Abstract
Background
Although there have been some studies focusing on the relationship between body mass index (BMI), coronary artery disease (CAD) and acute coronary syndrome, the clinical effects of BMI on outcomes after percutaneous coronary intervention (PCI) in patients with acute myocardial infarction (AMI) are not well known in a Taiwanese population.
Methods
From January 2005 to December 2011, 1298 AMI patients who received PCI were enrolled from a single center in Taiwan. The patients were divided into 4 groups according to their BMI: underweight (BMI < 18.5 kg/m2); normal weight (18.5 ≤ BMI < 24 kg/m2); overweight (24 ≤ BMI < 27 kg/m2) and obese (BMI ≥ 27). All patients had been followed up for at least 12 months, and 30-day and 5-year all-cause and cardiovascular-cause mortality were compared among the study groups.
Results
The patients in the underweight group had a lower 30-day survival rate than the other 3 groups, and the underweight and normal weight patients had a lower 5-year survival rate than the overweight and obese patients. The multivariate regression analysis showed that Killip class ≥ 2, non-use of statin, older age, hemoglobin < 12 g/dl and chronic kidney disease, but not BMI, are independent predictors of all-cause mortality.
Conclusions
In this present study, the major factors affecting long-term survival are lack of using statin and older age, but not obese paradox.
Keywords: Acute myocardial infarction, Mortality, Obesity, Percutaneous coronary intervention, Survival
Obesity is associated with increased morbidity and mortality, and it is also associated with insulin resistance, often resulting in diabetes mellitus, hypertension, and dyslipidemia.1-4 However, other previous studies suggested a phenomenon, called “obesity paradox”, which meant that obese patients had better outcomes than normal-weight patients after percutaneous coronary intervention (PCI).5-8 In the BARI study, which enrolled patients with stable angina and multi-vessel coronary artery disease (CAD), each unit increase in body mass index (BMI) was associated with a 5.5% lower adjusted risk of a major in-hospital event, but BMI was not associated with five-year mortality in the percutaneous transluminal coronary angioplasty group.6 Acute myocardial infarction (AMI) is a leading cause of morbidity and mortality.9 However, evaluating the risk stratification in patients with AMI remains challenging.10-15 Obesity paradox was also found in patients with acute coronary syndrome.16,17 However, these available large-scale “obesity paradox” studies were largely based on the western populations, not on the Asian population, and the follow-up periods of the studies enrolling patients with acute coronary syndrome were usually less than 2 years. It is well-known that the Asian population is generally leaner than the western population; therefore, is the obesity paradox present in the Asian population? Furthermore, there have been few articles published addressing the relationship between obesity and long-term (more than 5 years) mortality. The clinical effects of BMI on outcomes after percutaneous coronary intervention (PCI) in patients with acute myocardial infarction also remain unknown in Taiwan. Therefore, we intended to evaluate the clinical effects of BMI on the outcomes in AMI patients after PCI in Kaohsiung Veterans General Hospital Taiwan.
METHODS
Study population
From January 2005 to December 2011, 1491 consecutive AMI patients were retrospectively reviewed. All patients were followed up through March 2013. All living patients had been followed for at least 12 months. This retrospective study protocol was approved by the Human Research Committee of our hospital. The diagnosis of AMI was based on the Third Universal Criteria of Myocardial Infarction18 and it should meet the detection of a rise and/or fall of cardiac biomarker values with at least one of the following: 1) symptoms of ischemia; 2) new or presumed new significant ST-segment - T wave changes or new left bundle branch block; 3) development of pathological Q waves in the ECG; 4) imaging evidence of new loss of viable myocardium or new regional wall motion abnormality; or 5) identification of an intracoronary thrombus by angiography or autopsy.
The inclusion criteria was AMI patients who received PCI during hospitalization due to AMI, and the exclusion criteria included patients who ever received coronary artery bypass surgery, AMI patients who did not received PCI during the hospitalization due to AMI, preexisting severe left-sided valvular heart diseases, congenital heart diseases, hypertrophy or dilated cardiomyopathy, and patients who had profound cardiogenic shock and died in the first 24 hours after presenting to our emergency room. Medical treatment of AMI patients followed the ACC/AHA ST-elevation and non-ST-elevation myocardial infarction guidelines.19-22 The coronary angiograms were performed by experienced cardiologists via Philips MultiDiagnost Eleva interventional radiography/fluoroscopy system. Following balloon dilatation, the choice of bare-metal stent or drug-eluting stent deployment was dependent on the decision of operators.
Body mass index
Body mass index is defined as an individual’s body weight divided by the square of their height. For the analysis, patients were classified into 4 groups based on a recommendation by the Taiwan Department of Health for the Taiwanese population: underweight (group 1: BMI < 18.5 kg/m2); normal weight (group 2: 18.5 ≤ BMI < 24 kg/m2); overweight (group 3: 24 ≤ BMI < 27 kg/m2) and obese (group 4: BMI ≥ 27 kg/m2).
