Abstract
Aims
Within 12-step mutual-help organizations (MHOs), a sponsor plays a key recovery-specific role analogous to a ‘lay therapist’, serving as a role model, support and mentor. Research shows that attendees who have a sponsor have higher rates of abstinence and remission from substance use disorder (SUD), yet, while myriad formal psychotherapy studies demonstrate the therapeutic significance of the alliance between patients and professional clinicians on treatment outcomes, very little is known about the influence of the ‘therapeutic alliance’ between 12-step members and their sponsor. Greater knowledge about this key 12-step relationship could help explain greater degrees of 12-step effects. To bridge this gap, this study sought to develop and test a measure assessing the 12-step sponsee–sponsor therapeutic alliance—the Sponsor Alliance Inventory (SAI).
Method
Young adults (N = 302) enrolled in a prospective effectiveness study who reported having a 12-step sponsor during the study (N = 157) were assessed at treatment entry, and 3, 6 and 12 months later on the SAI, their 12-step MHO attendance, involvement and percent days abstinent (PDA).
Results
Principal axis extraction revealed a single, 10-item, internally consistent (α's ≥ 0.95) scale that explained the majority of variance and was largely invariant to primary substance, gender and time. Criterion validity was also supported with higher SAI scores predicting greater proximal 12-step attendance, involvement and PDA.
Conclusion
The SAI may serve as a brief, valid measure to assess the degree of sponsee–sponsor ‘therapeutic alliance’ within 12-step communities and may help augment explanatory models estimating the effects of MHOs on recovery outcomes.
INTRODUCTION
The extent to which clinicians and patients agree on the goals, tasks, activities and pacing of treatment has been termed the ‘working’, ‘helping’ or ‘therapeutic’ alliance (Barrett-Lennard, 1962; Luborsky et al., 1988; Wampold et al., 2001). In the general psychotherapy literature (Horvath and Luborsky, 1993; Wampold et al., 2001) as well as the addiction-specific clinical literature (Beutler et al., 1994; Moos, 2007; Urbanoski et al., 2012; Kiluk et al., 2014), this common treatment relationship factor is deemed vital to treatment effectiveness because it is purported to create the necessary climate and conditions in which other intervention contents, from whichever specific theoretical orientation, can be successfully delivered and absorbed by the patient (Luborsky et al., 1988; Wampold et al., 2001). There is much empirical evidence too that supports the value of establishing a strong therapeutic patient–clinician alliance as this contextual factor has been strongly associated with enhancing treatment engagement, compliance and substance use outcomes independent of the presumed ‘active’ ingredients of treatment, such as teaching of coping skills (Orlinsky et al., 2004).
As the management of addiction is increasingly accepted as a chronic illness (McLellan et al., 2000; Kelly and White, 2011), and with an increase in awareness of the potential health-care cost offset potential of engaging patients suffering from substance use disorder (SUD) with free community-based recovery mutual-help organizations (MHOs), such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) to support long-term recovery (Humphreys and Moos, 2001; Kelly and Yeterian, 2012), a common clinical continuing care recommendation in the USA, and increasingly in the UK and other countries (Hacker and Walker, 2013; Maust et al., 2013; Public Health England, 2013), is to link patients with MHOs (Weisner et al., 1995; Greenfield et al., 1998; Kelly and Yeterian, 2013; SAMHSA, 2013). In addition to recommending regular 12-step meeting attendance, another common suggestion is to obtain an AA or NA ‘sponsor’. A sponsor is a fellow 12-step MHO attendee who is typically in long-term stable recovery from SUD and who agrees to serve as a recovery role model and supportive guide. These individuals often make themselves available 24 h a day in order to support other members through the challenges of early recovery and beyond (Alcoholics Anonymous, 1976). Highlighting the significance of sponsors within AA, data from AA's own surveys estimate that 80% of AA members have a current sponsor, and 72% obtained a sponsor within the first 90 days of attending AA (AA, 2012).
From an outsider's perspective, these non-professional sponsors might be considered ‘lay therapists' and the 12-step MHO equivalent of the professional treatment clinician. They possess the lived experience of addiction and recovery and can serve as a role model for success, share personal recovery experiences, and communicate and demonstrate explicit recovery skills that can boost newcomers' confidence in their ability to stay sober (Tonigan and Rice, 2010; Kelly and Yeterian, 2012). Despite the numerous studies that show a benefit for having a sponsor (Bond et al., 2003; Kelly and Urbanoski, 2012; Witbrodt et al., 2012), especially during early AA affiliation (Emrick et al., 1993; Tonigan and Rice, 2010), such studies have typically only measured the presence or absence of a sponsor; more nuanced assessment of the quality of sponsorship, however, may help elucidate more of the impact and directionality of the relationship between having a sponsor and greater abstinence. Yet, there is currently very little information regarding the sponsee–sponsor ‘therapeutic bond’. A lingering question, therefore, has been whether the therapeutic bond in peer-led MHOs carries similar benefit to that shown in studies of professional treatment. If so, this could help explain a significant proportion of the effect of AA and similar MHOs on remission and recovery outcomes. No measures currently exist, however, to assess this unique aspect of this critically important 12-step MHO relationship. To develop and validate such a measure is the principal aim of the current investigation.
