Abstract
Background
Although there is strong scientific, policy, and community support for community-engaged research (CEnR)—including community-based participatory research (CBPR)—the science of CEnR is still developing.
Objective
To describe structural differences in federally funded CEnR projects by type of research (i.e., descriptive, intervention, or dissemination/policy change) and race/ethnicity of the population served.
Methods
We identified 333 federally funded projects in 2009 that potentially involved CEnR, 294 principal investigators/project directors (PI/PD) were eligible to participate in a key informant (KI) survey from late 2011 to early 2012 that asked about partnership structure (68% response rate).
Results
The National Institute on Minority Health & Health Disparities (19.1%), National Cancer Institute (NCI; 13.3%), and the Centers for Disease Control and Prevention (CDC; 12.6%) funded the most CEnR projects. Most were intervention projects (66.0%). Projects serving American Indian or Alaskan Native (AIAN) populations (compared with other community of color or multiple-race/unspecified) were likely to be descriptive projects (p < .01), receive less funding (p < .05), and have higher rates of written partnership agreements (p < .05), research integrity training (p < .05), approval of publications (p < .01), and data ownership (p < .01). AIAN-serving projects also reported similar rates of research productivity and greater levels of resource sharing compared with those serving multiple-race/unspecified groups.
Conclusions
There is clear variability in the structure of CEnR projects with future research needed to determine the impact of this variability on partnering processes and outcomes. In addition, projects in AIAN communities receive lower levels of funding yet still have comparable research productivity to those projects in other racial/ethnic communities.
Keywords: Community-based participatory research, health disparities, health promotion, power sharing, structural dynamics, American Indian/Alaska Native research, dissemination/implementation, extramural funding
In the past two decades, the importance of stakeholder knowledge and participation in research addressing complex health problems has grown exponentially1 and is reflected in a number of major federal initiatives and engagement recommendations by the Patient Centered Outcomes Research Institute,2 the CDC’s Prevention Research Centers (PRCs),3,4 Agency for Healthcare Research and Quality (AHRQ)’s Practice-Based Research Networks,5 the Clinical Translational Science Awards,6,7 and the Community-Based Participatory Research Program Announcements from many of the National Institutes of Health (NIH)’s institutes and centers.8-11 Additionally, the Patient Protection and Affordability Care Act’s focus on eliminating disparities and reducing costs relies on CEnR to align academic center agendas with community priorities, enhance public trust, and build bidirectional capacity and empowerment especially among hard to reach populations.12 In CBPR, stakeholders participate equitably in all phases of the research process. Using a broader perspective, the NIH adopted the term CEnR, which involves collaboration to improve health, “regardless of the specific types or degrees of engagement.”13,14 This does not mean engagement is necessarily less than in CBPR, but that collaboration may not be based solely on equality. Although our focus started with CBPR projects that have an emphasis on shared leadership and partnership, we found a broader range of CEnR15 and, therefore, use the term ‘CEnR’ when describing our sample. We use CBPR when we focused specifically on CBPR principles or CBPR specific articles.
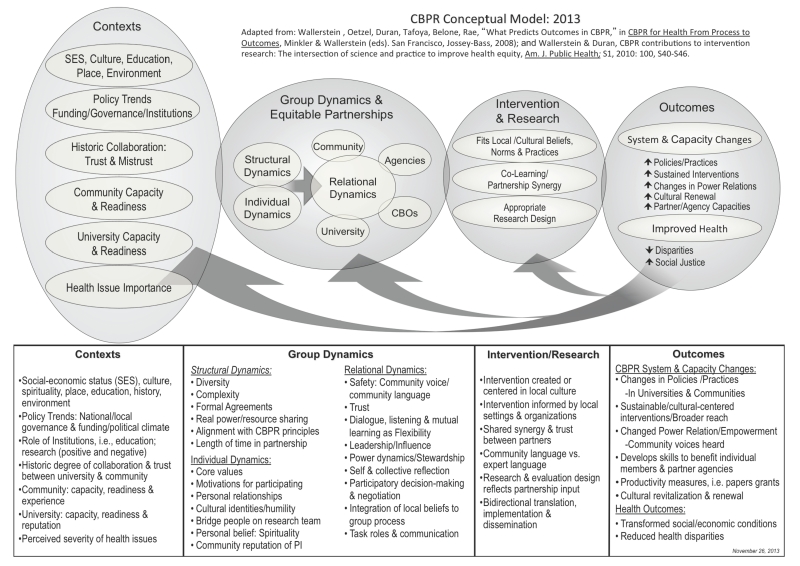
CEnR/CBPR initiatives advance these goals, in part, by addressing concerns with translation and dissemination. The NIH roadmap and policy documents from public health agencies and voluntary and professional organizations have identified the lack of uptake of scientific findings by clinical and community practitioners to be significant in having little impact on improving health and reducing health disparities. Consequently, the NIH has elevated the importance of translational research and has identified issues of context and external validity as central to the problem of the utilization of evidenced-based practices. Efficacy studies and randomized, controlled trials, which focus on internal validity, are necessary but not sufficient knowledge for translating and disseminating interventions to real-world settings with high variability in culture, context, and levels of acceptance.16-18 As a result, academic researchers, community and patient advocacy groups, and policy leaders argue for greater practitioner and community engagement in the research process to enhance the translation and dissemination of research findings, and thus help to reduce health disparities (Figure 1).1
Figure 1. CBPR conceptual Model 2013.
A key step in identifying how community engagement contributes to improved research outcomes is to identify and describe the structural dynamics of partnered projects. Wallerstein et al.’s CBPR conceptual model19 identifies important context features and structural dynamics (Figure 1) that purport to directly and indirectly affect overall outcomes. Structural dynamics refer to the partnership in terms of membership composition (i.e., organizational representation, demographic diversity) and level of complexity in agreements, policies, and resources used to guide CBPR partnerships. Partnerships differ in their structure; tribal partners, for example, often require formal tribal resolutions or memoranda of agreement, whereas other partnerships may use informal processes.20-22 Other factors, such as the degree of alignment among CBPR principles and expectations and the length of time the partnership has existed, may also influence the need for formal agreements. Diversity in partnerships may have great value for producing relevant and robust outcomes. However, differences in values and perspectives across partners may influence communication in research study teams, and thus partnerships may face challenges because of cross-cultural distance or lack of congruence in values, ethnic/racial identities, or in profession among partners. Higher complexity, such as that found with health coalitions or community-academic partnered centers—which address many issues with multiple organizations—may also pose challenges not seen in a more limited partnership that addresses one set of issues, such as immunizations with providers as partners.23 Increasingly, CBPR projects are realizing the importance of infrastructure or agreements for group decision making, and expectations on data sharing and dissemination.24-26
Despite the increase in CEnR, understanding the range of community engagement has remained largely theoretical.27,28 The first step, therefore, in studying CEnR and its impact on health, is to conduct an in-depth mapping of the variability of CEnR projects. Examining structural dynamics of partnerships per se, which has not been examined previously in the literature, helps to illustrate the range of project features and provides empirical data that goes beyond single CEnR projects.27 Given that these structural features provide context for a project, and may impact communication processes and outcomes of projects, research is needed to explore the variability of structural dynamics in CBPR projects.
