Abstract
The term sepsis-associated encephalopathy (SAE) has been applied to animal models, postmortem studies in patients, and severe cases of sepsis. SAE is considered to include all types of brain dysfunction, including delirium, coma, seizure, and focal neurological signs. Clinical data for sepsis-associated delirium (SAD) have been accumulating since the establishment of definitions of coma or delirium and the introduction of validated screening tools. Some preliminary studies have examined the etiology of SAD. Neuroinflammation, abnormal cerebral perfusion, and neurotransmitter imbalances are the main mechanisms underlying the development of SAD. However, there are still no specific diagnostic blood, electrophysiological, or imaging tests or treatments specific for SAD. The duration of delirium in intensive care patients is associated with long-term functional disability and cognitive impairment, although this syndrome usually reverses after the successful treatment of sepsis. Once the respiratory and hemodynamic states are stabilized, patients with severe sepsis or septic shock should receive rehabilitation as soon as possible because early initiation of rehabilitation can reduce the duration of delirium. We expect to see further pathophysiological data and the development of novel treatments for SAD now that reliable and consistent definitions of SAD have been established.
Keywords: Delirium, Coma, Acute brain dysfunction, Confusion Assessment Method for the Intensive Care Unit (CAM-ICU), Intensive Care Delirium Screening Checklist (ICDSC), Sepsis-associated encephalopathy (SAE)
Introduction
The Pneumonia Severity Index, which was developed in the USA, includes five key clinical factors: pulse rate, respiratory rate, systolic blood pressure, body temperature, and mental status [1]. Altered mental status was also cited in the diagnostic criteria for sepsis proposed by Levy et al. [2]. Mental confusion, rather than altered mental status, was used to assess the severity of community-acquired pneumonia in another study [3]. Although these studies did not clearly define altered mental status or mental confusion, these states may be indicative of delirium because an acute change in mental status is a major feature of delirium [4].
The American Psychiatric Association’s Fifth Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) revised the diagnostic criteria for delirium [5]. All states of altered arousal, except coma, are included in the definition of delirium (Fig. 1). Delirium and coma occurring in patients with critical illness are referred to as acute brain dysfunction (Fig. 2) [6]. The terms septic encephalopathy or sepsis-associated encephalopathy (SAE) are often used in Japan. However, “delirium” is used globally instead of“encephalopathy” in current diagnostic manuals such as DSM-5 and the International Classification of Diseases (ICD-10). In the present review, we have used the terms sepsis-associated delirium (SAD) or infectious delirium. SAD is considered a diffuse cerebral dysfunction caused by the systemic inflammatory response to an infection without evidence of a central nervous system infestation (i.e., infection) [7].
Fig. 1.
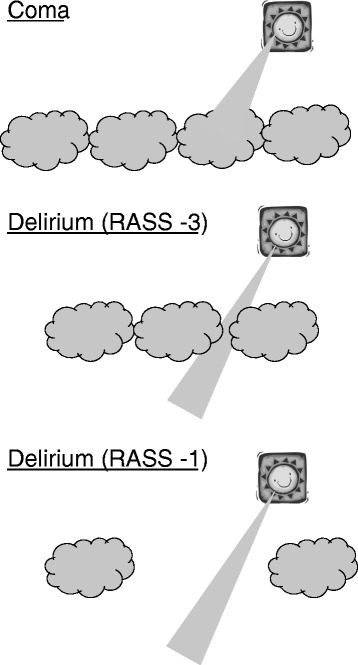
Illustration of acute brain dysfunction (coma and delirium). The sun represents the investigator. The sunbeam represents the interview or tests (i.e., CAM-ICU) used to assess inattention. The clouds (i.e., RASS score of ≤−4) represent cover on some levels of arousal required to maintain cognition. RASS −3 the patient opens their eyes or moves in response to a voice but does not make eye contact. RASS −1 the patient is not fully alert but opens their eyes and makes eye contact, which is sustained for more than 10 s in response to a voice
Fig. 2.
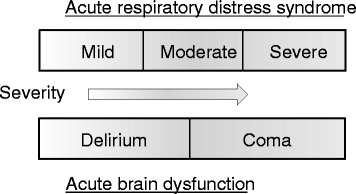
The relationships between coma and delirium in contrast to acute respiratory distress syndrome
Review
Pathophysiology of SAD
Neuroinflammation
The systemic inflammatory response is a key phenomenon in critical illnesses and may progress to organ dysfunction, including the brain. Systemic inflammation and endothelial activation frequently occur during critical illnesses and may augment cytokine transport across the blood–brain barrier (BBB) [8], BBB disruption [9], and the infiltration of leukocytes and cytokines into the central nervous system [10]. These events may result in ischemia and neuronal apoptosis, which may present clinically as delirium [11]. These mechanisms have been investigated using animal models [7, 12, 13] (Fig. 3).
