Abstract
Objectives:
There is a need to remove excess iron with iron chelation therapy (ICT) to avoid the serious clinical sequelae associated with iron overload in patients with beta thalassemia major (BTM) and sickle cell anemia (SCA). Due to the effects of the diseases and their treatments, ICT is still a major reason for unsatisfactory compliance. The aim of this single-center observational study was to evaluate the quality of life, clinical effectiveness, and satisfaction in pediatric and adult patients with BTM and SCA receiving deferasirox (DFX) chelation therapy.
Methods:
In this study, 37 pediatric and 35 adult patients with BTM or SCA receiving DFX for at least 6 months participated. Upon receipt of Informed Consent Form, Case Report Form, Demographic Data Collection Form, Child Health Questionnaire-Parent Form, Life Quality Survey Short Form-36, and ICT Satisfaction Survey were used to obtain data for the effectiveness of ICT and parameters that may affect compliance to treatment and life quality of the participants.
Results:
As a main index for the effectiveness of DFX chelation therapy, serum ferritin levels were higher than the normal values in the patients receiving DFX. The increased ferritin levels were also associated with hematological and biochemical abnormalities. Our findings regarding quality of life and satisfaction with DFX chelation therapy indicated that the patients with BTM or SCA had lower scores. Overall, problems with treatment regimen and side effects appeared to be common causes of poor compliance to DFX chelation therapy.
Conclusions:
Our findings suggest that health care providers should be aware of the importance of monitoring iron load with timely initiation of DFX chelation therapy and ongoing adjustments to chelation regimens and/or transfusion methods to decrease hospitalizations and improve compliance to ICT of the patients with BTM and SCA.
Keywords: Beta thalassemia major, compliance, deferasirox chelation therapy, sickle cell anemia
Introduction
The thalassemias together with sickle cell anemia (SCA) and its variants are the world's most common form of inherited anemia. The beta thalassemias are a group of hereditary hematological diseases caused by over 300 mutations of the adult beta-globin gene. Beta thalassemia is characterized by reduced synthesis of the hemoglobin subunit beta globin protein that results in microcytic hypochromic anemia, an abnormal peripheral blood smear with nucleated red blood cells, and reduced amounts of hemoglobin A on hemoglobin analysis. Severity is variable from mild anemia, through intermediate forms, to severe anemia. For instance, beta thalassemia major (BTM) is a severe transfusion-dependent anemia.[1,2,3,4,5,6,7,8,9,10] Sickle cell disease (SCD) is an autosomal recessive disorder in the gene encoding the β-chain of hemoglobin causing a weakening systemic syndrome characterized by chronic anemia, acute painful episodes, tissue ischemia, and chronic organ damage in addition to a significant reduction in life expectancy. SCA is the homozygoid form of SCD, which includes a group of genetic disorders characterized by production of an abnormal hemoglobin S, hemolysis, and vasoocclusive phenomena with recurrent painful episodes that can lead to life-long disabilities and death.[2,6,9,11,12] The patients with transfusion-dependent iron overload conditions such as BTM and SCA require frequent blood transfusions.
The conventional approach to treatment of BTM and SCA is based on the correction of hemoglobin status through regular blood transfusions and iron chelation therapy (ICT) for iron overload.[2,3,4,6,8,9,11,13,14,15] On the other hand, iron overload causes iron deposition and accumulation in the liver, heart, skin, and other tissues resulting in serious tissue damages. Thus, there is a need to remove excess iron with chelation therapy using deferoxamine (DFO) (Desferal®; Novartis Pharma AG, Basel, Switzerland), deferiprone (DFP) (Ferriprox®; Apotex Inc., Toronto, Canada), deferasirox (DFX) (Exjade®; Novartis Pharma AG, Basel, Switzerland), or in combination with each other (DFO-DFP or DFP-DFX) to avoid the serious clinical sequelae associated with iron accumulation in target organs, morbidity, and mortality. On the other hand, due to the effects of the diseases and their treatments, ICT is still a major reason for unsatisfactory compliance of these patients. Although DFO, which is administered intravenously or subcutaneously, is clinically effective at removing excess iron, many patients are not satisfactorily chelated by it. The reasons for the poor compliance of patients to DFO include cost of the drug, pump and tubing and its side effects (such as local problems at the site of the infusions, hematological toxicity, allergy, shortness of breathless, headaches, dizziness, and Yersinia infection) that negatively affect patient's health-related quality of life (HRQOL). DFX and DFP are orally effective iron chelators alternative to DFO that have proven their efficacy in reducing iron burden in addition to increase in patient's compliance. However, these drugs have also unwanted side effects that negatively impact on patient's adherence to ICT (nausea, vomiting, abdominal pain, neutropenia/agranulocytosis, arthralgia, rise in transaminases, and zinc deficiency with DFP, and diarrhea, abdominal pain, nausea, vomiting, changes in renal and liver function, auditory and ocular alterations, skin rash, headache, and dizziness with DFX).[2,3,6,8,9,11,13,15] Since each chelation regimen has a distinct safety/efficacy profile and particular costs associated with its use, when choosing a chelator regimen, physicians, patients, parents, and providers may consider a variety of factors, including the severity of iron overload, administration schedule, and adverse effect profile. DFX is one of the most widely used iron chelators despite warnings of life-threatening toxic side effects. To better understand the potential impact of current therapeutic approaches for iron overload, it is important to understand the clinical effectiveness, patient acceptability, and side effects of DFX in addition to patient's HRQOL. Therefore, the aim of this single-center observational study was to evaluate the quality of life, clinical effectiveness, and satisfaction in pediatric and adult patients with BTM and SCA receiving DFX chelation therapy.
Methods
Patients and study design
The single-center observational study was conducted among 37 pediatric and 35 adult patients with BTM or SCA who received DFX (Exjade®; Novartis Pharma Stein AG, Stein, Switzerland) (20–40 mg/kg/day) ICT at the Hematology Units of Departments of Internal Medicine and Pediatrics, Faculty of Medicine, Mersin University, Mersin, Turkey from December 2013 to May 2014 participated. The protocol of this study was approved by Mersin University Clinical Research Ethics Committee and Pharmaceuticals and Medical Devices Administration of Turkey.
Inclusion and exclusion criteria
Participants were selected based on the inclusion and exclusion criteria. The inclusion criteria were (1) patients willing to participate in the study, (2) patients diagnosed with BTM or SCA, and (3) patients receiving DFX for at least 6 months. The exclusion criteria were (1) patients not meeting the inclusion criteria, (2) patients not willing to participate in the study, (3) patients diagnosed with other types of anemia, (4) patients not receiving DFX for at least 6 months, and (5) patients having other conditions such as physical and/or mental difficulties which may affect their quality of life.
