Abstract
Background
An adequate bowel preparation is an important quality measure for optimal colonoscopy.
Aims
The aim of this article is to study the burden of bowel preparations by examining seven specific variables (hunger, taste, volume, sleep, social, work, and adverse events (AEs)).
Methods
Ambulatory patients undergoing elective colonoscopy completed a questionnaire regarding their experience with the prescribed preparation. The seven study variables were graded using a numerical scale of 0–10 (best to worst). A score >6 was considered to indicate a significant impact and used as primary outcome. Patients were also asked to grade in descending order what they perceived as the worst aspect of the preparation.
Results
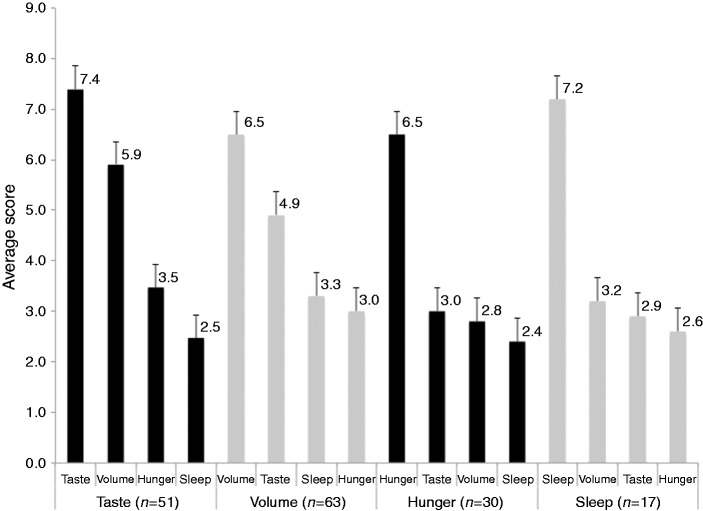
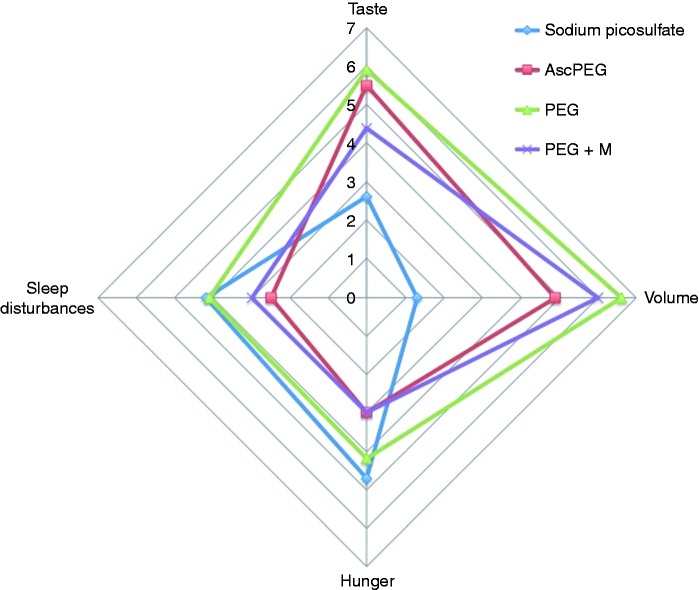
A total of 216 patients completed the survey. Preparations consisted of split-dose sodium picosulfate (SPS) (n = 49), split-dose 4 l PEG ± menthol (n = 49), full-dose PEG (n = 68), and 2 l split-dose PEG + ascorbic acid (n = 50). Except for work and AEs, all variables were considered to have a negative impact by >20% of patients (range 20.4–34.2). SPS was superior to PEG regimens in taste (4.1% vs. 35.9%) and volume (0% vs. 44.9%) (p < 0.05 for both) but inferior for hunger (30.6% vs. 19.2%; p = 0.09). The addition of menthol to PEG significantly improved taste (22.4% vs. 41.5%; p = 0.02). Sleep disturbances were most common with SPS and least with split-dose PEG (30.6% vs. 17.4%; p < 0.05). Overall, patients ranked volume, taste, and hunger as most burdensome.
Conclusions
The burden of bowel preparation is substantial. An informed personalized choice of preparation may improve adherence, tolerability and colon cleansing.
