Abstract
Background
Diabetes mellitus (DM) is a strong risk factor of cardiovascular disease. To date, the impact of DM on outcomes after acute myocardial infarction (AMI) in Taiwan is undetermined. The aim of this study was to compare five-year outcomes after AMI in patients with and without diabetes in Taiwan.
Methods
A nationwide cohort of 25,028 diabetic and 56,028 non-diabetic patients who were first hospitalized with AMI between 1996 and 2005 was enrolled through linkage with the Taiwan National Health Insurance research database. Patient mortality rates within 30 days after AMI, and 1, 3, and 5 years thereafter were compared.
Results
Length of hospital stay (8.9 ± 8.7 vs. 8.2 ± 8.0 days, p < 0.01) and medical cost during admission (in Taiwan dollars: $129,123 ± $158,073 vs. $121,631 ± $157,018, p < 0.01) were significantly higher in diabetic patients. The difference in mortality rate within 30 days was insignificant between diabetic and non-diabetic patients (18.1% vs. 17.6%, p = 0.06). Mortalities within 1 year (31.0% vs. 26.8%, p < 0.01), 3 years (42.4% vs. 34.7%, p < 0.01), and 5 years (50.6% vs. 41.1%, p < 0.01) were significantly higher in diabetic patients. In patients with AMI who underwent percutaneous coronary intervention (PCI) during index admission, the mortality rate within 30 days was insignificant (6.3% vs. 6.4%, p = 0.70) but mortalities within 1 year (15.2% vs. 11.6%, p < 0.01), 3 years (24.1% vs. 17.2%, p < 0.01), and 5 years (32.2% vs. 22.6%, p < 0.01) were significantly higher in diabetic patients.
Conclusions
The average patient length of hospital stay and medical cost during admission were significantly higher in diabetic patients. Additionally, the difference in mortality rate within 30 days after AMI was insignificant between diabetic and non-diabetic patients. Also, long-term mortality after AMI was significantly higher in diabetic patients.
Keywords: Acute myocardial infarction, Diabetes mellitus, Length of hospital stay, Medical cost, Mortality, National health insurance
INTRODUCTION
Cardiovascular disease (CVD) has become the second-most prevalent cause of death in Taiwan since 2004, just behind cancer. In 2011, CVD was responsible for 16,513 deaths (10.9% of total mortality) in Taiwan.1 Coronary artery disease (CAD), which often is the consequence of atherosclerosis, is the leading cause of CVD. Acute myocardial infarction (AMI), the most urgent and serious status of CAD, frequently requires immediate revascularization to prevent further potentially lethal arrhythmia, hemodynamic instability, or death.2
Diabetes mellitus (DM) is well-known as a coronary artery equivalent disease and a strong risk factor associated with CVD.3 Some studies have demonstrated that in-hospital or short-term mortality after AMI was similar between diabetic and non-diabetic patients.4,5 But conflicting results were found in other studies, which revealed that in-hospital or short-term mortality was significant higher in diabetic patients.6-10
Diabetic patients with AMI may experience more severe CAD and a greater number of complications (left ventricular dysfunction, heart failure, or significant ventricular arrhythmia) than non-diabetic patients.10 As a result, long-term mortality after AMI may be different in patients with and without diabetes. In fact, some studies have revealed that diabetic patients have a higher long-term mortality rate.5,7,11
Some studies revealed that the length of hospital stay and the medical cost of CVD were significantly higher in diabetic patients, which were related to the older age and added complications in patients with diabetes.12,13
As we know, previous studies focusing on both short-term and long-term impact of DM on the outcomes after AMI in a Taiwanese population have been limited. Therefore, the aim of this study was to compare the length of hospital stay, the medical cost, the mortality rate within 30 days and the long-term mortality after patients were first hospitalized with AMI with and without diabetes, through data linkage from the National Health Insurance Research Database (NHIRD) of Taiwan.
MATERIALS AND METHODS
Data sources
This study used the data from Taiwan’s NHIRD. The applicable data set included all claims data from the National Health Insurance (NHI) program in Taiwan, which finances the healthcare of all residents in Taiwan and offers unrestricted access to any healthcare provider that patients may choose. The single-payer NHI program was launched in Taiwan on March 1, 1995, and now approximately 99% of the country’s entire population is enrolled.14 The NHIRD is one of the largest database sets in the world, and it was encrypted in order to protect the privacy of all patients enrolled. Because the database consists of de-identified secondary data released to the public for research purposes, this study was exempt from full review by the Institutional Review Board.