Study instruments and data collection
At the beginning of the study, all eligible patients and/or their parents were informed of the objectives of the study and assured that all information would remain confidential. After taking signed written informed consent from the patients and/or their parents, the following data were obtained: (1) Demographic and clinical characteristics of pediatric and adult patients (using Case Report Form and Demographic Data Collection Form), (2) health status of pediatric patients (using Child Health Questionnaire-Parent Form; CHQ-PF50),[16,17,18] (3) quality of life of adult patients (using Life Quality Survey Short Form-36; [SF-36]),[19,20,21,22,23,24,25] (4) effectiveness of ICT in pediatric and adult patients (using Case Report Form and ICT Satisfaction Survey),[17,23,26,27,28] and (5) compliance to ICT in pediatric and adult patients (using ICT Satisfaction Survey).[7,11,17,23,27,29,30,31]
The CHQ-PF50 (for children aged 5–18 years) measures HRQOL children as reported by the parent. The form contains 50 items yielding 15 subtitles: General health, physical functioning, role/social limitations-emotional/behavioral, role/social limitations-physical, bodily pain/discomfort, behavior, global behavior, emotional state, self-esteem, general health state, health transition, parent impact-emotional, parent impact-time, family activities, and family cohesion.[16,17,18] In this study, the items were scored and the computed scores were transformed to a scale from 0 to 100. Higher scores indicate better health.
SF-36 is a self-administered generic questionnaire that measures two major subjective health concepts (i.e., physical and mental health). The form comprises 36 multichoice questions yielding a profile of eight concepts: (1) Physical functioning, (2) physical role limitation, (3) pain, (4) mental health, (5) emotional role limitation, (6) social functioning, (7) vitality, and (8) general health perception. SF-36 has also an item measuring health transition over the past year. The reliability and validity of SF-36 are well documented in all available language versions.[19,20,21,22,23,24,25,32] In this study, responses to each of the SF-36 items were scored and summed according to a standardized scoring protocol and expressed as a score on a 0–100 scale for each of the eight health concepts. Higher scores indicate better self-perceived health.
The ICT Satisfaction Survey used in the study consisted of satisfaction-specific items measuring four domains: (1) Perceived effectiveness, (2) acceptance/approval, (3) burden of ICT, and (4) side effects.[15,23,28,31] Patient responses to the items comprising these domains were scored, and the scores were transformed to a scale from 0 (worst satisfaction) to 100 (best satisfaction).
Statistical analysis
Qualitative variables were expressed as number and percent. Quantitative variables regarding health status of pediatric patients and compliance to ICT in pediatric and adult patients were described in the form of mean ± standard deviation (SD), median, and range. The other quantitative variables were expressed as mean ± SD. Statistical analysis was based on descriptive statistic procedures, and the comparison of means between two different groups was performed with the Student's t-test and Mann–Whitney U-test, for variables with normal and skewed distribution, respectively, STATA/MP11 Package (StataCorp LP, TX, USA) or GraphPad Prism version 5.01 for Windows (GraphPad Software, Inc., CA, USA). A P < 0.05 was considered statistically significant.
Results
Demographic and clinical characteristics
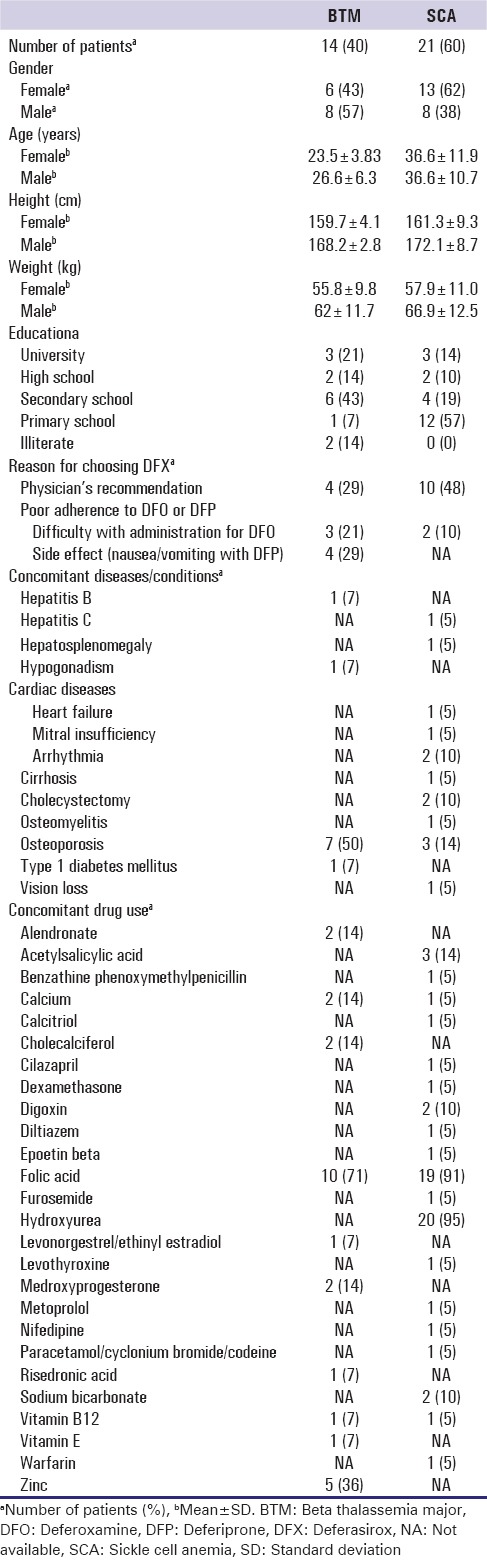
The demographic and clinical characteristics of the pediatric and adult patients are summarized in Tables 1 and 2, respectively. The study population comprised 37 pediatric (BTM: n = 25 [52% female and 48% male]; SCA: n = 12 [50% female and 50% male]) and 35 adult (BTM: n = 14 [43% female and 57% male]; SCA: n = 21 [62% female and 38% male]) patients with BTM or SCA. All patients were receiving periodic blood transfusions. At the time of the study visit, the pediatric patients were being treated with DFX. The adult patients were receiving DFX therapy (78% BTM and 91% SCA). The reasons for choosing their therapy were physician's recommendation, poor adherence to DFO, DFP, or DFX, and the failure of reimbursement system for DFO. The percentages of pediatric patients with BTM or SCA who had formal education were 88% and 83%, respectively. In the adult patients with BTM or SCA, the percentages were 86% and 100%, respectively. Eight (32%) and six (50%) of pediatric patients with BTM or SCA had undergone splenectomy. Two (8%) pediatric patients with BTM had hepatomegaly or splenomegaly and one (4%) adult patient with SCA had hepatosplenomegaly. The patients also had one or more concomitant diseases/conditions and were using other drugs for their diseases in addition to the iron chelators.
