Abstract
Background:
Several studies using functional magnetic resonance imaging (fMRI) and positron emission tomography (PET) have indicated that cognitive remediation therapy (CRT) might improve cognitive function by changing brain activations in patients with schizophrenia. However, the results were not consistent in these changed brain areas in different studies. The present activation likelihood estimation (ALE) meta-analysis was conducted to investigate whether cognitive function change was accompanied by the brain activation changes, and where the main areas most related to these changes were in schizophrenia patients after CRT. Analyses of whole-brain studies and whole-brain + region of interest (ROI) studies were compared to explore the effect of the different methodologies on the results.
Methods:
A computerized systematic search was conducted to collect fMRI and PET studies on brain activation changes in schizophrenia patients from pre- to post-CRT. Nine studies using fMRI techniques were included in the meta-analysis. Ginger ALE 2.3.1 was used to perform meta-analysis across these imaging studies.
Results:
The main areas with increased brain activation were in frontal and parietal lobe, including left medial frontal gyrus, left inferior frontal gyrus, right middle frontal gyrus, right postcentral gyrus, and inferior parietal lobule in patients after CRT, yet no decreased brain activation was found. Although similar increased activation brain areas were identified in ALE with or without ROI studies, analysis including ROI studies had a higher ALE value.
Conclusions:
The current findings suggest that CRT might improve the cognition of schizophrenia patients by increasing activations of the frontal and parietal lobe. In addition, it might provide more evidence to confirm results by including ROI studies in ALE meta-analysis.
Keywords: Activation Likelihood Estimation, Cognitive Remediation Therapy, Meta-analysis, Schizophrenia
INTRODUCTION
Schizophrenia is a serious psychiatric illness that about 1% of the population suffers from it.[1] Cognitive deficits are a core feature of schizophrenia, affects up to 80% of the patients,[2] which were among the most treatment-resistant symptoms and associated with the poor social function.[3,4,5] Though traditional pharmacotherapy of schizophrenia has positive effects on symptom reduction, especially positive symptom, the effects on neurocognitive and social cognitive impairments are limited with current medications.[5]
Cognitive remediation is defined as a nonpharmaceutical and psychosocial treatment modality and a promising treatment with an ultimate goal of enhancing the cognitive function of schizophrenia.[6,7,8] So far the most commonly reported deficits of schizophrenia are mainly associated with attention, working memory, learning ability, processing speed, and executive/reasoning functions.[9,10,11,12] Many studies have demonstrated that cognitive remediation is effective in improving the function of schizophrenia.[6,13,14,15,16,17]
Recently, the neuroimaging methods are widely adopted to evaluate the effect of cognitive remediation therapy (CRT) and explore the neuromechanism of cognitive dysfunction of schizophrenia. With the help of functional magnetic resonance imaging (fMRI) and positron emission tomography (PET), researchers indicated that cognitive training could improve participants’ performance by increasing activation in the middle frontal gyrus, the superior and inferior parietal cortices.[18,19,20] Studies evaluating brain activation changes from pre- to post-CRT can use either whole-brain or region of interest ([ROI], a priori hypothesized region or functionally defined regions from previous studies) study approach. Traditional opinions believe that only whole-brain studies should be included in activation likelihood estimation (ALE) analysis because including ROI studies might bias findings toward these hypothesized regions. However, a recent ALE study suggested that future studies might consider conducting and reporting both ROI and whole-brain voxel-wise analyses.[21]
So far the changes of brain areas in schizophrenia after CRT reported in different studies are variable, and the underlying neurobiological mechanisms that support cognitive improvement are largely unknown. Many researchers also have reported different increased activation regions in schizophrenia patients from pre- to post-CRT. fMRI studies found that compared with the control group, only schizophrenia patients had increased brain activation after CRT in regions associated with working memory, particularly in the inferior frontal gyrus.[15,22,23] Randomized study found that compared with both patients and healthy controls, patients with CRT had increased activation in attention and working memory networks, including the dorsolateral prefrontal cortex (PFC), the anterior cingulate, and the frontopolar cortex.[24] Recently, studies found that following treatment, patients who received CRT exhibited increased ability to activate the prefrontal regions that could improve attention and working memory function.[25] Besides, researchers found that following cognitive exercises, patients’ verbal working memory performance improved and the task-related left inferior frontal cortex activation increased.[23] In contrast to the increased brain activation, decreased brain activation areas were also found in some studies. Some researchers reported that compared with computer games, schizophrenia patients with cognitive plus social cognitive training showed decreased activation in medial superior frontal gyrus.[26,27] A working memory training study found that short-term learning of stimulus material was associated with significant performance improvements and exponential signal decreases in a fronto-parieto-cerebellar network in both schizophrenia patients and healthy volunteers. Patients exhibited stronger signal decreases which were relative to controls in anterior cingulate, middle and superior temporal, superior frontal, and posterior parietal regions.[28]
ALE is widely used in neuroimaging meta-analysis, but study selection criteria vary from whole-brain studies to both whole-brain and ROI studies, which might induce differences in the results. Recently, an ALE meta-analysis found increased activation in the lateral and medial PFC, parietal cortex, insula, and the caudate and thalamus.[29] However, decreased activation and the effect of different study methods (ROI vs. whole-brain + ROI) were not mentioned in the study. In our study, ALE was used to conduct regions that changed brain activation from pre- to post-training. Both increased and decreased brain activation were systematically reviewed to conclude how the brain activation will change from pre- to post-CRT in patients with schizophrenia. At the same time, we compare the results of whole-brain studies with those of whole-brain + ROI studies to explore the effectiveness of different study methods.
