Abstract
Background
The benefit of utilizing an invasive strategy in elderly Chinese patients with non-ST-elevation myocardial infarction (NSTEMI) remains unclear. The aim of this study was to determine whether in-hospital revascularization is associated with long-term prognosis in elderly Chinese patients with NSTEMI, as compared with younger patients.
Methods
All patients were followed up for at least 3 years or until the occurrence of a major event. The primary endpoint was all-cause mortality, and the secondary endpoint was the combined occurrence of major adverse cardiovascular events (MACE), including death, nonfatal MI, and ischemic stroke.
Results
A total of 343 consecutive NSTEMI patients (148 over the age of 75 years and 195 aged < 75 years) were enrolled. Coronary angiography was performed less frequently in elderly patients (66% vs. 76%; p = 0.027). Multiple logistic regression analysis confirmed the benefit of in-hospital revascularization in the elderly and younger patients, with a statistically significant reduction in the odds of all-cause death and MACE at 1 year and 3 years, respectively. In a multivariable Cox regression analysis, in-hospital revascularization was an independent predictor of future MACE not only in elderly patients [hazard ratio (HR), 0.61; 95% confidence interval (CI), 0.38-0.97] but also in younger patients as well (HR, 0.51; 95% CI, 0.31-0.84).
Conclusions
In Chinese patients with NSTEMI, in-hospital revascularization was associated with significant benefits at 1 year and 3 years in both younger and elderly groups. These results are consistent with the published literature and suggest that advanced age alone should not be regarded as a contraindication to invasive management following presentation with NSTEMI.
Keywords: Elderly, Invasive strategy, Myocardial infarction
INTRODUCTION
Managing patients with non-ST-segment elevation acute coronary syndrome (NSTE-ACS) has evolved rapidly with the development of new care strategies in recent years. In patients who are regarded as high risk, guidelines1,2 emphasize intensive and early interventional therapy, including routine use of coronary angiography and subsequent revascularization. Elderly patients, who are frequently underrepresented in randomized trials of ACS relative to their disease prevalence,3 constitute an increasing proportion of patients with NSTE-ACS. In a previously published Italian registry of patients with NSTE-ACS, more than 35% of the patients were 75 years of age or older.4 Compared with younger patients, elderly patients have a greater extent of coronary artery disease and a higher rate of comorbid conditions, and are more likely to suffer complications after revascularization procedures.4,5 Accumulated evidence has demonstrated that advanced age is an independent risk factor for early mortality and (re)infarction in patients presenting with NSTE-ACS.6
In addition, elderly patients are less likely to undergo revascularization therapies and to receive optimal evidence-based medications than younger patients, emphasizing the growing importance of investigating therapeutic modalities in elderly patients with NSTE-ACS.7-10 Subgroup analysis of a previously published randomized control trial suggests that elderly patients with NSTE-ACS have better ischemic outcomes when they undergo routine early invasive strategy compared with those managed conservatively.11 However, patients with severe comorbid conditions or other serious systemic illness were excluded, and the benefit of invasive strategy in elderly Chinese patients with non-ST-segment elevation myocardial infarction (NSTEMI) has not been carefully studied. The aim of this study was to determine whether in-hospital revascularization is associated with long-term prognosis in elderly Chinese patients with NSTEMI, as compared with younger patients.
METHODS
Study population
This was a retrospective study of consecutive patients with NSTEMI admitted to a coronary care unit (CCU) in the Cardiology Division at Taipei Veterans General Hospital between May 2002 and December 2005. NSTEMI was defined as detection of a rise of cardiac troponin I, accompanied by either ischemic symptoms or electrocardiographic changes (including ischemic ST-segment depression or T-wave inversion or even “normal” results). Elevated cardiac troponin I was defined as a measurement exceeding the 99th percentile of the upper reference limit. Before enrollment, a detailed review of each patient’s chart was conducted to gather data on symptoms, medications, coronary risk factors, earlier cardiac events, smoking status, and other systemic diseases. Hypertension was defined as a systolic blood pressure ≥ 140 mmHg, a diastolic blood pressure ≥ 90 mmHg, or use of antihypertensive treatment. Diabetes mellitus was defined according to World Health Organization criteria.12 Hypercholesterolemia was defined as serum cholesterol ≥ 200 mg/dL or being medicated with lipid-lowering drugs. Serum creatinine > 2 mg/dl was classified as renal insufficiency. Smokers were classified as former only if they had not smoked for more than 6 months. Patients who died early (within 24 h) were excluded. To reduce patient selection bias, there were no other specific exclusion criteria. The study was approved by the local research ethics committee.
