Abstract
Critically ill post-surgical, post-trauma and/or septic patients are characterised by severe inflammation. This immune response consists of both a pro- and an anti-inflammatory component. The pro-inflammatory component contributes to (multiple) organ failure whereas occurrence of immune paralysis predisposes to infections. Strikingly, infectious complications arise in these patients despite the presence of a clear neutrophilia. We propose that dysfunction of neutrophils potentially increases the susceptibility to infections or can result in the inability to clear existing infections. Under homeostatic conditions these effector cells of the innate immune system circulate in a quiescent state and serve as the first line of defence against invading pathogens. In severe inflammation, however, neutrophils are rapidly activated, which affects their functional capacities, such as chemotaxis, phagocytosis, intra-cellular killing, NETosis, and their capacity to modulate adaptive immunity. This review provides an overview of the current understanding of neutrophil dysfunction in severe inflammation. We will discuss the possible mechanisms of downregulation of anti-microbial function, suppression of adaptive immunity by neutrophils and the contribution of neutrophil subsets to immune paralysis.
Background
Severe inflammation induced by trauma, sepsis or ischemia/reperfusion injury is known to contribute to devastating complications such as acute respiratory distress syndrome (ARDS) and (multiple) organ failure [1]. This has been attributed to microvascular dysfunction, tissue damage and dysregulation of metabolism caused by severe inflammation [2]. In recent years, however, it has been recognised that severe systemic inflammation can also result in a profound ‘compensatory’ down-regulation of immune responses, rendering the host susceptible to infections or unable to clear existing infections [3]. Although conceivably an evolutionarily preserved response to protect the host from immune-mediated tissue damage, downregulation of anti-microbial immunity creates an unwanted consequence: susceptibility to bacterial infections such as caused by Staphylococcus aureus, Pseudomonas aeruginosa and Escherichia coli as well as opportunistic fungal infections such as (disseminated) candidiasis [4–6]. In addition, reactivation of viruses such as cytomegalovirus are found in critically ill patients [7]. These findings clearly indicate that both the innate and the adaptive immune system are dysfunctional in these patients. Nosocomial infections in critically ill patients are associated with an increased length of hospital stay, increased health care costs and profound additional morbidity and mortality [8].
Neutrophils, effector cells of the innate immune system, are abundantly present in the circulation and comprise up to 50–70 % of total circulating leukocytes in humans. The enhanced frequency and severity of bacterial and fungal infections in patients with congenital neutrophil disorders demonstrate that neutrophils are indispensable for adequate protection against microbes [9]. Patients suffering from leucocyte adhesion deficiency (LAD)-I are at risk for development of necrotizing infections and sepsis because of inadequate neutrophil transendothelial migration to the site of infection [10]. The Chediak-Higashi syndrome and chronic granulomatous disease (CGD) underscore the eminent importance of intracellular bacterial killing by neutrophils. Chediak-Higashi syndrome is caused by a mutation in the LYST gene, which encodes a lysosomal trafficking regulator [11]. The mutation leads to the absence of a proper formation of phagolysosomes. Patients suffering from Chediak-Higashi are extremely susceptible to pyogenic infections and this syndrome is usually fatal before the age of 10 [11]. CGD is characterised by a defect in production of the bactericidal reactive oxygen species (ROS) due to defective NADPH oxidase and results in recurrent infections, reducing life-expectancy significantly [12]. In murine models of sepsis, knockout of essential neutrophil antimicrobial functions leads to rapid death. For instance, mice lacking the neutrophil granule proteins myeloperoxidase or elastase die more rapidly from sepsis [13, 14]. Apart from the severe phenotypes seen in patients with inborn errors and murine knockout models, more subtle effects were seen in a murine sepsis model where rapid death coincided with inadequate phagosomal acidification of neutrophils after phagocytosis [15]. These studies highlight the generally accepted importance of neutrophils in antimicrobial defence in acute inflammatory models. In addition, they demonstrate disturbances in the anti-microbial functionality of these cells during severe inflammation.
In this review we will discuss neutrophil functions required for adequate microbial defence and the mechanisms leading to neutrophil-mediated immune dysfunction.
Functions of neutrophils associated with anti-microbial defence
Chemotaxis
The controlled process of phagocytosis and killing of microbes by neutrophils firstly requires chemotaxis towards the site of infection. Chemotaxis is the propensity of cells to migrate in the direction of gradients of chemotactic stimuli [16]. The ability to adequately sense chemotactic gradients is one of the final capabilities acquired by neutrophils during maturation in the bone marrow and this functionality appears to be the most sensitive to perturbations in vivo and in vitro [17]. Impairment of chemotaxis has been described in a wide variety of diseases associated with increased susceptibility to infections: diabetes mellitus, viral infections (influenza), cytomegalovirus, HIV and tropical diseases (malaria) [18–22]. In sepsis, chemotaxis of neutrophils is impaired through various mechanisms [23–25]. Interleukin (IL)-33 limits this impairment by preventing downregulation of CXCR2 and improves outcome in a murine model [26]. In humans, extensive research has focused on the chemotactic capacity of neutrophils from burn patients. It has been shown that neutrophils from thermally injured subjects are characterised by impaired chemotaxis, both in vivo in the tissue and in vitro, towards the bacterial peptide fMLF, which is believed to contribute to the increased susceptibility to infections in this group of patients [27, 28].
Intracellular killing
Once neutrophils have found and recognised a pathogen, phagocytosis can take place and subsequent bacterial killing occurs in the phagolysosome. Neutrophils possess two separate but intercalating anti-microbial mechanisms, one dependent on oxygen and the other independent of it. Although categorisation of killing mechanisms in this manner creates a comprehensive understanding, it does not reflect the in vivo situation in which both systems operate simultaneously. Furthermore, it is likely that the individual significance of both killing mechanisms shifts during the course of inflammation. This is due to fluxes in oxygen demand and supply caused by dynamic tissue perfusion and oxygenation during the inflammatory response [29].
The oxygen-dependent mechanisms are mediated by ROS downstream of O2− formed by the NADPH oxidase complex [30]. In short, upon activation of a neutrophil, either via ingestion of bacteria or by extracellular stimuli, the NADPH oxidase complex is assembled from both cytosolic and membrane-bound components [31]. The active oxidase complex transports electrons from cytosolic NADPH across the membrane to the electron acceptor, molecular oxygen, generating superoxide anion [29]. This is in turn metabolises in the phagosome into highly bactericidal end products, such as hydroxyl radical, hydrogen peroxide and hypochlorous acid [31]. In sterile inflammation, such as trauma or acute liver failure, neutrophils are known to produce elevated levels of spontaneous ROS [32, 33]. Furthermore, ROS production in these patients in response to a stimulus is strongly elevated in comparison with that found in neutrophils from healthy controls; a process generally referred to as priming [27, 34–36]. Uncontrolled release of ROS by neutrophils accumulating in vascular beds can contribute to loss of endothelial barrier integrity and subsequent vascular leakage, predisposing patients to organ injury as a result of pro-inflammatory complications (acute lung injury, ARDS) [37, 38]. This hypothesis is in line with the findings of increased ROS production in trauma patients developing ARDS in comparison with control trauma patients [39]. In addition, the observation that neutrophils from patients with fatal sepsis are characterised by markedly increased production of ROS compared with survivors is noteworthy [40].