Table 1.
Demographic and clinical characteristics of deferasirox-treated pediatric patients
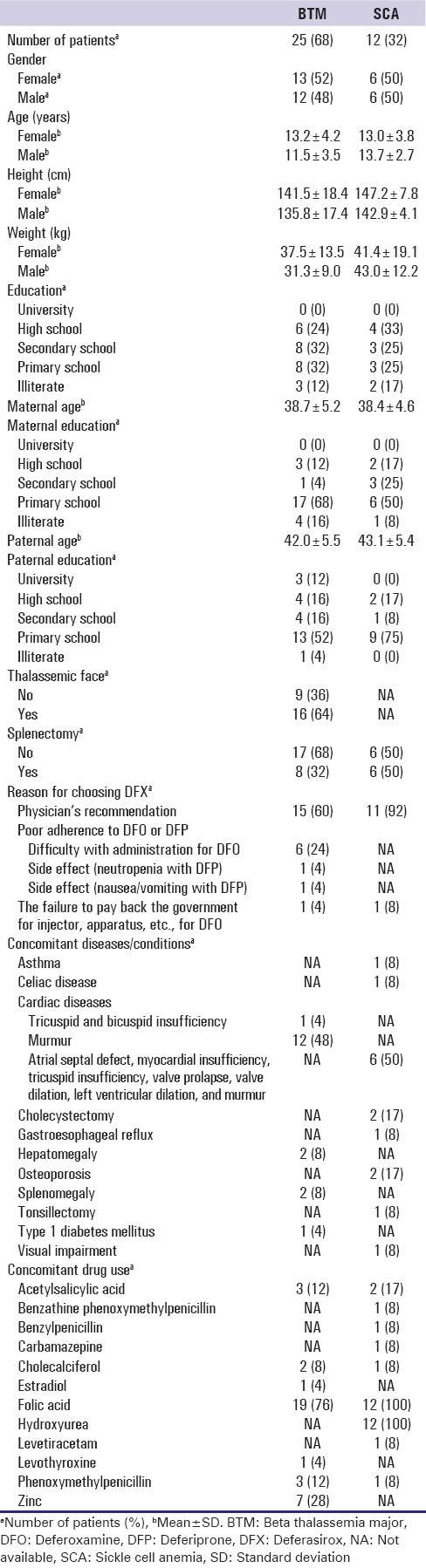
Table 2.
Demographic and clinical characteristics of deferasirox-treated adult patients
Quality of life
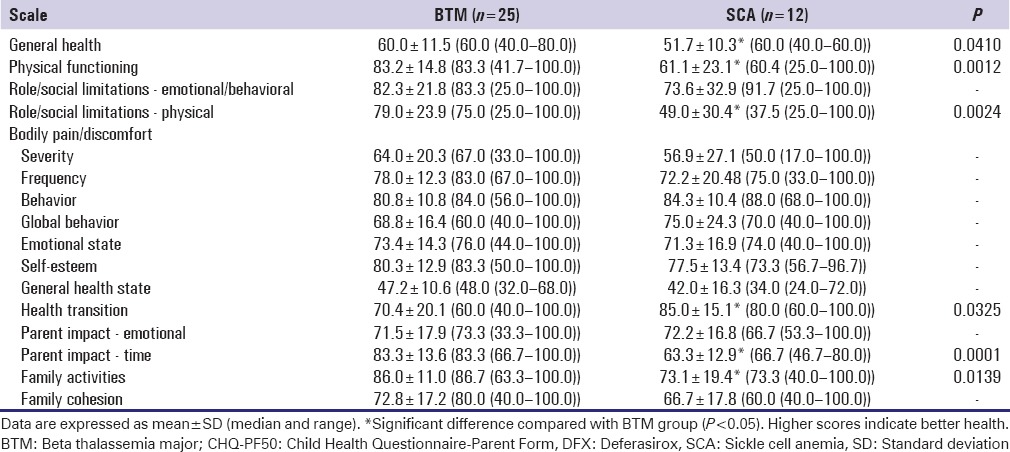
Table 3 shows the CHQ-PF50 summary scores regarding HRQOL in DFX-treated pediatric patients with BTM or SCA. In particular, the mean CHQ-PF50 scores in the patients with BTM ranged from 86.0 ± 11.0 (n = 25) for the family activities to 47.2 ± 10.6 (n = 25), the general health state. In the patients with SCA, the scores ranged from 85.0 ± 15.1 (n = 12) for the health transition to 42.0 ± 16.3 (n = 12) for the general health state. The scores for general health, physical functioning, role/social limitations-physical, parent impact-time, and family activities were significantly lower, and the scores for health transition were higher in the patients with SCA than the patients with BTM (P < 0.05). The differences between patient groups for the other scales were not statistically different.
Table 3.
Child Health Questionnaire-Parent Form 50 summary scores (%) in deferasirox-treated pediatric patients with beta thalassemia major or sickle cell anemia
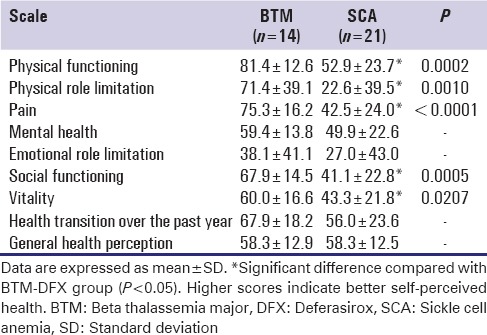
The SF-36 summary scores regarding the quality of life in adult patients with BTM or SCA who received DFX are shown in Table 4. In particular, the mean SF-36 scores in the DFX-treated patients with BTM ranged from 81.0 ± 12.6 (n = 14) for the physical functioning to 38.1 ± 41.1 (n = 14) the emotional role limitation. The scores in the DFX-treated patients with SCA ranged from 58.3 ± 12.5 (n = 21) for the general health perception to 22.6 ± 39.5 (n = 21) the physical role limitation. When compared with the scores of the DFX-treated patients with BTM, the scores for physical functioning, physical role limitation, pain, social functioning, and vitality were significantly lower in the DFX-treated patients with SCA (P < 0.05). The differences between patient groups for the other scales were not statistically different.
Table 4.
