Abstract
Background
The aim of this study was to conduct a national survey of hand surgery fellowship program directors to determine differences of opinions of essential components of hand surgery training among program directors from plastic and orthopedic surgery programs.
Methods
We performed a web-based survey of 74 program directors from all ACGME accredited hand surgery fellowship programs to determine components that are essential for hand surgery training. The survey included assessment of 9 general areas of practice, 97 knowledge topics, and 172 procedures. 27 scales of related survey items were created to determine differences between specialty groups based on clinical themes.
Results
We had an 84% response rate, including 49 orthopedic and 12 plastic surgery program directors. There were significant differences in mean responses between the specialty groups in 11 of 27 scales. Only one scale, forearm fractures, contained items with a significantly stronger preference for essential rating among orthopedic surgeons. The other 10 scales contained items with a significantly higher preference for essential rating among plastic surgeons, most of which related to soft tissue injury and reconstruction. The burn scale had the greatest discrepancy in opinion of essential ratings between the groups, followed by pedicled and free tissue transfer, and amputation and fingertip injuries.
Conclusions
Despite being united under the subspecialty of hand surgery, program directors tend to emphasize clinical areas that are stressed in their respective primary disciplines. These differences promote the advantage of programs providing exposure to both plastic and orthopedic surgery trained hand surgeons.
Keywords: Competencies, fellowship, hand surgery training
Over the past decade, program directors of all Accreditation Council for Graduate Medical Education (ACGME) accredited training programs have been required to assess graduates’ proficiency in six competency domains (1, 2). ACGME competency domains include patient care, medical knowledge, interpersonal and communication skills, practice-based learning and improvement, systems-based practice, and professionalism (1, 3). These competency domains are broadly defined in order to be applicable to all disciplines (4). However, the movement toward competency-based training has prompted several surgical specialties to better define skills that are expected of trainees as it relates to patient care and medical knowledge (5-13).
Defining competencies and implementing competency-based training in hand surgery training is challenging for a number of reasons. Hand surgeons and trainees come from three different specialties—plastic surgery, orthopedic surgery, or general surgery. Thus clinical experience of fellows prior to starting hand surgery training can vary considerably. There is also ongoing debate as to the anatomic regions of the upper extremity in which hand surgeons should be proficient. Thus, clinical exposure during fellowship can differ considerably. There are disparities in passage rates for the hand surgery certification examination among plastic, orthopedic, and general surgeons (14), which may be due to differences in residency or fellowship experiences among these specialties. Thus, it is important to understand how educational priorities differ among training programs based on their accreditation specialty.
General strengths and weaknesses of plastic and orthopedic surgery accredited programs can be highlighted through a better understanding of philosophical differences of clinical priorities of training. The aim of this study was to conduct a national survey of hand surgery fellowship program directors to determine differences of opinions of essential components of hand surgery training among program directors from plastic surgery and orthopedic surgery accredited programs. We hypothesize that program directors will favor skills that are relevant to their primary residency background, despite being united under the subspecialty of hand surgery.
METHODS
Study Sample
This study was approved by our institutional review board. We recruited all program directors of the 76 ACGME accredited hand surgery fellowship programs (as of September 2011) to participate in this study. Two programs had dual oversight by both plastic and orthopedic surgery residency review committees with the same program director. Thus, in the end, 74 program directors were invited to participate via email, with two weekly reminders to nonresponders. Programs having dual accreditation and a single program director were assigned to the specialty of the program director's primary board certification for the purposes of subgroup analysis.