Study population
This retrospective cohort study included all patients who were admitted to hospitals with the main diagnosis of AMI (ICD-9-CM code from 410 to 410.92) between January 1996 and December 2005. We excluded the patients who had been previously admitted due to AMI, whose gender was undetermined, and whose age was younger than 18 years. After selection, 76,556 patients were selected. The diagnosis of DM is defined whenever any of the ICD-9-CM codes of the index admission was recorded as 250 to 250.90. Mortality within 30 days after AMI is defined when the ending date of coverage from NHI minus the date of hospital admission is less than or equal to 30 days. The mortality within 1 year, 3 years or 5 years is defined when the ending date of coverage from NHI minus the date of admission is less than or equal to 1 year, 3 years, or 5 years, respectively. Because NHI is compulsory, there are very few occasions that a patient, especially an ill patient, can be dropped from insurance coverage for any cause other than death. Moreover, given that the NHI premium is paid on a monthly basis, coverage can easily be dropped immediately after death. Thus, the ending date of coverage from NHI is a good proxy for the mortality date.15 The age of patients was divided into four groups: below 45 years, over or equal to 45 years but below 60 years, over or equal to 60 years but below 75 years, and over or equal to 75 years. Patients who underwent percutaneous coronary intervention (PCI) was defined when any of the ICD-9-CM procedure codes during index admission was recorded as 36.0, 36.01, 36.02, 36.05, 36.06, or 36.09. The length of hospital stay was defined as the number of days a patient remained in the acute inpatient ward. The medical cost during admission was defined as the financial cost incurred by the medical institution noted on their application to NHI. The unit of medical cost was Taiwan Dollars (TWD).
Statistical analyses
Extraction and computation of the data were performed by Microsoft SQL Server 2005 (Microsoft Corp., Redmond, WA, USA). Statistical analysis was performed by SPSS software (version 18.0, SPSS Inc., Chicago, Illinois, USA). All data were expressed as the frequency (percentage) for categorical data or as mean and standard deviation (SD) for continuous data. Logistic regressions were used to determine the difference of gender, age groups, and mortality between diabetic and non-diabetic patients. Simple linear regression was used to determine the difference of age, length of hospital stay, and medical cost between diabetic and non-diabetic patients. Odds ratio (OR) with 95% confidence interval (95% CI) was presented for categorical data and two-sided values of p < 0.05 were considered statistically significant.
RESULTS
Basic characteristics
The characteristics of diabetic and non-diabetic patients when first hospitalized for AMI were presented in Table 1. During January 1996 and December 2005, 76,556 patients were enrolled, including 25,028 diabetic patients and 56,028 non-diabetic patients. The majority (72.1%) of the patients were men, either with diabetes (62.7%) or without diabetes (75.5%). The average age was significantly older in diabetic patients than in non-diabetic patients (66.4 ± 11.5 vs. 66.1 ± 13.8 years, p = 0.01). The ratio of PCI during index admission was similar in diabetic and non-diabetic patients (32.7% vs. 33.2%, p = 0.17). The age distribution of diabetic patients tended to be younger or older than non-diabetic patients (age below 45 years: 8.3% vs. 4.0%, p < 0.01; age over or equal to 75 years: 29.2% vs. 23.1%, p < 0.01).
Table 1. Characteristics of first hospitalized diabetic and non-diabetic patients with acute myocardial infarction in Taiwan.
| With diabetes | Without diabetes | p value | |
| Number of patients | 20,528 (26.8) | 56,028 (73.2%) | |
| Gender (Male) | 12,880 (62.7%) | 42,329 (75.5%) | < 0.01 |
| Age at admission (years ± SD) | 66.4 ± 11.5 | 66.1 ± 13.8 | 0.01 |
| PCI | 6,706 (32.7%) | 18,600 (33.2%) | 0.17 |
| Age | |||
| < 45years | 821 (4.0%) | 4,644 (8.3%) | < 0.01 |
| 45-60 years | 4,988 (24.3%) | 13,017 (23.2%) | < 0.01 |
| 60-75 years | 9,768 (47.6%) | 22,003 (39.3%) | < 0.01 |
| ≥ 75 years | 4,951 (23.1%) | 16,364 (29.2%) | < 0.01 |
Values are mean ± standard deviation or number (%). SD, Standard deviation; PCI, percutaneous coronary intervention.