Short form-36 summary scores (%) in deferasirox-treated adult patients with beta thalassemia major or sickle cell anemia
Effectiveness of iron chelation therapy
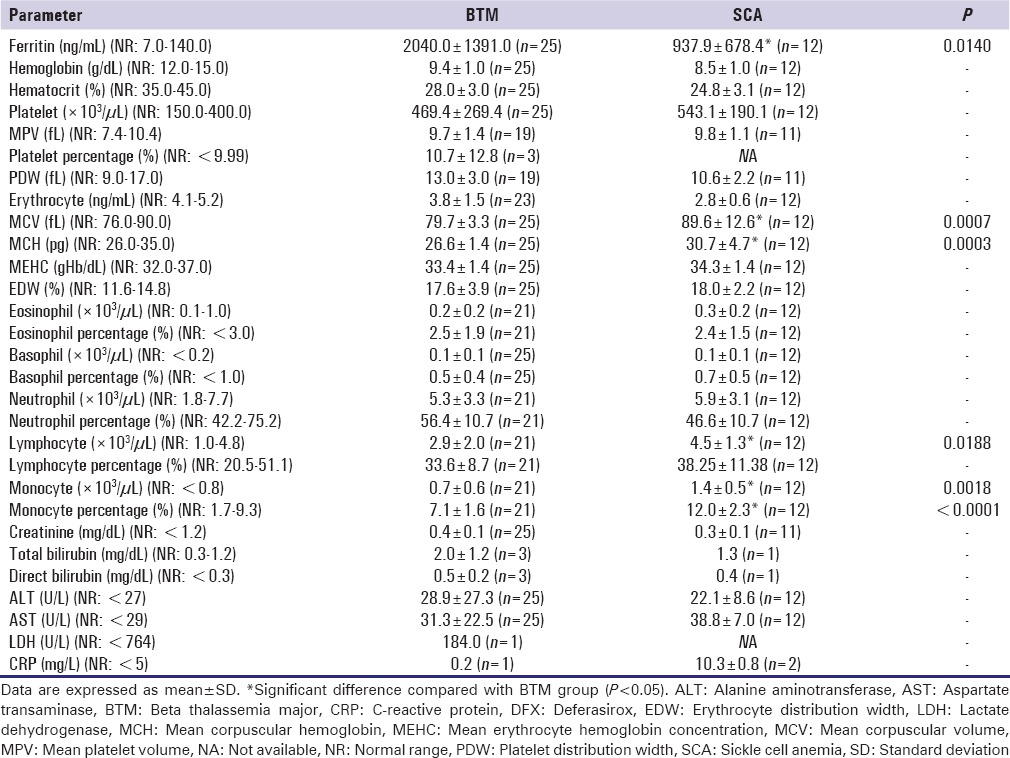
Table 5 details hematological and biochemical parameters in DFX-treated pediatric patients with BTM or SCA. As a main index for effectiveness of ICT, mean serum ferritin levels were higher than the normal values (7.0–140.0 ng/mL) in the pediatric patients receiving DFX (BTM: 2040.0 ± 1391 ng/mL, n = 25; SCA: 937.9 ± 678.4 ng/mL, n = 12). In the patients with BTM, the values regarding platelet, platelet percentage, erythrocyte distribution width (EDW), total bilirubin, direct bilirubin, alanine aminotransferase (ALT), and aspartate transaminase (AST) were found to be higher than the normal values. In the patients with oral hypoglycaemic agent, the values for platelet, EDW, monocyte, monocyte percentage, total bilirubin, direct bilirubin, AST, and C-reactive protein (CRP) were higher than the normal values. However, the values regarding hemoglobin, hematocrit, and erythrocyte were lower than the normal values in both patient groups. In addition, the values regarding other hematological and biochemical parameters measured were in their normal ranges. Moreover, serum ferritin levels were lower, and the values for mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), lymphocyte, monocyte, and monocyte percentage were significantly higher in the pediatric patients with SCA than the patients with BTM receiving DFX (P < 0.05). The differences between patient groups for the other parameters were not statistically different.
Table 5.
Hematological and biochemical parameters in deferasirox-treated pediatric patients with beta thalassemia major or sickle cell anemia
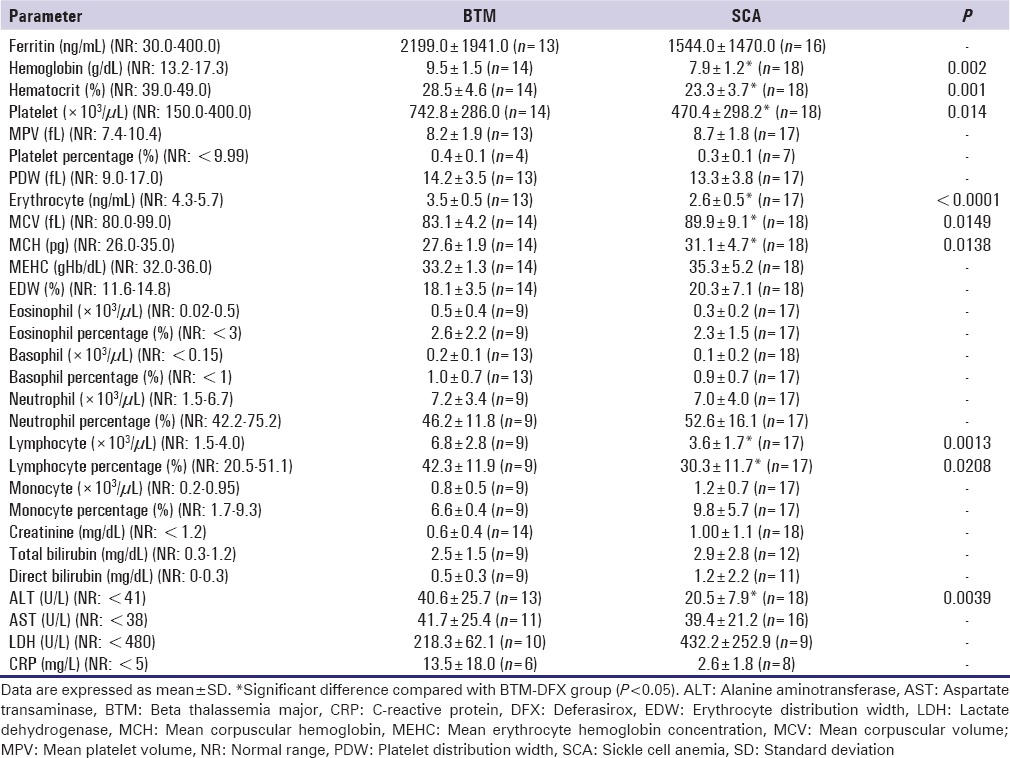
The parameters for adult patients with BTM or SCA who received DFX are shown in Table 6. Especially, mean serum ferritin levels were significantly higher than the normal values (30.0–400.0 ng/mL) in the patients receiving DFX (BTM: 2199.0 ± 1941.0 ng/mL, n = 13; SCA: 1544.0 ± 1470.0 ng/mL, n = 16) (P < 0.05). In the DFX-treated patients with BTM, the values regarding platelet, EDW, basophil, neutrophil, lymphocyte, total bilirubin, direct bilirubin, AST, and CRP were higher than the normal values. The values regarding platelet, EDW, monocyte, monocyte percentage, total bilirubin, direct bilirubin, and AST were found to be higher than the normal values in the DFX-treated patients with SCA. The values regarding hemoglobin, hematocrit, and erythrocyte were lower in the DFX-treated patients with BTM or SCA. In the DFX-treated patients, the values for hemoglobin, hematocrit, platelet, erythrocyte, lymphocyte, lymphocyte percentage, and ALT were lower, and MCV and MCH were significantly higher in the patients with SCA than the patients with BTM (P < 0.05). The differences between patient groups for the other parameters were not statistically different.