Fig. 3.

The mechanism of sepsis-associated delirium. Double-lined boxes correspond to the clinical evidence reported in the main text. SIRS systemic inflammatory response syndrome, ROS reactive oxygen species, NO nitric oxide
Some recent clinical studies have sought to standardize the detection of delirium in critically ill patients. In a prospective cohort study [14], interleukin 6 (IL-6) concentrations were higher in delirious patients than those in comatose patients [14]. Another study revealed that, after adjusting for covariates, lower plasma concentrations of matrix metalloproteinase-9 (MMP-9) and protein C and higher concentrations of soluble tumor necrosis factor receptor-1 (sTNFR1) were associated with increased risk of delirium [15]. These results suggest that inflammation and coagulation may play important roles in the development of delirium in patients with critical illness. We also assessed delirium and obtained blood samples at two times: extubation (0 h) and 24 h after extubation (24 h) [16]. We found that the serum concentrations of procalcitonin and IL-6 were significantly higher in the delirious patients than those in the non-delirious patients at 24 h, but not at 0 h. Crucially, these studies showed an association between the onset of delirium and circulating biomarkers in critically ill patients in both infectious and non-infectious conditions. However, there are no clinical studies describing an association between SAD (i.e., infectious delirium) and biomarkers, even though much data have been accumulated in animal models of sepsis [17, 18].
Two important studies have examined the association between delirium and biomarkers in two different situations. The first study of intensive care unit (ICU) patients with or without infection/systemic inflammatory response syndrome (SIRS) revealed that IL-8 concentrations were significantly associated with delirium in infected patients, whereas the anti-inflammatory cytokine IL-10 and amyloid β1-42/40 were associated with delirium in non-infected patients [19]. The second study examined the association between delirium and biomarkers in critically ill patients with or without sepsis [20] and revealed that plasma sTNFR1, sTNFR2, adiponectin, and IL-1β concentrations were higher in delirious patients than those in non-delirious patients. However, sepsis did not modify the associations between these biomarkers and the presence of delirium.
Cerebral perfusion abnormalities
Several studies have measured cerebral perfusion in patients with SAD. Pfister et al. [21] reported that SAD was significantly associated with C-reactive protein (CRP), S-100β, and cortisol concentrations, but not with IL-6 concentrations, and that elevated CRP was significantly associated with disturbed autoregulation. The impairments in cerebrovascular autoregulation were subsequently investigated daily for 4 days after onset in patients with severe sepsis or septic shock [22]. Autoregulation was impaired in 60 % of patients on day 1, 59 % on day 2, 41 % on day 3, and 46 % on day 4. SAD was present in 76 % of patients. Impaired autoregulation on day 1 was also associated with the presence of SAD on day 4. These results suggest that dysfunction of cerebral autoregulation is a trigger for the development of SAD. Impaired autoregulation might result in cerebral hypoperfusion or hyperperfusion, as well as SAD.
In another study, reduced vascular reactivity (as measured by peripheral artery tonometry) was associated with a longer duration of delirium in a study of critically ill patients, in which 30 % of patients had severe sepsis on admission [23].
Neurotransmitter imbalances
Imbalances in several neurotransmitters, including the dopamine, γ-aminobutyric acid (GABA), and acetylcholine [24, 25] systems are also implicated in the etiology of delirium. Dopamine increases the neuronal excitability, while GABA and acetylcholine decrease neuronal excitability. An imbalance in one or more of these neurotransmitters results in neuronal instability and unpredicatable neurotransmission. Dopamine excess and acetylcholine depletion have been associated with delirium. Several studies in non-ICU settings have found a strong association between plasma anticholinergic activity (PAA), a measure of cholinergic blockade [26], and the development of delirium [27, 28]. Inflammation and cholinergic blockade, as measured by serum CRP and PAA, respectively, were associated with delirium in critically ill patients, and serum CRP and PAA were correlated with each other [29]. Another study in postoperative patients showed that the preoperative plasma cholinesterase activity was correlated with the changes in CRP and IL-6 concentrations after surgery in delirious patients [30]. Delirium was associated with impaired interactions between the cholinergic and immune systems. However, prophylactic, short-term administration of oral rivastigmine, a cholinesterase inhibitor, did not reduce the incidence of delirium in elderly patients for up to 6 days after elective cardiac surgery [31]. Therefore, owing to the multifactorial pathophysiology of delirium, interventions that only target the cholinergic system might be insufficient to prevent delirium.