Clinical evaluation and outcomes
The characteristics of patients consisted of medical history (hypertension, diabetes mellitus, current smoker, hyperlipidemia, previous coronary artery disease, and previous ischemic cerebral event), hemodynamic parameters (systolic blood pressures and heart rates) at the emergency room, and the laboratory parameters. The definition of chronic kidney disease was defined as previous known estimated glomerular filtration rate < 60 ml/min/1.73 m2. The blood biochemistry tests (including renal function tests, electrolytes, serum lipids, high-sensitivity C-reactive protein) and complete blood cell counts were measured at the emergency room and on the first day of hospitalization. The length of hospital stay was defined by the medical record. To determine the status and the causes of mortality, we used 2 methods. First, we used chart review to confirm the cause of mortality if the patient died or was discharged in critical condition from our hospital; otherwise, we used telephone interview. The causes of death were defined as all-cause mortality and cardiovascular-cause mortality.
Statistics
All statistical analyses were performed with SPSS software, version 21 (IBM Inc., USA). Categorical data are presented as absolute values and percentages, whereas continuous variables are summarized as mean values ± standard deviation. The Chi-squared test was used for comparison of categorical data, and ANOVA with post hoc correction was applied for comparison of continuous variables among the 4 groups. To evaluate the influence of age on survival rate using Kaplan-Meier survival analysis, we also divided the patients into 4 groups by age: 1) age < 55 years; 2) ≥ 55 years and < 65 years; 3) 65 ≥ age but < 75 years; 4) age ≥ 75 years. The analysis of survival rate after AMI was estimated using the Kaplan-Meier method with the log-rank test to compare mortality among the 4 BMI groups with stratification by age category. Univarate and multivariate regression analysis were done to identify the prognostic factors affecting the long-term and short-term mortality. Differences were considered statistically significant if the p value was < 0.05 with a 95% confidence interval.
RESULTS
Baseline characteristics
After reviewing medical records, 1298 patients were enrolled in this study (Figure 1). The 4 groups were classified as underweight group (n = 52), normal weight group (n = 477), overweight group (n = 428) and obese group (n = 340), according to the pre-defined BMI categories. The basic clinical characters of each group were listed in Table 1. The age of patients was all statistically significant among the 4 study groups, in that the obese patients had lowest ages and the underweight patients had the highest ages. The patient’s previous medical history, including diabetes mellitus, hypertension, current smoker and previous known CAD and ischemic cerebral events, were not statistically different among the 4 study groups. We enrolled patients with non-ST-elevation myocardial infarction (NSTEMI) or ST-elevation myocardial infarction (STEMI), but there was no difference in the subtype of AMI among the groups. However, the patients in the underweight group had increased the severity of AMI, with Killip classification ≥ 2.
Figure 1.
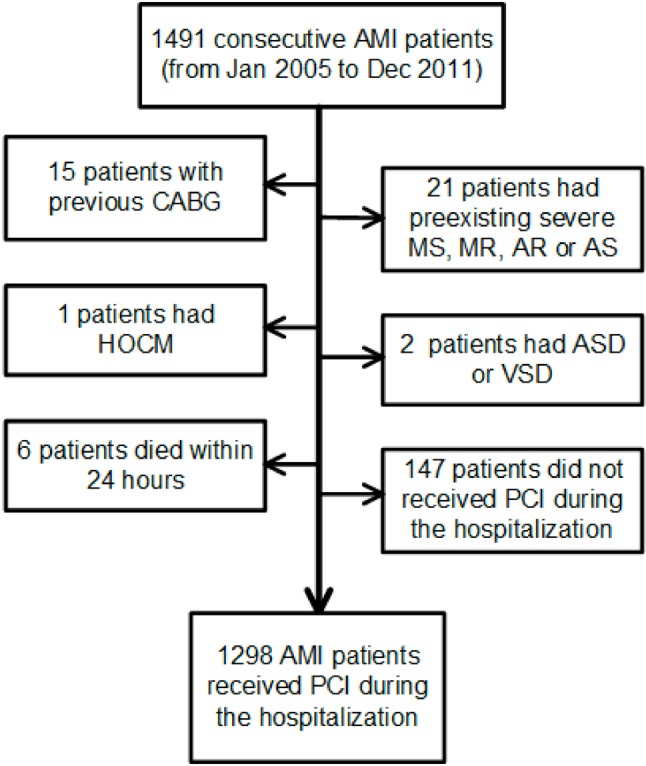
Enrollment algorithm. AMI, acute myocardial infarction; AR, aortic regurgitation; AS, aortic stenosis; ASD, atrial septal defect; CABG, coronary artery bypass surgery; HOCM, hypertrophic obstructive cardiomyopathy; MR, mitral regurgitation; MS, mitral stenosis; PCI, percutaneous coronary intervention; VSD, ventricular septal defect.