Table 6.
Hematological and biochemical parameters in deferasirox-treated adult patients with beta thalassemia major or sickle cell anemia
Satisfaction with iron chelation therapy
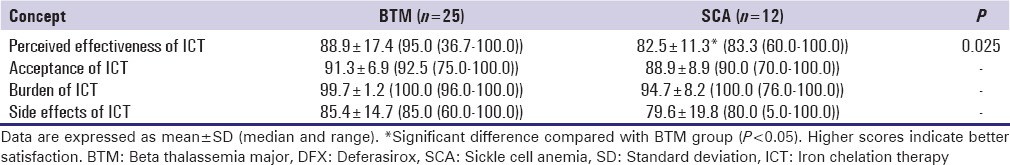
Table 7 shows ICT satisfaction summary scores regarding compliance level of DFX-treated pediatric patients with BTM or SCA. In particular, the mean scores in the patients with BTM ranged from 99.7 ± 1.2 (n = 25) for the burden of ICT to 85.4 ± 14.7 (n = 25) the side effects of ICT. Similarly, the scores ranged from 94.7 ± 8.2 (n = 12) for the burden of ICT to 85.4 ± 14.7 (n = 25) for the side effects of ICT in the patients with SCA. When compared with the scores of the patients with BTM, the scores for perceived effectiveness of ICT was significantly lower in the patients with SCA (P < 0.05). The differences between patient groups for the other scales were not statistically different.
Table 7.
Iron chelation therapy satisfaction summary scores (%) in deferasirox-treated pediatric patients with beta thalassemia major or sickle cell anemia
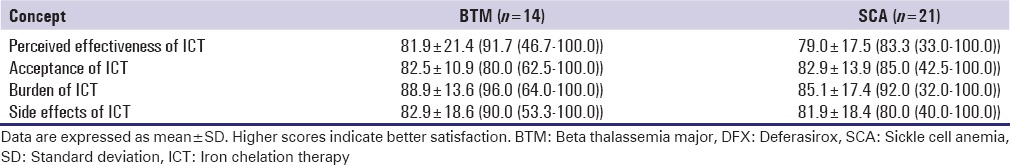
The ICT scores for adult patients with BTM or SCA who received DFX are presented in Table 8. In particular, the mean scores in the DFX-treated patients with BTM ranged from 88.9 ± 13.6 (n = 14) for the burden of ICT to 81.9 ± 21.4 (n = 14) for the perceived effectiveness of ICT. Similarly, the scores in the DFX-treated patients with SCA ranged from 85.1 ± 17.4 (n = 21) for the burden of ICT to 79.0 ± 17.5 (n = 21) the perceived effectiveness of ICT. The differences between patient groups for the other scales were not statistically different.
Table 8.
Iron chelation therapy satisfaction summary scores (%) in deferasirox-treated adult patients with beta thalassemia major or sickle cell anemia
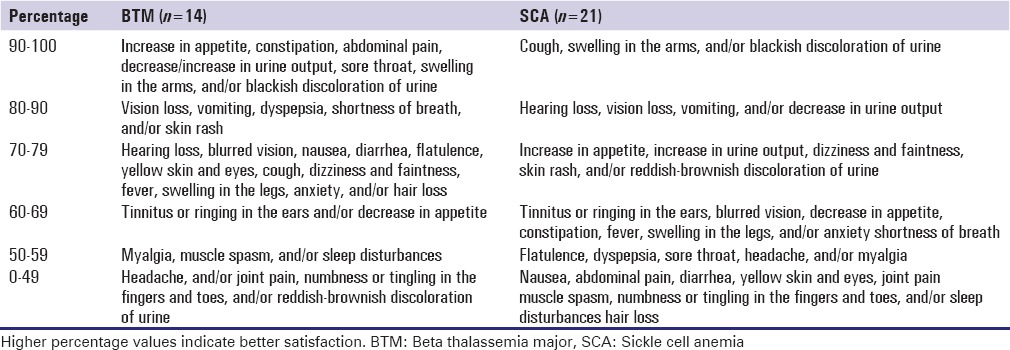
Tables 9 and 10 detail the proportional distribution of side effects in the DFX-treated pediatric and adult patients with BTM or SCA. No serious side effects necessitating discontinuation or interruption of therapy in the patients were reported, and no patients died during the study.
Table 9.
Proportional distribution of side effects in deferasirox-treated pediatric patients with beta thalassemia major or sickle cell anemia
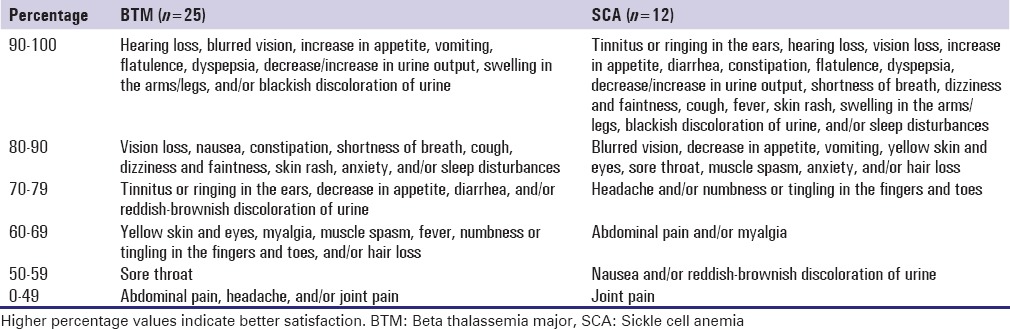
Table 10.
