Abstract
Background
Reflux symptoms (heartburn and regurgitation) are common in patients with functional dyspepsia who do not have gastroesophageal reflux disease (GERD).
Objective
The purpose of this study was to assess the relationship of reflux symptoms with sleep disturbances in patients with functional dyspepsia without GERD and in those with GERD.
Methods
This post-hoc analysis of data from the Diamond study (NCT00291746) included patients with frequent upper gastrointestinal symptoms, of whom 137 had functional dyspepsia and 193 had GERD (diagnosed by endoscopy and pH monitoring). Patients completed symptom questionnaires and were interviewed by physicians.
Results
During the seven nights before study entry, 46.0% of patients with functional dyspepsia and 64.8% of those with GERD reported sleep disturbances (any frequency) related to reflux symptoms. Frequent (often/every night) sleep disturbances were experienced by 12.4% of patients with functional dyspepsia and 24.9% of those with GERD (p = 0.005). Among patients with functional dyspepsia, the prevalence of sleep disturbances was highest in those whose heartburn and/or regurgitation were moderate to severe (vs mild/very mild) and frequent (4–7 vs 1–3 days/week).
Conclusions
Sleep disturbances due to reflux symptoms are common in patients with functional dyspepsia who do not have GERD, and become more frequent with increasing reflux symptom severity and frequency.
Keywords: Functional dyspepsia, gastroesophageal reflux disease, heartburn, regurgitation, sleep
Introduction
Impaired sleep is a recognized problem in patients with gastroesophageal reflux disease (GERD).1–4 Results from controlled clinical trials have shown that acid suppression with a proton pump inhibitor (PPI) significantly improves sleep quality in patients with GERD.5–7 Nocturnal heartburn, arousal from sleep and poor sleep quality may arise from the unusually long duration of periods of esophageal acidification resulting from some reflux episodes that occur during the sleep period.4 A lower gastric pH during the night than during the day may also have a role in provoking damaging nocturnal esophageal acidification episodes.8
Patients with GERD and those with functional dyspepsia often have overlapping symptom patterns. In particular, many individuals with functional dyspepsia also report being troubled by heartburn and regurgitation.9 Sleep disturbances have been described in patients with functional dyspepsia,10 but the relationship between sleep disturbances and the presence of reflux symptoms remains to be explored in this population.
The aim of this analysis was to assess the frequency of patient-reported disrupted sleep caused by heartburn and/or regurgitation in individuals with functional dyspepsia. An additional aim was to assess the frequency of sleep disturbances caused by heartburn and/or regurgitation in patients with functional dyspepsia compared with that in individuals with GERD. The analysis used data from the Diamond study, which compared the accuracy of a symptom-based diagnosis of GERD by the Reflux Disease Questionnaire (RDQ) with that by primary care physicians and gastroenterologists, using investigation-based diagnostic criteria to provide an objective reference standard.11
Methods
Study population
The Diamond study (ClinicalTrials.gov Identifier: NCT00291746) was a single-blind, single-arm study conducted in north-western Europe and Canada, and recruited individuals aged 18–79 years who presented in primary care with frequent upper gastrointestinal symptoms.11 The Diamond study enrolled 507 patients, of whom 308 were fully suitable for the primary analysis11 and 336 were evaluable for post-hoc exploratory analyses.9,12 Study inclusion and exclusion criteria have been described in detail previously.11 Briefly, patients were included if they had not taken a PPI in the previous two months and had experienced upper gastrointestinal symptoms of any severity (from very mild to severe) on at least two days per week in the four weeks before the start of the study, and upper gastrointestinal symptoms of at least mild severity on at least three days in the seven days before study inclusion. The Diamond study included a PPI treatment test, with a positive response defined as absence of the most bothersome upper gastrointestinal symptom during the last three days of the two-week treatment period with esomeprazole 40 mg daily. The PPI test was evaluated using a symptom diary that patients completed daily at home throughout the study.
