Abstract
Cutaneous leishmaniasis is caused by different species of theLeishmania genus. Leishmania(Leishmania) infantum, causing cutaneous leishmaniasis, has been described in patients living in areas where visceral leishmaniasis is endemic. In this study, it was possible to characterize this species in seven slides from cutaneous tissue imprints from patients with cutaneous leishmaniasis in the State of Mato Grosso do Sul, Brazil.
Keywords: Cutaneous leishmaniasis, PCR, Leishmania infantum
The present study reports a case of Leishmania(Leishmania) infantum as an agent of cutaneous leishmaniasis (CL) in patients from the State of Mato Grosso do Sul(Brazil). This is the first description of CL in immunocompetent patients in Brazil.
The species L. infantum was first associated with CL in France, in 19801, where more autochtonous cases have been reported since then1 , 2 , 3. Since this first retrieval, several cases of CL have been reported in other Mediterranean countries4 , 5 , 6 , 7 , 8. Cutaneous leishmaniasis cases due toL. infantum are mainly reported in areas where the visceral disease is endemic.
In Mato Grosso do Sul (Fig. 1), leishmaniasis is endemic and is a significant threat to public health9 , 10, where 42.9 cases were reported per 100,000 inhabitants from 2010 to 2013 for visceral leishmaniasis (VL), and 21.6 cases per 100,000 inhabitantsfor CL in the same period. Despite the fact that Leishmania(Leishmania) amazonensis andLeishmania (Viannia) braziliensishave been detected in the human population10 , 11 , 12, studies on the isolation of species that cause CL in the State are scarce.
Fig. 1. - The State of Mato Grosso do Sul (MS) in Brazil.

From 2010 to 2013, 52 slides from cutaneous tissue imprints following punch biopsy, stained by the Giemsa method, with positive diagnosis of CL by direct examination were retrospectively scraped using a sterile scalpel for removal of all the material, which was inserted in a polypropylene tubes of 1.5 ml. Then, 600 µL of Cell Lysis Solution was added, and this solution was subjected to DNA extraction with a commercial kit (Promega Wizard(r) Genomic DNA Purification), following the manufacturer's instructions.
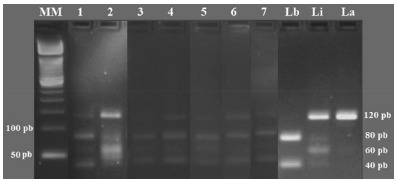
The PCR reaction was performed as described by VOLPINI et al. 13 and DE ANDRADE et al. 14. For amplification of the kinetoplast DNA ofLeishmania sp., the following primers were used: A: 5'-(C/G)(C/G)(G/C)CC(C/A)CTA T(T/A)TTACACCAACCCC 3' and B: 5'-GGGGAGGGGCGTTCTGCGAA-3'. A fragment of 120 bp was obtained.
Afterwards, 43 samples were considered positive, and subjected to RFLP analysis, where the PCR product was incubated with 10 U of the enzyme Hae III for 4 hours at 37 °C13. In all the reactions, DNA ofL. braziliensis (MHOM/BR/75/M2903), L. infantum(MHOM/BR/74/PP75), L. amazonensis (IFLA/BR/67/PH8), and negative controls were used. The DNA used as a positive control was obtained by washing parasites from a culture mass with PBS and a subsequent DNA extraction. A sample containing the reagents mixture with 5 µL of water, without DNA, was used as a negative control.
After the sample analysis, it was possible to characterize the species ofLeishmania, in 40 patients, but in three cases the profile generated in RFLP was not conclusive. Thus, Leishmania(Leishmania) infantum was characterized in the lesions of seven patients with CL (17.5%) (Fig. 2). Of these patients, only one had coinfection with HIV and VL and presented skin lesions. The other patients did not exhibit immunodepression or the associated visceral disease during the diagnosis and therapy.
Fig. 2. - RFLP patterns obtained after Hae III digestion of kDNA amplicons. MM - molecular marker - 50 bp, 1 to 7 - analyzed samples, Lb - positive control of L. braziliensis, Li - positive control of L. infantum, La - positive control of L. amazonensis.
Leishmania infantum has been identified as a causative agent of CL in humans from the Mediterranean. In the Southeast of Europe, this is the only species that has been detected in autochthonous cases5.
In France, a fairly comprehensive study examined all the cases of leishmaniasis in the country, from 2009 to 2012. At that time, of the 317 autochthonous cases of leishmaniasis, 39 (12.3%) were cases of CL and all of them due to L. infantum 2.
Cases of L. infantum as an etiological agent of CL have previously been described in the Americas15 , 16 , 17 , 18. In Brazil, this species was first reported in the cutaneous lesions of immunosupressed patients by OLIVEIRA NETO et al. 19. However, in the State of MatoGrosso do Sul, this species has only been isolated in patients with VL12 , 20.