The objective for this study was to explore the range of structural features across types of funding and population served by CEnR. Specifically, we 1) describe the funding differences in types of projects—descriptive projects, intervention projects, and other (policy change or dissemination projects; i.e., from the policies and trends oval in Figure 1), and 2) describe the structure of the partnership in terms of resource sharing, formal agreements, research integrity, and partners’ involvement in research (i.e., the structural dynamics oval/box in Figure 1) and their impact on a few intermediate outcomes. These structural characteristics were then analyzed to assess differences by race/ethnicity of the community engaged with the research.
METHODS
The Research for Improved Health study seeks to understand the ways community partners are engaged in their own health research and intervention projects.29 The overall study Research for Improved Health (RIH): A Study of Community–Academic Partnerships is a national, NIH-funded study that has sought to further the science of CBPR by exploring and explicating a theoretical model of CBPR linking context and partnering processes to outcomes at the individual, organizational, and social determinant levels.29 With its core research questions to assess the variability of CBPR projects across the nation, and to better understand how added value is created both for research and for improving health and health equity in AIAN communities, communities of color, and other disadvantaged communities, RIH chose a mixed methods approach, using in-depth interviews, focus groups, a project-level/KI survey and a partnership-level survey to deepen its understanding of CBPR contexts, partnership processes, and a broad range of outcomes.29 This article describes the project-level KI survey findings. This study includes a particular focus on tribal partnerships because they often have a different set of structural characteristics in research owing to tribal sovereignty, and partners explored how this structure, when compared with others, might lend insight into improving CBPR partnerships and reducing health disparities.
Partnership
Our partnership includes a national organization representing tribal communities across the United States, and academic partners from two universities. Funded under the NIH Native American Research Centers for Health (NARCH) mechanism, the primary grant recipient was the National Congress of American Indians Policy Research Center (NCAI) with subcontracts to the Universities of New Mexico and Washington (2009–2013). Funds were distributed evenly with each partner receiving about one third of total dollars. This partnership stemmed from the academic partners earlier pilot work (2006–2009) developing the CBPR model.27 The NCAI provided oversight and direction, developed collaboration policies, guided scholarship in governance, and assisted in instrument development, data collection, analyses planning, interpretation of findings and authored manuscripts. The University of New Mexico took the lead on the qualitative arm of seven case studies, and the University of Washington took the lead on the quantitative arm (reported here). Primary academic responsibilities included ensuring scientific integrity, data collection, and analyses. In addition, we had qualitative and quantitative advisory committees, referred to as Special Interest Groups (SPIGs), of four to six academic and community CBPR experts. The study protocol was approved by the two university institutional review boards (IRBs) and by the National Indian Health Service IRB.
Population
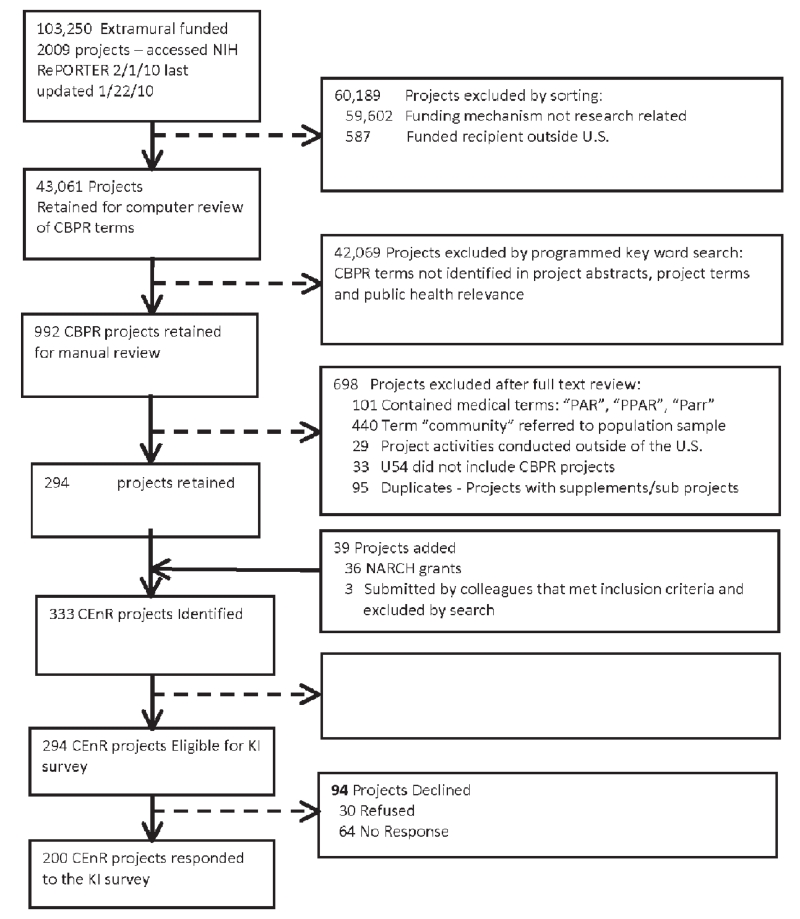
We conducted a national, cross-sectional, Internet survey of extramural CEnR partnerships funded in 2009 (Figure 2). To identify the CEnR project population, in February 2010, we downloaded all available information on federally funded projects active in 2009 from the NIH Research Portfolio Online Reporting Tools (RePORTER) database (n = 103,250).30 With help from the SPIGs, we identified the inclusion criteria. We retained U.S.-based research projects funded through R and U mechanisms (R01, R18, R24, R34, RC1, RC2, U01, U19, U26, U48, U54) with at least 2 years of funding remaining (n = 43,061). Using Python 3.1 programming, we searched the abstracts, key words, and specific aims to identify the following words in a variety of combinations: community, community-based, participatory, tribal, AIAN, action, engagement, research, tribally driven, CBPR, CEnR, and PAR (Participatory Action Research) (n = 992). Two members of the research team manually reviewed 10% of all project abstracts to verify the computer program’s accuracy of screening projects. Upon verification of accuracy, the two team members conducted the second phase by reviewing all abstracts. One member coded the projects into three categories: as “CEnR,” “possible CEnR,” or “not CEnR.” All projects falling within the “possible CEnR” or “not CEnR” categories were reviewed by the second member. Discrepancies between the two reviewers coding determination were decided on by team consensus. When in doubt whether the project would be considered CEnR (i.e., abstract referenced a community advisory board), we kept the project in the sample. In addition to the aforementioned review process, we consulted with the Indian Health Service, CDC, and NIH project officers as to whether there were key projects we should consider including. As a result, we added NARCH grants (n = 36) and individual research projects of the PRC, which were not in the original RePORTER database, resulting in 333 identified CEnR projects.