METHODS
Literature search and selection
Computerized literature search was conducted through online scientific databases: PubMed/Medline, EMBASE, Web of Science, and PsycINFO. The literature search was performed in March 2015, with no restrictions on the date of publication. Search terms included “cogniti*,” “rehabilitation,” “remediation,” “training,” or “enhancement,” with different combinations of “magnetic resonance imaging (MRI),” “fMRI” or “PET,” and “schizophrenia”. Two persons selected studies independently according to the following inclusion criterion: (1) they were peer-reviewed research articles; (2) they were written in English; (3) samples of participants diagnosed with schizophrenia using research diagnostic criteria[30] diagnostic and statistical manual of mental disorders III (DSM-III), DSM-III-R, DSM-IV, or ICD-10; (4) the data of regions that reported changed activation were available. The study by Wexler et al.[23] was discarded as the data were not available, though we contacted the authors for the missing data; (5) studies assessing brain activation changes from pre- to post-CRT on patients with schizophrenia, respectively; (6) a pre- to post-improvement in at least one cognitive or social cognitive domain in patients after CRT; (7) brain activations were tested by MRI, fMRI, or PET. Six hundred and fifty-eight articles were identified through the literature search. Two authors used exactly the same include and exclude standards to retrieve the papers independently. Any disagreement was discussed to make sure that papers were chosen following those standards we made ahead of schedule. If we could not reach an agreement, we turn to an expert to confirm whether the study should be included or not. One article was added through hand searching. The papers that we retrieved were all peer-reviewed articles. Academic dissertation, conference paper, and review were all discarded. For the above criterion, the articles holding the most relevant information were provided in Table 1.[15,24,25,26,27,28,31,32,33] The procedure of selecting articles was listed in Figure 1.
Table 1.
Summary of the selected studies in the present meta-analysis
| Studies | Participants, n | Age of patients (years), mean ± SD | Gender (male/female, n) | Medication (%) | Contrast | fMRI/PET analyses | Type (chronic/FES) | Coordinate space | Cognitive training task | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| CRT patients | Control group | ||||||||||
| Non-CRT patients | Healthy control | ||||||||||
| Wykes et al., 2002[15] | 3 | 6 | 6 | 35 | 18/0 | 100 | b | Whole brain | Chronic | Talairach | Working memory |
| Bor et al., 2011[25] | 8 | 9 | 15 | 30.5 ± 8.3 | 22/10 | 100 | b | Whole brain | Chronic | MNI | Spatial working memory |
| Vianin et al., 2014[33] | 8 | 8 | 0 | 27.6 ± 8.2 | 13/3 | 87.5 | ab | Whole brain | Chronic | MNI | Executive function |
| Hooker et al., 2013[26] | 11 | 11 | 0 | 51.2 ± 5.8 | 18/4 | 100 | bc | Whole brain | Chronic | MNI | Social cognition |
| Hooker et al., 2012[27] | 11 | 11 | 0 | 51.2 ± 5.8 | 18/4 | 100 | bc | Whole brain | Chronic | MNI | Social cognition |
| Habel et al., 2010[32] | 10 | 10 | 10 | 31.4 ± 7.8 | 30/0 | 100 | b | Whole brain | Chronic | MNI | Affect recognition |
| Edwards et al., 2010[31] | 22 | 0 | 14 | 34.8 ± 9.7 | 29/7 | 100 | b | ROI | Chronic | Talairach | Cognitive control |
| Haut et al., 2010[24] | 9 | 9 | 9 | 36.4 ± 9.2 | 20/7 | 100 | b | ROI | Chronic | Talairach | Attention and working memory |
| Koch et al., 2007[28] | 13 | 0 | 13 | 26.2 ± 5.4 | 16/10 | 92.3 | c | ROI | Chronic | Talairach | Working memory |
a: CRT patients increased activation from pre- to post-training; b: Compared to non-CRT patients, CRT patients increased brain activation from pre- to post-training; c: Compared to non-CRT patients CRT patients decreased brain activation from pre- to post-training. The selected 2 studies of Hooker et al. used the same participant; we collapsed the data from the two studies into one experiment entry in Ginger ALE. In the study of Wykes, among the 6 participants only 3 participants received benefit from the CRT, so we used 3 as the subject number for the analyses. In the study of Haut et al., 10 participants in each patient group only 9 imaged. CRT: Cognitive remediation therapy; fMRI: Functional magnetic resonance imaging; PET: Photon emission tomography; FES: First-episode schizophrenia; ROI: Region of interest; SD: Standard deviation; MNI: Montreal Neurological Institute.
Figure 1.
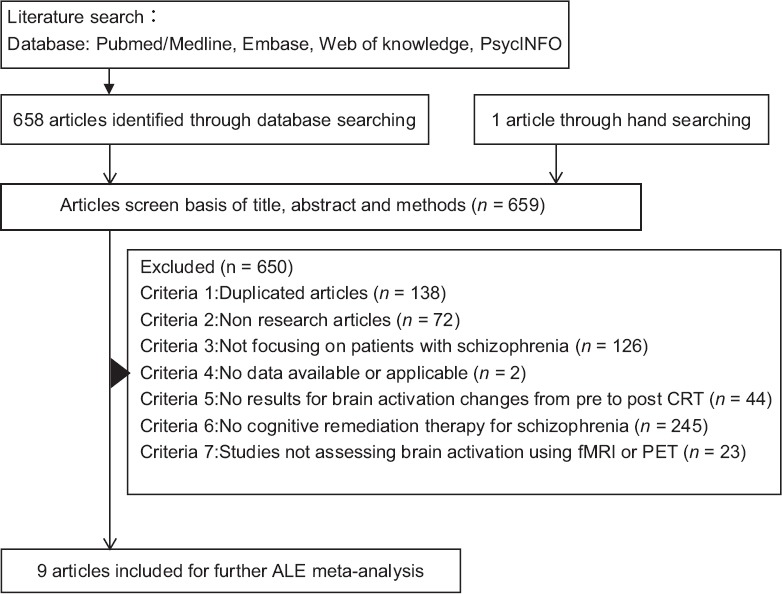
The procedure of studies searching. CRT: Cognitive remediation therapy; fMRI: Functional magnetic resonance imaging; PET: Photon emission tomography; ALE: Activation likelihood estimation.