Proportional distribution of side effects in deferasirox-treated adult patients with beta thalassemia major or sickle cell anemia
Discussion
The purpose of this single-center observational study was to evaluate quality of life, clinical effectiveness, and satisfaction in pediatric and adult patients with BTM and SCA receiving DFX chelation therapy to contribute to their treatment and support process. The results of the present study indicate that the DFX-treated pediatric and adult patients with BTM or SCA are not achieving their target hematological marker thresholds (mainly serum ferritin levels) despite long-term treatment for iron overload. In addition, DFX chelation therapy appears to negatively impact their HRQOL so that the patient's satisfaction with ICT is generally poor.
Iron overload is a major concern in patients with congenital (e.g., transfusion-dependent thalassemia [including BTM], nontransfusion-dependent thalassemia [including beta thalassemia intermedia], SCA, fanconi anemia, hemolytic anemia, and sideroblastic anemia) and acquired (e.g., aplastic anemia, red cell aplasia, neoplastic diseases, and bone marrow transplantation) anemias for whom regular transfusions are needed.[2,6] Untreated transfusional iron load results in damage to the liver, endocrine organs, and most importantly to the heart. International guidelines for management of BTM and SCA concur on achieving a target serum ferritin of 1.000–2.500 μg/L and <1.000 μg/L, respectively.[3,33] In patients with iron overload as a result of regular blood transfusions because of BTM and SCA, oral chelating agents (e.g. DFX and DFP) are preferred over DFO because of their ease of administration, lesser side effects and better compliance. On the other hand, it takes months, even years, to reduce serum ferritin levels to a safe range. Combinations of chelators are often used in cases of high iron overload. Patients sometimes switch from one chelator to another for a variety of reasons, including worsening health status because of iron overload, side effects, and personal preference. In fact, life expectancy is directly related to the quality of chelation therapy and poor compliance to treatment increases the risk of complications and shortens survival. Serum ferritin measurement is useful for close and frequent patient monitoring to indicate changes in iron burden and determine current treatment needs. In the case of increased ferritin levels, dosage may be lowered and patient preference in choice of chelator can be better accommodated. On the other hand, all forms of treatment can be inconvenient, time-consuming, and result in unpleasant side effects, all which could potentially impact physical and emotional functioning of patients.[2,3,6,9,13,14,30,34] In our study, the DFX-treated pediatric and adult patients with BTM or SCA were heavy iron overloaded in agreement with previous reports.[20,26,35,36,37,38,39,40,41,42] The lack of treatment may explain the high ferritin levels. The increased serum ferritin levels were also associated with abnormalities in hematological and biochemical parameters. For instance, in the DFX-treated patients with BTM or SCA, the values regarding platelet, platelet percentage, MCH, EDW, basophil, neutrophil, lymphocyte, monocyte, monocyte percentage, total bilirubin, direct bilirubin, ALT, AST, and CRP were found to be higher than the normal values. On the other hand, the values regarding hemoglobin, hematocrit, and/or erythrocyte were lower than the normal values in the patients. Furthermore, serum ferritin levels were lower, and the values for MCV, MCH, lymphocyte, monocyte, and monocyte percentage were higher in the pediatric patients with SCA than the patients with BTM receiving DFX. In the DFX-treated adult patients, the values for hemoglobin, hematocrit, platelet, PDW, lymphocyte, lymphocyte percentage, and ALT were lower, and MCV and MCH were higher in the patients with SCA than the patients with BTM. Therefore, it appears that in addition to their side effects on hematopoietic and hepatic functions, DFX is not to be effective in reducing serum ferritin levels in the pediatric and adult patients with BTM or SCA.
HRQOL involves several aspects which include domains related to emotional, physical, mental, and social functioning and focuses on the impact health status has on quality of life. Supporting healthy emotional functioning is important not only to psychological well-being but also to physical health as it may impact compliance to medical regimens. The importance of the CHQ-PF50 and SF-36 questionnaires and the results of the individual scales on the actions that should be taken for pediatric and adult patients with thalassemia or SCD have been reported.[8,20,21,23,24] On the other hand, there is a little-published data on HRQOL in DFX-treated pediatric and adult patients with BTM or SCA.[20,21] Overall, our findings regarding quality of life and satisfaction with ICT indicate that the patients with BTM or SCA had lower scores. For instance, the highest CHQ-PF50 scores were found to be for the family activities (86.0%) and the health transition (85.0%) in the DFX-treated pediatric patients with BTM or SCA, respectively. The highest SF-36 score was for the physical functioning (81%) in the DFX-treated adult patients with BTM. In the patients with SCA, the highest score was found to be for the general health perception (58.3%) in the DFX group. It is also notable that the scores for general health, physical functioning, role/social limitations-physical, parent impact-time, and family activities were lower, and the scores for health transition were higher in the DFX-treated pediatric patients with SCA than the patients with BTM. Regarding satisfaction with ICT, when compared with the scores of the DFX-treated pediatric patients with BTM, the scores for perceived effectiveness of ICT was lower in the patients with SCA. It seems that poor compliance to DFX chelation therapy in these patients is probably due to a complex combination of psychological/social/demographic factors, living with a chronic disease, concomitant diseases/conditions and drug use, and new challenges related to improved life expectancy in the diseases. It is also possible that problems with treatment regimen and side effects appear to be common causes of poor compliance to DFX chelation therapy in these patients. Overall, our findings suggest that the patients are not achieving their target serum ferritin thresholds despite chronic treatment for iron overload, ICT appears to negatively impact their HRQOL, and compliance to ICT is poor. These findings are not surprising in the context of studies on poor compliance to ICT.[7,8,18,20,21,23,24,27,43,44] Therefore, the results are clinically meaningful and infer that changes need to be made to DFX chelation therapy for patients with iron overload.
Conclusions
This study provides some evidence for differences in the limitations of quality of life and satisfaction among patients with BTM or SCA depending on the DFX chelation therapy. Overall, the patients involved in the study had not achieved target serum ferritin thresholds despite long-term treatment for iron overload with DFX chelation therapy. Observed compliance to DFX was generally poor, and treatment appeared to negatively impact the quality of life and satisfaction of the patients. Our data also suggest that majority of the patients and/or their parents do not know about the importance of their medication. This study highlights the importance of providing pediatric and adult patients with BTM or SCA with the optimal chelation treatment based on their individual needs, in order to increase the HRQOL and decrease the presence of metabolic, endocrine, hepatic, renal, and cardiac comorbidities in addition to side effects, leading to increased compliance, and thus resulting in optimal clinical benefit. In addition, our results emphasize the need of involvement of a multidisciplinary team (including physicians, pharmacists, psychologists, nurse specialists, and health educators) in the management of patients with these diseases. Health care providers should be aware of the importance of monitoring iron load with timely initiation of DFX chelation therapy, and ongoing adjustments to chelation regimens and/or transfusion methods in response to these measurements. Future research are needed to determine the demographic and clinical variables most likely to be associated with effective reductions in iron overload as well as strategies (e.g., combining two iron chelators, interventions for patient education about the tolerability of chelation, development of new oral chelators) to decrease hospitalizations, improve compliance to ICT of the patients, and reduce morbidity and mortality.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The results of this study were included in the Ankara University Health Sciences Institute Interdisiplinary Clinical Pharmacy Program Master's Thesis of Pharm. M. S. Sefika Pinar Senol.
