na+/K+-ATPase α1 subunit from Novus Biologicals, 1:1000; anti-SOD1 from Epitomics, 1:1000). A selection of human and rat brain samples were also fractionated by phase separation with Triton X-114 [26], yielding similar results. Protein contents of all obtained fractions were determined using the bicinchoninic acid method (Pierce), which was compatible with the employed buffer and reagent concentrations.
Protein carbonyl immunoblotting
Protein carbonyls were quantified by derivatization with 2,4-dinitrophenyl hydrazine (DNPH). Subcellular fractions containing 8 µg protein were adjusted to identical volume with buffer A, supplemented with 0.5 volumes of buffer B (180 mM TRIS pH 7.4, 30% sucrose, 6% SDS), mixed, and incubated with 0.5 volumes of freshly prepared DNPH derivatization solution (10 mM DNPH in 2 M HCl) for 20 min at room temperature. After neutralization with 0.33 volumes of 3 M TRIS base, the samples were supplemented with 0.33 volumes of loading buffer (200 mM TRIS pH 6.8, 40% glycerol, 20% β-mercaptoethanol, 8% SDS, 0.04% bromophenol blue), separated by SDS-PAGE in a 10% gel (acrylamide:bis-acrylamide 29:1) and transferred onto nitrocellulose membranes following standard protocols. After 1 h incubation with 5% fat-free dry milk in TBST, the membranes were probed with anti-2,4-dinitrophenyl (anti-DNP) antibody (1:1000; from Invitrogen) in TBST at 4 °C overnight. The membranes were washed three times with TBST, incubated for 1.5 h with peroxidase-conjugated donkey anti-rabbit antibody (1:10,000; from Jackson Immunoresearch) at room temperature, washed three times with TBST again, and visualized by enhanced chemiluminescence. Ponceau staining (0.1% Ponceau S in 5% acetic acid) of the blots was performed as loading control.
Anti-isoprostane enzyme immunoassay
The levels of anti-isoprostane immunoreactivity were determined by competitive enzyme immunoassay (Cayman Chemical), employing an antiserum that has been shown to be specific for 8-iso prostaglandin F2α against a considerable number of likely competitors (http://www.caymanchem.com/catalog/516351). Still, it cannot be excluded that it may have cross-reacted with oxidized, isoprostane-like derivatives of fatty acids other than arachidonic acid, particularly docosahexaenoic acid, which is an abundant, but rather evenly distributed component of the brain [27]. Hence, the obtained data are presented as relative immunoreactivities per unit of membrane protein rather than absolute 8-iso prostaglandin F2α concentrations.
Experimental design and statistical analysis
Primary objective of the current study was the comparison of membrane protein oxidation versus cytoplasmic protein oxidation in the brain of three mammalian species, i.e. human, mouse, and rat, with each species being represented by two anatomically distinct central nervous system tissues. Exploratory, secondary objectives of the current study were post-hoc analyses of probable sources of variation within each mammalian species, i.e. the potential role of central nervous system disease in the human samples, the potential role of age in the mouse samples, and the potential role of an ischemic lesion in the rat samples. All data were evaluated by two-way ANOVA (for the primary analysis of categorical variables) followed by Holm-Sidak's post-hoc test (for exploratory subgroup analysis); p values of 0.05 or less were considered significant. All data are given as mean±standard deviation.
Ethical standards
Human brain samples were obtained from the Brain Bank of the Paul Flechsig Institute for Brain Research at the University of Leipzig in accordance with the legal and institutional regulations under which it operates. Regarding animal housing and experimentation, appropriate procedures were used following the institutional guidelines of the Central Animal Facility of the University of Mainz, and approval was obtained in accordance with federal law.