In order to evaluate how methodological differences affect results, analysis of all studies reported coordinates in standard space and whole-brain studies only were conducted separately. Previous ALE meta-analysis found many commonalities between two analyses and suggested we not only include whole-brain, but also ROI studies.[21]
The contrast of the selected studies included: (1) compared with non-CRT patients, CRT patients showed increased brain activation from pre- to post-training; (2) compared with non-CRT patients, CRT patients showed decreased brain activation from pre- to post-training.
Statistical analysis
The meta-analysis was conducted by applying the Ginger ALE software[34] with the up-to-date revision Ginger ALE 2.3.1[35,36,37] (http://www.brainmap.org). The analyses were conducted in Talairach space, the coordinates that originally reported in MNI[38] space were converted to Talairach space using the Lancaster transform (“icbm2tal”).[39,40] Then, they were listed as text files for each focus to be imported into Ginger ALE 2.3.1 and analyzed separately.
ALE is a coordinate-based method to identify concordance among results from different functional imaging studies. Coordinates were modeled with a three-dimensional Gaussian distribution. Coordinate-based meta-analysis is that the reported foci in the selected studies should be treated as spatial probability distributions around them.[34] Ginger ALE provides random effects model instead of a fixed effects model.
Clusters identified in the meta-analysis were obtained after controlling the statistical significance with a false discovery rate[36] at P < 0.05 and applying a minimum cluster size of 200 mm3. This threshold has been used in former ALE analyses.[41,42] Significant clusters were overlaid onto an anatomical Talairach template, colin_tlrc_1 × 1 × 1.nii (http://www.brainmap.org/ale), using the Mango software (version 3.2.7, 2014, Research Imaging Institute, University of Texas Health Science Center, TX, USA; http://www.ric.uthscsa.edu/mango).
RESULTS
Table 1 showed that nine studies with a total of 204 subjects (active = 84, patient control = 53, healthy control = 67) met the inclusion criteria for the ALE meta-analysis and 104 foci that reported changed brain activation in CRT patients from pre- to post-training. Six studies were whole-brain analyses while three studies used ROI approaches. Although these studies differed in cognitive training approaches and cognitive domains, they had the same purpose of improving schizophrenia patients’ cognitive or social function. Only Vianinia's study reported CRT group had an increased brain activation from pre- to post-training; besides, compared with the non-CRT group, CRT group showed increased brain activation after treatment, excluding baseline differences. The other selected studies all reported Group × Time interaction in brain activation changes. Among the selected studies, three of them reported decreased activation from pre- to post-training, compared with non-CRT patients. In order to confirm our results, meta-analysis was made with and without ROI studies separately. ALE analysis of foci that reported increased and decreased brain activation was conducted separately.
Areas increased activation from pre- to post-cognitive remediation therapy
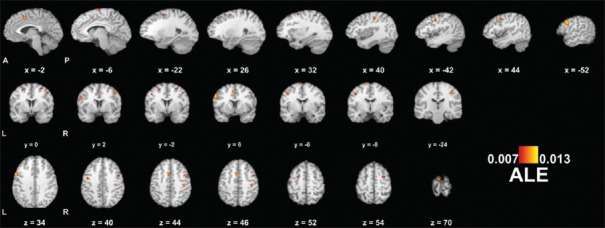
All studies (whole-brain +ROI)
A total of 90 foci in seven studies (the two studies by Hooker et al. were conducted only once as they used the same participants) exhibited increased brain activation in schizophrenia patients after CRT. Table 2 presented the significantly increased brain regions. Eight significant clusters were found with increased brain activation from pre- to post-training, compared with non-CRT patients [Table 2 and Figure 2], (1) the left inferior frontal gyrus (1120 mm3, BA9); (2) the left medial frontal gyrus (512 mm3, BA32); (3) the right middle frontal gyrus (464 mm3, BA6); (4) the left precentral gyrus (416 mm3, BA6); (5) the right postcentral gyrus (416 mm3, BA2); (6) the left medial frontal gyrus (352 mm3, BA6); (7) the right sub-gyral (296 mm3, BA6); and (8) the left sub-gyral (216 mm3, BA6). These increased brain regions were mainly located in the frontal lobe and the parietal lobe. The final maps with significant regions of increased brain activation in patients with schizophrenia after cognitive remediation therapy among all the selected studies were displayed in Figure 2.[15,24,25,26,27,31,32,33]
Table 2.
Increased brain activation from all studies in CRT patients compared with non-CRT patients from pre- to post-training
| Cluster number | Volume (mm3) | Peak ALE value | Talairach coordinates | Label | Brodmann area | Contributed number of foci | ||
|---|---|---|---|---|---|---|---|---|
| X | Y | Z | ||||||
| 1 | 1120 | 0.013162 | −52 | 6 | 34 | Left, inferior frontal gyrus | 9 | 4 |
| 2 | 512 | 0.012385 | −2 | 6 | 46 | Left, medial frontal gyrus | 32 | 2 |
| 3 | 464 | 0.010715 | 44 | 2 | 44 | Right, middle frontal gyrus | 6 | 3 |
| 4 | 416 | 0.009548 | −42 | −6 | 40 | Left, precentral gyrus | 6 | 3 |
| 5 | 416 | 0.010841 | 40 | −24 | 44 | Right, postcentral gyrus | 2 | 3 |
| 6 | 352 | 0.010826 | −6 | −8 | 70 | Left, medial frontal gyrus | 6 | 2 |
| 7 | 296 | 0.009176 | 26 | −2 | 54 | Right, sub-gyral | 6 | 2 |
| 0.007607 | 32 | 0 | 54 | Right, middle frontal gyrus | 6 | |||
| 8 | 216 | 0.009195 | −22 | −2 | 52 | Left, sub-gyral | 6 | 1 |
The peak coordinates were in the Talairach system (right; left). Clusters identified in the meta-analysis were obtained after controlling the false discovery rate corrected at P<0.05 and applying a minimum cluster size of 200 mm3. CRT: Cognitive remediation therapy; ALE: Activation likelihood estimation.