Figure 2. Selection Flowchart of the 2009 Computer-Identified CEnR Projects From NIH RePORTER Database.
KI = key informant survey; PI/PD = principle investigators or project directors.
Procedures
For this manuscript, we used the project-level data from the nested sampling design. First, the PI/PD took a 15-minute KI survey that collected objective project-related information (i.e., funding dates, budget amounts, use of formal agreements). The PI/PDs identified up to four project partners (one academic and three community) to complete the community-engaged survey. The community-engaged survey obtained information on perceptions of CBPR model constructs: group and relational dynamics and individual and project outcomes. Project-level data analyzed here include the KI survey data and the RePORTER database data.
Pretest, Pilot, and Cognitive Debriefing
We pretested the survey with study team and SPIG members who provided feedback to the appropriateness of measures, the timing and sequencing of measures, length of the survey, and recruitment procedures. They identified user-ability errors and glitches and made recommendations to refine formatting and the survey’s visual display. After making revisions, we conducted a pilot of the study procedures and cognitive debriefing interviews with two CEnR projects not funded in 2009. From the pilot and debriefing interviews, we clarified words and concepts and added in definitions to clarify meaning in the survey, reduced the length of the recruitment period, simplified the recruitment email (i.e., length and format), and revised the online survey formatting and flow. We changed the eligibility requirements to include English speakers with email and Internet access.
Survey Recruitment
Each project PI/PD was sent an invitation letter, $20.00 cash incentive, project information sheet, and consent form via U.S. mail. The survey consisted of up to five follow-up emails including contact via phone as needed. Surveys were conducted using DatStat Illume from November 2011 through August 2012. Of the 333 projects invited to participate, 137 projects contacted study staff 209 times with the following results: (a) clarified eligibility criteria (n = 35), (b) corrected email or mailing addresses (n = 33), (c) reported they were busy or wanted to discuss participation with their partners (n = 28), (d) reported technical problems(n = 28), (e) declined to participate (n = 28), (f) reported they had already completed the survey but were still getting email reminders for other projects for which they were PI/PD (n = 23), (g) reported they did not receive the invitation letter or incentive (n = 21), and (h) reported their project was not a CEnR (n = 11).
Survey participation
From the 333 identified CEnR projects, 294 self-identified as CEnR projects, of which 200 (68%) competed the KI survey (Figure 2). Of the 33 projects who self-screened out as not “CEnR/CBPR” projects, abstract review showed that 45.2% used the term “CBPR” or “participatory approach/planning methods” and 32.3% referred to “community partners.”
Measures
Guided by the CBPR conceptual model (Figure 1), we first identified project-level measures that included project descriptors and structural dynamics that could be collected via a KI survey or abstracted from RePORTER data. We obtained measures from a library of available CBPR measures that mapped onto constructs and domains represented in the CBPR conceptual model (see Pearson et al., 201131; also available at several websites: http://fcm.unm.edu/cpr/cbpr_project.html; http://narch.ncaiprc.org;http://iwri.org/health). In collaboration with our SPIG and off-site academic and community partners, we prioritized key measurable constructs to include in the survey. In addition, case study findings from the qualitative arm of the RIH study informed development of the scales. Almost all scales in the KI survey were created from this process and/or through consultation with SPIG members and partners on our team.
Project descriptive measures were primarily gathered from RePORTER and designed to assess the policy and trends in Figure 1. For projects embedded in centers such as the CDC, PRC, and the Indian Health Service funded NARCH projects PI/PD were asked to provide the information. Project descriptive measures included type of mechanism and were coded into five categories: (1) R01; (2) R18, R23, R24, R34, RC1, RC2; (3) U26 NARCH; (4) U48 PRCs; and (5) U01, U19, U54. The funding institute and center (IC) was coded separately if they represented 4% or more of the reporting ICs. ICs less than 4% were collapsed together; they included the AHRQ, Agency for Toxic Substances and Disease Registry (ATSDR),
COTPER, Coordinating Office for Terrorism Preparedness and Emergency Response (COTPER), Complementary and alternative medicine (CAM), National Center for Environmental Health (NCEH), National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), Center for Urban Horticulture (CUH), National Center for Research Resources (NCRR), Nuclear Energy Institute (NEI), National Human Genome Research Institute (NHGRI), National Institute of General Medical Sciences (NIGMS), National Institute for Occupational Safety and Health (NIOSH), National Institute of Allergy and Infectious Diseases (NIAID), National Institute of Dental and Craniofacial Research (NIDCR), National Institute of Nursing Research (NINR), National Institute of Aging (NIA), National Institute on Alcohol Abuse and Alcoholism (NIAAA), and United States Public Health Service (USPHS). Other project descriptors were total funding dollars, grant start and end dates, and type of project and population served. Types of project were classified as descriptive study (i.e., needs assessment, community profile, epidemiological study, secondary data analysis), intervention study (i.e., specific development and evaluation programs to reduce or address health disparities), and other (i.e., dissemination and implementation, policy analysis, efforts to change policies, or a systematic study of alternative public policies). When this information was missing, we reviewed the project abstract and project website when available and made the determination. Population served was coded first by computer generated coding, then confirmed by a study team member. Discrepancies were reviewed by a second coder and agreement was made by consensus. NARCH projects were coded as serving an AIAN population. When abstracts for PRC projects were not available, they were coded as no specific race or ethnicity. The race/ethnicity of the communities served by the projects included the following: (a) AIAN (n = 47); (b) African American (n = 20); (c) Asian American (n = 7); (d) Hispanic/Latino (n = 24); (e) no race/ethnicity specified (n = 85); and (f) multiple race/ethnicity (n = 17). Three categories were created for population served to balance distribution of cell sizes and retain enough power to conduct meaningful analysis: AIAN (included American Indian, Alaska Native, Native Hawaiians, and Pacific Islanders), other community of color (specified as African American, Asian American, or Hispanic), and the third category of not specified or multiple races and ethnicities. When the project served AIAN and one other group, the project was coded as serving AIAN. Other underserved group represented included physical (n = 7) and mental (n = 14) disabilities, and homeless populations (n = 2). The latter two groups were not mutually exclusive from race or ethnicity groups.