Survey Instrument
We created a web-based survey in order to rate program directors’ individual opinions of skills and knowledge topics that are essential for graduates to master by the end of hand surgery training. We asked respondents to rate items into one of three categories: essential, exposure needed, or unnecessary (Figure 1). Survey items included general areas of practice, specific knowledge topics, and specific procedures relevant to the practice of hand surgery. We included general areas of practice of conditions outside of the hand, including wrist, distal radius/ulna, mid/proximal forearm, elbow, upper arm/shoulder, clavicle/scapula, brachial plexus conditions, and microsurgery/free tissue transfer. The Surgery of the Hand and Upper Extremity (SHUE) Curriculum, developed as a model curriculum for the upcoming pilot two-year hand and upper extremity fellowship programs, was used to create the initial list of detailed knowledge topics and procedures. Components of the SHUE involving peripheral nerves and structures distal to the elbow were extracted for inclusion in the survey. The detailed components were organized into 18 thematic categories (Figure 2). We initially pilot tested the survey on four practicing hand surgeons to identify omitted and redundant items. The final survey included assessment of 9 general areas of practice, 97 knowledge topics, and 172 procedures.
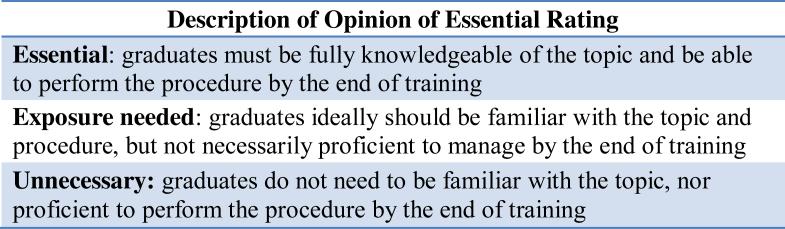
Figure 1.
Survey description provided to respondents to provide rating of essential nature of hand surgery training components.
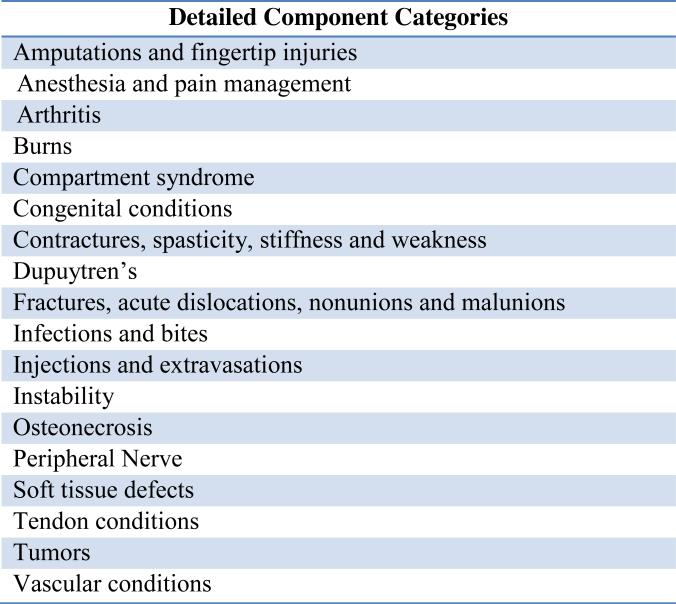
Figure 2.
Detailed components of survey divided into 18 thematic categories.
Data Analysis
Frequencies of responses were calculated for each item among all respondents and among respondents from plastic surgery and orthopedic surgery accredited programs for subgroup comparison. We did not perform a subgroup analysis of general surgery accredited programs because at the time of the survey, there was only 1 general surgery program. Fisher's exact tests were performed to test differences of each item rating among orthopedic and plastic surgery groups.
