A 40-year-old man presented with recurrent ulceration over both elbows and forearms since early childhood. The onset of lesions was spontaneous with every episode presenting as skin colored raised painless lesions over both elbows and extensor forearms, which subsequently ulcerated and healed spontaneously leaving behind light- and dark-colored scars.
Examination revealed polymorphic lesions varying from a few skin-colored to erythematous papules, ulcers with central keratinous plug, and some in stages of healing with evidence of postinflammatory hypo- and hyperpigmentation [Figure 1].
Figure 1.

Skin-colored to erythematous hyperkeratotic papules in various stages of evolution, some with ulceration with a central keratinous plug
A skin biopsy was undertaken with a clinical suspicion of a transepidermal elimination disorder. Histopathology revealed epidermal proliferation with compact ortho- and parakeratosis, some with granular nuclear debris and an adjacent mixed cell infiltrate. Altered collagen was seen extruding transepidermally [Figure 2]. Laboratory parameters revealed a normal hemogram, blood sugar profile, and renal parameters. The case was diagnosed as reactive perforating collagenosis and managed with topical tretinoin cream 0.05% once at night with partial response.
Figure 2.
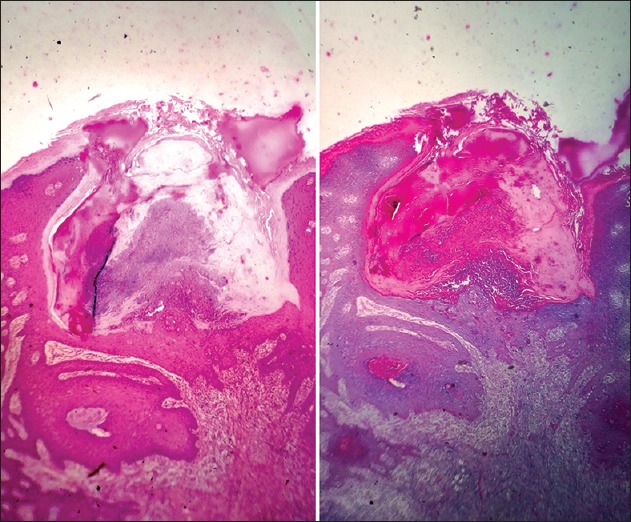
Epidermal proliferation with compact ortho- and parakeratosis, and adjacent mixed cell infiltrate. Altered collagen is seen extruding transepidermally, H and E, 10× (left) and Masson's Trichrome 10× (right)
Perforating disorders of the skin classically include Kyrle's disease, perforating folliculitis, reactive perforating collagenosis, and elastosis perforans serpiginosa. These disorders manifest clinically in varied forms, but histopathologically share evidence of transepidermal elimination of dermal constituents. Reactive perforating collagenosis is a rare form of perforating disorder characterized by transepidermal elimination of altered collagen. Both inherited and acquired forms are known. Inherited are rarer[1,2] and manifest in early childhood as was in our case and acquired appear in middle age often associated with chronic renal failure and diabetes.[3,4]
Treatment modalities reported to be beneficial include ultraviolet B phototherapy, allopurinol, and topical retinoids.[5,6,7]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Verma R, Vasudevan B, Pragasam V, Deb P, Venugopal R, Mitra D. A rare case of familial reactive perforating collagenosis. Indian J Dermatol. 2013;58:408. doi: 10.4103/0019-5154.117341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pai VV, Naveen KN, Athanikar SB, Shastri DU, Rai V. Familial reactive perforating collagenosis: A report of two cases. Indian J Dermatol. 2014;59:287–9. doi: 10.4103/0019-5154.131405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim SW, Kim MS, Lee JH, Son SJ, Park KY, Li K, et al. A clinicopathologic study of thirty cases of acquired perforating dermatosis in Korea. Ann Dermatol. 2014;26:162–71. doi: 10.5021/ad.2014.26.2.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deshmukh SP, Sharma YK, Dash K, Chaudhari NC, Deo KS. Clinicoepidemiological study of skin manifestations in patients of chronic renal failure on hemodialysis. Indian Dermatol Online J. 2013;4:18–21. doi: 10.4103/2229-5178.105458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tilz H, Becker JC, Legat F, Schettini AP, Inzinger M, Massone C. Allopurinol in the treatment of acquired reactive perforating collagenosis. An Bras Dermatol. 2013;88:94–7. doi: 10.1590/S0365-05962013000100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sehgal VN, Verma P, Bhattacharya SN, Sharma S. Familial reactive perforating collagenosis in a child: Response to narrow-band UVB. Pediatr Dermatol. 2013;30:762–4. doi: 10.1111/j.1525-1470.2012.01736.x. [DOI] [PubMed] [Google Scholar]
- 7.Bhat YJ, Manzoor S, Qayoom S, Wani R, Baba AN, Bhat AH. Familial reactive perforating collagenosis. Indian J Dermatol. 2009;54:334–7. doi: 10.4103/0019-5154.57608. [DOI] [PMC free article] [PubMed] [Google Scholar]