Length of hospital stay and medical cost during admission
The length of hospital stay after AMI (Figure 1) was significantly longer in patients with diabetes (8.9 ± 8.7 vs. 8.2 ± 8.0 days, p < 0.01), including those who underwent PCI during index admission (8.7 ± 7.2 vs. 8.2 ± 6.6 days, p < 0.01). The medical cost during admission (Figure 2) was significantly higher in AMI patients with diabetes [Taiwan Dollars (TWD) $129,123 ± $158,073 vs. $121,631 ± $157,018, p < 0.01], including those who underwent PCI during index admission (TWD $188,556 ± $120,717 vs. $187,005 ± $129,728, p < 0.01).
Figure 1.
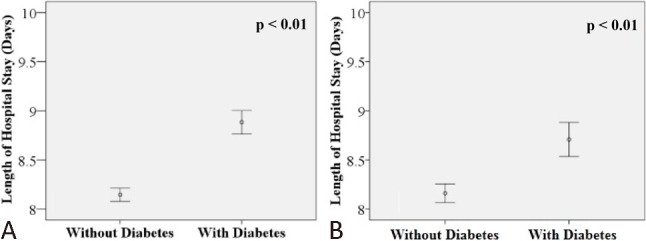
Mean and 95% confidence interval of the length of hospital stay of first acute myocardial infarction hospitalized patients with and without diabetes mellitus: (A) length of hospital stay of all patients; (B) length of hospital stay of patients who underwent PCI.
Figure 2.
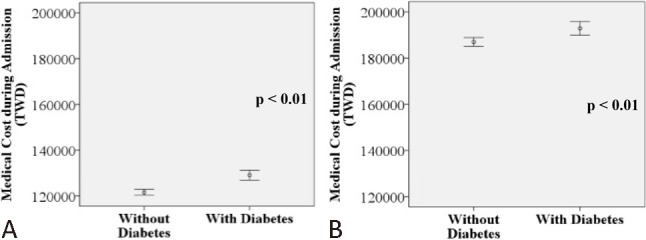
Mean and 95% confidence interval of the medical cost during admission of first acute myocardial infarction hospitalized patients with and without diabetes mellitus: (A) medical cost during admission of all patients; (B) medical cost during admission of patients who underwent PCI. TWD, Taiwan Dollars.
Mortality within 30 days after AMI
Mortality within 30 days after AMI was shown in Table 2. The overall mortality within 30 days after AMI was insignificant between diabetic and non-diabetic patients (18.1% vs. 17.6%, respectively, where p = 0.06).
Table 2. Mortality within 30 days and long-term mortality of first hospitalized diabetic and non-diabetic patients with acute myocardial infarction.