Risk score calculation
The Global Registry of Acute Coronary Events (GRACE) risk sore13 was calculated from the initial clinical history, electrocardiogram, and laboratory values collected upon admission. Although the present study was retrospective, all data were collected completely and entered into a computer database.
Intervention strategies
A diseased vessel was defined as a major epicardial artery with at least 50% stenosis. Revascularization was recommended for all patients with ≥ 70% diameter obstruction in any artery supplying a significant proportion of the myocardium. Percutaneous coronary intervention was recommended if there were 1 or 2 target lesions; otherwise, coronary artery bypass grafting (CABG) was preferred in patients with 3-vessel or left main coronary artery disease (CAD).
Clinical follow-up for endpoints
All patients included were followed up for at least 3 years or until the occurrence of a major event. The primary endpoint was all-cause mortality. The secondary endpoint was the combined occurrence of major adverse cardiovascular events (MACE), including death, nonfatal MI, and ischemic stroke. We contacted all patients by telephone and followed up their medical records retrospectively. Nonfatal MI was defined by a rise of cardiac troponin I with ischemic symptoms and/or characteristic electrocardiographic changes. Ischemic stroke was defined as the presence of a new neurological deficit lasting for at least 24 h with definite evidence of a cerebrovascular accident verified by either magnetic resonance imaging or computed tomography. The endpoint was analyzed at discharge, 1 year, and 3 years.
Statistical analysis
Data were expressed as the mean ± standard deviation for numeric variables and as the number (percent) for categorical variables. Comparisons of continuous variables between groups were performed by Student’s t-test. Subgroup comparisons of categorical variables were assessed by a Chi-square or Fisher’s exact test. Survival curves were generated by the Kaplan-Meier method and survival among groups was compared by use of the log-rank test. Multiple logistic regression analysis was used to evaluate the effect of in-hospital revascularization on in-hospital and long-term outcomes, and to assess the interaction between age group and invasive strategy. Multivariable Cox regression analysis was performed to determine the independent effect of invasive strategy on long-term outcomes in elderly patients. The variables included in the multivariable model were age, sex, medical history (hypertension, diabetes, hypercholesterolemia, and current smoker), in-hospital revascularization, GRACE risk score, and medications (angiotensin-converting enzyme inhibitors, β-blockers, and statins). Data were analyzed using SPSS software (version 17, SPSS, Chicago, Illinois, USA). A p value of < 0.05 was considered to indicate statistical significance.
RESULTS
Patient characteristics
A total of 343 consecutive patients (239 males, 70%) were enrolled in this study. There were 148 (43%) patients over the age of 75 years and 195 (57%) aged < 75 years. The baseline characteristics of the two groups are shown in Table 1. Systemic hypertension, Killip class > 1, and higher GRACE score were more often present in elderly patients. Moreover, angiotensin-converting enzyme inhibitors and calcium-channel blockers were used more frequently in elderly patients. However, elderly patients less often were current smokers and with hypercholesterolemia compared with younger patients.
Table 1. Baseline characteristics of NSTEMI patients in younger and elderly group.
| < 75 years (n = 195) | ≥ 75 years (n = 148) | p value | |
| Age (years) | 63.0 ± 9.7 | 79.5 ± 4.2 | < 0.001 |
| Male | 135 (69.2%) | 104 (70.3%) | 0.836 |
| Current smoker | 74 (37.9%) | 40 (27.0%) | 0.033 |
| Hypertension | 139 (71.3%) | 120 (81.1%) | 0.037 |
| Diabetes mellitus | 97 (49.7%) | 60 (40.5%) | 0.09 |
| Hypercholesterolemia | 49 (25.1%) | 24 (16.2%) | 0.046 |
| Renal insufficiency | 52 (26.7%) | 37 (25.0%) | 0.727 |
| Previous MI | 31 (15.9%) | 22 (14.9%) | 0.793 |
| Previous stroke/TIA | 32 (16.4%) | 28 (18.9%) | 0.545 |
| Prior PCI/CABG | 37 (19.0%) | 40 (27.0%) | 0.077 |
| SBP (mmHg) | 133 ± 30 | 137 ± 32 | 0.243 |
| DBP (mmHg) | 75 ± 18 | 74 ± 17 | 0.681 |
| GRACE score | 153.4 ± 50.0 | 191.2 ± 41.2 | < 0.001 |
| Killip classification | < 0.001 | ||
| Killip = 1 | 123 (63.1%) | 65 (43.9%) | |
| Killip > 1 | 72 (36.9%) | 83 (56.1%) | |
| Medication use at discharge | |||
| Antiplatelet agent | 194 (99.5%) | 146 (98.6%) | 0.58 |
| β-blocker | 74 (37.9%) | 56 (37.8%) | 0.983 |
| Calcium channel blocker | 64 (32.8%) | 69 (46.6%) | 0.009 |
| ACE inhibitor | 48 (24.6%) | 61 (41.2%) | 0.001 |
| A II receptor blocker | 34 (17.4%) | 22 (14.9%) | 0.523 |
| Statin | 51 (26.2%) | 33 (22.3%) | 0.411 |
Values are mean ± SD or number (%).