References
- 1.Anie KA, Massaglia P. Psychological therapies for thalassaemia. Cochrane Database Syst Rev. 2014;3:CD002890. doi: 10.1002/14651858.CD002890.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aydinok Y, Kattamis A, Viprakasit V. Current approach to iron chelation in children. Br J Haematol. 2014;165:745–55. doi: 10.1111/bjh.12825. [DOI] [PubMed] [Google Scholar]
- 3.Cappellini MD, Cohen A, Porter J, Taher A, Viprakasit V, editors. Guidelines for the Management of Transfusion Dependent Thalassaemia (TDT) 3rd ed. Nicosia, CY: Thalassaemia International Federation; 2014. [PubMed] [Google Scholar]
- 4.Coates TD. Physiology and pathophysiology of iron in hemoglobin-associated diseases. Free Radic Biol Med. 2014;72:23–40. doi: 10.1016/j.freeradbiomed.2014.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Finotti A, Breda L, Lederer CW, Bianchi N, Zuccato C, Kleanthous M, et al. Recent trends in the gene therapy of ß-thalassemia. J Blood Med. 2015;6:69–85. doi: 10.2147/JBM.S46256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoffbrand AV, Taher A, Cappellini MD. How I treat transfusional iron overload. Blood. 2012;120:3657–69. doi: 10.1182/blood-2012-05-370098. [DOI] [PubMed] [Google Scholar]
- 7.Javaid A, Khushab M, Mahmood KT, Zaka M. Benefits of pharmaceutical care in thalassemia. J Biomed Sci Res. 2011;3:322–31. [Google Scholar]
- 8.Lee TA, von Riedemann S, Tricta F. Cost-utility of chelators in transfusion-dependent ß-thalassemia major patients: A review of the pharmacoeconomic literature. Expert Rev Pharmacoecon Outcomes Res. 2014;14:651–60. doi: 10.1586/14737167.2014.927314. [DOI] [PubMed] [Google Scholar]
- 9.Marsella M, Borgna-Pignatti C. Transfusional iron overload and iron chelation therapy in thalassemia major and sickle cell disease. Hematol Oncol Clin North Am. 2014;28:703–27. doi: 10.1016/j.hoc.2014.04.004. vi. [DOI] [PubMed] [Google Scholar]
- 10.Mettananda S, Gibbons RJ, Higgs DR. α-Globin as a molecular target in the treatment of ß-thalassemia. Blood. 2015;125:3694–701. doi: 10.1182/blood-2015-03-633594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lucania G, Vitrano A, Filosa A, Maggio A. Chelation treatment in sickle-cell-anaemia: Much ado about nothing? Br J Haematol. 2011;154:545–55. doi: 10.1111/j.1365-2141.2011.08769.x. [DOI] [PubMed] [Google Scholar]
- 12.Vermylen C. Sickle cell anaemia: Current therapies. Transfus Apher Sci. 2013;49:151–4. doi: 10.1016/j.transci.2013.07.018. [DOI] [PubMed] [Google Scholar]
- 13.Brittenham GM. Iron-chelating therapy for transfusional iron overload. N Engl J Med. 2011;364:146–56. doi: 10.1056/NEJMct1004810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cario H, Janka-Schaub G, Janssen G, Jarisch A, Strauss G, Kohne E. Recent developments in iron chelation therapy. Klin Padiatr. 2007;219:158–65. doi: 10.1055/s-2007-973845. [DOI] [PubMed] [Google Scholar]
- 15.Porter JB, Garbowski M. The pathophysiology of transfusional iron overload. Hematol Oncol Clin North Am. 2014;28:683–701. doi: 10.1016/j.hoc.2014.04.003. vi. [DOI] [PubMed] [Google Scholar]
- 16.Ozdogan H, Ruperto N, Kasapçopur O, Bakkaloglu A, Arisoy N, Ozen S, et al. The Turkish version of the childhood health assessment questionnaire (CHAQ) and the child health questionnaire (CHQ) Clin Exp Rheumatol. 2001;19(4 Suppl 23):S158–62. [PubMed] [Google Scholar]
- 17.Payne KA, Rofail D, Baladi JF, Viala M, Abetz L, Desrosiers MP, et al. Iron chelation therapy: Clinical effectiveness, economic burden and quality of life in patients with iron overload. Adv Ther. 2008;25:725–42. doi: 10.1007/s12325-008-0085-z. [DOI] [PubMed] [Google Scholar]
- 18.Wrotniak BH, Schall JI, Brault ME, Balmer DF, Stallings VA. Health-related quality of life in children with sickle cell disease using the child health questionnaire. J Pediatr Health Care. 2014;28:14–22. doi: 10.1016/j.pedhc.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Demiral Y, Ergor G, Unal B, Semin S, Akvardar Y, Kivircik B, et al. Normative data and discriminative properties of short form 36 (SF-36) in Turkish urban population. BMC Public Health. 2006;6:247. doi: 10.1186/1471-2458-6-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gollo G, Savioli G, Balocco M, Venturino C, Boeri E, Costantini M, et al. Changes in the quality of life of people with thalassemia major between 2001 and 2009. Patient Prefer Adherence. 2013;7:231–6. doi: 10.2147/PPA.S42133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goulas V, Kourakli-Symeonidis A, Camoutsis C. Comparative effects of three iron chelation therapies on the quality of life of greek patients with homozygous transfusion-dependent Beta-thalassemia. ISRN Hematol 2012. 2012 doi: 10.5402/2012/139862. 139862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pinar R. Reliability and construct validity of the SF-36 in Turkish cancer patients. Qual Life Res. 2005;14:259–64. doi: 10.1007/s11136-004-2393-3. [DOI] [PubMed] [Google Scholar]
- 23.Rofail D, Viala M, Gater A, Abetz-Webb L, Baladi JF, Cappellini MD. An instrument assessing satisfaction with iron chelation therapy: Psychometric testing from an open-label clinical trial. Adv Ther. 2010;27:533–46. doi: 10.1007/s12325-010-0049-y. [DOI] [PubMed] [Google Scholar]