Scales of related survey items were created to determine differences in subgroup ratings based on anatomical or clinical themes. Scales for 27 clinical themes were created in total. Initially scales were created based on the organization of the survey into 18 themes, as outlined in Figure 2 (see Table, Supplemental Digital Content 1, which demonstrates the components included in the 18 mutually exclusive thematic scales). We created 9 additional scales for additional procedure types with themes overlapping the 18 primary survey categories (see Table, Supplemental Digital Content 2, which demonstrates the components included in the additional procedure type scales). Essential, exposure needed, and unnecessary ratings of reach item were assigned a numeric value of 1, 2, and 3 respectively. A numerical value of each scale was calculated for each respondent, which equaled the mean response of all items within the respective scale. A scale value less than 1.5 indicates that the majority of items within the scale were rated as essential, and a value greater than 1.5 indicates the majority of items within the scale were rated as exposure needed. The closer the mean scale response is to 1.0, the greater the number of items within the scale that were rated as essential. T-tests were performed to compare mean scale responses among plastic surgery and orthopedic surgery respondents. Cronbach alpha statistics, a measure of internal consistency of items within a scale, were calculated for each scale. A group of items with a Cronbach alpha greater than 0.7 are generally accepted as having good reliability of measuring a common theme (15). The higher the Cronbach alpha, the more related the responses of items are to one another.
RESULTS
We had a response rate of 84%, with 62 program directors responding to the survey. Survey participants included program directors from 49 orthopedic surgery, 12 plastic surgery, and 1 general surgery accredited program. Responses of the general surgery accredited program director were not included for subgroup analysis due to the sample size.
There were statistically significant differences in essential ratings of four general areas of practice between the plastic surgery and orthopedic surgery groups (Table 1). All of the orthopedic surgeons (100%; n=49) rated wrist conditions and distal radius/ulna conditions as essential, whereas 83% of plastic surgeons (n=10) rated these items as essential (p=0.036). There was a much larger difference of opinion of forearm and elbow conditions. Forearm conditions were rated as essential by 74% of orthopedic surgeons (n=36) and only 17% of plastic surgeons (n=2) (p<0.001). Elbow conditions were rated as essential by a minority of both groups. However, there was a significant difference in the frequency of orthopedic surgery program directors rating elbow conditions as essential (41%) compared to plastic surgery program directors (8%, p=0.044) (Table 1).
Table 1.
Frequency of Essential Rating of General Areas of Practice by Accreditation Type
| Component | ALL | ORTHO | PLASTICS | P |
|---|---|---|---|---|
| Wrist conditions | 96.8% | 100.0% | 83.3% | 0.036 |
| Distal radius and ulna conditions | 95.2% | 100.0% | 83.3% | 0.036 |
| Mid forearm and proximal forearm conditions | 61.3% | 73.5% | 16.7% | <0.001 |
| Elbow conditions | 33.9% | 40.8% | 8.3% | 0.044 |
| Upper arm and shoulder conditions | 8.1% | 10.2% | 0.0% | 0.573 |
| Clavicle and scapula conditions | 3.2% | 4.1% | 0.0% | 1.000 |
| Peripheral nerve conditions | 98.4% | 98.0% | 100.0% | 1.000 |
| Brachial plexus conditions | 29.0% | 28.6% | 33.3% | 0.736 |
| Microsurgery and free tissue transfer | 48.4% | 44.9% | 66.7% | 0.211 |
Response frequencies and Fisher's exact test statistics for subgroup comparisons of each detailed knowledge topic and procedure are outlined as Supplemental Digital Content (Table, Supplemental Digital Content 1). Items that were noted to have a significant difference in essential ratings between plastic surgery and orthopedic subgroups are outlined in Table 2. Only 4 detailed components (the knowledge topic of forearm fractures, ORIF of forearm fractures, limited intercarpal arthrodesis, and MCP/PIP joint implant arthroplasty) had a significantly higher frequency of essential rating among orthopedic surgeons compared to the plastic surgery group. However, 33 detailed items had significantly higher frequency of essential ratings among plastic surgeons compared to the orthopedic surgery subgroup (Table 2). General themes of items rated as essential more frequently among plastic surgeons include thumb and soft tissue reconstruction, burns, injection and extravasation injury, nerve reconstruction, and vascular repair.
Table 2.