Study investigations
Study investigations were conducted at clinic visits. The frequency of sleep disturbances due to heartburn and/or regurgitation during the seven nights before study entry was assessed by using the following question from the psychometrically validated GERD Impact Scale: ‘How often have you had difficulty getting a good night's sleep because of your symptoms?’ Responses were recorded on a four-point scale (never, sometimes, often and daily). The GERD Impact Scale is an eight-item patient-reported outcome instrument that was developed based on a systematic literature review, and the input of focus groups of patients and primary care physicians, and patient cognitive interviews. The psychometric validation was based on a study involving two consultations in patients with new (n = 100) or chronic (n = 105) GERD.13 The GERD Impact Scale was developed to aid patient–doctor communication and therefore improve disease management.13
Frequency and severity of symptoms of heartburn, regurgitation and dyspepsia were assessed at study entry using the RDQ. The RDQ is a 12-item patient-reported outcome instrument that has undergone psychometric validation for evaluative and diagnostic purposes.14,15 The six symptom descriptors covering heartburn (burning feeling and/or pain behind the breastbone), regurgitation (an acid taste in the mouth and/or unpleasant movement of material upwards from the stomach) and dyspepsia (pain and/or burning in the upper stomach) were assessed separately for frequency (0 days, 1 day, 2–3 days, 4–6 days or daily) and severity (very mild, mild, moderate, moderately severe or severe).
Presence and severity (mild, moderate or severe) of the following 19 upper gastrointestinal symptoms in the previous seven days were assessed at study entry by physician interviews, using a predefined symptom list: belching, bloating, central chest pain, central upper abdominal discomfort, central upper abdominal pain, dysphagia, early satiety, generalized upper abdominal discomfort, generalized upper abdominal pain, heartburn, nausea, left-sided upper abdominal discomfort, left-sided upper abdominal pain, pancreatic pain, postprandial fullness, regurgitation, right-sided upper abdominal discomfort, right-sided upper abdominal pain and vomiting.11
All participants underwent upper gastrointestinal endoscopy and 48-hour pH monitoring (using a wireless pH-monitoring capsule). Reflux esophagitis and other endoscopic abnormalities were noted. Reflux esophagitis was diagnosed and graded according to the Los Angeles (LA) classification. Esophageal acid exposure was analyzed for 24 h from midnight on the first day after capsule placement, in order to standardize the time window for pH data analysis. Symptom–acid association probability (SAP) was also determined for 24 h from midnight after placement of the pH-monitoring capsule.
Diagnostic criteria
Functional dyspepsia was defined as the presence of upper gastrointestinal symptoms with no evidence of peptic ulcer disease or reflux esophagitis, with normal pH-monitoring results and a negative SAP. GERD was defined as the presence of at least one of the following three criteria: reflux esophagitis on endoscopy (LA grades A–D); pathological distal esophageal acid exposure (esophageal pH<4 for >5.5% of the 24-h period of analysis); and/or positive (>95%) SAP for association of symptoms with acid reflux episodes.
Statistical analyses
The frequency distribution of weekly sleep disturbance (never or sometimes vs often or nightly) in patients with GERD vs those with functional dyspepsia was tested using the Cochran–Mantel–Haenszel test. The prevalence of frequent (often or nightly) sleep disturbance categories in patients with GERD vs those with functional dyspepsia was tested using the χ2 test. The prevalence of sleep disturbances (any frequency) according to the presence of the RDQ items in patients with GERD vs those with functional dyspepsia was tested using the Fisher's exact test. The frequency distribution of weekly sleep disturbances (sometimes vs often or nightly) was compared with reflux/dyspepsia symptom frequency (1–3 days/week vs 4–7 days/week) and severity (very mild or mild vs moderate, moderately severe or severe), as well as severity of early satiety and postprandial fullness (physician interview; mild vs moderate or severe) using the Cochran–Mantel–Haenszel test.