| With diabetes | Without diabetes | |||||
| Death (N) | Death (%) | Death (N) | Death (%) | Odds ratio (95% confidence interval) | p value | |
| Patients with all age | ||||||
| Within 30 days | 3724 | 18.1% | 9834 | 17.6% | 1.04 (1.00-1.09) | 0.06 |
| Within 1 year | 6363 | 31.0% | 14996 | 26.8% | 1.23 (1.19-1.27) | < 0.01 |
| Within 3 years | 8706 | 42.4% | 19417 | 34.7% | 1.39 (1.34-1.44) | < 0.01 |
| Within 5 years | 10396 | 50.6% | 23031 | 41.1% | 1.47 (1.42-1.52) | < 0.01 |
| Patients with age < 45 years | ||||||
| Within 30 days | 52 | 6.3% | 264 | 5.7% | 1.12 (0.83-1.53) | 0.46 |
| Within 1 year | 89 | 10.8% | 348 | 7.5% | 1.50 (1.17-1.92) | < 0.01 |
| Within 3 years | 119 | 14.5% | 454 | 9.8% | 1.56 (1.26-1.94) | < 0.01 |
| Within 5 years | 143 | 17.4% | 590 | 12.7% | 1.45 (1.19-1.77) | < 0.01 |
| Patients with age between 45 and 60 years | ||||||
| Within 30 days | 436 | 8.7% | 929 | 7.1% | 1.25 (1.11-1.40) | < 0.01 |
| Within 1 year | 767 | 15.4% | 1289 | 9.9% | 1.65 (1.50-1.82) | < 0.01 |
| Within 3 years | 1122 | 22.5% | 1717 | 13.2% | 1.91 (1.76-2.08) | < 0.01 |
| Within 5 years | 1393 | 27.9% | 2143 | 16.5% | 1.97 (1.82-2.12) | < 0.01 |
| Patients with age between 60 and 75 years | ||||||
| Within 30 days | 1782 | 18.2% | 3590 | 16.3% | 1.14 (1.08-1.22) | < 0.01 |
| Within 1 year | 3063 | 31.4% | 5498 | 25.0% | 1.37 (1.30-1.45) | < 0.01 |
| Within 3 years | 4247 | 43.5% | 7183 | 32.6% | 1.59 (1.51-1.67) | < 0.01 |
| Within 5 years | 5132 | 52.5% | 8680 | 39.4% | 1.70 (1.62-1.78) | < 0.01 |
| Patients with age ≥ 75 years | ||||||
| Within 30 days | 1454 | 29.4% | 5051 | 30.9% | 0.93 (0.87-1.00) | 0.05 |
| Within 1 year | 2444 | 49.4% | 7861 | 48.0% | 1.06 (1.00-1.13) | 0.06 |
| Within 3 years | 3218 | 65.0% | 10063 | 61.5% | 1.17 (1.09-1.25) | < 0.01 |
| Within 5 years | 3728 | 75.3% | 11618 | 71.0% | 1.25 (1.16-1.34) | < 0.01 |
Long-term mortality after AMI
Long-term mortality after AMI was showed in Table 2. The overall mortalities within 1 year, 3 years and 5 years after AMI were significantly higher in diabetic patients (within 1 year: 31.0% vs. 26.8%, p < 0.01; within 3 years: 42.4% vs. 34.7%, p < 0.001; within 5 years: 50.6% vs. 41.1%, p < 0.01).
Mortality after AMI with different age
Mortality after AMI in patients differing in age was shown in Table 2. The mortalities within 30 days after AMI were insignificant between diabetic and non-diabetic patients when the age was below 45 years (6.3% vs. 5.7%, p = 0.46) and over or equal to 75 years (29.4% vs. 30.9%, p = 0.05). In the age groups between 45 and 60 years and between 60 and 75 years, the mortalities within 30 days after AMI were significant higher in diabetic patients (45-60 years: 8.7% vs. 7.1%, p < 0.01; 60-75 years: 18.2% vs. 16.3%, p < 001). The mortalities within 1 year, 3 years, and 5 years after AMI were significant higher in diabetic patients of all ages, except patients over or equal to 75 years within 1 year (49.4% vs. 48.0%, p = 0.06).
Mortality after AMI of patients who underwent PCI during index admission
Mortality after AMI of patients who underwent PCI during index admission was showed in Table 3. The mortalities after AMI of patients who underwent PCI during index admission were significantly lower than those of patients without PCI treatment (within 30 days: 6.4% vs. 23.3%, p < 0.01; within 1 year: 12.6% vs. 35.5%, p < 0.01; with 3 years: 19.0% vs. 45.5%, p < 0.01; and within 5 years: 25.2% vs. 52.8%, p < 0.01). Regarding diabetic status, mortality within 30 days after AMI of patients who underwent PCI during index admission was insignificant between diabetic and non-diabetic patients (6.3% vs. 6.4%, p = 0.70), which included all age groups. Mortalities within 1 year, 3 years and 5 years after AMI were significantly higher in diabetic patients (within 1 year: 15.2% vs. 11.6%, p < 0.01; within 3 years: 24.1% vs. 17.2%, p < 0.01; within 5 years: 32.2% vs. 22.6%, p < 0.01), including all age groups, excepting patients over or equal to 75 years within 1 year (30.4% vs. 27.8%, p = 0.11).