Table 1. Baseline characteristics of the 4 study groups.
| All | Underweight (BMI < 18.5) | Normal weight (18.5 ≤ BMI < 24) | Overweight (24 ≤ BMI < 27) | Obese (BMI ≥ 27) | ||
| (n = 1298) | (Group 1, n = 52) | (Group 2, n = 477) | (Group 3, n = 428) | (group 4, n = 340) | p value | |
| Age, years | 63.6 ± 4.5 | 77.8 ± 11.0 | 67.74 ± 3.6 | 61.9 ± 13.7 | 57.9 ± 14.5 | < 0.001*† ‡ § #** |
| Male | 1074 (82.7%) | 42 (80.8%) | 382 (80.1%) | 361 (84.3%) | 289 (85%) | 0.23 |
| Hypertension | 717 (55.2%) | 29 (55.7%) | 255 (53.5%) | 239 (55.8%) | 194 (56.2%) | 0.94 |
| Diabetes mellitus | 463 (35.7%) | 20 (38.5%) | 175 (36.7%) | 156 (36.4%) | 112 (32.9%) | 0.66 |
| Current smoker | 533 (41.0%) | 25 (48.1%) | 210 (44.0%) | 173 (40.4%) | 124 (36.5%) | 0.12 |
| Previous CAD | 83 (6.4%) | 4 (7.7%) | 33 (6.9%) | 25 (5.8%) | 21 (6.2%) | 0.84 |
| Previous cerebral events | 82 (6.3%) | 5 (9.6%) | 24 (5.0%) | 31 (7.2%) | 22 (6.5%) | 0.48 |
| Gout | 94 (7.2%) | 5 (9.6%) | 37 (7.8%) | 23 (5.4%) | 29 (8.5%) | 0.28 |
| STEMI | 855 (65.9%) | 29 (55.8%) | 301 (63.1%) | 291 (68.0%) | 234 (68.8%) | 0.32 |
| Killip class ≥ 2 | 728 (56%) | 39 (75%) | 277 (58.1%) | 242 (56.5%) | 170 (50%) | 0.004 |
| Medication at discharge | ||||||
| Aspirin | 1289 (99.3%) | 51 (98.1%) | 474 (99.4%) | 426 (99.5%) | 338 (99.4%) | 0.75 |
| Clopidogrel | 1282 (98.8%) | 52 (100%) | 471 (98.7%) | 427 (99.8%) | 332 (97.6%) | 0.1 |
| β-blockers | 1116 (86.0%) | 46 (88.5%) | 398 (83.4%) | 373 (87.1%) | 299 (87.9%) | 0.24 |
| ACEIs/ARBs | 1143 (88.1%) | 45 (86.5%) | 408 (88.5%) | 381 (89.0%) | 309 (90.9%) | 0.12 |
| Statins | 633 (48.8%) | 14 (26.9%) | 198 (41.5%) | 213 (49.8%) | 208 (61.2%) | < 0.001 |
Category data were expressed as patients number and percentage; continuous data were expressed as mean ± SD.
ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin II receptor blocker; BMI, body mass index; CAD, coronary artery disease or myocardial infarction; STEMI, ST-segment-elevation myocardial infarction.
* Statistical significance between underweight group and normal weight group; † Statistical significance between underweight group and overweight group; ‡ Statistical significance between underweight group and normal BMI group; § Statistical significance between normal weight group and overweight group; # Statistical significance between normal weight group and obese group;
** Statistical significance between overweight group and obese group.
Hemodynamic and laboratory data
Table 2 showed the initial hemodynamic parameters and serum laboratory data at the emergency room and on the first day of admission among the 4 groups. Although the underweight group had higher Killip class (shown in Table 1) than other groups, there were no significant differences in heart rates and systolic blood pressures at ER among the study groups. The overweight and obese patients had higher hemoglobin than the patients in the other 2 groups (group 1: 11.2 ± 2.6 g/dl, group 2: 12.8 ± 5.5 g/dl, group 3: 13.6 ± 2.5 g/dl, and group 4: 14.1 ± 2.7 g/dl, p < 0.001), and there was a significant difference in white blood cell count between the obese patients and the normal weight patients (group 2: 10.7 ± 4.1 *1000/mm3, group 4: 11.6 ± 4.5 *1000/mm3, p = 0.04). However, there was no significant difference in the serum concentration of high-sensitivity C-reactive protein, creatinine and uric acid. Regarding the lipid profile, the underweight patients had the lowest concentration of serum total cholesterol, low-density lipoprotein cholesterol, and triglyceride. The concentration of serum total cholesterol increased significantly (group 1: 147.2 ± 36.8 mg/dl, group 2: 170.4 ± 43 mg/dl, group 3: 180.6 ± 42.7 mg/dl, and group 4: 185.7 ± 43.6 mg/dl, p < 0.001) as BMI category increase from 1 to 3, and there was no difference between group 3 and group 4. There was a similar finding on the serum concentration of low-density lipoprotein cholesterol (group 1: 81.9 ± 30.8 mg/dl, group 2: 100.9 ± 33.9 mg/dl, group 3: 108 ± 35.2 mg/dl, and group 4: 109.9 ± 34.2 mg/dl, p < 0.001). The serum concentration of triglyceride increased as BMI category increased from 1 to 4 (group 1: 62.8 ± 39.4 mg/dl, group 2: 98.4 ± 107.1 mg/dl, group 3: 117.7 ± 94.2 mg/dl, and group 4: 146 ± 143.2 mg/dl, p < 0.001). Therefore, a higher ratio of group 4 patients had received statins to control hyperlipidemia (Table 1).