Figure 2.
Regions of increased brain activation in patients with pre- to post-training from all studies. Significance threshold with a false discovery rate corrected at P < 0.05. Peak coordinates (x, y, z) in Talairach space are presented. A: Anterior; P: Posterior; R: Right; L: Left; ALE: Activation likelihood estimation.
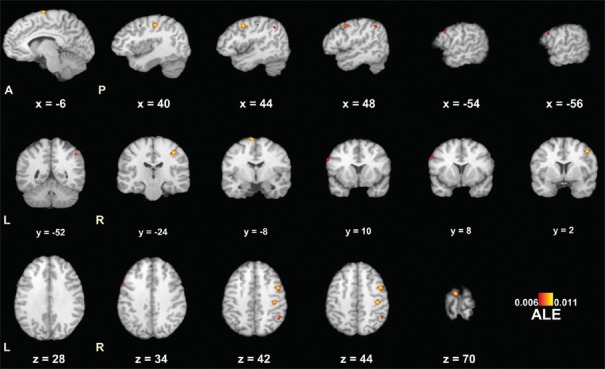
Whole-brain studies
In order to evaluate the effects of whole-brain studies and whole-brain + ROI studies, a separate analysis of six whole-brain studies (40 subjects) was conducted. Five clusters were found with increased brain activation in CRT patients from pre- to post-training, compared with non-CRT patients [Table 3 and Figure 3],[15,24,25,26,27,31] (1) the right middle frontal gyrus (568 mm3, BA6); (2) the right postcentral gyrus (552 mm3, BA2); (3) the left medial frontal gyrus (440 mm3, BA6); (4) the right inferior parietal lobule (280 mm3, BA40); (5) the left middle frontal gyrus (208 mm3, BA9).
Table 3.
Increased brain activation from whole-brain studies only in CRT patients compared with non-CRT patients from pre- to post-training
| Cluster number | Volume (mm3) | Peak ALE value | Talairach coordinates | Label | Brodmann area | Contributed number of foci | ||
|---|---|---|---|---|---|---|---|---|
| X | Y | Z | ||||||
| 1 | 568 | 0.010697 | 44 | 2 | 44 | Right, middle frontal gyrus | 6 | 3 |
| 2 | 552 | 0.010837 | 40 | −24 | 44 | Right, postcentral gyrus | 2 | 1 |
| 3 | 440 | 0.010826 | −6 | −8 | 70 | Left, medial frontal gyrus | 6 | 1 |
| 4 | 280 | 0.007419 | 48 | −52 | 42 | Right, inferior parietal lobule | 40 | 2 |
| 5 | 208 | 0.007155 | −54 | 8 | 34 | Left, middle frontal gyrus | 9 | 2 |
| 0.006542 | −56 | 10 | 28 | Left, inferior frontal gyrus | 9 | |||
The peak coordinates were in the Talairach system (right; left). Clusters identified in the meta-analysis were obtained after controlling the false discovery rate corrected at P<0.05 and applying a minimum cluster size of 200 mm3. CRT: Cognitive remediation therapy; ALE: Activation likelihood estimation.
Figure 3.
Regions of increased brain activation in patients with pre- to post-training from whole-brain studies only. Significance threshold with a false discovery rate at P < 0.05. Peak coordinates (x, y, z) in Talairach space are presented. A: Anterior; P: Posterior; R: Right; L: Left; ALE: Activation likelihood estimation.
According to the results of two analyses, we found that most of the increased brain activation regions were the same, and the results from all studies indicated that more regions exhibit increased brain activation from pre- to post-training. These different regions conducted from the two results locate in the right inferior parietal lobule, left middle frontal gyrus, and bilateral sub-gyrus.
Former neuroimaging studies found a decreased activation in the middle frontal gyrus and medial superior frontal gyrus which participated in emotion perception from pre- to post-training.[26,27] In addition, a study on practice information retrieval of working memory found patients showed significantly stronger activation decreases which were in anterior cingulate, middle and superior temporal, superior frontal, and posterior parietal regions. These regions were related to working memory processing and response preparation.[28] No significant cluster was found either in analysis of all studies or in whole-brain studies only.
DISCUSSION
In the present study, a voxel-wide and coordinate-based meta-analysis was performed to assess whether consistent brain activation changes were presented in nine fMRI studies. The main finding of the ALE meta-analysis was that patients with schizophrenia demonstrated an increase in activation from pre- to post-CRT and these regions were mainly in frontal and parietal lobe [Table 2]. It supports the idea that it is necessary to take into account the potential mechanisms of changes in brain activity in response to cognitive improvement.