Diagnosis of SAD
Delirium screening tools
The 2013 American College of Critical Care Medicine (ACCM)/Society of Critical Care Medicine (SCCM) clinical practice guidelines for pain, agitation, and delirium (PAD) recommend that critically ill patients should undergo routine monitoring for the onset of delirium in the ICU using a validated tool [32]. The Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) [33] and the Intensive Care Delirium Screening Checklist (ICDSC) [34] are the most valid and reliable tools for monitoring delirium in adult ICU patients [32].
The CAM-ICU, which was derived from DSM-4 criteria, evaluates four features of delirium: (1) acute changes or fluctuations in mental status from baseline, (2) inattention, (3) altered consciousness, and (4) disorganized thinking. The CAM-ICU is positive if the patient exhibits features 1 and 2 and either of features 3 or 4. Patients are defined as comatose if they respond only to physical/painful stimulation with movement but do not open their eyes (Richmond Agitation–Sedation Scale (RASS) [35] score, −4) or if they do not respond to verbal or physical stimuli (RASS score, −5) (Fig. 1). Delirium is defined as a response to verbal stimulation with eye opening (RASS score of −3 to +4) and a positive CAM-ICU value [4].
A change in the RASS score from −3 (the patient opens their eyes or move in response to a voice but does not make eye contact) to −4, a transition from delirium to coma, may be part of the continuum of progressively smaller levels of arousal. Alternatively, does this transition indicate a fundamental change in the pathophysiology of the acute brain dysfunction? [36]. The widespread administration of sedatives during mechanical ventilation of septic patients further complicates our understanding of acute brain dysfunction in such patients [36]. Subsequently, Patel et al. classified delirium into two categories: sedation-related delirium (delirium that abates shortly after sedative interruption) and persistent delirium [37]. After interrupting the patients’ sedatives, the investigator assessed whether the patients could follow four commands (squeeze the investigator’s hand, open their eyes, track an object with their eyes, or stick out their tongue) [38]. Patients who could not follow these commands after 2 h were classified as having persistent delirium. It was reported that the 1-year mortality rate was greater in patients with persistent delirium than that in patients without delirium or with sedation-related delirium [37]. In some studies, delirium was defined as a RASS score of >−3 [39] or >−2 [22].
The ICDSC, which is also derived from DSM-4 criteria, evaluates eight features of delirium: (1) altered consciousness; (2) inattention; (3) disorientation; (4) hallucinations, delusions, or psychoses; (5) psychomotor agitation or retardation; (6) inappropriate speech or mood; (7) disturbed sleep/wake cycles; and (8) symptom fluctuations [34]. The ICDSC, which incorporates the assessment of each feature over the course of the nursing shift, should not be used in heavily sedated patients (i.e., RASS score of ≤−4). The ICDSC is assessed based on the observations over the preceding 24 h. A total score of ≥4 denotes the presence of delirium, while total scores of 1–3 denote subsyndromal delirium [40]. The ICU mortality rates were 2.4, 10.6, and 15.9 % in patients without delirium, patients with subsyndromal delirium, and patients with delirium, respectively, defined according to ICDSC scores [40]. Therefore, the ICDSC allows ICU specialists to detect subsyndromal delirium, which is associated with intermediate adverse outcomes.
Electrophysiological testing
Electrophysiological testing and neuroimaging are not always needed for the diagnosis of acute brain dysfunction or delirium in septic patients (Fig. 4). These tests should be considered in patients with persistent coma or delirium despite improvements in the functions of other organs and if the sedatives have been washed out.
Fig. 4.
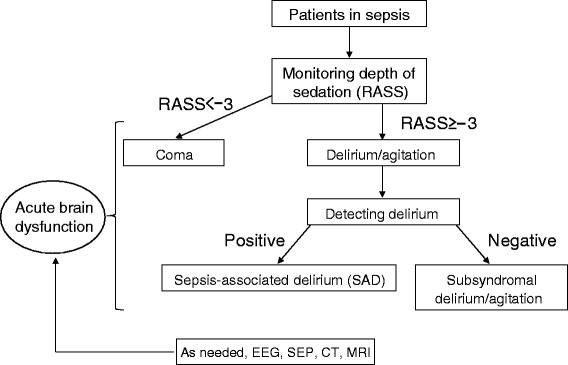
Diagnostic decision tree for acute brain dysfunction and sepsis-associated delirium (SAD). RASS Richmond Agitation–Sedation Scale, EEG electroencephalogram, SEP sensory evoked potential, CT computed tomography, MRI magnetic resonance imaging
The results of electroencephalograms (EEGs) are classified by severity based on the predominant waveform, including excessive θ, predominant δ, or triphasic waves, and suppression or burst suppression [41]. One study investigated the diagnosis of SAD by the CAM-ICU and the predominant EEG features on day 4 after a reduction of sedation to a RASS score of >−2 [22]. The authors reported that the diagnosis of SAD was not associated with EEG abnormalities. Furthermore, cerebrovascular autoregulation was not associated with EEG abnormalities.