Table 2. Hemodynamics and serum laboratory data of the 4 study groups.
| All | Underweight (BMI < 18.5) | Normal weight (18.5 ≤ BMI < 24) | Overweight (24 ≤ BMI < 27) | Obese (BMI ≥ 27) | ||
| (n = 1298) | (Goup 1, n = 52) | (Group 2, n = 477) | (Group 3, n = 428) | (Group 4, n = 340) | p value | |
| ER HR, beats per minute | 83.9 ± 23.5 | 92.4 ± 20.4 | 83.5 ± 24.2 | 84.1 ± 22.8 | 83.0 ± 23.6 | 0.1 |
| ER systolic BP, mmHg | 138.4 ± 31.4 | 138.8 ± 29.3 | 136.8 ± 32.4 | 138.6 ± 31.1 | 140.2 ± 30.7 | 0.56 |
| WBC, *1000/mm3 | 11.1 ± 4.2 | 10.9 ± 4.5 | 10.7 ± 4.1 | 11.0 ± 3.9 | 11.6 ± 4.5 | 0.04 |
| Hb, g/dl | 13.3 ± 4.0 | 11.2 ± 2.6 | 12.8 ± 5.5 | 13.6 ± 2.5 | 14.1 ± 2.7 | < 0.001*† ‡ §# |
| hs-CRP, mg/dl | 7.2 ± 7.9 | 6.7 ± 8.2 | 8.8 ± 7.9 | 7.6 ± 7.6 | 6.7 ± 8.2 | 0.38 |
| Cr, mg/dl | 1.40 ± 1.40 | 1.79 ± 1.9 | 1.47 ± 1.46 | 1.39 ± 1.44 | 1.27 ± 1.10 | 0.046 |
| uric acid, mg/dl | 6.6 ± 2.1 | 5.7 ± 2.6 | 6.5 ± 2.4 | 6.6 ± 2.0 | 6.8 ± 1.7 | 0.16 |
| Total cholesterol, mg/dl | 177.0 ± 43.6 | 147.2 ± 36.8 | 170.4 ± 43.0 | 180.6 ± 42.7 | 185.7 ± 43.6 | < 0.001*† ‡ § # |
| HDL cholesterol, mg/dl | 36.0 ± 10.7 | 37.8 ± 15.0 | 36.7 ± 10.6 | 35.8 ± 9.4 | 34.9 ± 11.8 | 0.11 |
| LDL cholesterol, mg/dl | 104.9 ± 34.8 | 81.9 ± 30.8 | 100.9 ± 33.9 | 108.0 ± 35.2 | 109.9 ± 34.2 | < 0.001*† ‡ § # |
| Triglyceride, mg/dl | 116.3 ± 114.5 | 62.8 ± 39.4 | 98.4 ± 107.1 | 117.7 ± 94.2 | 146.7 ± 143.2 | < 0.001*† ‡ § #** |
Continuous data were expressed as mean ± SD.
BMI, body mass index; BP, blood pressure; Cr, serum creatinine; ER, emergency room; Hb, hemoglobin; HDL, high-density lipoprotein; HR, heart rate; hs-CRP, high-sensitivity
C-reactive protein; LDL, low-density lipoprotein; WBC, white blood cell count. * Statistical significance between underweight group and normal weight group; †Statistical significance between underweight group and overweight group; ‡ Statistical significance between underweight group and normal BMI group; § Statistical significance between normal weight group and overweight group; # Statistical significance between normal weight group and obese group;