Results
Patient population
Of the 507 patients enrolled in the Diamond study, data from 336 (138 with functional dyspepsia and 197 with GERD) were suitable for exploratory analyses. The current analysis included 137 patients with functional dyspepsia and 193 with GERD for whom data on sleep disturbance frequency were available. Demographic characteristics of the two groups are shown in Table 1. Sleep disturbances of any frequency due to heartburn and/or regurgitation during the seven nights before study entry were reported by 63 individuals (46.0%) with functional dyspepsia and 125 patients (64.8%) with GERD, and often or nightly sleep disturbances by 17 (12.4%) and 48 (24.9%) of those with functional dyspepsia and GERD, respectively (Table 2). The distribution of weekly sleep disturbance categories (never/sometimes vs often/daily) differed significantly in patients with GERD vs those with functional dyspepsia (p = 0.0008). Frequent (often/daily) sleep disturbances were significantly more common in patients with GERD than in those with functional dyspepsia (p = 0.0050; relative risk: 2.00 (1.21–3.33)).
Table 1.
Demographic characteristics of patients with gastroesophageal reflux disease (GERD) or functional dyspepsia
| GERD, n = 193 | Functional dyspepsia, n = 137 | |
|---|---|---|
| Mean age, years (SD) | 47.9 (13.4) | 45.8 (14.8) |
| Sex | ||
| Male | 110 (57.0) | 42 (30.7) |
| Female | 83 (43.0) | 95 (69.3) |
| Mean BMI, kg/m2 (SD) | 27.5 (4.5) | 25.5 (4.4) |
| Positive for Helicobacter pylori | 45 (23.3) | 29 (21.2) |
| Hiatus hernia | 88 (45.6) | 38 (27.7) |
BMI: body mass index; SD: standard deviation.
Values are presented as n (%), unless otherwise indicated.
Table 2.
Sleep disturbances due to heartburn and/or regurgitation in seven nights before study entry
| Diagnosis | Frequency of sleep disturbances, n (%) |
|||
|---|---|---|---|---|
| Never | Sometimes | Often | Daily | |
| GERD, n = 193 | 68 (35.2) | 77 (39.9) | 34 (17.6) | 14 (7.3) |
| Functional dyspepsia, n = 137 | 74 (54.0) | 46 (33.6) | 10 (7.3) | 7 (5.1) |
GERD: gastroesophageal reflux disease.
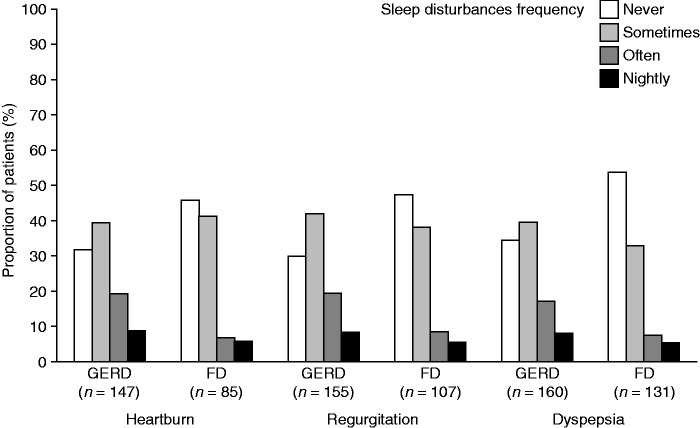
Sleep disturbances by upper gastrointestinal symptom profile
The proportions of patients with functional dyspepsia who reported sleep disturbances of any frequency were 54%, 52%, and 46% among individuals who reported symptoms of heartburn, regurgitation or dyspepsia, respectively (Figure 1). Among patients with GERD, the proportions who reported sleep disturbances of any frequency were 68%, 70% and 65% among those who reported symptoms of heartburn, regurgitation or dyspepsia on the RDQ, respectively (Figure 1). In the group who reported symptoms of heartburn, regurgitation or pain and/or burning feeling in the upper stomach (i.e. ‘dyspepsia’), the proportion of patients with sleep disturbances was significantly higher among individuals with GERD than among individuals with functional dyspepsia (all p < 0.05).
Figure 1.
Frequency of sleep disturbances by Reflux Disease Questionnaire symptom profile in patients with gastroesophageal reflux disease (GERD) and functional dyspepsia (FD).
In patients who reported early satiety at physician interview, the prevalence of sleep disturbances of any frequency was 52.7% (39/74) in the functional dyspepsia group and 66.1% (41/62) in the GERD group (p = 0.12). In patients who reported postprandial fullness, the prevalence of sleep disturbances of any frequency was 47.5% (38/80) in the functional dyspepsia group and 63.6% (63/99) in the GERD group (p < 0.05).