Structural dynamics included measures to address the structural dynamics elements within Figure 1: project features (12 items; e.g., confidence that the project will achieve its goals, length of partnership); resource and power sharing (four items; e.g., who hires personnel, decides how the resources are shared, coded as “sharing” when indicated both community and academic partners engaged in the activity as opposed to only community or academic or don’t know, and percent of resources allocated to community members); research integrity (three items; e.g., human subjects training, confidentiality agreements, guidelines on confidentiality); formal agreements (seven items; e.g., memorandum of understanding, resolutions, mission statement, conflict resolution, publication guidelines, data sharing agreement, student use of data); formal trainings or substantial discussions (eight items; e.g., cultural sensitivity and humility, self and collective reflection, privilege and power, and conflict resolution); and partnership roles and involvement (13 items; e.g., in each phase of the research process, items were coded 1 if actively engaged and 0 if served only as a consultants or not engaged). Concrete outcomes were also collected (four items; e.g., papers in press or published, additional research or funding) as well as PI demographics (e.g., race/ethnicity and gender).
Data Analysis
We described the project characteristics and funding institutes through descriptive statistics. We assess the difference between project type (descriptive, intervention, and other) and sample characteristics (funding mechanism, institutes and centers, and total funds awarded) and population served (a comparison of AIAN, other community of color, and “other”), and sample characteristics. We conducted analysis using logistic regressions for the dichotomous variables and linear regressions with a robust sandwich estimator of variance for the continuous variables. For the multinomial categorical variables, we used generalized linear model with a “mlogit” link function that identifies the multinomial response.32 When these models suggested significance, we followed up with Wald tests and F tests of the linear hypotheses after estimation to pinpoint group differences.
RESULTS
We first assessed the difference between CEnR projects’ PI/PDs who responded to the survey and those who did not respond. There were two important differences. Specifically, nonresponder projects compared with responder projects were more likely to be “other” (i.e., dissemination and policy change projects; p < .05) as opposed to a descriptive study or intervention, and were awarded more funding dollars (mean, $3.2 million vs. $2.5 million). There were no differences in responders and nonresponders by funding institutes and centers, length of project, or type of funding mechanism.
In Table 1, focusing on the policies and trends within Figure 1 and addressing our first objective, we describe the 294 CEnR projects identified through RePORTER by project type (descriptive, intervention, or other). We found that the R funding mechanism was more likely to support intervention development and evaluation projects, the U funding mechanism (other than NARCH and PRC) was more likely to support dissemination and implementation projects, and the NARCH and PRC mechanisms were more likely to support descriptive and epidemiology-type projects (p < .001). We also found that projects serving AIAN populations were more likely to be descriptive projects as opposed to intervention or dissemination and intervention implementation projects (p < .01), which tend to be funded at higher levels than descriptive studies. Finally, “other” projects composed of dissemination and policy change received more funding than the descriptive or intervention projects (p < .05). The top three funding institutes for CEnR were the NIMHD (19.1%), NCI (13.3%), and CDC (12.6%).
Table 1. Community-Engaged Research Projects Identified From the National Institutes of Health (NIH) RePORTER Funded in 2009 (N = 294) by Project Type: Descriptive, Intervention, or Other (Dissemination and Implementation or Policy Projects).
| Project Type, n (%) |
|||||
|---|---|---|---|---|---|
| Projects | Total (N = 294) | Descriptive, n = 61 (20.7) |
Intervention, n = 194 (66.0) |
Other, n = 39 (13.3) |
Statistics |
| Type of Funding Mechanism | 51.39*** | ||||
| R01 R18, R23, R24, R34, RC1, RC2 | 173 (58.8) | 28 (45.9) | 132 (68.0)a,c | 13 (33.3) | 3.24*** |
| U01, U19, U54 | 54 (18.4) | 8 (13.1) | 25 (12.9) | 21 (53.9) ab | −3.48** |
| U26 NARCH/ U48 PRC | 67 (22.8) | 25 (41.0)b,c | 37 (19.1) | 5 (12.8) | 4.00*** |
| Total Funds Awarded ($ millions: M, SD) |
2.7 (2.8) | 2.3 (2.3) | 2.6 (2.3) | 4.2 (4.8) ab | 2.41* |
| Length of Project (years: M, SD) |
4.6 (2.1) | 4.6 (1.9) | 4.6 (2.1) | 5.0 (2.1) | 0.64 |
| Race/Ethnicity of Population Served | 15.27** | ||||
| AIAN | 63 (21.4) | 24 (39.3) b,c | 32 (16.5) | 7 (18.0) | |
| Other: Asian, AA, Hispanic | 68 (23.1) | 9 (14.8) | 50 (25.8) | 9 (23.1) | |
| None specified or multiple | 169 (55.4) | 29 (45.9) | 117 (57.7) | 23 (59.0) | |
| Funding Institute and Center | |||||
| NIMHD | 56 (19.1) | 3 (4.9) | 47 (24.2) | 6 (15.4) | |
| NCI | 39 (13.3) | 4 (6.6) | 21 (10.8) | 14 (35.9) | |
| CDC affiliated | 37 (12.6) | 8 (13.1) | 29.0 (15.0) | 0 (0.0) | |
| IHS-NARCH | 23 (7.8) | 10 (16.4) | 9 (4.6) | 4 (10.3) | |
| NIMH | 20 (6.8) | 1 (1.6) | 17 (8.8) | 2 (5.1) | |
| NIHLBI | 19 (6.5) | 2 (3.3) | 14 (7.2) | 3 (7.7) | |
| Child Health Human Development | 17 (5.8) | 9 (14.8) | 7 (3.6) | 1 (2.6) | |
| NIDA | 15 (5.1) | 3 (4.9) | 10 (5.2) | 2 (5.1) | |
| Environmental Health Sciences | 12 (4.1) | 9 (14.8) | 3 (1.6) | 0 (0.0) | |
| Other IC (<4%) | 56 (19.1) | 12 (19.7) | 37 (19.1) | 7 (17.9) | |
AA = African American; AIAN = American Indian/Alaskan Native; Asian = Asian American.