Participants
Participants in the original study from which the sample used in the current analysis was drawn were young adults (N = 302; 18–24 years old) enrolled in a prospective study of residential SUD treatment effectiveness (see Kelly et al., 2012 for more details). For the purposes of the current analyses, we excluded individuals who did not report having a 12-step sponsor (n = 100) and/or did not complete the Sponsor Alliance Inventory (SAI) (n = 131) at any of the post-treatment assessments, which resulted in a final analytical sample of n = 157.
At admission, these participants were 20.5 years old on average (SD = 1.56). Most were Caucasian (96.8%), male (70.7%), and all were single. The most commonly reported primary substance of use at treatment intake was alcohol (31.0%), followed by marijuana (23.2%), heroin or other opiates (21.3%), stimulants (19.4%) and other drugs (5.2%).
In terms of national treatment representativeness of the current sample, participants in this private treatment sample were more likely to be Caucasian than young adults (18–24 years old) in public sector residential treatment (76%) (SAMHSA, 2006) or adults (18+ years old) in the broader private treatment sector (71%) (Roman and Johnson, 2004). They were, however, comparable in terms of gender, marital status and employment status, suggesting that the results are broadly generalizable to youth treated for substance-related disorders in the USA. Regarding payment source, 61% of treatment funding was from insurance reimbursement and 35% from family. Also, 34% of the sample came from households below the US median household income of $50,221; half of our sample came from households below $56,000.
Treatment
Treatment was comprehensive and multifaceted, based in a 12-step philosophy of recovery. In addition to the 12-step orientation, motivational enhancement and cognitive-behavioral therapeutic approaches, as well as family therapy, were used to facilitate problem recognition and treatment engagement and to support recovery. Programming included clinical assessment, individual and group therapy, and a host of specialty groups tailored to meet the needs of individual clients (e.g. relapse prevention, anger management). Integrated mental health care was available, including clinical assessment, therapy and medication management.
Participants' average length of stay at the residential treatment center was 27.0 days (SD = 3.8, ranging from 6 to 35 days). The majority (94.9%) were discharged with staff approval, indicating a high rate of treatment completion.
Procedure
Participants were enrolled in the study shortly after admission. A total of 607 young adults were admitted to treatment during the recruitment period (October 2006 to March 2008). All of those aged 21–24 years were approached for study enrollment, as well as every second individual aged 18–20 years to ensure sufficient representation of the older age group, given the predominance of those aged 18–20 years at the treatment center. A small number of potential participants left treatment before recruitment could take place (n = 6) or were not approached by staff for recruitment (n = 14). Totally, 302 individuals consented to participate, representing 78.6% of those approached for participation.
Research staff conducted assessments at baseline, 3, 6 and 12 months post-discharge. Each assessment included an interview portion and self-administered survey. Participants were reimbursed $30 for the baseline assessment and $30, $40 and $50 for the post-treatment assessments at 3, 6 and 12 months, respectively. Assessment completion rates in this subsample were 93.6%, 91.7% and 93.6% at the 3-, 6- and 12-month follow-ups, respectively.
At each time point, those who did not complete the assessment were compared with those who were retained in terms of demographic and clinical characteristics. Relative to those with post-secondary education, those with a high school education or less were more likely to be missed at all time points. Additionally, participants that did report a sponsor, but did not complete the SAI post-treatment, had significantly lower percent days abstinent (PDA) relative to those that did complete the SAI.
The study was conducted in accordance with the Institutional Review Board (IRB) at Schulmann Associates, an independent review board, and all participants signed informed consent documents.
Measures
Background sociodemographic information, including age, gender, marital status, race and ethnicity, employment status, educational attainment and student status, was obtained, with full permission, from the medical record.
Structured Clinical Interview for DSM-IV-TR (SCID): The SCID (First et al., 2002) was conducted by trained personnel at baseline to assess Axis I diagnoses. To ensure inter-rater reliability, supervisory reviews of audiotaped SCID interviews were conducted on all assessments during the first month of data collection and for two randomly chosen interviews each week thereafter.
Form-90: The Form-90 (Project MATCH Research Group, 1993; Miller and Del Boca, 1994) is an interview-based measure capturing substance use, use of psychiatric medications, criminal justice system and treatment involvement, and consequences related to work or school. The recall period for the baseline interviews was 90 days. Modifications were made to subsequent assessments to capture the entire time period elapsed since the previous interview (i.e. averaging 60 days for the 3-month follow-up, 90 days for the 6-month follow-up and 180 days for the 12-month follow-up). However, a subsample (n = 35) completed an interview subsequent to missing one and, thus, reported over a longer than average period of time assessment window (e.g. they missed the 6-month assessment and reported on activities between 3- and 12-month follow-up interviews). The primary outcome measure derived from this instrument was percentage of days abstinent (PDA). The Form-90 has been tested with adult and adolescent samples and has demonstrated test–retest reliability and validity (Tonigan et al., 1997; Slesnick and Tonigan, 2004).