Knowledge Topics and Procedures Favored Based on Program Type§
| Thematic Category | Orthopedics Favored | Plastics Favored |
|---|---|---|
| General Areas of Practice | - Wrist conditions** - Distal radius and ulna conditions** - Mid forearm and proximal forearm conditions - Elbow conditions* |
|
| Amputations and Fingertip Injuries | - Nail matrix lesions (pigmented and nonpigmented) - Ray amputation** - Thumb reconstruction with local and regional flaps** - Nail bed graft - Thumb reconstruction with bone graft and flap reconstruction - Thumb reconstruction with wrap around flap and distant flaps - Thumb reconstruction with toe transfer* |
|
| Arthritis | - Limited intercarpal arthrodesis (incl. radiocarpal, four-corner, STT, mid-carpal)** - MCP and PIP joint implant arthroplasty** |
- Thumb CMC arthrodesis** |
| Burns | - Thermal burns - Chemical burns - Frostbite (evaluation and rewarming) - Escharotomy - Burn debridement / excision - Burn reconstruction (incl. syndactyly / contracture release) |
|
| Dupuytren's | - Finger and palm fasciectomy and dermofasciectomy** | |
| Fractures, Acute Dislocations, Nonunions, Malunions | - Forearm fracture (incl. radius/Galeazzi, ulna/Monteggia, both bone fracture) - ORIF forearm fracture (incl. Galeazzi, Monteggia) |
- External fixation distal radius and ulna fracture (incl. intra/extra-articular)** |
| Infections and Bites | - Snake, spider, and other insect bites | |
| Injections and Extravasations | - Injection injuries (incl. oil-based, paint-based, water, air) - Extravasation injuries (incl. chemotherapeutics, anti-epileptics, saline) |
|
| Instability | - PIP collateral ligament repair and reconstruction | |
| Peripheral Nerve | - Major peripheral nerve reconstruction with autograft or cable grafts (incl. median, radial, ulnar nerves)** - Reconstruction of neuroma with restoration of nerve continuity** |
|
| Soft Tissue Defects | - Skin substitutes (incl. allografts and xenografts)** - Distant flaps (incl. groin, abdomen, chest)** - Neurovascular island flap |
|
| Tendon Conditions | - FCR tunnel release | |
| Tumors | - Skin and nail tumors** - Wide excision and reconstruction |
|
| Vascular Conditions | - Acute occlusive disease (incl. thrombus and embolus)** - Vascular malformations (incl. AVM, venous malformation, hemangioma, lymphatic malformation) - Vein graft artery and vein laceration (small and large size)** - Repair and excision large artery aneurysm - Excision vascular mass |
Items listed demonstrated statistically significant difference in frequency of essential rating between groups (P<0.05)
Item not rated essential by >50% from either group
Item rated essential by >50% from both groups
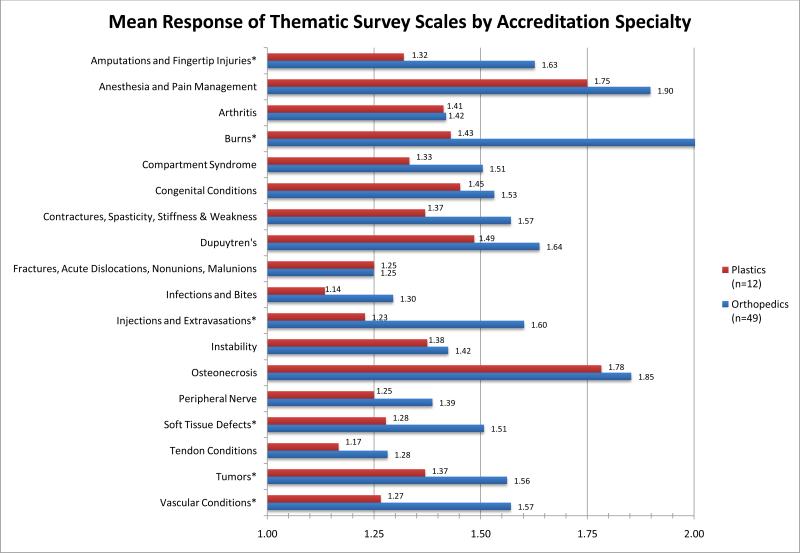