Granule products comprise the backbone of non-oxidative killing by neutrophils [41]. The azurophilic granule is a reservoir of serine proteases: neutrophil elastase, cathepsin G, proteinase 3, and azurocidin [42]. These digestive proteases are delivered into the phagolysosome upon fusion of granules with a phagosome containing bacteria. During maturation of the phagolysosome the intraphagosomal pH is rigorously altered. The early shift of intraphagosomal pH towards an alkaline level (pH 8.5–9.5) due to dismutation of O2− provides the initial milieu for the proper activation of proteases, leading to optimal microbicidal and digestive function of these enzymes [43]. Concomitant with the waning of production of ROS the phagosome progressively acidifies, coinciding with granule–phagosome fusion. These granules contain the Na+/H+-antiporter V-ATP-ase, which is responsible for pumping of protons into the phagosome [44–46]. Neutrophils of burn-injured patients are characterised by dysfunctional pH control of their phagolysosomes since these patients fail to demonstrate transient phagosomal alkalinisation in the first 5 minutes and acidify promptly after ingestion of bacteria [47]. This situation might lead to improper activation of the proteases and impaired killing of ingested microbes. On the other hand, deficient acidification of peritoneal neutrophils in a murine model of sepsis was associated with increased mortality [15]. These findings demonstrate the importance of adequate intraphagosomal pH regulation for microbial control.
The presence and proper function of granules intracellulary are crucial as these organelles supply neutrophils with an arsenal of antimicrobial mechanisms. However, uncontrolled activation of neutrophils in an inflammatory microenvironment can lead to collateral tissue damage by excessive extracellular degranulation and the release of neutrophil proteases. Neutrophil extravasation, homing and activation are mediated by activation of several surface receptors, including β2 integrins, complement receptors, Fcγ-receptors, and formyl peptide receptors. Uncontrolled activation of neutrophils is mediated through these same receptors by responding to aberrant production of chemokines, cytokines and release of extracellular peptides [48]. During this process granules fuse with the plasma membrane, releasing their content into the environment [49]. More tissue damage will lead to increased influx and activation of neutrophils, which then leads to a vicious cycle of tissue destruction [50].
Neutrophil extracellular traps
In addition to conventional intracellular killing and degradation of individual bacteria, the concept of extracellular killing by neutrophils using neutrophil extracellular traps (NETs) has received much attention during the past decade [51, 52]. NETs consist of fibrils formed by active expulsion of DNA, chromatin and granule proteins from neutrophils [52, 53]. They are formed in response to a variety of pro-inflammatory stimuli of which IL-8, tumour necrosis factor-alpha and lipopolysaccharide are the most relevant [54]. During formation of NETs neutrophils die and this process is generally referred to as NETosis. This form of cell death is dependent on the NADPH-oxidase complex since neutrophils treated with the pharmacological NADPH-oxidase inhibitor DPI and CGD patients are unable to release NETs [53]. In vitro NETs were shown to be a cell-death-associated event occurring hours after stimulation [53]. However, intravital microscopy revealed viable neutrophils after formation of NETs and the resulting anuclear neutrophils were subsequently capable of phagocytosis and formation of mature phagosomes. These data indicate that NETosis does not necessarily result in cell death [55]. The direct bactericidal properties of NETs are a topic of discussion, and prevention of bacterial dissemination in vivo might be their main function [56]. Apart from this antimicrobial function, the cytotoxicity of NETs can be harmful to the host if their release is inappropriately controlled. NETs are released following sepsis, trauma and ischemia–reperfusion injury and a growing body of evidence shows they can contribute to tissue destruction, as reviewed by Liu et al. [57]. The potential of NETs to cause tissue destruction was elegantly demonstrated in a murine model of primary graft-dysfunction after lung transplantation [58]. In addition, several studies argue that NETs might be involved in triggering auto-immune diseases since auto-antibodies against NET constituents (e.g. DNA) are often found in these diseases [59, 60]. Although NETs have firmly established their tissue-damaging properties, scepticism still exists about the in vivo anti-microbial relevance of NETs [61].
Neutrophil dysfunction in acute inflammation
The mechanisms involved in adequate anti-microbial defence can also disrupt subsequent immunity. This is caused by aberrant control of their own essential antimicrobial arsenal, such as: (1) auto- and paracrine cleavage of essential surface receptors; (2) downregulation of surface receptors and signalling pathways in non-resolving inflammation or during a second microbial hit following initial sterile inflammation (damage-associated molecular pattern (DAMP)–microbe-associated molecular pattern (MAMP) interference); and (3) the release of neutrophil populations with decreased microbicidal properties. In addition, neutrophils in inflammatory conditions can affect other immune cells and contribute to immune paralysis of the adaptive immune system.
Proteolytic cleavage by neutrophil-derived proteases and downregulation of immune receptors
Serine proteases released by neutrophils influence the expression of receptors critical to neutrophil–microbial interactions (Fig. 1a). Apart from stimulatory effects through serine protease activated receptors (PARs), they can downregulate immune responses by cleaving essential receptors on the surface of both adaptive and innate immune cells [62]. For instance, neutrophil elastase cleaves CXCR1, a receptor for IL-8, on the surface of neutrophils [63, 64]. This mechanism is relevant during acute inflammation in which circulating neutrophils from trauma and sepsis patients selectively downregulate CXCR2, the only other neutrophil receptor for IL-8 [65, 66]. Tarlowe et al. [67] provided evidence that downregulation of this receptor preceded the occurrence of pneumonia in critically ill trauma patients. Downregulation of CXCR2 and cleavage of CXCR1 would result in severe hyporesponsiveness to IL-8, an important neutrophil chemoattractant.
Fig. 1.