Sponsor Alliance Inventory (SAI): Adapted from the Working Alliance Inventory-Short Form, WAI-S (Horvath and Greenberg, 1989; Busseri and Tyler, 2003), the SAI was used to assess client perspectives of the sponsor alliance at each post-discharge assessment. The WAI-S consists of 12 items that assess the degree to which patients perceive commonality and mutual trust between themselves and their professional therapists/counselors in terms of common therapeutic goals and whether their therapist likes them. The WAI-S was used as a starting point for the current SAI instrument because 12-step MHOs have been found to possess therapeutic similarities to formal treatment interventions (e.g. they mobilize and enhance similar mechanisms such as coping skills, self-efficacy and recovery motivation and are run in group formats; Kelly and Yeterian, 2013). Consequently, for the purposes of this study, these 12 items were reworded to capture the same elements of the therapeutic alliance, but from a 12-step MHO perspective. To achieve this, 12-step literature, prior relevant research studies, and patients and staff with 12-step experience were consulted to construct 12-step-specific item wording for the SAI. Thus, an original item such as ‘My therapist and I agree about the things I will need to do in therapy to improve my situation’ was changed to ‘My sponsor and I agree about the things I will need to do in AA/NA to improve my situation’ and the original WAI-S item ‘I believe my therapist likes me’ was changed to say ‘I believe my sponsor likes me’. (See Table 2 for a listing of the wording used in the final SAI.) As in the original WAI-S, each of the 12 items is rated from 1 to 7 capturing the extent to which each item applies to the sponsee (1 = ‘Never’ to 7 = ‘Always'). Subsequently, all items are summed to provide a total score ranging from 12 to 84 (higher scores indicating a more positive alliance with a 12-step sponsor). Two items are reverse coded: ‘My sponsor does not understand what I am trying to accomplish in AA/NA’ and ‘My sponsor and I have different ideas on what my problems are.’
Table 2.
Descriptive characteristics by drug of choice and gender (n = 157)
| n | M Age | % Male | Median SAI (3 months) | Median SAI (6 months) | Median SAI (12 months) | |
|---|---|---|---|---|---|---|
| Primary substance | ||||||
| Alcohol | 45 | 20.78 | 57.78 | 55.50 | 54.00 | 64.00 |
| Cannabis | 36 | 20.25 | 77.78 | 59.00 | 65.00 | 65.00 |
| Opiates | 33 | 20.70 | 75.76 | 60.00 | 60.00 | 61.50 |
| Stimulants | 30 | 20.03 | 76.67 | 63.00 | 61.00 | 64.00 |
| Other | 8 | 20.50 | 75.00 | 59.00 | 62.00 | 59.50 |
| Gender | ||||||
| Male | 108 | 20.57 | 58.00 | 60.00 | 61.00 | |
| Female | 45 | 20.24 | 61.00 | 62.00 | 66.50 | |
| Total | 153 | 20.48 | 70.59 | 54.17 | 54.17 | 56.67 |
Not all participants reported drug of choice.
‘Other’ drug of choice includes benzodiazepines, DXM, TCB, painkillers and polydrug users.
Twelve-Step Affiliation: The Multidimensional Mutual Help Activity Scale is a 32-item, interview-based index assessing several dimensions of involvement in 12-step, mutual-help groups. Responses for each item are provided separately for four types of 12-step groups: AA, NA, Cocaine Anonymous (CA) and ‘other’, which can be specified by respondents. Items tap frequency of attendance, as well as level of involvement (i.e. contact with sponsor and other members, step work, reading 12-step literature, and speaking at meetings), perceived importance and helpfulness of the groups to recovery, perceived safety at meetings and degree of legally mandated participation. The measure has shown to have excellent content validity and internal consistency and predictive validity in young adults (Kelly et al., 2012).
Biological assay
To verify self-reported abstinence from alcohol and other drugs, saliva tests (Cone et al., 2002) were administered on a subsample of subjects that lived within 50 miles of the treatment facility and could attend follow-up interviews in-person. Abstinence was confirmed in 94.5–100% of subjects who self-reported abstinence from all substances during the assessment period prior to each follow-up. Positive tests results were obtained for three subjects who reported abstinence prior to the 1-month follow-up and one subject who reported abstinence prior to the 3-month follow-up. These participants were excluded from the analyses.
Data analysis plan
We first evaluated the proportion of the entire sample that reported a sponsor at baseline and post-treatment assessments, respectively. We then assessed the proportion of the sample that completed the SAI at each post-treatment assessment. Subsequently, factor structure and internal consistency measures were examined at each time point to assess factorial invariance. Although orthogonal rotation of factors is common in the social sciences (e.g. Varimax rotation) due to ease of interpretation, this method assumes that the factors are uncorrelated. Given that most phenomena are correlated in the social sciences, oblique rotations are considered optimal (Costello and Osborne, 2005). Consequently, we chose an oblique Promax rotation.