Summary statistics of the 27 survey scales, including the number of items included in each scale and Cronbach alpha statistics are outlined in Table 3. All scales had a Cronbach alpha of at least 0.7, which means that the scale items had good internal consistency. The mean responses for each scale among plastic and orthopedic surgery groups are displayed for the 18 thematic survey scales and 9 procedure-type scales in Figure 3 and Figure 4 respectively. There were significant differences in mean responses between the specialty groups in 11 of the 27 scales. Only one scale, forearm fractures, contained items with a stronger preference for essential rating among orthopedic surgery respondents compared to plastic surgery respondents. The other 10 scales with significant differences among specialty subgroups contained items with a higher preference for essential rating among plastic surgeons compared to orthopedic surgery respondents; the majority of these scales contained items related to soft tissue injury and reconstructive procedures (Figure 3 and Figure 4). The burn scale had the greatest discrepancy in opinion of essential ratings between plastic and orthopedic surgeons, followed by pedicled and free tissue transfer, and amputation and fingertip injuries (Figure 3 and Figure 4).
Table 3.
Summary Statistics of Survey Scales
| Thematic Survey Scales | # items | Cronbach α |
|---|---|---|
| Amputations and Fingertip Injuries | 19 | 0.90 |
| Anesthesia and Pain Management | 6 | 0.80 |
| Arthritis | 25 | 0.87 |
| Burns | 6 | 0.89 |
| Compartment Syndrome | 8 | 0.73 |
| Congenital Conditions | 21 | 0.95 |
| Contractures, Spasticity, Stiffness & Weakness | 9 | 0.84 |
| Dupuytren's | 11 | 0.80 |
| Fractures, Acute Dislocations, Nonunions, Malunions | 30 | 0.91 |
| Infections and Bites | 24 | 0.95 |
| Injections and Extravasations | 4 | 0.92 |
| Instability | 20 | 0.92 |
| Osteonecrosis | 15 | 0.89 |
| Peripheral Nerve | 19 | 0.83 |
| Soft Tissue Defects | 9 | 0.72 |
| Tendon Conditions | 15 | 0.83 |
| Tumors | 9 | 0.75 |
| Vascular Conditions | 16 | 0.92 |
| Procedure-Type Scales | # items | Cronbach α |
|---|---|---|
| All Microsurgical Procedures | 19 | 0.84 |
| Replantation Procedures | 3 | 0.85 |
| Microsurgical Nerve and Revascularization Procedures | 13 | 0.77 |
| Microsurgical Nerve Procedures | 8 | 0.70 |
| Microsurgical Revascularization Procedures | 5 | 0.81 |
| Pedicled and Free Tissue Transfer | 12 | 0.83 |
| All Forearm Procedures | 12 | 0.81 |
| Forearm Fractures | 5 | 0.83 |
| All Distal Radius Procedures | 26 | 0.87 |
| Distal Radius Fractures | 8 | 0.81 |
| All Wrist Procedures | 38 | 0.91 |
| Wrist Fractures | 5 | 0.76 |
Figure 3.
Mean scaled response of 18 thematic survey scales based on program accreditation type. Mean scale response of 1.0 indicates all items in the scale rated as essential; mean scale response of 2.0 indicates all items in scale rated as exposure needed.
* Indicates statistically significant difference (p<0.05) between plastic surgery and orthopedic surgery subgroup responses.