Table 3. Mortality within 30 days and long-term mortality of first hospitalized diabetic and non-diabetic patients with acute myocardial infarction underwent percutaneous coronary intervention (PCI) during index admission.
| With diabetes | Without diabetes | |||||
| Death (N) | Death (%) | Death (N) | Death (%) | Odds ratio (95% Confidence interval) | p value | |
| Patients with all age underwent PCI | ||||||
| Within 30 days | 420 | 6.3% | 1190 | 6.4% | 0.98 (0.87-1.10) | 0.7 |
| Within 1 year | 1020 | 15.2% | 2157 | 11.6% | 1.37 (1.26-1.48) | < 0.01 |
| Within 3 years | 1615 | 24.1% | 3190 | 17.2% | 1.53 (1.43-1.64) | < 0.01 |
| Within 5 years | 2162 | 32.2% | 4212 | 22.6% | 1.63 (1.53-1.73) | < 0.01 |
| Patients with age < 45 years underwent PCI | ||||||
| Within 30 days | 10 | 2.6% | 36 | 1.9% | 1.39 (0.68-2.82) | 0.37 |
| Within 1 year | 22 | 5.7% | 61 | 3.2% | 1.83 (1.11-3.02) | 0.02 |
| Within 3 years | 31 | 8.1% | 87 | 4.6% | 1.83 (1.20-2.80) | 0.01 |
| Within 5 years | 42 | 11.0% | 138 | 7.3% | 1.57 (1.09-2.26) | 0.02 |
| Patients with age between 45 and 60 years underwent PCI | ||||||
| Within 30 days | 59 | 2.8% | 153 | 2.6% | 1.07 (0.79-1.45) | 0.66 |
| Within 1 year | 144 | 6.8% | 246 | 4.2% | 1.67 (1.35-2.05) | < 0.01 |
| Within 3 years | 248 | 11.7% | 378 | 6.4% | 1.93 (1.63-2.28) | < 0.01 |
| Within 5 years | 347 | 16.4% | 530 | 9.0% | 1.98 (1.71-2.29) | < 0.01 |
| Patients with age between 60 and 75 years underwent PCI | ||||||
| Within 30 days | 192 | 6.2% | 472 | 6.4% | 0.96 (0.81-1.14) | 0.65 |
| Within 1 year | 523 | 16.8% | 889 | 12.1% | 1.47 (1.31-1.66) | < 0.01 |
| Within 3 years | 835 | 26.8% | 1313 | 17.8% | 1.69 (1.53-1.87) | < 0.01 |
| Within 5 years | 1127 | 36.2% | 1753 | 23.8% | 1.82 (1.66-1.99) | < 0.01 |
| Patients with age ≥ 75 years underwent PCI | ||||||
| Within 30 days | 159 | 14.6% | 529 | 15.3% | 0.94 (0.78-1.14) | 0.55 |
| Within 1 year | 331 | 30.4% | 961 | 27.8% | 1.13 (0.97-1.31) | 0.11 |
| Within 3 years | 501 | 46.0% | 1412 | 40.9% | 1.23 (1.07-1.41) | < 0.01 |
| Within 5 years | 646 | 59.3% | 1791 | 51.9% | 1.35 (1.18-1.55) | < 0.01 |
DISCUSSION
This study provides a nationwide estimate in Taiwan about the outcomes after 5-year follow-up among first hospitalized AMI patients with and without diabetes. The number of patients who participated was quite large, and nearly all the residents in Taiwan were enrolled. The duration of follow-up was also quite long. The length of hospital stay and the medical cost during admission were significantly higher in diabetic patients. The overall mortality within 30 days after AMI was insignificant, but the long-term mortality after AMI was significantly higher in diabetic patients than in non-diabetic patients. In patients with AMI who underwent PCI during index admission, the mortality rate within 30 days was insignificant, but the long-term mortality was significantly higher in diabetic patients than in non-diabetic patients. The mortalities within 30 days after AMI were insignificant when patients were under 45 years of age, or over or equal to 75 years, but they became significantly higher in diabetic patients between 45 and 60 years of age, or between 60 and 75 years. The long-term mortality after AMI was significantly higher in diabetic patients of all ages, except for those patients over or equal to 75 years of age within 1 year.