We then examined the SAI measures of central tendency and dispersion at each time point and determined that SAI was moderately negatively skewed at all time points (Fig. 1). Accordingly, we used non-parametric Mann–Whitney and Kruskal–Wallis tests to examine SAI differences across patients' primary substance at treatment entry and gender. We then conducted the Spearman rank order (non-parametric) correlations between SAI, percent days attending a 12-step meeting (PDATSM), 12-step involvement and PDA across all time points.
Fig. 1.
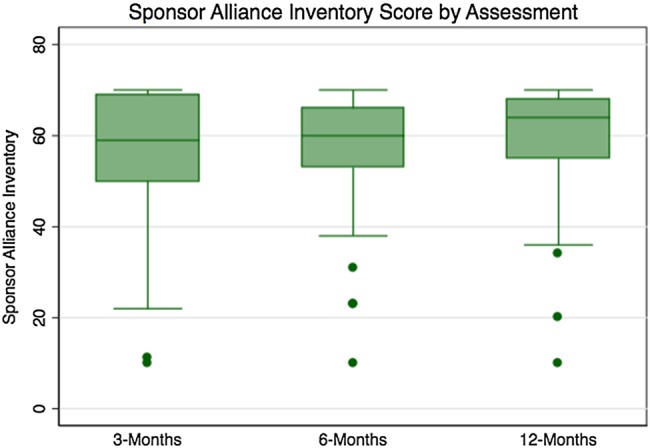
Distributions of SAI scores by assesment time points.
Finally, given that we expected higher SAI scores to be predictive of greater 12-step attendance, involvement and PDA, we evaluated criterion validity by examining the relationship between SAI and both contemporaneous and prospective PDATSM, 12-step involvement and PDA using multivariate linear regression models adjusted for the predictor of study attrition (i.e. education) and the predictor of SAI-eligible non-completers (i.e. baseline PDA). Contemporaneous regression models evaluated the association between SAI and the outcomes of interest at 3, 6 and 12 months. Prospective regression models used a lagged design to establish temporality by regressing 3-month SAI on 6-month outcomes and similarly regressing 6-month SAI on 12-month outcomes. All analyses were generated using SAS (Version 9.2. Copyright © 2002–2008, SAS Institute, Inc., Cary, NC, USA).
RESULTS
Prevalence of 12-step sponsorship and SAI completion
At baseline, 13.6% of the sample reported having a 12-step sponsor. This proportion increased to 65.3%, 61.0% and 57.0% at 3, 6 and 12 months post-treatment, respectively. Between 43.3% and 44.0% of the sample completed the SAI at the post-treatment assessments. As described in the methods, participants reporting a sponsor, but not completing the SAI at any post-treatment assessment, had significantly fewer PDA compared with participants that reported a sponsor and completed the SAI at one or more post-treatment assessments.
SAI factor structure and internal consistency
The principal axis factoring extraction initially produced a single 12-item factor. Based on low factor loadings and lack of internal consistency, however, we removed the two reverse-coded items from the scale, which markedly improved internal consistency. The modified factoring extraction (10 items) yielded a robust, single interpretable factor that was consistent across time points accounting for 75.8%, 71.8% and 70.2% of the variance at 3, 6, and 12 months, respectively. Consequently, no factor rotation was necessary. Loadings were all of high magnitude and ranged from 0.718 (Item 5 at 6 months) to 0.921 (Item 4 at 3 months) (Table 1). The internal consistency for a single factor was also very high and ranged from α = 0.95 at 12 months to α = 0.96 at 3 and 6 months. The internal consistency did not appreciably change when any one item was removed. As a consequence, the range of potential scores on the SAI is 10–70.
Table 1.
Individual SAI item loading and internal consistencies across time points
| Item | Factor 1 |
||
|---|---|---|---|
| 3 months | 6 months | 12 months | |
| 1. My sponsor and I agree about the things I will need to do in AA/NA to help improve my situation. | 0.859 | 0.892 | 0.784 |
| 2. What I am doing in AA/NA gives me new ways of looking at my problem. | 0.720 | 0.718 | 0.804 |
| 3. I believe my sponsor likes me. | 0.831 | 0.862 | 0.692 |
| 4. I am confident in my sponsor's ability to help me. | 0.921 | 0.891 | 0.877 |
| 5. My sponsor and I are working towards mutually agreed upon goals. | 0.899 | 0.811 | 0.879 |
| 6. I feel that my sponsor appreciates me. | 0.910 | 0.854 | 0.880 |
| 7. We agree on what is important for me to work on. | 0.910 | 0.877 | 0.920 |
| 8. My sponsor and I trust one another. | 0.886 | 0.892 | 0.889 |
| 9. We have established a good understanding of the kind of changes that would be good for me. | 0.903 | 0.818 | 0.762 |
| 10. I believe the way we are working with my problem is correct. | 0.850 | 0.843 | 0.865 |
| Total variance Explained by Factor | 75.80% | 71.81% | 70.20% |
| Cronbach's α (10 items) | 0.96 | 0.96 | 0.95 |
Factor 1: Items 1, 2, 3, 5, 6, 7, 8, 9, 11 and 12.