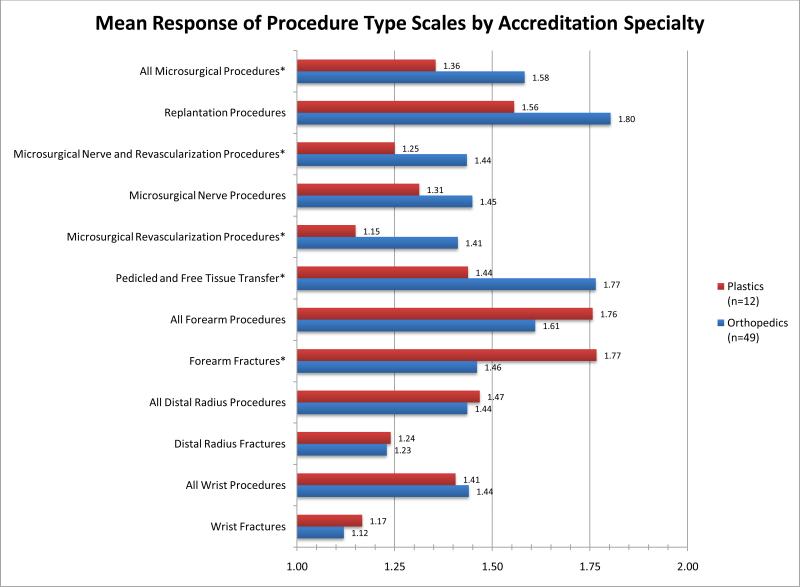
Figure 4.
Mean scaled response of 9 procedure-type scales based on program accreditation type. Mean scale response of 1.0 indicates all items in the scale rated as essential; mean scale response of 2.0 indicates all items in scale rated as exposure needed.
* Indicates statistically significant difference (p<0.05) between plastic surgery and orthopedic surgery subgroup responses.
The scale containing all microsurgical procedure items contained items more commonly rated as essential among plastic surgeons. When the procedures were further divided into subtypes, the preference for essential rating among plastic surgeons persisted when we examined only revascularization procedures. However, the mean scale response for microsurgical nerve procedures was not significantly different between the two groups. In addition, mean ratings for all procedures involving the forearm was not significantly different between the two groups, but when we examine only procedures and topics related to forearm fractures, there was a significantly greater tendency for orthopedic surgery respondents to rate forearm fracture items as essential.
DISCUSSION
We found that plastic and orthopedic surgery program directors have different opinions as to what is considered essential for hand surgery training, despite being united under the umbrella subspecialty of hand surgery. Program directors tend to emphasize the importance of knowledge topics and procedures that are often highlighted in their respective primary disciplines. Orthopedic surgeons favor inclusion of the elbow and more proximal structures in the essential practices of hand surgery compared to plastic surgery program directors. In addition, orthopedic surgeons more commonly rate forearm fracture procedures as being essential to hand surgery training. However, we found it interesting to note that there were no differences between the two groups in overall ratings of items related to distal radius conditions and wrist conditions. Both groups feel that the wrist is essential, and as the distal radius is intimately associated with the wrist, both groups again feel that distal radius fracture training should be a core component of the hand surgery training experience. Similarly, plastic surgeons more commonly favored components that are typically emphasized in plastic surgery residency training, such as burns, soft tissue reconstruction, and microsurgical procedures. It is not surprising for individual scope of practice to favor experiences gained in respective primary residency training. However, it is interesting to see that program directors, who ultimately have the greatest influence on fellowship curricula, still prioritize clinical areas emphasized by their respective accreditation specialty.
Over time, plastic surgeons are having less of a presence in hand surgery (16-18). Higgins et al. demonstrated that the proportion of plastic surgeons applying to hand surgery fellowship, the proportion of new plastic surgeons obtaining subspecialty certification, and the total proportion of actively practicing plastic surgeons holding subspecialty certification in hand surgery have all steadily declined (16). Based on differences in clinical emphasis in training between plastic and orthopedic surgery programs, this diminished presence of plastic surgeons in the field of hand surgery can have a great impact on patient care. Payatakes et al. performed a survey of American Society for Surgery of the Hand members to evaluate the practice of microsurgery among members. Practicing orthopedic surgery-trained hand surgeons predictably performed replantation and free tissue transfer much less frequently than plastic surgeons (19). However, 39% of respondents reported not performing replantation due to lack of confidence in microsurgical skills, 42% believed there is an additional need for surgeons willing to accept replantation cases, and 56% show a desire for continuous training programs to preserve microsurgical and other specialized skills (19). Such data highlight the effect that philosophical differences of training priorities can have on surgeons in practice.