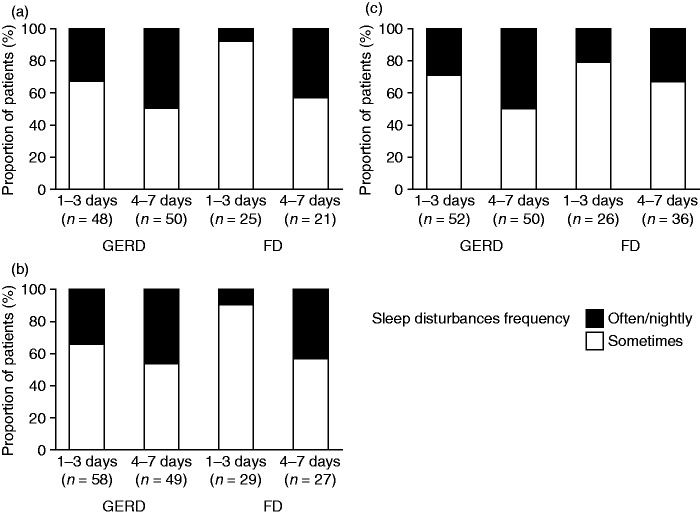
Sleep disturbances by upper gastrointestinal symptom frequency and severity
In patients with functional dyspepsia, the prevalence of frequent (often or nightly) sleep disturbances was numerically higher in patients who reported moderate to severe symptoms of heartburn, regurgitation or dyspepsia than in patients in whom these symptoms were very mild or mild (Figure 2). The prevalence of frequent sleep disturbances in the group with functional dyspepsia was also numerically higher in those who reported moderate or severe early satiety or postprandial fullness at physician interview than in patients in whom these symptoms were mild (Figure 2).
Figure 2.
Frequency of sleep disturbances according to severity of upper gastrointestinal symptoms of (a) heartburn, (b) regurgitation, (c) dyspepsia, (d) early satiety and (e) postprandial fullness in patients with GERD and FD. Information on the severity distribution of heartburn, regurgitation and dyspepsia was obtained from the Reflux Disease Questionnaire (very mild or mild vs moderate to severe), and that of early satiety and postprandial fullness from physician interview (mild vs moderate or severe). FD: functional dyspepsia; GERD, gastroesophageal reflux disease.
The prevalence of frequent sleep disturbances was numerically higher in patients with functional dyspepsia who had frequent (4–7 days/week) symptoms of heartburn, regurgitation or dyspepsia than in those with functional dyspepsia who had these symptoms less frequently (1–3 days) (Figure 3).
Figure 3.
Frequency of sleep disturbances according to frequency of upper gastrointestinal symptoms of (a) heartburn, (b) regurgitation and (c) dyspepsia in patients with gastroesophageal reflux disease (GERD) or functional dyspepsia (FD), as reported on the Reflux Disease Questionnaire.
In the group with GERD, a numerically higher prevalence of frequent sleep disturbances was observed in patients who reported moderate to severe regurgitation or dyspepsia on the RDQ than in those in whom these symptoms were very mild or mild (Figure 2). The prevalence of frequent sleep disturbances was also numerically higher in patients with GERD who had frequent symptoms of heartburn, regurgitation or dyspepsia than in those with GERD who had these symptoms less frequently (Figure 3). In contrast, no increase in sleep disturbance frequency was observed with increasing severity of heartburn, early satiety or postprandial fullness in patients with GERD (Figure 2).
The association between diagnosis (GERD or functional dyspepsia) and sleep disturbances was significant when controlling for severity of heartburn symptoms (using the Cochran–Mantel–Haenszel method; p < 0.05), but was not significant when controlling for severity of symptoms of regurgitation, dyspepsia, early satiety or postprandial fullness (p > 0.05). Similarly, the association between diagnosis and sleep disturbances was significant when controlling for frequency (1–3 vs 4–7 days) of heartburn symptoms (p < 0.05), but was not significant when controlling for frequency of symptoms of regurgitation or dyspepsia (p > 0.05).