Hosokawa et al. conducted a systematic review of EEG abnormalities in patients diagnosed with SAE or sepsis-associated brain dysfunction (SABD) [42]. The diagnostic methods were not reported in the systematic review and 5/17 studies were conducted before the introduction of the CAM-ICU and ICDSC in 2001. It is possible that SAE and SABD include coma and/or delirium in septic patients. The incidence of EEG abnormalities in septic patients ranged from 12 to 100 % for background abnormalities and from 6 to 12 % for triphasic waves. The authors concluded that EEG is a sensitive tool for the detection and diagnosis of SAE/SABD. A slowing of the normal α rhythm coinciding with the appearance of θ activity occurs in patients without evidence of encephalopathy and in patients with mild to moderate encephalopathy (e.g., confusion and delirium) and therefore reflects cortical dysfunction. More severe states of altered consciousness (e.g., stupor and coma) are associated with greater slowing together with increased δ activity, triphasic waves, and the more malignant burst suppression patterns that indicate impaired function of deeper brain structures, such as the basal ganglia and the diencephalon.
One study has sought to differentiate between coma and delirium in septic shock patients [43]. Coma was defined as a Glasgow Coma Scale (GCS) score of <8 in non-sedated patients or at 3 days after discontinuing sedation in previously sedated patients. Delirium was evaluated using the CAM-ICU. EEGs were analyzed using the Synek 5-point scale [44]. The median EEG grade was 3.5 (range 3.0–4.0) in coma and 3.0 (range 1.0–3.5) in delirium. An EEG grade of >3 was significantly more frequent in patients who died.
Compared with EEG, few studies have investigated sensory evoked potentials (SEP) in sepsis. The peak latency was significantly longer in patients with severe sepsis or septic shock than that in healthy controls, and it was correlated with the severity of sepsis [45]. However, the peak latency was not significantly different between patients with severe sepsis and those with septic shock. Although no studies have measured SEP in patients with SAD, a benefit of SEP is that it is not affected by sedation.
Neuroimaging
Brain computed tomography (CT) is often performed when septic patients display sudden changes in arousal or mental status, or persistent coma or delirium is unexplained by sedation. CT scans provide some information to aid the differential diagnosis, including focal brain infection, bleeding, and air embolism.
Magnetic resonance imaging (MRI) provides better and earlier information on brain damage, especially of the white matter and BBB. In a prospective study of 71 patients with septic shock, ischemic stroke and leukoencephalopathy were the two most frequent lesions [43]. Sharshar et al. hypothesized that leukoencephalopathy reflects BBB changes and identified it neuropathologically in a patient with diffuse leukoencephalopathy [46]. They also showed that an EEG grade of >3, as defined by Synek’s scale [44], was correlated with the presence of ischemic stroke or leukoencephalopathy on MRI in comatose or delirious patients. Therefore, they recommended that EEG should be done continuously or every day before MRI because of the risk of transport from the ICU to the MRI suite.
Treatment of SAD
There are still no specific treatments for SAD. The treatment options for severe sepsis and septic shock are described in established guidelines [47], which recommend that continuous or intermittent sedation should be limited in mechanically ventilated septic patients and that the treatments should target specific titration endpoints. An a priori subgroup analysis of the Maximizing Efficacy of Targeted Sedation and Reducing Neurological Dysfunction (MENDS) study revealed that septic patients treated with dexmedetomidine had more days free of delirium than patients treated with a lorazepam-based sedation regimen [48]. However, lorazepam infusion is not available and dexmedetomidine at doses >0.7 μg/kg/h is not permitted in Japan.
Interestingly, two clinical trials have examined the association between stain use in an ICU and delirium in critically ill patients [49, 50]. Statins have pleiotropic effects on inflammation and coagulation. In the first study, statin exposure was independently associated with 2.28 times greater odds of being free of delirium [49]. In the second study, in which 55 % of patients had sepsis on day 1, statin exposure was associated with reduced risk of delirium among patients with sepsis on day 1 but not among patients without sepsis on day 1 [50]. A phase 2, randomized, placebo-controlled trial investigating whether simvastatin can reduce the risk of delirium in mechanically ventilated critically ill patients is ongoing (ISRCTN89079989).