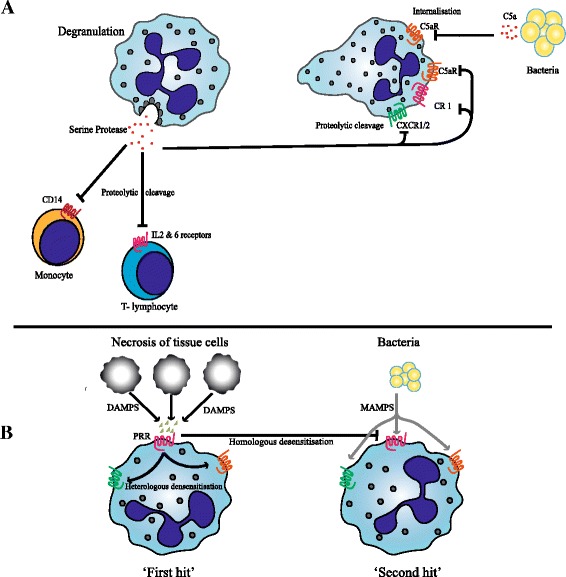
Downregulation of immune receptors by serine proteases from degranulated neutrophils and desensitisation by pattern recognition receptors. a Schematic representation of downregulation of receptors on neutrophils, monocytes and lymphocytes during inflammation due to cleavage by neutrophil serine proteases after degranulation. Binding of C5a to neutrophils results in internalisation of C5aR. Decreased expression of these receptors impairs neutrophil effector functions during subsequent challenges. b Biological mimicry between DAMPs and MAMPs. Danger signals derived from necrotic tissue cells ("First hit") bind to pattern recognition receptors (PRRs) and limit subsequent responses to microbial signals ("Second hit") through homo- and heterologous desensitisation. DAMP damage-associated molecular pattern, IL interleukin, MAMP microbe-associated molecular pattern
Furthermore, neutrophil serine proteases can cleave complement receptors such as the CR1 receptor (CD35) and C5aR (CD88) on neutrophils [68, 69]. These receptors are important as they mediate chemotaxis, degranulation and proper recognition of opsonised microbial targets by CR1 and C5aR, respectively [70]. During inflammation, decreased expression of C5aR is seen due to engagement and subsequent internalisation. This can result in a profound defect in neutrophil phagocytosis of subsequent pathogens as C5a-induced chemotaxis is important for neutrophils to find opsonised targets [71]. Proteases not only inhibit the function of neutrophils, they can also affect monocytes in the micro-environment. Neutrophil elastase cleaves CD14, a receptor necessary for the high affinity recognition of lipopolysaccharide by TLR4, thereby impairing proper bacterial recognition by monocytes [72]. Lastly, elastase and cathepsin G mediate shedding of cytokine receptors for IL-2 and IL-6 on T lymphocytes [73].
DAMP–MAMP interference
Trauma and ischemia/reperfusion injury can evoke the release of large amounts of cellular components from necrotic cells. These intracellular constituents are known as damage-associated molecular patterns (DAMPS). They are host-derived and serve as important pro-inflammatory non-microbial stimuli after injury [74]. Since the development of the ‘danger hypothesis’ by Matzinger [74], a large number of studies have focussed on molecules driving this response. The most extensively studied DAMPS are high-mobility group box 1, heat shock proteins, ATP, uric acid, formylated peptides from mitchondria and mitochondrial DNA [75–80]. Inflammation induced by pathogens on the other hand is mediated through microbial constituents referred to as microbe-associated molecular patterns (MAMPS), which resemble DAMPS and, importantly, share similar pattern recognition receptors (PRRs) on the neutrophil [81]. This biological mimicry and utilisation of similar receptors creates a problem for the immune system since injury (DAMPS) causes downregulation of many of these receptors by hetero- and homologous desensitisation. This can render neutrophils unable to mount an adequate response to a subsequent microbe (MAMP) (Fig. 1b). To illustrate the relevance of this phenomenon, Zhang et al. [80] showed the release of vast amounts of mitochondrial formylpeptides into the circulation of major trauma patients. These molecules stimulate neutrophils via formyl peptide receptor 1 (FPR1), an important receptor in recognizing microbes that produce danger signals by release of formyl-peptides [80] (Fig. 1b). It was shown that heterologous desensitisation of chemokine receptors and homologous desensitisation of FPR1 occurred simultaneously, predisposing trauma patients to infection [82].
Release of incompetent neutrophil populations
Much of the work detailed in the previous sections did not take into account the variations in functional phenotypes that appear in the circulating neutrophil compartment during severe inflammation. After maturation neutrophils are retained in the bone marrow via expression of chemokine receptor CXCR4 (ligand CXCL12), whilst CXCR2 (ligands IL-8/CXCL1 and 2) controls release into the peripheral blood. Inflammatory stimuli can induce the release of neutrophils by disrupting the balance in CXCR4/CXCL12 signalling through various mechanisms [60]. In severe inflammation large numbers of neutrophils are released into the circulation from the bone marrow post-mitotic pool as well as from the marginated pool (i.e. neutrophils not freely circulating but attached to the microvasculature) [83]. Under these conditions we have previously shown that peripheral neutrophils consist of heterogeneous subsets with different priming states and function [84]. During severe inflammation a large number of immature or banded cells appear in the circulation and even neutrophil progenitor cells can be identified. As a result, persistent severe inflammation might lead to "bone marrow exhaustion" of neutrophils, which is thought to inevitably result in a state of compromised innate immunity [85]. At present, however, it is unclear how to interpret the presence of immature cells in the bloodstream in response to inflammation. It might be a compensatory response initiated by the depletion of mature neutrophils in the bone marrow or a dedicated inflammatory reaction to a bacterial stimulus. Our data support the first hypothesis since these immature neutrophils also show a pronounced decrease of various receptors in comparison with their mature circulating counterparts [84]. In addition to the IL-8 receptors (CXCR1 and CXCR2) and the C5a receptor, the Fc receptors (CD16 and CD32), which are important in pathogen recognition, phagocytosis and killing, are also downregulated on immature cells (Fig. 2) [84]. Relatively few studies have assessed the functionality of immature and progenitor neutrophils subsets in severe human inflammation. In septic patients, immature neutrophils were shown to have decreased phagocytic capacity [86]. Importantly, reduced phagocytosis and increased numbers of circulating neutrophil progenitors are both associated with poor outcome in septic patients as well as in patients with severe inflammation [87, 88].
Fig. 2.