Results
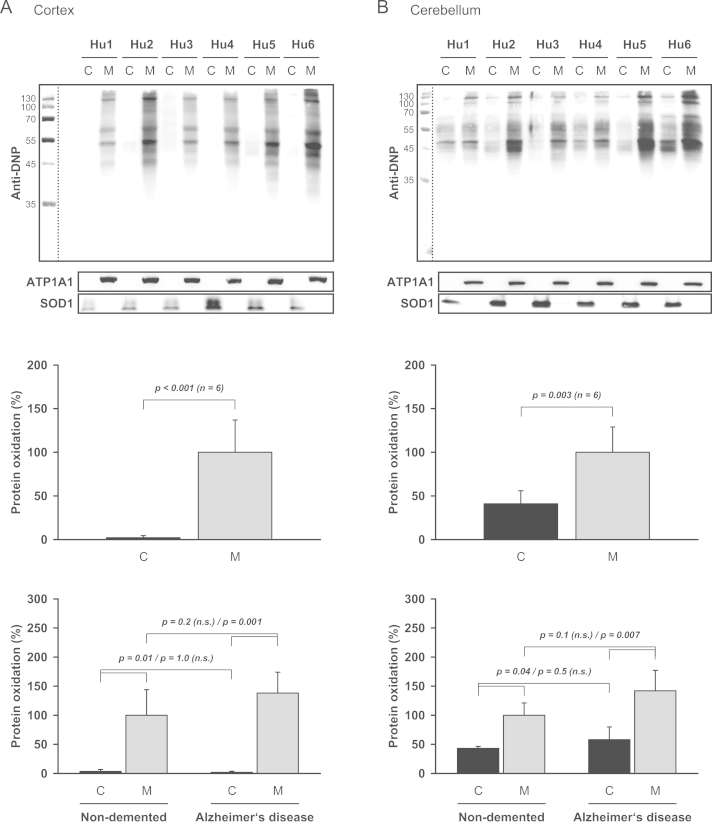
Membrane protein oxidation in human samples
To investigate whether membrane proteins were relevant targets of oxidation in the aged human brain, we have analyzed frozen post mortem tissue samples (n=6) from neocortex (superior temporal gyrus) and cerebellum, encompassing three Alzheimer's disease cases (AD) and three age-matched, non-demented individuals (ND). Protein carbonylation was chosen as index of oxidation because it reflects different types of oxidative insults, can be detected with high sensitivity by derivatization-Western blotting, and appears to be largely irreversible [28], [29]. We have found that in both brain regions, membrane proteins were significantly more affected by carbonylation and thus oxidative damage than cytoplasmic proteins (Fig. 1). This effect was more pronounced in cortex than in cerebellum, as evidenced by the calculated membrane/cytoplasm (M/C) oxidation ratios (cortex: 47; cerebellum: 2.4). Moreover, a trend towards higher membrane protein oxidation in Alzheimer's disease samples versus non-demented individuals was noted (cortex: 138%; cerebellum: 142%).
Fig. 1.
Protein oxidation in human cortex and cerebellum. (A) Cortical and (B) cerebellar tissue samples from three non-demented individuals (Hu1–Hu3) and three Alzheimer's disease patients (Hu4–Hu6) were separated by centrifugation into cytoplasmic (C) and membrane (M) fractions and analyzed by derivatization-Western blotting using an anti-DNP antibody. The numbers in the margin indicate molecular weights (kDa). Parallel blots were probed for the membrane marker Na+/K+-ATPase (ATP1A1) and the cytoplasmic marker superoxide dismutase (SOD1). The bar graphs represent a quantification of the anti-DNP immunoreactivity. In both cortex and cerebellum, membrane proteins were significantly more oxidized than cytoplasmic proteins (upper panels: p<0.001 for cortex, p=0.003 for cerebellum by two-way ANOVA; n=6 for each tissue). Significance levels obtained by post-hoc analysis for the non-demented and Alzheimer's disease subgroups are given in the figure (lower panels).
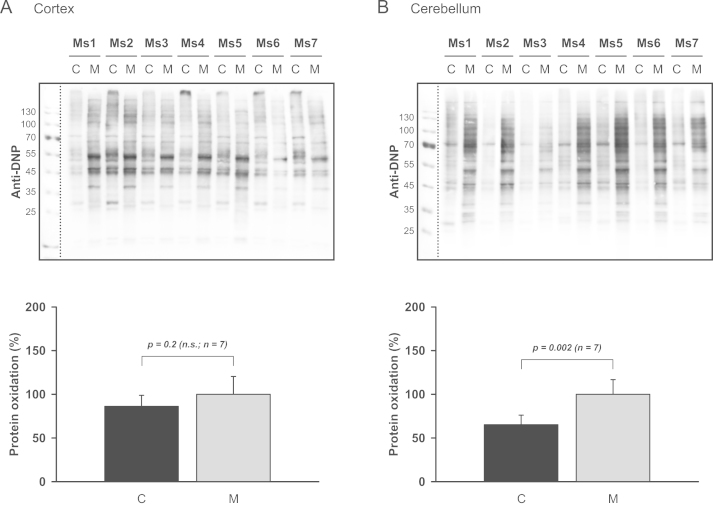
Membrane protein oxidation in mouse samples
Mice are the most widely employed species to model human neurological diseases associated with oxidative stress. Hence, it was investigated whether the apparently high levels of membrane protein carbonylation in the human cortex might also be detected in mice. As an effect of aging on protein carbonyl content has been described for a variety of settings [28], the aspect of age was explored as a potential source of variation. Thus, a cohort of C57BL/6J mice was grouped into categories young (aged ~150 d) and old (aged ~720 d; details are given in the materials and methods) and tested for brain protein oxidation. The analysis of cortical and cerebellar membrane and cytoplasmic fractions (n=7) shown in Fig. 2 indicates that mouse cortex did not exhibit any bias towards membrane protein oxidation as observed in the human cortical samples. In cerebellum, though, mouse samples resembled human samples in terms of their M/C oxidation ratio. However, there was no significant effect of age on carbonyl content throughout. In all fractions, human and murine, significant immunoreactivity was exclusively detected in proteins with molecular weights higher than ~45 kDa. Interestingly, some of the most intensely stained bands (at ~45 and ~55 kDa) in young cortical fractions were largely absent in the two “oldest old” animals (Ms6 and Ms7; Fig. 2A).