** Statistical significance between overweight group and obese group.
Mortality and survival curve analysis
The obese patients had significantly lower all-cause mortality (group 1: 28.8%, group 2: 19.3%, group 3: 12.1%, group 4: 8.5%, p < 0.001) and lower cardiovascular mortality (group 1: 21.2%, group 2: 13.6%, group 3: 8.4%. group 4: 7.0%) than the other groups (Figure 2). Kaplan-Meier survival curve analysis for 30-day survival showed significant lower overall survival in the underweight group (log-rank p < 0.001) (Figure 3). We also examined the long-term survival and found that significant lower overall survival and survival free of death from cardiovascular events in the underweight and normal weight groups (log-rank p < 0.001) (Figure 4). In the 5-year follow-up, we found that survival of the underweight patients almost reached the trough at 1 year and the survival rate of the normal weight patients decreased more rapidly after the second year follow-up (Figure 4). When processing Kaplan-Meier survival an-alysis, we also stratified the patients by age and BMI according the Method section. We found that patients’ age ≥ 65 years resulted in lower survival rates in the underweight and normal weight groups, and age ≥ 75 year resulted in lower survival rates in the overweight and obese group. However, the survival rates were not significantly different among the 4 age-categorized groups, which stratified by BMI category. (data not shown).
Figure 2.
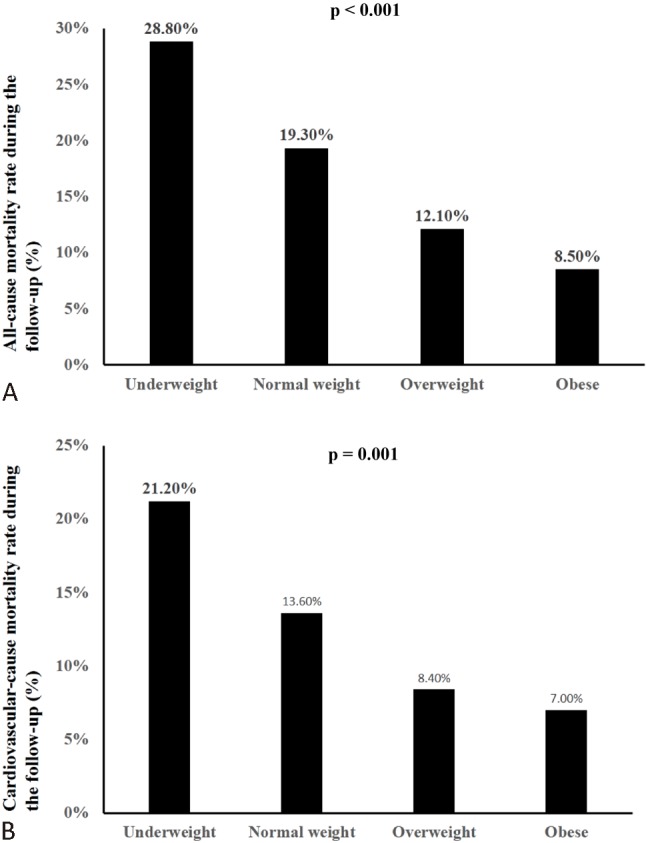
The overall mortality significantly differed among the 4 study groups during the follow-up period (p < 0.001).
Figure 3.
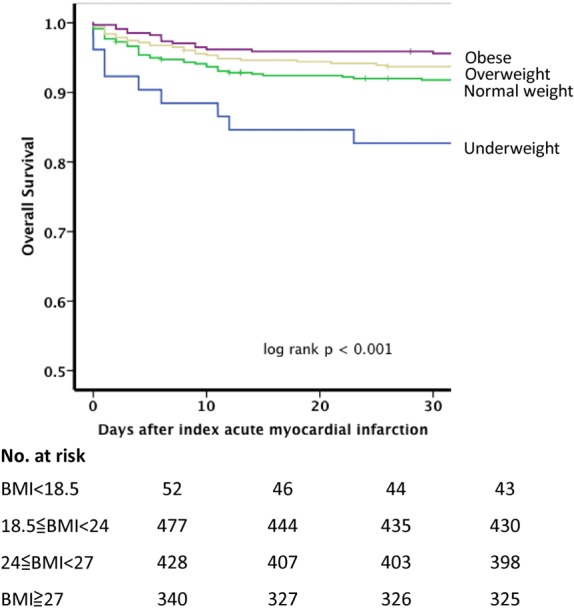
Kaplan-Meir survival curve analysis for 30-day survival rates among 4 study groups (log rank p < 0.001).
Figure 4.