Increased brain activation
Consistently increased brain activation in medial frontal gyrus, middle frontal gyrus, precentral and postcentral gyrus, and sub-gyrus was found in schizophrenia patients from pre- to post-CRT, though the training approaches were different. These regions were mainly located in frontal and parietal lobe which were considered as a key region of cognitive function.[15,33,43] Compared with healthy controls, these regions had shown hyper- or hypo-activation before training in patients.[44,45,46,47] Increased brain activity in medial and middle frontal gyrus after CRT related to the improvement in working memory performance, increased activity in left inferior frontal might compensate schizophrenia patients in helping them catch up with healthy controls on cognitive tasks.[24,48] Areas of pre- and post-central gyrus are related to emotion recognition, and the increased activity could be explained by facilitating emotion recognition through stimulation, a process in which people understand the feelings of others by generating those feelings in themselves.[26,27]
Overall, the increased activation demonstrated in our study provided preliminary evidence of training-induced neuroplasticity in schizophrenia patients. The findings substantiate prior data showed that increased activation was found in frontal regions (BA6/9) after cognitive training and concluded that frontal regions were related to cognition of working memory. A former study in reality monitoring system found increased activity in medial PFC and postcentral gyrus in patients with schizophrenia and is consistent with the results presented in our study.[10,26] Higher activation in right inferior frontal gyrus was also demonstrated and relative to the unsuccessful attempts of patients who inhibited preservative answers in Wisconsin Card Sorting Test (WCST) learning test; besides, activation in right inferior gyrus was associated with inhibition.[49,50]
Recently, ALE meta-analysis comparing pre- and post-training brain activation has showed increased activity in the lateral and medial PFC, parietal cortex, insula, and the caudate and thalamus, though the training intensity and approaches were different.[29] These were consistent with our findings that increased brain activation exhibited from pre- to post-CRT and were related to the improvement of cognition.
Decreased brain activation
Among the selected studies, only three reported decreased activation from pre- to post-training. The regions with decreased activation were in anterior cingulate, middle and superior temporal, superior frontal, and posterior parietal; in addition, these regions might reflect learning related behavioral performance.[28] Besides, deactivation in the central executive network and default mode network were reported in former studies which might reflect working memory and cognitive and emotion control.[51,52] Some of the studies selected in the meta-analysis had not found decreased activation, observed but had not reported, or had not examined deactivation regions, therefore, when three studies that reported decreased activation after CRT were conducted by ALE, there was no significant region identified. Further studies should also examine decreased activation from pro- to post-CRT. Further by combining increased and decreased activation will help us to better understand how the brain activation will change after CRT.
Effect of different study methodologies
Studies measuring the brain activation changes often use an ROI (a prior hypothesized region or functionally defined regions from previous studies or meta-analysis) or whole-brain methods. Authors have different opinions on excluding ROI studies from ALE meta-analysis. Among the former ALE meta-analysis, some included all studies reporting coordinates in standard space,[53] while some restricted analyses to only whole-brain studies.[54,55] Instead of excluding ROI studies, our meta-analysis evaluated the impact of different methods on results. Therefore, analyses with or without ROI studies were conducted separately. Finally, eight clusters were found increased activation from all studies, while five clusters were found increased activation from whole-brain studies only [Tables 2 and 3]. Comparing the two results, there are many commonalities between them. The clusters identified without ROI analyses were subjected to those found in the meta-analysis of both whole-brain and ROI studies, so ROI analyses could overlook some regions and favor others which indicated that the ROI studies might not cause bias in the results. Meanwhile, analyses with ROI studies had a higher ALE value which could provide more evidence to confirm the conclusion. What is more, ALE analysis including both whole-brain and ROI studies was also conducted by Goghari to demonstrate relatives of schizophrenia patients with brain abnormalities in prefrontal cortical activation during executive processing,[21] and concluded that ROI studies did not cause bias in the results. From the above findings, we suggest that ROI studies could be included in future ALE studies.
Limitations
There are several limitations in the present study. Firstly, the number of selected studies was restricted by current numbers of relevant publications. Only three studies reported decreased activation, and no significant clusters were found with decreased activation. Secondly, because of the limitation of the study method we could not put other factors (such as medication and the course of disease) as covariates into ALE analyses and could not assess the effect of these factors. Moreover, we could not create a funnel plot to evaluate the publication bias of the selected studies. Thirdly, the correlation between brain activation changes and cognitive improvement could not be made because of the study method. Further studies with larger samples and follow-up studies are needed.