Early physical and occupational therapy in mechanically ventilated patients, of whom 14 % had sepsis, decreased the number of days with delirium to half of that in the control group, even though the sedation regimen was identical in both groups (median 2 vs 4 days) [51]. Patients with severe sepsis or septic shock who display improvements and stabilization of their respiratory and hemodynamic states should receive rehabilitation as soon as possible. Delirium associated with sepsis or other causes was an independent predictor of the 6-month mortality rate [4], and the duration of delirium in the ICU was associated with long-term functional disability [52] and cognitive impairment [53, 54]. Furthermore, a cohort study revealed that severe sepsis was independently associated with persistent cognitive and functional limitations [55]. The risk of moderate to severe cognitive impairment tripled in septic patients. Taken together, these findings indicate that cognitive and physical rehabilitation is essential and should be initiated as soon as possible in the ICU and continued for as long as possible after discharge from the ICU.
Conclusions
The pathogenesis of SAD (infectious delirium) and the features of this disorder in vivo are still unclear. Systemic inflammation and endothelial activation are common in critical illnesses and are associated with central nervous system disorders that may present clinically as delirium. Studies of patients with SAD have increased since the development of validated and reliable screening tools for delirium. However, when interpreting these studies, we should carefully assess their definitions of coma or delirium in septic patients. Finally, we believe that blood biomarkers, cerebrovascular autoregulation, electrophysiological, and neuroimaging tests are necessary in septic patients to establish consistent, pan-institutional definitions of coma/delirium.
Acknowledgements
This work was supported by a Grant-in-Aid for Scientific Research (C) (No. 22592015) from the Japan Society for the Promotion of Science.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
RT conducted the literature search and drafted the manuscript. YO helped to revise the manuscript. Both authors read and approved the final manuscript.
References
- 1.Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, Coley CM, Marrie TJ, Kapoor WN. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336:243–50. doi: 10.1056/NEJM199701233360402. [DOI] [PubMed] [Google Scholar]
- 2.Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent J-L, Ramsay G, For the International Sepsis Definitions Conference SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2001;2003(31):1250–6. doi: 10.1097/01.CCM.0000050454.01978.3B. [DOI] [PubMed] [Google Scholar]
- 3.Lim WS, van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, Lewis SA, Macfarlane JT. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58:377–82. doi: 10.1136/thorax.58.5.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE, Jr, Inouye SK, Bernard GR, Dittus RS. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291:1753–62. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 5.European Delirium Association and American Delirium Society The DSM-5 criteria, level of arousal and delirium diagnosis: inclusiveness is safer. BMC Med. 2014;12:141. doi: 10.1186/s12916-014-0141-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pandharipande PP, Pun BT, Herr DL, Maze M, Girard TD, Miller RR, Shintani AK, Thompson JL, Jackson JC, Deppen SA, Stiles RA, Dittus RS, Bernard GR, Ely EW. Effect of sedation with dexmedetomidine vs lorazepam on acute brain dysfunction in mechanically ventilated patients: the MENDS randomized controlled trial. JAMA. 2007;298:2644–53. doi: 10.1001/jama.298.22.2644. [DOI] [PubMed] [Google Scholar]
- 7.Iacobone E, Bailly-Salin J, Polito A, Friedman D, Stevens RD, Sharshar T. Sepsis-associated encephalopathy and its differential diagnosis. Crit Care Med. 2009;37:S331–6. doi: 10.1097/CCM.0b013e3181b6ed58. [DOI] [PubMed] [Google Scholar]