The Centers for Disease Control and Prevention (CDC) includes the Prevention Research Center (PRC). Other funding institute and centers (IC) include the Agency for Healthcare Research and Quality (AHRQ), Agency for Toxic Substances and Disease Registry (ATSDR), Coordinating Office for Terrorism Preparedness and Emergency Response (COTPER), Complementary and alternative medicine (CAM), National Center for Environmental Health (NCEH), National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), Center for Urban Horticulture (CUH), National Center for Research Resources (NCRR), Nuclear Energy Institute (NEI), National Human Genome Research Institute (NHGRI), National Institute of General Medical Sciences (NIGMS), National Institute for Occupational Safety and Health (NIOSH), National Institute of Allergy and Infectious Diseases (NIAID), National Institute of Dental and Craniofacial Research (NIDCR), National Institute of Nursing Research (NINR), National Institute of Aging (NIA), National Institute on Alcohol Abuse and Alcoholism (NIAAA), and United States Public Health Service (USPHS).
Data are reported as frequency (n) and percent (%), unless noted as mean (M) and standard deviation (SD).
No statistical test were conducted for funding institute and center.
Test statistics: analyses are conducted using the F test, t test, and Pearson χ2 and Wald χ2 as appropriate.
p < .05.
p < .01.
p < .001.
Project is significantly different than Project 1.
Project is significantly different than Project 2.
Project is significantly different than Project 3.
In Table 2, focusing on the structural dynamics within Figure 1 and addressing our second objective, we examined the difference between CEnR projects’ structural characteristics and the populations they serve. Projects serving an AIAN population, compared with other communities of color and multiple-race/unspecified groups, were more likely to report greater resource and power sharing (i.e., in hiring staff [p < .001], deciding how finances are shared [p < .001], determining how in-kind resources are shared [p < .001], and receiving a greater percentage of the financial resource [p < .01]). In addition, AIAN-serving projects were more likely to have a written formal agreement (p < .05), which includes publication or authorship guidelines (p < .001), intellectual property agreements (p < .001), and data use/sharing guidelines (p < .01). Pertaining to concrete outcomes, AIAN-serving projects were more likely to have developed or revised IRB polices or procedures as compared with projects serving multiple-race/unspecified groups (p < .001), but were less likely to have developed their own study measures (p < .05). Also, AIAN-serving projects received less total funds as compared with funds awarded for projects serving multiple-race/unspecified groups (p < .05), although there was no difference in research productivity as measured by papers in-press/published or obtained other funding. Projects that serve AIAN populations compared with multiple-race/unspecified groups were less confident that their study would achieve its goal (p < .05).
Table 2. Population Served by Project Characteristics Among the 200 Self-identified Community-Engaged Research Projects Who Responded to the Survey.
| Project Features | Total (N = 200) |
AIAN (n = 47) |
Other Comm of Color (n = 51) |
Multi-Race Unspecified (n = 102) |
Statistic |
|---|---|---|---|---|---|
| Confident project will achieved its goal | 191 (95.5) | 41 (87.2)c | 49 (96.1) | 101 (99.0)a | 10.45** |
| Total funds awarded ($ millions: M, SD) | 2.5 (1.9) | 2.0 (2.4)c | 2.2 (1.2)c | 2.9 (2.0)a,b | 3.56* |
| Resource and Power Sharing by Both Community and Academic Partner | |||||
| Hire project staff | 126 (63.3) | 28 (60.9) | 34 (66.7) | 64 (62.8) | 0.38 |
| Decides how finances are shared | 127 (63.5) | 26 (55.3) | 36 (70.6) | 65 (63.7) | 2.46 |
| Decides how in-kind resources are shared | 148 (74.8) | 33 (70.2) | 38 (74.5) | 77 (77.0) | 0.78 |
| Percent of financial resource community receives (M, SD) |
37.2 (25.2) | 48.3 (30.5)b,c | 33.3 (16.6)a | 34.0 (25.0)a | 5.42** |
| Research Integrity—All or Most Partners Have: | |||||
| Received human subject training | 128 (64.3) | 34 (74.0)c | 38 (74.5)c | 56 (54.9)a,b | 8.09* |
| Sign confidentiality agreements | 114 (57.0) | 31 (66.0) | 28 (54.9) | 55 (53.9) | 2.02 |
| Formal Agreements | |||||
| Guideline to address breach in confidentiality |
111 (55.5) | 31 (66.0) | 28 (54.9) | 52 (50.9) | 2.93 |
| Written formal agreement (MOU/ resolution) |
152 (76.0) | 44 (93.6) bc | 36 (70.6) a | 72 (70.6)a | 10.45** |
| Written Agreements Include: (n = 152) | |||||
| Distributions of funds | 102 (68.0) | 26 (59.1) | 27 (75.0) | 49 (70.0) | 2.54 |
| Written mission or objectives | 138 (90.8) | 41 (93.2) | 35 (97.2) | 62 (86.1) | 3.97 |
| Clear expectation for partner s role | 138 (91.4) | 39 (88.6) | 33 (91.7) | 66 (93.0) | 0.65 |
| Clear decision-making process | 76 (50.0) | 21 (47.7) | 19 (52.8) | 36 (50.0) | 0.20 |
| Conflict resolution | 52 (34.2) | 16 (36.4) | 10 (27.8) | 26 (36.1) | 0.87 |
| Intellectual property agreements | 56 (37.3) | 26 (60.5) c | 15 (41.7)a,b | 15 (21.1) | 18.09*** |
| Data use/sharing guidelines | 98 (64.9) | 38 (86.4)bc | 23 (63.9) a | 37 (52.1) a | 14.01** |
| Publication or authorship agreement | 79 (52.7) | 33 (76.7) bc | 13 (36.1) a | 33 (46.5) a | 15.05*** |
| Final approval of publications | 56 (71.8) | 30 (90.9)bc | 5 (38.5) a | 21 (65.6) a | 13.69** |
| Students data access | 47 (49.0) | 18 (48.7) | 8 (34.8) | 21 (58.3) | 3.12 |
| Concrete Outcomes | |||||
| Papers in press/published | 132 (66.3) | 27 (57.5) | 37 (72.6) | 68 (67.3) | 2.59 |
| Obtained other funding | 123 (61.5) | 25 (53.2) | 31 (60.8) | 67 (65.7) | 2.14 |
| Developed own measures | 157 (78.5) | 32 (68.1)b | 45 (88.2) a | 80 (78.4) | 5.88* |
| Developed/revised IRB polices or procedures |
90 (45.0) | 28 (59.6) c | 22 (43.1) | 40 (39.2) a | 5.48* |
| Project Members Has Received Moderate or More Training in | |||||
| Cultural sensitivity | 159 (80.3) | 44 (93.6) c | 43 (84.3) | 72 (72.0)a | 10.14** |
| Cultural humility | 120 (60.9) | 34 (72.3) b,c | 34 (66.7) a | 52 (52.5)a | 6.21* |
| CBPR | 168 (84.9) | 43 (91.5) b,c | 47 (92.2) a | 78 (78.0)a | 7.38* |
| Self and collective reflection | 110 (55.8) | 28 (61.7) | 31 (60.8) | 50 (50.5) | 2.30 |
| Privilege and power; forms of oppression | 131 (65.5) | 27 (65.8) | 91 (64.5) | 13 (72.2) | 0.42 |
| Dialogue, listening, and mutual learning | 146 (74.1) | 40 (85.1) | 40 (78.4) | 66 (66.7) | 6.32* |
| Race/Ethnicity of Principle Investigator (PI) | 56.27*** | ||||
| AIAN | 16 (8.0) | 15 (31.9) b,c | 0 (0.0) | 1 (1.0) | |
| Hispanic, Asian, Black, mixed race | 50 (25.0) | 9 (19.2) | 21 (41.2)a,c | 20 (19.6) | |
| White or not reported | 134 (67.0) | 23 (48.9) | 30 (58.8) | 81 (79.4) a,b | |
| Gender of PI is female | 128 (70.3) | 32 (74.4) | 35 (71.4) | 61 (67.8) | 0.65 |
AIAN = American Indian or Alaskan Native; CBPR = community-based participatory research; IRB = institutional review board; MOU = memorandum of understanding; PI = principal investigator.