ACE, angiotensin-converting enzyme; A II, angiotensin II; CABG, coronary artery bypass grafting; DBP, diastolic blood pressure; MI, myocardial infarction; NSTEMI, non-ST-elevation myocardial infarction; PCI, percutaneous coronary intervention; SBP, systolic blood pressure; TIA, transient ischemic attack.
Angiographic and procedural characteristics
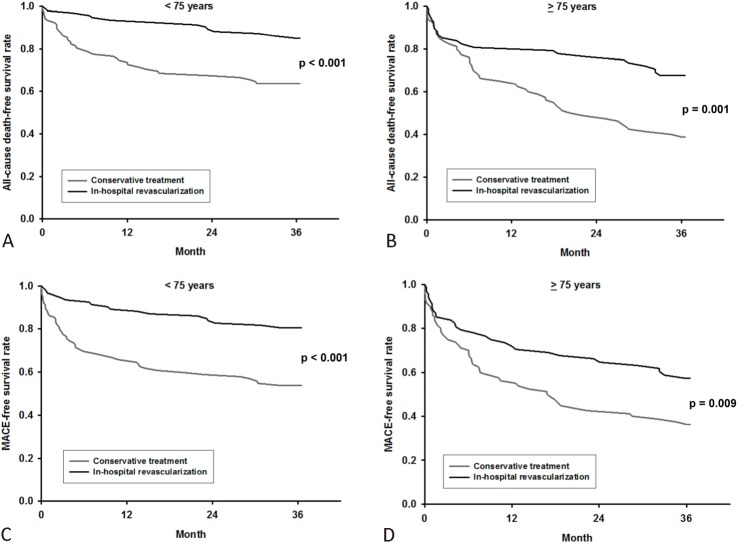
Coronary angiography was globally performed in 246 patients, 97 (66%) in the elderly group and 149 (76%) in the younger group. As shown in Table 2, coronary angiography was less frequently undertaken in patients with higher GRACE score and Killip class > 1, whether in the elderly or younger groups. Moreover, younger patients with lower peak creatine kinase level were less likely to undergo coronary angiography. There was a greater extent of CAD in the elderly than in younger patients (chi-square for linear trend, p = 0.011), as illustrated in Figure 1. Revascularization procedures were performed in 68 (46%) elderly patients and in 93 (48%) younger patients with no difference between the groups in the technique, percutaneous or surgical, that was applied.
Table 2. Baseline characteristics of NSTEMI patients undergoing or not undergoing angiography in younger and elderly group.