Fig. 2.
Protein oxidation in mouse cortex and cerebellum. (A) Cortical and (B) cerebellar tissue samples from three young (Ms1–Ms3) and four old (Ms4–Ms7) mice were analyzed for membrane (M) and cytoplasmic (C) protein oxidation as in Fig. 1. In cerebellum, membrane proteins were significantly more oxidized than cytoplasmic proteins (p=0.002 by two-way ANOVA; n=7). In cortex, no statistically significant difference was detected.
Effect of species, brain region, and sample storage on membrane protein oxidation
The large oxidation bias in the human cortical samples (Fig. 1A) could basically be attributable to an increased membrane signal, or to a decreased cytoplasmic signal. To distinguish these alternatives and to achieve a global comparison between brain regions and animal species, calibration blots were performed with selected samples already analyzed in Fig. 1, Fig. 2. A representative result is shown in Fig. 3A. Image quantification data from duplicate blots were used to calculate calibration factors, by which the cross-comparison of all subgroups shown in Fig. 3B was generated. The result suggests that human cortical samples are unusual in both respects, high membrane protein oxidation, and low cytoplasmic protein oxidation. In contrast, cerebellar samples were very similarly affected by protein oxidation in mice and humans. In order to assess the potential influence of post mortem handling on these results, oxidative and elevated temperature storage experiments with aged mouse cortices were performed. Incubation of cortex quarters for 2 d in air-exposed TBS at room temperature resulted in mildly elevated cytoplasmic protein oxidation, whereas membrane proteins were not affected (Fig. 3C and D). Incubation at 37 °C, however, led to pronounced protein oxidation, particularly in the cytoplasmic fractions. Thus, the absence of cytoplasmic oxidation in the human cortical samples strongly argues against any post mortem etiology of the observed high membrane protein oxidation, together with several other observations reconsidered in the discussion.
Fig. 3.
Influence of sample origin and sample handling on protein oxidation. (A) Cross-comparison of protein oxidation in four samples chosen as calibration benchmarks. The same, indicated samples as analyzed in Figs. 1 A, B and 2 A, B were blotted side by side and quantified to enable a direct comparison of the full blots. (B) Quantification of protein oxidation in human and mouse tissues based on two calibration blots as in (A). The abbreviations Y and O denote young and old animals, respectively. ND, non-demented individuals; AD, individuals with Alzheimer's disease. (C) Influence of storage conditions on protein oxidation in dissected cortices. Cortical quarters from two old mice (Ms8–Ms9) were frozen at −80 °C or incubated for 48 h at the indicated temperatures in air-exposed TBS before analyzing cytoplasmic (C) and membrane (M) fractions for anti-DNP immunoreactivity. (D) Quantification of the results depicted in (C). Protein oxidation was strongly associated with storage temperature (p=0.005 by two-way ANOVA; n=4). In the post-hoc analysis, this effect was attributable to the cytoplasmic fractions; subgroup p values are indicated in the figure. Differences at each temperature were statistically insignificant.
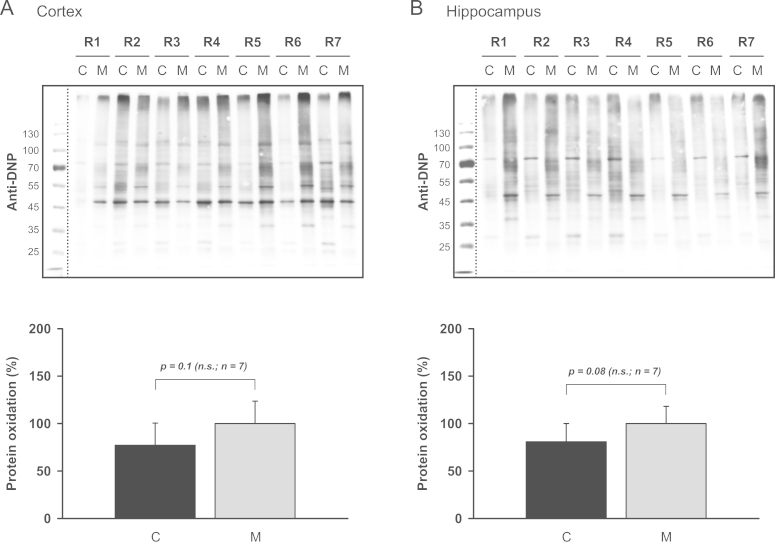
Membrane protein oxidation in rat samples
To investigate whether the second most important model species in clinical neuroscience, rats, were more predictive of the human situation, cortical and hippocampal tissues from Sprague–Dawley rats were analyzed for membrane and cytoplasmic protein oxidation. Since perimortal influences and acute lesional effects due to cerebral ischemia or trauma might have an impact on irreversible markers of oxidation, a subgroup of these animals was subjected to bilateral carotid artery occlusion with hemorrhagic hypotension 2 h prior to tissue sampling. As shown in Fig. 4, rats closely resembled mice in terms of an approximately equal level of protein oxidation in cytoplasmic and membrane cortical fractions (n=7), even if there was a trend towards higher oxidation of membrane proteins in ischemic samples (ischemic/native: 151%). In the hippocampus, which was analyzed instead of cerebellum in this experiment because it is severely affected by neurodegeneration under the employed ischemia protocol [25], no statistically significant differences between fractions or treatments could be detected. These data strengthen the idea that the observed patterns of oxidation in the human cortex indeed mirror physiological variables established prior to the event of death.