- 8.Qin L, Wu X, Block ML, Liu Y, Breese GR, Hong J-S, Knapp DJ, Crews FT. Systemic LPS causes chronic neuroinflammation and progressive neurodegeneration. Glia. 2007;55:453–62. doi: 10.1002/glia.20467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Descamps L, Coisne C, Dehouck B, Cecchelli R, Torpier G. Protective effect of glial cells against lipopolysaccharide-mediated blood-brain barrier injury. Glia. 2003;42:46–58. doi: 10.1002/glia.10205. [DOI] [PubMed] [Google Scholar]
- 10.Alexander JJ, Jacob A, Cunningham P, Hensley L, Quigg RJ. TNF is a key mediator of septic encephalopathy acting through its receptor, TNF receptor-1. Neurochem Int. 2008;52:447–56. doi: 10.1016/j.neuint.2007.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hughes CG, Patel MB, Pandharipande PP. Pathophysiology of acute brain dysfunction: what’s the cause of all this confusion? Curr Opin Crit Care. 2012;18:518–26. doi: 10.1097/MCC.0b013e328357effa. [DOI] [PubMed] [Google Scholar]
- 12.Burkhart CB, Siegemund M, Steiner LA. Cerebral perfusion in sepsis. Crit Care. 2010;14:215. doi: 10.1186/cc8856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Gool WA, van de Beek D, Eikelenboom P. Systemic infection and delirium: when cytokines and acetylcholine collide. Lancet. 2010;375:773–5. doi: 10.1016/S0140-6736(09)61158-2. [DOI] [PubMed] [Google Scholar]
- 14.Skrobik Y, Leger C, Cossette M, Michaud V, Turgeon J. Factors predisposing to coma and delirium: fentanyl and midazolam exposure; CYP3A5, ABCB1, and ABCG2 genetic polymorphisms; and inflammatory factors. Crit Care Med. 2013;41:999–1008. doi: 10.1097/CCM.0b013e318275d014. [DOI] [PubMed] [Google Scholar]
- 15.Girard TD, Ware LB, Bernard GR, Pandharipande PP, Thompson JL, Shintani AK, Jackson JC, Dittus RS, Ely EW. Associations of markers of inflammation and coagulation with delirium during critical illness. Intensive Care Med. 2012;38:1965–73. doi: 10.1007/s00134-012-2678-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ogino Y, Kaneda K, Nakahara T, Todani M, Miyauchi T, Fujita M, Kawamura Y, Oda Y, Tsuruta R. Systemic inflammation and delirium in the peri-extubation period of mechanical ventilation: an observational prospective study of intensive care unit patients. Bull Yamaguchi Med School. 2015;62:1–10. [Google Scholar]
- 17.Ari I, Kafa IM, Kurt MA. Perimicrovascular edema in the frontal cortex in a rat model of intraperitoneal sepsis. Exp Neurol. 2006;198:242–9. doi: 10.1016/j.expneurol.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Q-H, Sheng Z-Y, Yao Y-M. Septic encephalopathy: when cytokines interact with acetylcholine in the brain. Mil Med Res. 2014;1:20. [DOI] [PMC free article] [PubMed]
- 19.van den Boogaard M, Kox M, Quinn KL, van Achterberg T, van der Hoeven JG, Schoonhoven L, Pickkers P. Biomarkers associated with delirium in critically ill patients and their relation with long-term subjective cognitive dysfunction; indications for different pathways governing delirium in inflamed and noninflamed patients. Crit Care. 2011;15:R297. doi: 10.1186/cc10598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ritter C, Tomasi CD, Dal-Pizzol F, Pinto BB, Dyson A, de Miranda AS, Comim CM, Soares M, Teixeira AL, Quevedo J, Singer M. Inflammation biomarkers and delirium in critically ill patients. Crit Care. 2014;18:R106. doi: 10.1186/cc13887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pfister D, Siegemund M, Dell-Kuster S, Smielewski P, Rüegg S, Strebel SP, Marsch SCU, Pargger H, Steiner LA. Cerebral perfusion in sepsis-associated delirium. Crit Care. 2008;12:R63. doi: 10.1186/cc6891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schramm P, Klein KU, Falkenberg L, Berres M, Closhen D, Werhahn KJ, David M, Werner C, Engelhard K. Impaired cerebrovascular autoregulation in patients with severe sepsis and sepsis-associated delirium. Crit Care. 2012;16:R181. doi: 10.1186/cc11665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hughes CG, Morandi A, Girard TD, Riedel B, Thompson JL, Shintani AK, Pun BT, Ely EW, Pandharipande PP. Association between endothelial dysfunction and acute brain dysfunction during critical illness. Anesthesiology. 2013;118:631–9. doi: 10.1097/ALN.0b013e31827bd193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Adinoff B, Bone GHA, Linnoila M. Acute ethanol poisoning and the ethanol withdrawal syndrome. Med Toxicol. 1988;3:172–96. doi: 10.1007/BF03259881. [DOI] [PubMed] [Google Scholar]