Krumholz et al. found that the 30-day mortality rates of AMI patients in the United States were 18.9% in 1995 and 17.6% in 2006.16 In our study, the 30-day morality rates of AMI patients were 18.1% in diabetic and 17.6% in non-diabetic patients during the study period. The mortality rates of AMI patients between the United States and Taiwan were similar.
Lopez-de-Andres et al. found that in patients admitted to hospital due to AMI from 2001 to 2006 in Spain, the mean hospital stay was significantly higher in diabetic patients than in non-diabetic patients (10.1 ± 8.7 vs. 9.2 ± 9.2 days, p < 0.05), but the medical cost did not differ significantly.17 However, Carral et al. found that diabetic patients hospitalized for CVD had longer hospital stays and were more costly than non-diabetic patients.13 In our study, both the length of hospital stay and the medical cost during admission were significantly higher in diabetic patients. Older age and additional comorbid conditions could explain the increased medical cost in diabetic patients.18 Local healthcare policy, such as diagnosis-related group (DRG), may also have an influence on the medical cost in different countries.19
Some studies have shown that short-term mortality after AMI was insignificant between diabetic and non-diabetic patients.4,5,20 However, the results of some other studies reached opposite results, which revealed that diabetic patients had a higher rate of short-term mortality after AMI than non-diabetic patients.6-10,17,21 Regarding those patients with AMI who underwent revascularization during index admission, some studies found that short-term mortality was insignificant between diabetic and non-diabetic patients.9,22 Nevertheless, other studies had a conflicting result, which discovered that diabetic patients have a higher short-term mortality.23-25 The influence of diabetes on short-term mortality after AMI seemed inconsistent, including in overall patients and in patients underwent revascularization, according to the finding of above studies. In our study, the mortality within 30 days after AMI was insignificant between diabetic and non-diabetic patients, including in overall patients and in patients underwent PCI during index admission. The differences of race, duration of follow-up, and predictors of mortality enrolled should influence the impact of diabetes on short-term mortality. The strength of our study in part relied on the large sample size, the lack of selection of the cohort, and the long duration of follow-up.
Previous studies found that the long-term mortality after AMI was significantly higher in diabetic patients,7,9,21 which was consistent with our study. Besides, the difference in mortality after AMI between diabetic and non-diabetic patients increased with time in our study [OR ranging from 1.23 (95% CI 1.19-1.27) within 1 year to 1.39 (95% CI 1.34-1.44) within 3 years and 1.47 (95% CI 1.42-1.52) within 5 years], which was identical with another study.26 In patients with AMI who underwent PCI, the long-term mortality was significant higher in diabetic patients and the difference also increased with time, compatible with previous studies.23-25 However, when patient age exceeded or was equal to 75 years, the mortality after AMI within 1 year became insignificant between diabetes and non-diabetes, including in overall patients and in patients underwent PCI. Nicolau et al. found that in patients with AMI, hyperglycemia was a better predictor for mortality in younger patients than in an elderly population, and advanced age itself was a strong independent risk factor for mortality in patients with AMI.27 Therefore, diabetes had a weaker impact in elderly population, which was consistent with our study.
The mortality after AMI was significantly lower in patients who underwent PCI during index admission than in patients with conservative treatment. Gasior et al. found that the intervention group of AMI had significantly lower short-term and long-term mortalities than the conservative group,9 which was consistent with our study. As a result, the strategy of intervention should be a priority for consideration in patients with AMI to decrease the mortality, if the clinical conditions meet the suggestion of current guidelines for interventional treatment.28,29
Study limitation
There are several limitations of our study. First, the date of mortality was defined as the ending date of coverage from NHI. However, Lien et al. found that the ending date of coverage from NHI is a good proxy for the mortality date.15 Second, some predictors of mortality after AMI, such as Killip classifications, ST or non-ST elevation myocardial infarction, left ventricular ejection fraction, the medication used and renal function could not be jointly evaluated with diabetes, due to the limitation of NHIRD. The impacts of these predictors on diabetic and non-diabetics patients with AMI might need further investigation.