| < 75 years | ≥ 75 years | ||||||
| Angiography (n = 149) | No angiography (n = 46) | p value | Angiography (n = 97) | No angiography (n = 51) | p value | ||
| Male | 104 (69.8%) | 31 (67.4%) | 0.757 | 74 (76.3%) | 30 (58.8%) | 0.027 | |
| Current smoker | 60 (40.3%) | 14 (30.4%) | 0.23 | 30 (30.9%) | 10 (19.6%) | 0.141 | |
| Hypertension | 103 (69.1%) | 36 (78.3%) | 0.231 | 80 (82.5%) | 40 (78.4%) | 0.551 | |
| Diabetes mellitus | 72 (48.3%) | 25 (54.3%) | 0.475 | 38 (39.2%) | 22 (43.1%) | 0.641 | |
| Hypercholesterolemia | 40 (26.8%) | 9 (19.6%) | 0.32 | 18 (18.6%) | 6 (11.8%) | 0.287 | |
| Renal insufficiency | 35 (23.5%) | 17 (37.0%) | 0.071 | 24 (24.7%) | 13 (25.5%) | 0.92 | |
| Previous MI | 24 (16.1%) | 7 (15.2%) | 0.885 | 17 (17.5%) | 5 (9.8%) | 0.209 | |
| Previous stroke/TIA | 19 (12.8%) | 13 (28.3%) | 0.013 | 16 (16.5%) | 12 (23.5%) | 0.299 | |
| Prior PCI/CABG | 31 (20.8%) | 6 (13.0%) | 0.241 | 30 (30.9%) | 10 (19.6%) | 0.141 | |
| SBP (mmHg) | 132 ± 29 | 137 ± 33 | 0.376 | 136 ± 33 | 139 ± 31 | 0.629 | |
| DBP (mmHg) | 74 ± 17 | 78 ± 21 | 0.247 | 74 ± 18 | 74 ± 14 | 0.929 | |
| Peak creatine kinase (U/L) | 629 ± 742 | 397 ± 340 | 0.043 | 669 ± 905 | 547 ± 536 | 0.303 | |
| GRACE score | 148.8 ± 52.1 | 168.4 ± 39.2 | 0.008 | 186.2 ± 38.7 | 200.8 ± 44.6 | 0.040 | |
| Killip > 1 | 49 (32.9%) | 23 (50.0%) | 0.036 | 48 (49.5%) | 35 (68.6%) | 0.026 |
Values are mean ± SD or number (%).
CABG, coronary artery bypass grafting; DBP, diastolic blood pressure; MI, myocardial infarction; PCI, percutaneous coronary intervention; SBP, systolic blood pressure; TIA, transient ischemic attack.
Figure 1.
Extent of coronary artery disease was greater in elderly than in younger patients.
Early and late clinical outcomes
All study subjects were followed up until July 2009. The incidence of in-hospital mortality was not significantly different between elderly and younger patients, as well as the combined triple endpoint. At 1 year, all-cause death and MACE were significantly more common among elderly than among younger patients (27.7% vs. 17.4%, p = 0.023 and 36.5% vs. 23.1%, p = 0.007, respectively). At 3 years, overall mortality and MACE were still significantly more common among elderly than among younger patients (48.0% vs. 26.2%, p < 0.001 and 54.1% vs. 33.8%, p < 0.001, respectively), as shown in Table 3. After adjustment for age, sex, medical history (hypertension, diabetes, hypercholesterolemia, current smoker), in-hospital revascularization, GRACE risk score, and medications (angiotensin-converting enzyme inhibitors, β-blockers, statins), the long-term clinical outcomes also were statistically different between elderly and younger patients.
Table 3. In-hospital and long-term clinical outcomes of NSTEMI patients.
| < 75 years (n = 195) | ≥ 75 years (n = 148) | p value | Adjusted* OR (95% CI) | |
| All-cause mortality | ||||
| In-hospital | 12 (6.2%) | 15 (10.1%) | 0.175 | 1.75 (0.74-4.14) |
| One-year | 34 (17.4%) | 41 (27.7%) | 0.023 | 1.74 (0.98-3.11) |
| Three-year | 51 (26.2%) | 71 (48.0%) | < 0.001 | 2.45 (1.46-4.11) |
| MACE (death/MI/stroke) | ||||
| In-hospital | 17 (8.7%) | 18 (12.2%) | 0.297 | 1.34 (0.63-2.84) |
| One-year | 45 (23.1%) | 54 (36.5%) | 0.007 | 1.77 (1.05-3.00) |
| Three-year | 66 (33.8%) | 80 (54.1%) | < 0.001 | 2.04 (1.24-3.35) |
Values are number (%).
* Adjusted for age, sex, medical history (hypertension, diabetes mellitus, hypercholesterolemia, current smoker), in-hospital revascularization, GRACE risk score, and medications (angiotensin-converting enzyme inhibitors, β-blockers, statins).