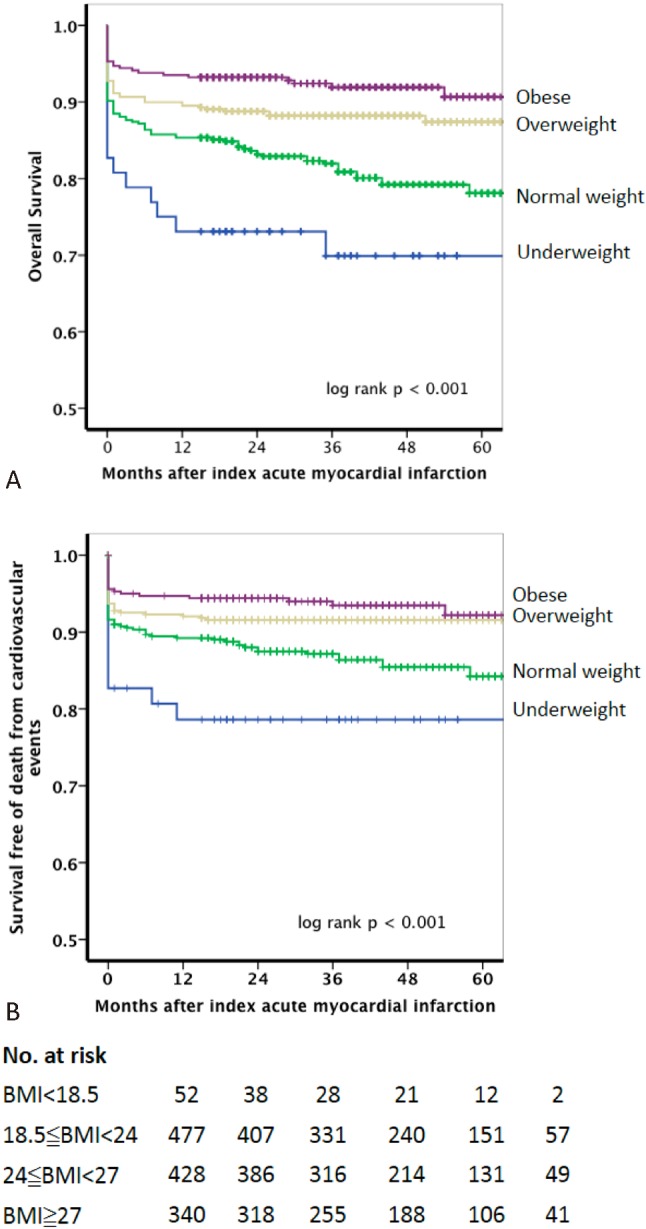
Kaplan-Meir survival curve analysis for 5-year overall survival rates (A) and survival free of death from cardiovascular events (B) among 4 study groups (log rank p < 0.001).
To find out the predictors of 5-year all-cause mortality, we used univariate regression analysis and found old age (age ≥ 65 years), presence of chronic kidney disease (estimated glomerular filtration rate < 60 ml/kg/ 1.73 m2), BMI < 24 kg/m2, heart rate and systolic blood pressure at emergency room, lipid profile, and use of aspirin, clopidogrel, β-blockers, and angiotensin converting enzyme inhibitors/angiotensin II receptor blockers were related to mortality. In the multivariate regression analysis, we found that Killip class ≥ 2, lack of using statin, age ≥ 65 years, and hemoglobin < 12 g/dl were strong predictors, and chronic kidney disease was a weaker predictor. However, neither BMI < 24 kg/m2 nor other parameters were independent predictors for 5-year all-cause mortality (Table 3).
Table 3. Multivariate analysis of 5-year mortality stratified by presenting characteristics.
| Odds ratio | 95% confidence interval | p value | |
| Killip class ≥ 2 | 3.7 | 2.10-6.51 | < 0.001 |
| Lacking of using statin | 3.56 | 1.98-6.43 | < 0.001 |
| Age ≥ 65 years | 3.05 | 1.78-5.23 | < 0.001 |
| Hemoglobin < 12 g/dl | 2.22 | 1.42-3.48 | < 0.001 |
| Chronic kidney disease | 2.04 | 1.07-3.91 | 0.03 |
| Body mass index < 24 kg/m2 | 1.11 | 0.69-1.79 | 0.66 |
DISCUSSION
In the present study, we enrolled all patients who had acute myocardial infarction and received percutaneous coronary intervention, not only patients with ST-elevation myocardial infarction (STEMI) but also patients with non-ST-elevation myocardial infarction (NSTEMI). This made our study population more heterogeneous and more similar with the real world of acute coronary syndrome, unlike other studies which enrolled only STEMI, NSTEMI/unstable angina, or chronic stable angina patients.5,6,8,17,23 In our hospital, we strictly implanted the ACC/AHA AMI treatment guidelines,19-22 and we had a very high percentage of AMI patients who taking aspirin (99.3%), clopidogrel (98.8%), β-blockers (86%), and angiotensin converting enzyme inhibitors or angiotensin II receptor blockers (88.1%). Therefore, we could eliminate the effects of these drugs, or non-use of these drugs on mortality.