Response to PPI treatment
Data on response to two weeks of PPI treatment were available for 31 patients with functional dyspepsia and 86 patients with GERD. A positive response (defined as absence of the most bothersome upper gastrointestinal symptom during the last three days of the treatment period) was observed in 58% of patients with functional dyspepsia (54.5% (12/22) and 66.7% (6/9) of patients with dyspepsia with sleep disturbances occurring sometimes and often/nightly, respectively) and 65% of patients with GERD (62.5% (30/48) and 68.4% (26/38) of patients with GERD with sleep disturbances occurring sometimes and often/nightly, respectively) (p = 0.157 for functional dyspepsia vs GERD).
Discussion
In this unselected primary care population with frequent upper gastrointestinal symptoms, almost half of patients with functional dyspepsia and two-thirds of patients with GERD reported sleep disturbances due to heartburn and/or regurgitation in the seven days before study entry. Patients with GERD and moderate to severe heartburn were more likely to have frequent sleep disturbances than those with functional dyspepsia and moderate to severe heartburn. The association between frequent sleep disturbances and diagnosis (GERD vs functional dyspepsia) was significant when adjusting for heartburn, but not when adjusting for other upper gastrointestinal symptoms, indicating that the prevalence of frequent sleep disturbances in patients with upper gastrointestinal symptoms other than heartburn did not tend to differ between patients with GERD and individuals with functional dyspepsia.
The proportion of patients with GERD or functional dyspepsia who had sleep disturbances due to heartburn and/or regurgitation in the current study was higher than the 31% prevalence of any sleep problems reported for western Europe in a large, general-population survey.16 The current analysis looked specifically at sleep disturbances due to heartburn and/or regurgitation and thus did not capture the overall proportion of patients with any sleep disturbances, which is likely to have been substantially higher.
Sleep disturbances are frequent in the functional dyspepsia population. In an academic referral center for functional gastrointestinal disorders, 68% of patients with functional dyspepsia had disordered sleep, which was not related to anxiety and depression.17 In another study, functional dyspepsia was also associated with sleep disturbances, and sleep disturbances were more likely in women than men and in patients who had moderate or severe symptoms related to dyspepsia than in those with mild symptoms.10 Population-based data have suggested that sleep disturbances are related to both upper and lower gastrointestinal symptoms, although the nature of their relationship with sleep disturbances is uncertain.18
In patients with GERD, sleep disturbances are common.19,20 In a large primary care study in France, nocturnal reflux symptoms were reported by 64% of patients with reflux disease, and regular (at least weekly) GERD-related sleep disturbances by 62%.19 Other reports suggest that the majority of patients with GERD experience night-time reflux symptoms and two-thirds of individuals with night-time symptoms believe that heartburn negatively affects their ability to sleep well.2,20 Patients with incomplete responses to PPI therapy also report sleep disturbances: in a Canadian primary care study, 55% of patients with reflux disease who had incomplete symptom control with a PPI reported sleep disturbances.21 Sleep disturbances have a profound effect on quality of life in individuals with GERD.22 In people with undiagnosed sleep disorders, reflux disease is common and is associated with increased arousals from sleep and a decrease in the time spent in stage two (the restorative phase) of sleep.23
We have recently shown that, in a primary care population of patients who have functional dyspepsia with no evidence of GERD on endoscopy and pH monitoring, heartburn and regurgitation are frequent complaints.9 In the current analysis, we show that heartburn and regurgitation in the functional dyspepsia population are related to adverse effects on sleep, with increased symptom frequency and severity paralleling an increased frequency of sleep disturbances. There is little information in the literature about the impact of heartburn and regurgitation on sleep in patients with functional dyspepsia; however, indirect evidence from a recent study supports our findings, showing that sleep disturbances were more common in Japanese patients with functional dyspepsia than in healthy controls.24 The same study also found that sleep disturbances were related to GERD symptoms and improved with acid inhibition.24
Strengths of the Diamond study include its large size, the unselected, consecutive inclusion of the population of patients presenting with upper gastrointestinal symptoms in primary care, and the use of endoscopy and wireless pH monitoring.11 The entry criteria of the Diamond study, however, required patients to have had symptoms for at least four weeks, while the Rome III criteria for functional dyspepsia require symptoms to have been present for at least three months.25 A limitation of this post-hoc analysis is that sleep disturbance due to heartburn and/or regurgitation was determined based on a single question from the psychometrically validated GERD Impact Scale; additional data from sleep-specific questionnaires were not available for this analysis. However, single question evaluations on the quality of sleep have been used in clinical practice and have been shown to be as effective as the Epworth Sleepiness Scale and the multiple sleep latency test at measuring sleepiness.26 A further limitation of this post-hoc analysis is that, unfortunately, only a small number of patients in the current analysis had evaluable data on PPI treatment outcome available by diagnosis and sleep disturbance category.