Impact of in-hospital revascularization on outcomes
In order to evaluate the association of in-hospital revascularization with clinical outcomes, and to assess the interaction between age group and invasive strategy, multiple logistic regression analysis was performed. In elderly patients, in-hospital revascularization was not significantly associated with all-cause death and the composite endpoint during index admission. However, at 1 year, compared with the conservative strategy, the odds ratio (OR) for death with an invasive strategy was 0.43 [95% confidence interval (CI), 0.19-0.98], and the OR for composite endpoint was 0.42 (95% CI, 0.19-0.91), as shown in Table 4. Elderly patients undergoing in-hospital revascularization were associated with a substantial 73% and 59% significant decrease in the odds of death and composite endpoint at 3 years, which resulted in OR (95% CI) of 0.27 (0.12 to 0.58) and 0.41 (0.20 to 0.85), respectively. In younger patients, in-hospital revascularization was associated with significantly lower odds of death and composite endpoint throughout the 3 year follow-up period. Multiple logistic regression analysis confirmed the benefit of in-hospital revascularization in elderly and younger patients, with statistically significant reductions not only in all-cause mortality alone but also in the incidence of MACE at 1 year and 3 years. This benefit remained evident after testing for the interaction between age group and invasive strategy (Table 4).
Table 4. Age-specific results from multiple logistic regression* to evaluate the effect of invasive strategy on in-hospital and long-term outcomes.
| < 75 years | ≥ 75 years | Interaction† | |||||
| OR | 95% CI | p value | OR | 95% CI | p value | p value | |
| All-cause mortality | |||||||
| In-hospital | 0.204 | 0.041-0.991 | 0.048 | 1.096 | 0.351-3.416 | 0.875 | 0.077 |
| One-year | 0.168 | 0.061-0.463 | 0.001 | 0.429 | 0.188-0.977 | 0.044 | 0.201 |
| Three-year | 0.323 | 0.150-0.695 | 0.004 | 0.267 | 0.123-0.578 | 0.001 | 0.81 |
| MACE (death/MI/stroke) | |||||||
| In-hospital | 0.212 | 0.056-0.800 | 0.022 | 1.049 | 0.361-3.046 | 0.93 | 0.072 |
| One-year | 0.236 | 0.103-0.543 | 0.001 | 0.416 | 0.191-0.907 | 0.028 | 0.273 |
| Three-year | 0.327 | 0.158-0.676 | 0.003 | 0.407 | 0.195-0.851 | 0.017 | 0.578 |
* Adjusted for age, sex, medical history (hypertension, diabetes mellitus, hypercholesterolemia, and current smoker), GRACE risk score, and medications (angiotensin-converting enzyme inhibitors, β-blockers, statins).
† Testing the interaction between age group and invasive treatment.
In order to investigate the independent predictors of MACE in elderly and younger patients, multivariable Cox regression analysis was performed. As shown in Table 5, in-hospital revascularization was an independent predictor of future MACE not only in the elderly [hazard ratio (HR), 0.61; 95% CI, 0.38-0.97], but also in the younger patients (HR, 0.51; 95% CI, 0.31-0.84).
Table 5. Multivariate Cox regression analysis* to investigate the independent predictors of MACE.
| < 75 years | ≥ 75 years | |||||
| HR | 95% CI | p value | HR | 95% CI | p value | |
| GRACE score | 1.012 | 1.006-1.018 | < 0.001 | 1.007 | 1.002-1.013 | 0.013 |
| In-hospital revascularization | 0.513 | 0.314-0.839 | 0.008 | 0.61 | 0.384-0.967 | 0.036 |
| Diabetes mellitus | 1.893 | 1.138-3.149 | 0.014 | NS |
* Adjusted for age, sex, medical history (hypertension, diabetes mellitus, hypercholesterolemia, and current smoker), in-hospital revascularization, GRACE risk score, and medications (angiotensin-converting enzyme inhibitors, β-blockers, statins).
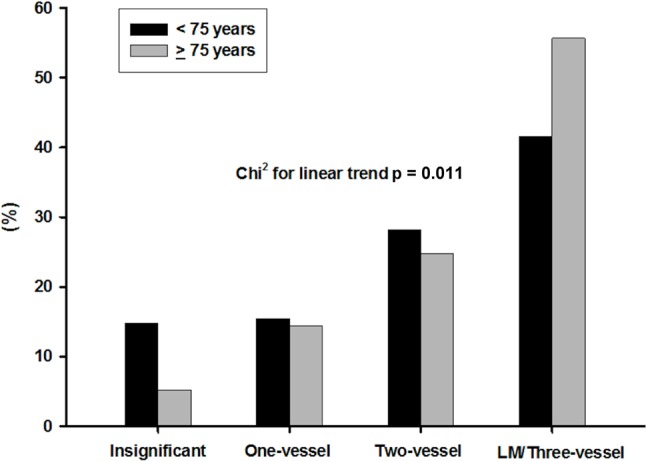
Prognostic significance of in-hospital revascularization
In order to determine the relationship between survival free of adverse events and in-hospital revascularization, Kaplan-Meier survival analysis was performed. Elderly patients who received invasive strategy had significantly higher all-cause death-free and MACE-free survival rates (p = 0.001). In addition, significantly higher all-cause death-free and MACE-free survival rates were also found in younger patients who received revascularization (p < 0.001), as illustrated in Figure 2.