Keywords: Colonoscopy, bowel preparation, quality of life, acceptability, tolerability, adherence
Introduction
Colonoscopy is the current gold standard for colorectal cancer screening because of its high diagnostic sensitivity and specificity and its unique capability to permit sampling and removal of polyps. For optimal performance and visualization of mucosal lesions and details, however, an adequate bowel preparation is essential. Unfortunately, around 20% of bowel preparations are considered suboptimal, resulting in longer examination time, higher adenoma miss rates, earlier repeat examinations and higher cost.1,2 In a recent publication, The United States (US) Multi-Society Task Force on Colorectal Cancer stressed the importance of bowel preparation as a critical quality indicator in colonoscopy. Efficacy, safety and tolerability were recognized as interrelated main factors. Cleansing efficacy was identified as being more important than patient tolerability.3
From a patient standpoint, bowel preparation remains the biggest deterrent to an elective colonoscopy examination.4 Bowel preparations are generally poorly tolerated, which results in an important impediment to colorectal cancer screening and surveillance. Tolerability, often measured in clinical trials with “willingness to retake the preparation” or with respect to taste of the purgative solution, involves other factors that may lead to negative patient assessment. These include various dietary modifications or restrictions and important adjustments in work or social schedule that may affect the pre-procedural quality of life and directly influence adherence. Although important for the individual patient, these are often unregistered in clinical trials and may not be necessarily discussed with the patient when a particular preparation is proposed. Rather, what often happens is that a preferred preparation regimen is selected and used in all or most patients without an informed patient decision. The US Multi-Task Force on Colorectal Cancer did not address the impact of bowel preparations on different aspects of quality of life.3
Patel et al. recently pointed out the lack of a validated instrument to assess tolerability of bowel preparation that may uncover factors leading to inadequate preparation.5 For that propose, they investigated a simple questionnaire called The Mayo Clinic Bowel Prep Tolerability Questionnaire, which examined the tolerability of the preparation and the willingness to take it again, taste, fullness, lack of sleep, and side effects. The bowel preparations used were largely polyethylene glycol (PEG)-electrolyte solutions and other unreported preparations. The authors found that the volume of the preparation did not affect tolerance, but gender did, with males having better scores than females. The study was, however, limited by the relatively small sample size (100 patients), the lack of assessment of the particular effect(s) on hunger, social or work schedule and the difference between various commercially available preparations.
Methods
In this prospective study, we evaluated the burden and tolerability of different bowel preparations in a large sample of patients, by examining seven specific variables: hunger, taste, volume, sleep, social, work, and adverse events. Patients scheduled for elective ambulatory colonoscopy were asked to complete a questionnaire regarding their experience with the prescribed bowel preparation. Study participants were chosen randomly from patients undergoing elective outpatient colonoscopies between January and May 2014 at the American University of Beirut Medical Center, Beirut, Lebanon. Bowel purgatives included PEG preparations as split-or full-dose (Fortrans®, Ibsen, Paris, France), split dose PEG + ascorbic acid (MoviPrep®, Norgine, Harefield, UK), or split-dose sodium picosulfate (Picoprep®, Ferring, Saint-Prex, Switzerland). Diet liberation was allowed with split-dose PEG (4 l PEG or 2 l MoviPrep®) while full-dose PEG consumers had to adhere to a clear fluid diet after breakfast on the day preceding the scheduled examination. Sodium picosulfate recipients had to follow two days of a low-fiber diet and one day of clear fluids prior to examination. Two research assistants administered the questionnaire immediately prior to colonoscopy. The seven aforementioned variables were graded using a numerical scale of 0–10 (best to worst). In addition, patients were asked to select in descending order from the list of seven variables what they perceived as “the worst aspect of the preparation.” The study was approved by the institutional review board and all patients gave informed verbal consent.