We also found the overweight and obese patients had worse serum concentrations of total cholesterol, low-density lipoprotein cholesterol and triglyceride, and higher hemoglobin than the underweight and normal weight patients. But the underweight and normal weight patients were older than the other 2 groups. Furthermore, the underweight patients had higher incidence of chronic kidney disease and were in a more severe clinical situation after acute myocardial infarction, according to the risk stratification by Killip class. After multivariate regression analysis, we demonstrated that higher Killip class, lack of using statin, elderly, anemia, and chronic kidney disease were associated with higher short-term and long-term mortality. The possible explanations of anemia in the underweight patients are older age, poor nutrition, and presence of chronic kidney disease. Recently, Lawler et al. also reported a similar result in which anemia in patients with acute coronary syndrome was independently associated with a significantly increased risk of early and late mortality.24
Some recent Asian clinical studies also demonstrated that BMI is not an independent factor affecting 1-year mortality,23,25 and possible independent predictors included chronic kidney disease, no use of statin, old age, higher Killip class and lower left ventricular ejection fraction.23 These findings were similar to that of our study, but our study had a longer follow-up period. In the Kaplan-Meier survival curve analysis, we found that lower 30-day survival rate occurred in the underweight patients after AMI, and the survival rate reached the trough (76.9%) at 1 year. This may imply that Killip class β 2 is the strongest predictor in underweight patients because other independent factors were chronic parameters. Furthermore, the 30-day overall survival in normal weight patients did not differ significantly when compared to the overweight and obese patients. However, the long-term survival rate decreased significantly after the 2-year follow-up. This may be due to other chronic parameters, such as older age, lack of using statin, chronic kidney disease and anemia. However, higher Killip class might play a lesser role on mortality after 2-year follow-up. In these independent predictors, only lack of using statin is the treatable parameter. In our study, we found that more patients were administered statins due to higher serum lipid concentration in the overweight and obese patients. Therefore, lack of using statin may cause long-term mortality and morbidity. The reason for lower rate of using statin may be due to the criteria of reimbursement of Taiwan’s Bureau of National Health Insurance, which did not reimburse statin if the serum cholesterol is less than 160 mg/dl or the low-density lipoprotein cholesterol is less than 100 mg/dl in AMI patients. Therefore, more aggressive treatment strategy on dyslipidemia is necessary.
Limitations
There are still some limitations of the present study. First, this study is not a prospective randomized study. Therefore, our study has all of the limitations of retrospective study. Second, it presents information from the experience in a single medical center. Third, the number of underweight patients is relatively small and the statistical power may be strong enough to exclude the other negative data to be conclusive.
CONCLUSIONS
Compared with underweight and obese patients, the underweight AMI patients had the worst 30-day and 5-year survival rates, and the normal-weight AMI patients had a similar 30-day mortality rate but a higher mortality rate after 2 years. In the present study, the major factors affecting long-term survival are more aggressive statin treatment and older age, but not obese paradox.
REFERENCES
- 1.Calle EE, Thun MJ, Petrelli JM, et al. Body-mass index and mortality in a prospective cohort of U.S.adults. New Engl J Med. 1999;341:1097–1105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 2.Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983;67:968–977. doi: 10.1161/01.cir.67.5.968. [DOI] [PubMed] [Google Scholar]
- 3.Yusuf S, Hawken S, Ounpuu S, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet. 2005;366:1640–1649. doi: 10.1016/S0140-6736(05)67663-5. [DOI] [PubMed] [Google Scholar]
- 4.Wilson PW, D’Agostino RB, Sullivan L, et al. Overweight and obesity as determinants of cardiovascular risk: the framingham experience. Arch Intern Med. 2002;162:1867–1872. doi: 10.1001/archinte.162.16.1867. [DOI] [PubMed] [Google Scholar]
- 5.Gurm HS, Brennan DM, Booth J, et al. Impact of body mass index on outcome after percutaneous coronary intervention (the obesity paradox) Am J Cardiol. 2002;90:42–45. doi: 10.1016/s0002-9149(02)02384-6. [DOI] [PubMed] [Google Scholar]
- 6.Gurm HS, Whitlow PL, Kip KE, Investigators B. The impact of body mass index on short- and long-term outcomes inpatients undergoing coronary revascularization. Insights from the bypass angioplasty revascularization investigation (BARI) J Am Coll Cardiol. 2002;39:834–840. doi: 10.1016/s0735-1097(02)01687-x. [DOI] [PubMed] [Google Scholar]