Statistics = analyses were conducted using F test, t test, Pearson χ2, and Wald χ2 as appropriate.
p < .05.
p < .01.
p < .001.
Population served is significantly different than AIAN served.
Population served is significantly different than other community of color served.
Population served is significantly different than multiple-race or unspecified.
We also explored differences in population served with both partners’ engagement in the research process and with whether members received formal trainings. As it pertains to partners’ engagement in the research process, there were no important differences across population served and engagement in the research process. AIAN-serving projects were more likely to conduct cultural and community research trainings compared with projects serving other community of color of multiple-race/unspecified groups. Finally, across all projects, community partners were engaged in an average of 6.5 research activities (median, 6; range, 0–13). In terms of PI/PD demographics, most CEnR principle investigators were female (70.3%), 58.5% identified as Caucasian, 25% identified as Hispanic, Asian, Black, or mixed-race, 8% as AIAN, and 8.5% did not report (n = 17).
DISCUSSION
The purpose of this study was to investigate the variability of contextual and structural characteristics of federally funded CEnR projects and explore differences by project type and ethnic population. The descriptive information demonstrates that the majority of these projects captured in our sample were funded through an R01 or R24 mechanism and by a wide range of institutes and organizations; the NIMHD, NCI, and CDC were the three largest funders. Slightly more than one half of the sample serves an AIAN population or other community of color. However, 85 project populations were unspecified.
Our findings by race/ethnicity of communities served showed that AIAN-serving projects receive less funding compared with other communities of color and multiple-race/unspecified groups. Although AIAN communities had a greater proportion of descriptive grants, which tended to receive less funding compared with intervention design or dissemination grants, this is still an alarming finding, given that most tribal communities are among the lowest resourced in the United States and face significant health disparities, a status shared by many communities of color. Our focus on AIAN communities emerges from a desire to add value and reflects the federal trust responsibility to tribal nations, which includes health research funding such as the NARCH mechanism that funded this project. The descriptive emphasis of these projects may also reflect the lack of data on AIAN populations throughout the local, state, and federal public health systems and the need to obtain basic epidemiological and other research data. Another factor influencing this finding may be reflective in the type of funding obtained by AIAN communities (NARCH as oppose to an NIH R01) and the inherent differences in agency mission and goals.
In general, the projects reported a moderate amount (50% of possible activities) of community partner involvement throughout the research. From one perspective, this level of involvement seems to be low, given that CBPR principles9 ideally envision researchers and community members partnering together in all phases of a research and intervention process.19 However, this ideal perspective may not reflect the often underfunded service orientation of many community partners or imbalances in power as experienced by the partnership members themselves. As such, our findings suggest that equality may not be a realistic goal, and that some partnerships may emphasize the role-based strengths of each partner while fostering opportunities for reciprocal learning and capacity building. In addition, our findings confirm variability of community engagement within the sample and raise the question about how different levels of engagement affect the research process and health outcomes. Future research should address whether this variability in partnership structures and processes has an impact on outcomes and thus may lead to better understanding of best practices of CEnR/CBPR.
Finally, we found that PI/PD of AIAN-serving projects, compared with those of projects serving multiple-race/unspecified groups, had less confidence in achieving their study goals and developed fewer study-specific measures. The lack of development of study-specific measures may be related to the greater proportion of descriptive projects relative to intervention projects. Intervention projects may involve more specific measurement development given the need to adapt intervention outcomes to the community and the fact that descriptive projects often measure a large number of constructs and thus the need to use validated measures. On the other hand, AIAN projects provided close oversight of the research process. AIAN-serving projects, compared with communities of color and multiple-race/unspecified groups, reported more resource and partnership power sharing, had formal agreements, owned the data, and were involved in publication and dissemination efforts, including final review of presentations and publications. It is difficult to assess the source of the doubt of achieving research aims, although AIAN populations do have some of the more egregious health inequities in the United States, which may reflect a lack of confidence of significant change given the “higher hill to climb.” AIAN communities have been at the forefront of establishing processes and outcomes for CBPR, owing in part to both the history of unethical research and the sovereign status of tribal governments. This is reflected in the greater level of overall oversight, formal regulation activities, and production of new and revised IRB protocols.33 Finally, despite there being fewer funding resources for AIAN projects in the sample, their research productivity, (i.e., published papers, additional funding) has been consistent to that of other non-AIAN research projects.
Implications and Contributions
This study makes several contributions to the literature on CEnR and CBPR. First, these findings demonstrate significant variability in structural characteristics of CEnR research projects, reflecting the range of health issues and populations served. Although the CBPR literature may reflect common principles, the reality of implementing that vision has great variability. The impact of this variability on many CBPR processes and outcomes remains to be seen. Future research is needed to explore the impact of structure on processes and outcomes and whether there is a set of best practices for CEnR or whether the variability reflects different contexts and philosophies and can be applied with relatively similar results. Second, there are significant resource inequities for AIAN communities when it comes to funding. Although the reason for these differences is not clear, many AIAN community members and leaders may see this underfunding as just one more instance in a long line of inequities faced by AIAN communities within the U.S. healthcare system (e.g., US Commission on Civil Rights, 2004). Alternatively, as mentioned, the focus on descriptive epidemiology and assessment may be appropriate, and the U48 NARCH funding (received by 49% of our AIAN sample) shares overall funding with training and pipeline programs, and thus reduces the amount of funding available for research. Despite these inequities, projects serving AIAN do not have differences in levels of research output compared with projects in other communities; which is a testament to the ingenuity and tenacity of all levels of the partnership.