Results
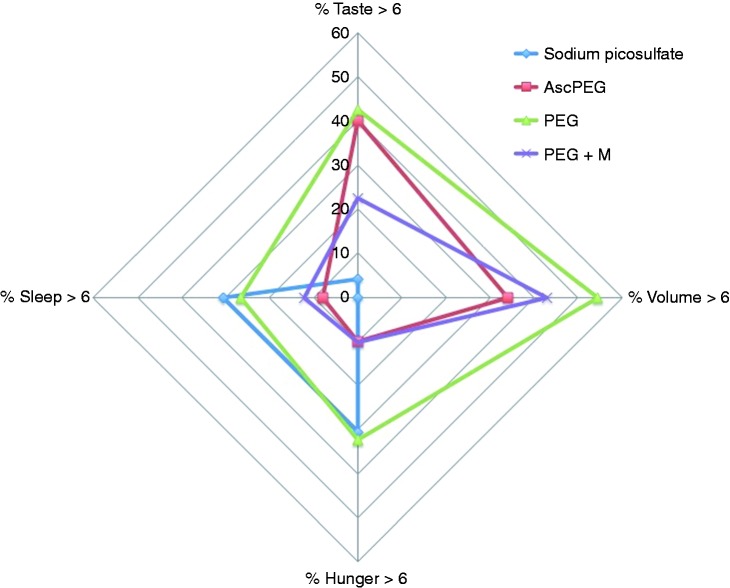
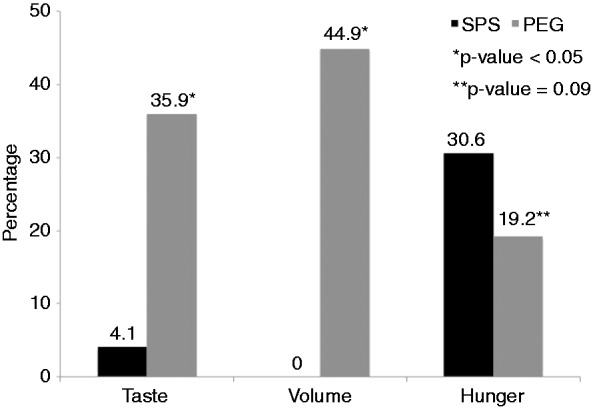
A total of 216 patients completed the survey (mean age 55.5 years; male to female ratio: 1:2). The bowel purgatives used were sodium picosulfate (SPS) (n = 49), 4 l split-dose PEG ± menthol candy6 (Halls®, Cadbury Adams, NJ, USA) (n = 49), full-dose PEG (n = 68), and split-dose ascorbic acid-PEG (M) (n = 50). With the exception of work and adverse effects, all studied variables were considered to have a negative impact (score >6) by at least 20% of patients (range 20.4–34.2). SPS was superior to the PEG regimens in taste (4.1% vs. 35.9%) and volume (0% vs. 44.9%) (p < 0.05 for both) but was inferior for hunger (30.6% vs. 19.2%; p = 0.09) (Figure 1). The addition of menthol to PEG resulted in a significant improvement of taste perception (22.4% vs. 41.5%; p = 0.02). Sleep disturbances were most common with sodium picosulfate and least with split-dose PEG (30.6% vs. 17.4%; p < 0.05) (Figure 2). Overall, volume, taste, hunger, and sleep disturbances were considered the worst aspects of the preparation. The worst variable selected consistently received >6 on the visual scale (Figure 3). Using the radar charts of the average scores for taste, volume, hunger, and sleep, a visual estimate of the burden of each type of bowel preparation was determined (Figure 4). The percentage of individuals with scores >6 for taste, volume, hunger, and sleep for each bowel preparation is shown in Figure 5. The surface area representing the overall burden associated with these variables was largest for PEG. Using PEG as reference, the burden was reduced by 65.4%, 70.3%, and 82.5% for PEG + ascorbic acid, PEG + menthol and sodium picosulfate respectively.
Figure 1.
Patients with scores >6 for the burden of taste, volume, and hunger in split-dose sodium picosulfate (SPS) vs. all PEG-based preparations.
Figure 2.
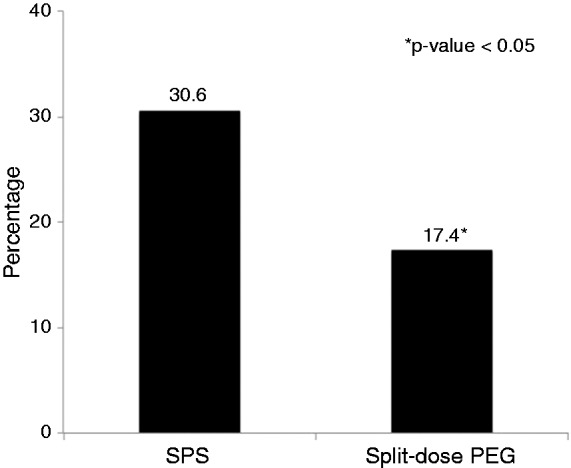
Sleep disturbance reported by patients in split-dose sodium picosulfate (SPS) vs. split-dose polyethylene glycol (PEG)-based preparations.
Figure 3.
Mean scores for taste, hunger, volume, and sleep according to descending order of most burdensome variable irrespective of preparation type.
Figure 4.
Radar chart of average scores for taste, volume, hunger, and sleep for all bowel preparations. (AscPEG = polyethylene glycol (PEG) + ascorbic acid (MoviPrep®); M = menthol).
Figure 5.