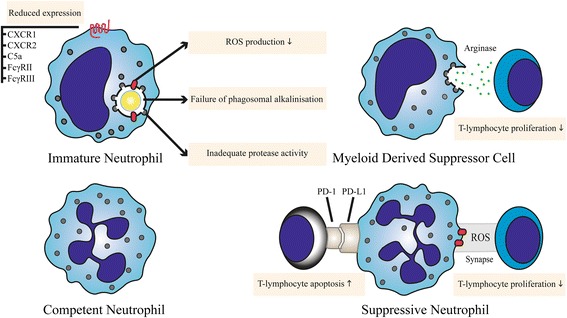
Circulating neutrophil subsets in severe inflammation. At least four types of neutrophils circulate in the bloodstream of patients during severe inflammation: immature, competent and suppressive neutrophils and myeloid-derived suppressor cells. Mechanisms contributing to immune dysfunction are displayed for neutrophils from different subsets. ROS reactive oxygen species
Suppression of adaptive immunity by neutrophils
Neutrophils have long been recognised as professional killers. Eradication of bacteria and fungi was thought to be their main task. Evidence is, however, accumulating that apart from their direct anti-microbial function, neutrophils participate in subsequent modulation of (adaptive) immune responses in severe inflammation [89–91]. Under these inflammatory conditions, neutrophils produce chemokines and secrete granule contents which can subsequently attract and modulate the function(s) of T cells both directly and indirectly [92, 93]. For instance, neutrophil elastase reduces expression of co-stimulatory molecules by dendritic cells, limiting maturation and induction of a proper Th1 response [94]. In addition, T cells in the inflammatory microenvironment may be affected by neutrophil elastase by cleavage of their IL-2 and IL-6 receptors (Fig. 1a) [95]. Another mechanism of immune-modulation was observed in macrophages after phagocytosis of apoptotic neutrophils. Under these conditions immune responses of macrophages shift towards a more anti-inflammatory cytokine profile [96]. Furthermore, neutrophils themselves have been shown to produce anti-inflammatory cytokines such as IL-1ra and IL-10 [97]. However, the evidence regarding IL-10 production by neutrophils is controversial, as it has only been shown in mice with mycobacterial infections [98]. In humans neutrophils are unable to produce IL-10 [99]. Direct regulation of T-cell responses by neutrophils is slowly becoming an established concept. A large body of evidence demonstrates that a heterogeneous group of immature mononuclear cells and neutrophils termed myeloid-derived suppressor cells (MDSCs) can suppress T-cell responses in several murine tumour models. In addition, these cells have been shown to play a role in various models of infectious diseases, organ transplantation and autoimmune diseases [100]. Identification of human immature granulocytic MDSCs has proven to be challenging though. In particular, their differentiation from mature neutrophil phenotypes seen in the blood during acute inflammation remains to be established, as we have reviewed in detail elsewhere [101]. The mechanisms by which MDSCs can suppress T cells include the expression and secretion of arginase-1, which depletes arginine from the microenvironment (Fig. 2) [102]. Depletion of L-arginine, which is an essential amino acid, results in cell cycle arrest of T cells in the G0–G1 phase [103]. Furthermore, in human inflammation we and others have observed a population of mature CD62Ldim neutrophils capable of suppressing T-cell responses through a mechanism which relies on ROS release in an immunological synapse [104]. Recently, similar neutrophils in septic shock patients have been found to express arginase-1 and suppress T-cell functions [105]. Another mechanism by which neutrophils might inhibit T-cell responses is through PD-L1 [106]. Neutrophils isolated from sepsis patients express the surface protein PD-L1, a potent inducer of apoptosis in T cells. The underlying mechanism of PD-L1 expression is an interferon-gamma-dependent process [106]. The PD-1–PD-L1 axis is thought to be an important mechanism in immune suppression in septic patients by inducing lymphocyte apoptosis and monocyte dysfunction [107]. Blocking this axis after the induction of sepsis by administering a PD-1-blocking antibody improved survival in mice [108]. This suppressive mechanism might be protective in tissues with severe inflammatory infiltrates. On the other hand, this process might be unwanted when neutrophils migrate to lymph nodes and engage with adaptive immunity, as has been described under various conditions [109]. In these lymph nodes neutrophils are able to inhibit humoral immune responses through interaction with T and B lymphocytes [109, 110].
Conclusion
Severe inflammation can result in immune paralysis through various mechanisms. We propose that neutrophils play a central role in this process, either through decreased antimicrobial functions or through direct suppression of (adaptive) immunity. Many experimental studies have been performed addressing the damaging role of neutrophils, which contributes to organ failure in severe inflammation. However, their role in immune paralysis remains understudied. Studies to explore their causative role in susceptibility to infections in animal models of severe inflammation should be designed. Decreased neutrophil antimicrobial functions and their ability to suppress adaptive immunity in vitro should be considered as important patient outcomes. This approach is necessary to increase understanding of the role of neutrophils in immune paralysis leading to detrimental outcome in post-surgical, post-trauma and septic patients.
Acknowledgments
JP was supported by the Lung Foundation the Netherlands (grant number 5.2.14.058JO).
Abbreviations
- ARDS
acute respiratory distress syndrome
- CGD
chronic granulomatous disease
- DAMP
damage-associated molecular pattern
- IL
interleukin
- MAMP
microbe-associated molecular pattern
- MDSC
myeloid-derived suppressor cell
- NET
neutrophil extracellular trap
- ROS
reactive oxygen species
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
PHCL designed search strategies, undertook search strategies, screened search results, organised retrieval of papers, appraised quality of papers and extracted data from papers, drafted the manuscript and wrote the review. CMW designed search strategies, undertook search strategies, screened search results, organised retrieval of papers, appraised quality of papers and extracted data from papers, drafted the manuscript and wrote the review. LPHL participated in designing this review, wrote the review and provided general advice on and coordinated the review. LK participated in designing this review, wrote the review and provided general advice on and coordinated the review. JP participated in designing this review, designed search strategies, undertook search strategies, screened search results, organised retrieval of papers, appraised quality of papers and extracted data from papers, drafted the manuscript and wrote the review. All authors participated in editing of the manuscript and approved the final version.
References