Demonstrating differences in opinions based on accreditation specialty suggests the need to better define the essential skills that graduates are expected to master. Based on the data collected in this survey, trainees are getting a mixed picture as to what is essential to the practice of hand surgery depending on the training program. These differences highlight further challenges in fully achieving competency-based training. These data also promote the potential advantage that training programs have where fellows have exposure to both plastic and orthopedic surgery trained hand surgeons. Because differences of clinical emphasis may exist based on primary specialty, it would be ideal for fellows to have exposure to both perspectives. Ultimately training experiences, subspecialty certification, and essential skills to care for the needs of the common hand surgery patient population should all be interrelated. Most of the differences between plastic and orthopedic surgeon opinions were instances in which plastic surgeons more commonly rated the clinical component as essential compared to orthopedic surgeons. Thus, it is possible that one factor contributing to lower passage rates on the hand surgery certification exam among plastic surgeons (14) may be due to overemphasis of clinical areas that are not emphasized on the certification exam.
The largest limitation of the study was the lengthy nature of the survey. Program directors were asked to rate 278 items in total. However, due to the important nature of the survey, we still had a high response rate by more than 80% of the program directors. Analysis of group differences within a single item required very large differences in response frequencies in order to detect a statistical difference between the two groups due to the small number of plastic surgery program directors. The creation of scales of related items allowed us to have greater power in detecting differences in themes between the plastic and orthopedic surgery groups due to the limited sample size of plastic surgery program directors. In addition, creation of survey scales helped to make analysis of the responses to the large number of survey items more manageable. Lastly, due to the already present survey burden, we could not ask about detailed procedures involving the elbow and proximal structures. However, we can assume that these procedures would have been more heavily favored by the orthopedic surgery program directors based on the differences noted in the general areas of practice section of the survey, with orthopedic surgeons more commonly rating elbow and upper arm/shoulder conditions as essential.
Differences in clinical emphasis during hand surgery training based on the accreditation specialty highlights one of the many challenges in achieving competency-based training in hand surgery. Naturally programs should retain their individual clinical strengths. However, the general differences of components thought to be essential to hand surgery training between program directors of plastic and orthopedic surgery accredited programs demonstrate potential areas of clinical exposure in need of improvement for trainees.
Supplementary Material
Acknowledgements
Support for this study was provided by a grant from the American Foundation for Surgery of the Hand (to Dr. Kevin C. Chung), by a grant from the Robert Wood Johnson Foundation/Veterans Affairs (to Dr. Erika D. Sears), and by a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) (to Dr. Kevin C. Chung). We would like to thank all of the hand surgery fellowship program directors who kindly completed the lengthy survey in this study. Without their participation this study would not have been possible.
Footnotes
Disclosure:
None of the authors has a financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Accreditation Council for Graduate Medical Education [February 23, 2012];Common program requirements, effective. 2011 Jul 1; http://www.acgme.org/acWebsite/dutyhours/dh_dutyhourscommonpr07012007.pdf.
- 2.Accreditation Council for Graduate Medical Education [February 23, 2012];History of medical education accreditation. http://www.acgme.org/acWebsite/GME_info/historyGME.pdf.