In conclusion, sleep disturbances are common in patients with functional dyspepsia who have no evidence of GERD on endoscopy or pH monitoring, and are related to reflux symptoms. Patients with more severe or more frequent upper gastrointestinal symptoms had more frequent sleep disturbances than those with less severe or less frequent symptoms. Our study demonstrates that the overlapping symptoms of GERD and functional dyspepsia may markedly impact patients' lives by affecting sleep.
Acknowledgements
Writing support was provided by Anja Becher and Nesta Hughes, from Oxford PharmaGenesis, Oxford, UK, and was funded by AstraZeneca R&D, Mölndal, Sweden.
Funding
This study was funded by AstraZeneca R&D, Mölndal, Sweden.
Conflicts of interest
N Vakil: consultancy fees from AstraZeneca, Ironwood Pharmaceuticals. J Dent: consultancy fees from AstraZeneca. J Wissmar: employee of AstraZeneca R&D, Mölndal, Sweden. B Wernersson: employee of AstraZeneca R&D, Mölndal, Sweden, at the time that this analysis was conducted.
References
- 1.Wiklund I. Review of the quality of life and burden of illness in gastroesophageal reflux disease. Dig Dis 2004; 22: 108–114. [DOI] [PubMed] [Google Scholar]
- 2.Shaker R, Castell DO, Schoenfeld PS, et al. Nighttime heartburn is an under-appreciated clinical problem that impacts sleep and daytime function: The results of a Gallup survey conducted on behalf of the American Gastroenterological Association. Am J Gastroenterol 2003; 98: 1487–1493. [DOI] [PubMed] [Google Scholar]
- 3.Mody R, Bolge SC, Kannan H, et al. Effects of gastroesophageal reflux disease on sleep and outcomes. Clin Gastroenterol Hepatol 2009; 7: 953–959. [DOI] [PubMed] [Google Scholar]
- 4.Dent J, Holloway RH, Eastwood PR. Systematic review: Relationships between sleep and gastro-oesophageal reflux. Aliment Pharmacol Ther 2013; 38: 657–673. [DOI] [PubMed] [Google Scholar]
- 5.Johnson D, Crawley JA, Hwang C, et al. Clinical trial: Esomeprazole for moderate-to-severe nighttime heartburn and gastro-oesophageal reflux disease-related sleep disturbances. Aliment Pharmacol Ther 2010; 32: 182–190. [DOI] [PubMed] [Google Scholar]
- 6.Johnson D, Orr WC, Crawley JA, et al. Effect of esomeprazole on nighttime heartburn and sleep quality in patients with GERD: A randomized, placebo-controlled trial. Am J Gastroenterol 2005; 100: 1914–1922. [DOI] [PubMed] [Google Scholar]
- 7.Fass R, Johnson DA, Orr WC, et al. The effect of dexlansoprazole MR on nocturnal heartburn and GERD-related sleep disturbances in patients with symptomatic GERD. Am J Gastroenterol 2011; 106: 421–431. [DOI] [PubMed] [Google Scholar]
- 8.Hatlebakk J, Zerbib F, Bruley des Varannes S, et al. Symptoms of gastroesophageal reflux disease are associated with higher night-time esophageal acid exposure and lower gastric ph. Gut 2011; 60: A375. [Google Scholar]
- 9.Vakil N, Halling K, Ohlsson L, et al. Symptom overlap between postprandial distress and epigastric pain syndromes of the Rome III dyspepsia classification. Am J Gastroenterol 2013; 108: 767–774. [DOI] [PubMed] [Google Scholar]
- 10.Lacy BE, Everhart K, Crowell MD. Functional dyspepsia is associated with sleep disorders. Clin Gastroenterol Hepatol 2011; 9: 410–414. [DOI] [PubMed] [Google Scholar]
- 11.Dent J, Vakil N, Jones R, et al. Accuracy of the diagnosis of GORD by questionnaire, physicians and a trial of proton pump inhibitor treatment: The Diamond Study. Gut 2010; 59: 714–721. [DOI] [PubMed] [Google Scholar]