Figure 2.
The all-cause death-free survival rate in (A) younger and (B) elderly patients in relation to treatment strategy; the MACE-free survival rate in (C) younger and (D) elderly patients in relation to treatment strategy.
DISCUSSION
The major findings of the present study indicated that in a cohort of Chinese patients with NSTEMI, in-hospital revascularization was associated with significantly lower odds of death and MACE at 1 year and 3 years, respectively. This benefit remained evident after testing for the interaction between age group and invasive strategy. These findings suggest that advanced age should not be regarded as a contraindication to invasive management in elderly Chinese patients with NSTEMI.
Previous studies have demonstrated that advanced age is an independent risk factor for early mortality and (re)infarction in patients presenting with NSTE-ACS.6 The rates of in-hospital death and 1-year mortality increased with increasing age.14 The progressive death rate with advancing age is higher in community populations than in clinical trials. Comorbidity is more prevalent among registry patients than like-aged trial patients.15 Coexisting conditions such as cerebral disease, renal failure, and chronic obstructive pulmonary disease may lead to higher mortality rates over time. Nonetheless, the incidence of death at 1 year after NSTE-ACS for patients over the age of 75 years is 1 in 5, and for those over the age of 85 years, it is more than 1 in 4.16 Compared to previous studies, our results showed a higher mortality rate of 27.7% at 1 year for elderly Chinese patients. The higher risk profile of our population (our patients tended to have a higher prevalence of diabetes and hyper-tension, and be more likely to present with positive troponin I on admission) may be a reason for the higher death rate observed.
In the FRISC II (Fragmin and Fast Revascularization during Instability in Coronary Artery Disease)17 and RITA-3 (Randomized Trial of a Conservative Treatment Strategy Versus an Interventional Treatment Strategy in Patients with Unstable Angina)18 trials, there was a clear benefit with a routine invasive strategy in men but not in women. However, a recent meta-analysis of eight ACS trials19 (3,075 women and 7,075 men) suggested that both men and high-risk women, defined by elevated biomarkers of necrosis, have a favorable outcome (reducing the odds of death, MI, or rehospitalization with ACS) from an invasive strategy in NSTE-ACS. Our previous study20 also showed that in-hospital revascularization has a benefit in men and high-risk women for reducing the all-cause death at 1 and 3 years. Although there was a high proportion of males (70%) in both age groups in the present study, in-hospital revascularization was still associated with a significant mortality benefit in elderly Chinese patients with NSTEMI, even after sex was taken into account in the multivariable analysis.
Previously, a subgroup analysis of the TACTICS-TIMI (Treat Angina with Aggrastat and Determine Cost of Therapy with an Invasive or Conservative Strategy — Thrombolysis in Myocardial Infarction) 18 trial,11 where patients hospitalized with unstable angina and NSTEMI were randomly assigned to an early interventional or conservative ischemia-guided procedure, showed that the invasive strategy conferred a significant reduction of nonfatal MI and MACE at 6 months (10.8% vs. 21.6%) among elderly patients. Liistro et al.8 also reported an early invasive strategy is feasible and leads to coronary revascularization in the majority of unselected elderly patients presenting with NSTE-ACS, resulting in encouraging immediate and 1-year clinical results. Recently, from the German acute coronary syndromes (ACOS) registry, Bauer et al.21 reported an invasive strategy is associated with an improved in-hospital (OR 0.55, 95% CI 0.35-0.86) and 1-year outcome (OR 0.56, 95% CI 0.38-0.81) in elderly patients with NSTEMI. In addition, a large, contemporary, real-life study22 highlights a significant mortality benefit — after adjustment for variables, which importantly included in-hospital events — was associated with an invasive approach at 6 months in elderly patients with high-risk NSTE-ACS. In our study, 19.6% of elderly patients with coronary angiography underwent coronary artery bypass grafting (CABG) during index hospitalization. Among patients with invasive strategy, due to the peri-operative risk and selection bias, the incidence of hospital death and MACE was highest in the CABG-patients. This may be a reason why invasive strategy was not beneficial for in-hospital outcome in our study, compared to previous study done by Bauer et al (9.8%). However, our data are consistent with the published literature and demonstrate that in elderly Chinese patients presenting with NSTEMI, in-hospital revascularization was associated with a substantial 58% and 59% significant decrease in the odds of composite endpoint at 1 year and 3 years, which resulted in OR (95% CI) of 0.42 (0.19 to 0.91) and 0.41 (0.20 to 0.85), respectively.