- 1.Lord JM, Midwinter MJ, Chen Y-F, Belli A, Brohi K, Kovacs EJ, et al. The systemic immune response to trauma: an overview of pathophysiology and treatment. Lancet. 2014;384:1455–1465. doi: 10.1016/S0140-6736(14)60687-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singer PM, De Santis V, Vitale D, Jeffcoate W. Multiorgan failure is an adaptive, endocrine-mediated, metabolic response to overwhelming systemic inaflammation. Lancet. 2004;364:545–548. doi: 10.1016/S0140-6736(04)16815-3. [DOI] [PubMed] [Google Scholar]
- 3.Boomer JS. Immunosuppression in patients who die of sepsis and multiple organ failure. JAMA. 2011;306:2594. doi: 10.1001/jama.2011.1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martin SJ, Yost RJ. Infectious diseases in the critically ill patients. J Pharm Pract. 2011;24:35–43. doi: 10.1177/0897190010388906. [DOI] [PubMed] [Google Scholar]
- 5.Vincent J-L, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, Moreno R, et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA. 2009;302:2323–2329. doi: 10.1001/jama.2009.1754. [DOI] [PubMed] [Google Scholar]
- 6.Viale P. Candida colonization and candiduria in critically ill patients in the intensive care unit. Drugs. 2009;69(Suppl 1):51–57. doi: 10.2165/11315640-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 7.Mansfield S, Grießl M, Gutknecht M, Cook CH. Sepsis and cytomegalovirus: foes or conspirators? Med Microbiol Immunol. 2015;204(3):431–437. doi: 10.1007/s00430-015-0407-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cobb JP, Buchman TG, Karl IE, Hotchkiss RS. Molecular biology of multiple organ dysfunction syndrome: injury, adaptation, and apoptosis. Surg Infect (Larchmt) 2000;1:207–213. doi: 10.1089/109629600750018132. [DOI] [PubMed] [Google Scholar]
- 9.Dinauer MC. Inherited neutrophil disorders: molecular basis and new therapies. Hematology. 2000;2000:303–318. doi: 10.1182/asheducation-2000.1.303. [DOI] [PubMed] [Google Scholar]
- 10.Anderson DC, Springer TA. Leukocyte adhesion deficiency: an inherited defect in the Mac-1, LFA-1, and p150,95 glycoproteins. Annu Rev Med. 1987;38:175–194. doi: 10.1146/annurev.me.38.020187.001135. [DOI] [PubMed] [Google Scholar]
- 11.Kjeldsen L, Calafat J, Borregaard N. Giant granules of neutrophils in Chediak-Higashi syndrome are derived from azurophil granules but not from specific and gelatinase granules. J Leukoc Biol. 1998;64:72–77. doi: 10.1002/jlb.64.1.72. [DOI] [PubMed] [Google Scholar]
- 12.Holland SM. Chronic granulomatous disease. Hematol Oncol Clin North Am. 2014;27:89–99. doi: 10.1016/j.hoc.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Belaaouaj A, McCarthy R, Baumann M, Gao Z, Ley TJ, Abraham SN, Shapiro SD. Mice lacking neutrophil elastase reveal impaired host defense against gram negative bacterial sepsis. Nat Med. 1998;4:615–618. doi: 10.1038/nm0598-615. [DOI] [PubMed] [Google Scholar]
- 14.Gaut JP, Yeh GC, Tran HD, Byun J, Henderson JP, Richter GM, et al. Neutrophils employ the myeloperoxidase system to generate antimicrobial brominating and chlorinating oxidants during sepsis. Proc Natl Acad Sci U S A. 2001;98:11961–11966. doi: 10.1073/pnas.211190298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chiswick EL, Mella JR, Bernardo J, Remick DG. Acute-phase deaths from murine polymicrobial sepsis are characterized by innate immune suppression rather than exhaustion. J Immunol. 2015;195:3793–3802. doi: 10.4049/jimmunol.1500874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zigmond SH. Mechanisms of sensing chemical gradients by polymorphonuclear leukocytes. Nature. 1974;249:450–452. doi: 10.1038/249450a0. [DOI] [PubMed] [Google Scholar]
- 17.Boner A, Zeligs B, Bellanti J. Chemotactic responses of various differentational stages of neutrophils from human cord and adult blood. Infect Immun. 1982;35:921–928. doi: 10.1128/iai.35.3.921-928.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wierusz-Wysocka B, Wysocki H, Siekierka H, Wykretowicz A, Szczepanik A, Klimas R. Evidence of polymorphonuclear neutrophils (PMN) activation in patients with insulin-dependent diabetes mellitus. J Leukoc Biol. 1987;42:519–523. doi: 10.1002/jlb.42.5.519. [DOI] [PubMed] [Google Scholar]
- 19.Larson HE, Parry RP, Tyrrell DA. Impaired polymorphonuclear leucocyte chemotaxis after influenza virus infection. Br J Dis Chest. 1980;74:56–62. doi: 10.1016/0007-0971(80)90008-X. [DOI] [PubMed] [Google Scholar]
- 20.Bale JF, Kern ER, Overall JC, Baringer JR. Impaired migratory and chemotactic activity of neutrophils during murine cytomegalovirus infection. J Infect Dis. 1983;148:518–525. doi: 10.1093/infdis/148.3.518. [DOI] [PubMed] [Google Scholar]
- 21.Martin LS, Spira TJ, Orloff SL, Holman RC. Comparison of methods for assessing chemotaxis of monocytes and polymorphonuclear leukocytes isolated from patients with AIDS or AIDS-related conditions. J Leukoc Biol. 1988;44:361–366. doi: 10.1002/jlb.44.5.361. [DOI] [PubMed] [Google Scholar]
- 22.de Leoratti FMS, Trevelin SC, Cunha FQ, Rocha BC, Costa PAC, Gravina HD, et al. Neutrophil paralysis in plasmodium vivax malaria. PLoS Negl Trop Dis. 2012;6:e1710. doi: 10.1371/journal.pntd.0001710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reddy RC, Standiford TJ. Effects of sepsis on neutrophil chemotaxis. Curr Opin Hematol. 2010;17:18–24. doi: 10.1097/MOH.0b013e32833338f3. [DOI] [PubMed] [Google Scholar]
- 24.Reddy RC, Narala VR, Keshamouni VG, Milam JE, Newstead MW, Standiford TJ. Sepsis-induced inhibition of neutrophil chemotaxis is mediated by activation of peroxisome proliferator-activated receptor-{gamma} Blood. 2008;112:4250–4258. doi: 10.1182/blood-2007-12-128967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rios-Santos F, Alves-Filho JC, Souto FO, Spiller F, Freitas A, Lotufo CMC, et al. Down-regulation of CXCR2 on neutrophils in severe sepsis is mediated by inducible nitric oxide synthase-derived nitric oxide. Am J Respir Crit Care Med. 2007;175:490–497. doi: 10.1164/rccm.200601-103OC. [DOI] [PubMed] [Google Scholar]
- 26.Alves-Filho JC, Sônego F, Souto FO, Freitas A, Verri W, Auxiliadora-Martins M, et al. Interleukin-33 attenuates sepsis by enhancing neutrophil influx to the site of infection. Nat Med. 2010;16:708–712. doi: 10.1038/nm.2156. [DOI] [PubMed] [Google Scholar]
- 27.Dong YL, Abdullah K, Yan TZ, Rutan T, Broemeling L, Robson M, et al. Effect of thermal injury and sepsis on neutrophil function. J Trauma. 1993;34:417–421. doi: 10.1097/00005373-199303000-00019. [DOI] [PubMed] [Google Scholar]