The finding of L. infantum in lesions of patients with CL inMato Grosso do Sul is expected, since there are several reports of the presence of this species causing this clinical manifestation in endemic areas for VL in the Old and New World, as already mentioned. The scarcity of molecular studies aimed at identifying the species involved in cases of CL in this area contributed to the fact that L. infantum have not been previously identified, so that CL cases for this etiology are probably underdiagnosed and certainly undernotified.
This is the first description of the participation of L. infantum as a causative agent of the disease in immunocompetent patients in Brazil.
The identification of Leishmania spp. in certain transmission foci, particularly in areas where different sympatric species occur is important since it will improve the epidemiological knowledge of this disease. In addition, it contributes to the adoption of control measures, improvement of prognosis, and selection of appropriate therapeutic protocols21 , 22 , 23.
Besides the characterization of the species, the isoenzyme identification of circulating strains can provide important information about these dermotropics strains, as observed in different locations24 , 25. Further studies are required to isolate and characterize the different strains of Leishmania spp. that affect humans in Mato Grosso do Sul, and to gain a better understanding of their tropism for cutaneous areas.
REFERENCES
- 1.Rioux JA, Lanotte G, Maazoun R, Perello R, Pratlong F. Leishmania infantum Nicolle, 1908, agent du bouton d'Orient autochtone. A propos de l'identification biochimique de deus souches isolées dans les Pyrénées-Orientales. CR Seances Acad Sci D. 1980;291:701–703. [PubMed] [Google Scholar]
- 2.Lachaud L, Dedet JP, Marty P, Faraut F, Buffet P, Gangneux JP. Surveillance of leishmaniases in France, 1999 to 2012. Euro Surveill. 2013;18:20534–20534. [PubMed] [Google Scholar]
- 3.Pratlong F, Dedet JP, Marty P, Portús M, Deniau M, Dereure J. Leishmania-human immunodeficiency virus coinfection the Mediterranean basin: isoenzymatic characterization of 100 isolates of the Leishmania infantum complex. J Infect Dis. 1995;172:323–326. doi: 10.1093/infdis/172.1.323. [DOI] [PubMed] [Google Scholar]
- 4.Aoun K, Bouratbine A. Cutaneous Leishmaniasis in North Africa: a review. Parasite. 2014;21:14–14. doi: 10.1051/parasite/2014014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Del Giudice P, Marty P, Lacour JP, Perrin C, Pratlong F, Haas H. Cutaneous leishmaniasis due to Leishmania infantum. Case reports and literature review. Arc Dermatol. 1998;134:193–198. doi: 10.1001/archderm.134.2.193. [DOI] [PubMed] [Google Scholar]
- 6.Frank C, Hadziandoniou M, Pratlong F, Garifallou A, Rioux JA. Leishmania tropica and Leishmania infantum responsible for cutaneous leishmaniasis in Greece: sixteen autochthonous cases. Trans R Soc Trop Med Hyg. 1993;87:184–185. doi: 10.1016/0035-9203(93)90482-6. [DOI] [PubMed] [Google Scholar]
- 7.Harrat Z, Pratlong F, Belazzoug S, Dereure J, Deniau M, Rioux JA. Leishmania infantum and L major in Algeria. Trans R Soc Trop Med Hyg. 1996;90:625–629. doi: 10.1016/s0035-9203(96)90410-1. [DOI] [PubMed] [Google Scholar]
- 8.Scott JA, Davidson RN, Grant HR, Felmingham D, Scott GM, Olliaro P. Aminosidine (paromomycin) in the treatment of leishmaniasis imported into the United Kingdom. Trans R Soc Trop Med Hyg. 1992;86:617–619. doi: 10.1016/0035-9203(92)90151-2. [DOI] [PubMed] [Google Scholar]
- 9.Menezes JF, Filho, Barros RM, Silva AL, Mambelli M, Silva PG. Leishmaniose cutâneo mucosa ou tegumentar americana: revisão da literatura e caso clínico. Odontol Mod. 1986;13:32–42. [Google Scholar]
- 10.Nunes VL, Dorval ME, Oshiro ET, Noguchi RC, Arão LB, Hans G., Filho Estudo epidemiológico sobre Leishmaniose Tegumentar (LT) no município de Corguinho, Mato Grosso do Sul - estudos na população humana. Rev Soc Bras Med Trop. 1995;28:185–193. doi: 10.1590/s0037-86821995000300004. [DOI] [PubMed] [Google Scholar]