- 7.Gruberg L, Weissman NJ, Waksman R, et al. The impact of obesity on the short-term and long-term outcomes after percutaneous coronary intervention: the obesity paradox? J Am Coll Cardiol. 2002;39:578–584. doi: 10.1016/s0735-1097(01)01802-2. [DOI] [PubMed] [Google Scholar]
- 8.Minutello RM, Chou ET, Hong MK, et al. Impact of body mass index on in-hospital outcomes following percutaneous coronary intervention (report from the New York State Angioplasty Registry) Am J Cardiol. 2004;93:1229–1232. doi: 10.1016/j.amjcard.2004.01.065. [DOI] [PubMed] [Google Scholar]
- 9.Shyu KG, Wu CJ, Mar GY, et al. Clinical characteristics, management and in-hospital outcomes of patients with acute coronary syndrome - observations from the Taiwan ACS Full Spectrum Registry. Acta Cardiol Sin. 2011;27:135–144. [Google Scholar]
- 10.Huang WC, Chiou KR, Liu CP, et al. Multidetector row computed tomography can identify and characterize the occlusive culprit lesions in patients early (within 24 hours) after acute myocardial infarction. Am Heart J. 2007;154:914–922. doi: 10.1016/j.ahj.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 11.Hsu HP, Jou YL, Lin SJ, et al. Comparison of in-hospital outcome of acute ST elevation myocardial infarction in patients with versus without diabetes mellitus. Acta Cardiol Sin. 2011;27:145–151. [Google Scholar]
- 12.Hsu HP, Jou YL, Wu TC, et al. Hyperglycemia increases new-onset atrial fibrillation in patients with acute ST-elevation myocardial infarction. Acta Cardiol Sin. 2012;28:279–285. [Google Scholar]
- 13.Huang SS, Leu HB, Lu TM, et al. The impacts of in-hospital invasive strategy on long-term outcome in elderly patients with non-ST-elevation myocardial infarction. Acta Cardiol Sin. 2013;29:115–123. [PMC free article] [PubMed] [Google Scholar]
- 14.Wang WH, Hsiao SH, Chiou KR, et al. Limited efficacy of myocardial tissue doppler for predicting left ventricular filling pressure, severe pulmonary edema,and respiratory failure in acute myocardial infarction. Acta Cardiol Sin. 2012;28:206–215. [Google Scholar]
- 15.Huang WC, Wu MT, Chiou KR, et al. Assessing culprit lesions and active complex lesions in patients with early acute myocardial infarction by multidetector computed tomography. Circ J. 2008;72:1806–1813. doi: 10.1253/circj.cj-08-0165. [DOI] [PubMed] [Google Scholar]
- 16.Dhoot J, Tariq S, Erande A, et al. Effect of morbid obesity on in-hospital mortality and coronary revascularization outcomes after acute myocardial infarction in the United States. Am J Cardiol. 2013;111:1104–1110. doi: 10.1016/j.amjcard.2012.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buettner HJ, Mueller C, Gick M, et al. The impact of obesity on mortality in UA/non-ST-segment elevation myocardial infarction. Eur Heart J. 2007;28:1694–1701. doi: 10.1093/eurheartj/ehm220. [DOI] [PubMed] [Google Scholar]
- 18.Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Circulation. 2012;126:2020–2035. doi: 10.1161/CIR.0b013e31826e1058. [DOI] [PubMed] [Google Scholar]
- 19.Kushner FG, Hand M, Smith SC, Jr., et al. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2009;120:2271–2306. doi: 10.1161/CIRCULATIONAHA.109.192663. [DOI] [PubMed] [Google Scholar]
- 20.Antman EM, Hand M, Armstrong PW, et al. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 writing group to review new evidence and update the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction, writing on behalf of the 2004 Writing Committee. Circulation. 2008;117:296–329. doi: 10.1161/CIRCULATIONAHA.107.188209. [DOI] [PubMed] [Google Scholar]
- 21.Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction) Circulation. 2004;110:e82–e292. [PubMed] [Google Scholar]
- 22.Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST-elevation myocardial infarction:a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 2002 guidelines for the management of patients with unstable angina/non ST-elevation myocardial infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Circulation. 2007;116:e148–e304. doi: 10.1161/CIRCULATIONAHA.107.181940. [DOI] [PubMed] [Google Scholar]
- 23.Kang WY, Jeong MH, Ahn YK, et al. Obesity paradox in Korean patients undergoing primary percutaneous coronary intervention in ST-segment elevation myocardial infarction. J Cardiol. 2010;55:84–91. doi: 10.1016/j.jjcc.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 24.Lawler PR, Filion KB, Dourian T, et al. Anemia and mortality in acute coronary syndromes: a systematic review and meta-analysis. Am Heart J. 2013;165:143–153, e5. doi: 10.1016/j.ahj.2012.10.024. [DOI] [PubMed] [Google Scholar]
- 25.Ndrepepa G, Keta D, Byrne RA, et al. Impact of body mass index on clinical outcome in patients with acute coronary syndromes treated with percutaneous coronary intervention. Heart Vessels. 2010;25:27–34. doi: 10.1007/s00380-009-1160-3. [DOI] [PubMed] [Google Scholar]