Overall, these findings identify some key patterns for funded CEnR in 2009 and serve as a foundation for understanding these partnerships, particularly for researchers, policymakers, and PI/PD of CEnR. Specifically, these findings help to identify some of the key policies and funding trends within the contextual factors and some of the structural dynamics elements within the group dynamic factors of the CBPR conceptual model. These contextual and structural features likely have a strong influence on partner processes and outcomes, and thus are important to understand. Further, this study provides an initial foundation for unpacking the CBPR conceptual model and opens up further research to test additional relationships within the model.
Although this study is primarily a description of the structural characteristics of CEnR projects, there are some potential implications for members of campus–community partnerships. Much of the focus on CEnR and CBPR projects has been on group dynamic processes.10 Certainly these processes are important and yet the structural characteristics shape these processes and outcomes.34 Increasingly, there is recognition in the literature of these characteristics, and reporting of memoranda of understanding, data sharing agreements, bylaws, and decision-making agreements.24-26,35 Partners and project leaders would be wise to review their structural characteristics to ensure they will meet project goals and enable them to engage in meaningful participatory research. For example, they can review the level of complexity in the policies and resources used to guide their partnership.36
Limitations
There were several limitations. First, the cross-sectional, web-based survey was necessary given the constraints of budget and time. Conducting the KI interview as a survey, however, may have increased our response rate, because the interview was 15 minutes in length and could be conducted at responders’ convenience. Additionally, we used multiple contact strategies (i.e., email, mail, and phone). Second, inclusion criteria of federally funded CBPR and CEnR projects may have limited some of the variability in these projects, because we did not include partnerships that may have been temporarily unfunded or foundation-funded projects. The CEnR/CBPR definitions we used may have excluded unintentionally projects that were not able to share resources or research tasks but that nonetheless had some community engagement. This was evident in some comments we received from PIs/PDs who chose not to complete the survey because they felt their project did not meant our criteria of a CBPR partnerships. However, the definitions and benchmarks we chose (i.e., CBPR principles) are well-accepted in the literature and thus represent a reasonable approach. Finally, we recognize that much of our sample was not specified as to racial/ethnic population which limited our analysis by individual racial/ethnic groups, whether owing to nonresponse, distribution of funding, or population served, we lacked representation of smaller diverse groups that may also be underresourced, yet producing outstanding science.
Although there are limitations, this study represents a rigorous and thorough survey on 2009 federally funded CEnR projects. We collected data through RePORTER and a web-based survey to characterize structural characteristics of CEnR projects. We found variability in the practice of CEnR across different racial/ethnic communities. This variability is important to understand given the increasing use of CEnR and the need to enhance the dissemination of scientific findings with communities to address health disparities. The next step will be to determine the degree to which the variability in these structural characteristics impact partnering processes and a greater range of CEnR and health disparities outcomes.
REFERENCES
- 1.Barkin S, Schlundt D, Smith P. Community-engaged research perspectives: Then and now. Acad Pediatr. 2013 Mar-Apr;13(2):93–7. doi: 10.1016/j.acap.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 2.Selby JV, Beal AC, Frank L. The Patient-Centered Outcomes Research Institute (PCORI) national priorities for research and initial research agenda. JAMA. 2012 Apr 18;307(15):1583–4. doi: 10.1001/jama.2012.500. [DOI] [PubMed] [Google Scholar]
- 3.Greenlund KJ, Giles WH. The Prevention Research Centers program: translating research into public health practice and impact. Am J Prev Med. 2012 Sep;43(3 Suppl. 2):S91–92. doi: 10.1016/j.amepre.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Casey BR. Innovations in primary prevention: Emerging research from CDC’s Prevention Research Centers. J Prim Prev. 2013 Apr;34(1-2):3–4. doi: 10.1007/s10935-013-0298-z. [DOI] [PubMed] [Google Scholar]
- 5.Meyers D, Parchman M. Re: The Agency for Healthcare Research and Quality (AHRQ) Practice-Based Research Network (PBRN) relationship: delivering on an opportunity, challenges, and future directions. J Am Board Fam Med. 2011 Sep-Oct;24(5):493. doi: 10.3122/jabfm.2011.05.110211. [DOI] [PubMed] [Google Scholar]
- 6.Rubin CL, Martinez LS, Chu J, et al. Community-engaged pedagogy: A strengths-based approach to involving diverse stakeholders in research partnerships. Prog Community Health Partnersh. 2012 Winter;6(4):481–90. doi: 10.1353/cpr.2012.0057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sadler LS, Newlin KH, Johnson-Spruill I, Jenkins C. Beyond the medical model: Interdisciplinary programs of community-engaged health research. Clin Transl Sci. 2011 Aug;4(4):285–97. doi: 10.1111/j.1752-8062.2011.00316.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmed SM, Palermo AG. Community engagement in research: frameworks for education and peer review. Am J Public Health. 2010 Aug;100(8):1380–7. doi: 10.2105/AJPH.2009.178137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Israel BA, Parker EA, Rowe Z, et al. Community-based participatory research: Lessons learned from the Centers for Children’s Environmental Health and Disease Prevention Research. Environ Health Perspect. 2005;113(10):1463–71. doi: 10.1289/ehp.7675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Minkler M, Wallerstein N. Introduction to CBPR: New issues and emphases. In: Minkler M, Wallerstein N, editors. Community-Based Participatory Research for Health: From Process to Outcome. John Wiley & Sons; San Francisco: 2008. [Google Scholar]
- 11.Viswanathan M, Ammerman A, Eng E, et al. Community-based participatory research: assessing the evidence. Evid Rep Technol Assess. 2004 Summer;(99):1–8. [PMC free article] [PubMed] [Google Scholar]