- 3.Swing SR. The ACGME outcome project: retrospective and prospective. Med Teach. 2007;29:648–654. doi: 10.1080/01421590701392903. [DOI] [PubMed] [Google Scholar]
- 4.Bell RH. National curricula, certification and credentialing. Surgeon. 2011;9(Suppl 1):S10–S11. doi: 10.1016/j.surge.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 5.Davis Sears E, Larson BP, Chung KC. A national survey of program director opinions of core competencies and structure of hand surgery fellowship training. J Hand Surg Am. 2012 Jun; doi: 10.1016/j.jhsa.2012.06.034. In Press. [DOI] [PubMed] [Google Scholar]
- 6.Sachdeva AK, Bell RH, Jr., Britt LD, et al. National efforts to reform residency education in surgery. Acad Med. 2007;82:1200–1210. doi: 10.1097/ACM.0b013e318159e052. [DOI] [PubMed] [Google Scholar]
- 7.Bell RH, Jr., Biester TW, Tabuenca A, et al. Operative experience of residents in US general surgery programs: a gap between expectation and experience. Ann Surg. 2009;249:719–724. doi: 10.1097/SLA.0b013e3181a38e59. [DOI] [PubMed] [Google Scholar]
- 8.Valani RA, Yanchar N, Grant V, et al. The development of a national pediatric trauma curriculum. Med Teach. 2010;32:e115–119. doi: 10.3109/01421590903398240. [DOI] [PubMed] [Google Scholar]
- 9.Carr MM. Program directors' opinions about surgical competency in otolaryngology residents. Laryngoscope. 2005;115:1208–1211. doi: 10.1097/01.MLG.0000163101.12933.74. [DOI] [PubMed] [Google Scholar]
- 10.Wadey VM, Halpern J, Bouchard J, et al. Orthopaedic surgery core curriculum: the spine. Postgrad Med J. 2007;83:268–272. doi: 10.1136/pgmj.2006.053900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wadey VM, Dev P, Buckley R, et al. Competencies for a Canadian orthopaedic surgery core curriculum. J Bone Joint Surg Br. 2009;91:1618–1622. doi: 10.1302/0301-620X.91B12.22542. [DOI] [PubMed] [Google Scholar]
- 12.ASSH [February 24, 2012];Executive summary of initiative to enhance hand and upper extremity education. 2010 Jul; http://www.assh.org/Members/GetInvolved/HandEducation/Documents/Executive_Summary_FINAL%20(July%202010).pdf.
- 13.ASSH [February 24, 2012];Patient care curriculum: Hand surgery, version 1.2. 2010 Oct; http://www.assh.org/Members/GetInvolved/HandEducation/Documents/Patient%20Care%20Curriculum%201.2%20(10-2010).pdf.
- 14.Stern PJ. Subspecialty certification in hand surgery. Clin Orthop Relat Res. 2006;449:165–168. doi: 10.1097/01.blo.0000224041.77215.b6. [DOI] [PubMed] [Google Scholar]
- 15.Bland JM, Altman DG. Cronbach's alpha. BMJ. 1997;314:572. doi: 10.1136/bmj.314.7080.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Higgins JP. The diminishing presence of plastic surgeons in hand surgery: a critical analysis. Plast Reconstr Surg. 2010;125:248–260. doi: 10.1097/PRS.0b013e3181c496a2c. [DOI] [PubMed] [Google Scholar]
- 17.Chang J, Hentz VR, Chase RA. Plastic surgeons in American hand surgery: the past, present, and future. Plast Reconstr Surg. 2000;106:406–412. doi: 10.1097/00006534-200008000-00025. [DOI] [PubMed] [Google Scholar]
- 18.Szabo RM. What is our identity? What is our destiny? J Hand Surg Am. 2010;35:1925–1937. doi: 10.1016/j.jhsa.2010.09.025. [DOI] [PubMed] [Google Scholar]
- 19.Payatakes AH, Zagoreos NP, Fedorcik GG, et al. Current practice of microsurgery by members of the American Society for Surgery of the Hand. J Hand Surg Am. 2007;32:541–547. doi: 10.1016/j.jhsa.2006.12.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.