Fig. 4.
Protein oxidation in rat hippocampus and cortex. (A) Cortical and (B) hippocampal tissue samples from three naive (R1–R3) and four ischemic (R4–R7) rats were separated into cytoplasmic (C) and membrane (M) fractions and analyzed by Western blotting. In both brain regions, cytoplasmic proteins and membrane proteins were similarly affected by protein oxidation.
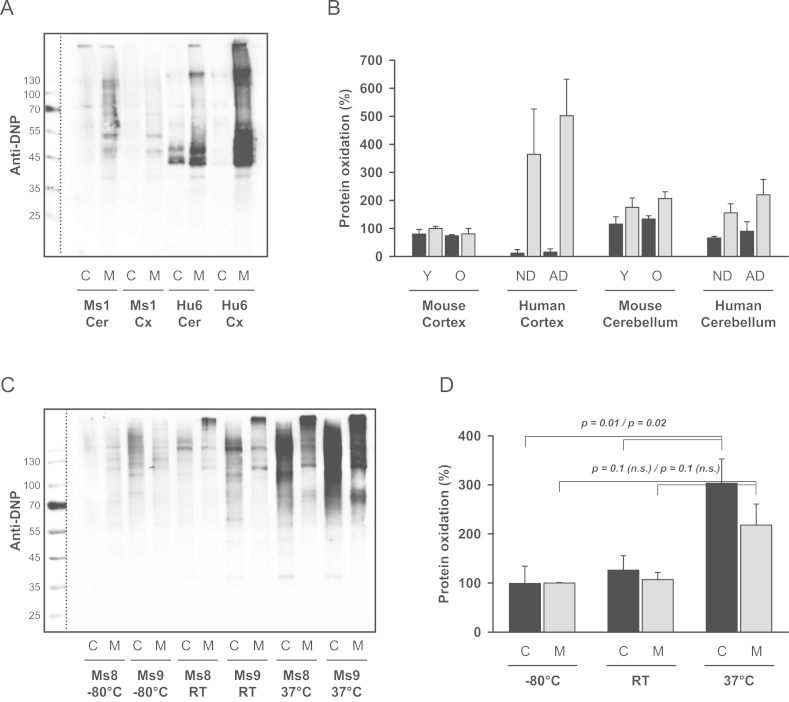
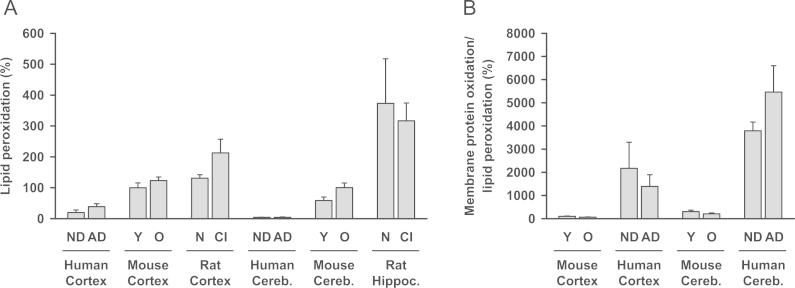
Relationship between membrane protein oxidation and lipid peroxidation
The defining characteristic of membrane proteins is their embedment into the lipid bilayer. To test whether membrane protein oxidation was predictable from more established markers of oxidation in the lipid bilayer, lipid peroxidation was quantified in terms of the detectable anti-isoprostane immunoreactivity in the membrane fractions already analyzed in Fig. 1, Fig. 2, Fig. 4. The result depicted in Fig. 5 demonstrates that there was at least no simple correlation between these two markers. Human samples were by far less affected by lipid peroxidation than rodent samples (Fig. 5A). The extent of the difference in cortex was approximately the same as in plasma samples reported individually in the literature (human: 100–300 pg/ml [30]; rat: ~500 pg/ml [31]; mouse: ~1500 pg/ml [32]; all samples had been analyzed by calibrated GC–MS or LC-MS). Dividing the relative level of membrane protein oxidation (Fig. 3B) by the relative level of lipid peroxidation (Fig. 5A), human samples from both cortex and cerebellum turned out to be about 20- to 40-fold more affected by membrane protein oxidation than the corresponding mouse tissues (Fig. 5B).
Fig. 5.