Financial support and sponsorship
This study was supported by the grants from the National Nature Science Foundation of China (No. 81372122, No. 31200844, No. 81171267 and No. 81361120403).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Peng Lyu
REFERENCES
- 1.Barch DM, Carter CS, Braver TS, Sabb FW, MacDonald A, 3rd, Noll DC, et al. Selective deficits in prefrontal cortex function in medication-naive patients with schizophrenia. Arch Gen Psychiatry. 2001;58:280–8. doi: 10.1001/archpsyc.58.3.280. doi: 10.1001/archpsyc.58.3.280. [DOI] [PubMed] [Google Scholar]
- 2.van Os J, Kapur S. Schizophrenia. Lancet. 2009;374:635–45. doi: 10.1016/S0140-6736(09)60995-8. doi: 10.1016/s0140-6736(09)60995-8. [DOI] [PubMed] [Google Scholar]
- 3.Green MF. Stimulating the development of drug treatments to improve cognition in schizophrenia. Annu Rev Clin Psychol. 2007;3:159–80. doi: 10.1146/annurev.clinpsy.3.022806.091529. doi: 10.1146/annurev.clinpsy.3.022806.091529. [DOI] [PubMed] [Google Scholar]
- 4.Medalia A, Saperstein AM. Does cognitive remediation for schizophrenia improve functional outcomes? Curr Opin Psychiatry. 2013;26:151–7. doi: 10.1097/YCO.0b013e32835dcbd4. doi: 10.1097/YCO.0b013e32835dcbd4. [DOI] [PubMed] [Google Scholar]
- 5.Barlati S, Deste G, De Peri L, Ariu C, Vita A. Cognitive remediation in schizophrenia: Current status and future perspectives. Schizophr Res Treatment. 2013;2013:156084. doi: 10.1155/2013/156084. doi: 10.1155/2013/156084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Medalia A, Choi J. Cognitive remediation in schizophrenia. Neuropsychol Rev. 2009;19:353–64. doi: 10.1007/s11065-009-9097-y. doi: 10.1007/s11065-009-9097-y. [DOI] [PubMed] [Google Scholar]
- 7.Thorsen AL, Johansson K, Løberg EM. Neurobiology of cognitive remediation therapy for schizophrenia: A systematic review. Front Psychiatry. 2014;5:103. doi: 10.3389/fpsyt.2014.00103. doi: 10.3389/fpsyt.2014.00103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wykes T, van der Gaag M. Is it time to develop a new cognitive therapy for psychosis –Cognitive remediation therapy (CRT)? Clin Psychol Rev. 2001;21:1227–56. doi: 10.1016/s0272-7358(01)00104-0. doi: 10.1093/schbul/sbr064. [DOI] [PubMed] [Google Scholar]
- 9.Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996;153:321–30. doi: 10.1176/ajp.153.3.321. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- 10.Subramaniam K, Luks TL, Fisher M, Simpson GV, Nagarajan S, Vinogradov S. Computerized cognitive training restores neural activity within the reality monitoring network in schizophrenia. Neuron. 2012;73:842–53. doi: 10.1016/j.neuron.2011.12.024. doi: 10.1016/j.neuron.2011.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Takahashi H, Iwase M, Nakahachi T, Sekiyama R, Tabushi K, Kajimoto O, et al. Spatial working memory deficit correlates with disorganization symptoms and social functioning in schizophrenia. Psychiatry Clin Neurosci. 2005;59:453–60. doi: 10.1111/j.1440-1819.2005.01398.x. doi: 10.1111/j.1440-1819.2005.01398.x. [DOI] [PubMed] [Google Scholar]
- 12.Kurtz MM, Wexler BE, Fujimoto M, Shagan DS, Seltzer JC. Symptoms versus neurocognition as predictors of change in life skills in schizophrenia after outpatient rehabilitation. Schizophr Res. 2008;102:303–11. doi: 10.1016/j.schres.2008.03.023. doi: 10.1016/j.schres.2008.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Green MF, Penn DL, Bentall R, Carpenter WT, Gaebel W, Gur RC, et al. Social cognition in schizophrenia: An NIMH workshop on definitions, assessment, and research opportunities. Schizophr Bull. 2008;34:1211–20. doi: 10.1093/schbul/sbm145. doi: 10.1093/schbul/sbm145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kern RS, Glynn SM, Horan WP, Marder SR. Psychosocial treatments to promote functional recovery in schizophrenia. Schizophr Bull. 2009;35:347–61. doi: 10.1093/schbul/sbn177. doi: 10.1093/schbul/sbn177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wykes T, Brammer M, Mellers J, Bray P, Reeder C, Williams C, et al. Effects on the brain of a psychological treatment: Cognitive remediation therapy: Functional magnetic resonance imaging in schizophrenia. Br J Psychiatry. 2002;181:144–52. doi: 10.1017/s0007125000161872. doi: 10.1192/bjp.181.2.144. [DOI] [PubMed] [Google Scholar]
- 16.Wykes T, Spaulding WD. Thinking about the future cognitive remediation therapy –What works and could we do better? Schizophr Bull. 2011;37(Suppl 2):S80–90. doi: 10.1093/schbul/sbr064. doi: 10.1093/schbul/sbr064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Franck N, Demily C. Improving functional outcome of schizophrenia with cognitive remediation. Presse Med. 2015;44:292–7. doi: 10.1016/j.lpm.2014.06.031. doi: 10.1016/j.lpm.2014.06.031. [DOI] [PubMed] [Google Scholar]
- 18.Klingberg T, Fernell E, Olesen PJ, Johnson M, Gustafsson P, Dahlström K, et al. Computerized training of working memory in children with ADHD –A randomized, controlled trial. J Am Acad Child Adolesc Psychiatry. 2005;44:177–86. doi: 10.1097/00004583-200502000-00010. doi: 10.1097/00004583-200502000-00010. [DOI] [PubMed] [Google Scholar]
- 19.Olesen PJ, Westerberg H, Klingberg T. Increased prefrontal and parietal activity after training of working memory. Nat Neurosci. 2004;7:75–9. doi: 10.1038/nn1165. doi: 10.1038/nn1165. [DOI] [PubMed] [Google Scholar]