Study limitations
There are some limitations that should be considered in this study. First, the study population was relatively small, and the numbers are not powered enough to draw final conclusions. Further studies in a larger number of Asian ethnic patients are required to confirm our findings. Second, many confounding variables, such as age, sex, medical history (hypertension, diabetes, hypercholesterolemia, current smoker), GRACE risk score, and medications (angiotensin-converting enzyme inhibitors, β-blockers, statins), were demonstrated to influence the occurrence of cardiovascular events. However, after these variables were adjusted, in-hospital revascularization was still associated with a significant mortality benefit in elderly Chinese patients with NSTEMI. Third, as a non-randomized observational study, there are some inherent limitations and potential biases including unknown or unmeasured confounders, so a cause-and-effect relationship should not be inferred. This relates in particular to our inability to report why angiography was less undertaken in high-risk patients, which must be kept in mind when interpreting the study results. Our findings should be regarded as hypothesis-generating, requiring confirmation in further studies.
CONCLUSIONS
In Chinese patients with NSTEMI, the long-term mortality and MACE were higher in elderly than in younger patients. In-hospital revascularization has a benefit for reducing the all-cause death and MACE at 1 year and 3 years in both groups. These results are consistent with the published literature and suggest that advanced age alone should not be regarded as a contraindication to invasive management following presentation with NSTEMI.
CONFLICT OF INTEREST
None declared.
REFERENCES
- 1.Bassand JP, Hamm CW, Ardissino D, et al. Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes:the Task Force for Diagnosis and Treatment of Non-ST-Segment Elevation Acute Coronary Syndromes of European Society of Cardiology. Eur Heart J. 2007;28:1598–1660. doi: 10.1093/eurheartj/ehm161. [DOI] [PubMed] [Google Scholar]
- 2.Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians,the Society for Cardiovascular Angiography and Interventions,and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Circulation. 2007;116:e148–e304. doi: 10.1161/CIRCULATIONAHA.107.181940. [DOI] [PubMed] [Google Scholar]
- 3.Lee PY, Alexander KP, Hammill BG, et al. Representation of elderly persons and women in published randomized trials of acute coronary syndromes. JAMA. 2001;286:708–713. doi: 10.1001/jama.286.6.708. [DOI] [PubMed] [Google Scholar]
- 4.De Servi S, Cavallini C, Dellavalle A, et al. Non-ST-Elevation acute coronary syndrome in the elderly: treatment strategies and 30-day outcome. Am Heart J. 2004;147:830–836. doi: 10.1016/j.ahj.2003.12.016. [DOI] [PubMed] [Google Scholar]
- 5.Yusuf S, Flather M, Pogue J, et al. Variations between countries in invasive cardiac procedures and outcomes in patients with suspected unstable angina or myocardial infarction without initial ST elevation. OASIS (Organisation to Assess Strategies for Ischaemic Syndromes) Registry Investigators. Lancet. 1998;352:507–514. doi: 10.1016/s0140-6736(97)11162-x. [DOI] [PubMed] [Google Scholar]
- 6.Hasdai D, Holmes DR, Jr., Criger DA, et al. Age and outcome after acute coronary syndromes without persistent ST-segment elevation. Am Heart J. 2000;139:858–866. doi: 10.1016/s0002-8703(00)90018-8. [DOI] [PubMed] [Google Scholar]
- 7.Alexander KP, Roe MT, Chen AY, et al. Evolution in cardiovascular care for elderly patients with non-ST-segment elevation acute coronary syndromes. J Am Coll Cardiol. 2005;46:1479–1487. doi: 10.1016/j.jacc.2005.05.084. [DOI] [PubMed] [Google Scholar]