SAI scores by gender and drug of choice
When stratified, we found that there were no significant differences in SAI at 3 months by drug of choice or gender (P > 0.05). At 6 months, people reporting alcohol as their drug of choice had significantly lower SAI relative to the other drug of choice groups (F = 11.32, P = 0.023). There were no significant differences in SAI score between males and females at 6 months (P > 0.05). Similar to the results found at 3 months, there were no significant differences in SAI score by drug of choice or gender at 12 months (Table 2). Average SAI scores were not significantly different between time points (P > 0.05).
Criterion validity
The Spearman rank order correlations show that SAI scores were significantly correlated with each other across time. With regard to the correlation between SAI and the outcomes of interest, SAI scores at 3 months were found to be correlated with 12-step attendance concurrently and prospectively at 12 months as well as PDA at 3 and 6 months. SAI scores at 6 months were correlated with 12-step attendance at all time points, 12-step involvement at 6 and 12 months, and PDA at 6 and 12 months. SAI scores at 12 months were associated with 12-step attendance at all time points, 12-step involvement at 6 and 12 months, and PDA at 3 and 12 months (Table 3).
Table 3.
The Spearman correlation between SAI, 12-step attendance and PDA during the year following residential treatment
| n | Mean | SD | Median | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. SAI (3 months) | 99 | 56.10 | 13.84 | 59.00 | 0.60*** | 0.51*** | 0.27** | 0.19 | 0.29** | 0.14 | 0.14 | 0.15 | 0.27** | 0.24* | 0.15 |
| 2. SAI (6 months) | 95 | 57.92 | 11.81 | 60.00 | 0.58*** | 0.24* | 0.22* | 0.28** | 0.21 | 0.25* | 0.25* | 0.19 | 0.27** | 0.20* | |
| 3. SAI (12 months) | 92 | 59.76 | 11.44 | 64.00 | 0.25* | 0.26* | 0.28** | 0.16 | 0.24* | 0.31** | 0.31** | 0.16 | 0.39*** | ||
| 4. PDATSM (3 months) | 143 | 61.91 | 13.84 | 57.14 | 0.52*** | 0.37*** | 0.31*** | 0.27** | 0.32*** | 0.33*** | 0.21* | 0.26** | |||
| 5. PDATSM (6 months) | 141 | 50.86 | 30.91 | 45.28 | 0.51*** | 0.05 | 0.48*** | 0.41*** | 0.27** | 0.38*** | 0.30*** | ||||
| 6. PDATSM (12 months) | 143 | 37.40 | 28.66 | 37.17 | 0.08 | 0.37*** | 0.62*** | 0.19* | 0.20* | 0.38*** | |||||
| 7. Involvement (3 months) | 146 | 6.94 | 1.27 | 7.00 | 0.21* | 0.13 | 0.10 | 0.07 | 0.10 | ||||||
| 8. Involvement (6 months) | 144 | 6.60 | 2.12 | 7.00 | 0.39*** | 0.26** | 0.32*** | 0.23** | |||||||
| 9. Involvement (12 months) | 147 | 6.20 | 2.59 | 7.00 | 0.26** | 0.20* | 0.44*** | ||||||||
| 10. PDA (3 months) | 147 | 96.78 | 11.49 | 100.00 | 0.46*** | 0.41*** | |||||||||
| 11. PDA (6 months) | 144 | 91.95 | 21.44 | 100.00 | 0.61*** | ||||||||||
| 12. PDA (12 months) | 147 | 87.07 | 25.82 | 100.00 |
*P < 0.05, **P < 0.01, **P < 0.001.
To account for the possibility of bias due to attrition and SAI non-completion, we constructed regression models that evaluated the relationship between SAI and 12-step attendance, involvement and PDA while controlling for education (predictor of attrition), baseline PDA (predictor of SAI non-completion) and baseline levels of the outcome. Results from the contemporaneous analyses revealed that 3-month SAI was associated with increased levels of 12-step attendance, involvement and PDA at 3 months. At 6 months, SAI was significantly associated with increased 12-step attendance and involvement. Finally, at 12 months, SAI was associated with all outcomes of interest: 12-step attendance, 12-step involvement and PDA (Table 4). Results from the lagged models showed only that SAI at 6 months was associated significantly with increased 12-step attendance and increased 12-step involvement at 12 months (Table 5).
Table 4.
Criterion validity: SAI predicting contemporaneous attendance, involvement and PDAa,b
| Percent days attendance |
Involvement |
PDA |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | t | P | B | SE | t | P | B | SE | t | P | |
| 3 months | ||||||||||||
| SAI | 0.077 | 0.031 | 2.48 | 0.015 | 0.055 | 0.026 | 2.14 | 0.035 | 0.272 | 0.091 | 2.98 | 0.004 |
| 6 months | ||||||||||||
| SAI | 0.103 | 0.033 | 3.12 | 0.002 | 0.063 | 0.031 | 2.04 | 0.044 | 0.242 | 0.132 | 1.84 | 0.069 |
| 12 months | ||||||||||||
| SAI | 0.081 | 0.032 | 2.52 | 0.014 | 0.230 | 0.044 | 5.21 | 0.000 | 0.684 | 0.156 | 4.38 | 0.000 |
aNote: Attendance and involvement were square root transformed; PDA was transformed using neg.log.
bControlling for education, baseline PDA and baseline levels of the outcome.