- 20.Westerberg H, Klingberg T. Changes in cortical activity after training of working memory –A single-subject analysis. Physiol Behav. 2007;92:186–92. doi: 10.1016/j.physbeh.2007.05.041. doi: 10.1016/j.physbeh.2007.05.041. [DOI] [PubMed] [Google Scholar]
- 21.Goghari VM. Executive functioning-related brain abnormalities associated with the genetic liability for schizophrenia: An activation likelihood estimation meta-analysis. Psychol Med. 2011;41:1239–52. doi: 10.1017/S0033291710001972. doi: 10.1017/S0033291710001972. [DOI] [PubMed] [Google Scholar]
- 22.Silver H, Feldman P, Bilker W, Gur RC. Working memory deficit as a core neuropsychological dysfunction in schizophrenia. Am J Psychiatry. 2003;160:1809–16. doi: 10.1176/appi.ajp.160.10.1809. doi: 10.1176/appi.ajp.160.10.1809. [DOI] [PubMed] [Google Scholar]
- 23.Wexler BE, Anderson M, Fulbright RK, Gore JC. Preliminary evidence of improved verbal working memory performance and normalization of task-related frontal lobe activation in schizophrenia following cognitive exercises. Am J Psychiatry. 2000;157:1694–7. doi: 10.1176/appi.ajp.157.10.1694. doi: org/10.1176/appi.ajp.157.10.1694. [DOI] [PubMed] [Google Scholar]
- 24.Haut KM, Lim KO, MacDonald A., 3rd Prefrontal cortical changes following cognitive training in patients with chronic schizophrenia: Effects of practice, generalization, and specificity. Neuropsychopharmacology. 2010;35:1850–9. doi: 10.1038/npp.2010.52. doi: 10.1038/npp.2010.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bor J, Brunelin J, d’Amato T, Costes N, Suaud-Chagny MF, Saoud M, et al. How can cognitive remediation therapy modulate brain activations in schizophrenia?An fMRI study. Psychiatry Res. 2011;192:160–6. doi: 10.1016/j.pscychresns.2010.12.004. doi: 10.1016/j.pscychresns.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 26.Hooker CI, Bruce L, Fisher M, Verosky SC, Miyakawa A, D’Esposito M, et al. The influence of combined cognitive plus social-cognitive training on amygdala response during face emotion recognition in schizophrenia. Psychiatry Res. 2013;213:99–107. doi: 10.1016/j.pscychresns.2013.04.001. doi: 10.1016/j.pscychresns.2013.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hooker CI, Bruce L, Fisher M, Verosky SC, Miyakawa A, Vinogradov S. Neural activity during emotion recognition after combined cognitive plus social cognitive training in schizophrenia. Schizophr Res. 2012;139:53–9. doi: 10.1016/j.schres.2012.05.009. doi: 10.1016/j.schres.2012.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koch K, Wagner G, Nenadic I, Schachtzabel C, Roebel M, Schultz C, et al. Temporal modeling demonstrates preserved overlearning processes in schizophrenia: An fMRI study. Neuroscience. 2007;146:1474–83. doi: 10.1016/j.neuroscience.2007.03.021. doi: 10.1016/j.neuroscience.2007.03.021. [DOI] [PubMed] [Google Scholar]
- 29.Ramsay IS, MacDonald AW., 3rd Brain correlates of cognitive remediation in schizophrenia: Activation likelihood analysis shows preliminary evidence of neural target engagement. Schizophr Bull. 2015;41:1276–84. doi: 10.1093/schbul/sbv025. doi: 10.1093/schbul/sbv025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spitzer HL, Johnston JM. Characterization of phosphatidate phosphohydrolase activity associated with isolated lamellar bodies. Biochim Biophys Acta. 1978;531:275–85. doi: 10.1016/0005-2760(78)90209-6. doi: 10.1016/0005-2760(78)90209-6. [DOI] [PubMed] [Google Scholar]
- 31.Edwards BG, Barch DM, Braver TS. Improving prefrontal cortex function in schizophrenia through focused training of cognitive control. Front Hum Neurosci. 2010;4:32. doi: 10.3389/fnhum.2010.00032. doi: 10.3389/Fnhum.2010.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Habel U, Koch K, Kellermann T, Reske M, Frommann N, Wölwer W, et al. Training of affect recognition in schizophrenia: Neurobiological correlates. Soc Neurosci. 2010;5:92–104. doi: 10.1080/17470910903170269. doi: 10.1080/17470910903170269. [DOI] [PubMed] [Google Scholar]
- 33.Vianin P, Urben S, Magistretti P, Marquet P, Fornari E, Jaugey L. Increased activation in Broca's area after cognitive remediation in schizophrenia. Psychiatry Res. 2014;221:204–9. doi: 10.1016/j.pscychresns.2014.01.004. doi: 10.1016/j.pscychresns.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 34.Turkeltaub PE, Eden GF, Jones KM, Zeffiro TA. Meta-analysis of the functional neuroanatomy of single-word reading: Method and validation. Neuroimage. 2002;16(3 Pt 1):765–80. doi: 10.1006/nimg.2002.1131. doi: 10.1006/nimg.2002.1131. [DOI] [PubMed] [Google Scholar]
- 35.Eickhoff SB, Laird AR, Grefkes C, Wang LE, Zilles K, Fox PT. Coordinate-based activation likelihood estimation meta-analysis of neuroimaging data: A random-effects approach based on empirical estimates of spatial uncertainty. Hum Brain Mapp. 2009;30:2907–26. doi: 10.1002/hbm.20718. doi: 10.1002/hbm.20718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Laird AR, Fox PM, Price CJ, Glahn DC, Uecker AM, Lancaster JL, et al. ALE meta-analysis:Controlling the false discovery rate and performing statistical contrasts. Hum Brain Mapp. 2005;25:155–64. doi: 10.1002/hbm.20136. doi: 10.1002/hbm.20136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Turkeltaub PE, Eickhoff SB, Laird AR, Fox M, Wiener M, Fox P. Minimizing within-experiment and within-group effects in activation likelihood estimation meta-analyses. Hum Brain Mapp. 2012;33:1–13. doi: 10.1002/hbm.21186. doi: 10.1002/hbm.21186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Collins DL, Neelin P, Peters TM, Evans AC. Automatic 3D intersubject registration of MR volumetric data in standardized Talairach space. J Comput Assist Tomogr. 1994;18:192–205. [PubMed] [Google Scholar]