- 11.Dorval ME, Oshiro ET, Cupolillo E, Castro AC, Alves T. Ocorrência de leishmaniose tegumentar americana no Estado Mato Grosso do Sul associada à infecção por Leishmania (Leishmania) amazonensis. Rev Soc Bras Med Trop. 2006;39:43–46. doi: 10.1590/s0037-86822006000100008. [DOI] [PubMed] [Google Scholar]
- 12.Lima MS, Júnior, Andreotti R, Dorval ME, Oshiro ET, Oliveira AG, Matos MF. Identificação de espécies de Leishmania isoladas de casos humanos em Mato Grosso do Sul por meio da reação em cadeia da polimerase. Rev Soc Bras Med Trop. 2009;42:303–308. doi: 10.1590/s0037-86822009000300012. [DOI] [PubMed] [Google Scholar]
- 13.Volpini AC, Passos VM, Oliveira GC, Romanha AJ. PCR-RFLP to identify Leishmania (Viannia) braziliensis and L: (Leishmania) amazonensis causing American cutaneous leishmaniasis. Acta Trop. 2004;90:31–37. doi: 10.1016/j.actatropica.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 14.de Andrade HM, Reis AB, dos Santos SL, Volpini AC, Marques MJ, Romanha AJ. Use of PCR-RFLP to identify Leishmania species in naturally-infected dogs. Vet Parasitol. 2006;140:231–238. doi: 10.1016/j.vetpar.2006.03.031. [DOI] [PubMed] [Google Scholar]
- 15.De Lima H, Rodríguez N, Feliciangeli MD, Barrios MA, Sosa A, Agrela I. Cutaneous leishmaniasis due to Leishmania chagasi/Le: infantum in an endemic area of Guarico State, Venezuela. Trans R Soc Trop Med Hyg. 2009;103:721–726. doi: 10.1016/j.trstmh.2008.11.019. [DOI] [PubMed] [Google Scholar]
- 16.Melby PC, Kreutzer RD, MacMahon-Pratt D, Gam AA, Neva FA. Cutaneous leishmaniais: review of 59 cases seen at the National Institutes of Health. Clin Infect Dis. 1992;15:924–937. doi: 10.1093/clind/15.6.924. [DOI] [PubMed] [Google Scholar]
- 17.Noyes H, Chance M, Ponce C, Ponce E, Maingon R. Leishmania chagasi: genotypically similar parasites from Honduras cause both visceral and cutaneous leishmaniasis in humans. Exp Parasitol. 1997;85:264–273. doi: 10.1006/expr.1996.4133. [DOI] [PubMed] [Google Scholar]
- 18.Zeledón R, Hidalgo H, Víquez A, Urbina A. Atypical cutaneous leishmaniasis in a semiarid region of north-west Costa Rica. Trans R Soc Trop Med Hyg. 1989;83:786–786. doi: 10.1016/0035-9203(89)90328-3. [DOI] [PubMed] [Google Scholar]
- 19.Oliveira MP, Neto, Grimaldi G, Jr, Momem H, Pacheco RS, Marzochi MC, MacMahon-Pratt D. Active cutaneous leishmaniasis in Brazil induced by Leishmania donovani chagasi. Mem Inst Oswaldo Cruz. 1986;81:303–309. doi: 10.1590/s0074-02761986000300006. [DOI] [PubMed] [Google Scholar]
- 20.Oliveira AG, Galati EA, de Oliveira O, de Oliveira GR, Espindola IA, Dorval ME. Abundance of Lutzomyia longipalpis (Diptera: Psychodidae: Phlebotominae) and urban transmission of visceral leishmaniasis in Campo Grande, state of Mato Grosso do Sul, Brazil. Mem Inst Oswaldo Cruz. 2006;101:869–874. doi: 10.1590/s0074-02762006000800008. [DOI] [PubMed] [Google Scholar]
- 21.Bañuls A, Hide M, Prugnolle F. Leishmania and the leishmaniases: a parasite genetic update and advances in taxonomy, epidemiology and pathogenicity in humans. Adv Parasitol. 2007;64:1–109. doi: 10.1016/S0065-308X(06)64001-3. [DOI] [PubMed] [Google Scholar]
- 22.Jirkù M, Zemanová E, Al-Jawabreh A, Schönian G, Lukes J. Development of a direct species-specific PCR assay for differential diagnosis of Leishmania tropica. Diagn Microbiol Infect Dis. 2006;55:75–79. doi: 10.1016/j.diagmicrobio.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 23.Wortmann G, Hochberg L, Houng HH, Sweeney C, Zapor M, Aronson N. Rapid identification of Leishmania complexes by a real-time PCR assay. Am J Trop Med Hyg. 2005;73:999–1004. [PubMed] [Google Scholar]
- 24.Belhadj S, Pratlong F, Hammami M, Kallel K, Dedet JP, Chaker E. Human cutaneous leishmaniasis due to Leishmania infantum in the Sidi Bourouis focus (Northern Tunisia): epidemiological study and isoenzymatic characterization of the parasites. Acta Trop. 2003;85:83–86. doi: 10.1016/s0001-706x(02)00255-3. [DOI] [PubMed] [Google Scholar]
- 25.Martin-Sanchez J, Gramiccia M, Di Muccio T, Ludovisi A, Morillas-Marquez F. Isoenzymatic polymorphism of Leishmania infantum in southern Spain. Trans R Soc Trop Med Hyg. 2004;98:228–232. doi: 10.1016/s0035-9203(03)00060-9. [DOI] [PubMed] [Google Scholar]