Lipid peroxidation in brain tissues of different origin. (A) Cortical and cerebellar tissues from human and mouse as well as cortical and hippocampal tissues from rat were analyzed for anti-isoprostane immunoreactivity by competitive enzyme immunoassay. The same membrane fractions as evaluated in Fig. 1, Fig. 2, Fig. 4 were employed in this assay. After normalization for protein content, young mouse cortex was arbitrarily defined as 100% as in Fig. 3B. The abbreviations denote: ND, non-demented; AD, Alzheimer's disease; Y, young; O, old; N, native; CI, cerebral ischemia. Tissue type and source had a significant influence on its level of lipid peroxidation (p<0.001 for species, p<0.001 for tissue by two-way ANOVA; n=12–14 for each species, n=7–20 for each tissue). In the post-hoc analysis, humans were less affected by lipid peroxidation than mice (p=0.008) and rats (p<0.001). (B) Calculated ratio of membrane protein oxidation versus membrane lipid peroxidation in cortex and cerebellum from mouse and human. Again, young mouse cortex was set as 100%.
Discussion
In this study, we have found that membrane proteins in the human brain are selectively affected by oxidation. Specifically, samples from the aged cerebral cortex exhibited severe membrane protein oxidation, which was accompanied by unusually low levels of cytoplasmic protein oxidation and lipid peroxidation (Figs. 1A, 3B, and 5A).
It is unlikely that the observed membrane protein oxidation bias in the human cortical samples is to a significant degree attributable to the post-mortem character of these tissues, for six reasons. (i) There was no correlation between the extent of membrane protein oxidation and post-mortem interval (PMI data are given in the materials and methods). (ii) Only cortical samples were more heavily oxidized than corresponding mouse samples. Human cerebellar samples exhibited the same degree of membrane protein oxidation as did directly frozen mouse cerebellar samples (Fig. 3B). (iii) Prolonged incubation of mouse cortices under oxidative conditions, in air-exposed TBS for 48 h at room temperature, did not induce membrane protein oxidation (Fig. 3D). (iv) At an elevated temperature of 37 °C, though, 48 h incubation did result in increased protein oxidation. However, cytoplasmic proteins were at least equally affected as membrane proteins (Fig. 3D). Still, the authentic human samples had been essentially devoid of cytoplasmic protein oxidation (Fig. 3B). (v) Incubation of mouse cortices for 48 h in a potentially more realistic, less oxidative body fluid mimetic, air-exposed serum (FCS), led to an apparent reduction of membrane protein oxidation by ~10% at room temperature, and by ~40% at 37 °C (data not shown). Thus, protein carbonylation appears to be a rather stable marker of oxidation even post mortem, which is in agreement with many previous studies [10], [33], [34]. (vi) The level of lipid peroxidation in the human samples was still much lower than in immediately frozen, but otherwise corresponding material from mouse or rat (Fig. 5A).
The origins of the higher steady-state levels of protein carbonylation in membrane proteins call for an explanation. Visibly, membrane proteins could be more exposed to carbonylating products of lipid peroxidation, such as 4-hydroxynonenal, malondialdehyde, or acrolein. However, the latter compounds are readily soluble in water, and experimental studies have indicated that even the most lipophilic of the mentioned agents, 4-hydroxynonenal, primarily reacts with cytoplasmic proteins [35]. Second, the transmembrane domains of membrane proteins might be sterically inaccessible to oxidized protein repair enzymes [13]. In general, though, protein carbonylation is thought to be irreversible and thus not subject to repair [29]. Third, the specific amino acid composition of transmembrane domains with their ample tyrosine and tryptophan residues could make these proteins particularly accessible to one-electron oxidation from within the lipid bilayer [18], [19]. If unrepaired [17], [36], these radicalized side chains could convert into DNPH-reactive quinones [37], or they might dissipate by attacking neighboring lysine residues or other susceptible moieties, transforming them into carbonyl end products [19], [38]. At present, though, none of these structural explanations appears to be fully satisfactory, as they should all apply to human, mouse, and rat membrane proteins to a basically similar extent.
As a more dynamic explanation, it is well possible that membrane proteins with their generally longer lifetimes, especially so in the brain [39], [40], simply accumulate more irreversible damage before finally being degraded. Intriguingly, this effect could be much more pronounced in the large human neocortex, in which the site of synthesis, site of function, and site of degradation of a protein are generally much more distant than in smaller brains [41]. Unfortunately, we are unaware of any experimental determination of protein lifetimes in the human brain. Regarding the unusually low levels of cytoplasmic protein oxidation in the human cortex, these proteins might profit more than membrane proteins from enhanced enzymatic antioxidant defenses, which tend to be considerably more active in the larger brains of longer-lived animals [42]. For example, catalase and manganese superoxide dismutase have been found to be more than 3-fold more active in cow or deer brain than in mouse or rat brain [42]. Most likely, a related effect also accounts for the low level of lipid peroxidation observed in human tissues.