- 25.Trzepacz PT. Is there a final common neural pathway in delirium? Focus on acetylcholine and dopamine. Semin Clin Neuropsychiatry. 2000;5:132–48. doi: 10.153/SCNP00500132. [DOI] [PubMed] [Google Scholar]
- 26.Tune LE, Coyle JT. Serum levels of anticholinergic drugs in treatment of acute extrapyramidal side-effects. Arch Gen Psychiatry. 1980;37:293–7. doi: 10.1001/archpsyc.1980.01780160063007. [DOI] [PubMed] [Google Scholar]
- 27.Flacker JM, Cummings V, Mach JR, Bettin K, Kiely DK, Wei J. The association of serum anticholinergic activity with delirium in elderly medical patients. Am J Geriatr Psychiatry. 1998;6:31–41. doi: 10.1097/00019442-199802000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Golinger RC, Peet T, Tune LE. Association of elevated plasma anticholinergic activity with delirium in surgical patients. Am J Psychiatry. 1987;144:1218–20. doi: 10.1176/ajp.144.9.1218. [DOI] [PubMed] [Google Scholar]
- 29.Tsuruta R, Girard TD, Ely EW, Fujimoto K, Ono T, Tanaka R, Oda Y, Kasaoka S, Maekawa T. Associations between markers of inflammation and cholinergic blockade and delirium in intensive care unit patients: a pilot study. Bull Yamaguchi Med School. 2008;55:35–42. [Google Scholar]
- 30.Cerejeira J, Nogueira V, Luís P, Vaz-Serra A, Mukaetova-Ladinska EB. The cholinergic system and inflammation: common pathways in delirium pathophysiology. J Am Geriatr Soc. 2012;60:669–75. doi: 10.1111/j.1532-5415.2011.03883.x. [DOI] [PubMed] [Google Scholar]
- 31.Gamberini M, Bolliger D, Buse GAL, Burkhart CS, Grapow M, Gagneux A, Filipovic M, Seeberger MD, Pargger H, Siegemund M, Carrel T, Seiler WO, Berres M, Strebel SP, Monsch AU, Steiner LA. Rivastigmine for the prevention of postoperative delirium in elderly patients undergoing elective cardiac surgery-a randomized controlled trial. Crit Care Med. 2009;37:1762–8. doi: 10.1097/CCM.0b013e31819da780. [DOI] [PubMed] [Google Scholar]
- 32.Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, Davidson JE, Devlin JW, Kress JP, Joffe AM, Coursin DB, Herr DL, Tung A, Robinson BRH, Fontaine DK, Ramsay MA, Riker RR, Sessler CN, Pun B, Skrobik Y, Jaeschke R. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41:263–306. doi: 10.1097/CCM.0b013e3182783b72. [DOI] [PubMed] [Google Scholar]
- 33.Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, Speroff T, Gautam S, Bernard GR, Inouye SK. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) Crit Care Med. 2001;29:1370–9. doi: 10.1097/00003246-200107000-00012. [DOI] [PubMed] [Google Scholar]
- 34.Bergeron N, Dubois M-J, Dumont M, Dial S, Skrobik Y. Intensive Care Delirium Screening Checklist: evaluation of a new screening tool. Intensive Care Med. 2001;27:859–64. doi: 10.1007/s001340100909. [DOI] [PubMed] [Google Scholar]
- 35.Sessler CN, Gosnell M, Grap MJ, Brophy GM, O’Neal PV, Keane KA, Tesoro EP, Elswick RK. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care patients. Am J Respir Crit Care Med. 2002;166:1338–44. doi: 10.1164/rccm.2107138. [DOI] [PubMed] [Google Scholar]
- 36.Kress JP. The complex interplay between delirium, sepsis and sedation. Crit Care. 2010;14:164. doi: 10.1186/cc9038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patel SB, Poston JT, Pohlman A, Hall JB, Kress JP. Rapidly reversible, sedation-related delirium versus persistent delirium in the intensive care unit. Am J Respir Crit Care Med. 2014;189:658–65. doi: 10.1164/rccm.201310-1815OC. [DOI] [PubMed] [Google Scholar]
- 38.Kress JP, O’Connor MF, Pohlman AS, Olson D, Lavoie A, Toledano A, Hall JB. Sedation of critically ill patients during mechanical ventilation: a comparison of propofol and midazolam. Am J Respir Crit Care Med. 1996;153:1012–8. doi: 10.1164/ajrccm.153.3.8630539. [DOI] [PubMed] [Google Scholar]
- 39.Shehabi Y, Bellomo R, Reade MC, Bailey M, Bass F, Howe B, McArthur C, Seppelt IM, Webb S, Weisbrodt L. Sedation Practice in Intensive Care Evaluation (SPICE) Study Investigators and the ANZICS Clinical Trials Group. Early Intensive care sedation predicts long-term mortality in ventilated critically ill patients. Am J Respir Crit Care Med. 2012;186:724–31. doi: 10.1164/rccm.201203-0522OC. [DOI] [PubMed] [Google Scholar]
- 40.Ouimet S, Riker R, Bergeon N, Cossette M, Kavanagh B, Skrobik Y. Subsyndromal delirium in the ICU: evidence for a disease spectrum. Intensive Care Med. 2007;33:1007–13. doi: 10.1007/s00134-007-0618-y. [DOI] [PubMed] [Google Scholar]