- 28.Butler KL, Ambravaneswaran V, Agrawal N, Bilodeau M, Toner M, Tompkins RG, et al. Burn injury reduces neutrophil directional migration speed in microfluidic devices. PLoS One. 2010;5:e11921. doi: 10.1371/journal.pone.0011921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nauseef WM. How human neutrophils kill and degrade microbes: an integrated view. Immunol Rev. 2007;219:88–102. doi: 10.1111/j.1600-065X.2007.00550.x. [DOI] [PubMed] [Google Scholar]
- 30.Babior BM. NADPH oxidase: an update. Blood. 1999;93:1464–1476. [PubMed] [Google Scholar]
- 31.Bedard K, Krause K-H. The NOX family of ROS-generating NADPH oxidases: physiology and pathophysiology. Physiol Rev. 2007;87:245–313. doi: 10.1152/physrev.00044.2005. [DOI] [PubMed] [Google Scholar]
- 32.Liao Y, Liu P, Guo F, Zhang Z-Y, Zhang Z. Oxidative burst of circulating neutrophils following traumatic brain injury in human. PLoS One. 2013;8:e68963. doi: 10.1371/journal.pone.0068963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Taylor NJ, Nishtala A, Manakkat Vijay GK, Abeles RD, Auzinger G, Bernal W, et al. Circulating neutrophil dysfunction in acute liver failure. Hepatology. 2013;57:1142–1152. doi: 10.1002/hep.26102. [DOI] [PubMed] [Google Scholar]
- 34.Hietbrink F, Koenderman L, Althuizen M, Pillay J, Kamp V, Leenen LPH. Kinetics of the innate immune response after trauma: implications for the development of late onset sepsis. Shock. 2013;40:21–27. doi: 10.1097/SHK.0b013e318295a40a. [DOI] [PubMed] [Google Scholar]
- 35.Botha J, Moore FA, Moore EE, Kim FJ, Banerjee A, Peterson VM. Postinjury neutrophil priming and activation: an early vulnerable window. Surgery. 1995;118:358–364. doi: 10.1016/S0039-6060(05)80345-9. [DOI] [PubMed] [Google Scholar]
- 36.Taylor JV, Gordon LE, Hall H, Heinzelmann M, Polk HC. Differences between bacterial species shown by simultaneous assessment of neutrophil phagocytosis and generation of reactive oxygen intermediates in trauma patients. Arch Surg. 1999;134:1222–1227. doi: 10.1001/archsurg.134.11.1222. [DOI] [PubMed] [Google Scholar]
- 37.Mittal M, Siddiqui MR, Tran K, Reddy SP, Malik AB. Reactive oxygen species in inflammation and tissue injury. Antioxid Redox Signal. 2014;20:1126–1167. doi: 10.1089/ars.2012.5149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fox ED, Heffernan DS, Cioffi WG, Reichner JS. Neutrophils from critically ill septic patients mediate profound loss of endothelial barrier integrity. Crit Care. 2013;17:R226. doi: 10.1186/cc13049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Simms HH, D’Amico R. Increased PMN CD11b/CD18 expression following post-traumatic ARDS. J Surg Res. 1991;50:362–367. doi: 10.1016/0022-4804(91)90204-Y. [DOI] [PubMed] [Google Scholar]
- 40.Santos SS, Brunialti MKC, Rigato O, Machado FR, Silva E, Salomao R. Generation of nitric oxide and reactive oxygen species by neutrophils and monocytes from septic patients and association with outcomes. Shock. 2012;38:18–23. doi: 10.1097/SHK.0b013e318257114e. [DOI] [PubMed] [Google Scholar]
- 41.Borregaard N, Cowland JB. Granules of the human neutrophilic polymorphonuclear leukocyte. Blood. 1997;89:3503–3521. [PubMed] [Google Scholar]
- 42.Spicer SS, Hardin JH. Ultrastructure, cytochemistry, and function of neutrophil leukocyte granules. A Rev Lab Invest. 1969;20:488–497. [PubMed] [Google Scholar]
- 43.Levine AP, Duchen MR, de Villiers S, Rich PR, Segal AW. Alkalinity of neutrophil phagocytic vacuoles is modulated by HVCN1 and has consequences for myeloperoxidase activity. PLoS One. 2015;10:e0125906. doi: 10.1371/journal.pone.0125906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cech P, Lehrer RI. Phagolysosomal pH of human neutrophils. Blood. 1984;63:88–95. [PubMed] [Google Scholar]
- 45.Bassøe CF, Laerum OD, Glette J, Hopen G, Haneberg B, Solberg CO. Simultaneous measurement of phagocytosis and phagosomal pH by flow cytometry: role of polymorphonuclear neutrophilic leukocyte granules in phagosome acidification. Cytometry. 1983;4:254–262. doi: 10.1002/cyto.990040311. [DOI] [PubMed] [Google Scholar]
- 46.Nanda A, Brumell JH, Nordström T, Kjeldsen L, Sengelov H, Borregaard N, et al. Activation of proton pumping in human neutrophils occurs by exocytosis of vesicles bearing vacuolar-type H + −ATPases. J Biol Chem. 1996;271:15963–15970. doi: 10.1074/jbc.271.27.15963. [DOI] [PubMed] [Google Scholar]
- 47.Bjerknes R, Vindenes H, Pitkänen J, Ninnemann J, Laerum OD, Abyholm F. Altered polymorphonuclear neutrophilic granulocyte functions in patients with large burns. J Trauma. 1989;29:847–855. doi: 10.1097/00005373-198906000-00024. [DOI] [PubMed] [Google Scholar]
- 48.Borregaard N. Neutrophils, from marrow to microbes. Immunity. 2010;33:657–670. doi: 10.1016/j.immuni.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 49.Lacy P. Mechanisms of degranulation in neutrophils. Allergy Asthma Clin Immunol. 2006;2:98–108. doi: 10.1186/1710-1492-2-3-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Weiss SJ. Tissue destruction by neutrophils. N Engl J Med. 1989;320:365–376. doi: 10.1056/NEJM198902093200606. [DOI] [PubMed] [Google Scholar]
- 51.Brinkmann V, Reichard U, Goosmann C, Fauler B, Uhlemann Y, Weiss DS, et al. Neutrophil extracellular traps kill bacteria. Science. 2004;303:1532–1535. doi: 10.1126/science.1092385. [DOI] [PubMed] [Google Scholar]
- 52.Remijsen Q, Vanden Berghe T, Wirawan E, Asselbergh B, Parthoens E, De Rycke R, et al. Neutrophil extracellular trap cell death requires both autophagy and superoxide generation. Cell Res. 2011;21:290–304. doi: 10.1038/cr.2010.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fuchs TA, Abed U, Goosmann C, Hurwitz R, Schulze I, Wahn V, et al. Novel cell death program leads to neutrophil extracellular traps. J Cell Biol. 2007;176:231–241. doi: 10.1083/jcb.200606027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Remijsen Q, Kuijpers TW, Wirawan E, Lippens S, Vandenabeele P, Vanden BT. Dying for a cause: NETosis, mechanisms behind an antimicrobial cell death modality. Cell Death Differ. 2011;18:581–588. doi: 10.1038/cdd.2011.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yipp BG, Petri B, Salina D, Jenne CN, Scott BNV, Zbytnuik LD, et al. Infection-induced NETosis is a dynamic process involving neutrophil multitasking in vivo. Nat Med. 2012;18:1386–1393. doi: 10.1038/nm.2847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Menegazzi R, Decleva E, Dri P. Killing by neutrophil extracellular traps: fact or folklore? Blood. 2012;119:1214–1216. doi: 10.1182/blood-2011-07-364604. [DOI] [PubMed] [Google Scholar]
- 57.Liu F-C, Chuang Y-H, Tsai Y-F, Yu H-P. Role of neutrophil extracellular traps following injury. Shock. 2014;41:491–498. doi: 10.1097/SHK.0000000000000146. [DOI] [PubMed] [Google Scholar]