In accordance with earlier investigations [8], [9], [10], we have seen only a mild increase in protein carbonylation in Alzheimer's disease (Fig. 1). Nevertheless, membrane protein oxidation might still be of critical importance for this and maybe other neurodegenerative conditions, as justified in the following. The conventional argument to implicate oxidative stress in neurodegeneration has usually been that steady-state levels of markers of oxidation were higher in tissue from affected patients than in control tissue. In slowly progressing diseases, though, this criterion might selectively point to markers of oxidation that are precisely not causally involved in the disease process. Why should this be the case? As neurodegeneration proceeds only very slowly in a progressive disorder like Alzheimer's disease, even in its later stages [43], there is only very little irreversible degeneration going on at any given point in time. Hence, the observed steady-state increase of the incriminated marker is apparently rather well tolerated by the brain. In contrast, unusually high levels of permanent baseline oxidation due to largely fixed anatomical, structural or metabolic circumstances specific to the human brain might be much more predictive of impending neurodegeneration. In these cases, even minor increases atop an already high baseline might move a synapse or neuron across the catastrophic threshold, generally followed by the rapid degradation of the collapsed structure by autophagy or glial cells. Hence, the very event that had triggered the catastrophe would have also secured its own disappearance, disabling its detection in steady-state comparisons. Hence, we believe that comparative investigations into the baseline levels of oxidation in young and healthy tissues might offer unconventional insight into the pathogenesis of neurodegeneration. In particular, the exploration of membrane protein oxidation as a separate and potentially autonomous manifestation of oxidative stress seems warranted.
Acknowledgments
Sincere thanks are given to Dr. Isabella Zwiener (Department of Medical Biometry, Epidemiology and Informatics, University Medical Center of the Johannes Gutenberg University) for her statistical advice, and to Michael Plenikowski (Institute for Physiological Chemistry, University Medical Center of the Johannes Gutenberg University) for the graphical abstract.
References
- 1.Halliwell B. Oxidative stress and neurodegeneration: where are we now? Journal of Neurochemistry. 2006;97(6):1634–1658. doi: 10.1111/j.1471-4159.2006.03907.x. 16805774 [DOI] [PubMed] [Google Scholar]
- 2.Sayre L.M., Perry G., Smith M.A. Oxidative stress and neurotoxicity. Chemical Research in Toxicology. 2008;21(1):172–188. doi: 10.1021/tx700210j. 18052107 [DOI] [PubMed] [Google Scholar]
- 3.Sohal R.S., Orr W.C. The redox stress hypothesis of aging. Free Radical Biology and Medicine. 2012;52(3):539–555. doi: 10.1016/j.freeradbiomed.2011.10.445. 22080087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Höhn A., König J., Grune T. Protein oxidation in aging and the removal of oxidized proteins. Journal of Proteomics. 2013;92:132–159. doi: 10.1016/j.jprot.2013.01.004. 23333925 [DOI] [PubMed] [Google Scholar]
- 5.Moosmann B., Behl C. Antioxidants as treatment for neurodegenerative disorders. Expert Opinion on Investigational Drugs. 2002;11(10):1407–1435. doi: 10.1517/13543784.11.10.1407. 12387703 [DOI] [PubMed] [Google Scholar]
- 6.Martínez A., Portero-Otin M., Pamplona R., Ferrer I. Protein targets of oxidative damage in human neurodegenerative diseases with abnormal protein aggregates. Brain Pathology. 2010;20(2):281–297. doi: 10.1111/j.1750-3639.2009.00326.x. 19725834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hensley K., Maidt M.L., Yu Z., Sang H., Markesbery W.R., Floyd R.A. Electrochemical analysis of protein nitrotyrosine and dityrosine in the Alzheimer brain indicates region-specific accumulation. Journal of Neuroscience. 1998;18(20):8126–8132. doi: 10.1523/JNEUROSCI.18-20-08126.1998. 9763459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pamplona R., Dalfó E., Ayala V. Proteins in human brain cortex are modified by oxidation, glycoxidation, and lipoxidation. Effects of Alzheimer disease and identification of lipoxidation targets. Journal of Biological Chemistry. 2005;280(22):21522–21530. doi: 10.1074/jbc.M502255200. 15799962 [DOI] [PubMed] [Google Scholar]