Radar chart showing percentage of individuals reporting scores >6 for taste, volume, hunger, and sleep in each bowel preparation group. (AscPEG = polyethylene glycol (PEG) ascorbic acid (MoviPrep®); M = menthol).
Discussion
According to the recommendations from the US Multi-Society Task Force on Colorectal Cancer, physicians ought to choose a specific preparation regimen based on the factors affecting patient’s compliance with the bowel preparation.1 We believe our results can be helpful when it comes to assigning patients to different preparation regimens according to their personal priorities. It is important to explain to patients that >20% of individuals may experience a negative effect on most of the above-studied variables. Taste and volume aversions are noticeably absent with low-volume sodium picosulfate but are important limitations of PEG preparations. On the other hand, compared to split-dose PEG regimens, low-volume split-dose sodium picosulfate is associated with worse disturbance in sleep because of its relatively delayed onset of action (sodium picosulfate is a prodrug that is hydrolyzed by bacteria in the colon into its active metabolite), as well as increased hunger as a result of the need for strict and longer dietary restriction. Using this information, patients can weigh the evidence and make a personal choice according to their preferences, eating habits and daily activities of the immediate pre-procedural period. A patient-friendly colorful visual aid such as radar charts may prove useful and effective when explaining the burden of each preparation leading to informed decision making, improved expectations and adherence, and ultimately improved bowel preparation.
Currently, there is no standardized questionnaire or instrument to evaluate the burden of bowel preparation. The Mayo Clinic Bowel Prep Tolerability Questionnaire developed by Patel et al. partly addressed this deficiency but is restricted by the relatively small number of patients surveyed (n = 100) and the lack of comparison between preparation regimens (77% of patients received PEG without specification of dosing schedule).5 Moreover, most clinical trials evaluating the safety and efficacy of bowel preparations use an overall global assessment of tolerability of the solution. The proverbial elephant in the colonoscopy room is the full effect of the preparation on specific patient-reported outcomes that are largely unregistered in clinical trials and are often dismissed in practice when patients present for their colonoscopy. Informing patients and setting clear expectations prior to colonoscopy can facilitate selection of the preferred preparation, which may lead to improved compliance. Compared to the limited existing literature on the topic, our prospective study involved a large number of patients, assessed more variables and types of preparations and used a numerical score to estimate the effect of each variable, providing a real-life evaluation of the burden of bowel preparation outside the context of clinical trials. A potential limitation of this study is the use of a non-validated scoring system and the empiric use of a cut-off score to indicate a significant effect. However, the average scores for the question related to “the worst aspect of the preparation” (Figure 4) seem to indicate that the selected cut-off (>6 for each variable) is reasonably accurate.
In conclusion, the real-life burden of bowel preparations is substantial. This information should be openly discussed with patients to set clear expectations and to guide choice and outcome. Additional work is needed in order to develop a validated global score for the burden of bowel preparation and prospectively investigate the impact of informed and individualized patient selection of preparation regimen on satisfaction, adherence and quality of colon cleansing.
Acknowledgments
The authors thank Robert Habib, PhD, for his advice with statistical analysis and critical review of the manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
None declared.
References
- 1.Lebwohl B, Kastrinos F, Glick M, et al. The impact of suboptimal bowel preparation on adenoma miss rates and the factors associated with early repeat colonoscopy. Gastrointest Endosc 2011; 73: 1207–1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sharara AI, Abou Mrad RR. The modern bowel preparation in colonoscopy. Gastroenterol Clin North Am 2013; 42: 577–598. [DOI] [PubMed] [Google Scholar]
- 3.Johnson DA, Barkun AN, Cohen LB, et al. Optimizing adequacy of bowel cleansing for colonoscopy: Recommendations from the US Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol 2014; 109: 1528–1545. [DOI] [PubMed] [Google Scholar]
- 4.Harewood GC, Wiersema MJ, Melton LJ 3rd. A prospective, controlled assessment of factors influencing acceptance of screening colonoscopy. Am J Gastroenterol 2002; 97: 3186–3194. [DOI] [PubMed] [Google Scholar]
- 5.Patel M, Staggs E, Thomas CS, et al. Development and validation of the Mayo Clinic Bowel Prep Tolerability Questionnaire. Dig Liver Dis 2014; 46: 808–812. [DOI] [PubMed] [Google Scholar]
- 6.Sharara AI, El-Halabi MM, Abou Fadel CG, et al. Sugar-free menthol candy drops improve the palatability and bowel cleansing effect of polyethylene glycol electrolyte solution. Gastrointest Endosc 2013; 78: 886–891. [DOI] [PubMed] [Google Scholar]