- 39.Laird AR, Robinson JL, McMillan KM, Tordesillas-Gutiérrez D, Moran ST, Gonzales SM, et al. Comparison of the disparity between Talairach and MNI coordinates in functional neuroimaging data: Validation of the Lancaster transform. Neuroimage. 2010;51:677–83. doi: 10.1016/j.neuroimage.2010.02.048. doi: 10.1016/j.neuroimage.2010.02.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lancaster JL, Tordesillas-Gutiérrez D, Martinez M, Salinas F, Evans A, Zilles K, et al. Bias between MNI and Talairach coordinates analyzed using the ICBM-152 brain template. Hum Brain Mapp. 2007;28:1194–205. doi: 10.1002/hbm.20345. doi: 10.1002/Hbm.20345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jardri R, Pouchet A, Pins D, Thomas P. Cortical activations during auditory verbal hallucinations in schizophrenia: A coordinate-based meta-analysis. Am J Psychiatry. 2011;168:73–81. doi: 10.1176/appi.ajp.2010.09101522. doi: 10.1176/appi.ajp.2010.09101522. [DOI] [PubMed] [Google Scholar]
- 42.Li H, Chan RC, McAlonan GM, Gong QY. Facial emotion processing in schizophrenia: A meta-analysis of functional neuroimaging data. Schizophr Bull. 2010;36:1029–39. doi: 10.1093/schbul/sbn190. doi: 10.1093/schbul/sbn190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Penadés R, Boget T, Lomeña F, Mateos JJ, Catalán R, Gastó C, et al. Could the hypofrontality pattern in schizophrenia be modified through neuropsychological rehabilitation? Acta Psychiatr Scand. 2002;105:202–8. doi: 10.1034/j.1600-0447.2002.1o421.x. doi: 10.1034/j.1600-0447.2002.1o421.x. [DOI] [PubMed] [Google Scholar]
- 44.Callicott JH, Bertolino A, Mattay VS, Langheim FJ, Duyn J, Coppola R, et al. Physiological dysfunction of the dorsolateral prefrontal cortex in schizophrenia revisited. Cereb Cortex. 2000;10:1078–92. doi: 10.1093/cercor/10.11.1078. doi: 10.1093/cercor/10.11.1078. [DOI] [PubMed] [Google Scholar]
- 45.Karlsgodt KH, Sanz J, van Erp TG, Bearden CE, Nuechterlein KH, Cannon TD. Re-evaluating dorsolateral prefrontal cortex activation during working memory in schizophrenia. Schizophr Res. 2009;108:143–50. doi: 10.1016/j.schres.2008.12.025. doi: 10.1016/j.schres.2008.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Manoach DS. Prefrontal cortex dysfunction during working memory performance in schizophrenia: Reconciling discrepant findings. Schizophr Res. 2003;60:285–98. doi: 10.1016/s0920-9964(02)00294-3. doi: 10.1016/S0920-9964(02)00294-3. [DOI] [PubMed] [Google Scholar]
- 47.Van Snellenberg JX, Torres IJ, Thornton AE. Functional neuroimaging of working memory in schizophrenia: Task performance as a moderating variable. Neuropsychology. 2006;20:497–510. doi: 10.1037/0894-4105.20.5.497. doi: 10.1037/0894-4105.20.5.497.Supp. [DOI] [PubMed] [Google Scholar]
- 48.Pedersen A, Wilmsmeier A, Wiedl KH, Bauer J, Kueppers K, Koelkebeck K, et al. Anterior cingulate cortex activation is related to learning potential on the WCST in schizophrenia patients. Brain Cogn. 2012;79:245–51. doi: 10.1016/j.bandc.2012.03.007. doi: 10.1016/j.bandc.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 49.Konishi S, Hayashi T, Uchida I, Kikyo H, Takahashi E, Miyashita Y. Hemispheric asymmetry in human lateral prefrontal cortex during cognitive set shifting. Proc Natl Acad Sci U S A. 2002;99:7803–8. doi: 10.1073/pnas.122644899. doi: 10.1073/pnas.122644899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Robbins TW. Shifting and stopping: Fronto-striatal substrates, neurochemical modulation and clinical implications. Philos Trans R Soc Lond B Biol Sci. 2007;362:917–32. doi: 10.1098/rstb.2007.2097. doi: 10.1098/rstb.2007.2097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bush G, Luu P, Posner MI. Cognitive and emotional influences in anterior cingulate cortex. Trends Cogn Sci. 2000;4:215–22. doi: 10.1016/s1364-6613(00)01483-2. doi: 10.1016/S1364-6613(00)01483-2. [DOI] [PubMed] [Google Scholar]
- 52.Penadés R, Pujol N, Catalán R, Massana G, Rametti G, García-Rizo C, et al. Brain effects of cognitive remediation therapy in schizophrenia: A structural and functional neuroimaging study. Biol Psychiatry. 2013;73:1015–23. doi: 10.1016/j.biopsych.2013.01.017. doi: 10.1016/j.biopsych.2013.01.017. [DOI] [PubMed] [Google Scholar]
- 53.Achim AM, Lepage M. Episodic memory-related activation in schizophrenia: Meta-analysis. Br J Psychiatry. 2005;187:500–9. doi: 10.1192/bjp.187.6.500. doi: 10.1192/bjp.187.6.500. [DOI] [PubMed] [Google Scholar]
- 54.Ragland JD, Laird AR, Ranganath C, Blumenfeld RS, Gonzales SM, Glahn DC. Prefrontal activation deficits during episodic memory in schizophrenia. Am J Psychiatry. 2009;166:863–74. doi: 10.1176/appi.ajp.2009.08091307. doi: 10.1176/appi.ajp.2009.08091307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yan C, Yang T, Yu QJ, Jin Z, Cheung EF, Liu X, et al. Rostral medial prefrontal dysfunctions and consummatory pleasure in schizophrenia: A meta-analysis of functional imaging studies. Psychiatry Res. 2015;231:187–96. doi: 10.1016/j.pscychresns.2015.01.001. doi: 10.1016/j.pscychresns.2015.01.001. [DOI] [PubMed] [Google Scholar]