- 8.Liistro F, Angioli P, Falsino G, et al. Early invasive strategy in elderly patients with non-ST elevation acute coronary syndrome: comparison with younger patients regarding 30 day and long term outcome. Heart. 2005;91:1284–1288. doi: 10.1136/hrt.2004.051607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosengren A, Wallentin L, Simoons M, et al. Age,clinical presentation, and outcome of acute coronary syndromes in the Euroheart acute coronary syndrome survey. Eur Heart J. 2006;27:789–795. doi: 10.1093/eurheartj/ehi774. [DOI] [PubMed] [Google Scholar]
- 10.Yan RT, Yan AT, Tan M, et al. Age-related differences in the management and outcome of patients with acute coronary syndromes. Am Heart J. 2006;151:352–359. doi: 10.1016/j.ahj.2005.03.039. [DOI] [PubMed] [Google Scholar]
- 11.Bach RG, Cannon CP, Weintraub WS, et al. The effect of routine, early invasive management on outcome for elderly patients with non-ST-segment elevation acute coronary syndromes. Ann Intern Med. 2004;141:186–195. doi: 10.7326/0003-4819-141-3-200408030-00007. [DOI] [PubMed] [Google Scholar]
- 12.Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003;26:5–20. doi: 10.2337/diacare.20.7.1183. [DOI] [PubMed] [Google Scholar]
- 13.Granger CB, Goldberg RJ, Dabbous O, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003;163:2345–2353. doi: 10.1001/archinte.163.19.2345. [DOI] [PubMed] [Google Scholar]
- 14.Bagnall AJ, Goodman SG, Fox KA, et al. Influence of age on use of cardiac catheterization and associated outcomes in patients with non-ST-elevation acute coronary syndromes. Am J Cardiol. 2009;103:1530–1536. doi: 10.1016/j.amjcard.2009.01.369. [DOI] [PubMed] [Google Scholar]
- 15.Steg PG, Lopez-Sendon J, Lopez de Sa E, et al. External validity of clinical trials in acute myocardial infarction. Arch Intern Med. 2007;167:68–73. doi: 10.1001/archinte.167.1.68. [DOI] [PubMed] [Google Scholar]
- 16.Alexander KP, Newby LK, Cannon CP, et al. Acute coronary care in the elderly, part I: non-ST-segment-elevation acute coronary syndromes: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology:in collaboration with the Society of Geriatric Cardiology. Circulation. 2007;115:2549–2569. doi: 10.1161/CIRCULATIONAHA.107.182615. [DOI] [PubMed] [Google Scholar]
- 17.Lagerqvist B, Säfström K, Ståhle E, et al. Is early invasive treatment of unstable coronary artery disease equally effective for both men and women? J Am Coll Cardiol. 2001;38:41–48. doi: 10.1016/s0735-1097(01)01308-0. [DOI] [PubMed] [Google Scholar]
- 18.Clayton TC, Pocock SJ, Henderson RA, et al. Do men benefit more than women from an interventional strategy in patients with unstable angina or non- ST-elevation myocardial infarction? The impact of gender in the RITA 3 trial. Eur Heart J. 2004;25:1641–1650. doi: 10.1016/j.ehj.2004.07.032. [DOI] [PubMed] [Google Scholar]
- 19.O'Donoghue M, Boden WE, Braunwald E, et al. Early invasive vs conservative treatment strategies in women and men with unstable angina and non-ST-segment elevation myocardial infarction: a meta-analysis. JAMA. 2008;300:71–80. doi: 10.1001/jama.300.1.71. [DOI] [PubMed] [Google Scholar]
- 20.Huang SS, Chen YH, Lu TM, et al. Effect of invasive strategy on different genders of Chinese patients with non-ST-elevation myocardial infarction. Catheter Cardiovasc Interv. 2012;79:946–955. doi: 10.1002/ccd.23166. [DOI] [PubMed] [Google Scholar]
- 21.Bauer T, Koeth O, Jünger C, et al. Effect of an invasive strategy on in-hospital outcome in elderly patients with non-ST-elevation myocardial infarction. Eur Heart J. 2007;28:2873–2878. doi: 10.1093/eurheartj/ehm464. [DOI] [PubMed] [Google Scholar]
- 22.Devlin G, Gore JM, Elliott J, et al. Management and 6-month outcomes in elderly and very elderly patients with high-risk non-ST-elevation acute coronary syndromes: The Global Registry of Acute Coronary Events. Eur Heart J. 2008;29:1275–1282. doi: 10.1093/eurheartj/ehn124. [DOI] [PubMed] [Google Scholar]