Table 5.
Criterion validity: SAI predicting lagged attendance, involvement and PDAa,b
| Percent days attendance |
Involvement |
PDA |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | t | P | B | SE | t | P | B | SE | t | P | |
| 3-month SAI -> 6-month DV | ||||||||||||
| SAI | 0.072 | 0.037 | 1.93 | 0.057 | 0.026 | 0.081 | 0.32 | 0.747 | 0.149 | 0.178 | 0.84 | 0.405 |
| 6-month SAI -> 12-month DV | ||||||||||||
| SAI | 0.089 | 0.033 | 2.73 | 0.008 | 0.185 | 0.083 | 2.23 | 0.028 | 0.228 | 0.170 | 1.34 | 0.183 |
aNote: Attendance and Involvement were square root transformed; PDA was transformed using neg.log.
bControlling for education, baseline PDA and baseline levels of the outcome.
DV, dependent variable.
DISCUSSION
A key therapeutic feature of 12-step MHOs is the sponsor. Research indicates having a sponsor is associated with better recovery outcomes, yet, despite the preponderance of research investigating the therapeutic alliance between a patient and clinician in the professional literature, there are no published measures or studies examining the sponsee–sponsor therapeutic relationship within ubiquitous 12-step MHOs. This study is the first to develop and test a measure of the therapeutic alliance between 12-step members and their sponsors. Findings revealed a brief, robust, 10-item scale with high internal consistency reliability and good criterion validity. Findings suggest that this scale may be useful in helping to elucidate the impact of the sponsee–sponsor relationship within 12-step MHOs and thus may help explain greater variability relating to 12-step benefit.
The SAI items were constructed in a straightforward manner to capture 12-step-specific elements of the sponsee–sponsor therapeutic alliance. Factor analyses consistently produced a single factor capturing the majority of the variance across administrations. This consistency suggests a single underlying dimension that is successfully captured by the SAI. Further analyses revealed that the reverse-coded items from the measure detracted from its reliability and were removed. This adjustment resulted in a briefer, 10-item measure with internal consistency coefficients above 0.95 across administrations. Tests of the SAI across different subgroups of gender and primary substance, as well as across time, found that the instrument was robust with one exception at the 6-month follow-up for those reporting alcohol as their primary substance. It is conceptually unclear why this anomaly occurred for this substance at this particular time point; future research may clarify this occurrence. On the whole, however, findings suggest that the SAI is a reliable instrument that may be used across different genders, primary substances and across time.
The distribution of the SAI was moderately negatively skewed across administrations with the majority reporting a positive alliance. This makes sense given that 12-step members are free, in theory, to choose and change sponsors at will if a poor match is perceived or the relationship becomes strained or fractured. That said, it may not be easy for newer members to be assertive enough to change sponsors, and such individuals may linger in a less than ideal sponsor–sponsee relationship for some time before changing. While SAI variability may be somewhat limited by this general ability within 12-step MHOs to change sponsors in order to maximize the chances of a good alliance, we discovered, nonetheless, enough variability across the SAI to predict consistent and meaningful relationships with other theoretically linked variables (i.e. greater SAI was associated with greater 12-step attendance, involvement and PDA). We did not assess how long individuals had sponsors for, or whether they were reporting on the same sponsor over time or different ones. These and many other questions need to be investigated in future research including the frequency and intensity of contact over time, average length of time with the same sponsor, predictors and consequences of sponsor changes and qualitative work investigating the many styles of sponsoring other members as well as experiences of being sponsored.
The criterion validity tests that examined the ability of the SAI to predict attendance, involvement and PDA found higher sponsee–sponsor alliance scores predicted greater 12-step attendance and involvement, and more abstinence within the same 90-day period. These findings suggest that the SAI has merit as a measure capturing conceptually meaningful 12-step MHO empirical relationships. The lack of predictive finding for the SAI predicting outcomes in the following time periods (i.e. lagged models) suggest either the sponsee–sponsor relationship, or the SAI measure itself, has more near term, proximal relevance. More specifically, the effect of having a good relationship with a sponsor is likely to affect other conceptually relevant behaviors within the same 90-day period as opposed to beyond 90 days. Future research with more frequent assessment capturing finer temporal resolutions (e.g. monthly or weekly SAI measurement) may clarify how long exactly any therapeutic benefits of a good sponsee–sponsor relationship might last.