CONCLUSIONS
The length of hospital stay and the medical cost of admission were higher in diabetic patients. Mortality within 30 days after AMI was insignificant, including in the overall enrolled patient population, and in patients who underwent PCI. Long-term mortality after AMI was significantly higher in diabetic patients and the difference increased with time. Diabetes has a stronger influence on long-term mortality. Therefore, diabetic patients with AMI should be reinforced with the importance of vigorous preventive measures by lifestyle modification and medication adherence, to decrease long-term mortality.
REFERENCES
- 1.http://www.doh.gov.tw [Google Scholar]
- 2.Shyu KG, Wu CJ, Mar GY. Clinical characteristics, management and in-hospital outcomes of patients with acute coronary syndrome observations from the Taiwan ACS full spectrum registry. Acta Cardiol Sin. 2011;27:135–144. [Google Scholar]
- 3.Haffner SM, Lehto S, Ronnemaa T, et al. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. New Engl J Med. 1998;339:229–234. doi: 10.1056/NEJM199807233390404. [DOI] [PubMed] [Google Scholar]
- 4.Hasin T, Hochadel M, Gitt AK, et al. Comparison of treatment and outcome of acute coronary syndrome in patients with versus patients without diabetes mellitus. Am J Cardiol. 2009;103:772–778. doi: 10.1016/j.amjcard.2008.11.034. [DOI] [PubMed] [Google Scholar]
- 5.Koek HL, Soedamah-Muthu SS, Kardaun JW, et al. Short- and long-term mortality after acute myocardial infarction:comparison of patients with and without diabetes mellitus. Eur J Epidemiol. 2007;22:883–888. doi: 10.1007/s10654-007-9191-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hsu HP, Jou YL, Lin SJ, et al. Comparison of in-hospital outcome of acute ST elevation myocardial infarction in patients with versus without diabetes mellitus. Acta Cardiol Sin. 2011;27:145–151. [Google Scholar]
- 7.Donnan PT, Boyle DI, Broomhall J, et al. Prognosis following first acute myocardial infarction in type 2 diabetes:a comparative population study. Diabet Med. 2002;19:448–455. doi: 10.1046/j.1464-5491.2002.00711.x. [DOI] [PubMed] [Google Scholar]
- 8.Lowel H, Koenig W, Engel S, et al. The impact of diabetes mellitus on survival after myocardial infarction:can it be modified by drug treatment? Results of a population-based myocardial infarction register follow-up study. Diabetologia. 2000;43:218–226. doi: 10.1007/s001250050032. [DOI] [PubMed] [Google Scholar]
- 9.Gasior M, Pres D, Gierlotka M, et al. The influence of diabetes on in-hospital and long-term mortality in patients with myocardial infarction complicated by cardiogenic shock:results from the PL-ACS registry. Kardiol Pol. 2012;70:1215–1224. [PubMed] [Google Scholar]
- 10.Franklin K, Goldberg RJ, Spencer F, et al. Implications of diabetes in patients with acute coronary syndromes. The Global Registry of Acute Coronary Events. Arch Intern Med. 2004;164:1457–1463. doi: 10.1001/archinte.164.13.1457. [DOI] [PubMed] [Google Scholar]
- 11.Brophy S, Cooksey R, Gravenor MB, et al. Population based absolute and relative survival to 1 year of people with diabetes following a myocardial infarction: a cohort study using hospital admissions data. BMC Public Health. 2010;10:338. doi: 10.1186/1471-2458-10-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Novo G, Scordato F, Cerruto G, et al. In-hospital stay of patient with acute coronary syndrome with or without diabetes mellitus. Minerva Cardioangiol. 2009;57:159–164. [PubMed] [Google Scholar]
- 13.Carral F, Aguilar M, Olveira G, et al. Increased hospital expenditures in diabetic patients hospitalized for cardiovascular diseases. J Diabetes Complications. 2003;17:331–336. doi: 10.1016/s1056-8727(02)00219-2. [DOI] [PubMed] [Google Scholar]
- 14.http://nhird.nhri.org.tw/en/index.htm [Google Scholar]