- 41.Young GB, Bolton CF, Archibald YM, Austin TW, Wells GA. The electroencephalogram in sepsis-associated encephalopathy. J Clin Neurophysiol. 1992;9:145–52. doi: 10.1097/00004691-199201000-00016. [DOI] [PubMed] [Google Scholar]
- 42.Hosokawa K, Gaspard N, Su F, Oddo M, Vincent J-L, Taccone FS. Clinical neurophysiological assessment of sepsis associated brain dysfunction: a systematic review. Crit Care. 2014;18:674. doi: 10.1186/s13054-014-0674-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Polito A, Eischwald F, Le Maho A-L, Polito A, Azabou E, Annane D, Chrétien F, Stevens RD, Carlier R, Sharshar T. Pattern of brain injury in the acute setting of human septic shock. Crit Care. 2013;17:R204. doi: 10.1186/cc12899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Synek VM. Prognostically important EEG coma patterns in diffuse anoxic and traumatic encephalopathies in adults. J Clin Neurophysiol. 1988;5:161–74. doi: 10.1097/00004691-198804000-00003. [DOI] [PubMed] [Google Scholar]
- 45.Zauner C, Gendo A, Kramer L, Funk GC, Bauer E, Schenk P, Ratheiser K, Madl C. Impaired subcortical and cortical sensory evoked potential pathways in septic patients. Crit Care Med. 2002;30:1136–9. doi: 10.1097/00003246-200205000-00030. [DOI] [PubMed] [Google Scholar]
- 46.Sharshar T, Carlier R, Bernard F, Guidoux C, Brouland J-P, Nardi O, de la Grandmaison GL, Aboab J, Gray F, Menon D, Annane D. Brain lesions in septic shock: a magnetic resonance imaging study. Intensive Care Med. 2007;33:798–806. doi: 10.1007/s00134-007-0598-y. [DOI] [PubMed] [Google Scholar]
- 47.Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb SA, Beale RJ, Vincent J-L, Moreno R, the Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41:580–637. doi: 10.1097/CCM.0b013e31827e83af. [DOI] [PubMed] [Google Scholar]
- 48.Pandharipande PP, Sanders RD, Girard TD, McGrane S, Thompson JL, Shintani AK, Herr DL, Maze M, Ely EW for the MENDS investigators Effect of dexmedetomidine versus lorazepam on outcome in patients with sepsis: an a priori-designed analysis of the MENDS randomized controlled trial. Crit Care. 2010;14:R38. doi: 10.1186/cc8916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Page VJ, Davis D, Zhao XB, Norton S, Casarin A, Brown T, Ely EW, McAuley DF. Statin use and risk of delirium in the critically ill. Am J Respir Crit Care Med. 2014;189:666–73. doi: 10.1164/rccm.201306-1150OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Morandi A, Hughes CG, Thompson JL, Pandharipande PP, Shintani AK, Vasilevskis EE, Han JH, Jackson JC, Laskowitz DT, Bernard GR, Ely EW, Girard TD. Statins and delirium during critical illness: a multicenter, prospective cohort study. Crit Care Med. 2014;42:1899–909. doi: 10.1097/CCM.0000000000000398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, Spears L, Miller M, Franczyk M, Deprizio D, Schmidt GA, Bowman A, Barr R, McCallister KE, Hall JB, Kress JP. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373:1874–82. doi: 10.1016/S0140-6736(09)60658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Brummel NE, Jackson JC, Pandharipande PP, Thompson JL, Shintani AK, Dittus RS, Gill TM, Bernard GR, Ely EW, Girard TD. Delirium in the ICU and subsequent long-term disability among survivors of mechanical ventilation. Crit Care Med. 2014;42:369–77. doi: 10.1097/CCM.0b013e3182a645bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.van den Boogaard M, Schoonhoven L, Evers AW, van der Hoeven JG, van Achterberg T, Pickkers P. Delirium in critically ill patients: impact on long-term health-related quality of life and cognitive functioning. Crit Care Med. 2012;40:112–8. doi: 10.1097/CCM.0b013e31822e9fc9. [DOI] [PubMed] [Google Scholar]
- 54.Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, Brummel NE, Hughes CG, Vasilevskis EE, Shintani AK, Moons KG, Geevarghese SK, Canonico A, Hopkins RO, Bernard GR, Dittus RS, Ely EW, for the BRAIN-ICU Study Investigators Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369:1306–16. doi: 10.1056/NEJMoa1301372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304:1787–94. doi: 10.1001/jama.2010.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]