LIMITATIONS
Findings from this study should be made cautiously in light of certain limitations regarding the nature of the young adult treatment-seeking sample and the nature and construction of the instrument itself. The sample comprised mostly of male, White, young adults. The young age of the participants may mean that many were entering recovery for the first time and sponsors were likely older; this may affect the current observed estimates of relationships among the SAI and other variables. Participants were also from a single residential, 12-step-oriented treatment program that would have prepared participants about the nature of sponsorship. The measure should be tested in other samples to confirm its factorial invariance, reliability and criterion validity. The SAI was adapted in a relatively straightforward way from an existing measure intended to capture the patient–therapist alliance in a professional context; the sponsee–sponsor alliance in 12-step MHOs may contain other 12-step-specific elements that are not captured in the SAI. Also, we found that the two reverse-coded items in the SAI were those that did not load in our factor analysis. Rather than being due to a true lack of fit with the underlying latent construct that was captured by the rest of the scale items, it is possible that at least some of this observed lack of fit is due to an acquiescent responding bias (i.e. measurement error). Specifically, at least some participants may have rated these reverse-coded items in the same direction as the majority of the other items in the scale. In addition, we only captured the nature of the sponsor–sponsee dyadic relationship from the sponsee's perspective. As with the original WAI, it may be useful for future research to examine sponsor–sponsee SAI concordance or discordance and any related differential predictive validity. While we estimate that the power to detect moderate-size effects was adequate (>0.80), the relatively small sample size of 157 individuals reporting a 12-step sponsor could affect the precision of observed estimates. Finally, not all individuals that reported having a sponsor completed the SAI and those that did not complete the SAI had significantly fewer PDA at follow-up. While this finding was factored into analyses (i.e. we controlled for PDA), there may be other ways in which these individuals differed that were not captured.
CONCLUSIONS
MHOs are the most commonly sought source of help for alcohol and other drug problems in the USA and are growing in the UK and internationally. Evidence indicates that these resources serve as cost-effective recovery aids for many in need of ongoing recovery monitoring and management and that the therapeutic mechanisms mobilized and enhanced by 12-step MHO participation are similar to those mobilized by formal professional treatment (e.g. recovery-focused coping skills, self-efficacy and recovery motivation; Kelly and Yeterian, 2013). The AA/NA sponsor, therefore, might be considered a lay therapist analogous to the professional addiction therapist or counselor, and the professional therapeutic alliance has been found to be a robust predictor of treatment engagement and outcome in the clinical realm. This study provides preliminary evidence that the same construct can be measured reliably in the MHO realm, and the SAI may serve as a useful tool to help capture and explicate more of the nature and scope of 12-step-related benefit.
FUNDING
This study was supported by funding from the U.S. National Institute of Alcohol Abuse and Alcoholism (R21AA018185 A102) and by an anonymous donation to the Hazelden Betty Ford Foundation in Minnesota, USA.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- Alcoholics Anonymous. (1976) Questions and Answers on Sponsorship. New York: Alcoholics Anonymous World Services; Available at: http://www.aa.org/assets/en_US/p-15_Q&AonSpon.pdf. [Google Scholar]
- Barrett-Lennard GT. (1962) Dimensions of therapist response as causal factors in therapeutic change. Psychol Monogr 76:1–36. [Google Scholar]
- Beutler LE, Patterson KM, Jacob T, et al. (1994) Matching treatment to alcoholism subtypes. Psychotherapy 30:463–72. [Google Scholar]
- Bond J, Kaskutas LA, Weisner C. (2003) The persistent influence of social networks and Alcoholics Anonymous on abstinence. J Stud Alc 64:579–88. [DOI] [PubMed] [Google Scholar]
- Busseri MA, Tyler JD. (2003) Interchangeability of the Working Alliance Inventory and Working Alliance Inventory, Short Form. Psychol Assess 15:193–7. [DOI] [PubMed] [Google Scholar]
- Cone EJ, Presley L, Lehrer M, et al. (2002) Oral fluid testing for drugs of abuse: positive prevalence rates by Intercept immunoassay screening and GC–MS–MS confirmation and suggested cutoff concentrations. J Anal Toxicol 26:541–6. [DOI] [PubMed] [Google Scholar]
- Costello AB, Osborne J. (2005) Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess Res Eval 10:1–10. Available online: http://pareonline.net/getvn.asp?v=10&n=7. [Google Scholar]
- Emrick CD, Tonigan JS, Montgomery H, et al. (1993) Alcoholics Anonymous: what is currently known? In McCrady BS, Miller WR. (eds). Research on Alcoholics Anonymous: Opportunities and Alternatives. Piscataway, NJ: Rutgers Center of Alcohol Studies, 41–76. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, et al. (2002) Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P). New York: Biometrics Research, New York State Psychiatric Institute. [Google Scholar]