- 9.Hensley K., Hall N., Subramaniam R. Brain regional correspondence between Alzheimer's disease histopathology and biomarkers of protein oxidation. Journal of Neurochemistry. 1995;65(5):2146–2156. doi: 10.1046/j.1471-4159.1995.65052146.x. 7595501 [DOI] [PubMed] [Google Scholar]
- 10.Lyras L., Cairns N.J., Jenner A., Jenner P., Halliwell B. An assessment of oxidative damage to proteins, lipids, and DNA in brain from patients with Alzheimer's disease. Journal of Neurochemistry. 1997;68(5):2061–2069. doi: 10.1046/j.1471-4159.1997.68052061.x. 9109533 [DOI] [PubMed] [Google Scholar]
- 11.Nunomura A., Perry G., Pappolla M.A. RNA oxidation is a prominent feature of vulnerable neurons in Alzheimer's disease. Journal of Neuroscience. 1999;19(6):1959–1964. doi: 10.1523/JNEUROSCI.19-06-01959.1999. 10066249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang J., Xiong S., Xie C., Markesbery W.R., Lovell M.A. Increased oxidative damage in nuclear and mitochondrial DNA in Alzheimer's disease. Journal of Neurochemistry. 2005;93(4):953–962. doi: 10.1111/j.1471-4159.2005.03053.x. 15857398 [DOI] [PubMed] [Google Scholar]
- 13.Bender A., Hajieva P., Moosmann B. Adaptive antioxidant methionine accumulation in respiratory chain complexes explains the use of a deviant genetic code in mitochondria. Proceedings of the National Academy of Sciences of the United States of America. 2008;105(43):16496–16501. doi: 10.1073/pnas.0802779105. 18946048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moosmann B., Behl C. Mitochondrially encoded cysteine predicts animal lifespan. Aging Cell. 2008;7(1):32–46. doi: 10.1111/j.1474-9726.2007.00349.x. 18028257 [DOI] [PubMed] [Google Scholar]
- 15.Schindeldecker M., Stark M., Behl C., Moosmann B. Differential cysteine depletion in respiratory chain complexes enables the distinction of longevity from aerobicity. Mechanisms of Ageing and Development. 2011;132(4):171–179. doi: 10.1016/j.mad.2011.03.002. 21453719 [DOI] [PubMed] [Google Scholar]
- 16.Butterfield D.A., Howard B.J., Yatin S., Allen K.L., Carney J.M. Free radical oxidation of brain proteins in accelerated senescence and its modulation by N-tert-butyl-alpha-phenylnitrone. Proceedings of the National Academy of Sciences of the United States of America. 1997;94(2):674–678. doi: 10.1073/pnas.94.2.674. 9012843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bisby R.H., Ahmed S., Cundall R.B. Repair of amino acid radicals by a vitamin E analogue. Biochemical and Biophysical Research Communications. 1984;119(1):245–251. doi: 10.1016/0006-291x(84)91644-9. 6704121 [DOI] [PubMed] [Google Scholar]
- 18.Moosmann B., Behl C. Cytoprotective antioxidant function of tyrosine and tryptophan residues in transmembrane proteins. European Journal of Biochemistry. 2000;267(18):5687–5692. doi: 10.1046/j.1432-1327.2000.01658.x. 10971578 [DOI] [PubMed] [Google Scholar]
- 19.Hajieva P., Bayatti N., Granold M., Behl C., Moosmann B. Membrane protein oxidation determines neuronal degeneration. Journal of Neurochemistry. 2015 doi: 10.1111/jnc.12987. Pubmed: 25393523. [DOI] [PubMed] [Google Scholar]
- 20.Moosmann B., Skutella T., Beyer K., Behl C. Protective activity of aromatic amines and imines against oxidative nerve cell death. Biological Chemistry. 2001;382(11):1601–1612. doi: 10.1515/BC.2001.195. 11767950 [DOI] [PubMed] [Google Scholar]
- 21.Chang H.J., Kim H.J., Chun H.S. Quantitative structure–activity relationship (QSAR) for neuroprotective activity of terpenoids. Life Sciences. 2007;80(9):835–841. doi: 10.1016/j.lfs.2006.11.009. 17166521 [DOI] [PubMed] [Google Scholar]
- 22.Mirra S.S., Heyman A., McKeel D. The consortium to establish a Registry for Alzheimer's disease (CERAD). Part II. Standardization of the neuropathologic assessment of Alzheimer's disease. Neurology. 1991;41(4):479–486. doi: 10.1212/wnl.41.4.479. 2011243 [DOI] [PubMed] [Google Scholar]
- 23.Braak H., Braak E. Neuropathological staging of Alzheimer-related changes. Acta Neuropathologica. 1991;82(4):239–259. doi: 10.1007/BF00308809. 1759558 [DOI] [PubMed] [Google Scholar]
- 24.Kapaki E., Liappas I., Lyras L. Oxidative damage to plasma proteins in patients with chronic alcohol dependence: the effect of smoking. In Vivo. 2007;21(3):523–528. 17591364 [PubMed] [Google Scholar]
- 25.Lasarzik I., Noppens R.R., Wolf T. Dose-dependent influence of sevoflurane anesthesia on neuronal survival and cognitive outcome after transient forebrain ischemia in Sprague–Dawley rats. Neurocritical Care. 2011;15(3):577–584. doi: 10.1007/s12028-011-9562-3. 21618067 [DOI] [PubMed] [Google Scholar]