- 12.Vakil N, Wernersson B, Ohlsson L, et al. Prevalence of gastroesophageal reflux disease with upper gastrointestinal symptoms without heartburn and regurgitation. United European Gastroenterol J 2014; 2: 173–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jones R, Coyne K, Wiklund I. The gastro-oesophageal reflux disease impact scale: A patient management tool for primary care. Aliment Pharmacol Ther 2007; 25: 1451–1459. [DOI] [PubMed] [Google Scholar]
- 14.Shaw M, Dent J, Beebe T, et al. The Reflux Disease Questionnaire: A measure for assessment of treatment response in clinical trials. Health Qual Life Outcomes 2008; 6: 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shaw MJ, Talley NJ, Beebe TJ, et al. Initial validation of a diagnostic questionnaire for gastroesophageal reflux disease. Am J Gastroenterol 2001; 96: 52–57. [DOI] [PubMed] [Google Scholar]
- 16.Léger D, Poursain B, Neubauer D, et al. An international survey of sleeping problems in the general population. Curr Med Res Opin 2008; 24: 307–317. [DOI] [PubMed] [Google Scholar]
- 17.Fass R, Fullerton S, Tung S, et al. Sleep disturbances in clinic patients with functional bowel disorders. Am J Gastroenterol 2000; 95: 1195–2000. [DOI] [PubMed] [Google Scholar]
- 18.Cremonini F, Camilleri M, Zinsmeister AR, et al. Sleep disturbances are linked to both upper and lower gastrointestinal symptoms in the general population. Neurogastroenterol Motil 2009; 21: 128–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cadiot G, Delaage PH, Fabry C, et al. Sleep disturbances associated with gastro-oesophageal reflux disease: Prevalence and impact of treatment in French primary care patients. Dig Liver Dis 2011; 43: 784–787. [DOI] [PubMed] [Google Scholar]
- 20.Farup C, Kleinman L, Sloan S, et al. The impact of nocturnal symptoms associated with gastroesophageal reflux disease on health-related quality of life. Arch Intern Med 2001; 161: 45–52. [DOI] [PubMed] [Google Scholar]
- 21.Moayyedi P, Hunt R, Armstrong D, et al. The impact of intensifying acid suppression on sleep disturbance related to gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther 2013; 37: 730–737. [DOI] [PubMed] [Google Scholar]
- 22.Madisch A, Kulich KR, Malfertheiner P, et al. Impact of reflux disease on general and disease-related quality of life - evidence from a recent comparative methodological study in Germany. Z Gastroenterol 2003; 41: 1137–1143. [DOI] [PubMed] [Google Scholar]
- 23.Guda N, Partington S, Vakil N. Symptomatic gastro-oesophageal reflux, arousals and sleep quality in patients undergoing polysomnography for possible obstructive sleep apnoea. Aliment Pharmacol Ther 2004; 20: 1153–1159. [DOI] [PubMed] [Google Scholar]
- 24.Futagami S, Yamawaki H, Izumi N, et al. Impact of sleep disorders in Japanese patients with functional dyspepsia (FD): Nizatidine improves clinical symptoms, gastric emptying and sleep disorders in FD patients. J Gastroenterol Hepatol 2013; 28: 1314–1320. [DOI] [PubMed] [Google Scholar]
- 25.Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology 2006; 130: 1377–1390. [DOI] [PubMed] [Google Scholar]
- 26.Zallek SN, Redenius R, Fisk H, et al. A single question as a sleepiness screening tool. J Clin Sleep Med 2008; 4: 143–148. [PMC free article] [PubMed] [Google Scholar]