- 12.Michener L, Cook J, Ahmed SM, Yonas MA, Coyne-Beasley T, Aguilar-Gaxiola S. Aligning the goals of community-engaged research: why and how academic health centers can successfully engage with communities to improve health. Acad Med. 2012 Mar;87(3):285–91. doi: 10.1097/ACM.0b013e3182441680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anderson EE, Solomon S, Heitman E, et al. Research ethics education for community-engaged research: a review and research agenda. J Empir Res Hum Res Ethics. 2012;7(2):3–19. doi: 10.1525/jer.2012.7.2.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCLoskey DJ, Aguilar-Gaxiola S, Michener JL, et al. Principles of Community Engagement. 2nd ed. National Institutes of Health, Centers for Disease Control and Prevention; Bethesda (MD): 2011. [Google Scholar]
- 15.Israel BA, Coombe CM, Cheezum RR, et al. Community-based participatory research: a capacity-building approach for policy advocacy aimed at eliminating health disparities. Am J Public Health. 2010;100(11):2094–102. doi: 10.2105/AJPH.2009.170506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wallerstein N. Making traces: Evidence for practice and evaluation. In: Reader A, Greene J, Labonte R, editors. Critical Public Health. Routledge; London: 2007. pp. 80–91. [Google Scholar]
- 17.Glasgow R, Green L, Klesges L, et al. External validity: We need to do more. Ann Behav Med. 2006;31:105–8. doi: 10.1207/s15324796abm3102_1. [DOI] [PubMed] [Google Scholar]
- 18.Fixsen D, Naoom S, Blasé K, Friedman R, Wallace F. Implementation Research: A Synthesis of the Literature. University of South-Florida, Louis de la Parte Florida Mental Health Institute; Tampa: 2005. [Google Scholar]
- 19.Wallerstein N, Oetzel JG, Duran B, Tafoya G, Belone L, Rae R. CBPR: What predicts outcomes? In: Minkler M, Wallerstein N, editors. CBPR for Health: From Process to Outcomes. 2nd ed. Jossey-Bass; San Francisco: 2008. pp. 371–92. [Google Scholar]
- 20.Ball TJ, Janyst P. Enacting research ethics in partnerships with indigenous communities in Canada: “Do it the right way”. J Empir Res Hum Res Ethics. 2008;3(2):33–51. doi: 10.1525/jer.2008.3.2.33. [DOI] [PubMed] [Google Scholar]
- 21.Carey TS, Howard DL, Goldmon M, Roberson JT, Godley PA, Ammerman A. Developing effective interuniversity partnerships and community-based research to address health disparities. Acad Med. 2005;80(11):1039–45. doi: 10.1097/00001888-200511000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baldwin JA, Johnson JL, Benally CC. Building partnerships between indigenous communities and universities: Lessons learned in HIV/AIDS and Substance abuse prevention research. Am J Public Health. 2009;99(Suppl. 1):S77–82. doi: 10.2105/AJPH.2008.134585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lucero JE, Wallerstein N. Trust and conflict in community academic partnerships. In: Oetzel JG, Ting-Toomey S, editors. The SAGE Handbook of Conflict Communication: Integrating Theory, Research, and Practice. SAGE; Thousand Oaks (CA): 2013. [Google Scholar]
- 24.Yonas M, Aronson R, Coad N, et al. Appendix C. Collaborative revised bylaws: Adopted/amended: (Month, Day, Year) In: Israel BA, Eng E, Schulz AJ, Parker E, editors. Methods for Community-Based Participatory Research for Health. 2nd ed. Jossey-Bass; San Francisco: 2013. p. 589. [Google Scholar]
- 25.Yonas M, Aronson R, Coad N, et al. Part 2: Partnership formation and maintenance Section 4. Infrastructure for equitable decision making in research. In: Israel BA, Eng E, Schulz AJ, Parker E, editors. Methods for Community-Based Participatory Research for Health. 2nd ed. Jossey-Bass; San Francisco: 2013. p. 97. [Google Scholar]
- 26.Becker AB, Israel BA, Gustat J, Reyes AG, Allen J. Part 2: Session 3. Strategies and techniques for effective group process in CBPR partnerships. In: Israel BA, Eng E, Schulz AJ, Parker E, editors. Methods for Community-Based Participatory Research for Health. 2nd ed. Jossey-Bass; San Francisco: 2013. p. 69. [Google Scholar]
- 27.Wallerstein N, Duran B. The theoretical, historical, and practice roots of community based participatory research and related participatory traditions. In: Wallerstein MMN, editor. Community-Based Participatory Research for Health: From Process to Outcomes. 2nd ed. Jossey-Bass; San Francisco: 2008. [Google Scholar]
- 28.Cargo M, Levesque L, Macaulay AC, et al. Community governance of the Kahnawake Schools Diabetes Prevention Project, Kahnawake Territory, Mohawk Nation, Canada. Health Promot Int. 2003;18(3):177–87. doi: 10.1093/heapro/dag013. [DOI] [PubMed] [Google Scholar]
- 29.Hicks S, Duran B, Wallerstein N, et al. Evaluating community-based participatory research to improve community-partnered science and community health. Prog Community Health Partnersh. 2012 Fall;6(3):289–299. doi: 10.1353/cpr.2012.0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.National Institutes of Health (NIH) NIH RePORTER. Research portfolio online reporting tools [updated 2009] Available from: http://projectreporter.nih.gov/reporter.cfm.
- 31.Pearson CR, Duran B, Oetzel J, Magarati M, Villegas M. Research for improved health: Patterns in federally-funded community engaged research studies. CES4health. doi: 10.1353/cpr.2015.0010. Available from: http://ces4health.info/find-products/view-product.aspx?code=FWYC2L2T2011. [DOI] [PMC free article] [PubMed]
- 32.Rabe-Hesketh S, Pickles A, Skrondal S. GLLAMM manual. U.C. Berkeley Division of Biostatistics Working Paper Series. Working Paper 160 [updated 2004] 2004 Available from: http://www.bepress.com/ucbbiostat/paper160/
- 33.Brugge D, Missaghian M. Protecting the Navajo people through tribal regulation of research. Sci Engineer Ethics. 2006;12:491–507. doi: 10.1007/s11948-006-0047-2. [DOI] [PubMed] [Google Scholar]
- 34.Wallerstein N, Duran B. The theoretical, historical, and practical roots of CBPR. In: Minkler M, Wallerstein N, editors. Community-Based Participatory Research for Health: From Process to Outcome. John Wiley & Sons; San Francisco: 2008. [Google Scholar]
- 35.Yonas M, Aronson R, Coad N, et al. Appendix B. Full value contract. In: Israel BA, Eng E, Schulz AJ, Parker E, editors. Methods for Community-Based Participatory Research for Health. 2nd ed. Jossey-Bass; San Francisco: 2013. [Google Scholar]
- 36.Israel BA, Schulz AJ, Parker EA, Becker AB, Allen J, Guzman JR. Critical issues in developing and following community-based participatory research principles. In: Minkler M, Wallerstein N, editors. Community-Based Participatory Research for Health. Jossey-Bass; San Francisco: 2008. pp. 56–73. [Google Scholar]