- Greenfield SF, Weiss RD, Muenz LR, et al. (1998) The effect of depression on return to drinking: a prospective study. Arch Gen Psychiatry 55:259–65. [DOI] [PubMed] [Google Scholar]
- Hacker K, Walker DK. (2013) Achieving population health in accountable care organizations. Am J Public Health 103:1163–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath AO, Greenberg LS. (1989) Development and validation of the working alliance inventory. J Couns Psychol 36:223–33. [Google Scholar]
- Horvath AO, Luborsky L. (1993) The role of the therapeutic alliance in psychotherapy. J Consult Clin Psychol 61:561–73. [DOI] [PubMed] [Google Scholar]
- Humphreys K, Moos R. (2001) Can encouraging substance abuse patients to participate in self-help groups reduce demand for health care? A quasi-experimental study. Alcohol Clin Exp Res 25:711–6. [PubMed] [Google Scholar]
- Kelly JF, Urbanoski K. (2012) Youth recovery contexts: The incremental effects of 12-step attendance and involvement on adolescent outpatient outcomes. Alcohol Clin Exp Res 36:1219–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, White WL. (eds). (2011) Addiction Recovery Management: Theory, Research, and Practice. New York: Spring Science+Business Media. [Google Scholar]
- Kelly JF, Yeterian JD. (2012) Empirical awakening: the new science on mutual help and implications for cost containment under health care reform. Subst Abus 33:85–91. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Yeterian JD. (2013) Mutual-help groups for alcohol and other substance use disorders. In McCrady BS, Epstein EE. (eds). Addictions a Comprehensive Guidebook. New York, NY: Oxford University Press. [Google Scholar]
- Kelly JF, Urbanoski KA, Hoeppner BB, et al. (2012) “Ready, willing, and (not) able” to change: young adults’ response to residential treatment. Drug Alcohol Depend 121:224–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiluk BD, Serafini K, Frankforter T, et al. (2014) Only connect: The working alliance in computer-based cognitive behavioral therapy. Behav Res Ther 63:139–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luborsky L, Crits-Christoph P, Mintz J, et al. (1988) Who Will Benefit from Psychotherapy?: Predicting Therapeutic Outcomes. New York: Basic Books. [Google Scholar]
- Maust DT, Oslin DW, Marcus SC. (2013) Mental health care in the accountable care organization. Psychiatr Serv 64:908–10. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O'Brien CP, et al. (2000) Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA 284:1689–95. [DOI] [PubMed] [Google Scholar]
- Miller WR, Del Boca FK. (1994) Measurement of drinking behavior using the Form 90 family of instruments. J Stud Alcohol Suppl 12:112–8. [DOI] [PubMed] [Google Scholar]
- Moos RH. (2007) Theory-based active ingredients of effective treatments for substance use disorders. Drug Alcohol Depend 88:109–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orlinsky DE, Rønnestad MH, Willutzki U. (2004) Fifty years of psychotherapy process-outcome research: continuity and change. In Lambert MJ. (ed). Bergin and Garfield's Handbook of Psychotherapy and Behavior Change. 5th edn New York: Wiley, 307–90. [Google Scholar]
- Project MATCH Research Group. (1993) Project MATCH (Matching Alcoholism Treatment to Client Heterogeneity): rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcohol Clin Exp Res 17:1130–45. [DOI] [PubMed] [Google Scholar]
- Public Health England. (2013) Mutual Aid Assessment Tool. Alcohol and Drug Recovery. London, UK: Public Health England, PHE. [Google Scholar]
- Roman PM, Johnson JA. (2004) National Treatment Center Study Summary Report: Private Treatment Centers. Athens, GA: Institute for Behavioral Research, University of Georgia. [Google Scholar]
- Slesnick N, Tonigan JS. (2004) Assessment of alcohol and other drug use by runaway youths: a test-retest study of the Form 90. Alcohol Treat Q 22:21–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2006) Characteristics of Young Adult (Aged 18-25) and Youth (Aged 12-17) Admissions: 2004. DASIS Series, Issue 21. Office of Applied Studies, Rockville, MD [http://archive.samhsa.gov/data/2k6/youngTX/youngTX.htm]. Accessed 12 October 2013.
- Substance Abuse and Mental Health Services Administration. (2013) Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. NSDUH Series H-46, HHS Publication No. SMA 13-4795. Office of Applied Studies, Rockville, MD.
- Tonigan JS, Rice SL. (2010) Is it beneficial to have an alcoholics anonymous sponsor? Psychol Addict Behav 24:397–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonigan JS, Miller WR, Brown JM. (1997) The reliability of Form 90: an instrument for assessing alcohol treatment outcome. J Stud Alcohol 58:358–64. [DOI] [PubMed] [Google Scholar]
- Urbanoski KA, Kelly JF, Hoeppner BB, et al. (2012) The role of therapeutic alliance in substance use disorder treatment for young adults. J Subst Abuse Treat 43:344–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wampold BE, Ahn H, Coleman HLK. (2001) Medical model as metaphor: old habits die hard. J Couns Psychol 48:268–73. [Google Scholar]
- Weisner C, Greenfield T, Room R. (1995) Trends in the treatment of alcohol problems in the US general population, 1979 through 1990. Am J Public Health 85:55–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witbrodt J, Kaskutas L, Bond J, et al. (2012) Does sponsorship improve outcomes above Alcoholics Anonymous attendance? A latent class growth curve analysis. Addiction 107:301–11. [DOI] [PMC free article] [PubMed] [Google Scholar]