- 24.Trachtenberg FL, Gerstenberger E, Xu Y, Mednick L, Sobota A, Ware H, et al. Relationship among chelator adherence, change in chelators, and quality of life in thalassemia. Qual Life Res. 2014;23:2277–88. doi: 10.1007/s11136-014-0671-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 26.Al-Khabori M, Bhandari S, Al-Huneini M, Al-Farsi K, Panjwani V, Daar S. Side effects of deferasirox iron chelation in patients with beta thalassemia major or intermedia. Oman Med J. 2013;28:121–4. doi: 10.5001/omj.2013.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arboretti R, Tognoni G, Alberti D Italian Colaborative Group on Thalassarmia. Pharmacosurveillance and quality of care of thalassaemic patients. A large scale epidemiological survey. Eur J Clin Pharmacol. 2001;56:915–22. doi: 10.1007/s002280000251. [DOI] [PubMed] [Google Scholar]
- 28.Prakash A, Aggarwal R. Thalassemia major in adults: Short stature, hyperpigmentation, inadequate chelation, and transfusion-transmitted infections are key features. N Am J Med Sci. 2012;4:141–4. doi: 10.4103/1947-2714.93886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Blinder MA, Vekeman F, Sasane M, Trahey A, Paley C, Duh MS. Age-related treatment patterns in sickle cell disease patients and the associated sickle cell complications and healthcare costs. Pediatr Blood Cancer. 2013;60:828–35. doi: 10.1002/pbc.24459. [DOI] [PubMed] [Google Scholar]
- 30.Porter JB, Evangeli M, El-Beshlawy A. Challenges of adherence and persistence with iron chelation therapy. Int J Hematol. 2011;94:453–60. doi: 10.1007/s12185-011-0927-3. [DOI] [PubMed] [Google Scholar]
- 31.Telfer P, Constantinidou G, Andreou P, Christou S, Modell B, Angastiniotis M. Quality of life in thalassemia. Ann N Y Acad Sci. 2005;1054:273–82. doi: 10.1196/annals.1345.035. [DOI] [PubMed] [Google Scholar]
- 32.Ware JE, Jr, Gandek B, Kosinski M, Aaronson NK, Apolone G, Brazier J, et al. The equivalence of SF-36 summary health scores estimated using standard and country-specific algorithms in 10 countries: Results from the IQOLA project. International quality of life assessment. J Clin Epidemiol. 1998;51:1167–70. doi: 10.1016/s0895-4356(98)00108-5. [DOI] [PubMed] [Google Scholar]
- 33.Ghosh K, Colah R, Manglani M, Choudhry VP, Verma I, Madan N, et al. Guidelines for screening, diagnosis and management of hemoglobinopathies. Indian J Hum Genet. 2014;20:101–19. doi: 10.4103/0971-6866.142841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yacobovich J, Tamary H. Thalassemia major and sickle cell disease in adolescents and young adults. Acta Haematol. 2014;132:340–7. doi: 10.1159/000360235. [DOI] [PubMed] [Google Scholar]
- 35.Belini Junior E, da Silva DG, Torres Lde S, de Almeida EA, Cancado RD, Chiattone C, et al. Oxidative stress and antioxidant capacity in sickle cell anaemia patients receiving different treatments and medications for different periods of time. Ann Hematol. 2012;91:479–89. doi: 10.1007/s00277-011-1340-y. [DOI] [PubMed] [Google Scholar]
- 36.Cancado R, Olivato MC, Bruniera P, Szarf G, de Moraes Bastos R, Rezende Melo M, et al. Two-year analysis of efficacy and safety of deferasirox treatment for transfusional iron overload in sickle cell anemia patients. Acta Haematol. 2012;128:113–8. doi: 10.1159/000338560. [DOI] [PubMed] [Google Scholar]
- 37.Elalfy MS, Adly AM, Wali Y, Tony S, Samir A, Elhenawy YI. Efficacy and safety of a novel combination of two oral chelators deferasirox/deferiprone over deferoxamine/deferiprone in severely iron overloaded young beta thalassemia major patients. Eur J Haematol. 2015;95:411–20. doi: 10.1111/ejh.12507. [DOI] [PubMed] [Google Scholar]
- 38.Kwiatkowski JL, Cohen AR, Garro J, Alvarez O, Nagasubramanian R, Sarnaik S, et al. Transfusional iron overload in children with sickle cell anemia on chronic transfusion therapy for secondary stroke prevention. Am J Hematol. 2012;87:221–3. doi: 10.1002/ajh.22228. [DOI] [PubMed] [Google Scholar]
- 39.Makis A, Chaliasos N, Alfantaki S, Karagouni P, Siamopoulou A. Chelation therapy with oral solution of deferiprone in transfusional iron-overloaded children with hemoglobinopathies. Anemia 2013. 2013 doi: 10.1155/2013/121762. 121762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Piga A, Longo F, Origa R, Roggero S, Pinna F, Zappu A, et al. Deferasirox for cardiac siderosis in ß-thalassaemia major: A multicentre, open label, prospective study. Br J Haematol. 2014;167:423–6. doi: 10.1111/bjh.12987. [DOI] [PubMed] [Google Scholar]
- 41.Soliman A, Yassin M, Al Yafei F, Al-Naimi L, Almarri N, Sabt A, et al. Longitudinal Study on liver functions in patients with thalassemia major before and after deferasirox (DFX) therapy. Mediterr J Hematol Infect Dis. 2014;6:e2014025. doi: 10.4084/MJHID.2014.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Totadri S, Bansal D, Bhatia P, Attri SV, Trehan A, Marwaha RK. The deferiprone and deferasirox combination is efficacious in iron overloaded patients with ß-thalassemia major: A prospective, single center, open-label study. Pediatr Blood Cancer. 2015;62:1592–6. doi: 10.1002/pbc.25533. [DOI] [PubMed] [Google Scholar]
- 43.Jordan LB, Vekeman F, Sengupta A, Corral M, Guo A, Duh MS. Persistence and compliance of deferoxamine versus deferasirox in Medicaid patients with sickle-cell disease. J Clin Pharm Ther. 2012;37:173–81. doi: 10.1111/j.1365-2710.2011.01276.x. [DOI] [PubMed] [Google Scholar]
- 44.Trachtenberg F, Vichinsky E, Haines D, Pakbaz Z, Mednick L, Sobota A, et al. Iron chelation adherence to deferoxamine and deferasirox in thalassemia. Am J Hematol. 2011;86:433–6. doi: 10.1002/ajh.21993. [DOI] [PMC free article] [PubMed] [Google Scholar]