- 58.Sayah DM, Mallavia B, Liu F, Ortiz-Muñoz G, Caudrillier A, Der Hovanessian A, et al. Neutrophil extracellular traps are pathogenic in primary graft dysfunction after lung transplantation. Am J Respir Crit Care Med. 2015;191:455–463. doi: 10.1164/rccm.201406-1086OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bosmann M, Ward PA. Protein-based therapies for acute lung injury: targeting neutrophil extracellular traps. Expert Opin Ther Targets. 2014;18:703–714. doi: 10.1517/14728222.2014.902938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yipp BG, Kubes P. NETosis: how vital is it? Blood. 2013;122:2784–2794. doi: 10.1182/blood-2013-04-457671. [DOI] [PubMed] [Google Scholar]
- 61.Nauseef WM. Editorial: Nyet to NETs? A pause for healthy skepticism. J Leukoc Biol. 2012;91:353–355. doi: 10.1189/jlb.1011495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Adams MN, Ramachandran R, Yau MK, Suen JY, Fairlie DP, Hollenberg MD, Hooper JD. Structure, function and pathophysiology of protease activated receptors. Pharmacol Ther. 2011;130:248–282. doi: 10.1016/j.pharmthera.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 63.Steinhoff M, Buddenkotte J, Shpacovitch V, Rattenholl A, Moormann C, Vergnolle N, et al. Proteinase-activated receptors: transducers of proteinase-mediated signaling in inflammation and immune response. Endocr Rev. 2005;26:1–43. doi: 10.1210/er.2003-0025. [DOI] [PubMed] [Google Scholar]
- 64.Hartl D, Latzin P, Hordijk P, Marcos V, Rudolph C, Woischnik M, et al. Cleavage of CXCR1 on neutrophils disables bacterial killing in cystic fibrosis lung disease. Nat Med. 2007;13:1423–1430. doi: 10.1038/nm1690. [DOI] [PubMed] [Google Scholar]
- 65.Quaid G, Cave C, Robinson C, Williams MA, Solomkin J. Preferential loss of CXCR-2 receptor expression and function in patients who have undergone trauma. Arch Surg. 1999;134:1367–1371. doi: 10.1001/archsurg.134.12.1367. [DOI] [PubMed] [Google Scholar]
- 66.Cummings CJ, Martin TR, Frevert CW, Quan JM, Wong VA, Mongovin SM, et al. Expression and function of the chemokine receptors CXCR1 and CXCR2 in sepsis. J Immunol. 1999;162:2341–2346. [PubMed] [Google Scholar]
- 67.Tarlowe MH, Duffy A, Kannan KB, Itagaki K, Lavery RF, Livingston DH, et al. Prospective study of neutrophil chemokine responses in trauma patients at risk for pneumonia. Am J Respir Crit Care Med. 2005;171:753–759. doi: 10.1164/rccm.200307-917OC. [DOI] [PubMed] [Google Scholar]
- 68.Sadallah S, Hess C, Miot S, Spertini O, Lutz H, Schifferli JA. Elastase and metalloproteinase activities regulate soluble complement receptor 1 release. Eur J Immunol. 1999;29:3754–3761. doi: 10.1002/(SICI)1521-4141(199911)29:11<3754::AID-IMMU3754>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 69.van den Berg CW, Tambourgi DV, Clark HW, Hoong SJ, Spiller OB, McGreal EP. Mechanism of neutrophil dysfunction: neutrophil serine proteases cleave and inactivate the C5a receptor. J Immunol. 2014;192:1787–1795. doi: 10.4049/jimmunol.1301920. [DOI] [PubMed] [Google Scholar]
- 70.van Kessel KPM, Bestebroer J, van Strijp JAG. Neutrophil-mediated phagocytosis of Staphylococcus aureus. Front Immunol. 2014;5:467. doi: 10.3389/fimmu.2014.00467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Morris AC, Brittan M, Wilkinson TS, McAuley DF, Antonelli J, McCulloch C, et al. C5a-mediated neutrophil dysfunction is RhoA-dependent and predicts infection in critically ill patients. Blood. 2011;117:5178–5188. doi: 10.1182/blood-2010-08-304667. [DOI] [PubMed] [Google Scholar]
- 72.Le-Barillec K, Si-Tahar M, Balloy V, Chignard M. Proteolysis of monocyte CD14 by human leukocyte elastase inhibits lipopolysaccharide-mediated cell activation. J Clin Invest. 1999;103:1039–1046. doi: 10.1172/JCI5779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bank U, Reinhold D, Schneemilch C, Kunz D, Synowitz HJ, Ansorge S. Selective proteolytic cleavage of IL-2 receptor and IL-6 receptor ligand binding chains by neutrophil-derived serine proteases at foci of inflammation. J Interferon Cytokine Res. 1999;19:1277–1287. doi: 10.1089/107999099312957. [DOI] [PubMed] [Google Scholar]
- 74.Matzinger P. An innate sense of danger. Semin Immunol. 1998;10:399–415. doi: 10.1006/smim.1998.0143. [DOI] [PubMed] [Google Scholar]
- 75.Scaffidi P, Misteli T, Bianchi ME. Release of chromatin protein HMGB1 by necrotic cells triggers inflammation. Nature. 2002;418:191–195. doi: 10.1038/nature00858. [DOI] [PubMed] [Google Scholar]
- 76.Quintana FJ, Cohen IR. Heat shock proteins as endogenous adjuvants in sterile and septic inflammation. J Immunol. 2005;175:2777–2782. doi: 10.4049/jimmunol.175.5.2777. [DOI] [PubMed] [Google Scholar]
- 77.Bours MJL, Swennen ELR, Di Virgilio F, Cronstein BN, Dagnelie PC. Adenosine 5’-triphosphate and adenosine as endogenous signaling molecules in immunity and inflammation. Pharmacol Ther. 2006;112:358–404. doi: 10.1016/j.pharmthera.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 78.Kono H, Chen CJ, Ontiveros F, Rock KL. Uric acid promotes an acute inflammatory response to sterile cell death in mice. J Clin Invest. 2010;120:1939–1949. doi: 10.1172/JCI40124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hazeldine J, Hampson P, Opoku FA, Foster M, Lord JM. N-formyl peptides drive mitochondrial damage associated molecular pattern induced neutrophil activation through ERK1/2 and P38 MAP Kinase signalling pathways. Injury. 2015;1–10. [DOI] [PubMed]
- 80.Zhang Q, Raoof M, Chen Y, Sumi Y, Sursal T. Circulating mitochondrial DAMPs cause inflammatory responses to injury. Nature. 2010;464:104–107. doi: 10.1038/nature08780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kumar H, Kawai T, Akira S. Pathogen recognition by the innate immune system. Int Rev Immunol. 2011;30:16–34. doi: 10.3109/08830185.2010.529976. [DOI] [PubMed] [Google Scholar]
- 82.Forsman H, Önnheim K, Andréasson E, Christenson K, Karlsson A, Bylund J, Dahlgren C. Reactivation of desensitized formyl peptide receptors by platelet activating factor: a novel receptor cross talk mechanism regulating neutrophil superoxide anion production. PLoS One. 2013;8:e60169. doi: 10.1371/journal.pone.0060169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Summers C, Rankin SM, Condliffe AM, Singh N, Peters M, Chilvers ER. Neutrophil kinetics in health and disease. Trends Immunol. 2010;31:318–324. doi: 10.1016/j.it.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pillay J, Ramakers BP, Kamp VM, Loi ALT, Lam SW, Hietbrink F, et al. Functional heterogeneity and differential priming of circulating neutrophils in human experimental endotoxemia. J Leukoc Biol. 2010;88:211–220. doi: 10.1189/jlb.1209793. [DOI] [PubMed] [Google Scholar]