- 26.Bordier C. Phase separation of integral membrane proteins in Triton X-114 solution. Journal of Biological Chemistry. 1981;256(4):1604–1607. 6257680 [PubMed] [Google Scholar]
- 27.Xiao Y., Huang Y., Chen Z.Y. Distribution, depletion and recovery of docosahexaenoic acid are region-specific in rat brain. British Journal of Nutrition. 2005;94(4):544–550. doi: 10.1079/bjn20051539. 16197579 [DOI] [PubMed] [Google Scholar]
- 28.Levine R.L. Carbonyl modified proteins in cellular regulation, aging, and disease. Free Radical Biology and Medicine. 2002;32(9):790–796. doi: 10.1016/s0891-5849(02)00765-7. 11978480 [DOI] [PubMed] [Google Scholar]
- 29.Nyström T. Role of oxidative carbonylation in protein quality control and senescence. EMBO Journal. 2005;24(7):1311–1317. doi: 10.1038/sj.emboj.7600599. 15775985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sircar D., Subbaiah P.V. Isoprostane measurement in plasma and urine by liquid chromatography–mass spectrometry with one-step sample preparation. Clinical Chemistry. 2007;53(2):251–258. doi: 10.1373/clinchem.2006.074989. 17200134 [DOI] [PubMed] [Google Scholar]
- 31.Parker C.E., Graham L.B., Nguyen M.N. An improved GC/MS-based procedure for the quantitation of the isoprostane 15-F2t-IsoP in rat plasma. Molecular Biotechnology. 2001;18(2):105–118. doi: 10.1385/MB:18:2:105. 11471453 [DOI] [PubMed] [Google Scholar]
- 32.Janicka M., Kot-Wasik A., Paradziej-Łukowicz J., Sularz-Peszyńska G., Bartoszek A., Namieśnik J. LC–MS/MS determination of isoprostanes in plasma samples collected from mice exposed to doxorubicin or tert-butyl hydroperoxide. International Journal of Molecular Sciences. 2013;14(3):6157–6169. doi: 10.3390/ijms14036157. 23507752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Floor E., Wetzel M.G. Increased protein oxidation in human substantia nigra pars compacta in comparison with basal ganglia and prefrontal cortex measured with an improved dinitrophenylhydrazine assay. Journal of Neurochemistry. 1998;70(1):268–275. doi: 10.1046/j.1471-4159.1998.70010268.x. 9422371 [DOI] [PubMed] [Google Scholar]
- 34.Chandana R., Mythri R.B., Mahadevan A., Shankar S.K., Srinivas Bharath M.M. Biochemical analysis of protein stability in human brain collected at different post-mortem intervals. Indian Journal of Medical Research. 2009;129(2):189–199. 19293447 [PubMed] [Google Scholar]
- 35.Zhu X., Castellani R.J., Moreira P.I. Hydroxynonenal-generated crosslinking fluorophore accumulation in Alzheimer disease reveals a dichotomy of protein turnover. Free Radical Biology and Medicine. 2012;52(3):699–704. doi: 10.1016/j.freeradbiomed.2011.11.004. 22137893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kagan V.E., Tyurina Y.Y. Recycling and redox cycling of phenolic antioxidants. Annals of the New York Academy of Sciences. 1998;854:425–434. doi: 10.1111/j.1749-6632.1998.tb09921.x. 9928449 [DOI] [PubMed] [Google Scholar]
- 37.Giulivi C., Traaseth N.J., Davies K.J. Tyrosine oxidation products: analysis and biological relevance. Amino Acids. 2003;25(3–4):227–232. doi: 10.1007/s00726-003-0013-0. 14661086 [DOI] [PubMed] [Google Scholar]
- 38.Granold M., Moosmann B., Behl C., Hajieva P. Integral membrane proteins are the predominant site of protein oxidation in the aged CNS and in Alzheimer's disease. Free Radical Biology and Medicine. 2010;49:S155. [Google Scholar]
- 39.Price J.C., Guan S., Burlingame A., Prusiner S.B., Ghaemmaghami S. Analysis of proteome dynamics in the mouse brain. Proceedings of the National Academy of Sciences of the United States of America. 2010;107(32):14508–14513. doi: 10.1073/pnas.1006551107. 20699386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Savas J.N., Toyama B.H., Xu T., Yates J.R., Hetzer M.W. Extremely long-lived nuclear pore proteins in the rat brain. Science. 2012;335(6071):942. doi: 10.1126/science.1217421. 22300851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wu H., Williams J., Nathans J. Complete morphologies of basal forebrain cholinergic neurons in the mouse. Elife. 2014;3:e02444. doi: 10.7554/eLife.02444. 24894464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Page M.M., Richardson J., Wiens B.E. Antioxidant enzyme activities are not broadly correlated with longevity in 14 vertebrate endotherm species. Age (Dordr) 2010;32(2):255–270. doi: 10.1007/s11357-010-9131-2. 20431992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Braak H., Braak E. Frequency of stages of Alzheimer-related lesions in different age categories. Neurobiology of Aging. 1997;18(4):351–357. doi: 10.1016/s0197-4580(97)00056-0. 9330961 [DOI] [PubMed] [Google Scholar]