- 15.Lien HM, Chou SY, Liu JT. Hospital ownership and performance: evidence from stroke and cardiac treatment in Taiwan. J Health Econ. 2008;27:1208–1223. doi: 10.1016/j.jhealeco.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 16.Krumholz HM, Wang Y, Chen J, et al. Reduction in acute myocardial infarction mortality in the united states: risk-standardized mortality rates from 1995-2006. JAMA. 2009;302:767–773. doi: 10.1001/jama.2009.1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lopez-de-Andres A, Hernandez-Barrera V, Carrasco-Garrido P, et al. Trends of hospitalizations, fatality rate and costs for acute myocardial infarction among Spanish diabetic adults, 2001-2006. BMC Health Serv Res. 2010;10:59. doi: 10.1186/1472-6963-10-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bramkamp M, Radovanovic D, Erne P, Szucs TD. Determinants of costs and the length of stay in acute coronary syndromes: a real life analysis of more than 10,000 patients. Cardiovasc Drugs Ther. 2007;21:389–398. doi: 10.1007/s10557-007-6044-0. [DOI] [PubMed] [Google Scholar]
- 19.Lema Devesa MC. Economics,health,and health care. Neurologia (Barcelona, Spain) 2003;18 Suppl 4:57–63. [PubMed] [Google Scholar]
- 20.Casella G, Savonitto S, Chiarella F, et al. Clinical characteristics and outcome of diabetic patients with acute myocardial infarction. Data from the BLITZ-1 study. Ital Heart J. 2005;6:374–383. [PubMed] [Google Scholar]
- 21.Norhammar A, Lindbäck J, Rydén L, et al. Improved but still high short- and long-term mortality rates after myocardial infarction in patients with diabetes mellitus: a time-trend report from the Swedish Register of Information and Knowledge about Swedish Heart Intensive Care Admission. Heart. 2007;93:1577–1583. doi: 10.1136/hrt.2006.097956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Janion M, Polewczyk A, Gąsior M, et al. Does reperfusion in the treatment of acute myocardial infarction improve the prognosis of acute myocardial infarction in diabetic patients? Clin Cardiol. 2009;32:E51–E55. doi: 10.1002/clc.20428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Park KH, Ahn Y, Jeong MH, et al. Different impact of diabetes mellitus on in-hospital and 1-year mortality in patients with acute myocardial infarction who underwent successful percutaneous coronary intervention: results from the Korean Acute Myocardial Infarction Registry. Korean J Intern Med. 2012;27:180–188. doi: 10.3904/kjim.2012.27.2.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brener SJ, Mehran R, Dressler O, et al. Diabetes mellitus, myocardial reperfusion, and outcome in patients with acute ST-elevation myocardial infarction treated with primary angioplasty (from HORIZONS AMI) Am J Cardiol. 2012;109:1111–1116. doi: 10.1016/j.amjcard.2011.11.046. [DOI] [PubMed] [Google Scholar]
- 25.Kahn MB, Cubbon RM, Mercer B, et al. Association of diabetes with increased all-cause mortality following primary percutaneous coronary intervention for ST-segment elevation myocardial infarction in the contemporary era. Diab Vasc Dis Res. 2012;9:3–9. doi: 10.1177/1479164111427752. [DOI] [PubMed] [Google Scholar]
- 26.Melchior T, Kober L, Madsen CR, et al. Accelerating impact of diabetes mellitus on mortality in the years following an acute myocardial infarction. TRACE Study Group. Trandolapril Cardiac Evaluation. Eur Heart J. 1999;20:973–978. doi: 10.1053/euhj.1999.1530. [DOI] [PubMed] [Google Scholar]
- 27.Nicolau JC, Serrano CV, Jr., Giraldez RR, et al. In patients with acute myocardial infarction, the impact of hyperglycemia as a risk factor for mortality is not homogeneous across age-groups. Diabetes Care. 2012;35:150–152. doi: 10.2337/dc11-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction:executive summary: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:529–555. doi: 10.1161/CIR.0b013e3182742c84. [DOI] [PubMed] [Google Scholar]
- 29.Anderson JL, Adams CD, Antman EM, et al. 2011 ACCF/AHA focused update incorporated into the ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;123:e426–e579. doi: 10.1161/CIR.0b013e318212bb8b. [DOI] [PubMed] [Google Scholar]