- 85.Navarini AA, Lang KS, Verschoor A, Recher M, Zinkernagel AS, Nizet V, et al. Innate immune-induced depletion of bone marrow neutrophils aggravates systemic bacterial infections. Proc Natl Acad Sci U S A. 2009;106:7107–7112. doi: 10.1073/pnas.0901162106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Taneja R, Sharma AP, Hallett MB, Findlay GP, Morris MR. Immature circulating neutrophils in sepsis have impaired phagocytosis and calcium signaling. Shock. 2008;30:618–622. doi: 10.1097/SHK.0b013e318173ef9c. [DOI] [PubMed] [Google Scholar]
- 87.Danikas DD, Karakantza M, Theodorou GL, Sakellaropoulos GC, Gogos CA. Prognostic value of phagocytic activity of neutrophils and monocytes in sepsis. Correlation to CD64 and CD14 antigen expression. Clin Exp Immunol. 2008;154:87–97. doi: 10.1111/j.1365-2249.2008.03737.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mare TA, Treacher DF, Shankar-Hari M, Beale R, Lewis SM, Chambers DJ, Brown KA. The diagnostic and prognostic significance of monitoring blood levels of immature neutrophils in patients with systemic inflammation. Crit Care. 2015;19:1–11. doi: 10.1186/s13054-015-0778-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Cuenca AG, Delano MJ, Kelly-Scumpia KM, Moreno C, Scumpia PO, Laface DM, et al. A paradoxical role for myeloid-derived suppressor cells in sepsis and trauma. Mol Med. 2011;17:281–292. doi: 10.2119/molmed.2010.00178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Goh C, Narayanan S, Hahn YS. Myeloid-derived suppressor cells: The dark knight or the joker in viral infections? Immunol Rev. 2013;255:210–221. doi: 10.1111/imr.12084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Delano MJ, Scumpia PO, Weinstein JS, Coco D, Nagaraj S, Kelly-Scumpia KM, et al. MyD88-dependent expansion of an immature GR-1(+)CD11b(+) population induces T cell suppression and Th2 polarization in sepsis. J Exp Med. 2007;204:1463–1474. doi: 10.1084/jem.20062602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Pelletier M, Maggi L, Micheletti A, Lazzeri E, Tamassia N, Costantini C, et al. Evidence for a cross-talk between human neutrophils and Th17 cells. Blood. 2010;115:335–343. doi: 10.1182/blood-2009-04-216085. [DOI] [PubMed] [Google Scholar]
- 93.Chertov O, Yang D, Howard OM, Oppenheim JJ. Leukocyte granule proteins mobilize innate host defenses and adaptive immune responses. Immunol Rev. 2000;177:68–78. doi: 10.1034/j.1600-065X.2000.17702.x. [DOI] [PubMed] [Google Scholar]
- 94.Roghanian A, Drost EM, MacNee W, Howie SEM, Sallenave JM. Inflammatory lung secretions inhibit dendritic cell maturation and function via neutrophil elastase. Am J Respir Crit Care Med. 2006;174:1189–1198. doi: 10.1164/rccm.200605-632OC. [DOI] [PubMed] [Google Scholar]
- 95.Bank U, Ansorge S. More than destructive: neutrophil-derived serine proteases in cytokine bioactivity control. J Leukoc Biol. 2001;69:197–206. [PubMed] [Google Scholar]
- 96.Filardy AA, Pires DR, Nunes MP, Takiya CM, Freire-de-Lima CG, Ribeiro-Gomes FL, DosReis GA. Proinflammatory clearance of apoptotic neutrophils induces an IL-12(low)IL-10(high) regulatory phenotype in macrophages. J Immunol. 2010;185:2044–2050. doi: 10.4049/jimmunol.1000017. [DOI] [PubMed] [Google Scholar]
- 97.Langereis JD, Oudijk EJD, Schweizer RC, Lammers JWJ, Koenderman L, Ulfman LH. Steroids induce a disequilibrium of secreted interleukin-1 receptor antagonist and interleukin-1Beta synthesis by human neutrophils. Eur Respir J. 2011;37:406–415. doi: 10.1183/09031936.00170409. [DOI] [PubMed] [Google Scholar]
- 98.Noel G, Wang Q, Schwemberger S, Hanson C, Giacalone N, Haar L, Ogle CK. Neutrophils, not monocyte/macrophages, are the major splenic source of postburn IL-10. Shock. 2011;36:149–155. doi: 10.1097/SHK.0b013e3182205cbc. [DOI] [PubMed] [Google Scholar]
- 99.Davey MS, Tamassia N, Rossato M, Bazzoni F, Calzetti F, Bruderek K, et al. Failure to detect production of IL-10 by activated human neutrophils. Nat Immunol. 2011;12:1017–1018. doi: 10.1038/ni.2111. [DOI] [PubMed] [Google Scholar]
- 100.Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol. 2009;9:162–174. doi: 10.1038/nri2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Pillay J, Tak T, Kamp VM, Koenderman L. Immune suppression by neutrophils and granulocytic myeloid-derived suppressor cells: similarities and differences. Cell Mol Life Sci. 2013;70:3813–3827. doi: 10.1007/s00018-013-1286-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Highfill SL, Rodriguez PC, Zhou Q, Goetz CA, Koehn BH, Veenstra R, et al. Bone marrow myeloid-derived suppressor cells (MDSC) inhibit graft-versus-host (GVHD) disease via an arginase-1 dependent mechanism that is upregulated by IL-13. Blood. 2010;116:612–626. doi: 10.1182/blood-2010-06-287839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Rodriguez PC, Quiceno DG, Ochoa AC. L-arginine availability regulates T-lymphocyte cell-cycle progression. Blood. 2007;109:1568–1573. doi: 10.1182/blood-2006-06-031856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Pillay J, Kamp VM, Van Hoffen E, Visser T, Tak T, Lammers J, et al. A subset of neutrophils in human systemic inflammation inhibits T cell responses through Mac-1. J Clin Invest. 2012;122:327–336. doi: 10.1172/JCI57990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Darcy CJ, Minigo G, Piera KA, Davis JS, Mcneil YR, Chen Y, et al. Neutrophils with myeloid derived suppressor function deplete arginine and constrain T cell function in septic shock patients. Crit Care. 2014;8(4):R163. doi: 10.1186/cc14003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.de Kleijn S, Langereis JD, Leentjens J, Kox M, Netea MG, Koenderman L, et al. IFN-γ-stimulated neutrophils suppress lymphocyte proliferation through expression of PD-L1. PLoS One. 2013;8:e72249. doi: 10.1371/journal.pone.0072249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hotchkiss RS, Monneret G, Payen D. Sepsis-induced immunosuppression: from cellular dysfunctions to immunotherapy. Nat Rev Immunol. 2013;13:862–874. doi: 10.1038/nri3552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Brahmamdam P, Inoue S, Unsinger J, Chang KC, McDunn JE, Hotchkiss RS. Delayed administration of anti-PD-1 antibody reverses immune dysfunction and improves survival during sepsis. J Leukoc Biol. 2010;88:233–240. doi: 10.1189/jlb.0110037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hampton HR, Bailey J, Tomura M, Brink R, Chtanova T. Microbe-dependent lymphatic migration of neutrophils modulates lymphocyte proliferation in lymph nodes. Nat Commun. 2015;6:7139. doi: 10.1038/ncomms8139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kamenyeva O, Boularan C, Kabat J, Cheung GYC, Cicala C, Yeh AJ, et al. Neutrophil recruitment to lymph nodes limits local humoral response to Staphylococcus aureus. PLoS Pathog. 2015;11 doi: 10.1371/journal.ppat.1004827. [DOI] [PMC free article] [PubMed] [Google Scholar]


